Abstract
Objective
To characterize the types of hospices with higher rates of patient dis-enrollment from the Medicare Hospice Benefit and the markets in which these hospices operate.
Data Source
Secondary analyses of Surveillance, Epidemiology and End Results (SEER)-Medicare data. Analyses included patients who died of cancer from 1998–2002 and who used hospice (N=90,826).
Study Design
We used generalized estimating equations to estimate the association of patient dis-enrollment with hospice size, years since Medicare certification, ownership, staff mix, competition, urban/rural status, region and fiscal intermediary. Other covariates included patient demographic and clinical characteristics.
Principal Findings
Patients were more likely to dis-enroll from hospice if they were served by newer hospices (OR=1.14, 95%CI 1.03, 1.26), by smaller hospices (OR=1.11, 95%CI 1.02, 1.20), or by hospices in more competitive markets (OR=1.17, 95%CI 1.03, 1.35). There was an independent effect of the hospice's fiscal intermediary on dis-enrollment, particularly dis-enrollment after 6 months with hospice (Wald χ2 = 21.2, p=0.006).
Conclusions
The reasons for higher dis-enrollment rates for newer hospices, for smaller hospices, and for hospices in highly competitive markets are likely complex; however, results suggest there are organizational-level barriers to keeping patients with cancer enrolled with hospice. Variation across fiscal intermediaries may indicate that regulatory oversight, particularly of long-stay patients, influences hospice dis-enrollment.
Keywords: Health care organization, hospice, Medicare hospice benefit
Approximately 10–15 percent of individuals with serious illness who enroll in the Medicare Hospice Benefit (MHB) subsequently dis-enroll from hospice prior to death (Carlson et al. 2008b; Casarett, Marenberg, and Karlawish 2001; Taylor et al. 2008). Dis-enrollment has been shown to be associated with greater likelihoods of hospitalization, emergency department use, intensive care unit admission, and hospital death (Carlson et al. 2008b). Patients who dis-enroll from hospice are almost 5 times more expensive to the Medicare program, on average, than those who remain with hospice until death (Carlson et al. 2008b). In addition, hospice dis-enrollment may be a marker for poor quality care and may limit access to interdisciplinary palliative care services at the end of life for patients and families.
Despite these concerns about individuals who dis-enroll from hospice, we know little about the hospice-level variation in dis-enrollment rates and the types of hospices with higher dis-enrollment rates. Hospice dis-enrollment may be initiated either by the patient or the hospice. Patients may revoke their election of hospice due to dis-satisfaction with hospice care, a change in preferences for hospice care, or the desire to pursue treatments not covered under the Medicare Hospice Benefit (MHB) (e.g., radiation or chemotherapy). A hospice may discharge a patient if the hospice determines the patient is no longer eligible for hospice care (i.e., terminally ill, defined as having a life expectancy of 6 months or less), the patient moves out of the hospice's service area, or the patient is admitted to a hospital that does not have a hospice contract. Previous studies, which have focused exclusively on patient-level factors associated with dis-enrollment, have identified younger age (Casarett et al. 2001; Johnson et al. 2008), non-White race (Johnson et al. 2008), male gender (Casarett et al. 2001), and non-cancer diagnosis (Casarett et al. 2001; Johnson et al. 2008) as associated with hospice dis-enrollment. However, we could find no previous studies that have examined characteristics of the hospice or of the market in which the hospice operates that might be associated with higher dis-enrollment rates.
Evaluating hospice-level characteristics associated with dis-enrollment may provide key insights into the system of care for hospice services in the U.S. We hypothesize that higher dis-enrollment rates for some types of hospices, including those that are less established, smaller, or lacking a full range of multidisciplinary staff, may indicate a lack of resources or inadequate care processes to manage the increasingly complex patient population served by hospice. Higher dis-enrollment rates for some hospices might also indicate variation in patients' and families' understanding of hospice prior to enrollment. We hypothesize that for-profit hospices may have higher dis-enrollment rates given that they have been found to provide a narrower range of hospice services to patients (Carlson, Gallo, and Bradley 2004). We also anticipate that hospices in more competitive markets or in urban areas may have higher rates of dis-enrollment because patients in these markets may be better able to switch to another hospice or palliative care provider if they are not satisfied with their care. Variation in dis-enrollment rates across hospice fiscal intermediaries might indicate variation in fiscal intermediaries' interpretation or enforcement of hospice eligibility criteria. For instance, fiscal intermediaries, who oversee hospices on a contract-basis for the Centers for Medicare and Medicaid Services (CMS), may provide different guidance or incentives to hospices for adhering to eligibility criteria.
We hypothesize that hospice-level features are significantly associated with patient dis-enrollment. Accordingly, we examined hospice-level variation in dis-enrollment rates in a national sample of hospice agencies and the association between characteristics of hospices (i.e., age since Medicare certification, size, ownership, staffing, market competitiveness, urban/rural location, fiscal intermediary, and region) and hospice dis-enrollment. Identifying the types of hospice agencies with higher dis-enrollment rates is critical in addressing potential organizational-level barriers to having patients and families remain with hospice care continuously until death.
METHODS
Sample
Our sample includes patients in the linked Surveillance, Epidemiology and End Results (SEER)-Medicare database (National Cancer Institute) who died with a primary diagnosis of cancer between 1998 and 2002 at age 66 or older and who used hospice during any part of the 6 months prior to death. We included patients aged 66 or older to ensure that individuals were eligible for Medicare in the year prior to death, to access data on comorbidity in the year prior to death. A primary diagnosis of cancer was identified as one with an International Classification of Diseases (9th revision) Clinical Modification (ICD-9-CM) code (US Department of Health and Human Services March 1989) between 140 and 239. We excluded patients who were enrolled in a Medicare managed care organization because their non-hospice claims and utilization data are not available in the SEER-Medicare database. We linked the SEER-Medicare data to the Medicare Provider of Services data by hospice provider number. The Yale School of Medicine Institutional Review Board approved this study.
Dependent and Independent Variables
The dependent variable was patient dis-enrollment from hospice. Patient demographic characteristics were age at death, reported race/ethnicity, sex, and marital status at the time of entry into the SEER cancer registry. Patient clinical characteristics were primary cancer diagnosis (colon, pancreatic, lung, breast, ovarian, prostate, kidney, bladder, uterine, lymph, or other), Charlson comorbidity index, and receipt of only the home hospice level of care compared with at least 1 day of the inpatient hospice level of care. We calculated the Charlson comorbidity index (Charlson et al. 1987; Klabunde et al. 2000) using the comorbidity weights and methodology suggested by NCI (National Cancer Institute) for use with the SEER-Medicare data. Specifically, for each individual, we reviewed all Medicare inpatient hospital, inpatient and outpatient physician, and hospice claims for the year prior to death to identify comorbid conditions. We included in the model specification length of hospice stay from hospice enrollment to death or dis-enrollment (measured at the quartiles of the distribution as ≤ 7 days, 8–17 days, 18–46 days, and ≥46 days) because we believe it is a potential confounder of the association between hospice characteristics and dis-enrollment. That is, certain types of hospices may tend to care for patients with types of cancers with longer length of stay and those patients may be more or less likely to dis-enroll. We also included the patient's year of death.
Hospice agency characteristics were: ownership (for-profit or non-profit), number of years the hospice had been Medicare certified (measured as <5 or ≥ 5 years since Medicare certification), number of full-time equivalent employees of the hospice (measured at the median of the distribution as ≤ 13 or > 13), , Census region, urban/rural location (measured as whether the hospice's county had ≥ 1 million population) and the hospice's fiscal intermediary. We chose a cut-off of <5 years for the number of years since Medicare certification as this represented the lower 20th percentile for all hospices and was consistent with the definition of a “new” hospice used in a previous study (Christakis, and Iwashyna 2000). We performed sensitivity analyses using cut-off values of 4 years (the lower 10th percentile) and 7 years (the lower 25th percentile). Hospice size is measured as ≤ 13 or > 13 full-time equivalent employees of the hospice based on the median of the distribution. We performed sensitivity analyses using cut-offs of 10 and 15 full-time equivalent employees.
Competition in a hospice's market was estimated by a Herfindahl index (measured as highly competitive, Herfindahl index ≤0.10 or less competitive, Herfindahl index >0.10). We used a variable market area approach (Baker 2001) to define hospice market areas. Specifically, we defined the set of counties from which the hospice was observed to draw any of its patients and defined the hospice's market as including only those counties. This method has been previously used in studies of hospitals (Melnick et al. 1992; Zwanziger, and Melnick 1988) and health maintenance organizations (Wholey, Feldman, and Christianson 1995). We used Medicare hospice claims data to identify the counties from which each hospice drew its patients. Consistent with a prior study (Kessler, and McClellan 2000), we calculated the hospice-level Herfindahl index as the weighted average of county-level Herfindahl indexes for the counties from which a hospice drew its patients, where the weights were each county's share of the hospice's Medicare patient load. The advantage of a variable market area approach compared with a fixed market area approach (e.g., defining a hospice's market as all counties within a 15 mile radius of the hospice) is that it accounts for the fact that some hospices draw patients from a larger geographic area than others (Baker 2001).
Statistical Analyses
We summarized patient and hospice characteristics for the total sample and estimated the bivariate associations between hospice dis-enrollment and patient and hospice characteristics. We used logistic generalized estimating equations (GEE) (Liang, and Zeger 1986) to estimate the associations between dis-enrollment and patient characteristics and we used t-tests and analysis of variance to compare unadjusted dis-enrollment rates by hospice characteristics. For hospices with at least 10 observations per year, we created a histogram reporting the distribution of dis-enrollment rates by hospice.
We used multivariate logistic GEE's to estimate the associations between dis-enrollment and patient characteristics and hospice characteristics (Liang, and Zeger 1986). All tests were performed using techniques to account for the clustering of patient observations within hospices.
In subgroup analyses, we estimated three separate multivariate models. First, we estimated a model for patients who dis-enrolled within 2 weeks of enrolling with hospice (i.e., “early dis-enrollment”) compared with patients who were enrolled with hospice for at least 2 weeks and remained with hospice until death. We chose the cut-off of 2 weeks to capture patients who may not have understood, desired, or been eligible for hospice care at the time of enrollment as most patients and families report having incomplete knowledge and understanding of hospice at the time of hospice admission (Casarett, Crowley, and Hirschman 2004). We performed sensitivity analyses using alternative cut-offs, and results did not materially differ. Second, we estimated a model for patients who dis-enrolled after 6 months of hospice care (i.e., “late dis-enrollment”) compared with patients who were enrolled with hospice for at least 6 months and remained with hospice until death. We defined late dis-enrollment to correspond to the MHB eligibility criteria that a patient has life expectancy of 6 months or less at the time of enrollment. Third, we estimated a model for the subgroup of patients who dis-enrolled from hospice (at any time) and were immediately hospitalized, defined as hospitalized within 2 days of hospice dis-enrollment (i.e., “crisis-dis-enrollment”), compared with patients who were enrolled with hospice continuously until death.
RESULTS
Characteristics of Patients
Our study sample included 90,826 individuals who died with a primary diagnosis of cancer and used hospice during the period 1998–2002 (Table 1). The average patient age at death was 78.5 years and 86 percent of hospice patients were reported to be White non-Hispanic. Fifty-two percent of the patients in the sample were female, and 49 percent were married. Twenty-six percent of patients had a primary diagnosis of lung cancer, followed by 12% with colon cancer and 9% with prostate cancer. The mean patient Charlson co-morbidity index value was 1.2 (standard deviation=1.3) and the range was 0 to 12. Approximately 86 percent received only the home hospice level of care. The mean and median lengths of stay with hospice were 41.0 days (standard deviation 67.3 days) and 17 days, respectively.
TABLE 1.
Patient Characteristics and Hospice Dis-Enrollment Rates
| Total | Dis-enroll from Hospice | Remain with Hospice Until Death | Unadjusted | |||||
|---|---|---|---|---|---|---|---|---|
| N=90,826 | % | N=9,936 | % | N=80,890 | % | OR | 95% CI | |
| Age at Death | ||||||||
| < 70 years | 10,682 | 11.8% | 1,208 | 11.3% | 9,474 | 88.7% | 1.00 | |
| 70 to 77 years | 31,944 | 35.2% | 3,370 | 10.5% | 28,574 | 89.5% | 0.93 | (0.87, 1.00) |
| 78 to 84 years | 28,526 | 31.4% | 3,138 | 11.0% | 25,388 | 89.0% | 0.97 | (0.91, 1.04) |
| 85 years and older | 19,674 | 21.7% | 2,220 | 11.3% | 17,454 | 88.7% | 0.99 | (0.92, 1.06) |
| Race | ||||||||
| White Non-Hispanic | 77,662 | 85.5% | 8,029 | 10.3% | 69,633 | 89.7% | 1.00 | |
| White Hispanic | 3,540 | 3.9% | 478 | 13.5% | 3,062 | 86.5% | 1.27 | (1.15, 1.40)** |
| Black | 6,672 | 7.3% | 976 | 14.6% | 5,696 | 85.4% | 1.51 | (1.40, 1.62)** |
| Other | 2,829 | 3.1% | 443 | 15.7% | 2,386 | 84.3% | 1.59 | (1.37, 1.83)** |
| Unknown | 123 | 0.1% | 10 | 8.1% | 113 | 91.9% | ||
| Sex | ||||||||
| Female | 47,168 | 51.9% | 5,063 | 10.7% | 42,105 | 89.3% | 1.00 | |
| Male | 43,658 | 48.1% | 4,873 | 11.2% | 38,785 | 88.8% | 1.04 | (1.00, 1.09)* |
| Marital Status | ||||||||
| Married | 44,332 | 48.8% | 4,758 | 10.7% | 39,574 | 89.3% | 1.00 | |
| Not married | 42,483 | 46.8% | 4,749 | 11.2% | 37,734 | 88.8% | 1.04 | (1.01, 1.08)* |
| Unknown | 4,011 | 4.4% | 429 | 10.7% | 3,582 | 89.3% | ||
| Site of Primary Cancer | ||||||||
| Lung | 23,550 | 25.9% | 2,455 | 10.4% | 21,095 | 89.6% | 1.00 | |
| Colon | 10,839 | 11.9% | 1,238 | 11.4% | 9,601 | 88.6% | 1.04 | (1.01, 1.16)* |
| Prostate | 8,066 | 8.9% | 967 | 12.0% | 7,099 | 88.0% | 1.13 | (1.05, 1.22)* |
| Breast | 6,432 | 7.1% | 743 | 11.6% | 5,689 | 88.4% | 1.09 | (1.00, 1.19)* |
| Pancreas | 5,869 | 6.5% | 616 | 10.5% | 5,253 | 89.5% | 1.00 | (0.92, 1.09) |
| Bladder | 3,126 | 3.4% | 302 | 9.7% | 2,824 | 90.3% | 0.91 | (0.81, 1.03) |
| Lymph | 2,954 | 3.3% | 298 | 10.1% | 2,656 | 89.9% | 0.96 | (0.84, 1.09) |
| Ovarian | 2,280 | 2.5% | 217 | 9.5% | 2,063 | 90.5% | 0.89 | (0.78, 1.01) |
| Kidney | 2,108 | 2.3% | 260 | 12.3% | 1,848 | 87.7% | 1.19 | (1.05, 1.35)* |
| Uterine | 1,721 | 1.9% | 179 | 10.4% | 1,542 | 89.6% | 0.98 | (0.84, 1.14) |
| Other | 23,881 | 26.3% | 2,661 | 11.1% | 21,220 | 88.9% | 1.06 | (1.01, 1.12)* |
| Comorbidity Index Value | ||||||||
| 0 | 35,642 | 39.2% | 3,917 | 11.0% | 31,725 | 89.0% | 1.00 | |
| 1 or more | 55,184 | 60.8% | 6,019 | 10.9% | 49,165 | 89.1% | 1.03 | (1.00, 1.07) |
| Type of Hospice Care | ||||||||
| Inpatient | 12,331 | 13.6% | 1,096 | 8.9% | 11,235 | 91.1% | 1.00 | |
| Home hospice only | 78,495 | 86.4% | 8,840 | 11.3% | 69,655 | 88.7% | 1.22 | (1.14, 1.30)** |
P<0.05
P<0.001
Dis-enrollment Rates of Patients
A total of 9,936 patients dis-enrolled from hospice prior to death. The median number of days from hospice enrollment to dis-enrollment was 28, and the median number of days from hospice dis-enrollment to death was 24. The majority (62 percent) of patients who dis-enrolled from hospice did not enroll with hospice again; 38 percent of patients who dis-enrolled from hospice re-enrolled a median of 28 days later. Of those who re-enrolled, 75 percent re-enrolled with the same hospice agency and 25 percent re-enrolled with a different hospice agency. For patients who re-enrolled with hospice and died with hospice, death occurred a median of 24 days following re-enrollment. There were 3,454 patients (35 percent of dis-enrollees) who dis-enrolled from hospice within 2 weeks of initiating hospice care (i.e., “early dis-enrollment”) and 751 patients (8 percent of dis-enrollees) who dis-enrolled from hospice after 6 months of hospice care (i.e., “late dis-enrollment”). Approximately 25 percent of patients who dis-enrolled from hospice were hospitalized within 2 days of hospice dis-enrollment (n=2,503). Dis-enrollment rates by patient characteristics are shown in Table 1.
Characteristics of Hospices
The patients in this sample were served by 1,384 hospices (Table 2). The mean and median number of years since Medicare certification were 8.9 (standard deviation 5.0) and 8.0, respectively. The inter-quartile range was 5 to 13 years and the majority (77 percent) of hospices had been Medicare certified for 5 or more years. Most hospices (62 percent) were nonprofit. The mean and median number of full-time equivalent employees of the hospice were 27.2 (standard deviation 48.4) and 13.3, respectively. The inter-quartile range was 7.3 to 27.8 full-time equivalent employees. Most hospices (90 percent) operated in a less competitive market and 57 percent operated in an urban area. The fiscal intermediary for approximately one-third (36 percent) of hospices in the sample was Blue Cross South Carolina, followed by Blue Cross Iowa (16 percent), and Blue Cross California (16 percent).
TABLE 2.
Hospice Characteristics and Hospice Dis-Enrollment Rates
| Total N=1,384 | % | Dis-Enrollment Rate | |
|---|---|---|---|
| Years since Medicare certification | |||
| < 5 years | 317 | 22.9% | 17.3% |
| ≥ 5 years | 1,067 | 77.1% | 14.6% |
| Size | |||
| ≤ 13 full-time equivalent employees | 682 | 49.3% | 16.1% |
| > 13 full-time equivalent employees | 702 | 50.7% | 14.5% |
| Ownership | |||
| For-profit ownership | 419 | 30.3% | 15.0% |
| Nonprofit | 862 | 62.3% | 15.1% |
| Government | 67 | 4.8% | |
| Unkown | 37 | 2.7% | |
| Market competition | |||
| Highly competitive market | 138 | 10.0% | 18.1% |
| Less competitive market | 1,246 | 90.0% | 14.9% |
| Urban/rural location | |||
| Urban | 792 | 57.2% | 14.6% |
| Rural | 592 | 25.2% | 16.1% |
| Fiscal intermediary | |||
| Cahaba | 53 | 3.8% | 15.6% |
| Blue Cross Iowa | 220 | 15.9% | 14.4% |
| Blue Cross Maine | 64 | 4.6% | 20.1% |
| Blue Cross South Carolina | 500 | 36.1% | 16.1% |
| Blue Cross California | 219 | 15.8% | 16.9% |
| U.S. Government California | 42 | 3.0% | 12.9% |
| Mutual of Omaha | 24 | 1.7% | 20.7% |
| Other | 70 | 5.1% | 9.3% |
| Blue Cross Wisconsin | 192 | 13.9% | 12.4% |
| Census region | |||
| Middle Atlantic | 122 | 8.8% | 13.7% |
| South Atlantic | 202 | 14.6% | 14.3% |
| East North Central | 182 | 13.2% | 11.2% |
| West North Central | 160 | 11.6% | 14.9% |
| East South Central | 90 | 6.5% | 20.8% |
| West South Central | 156 | 11.3% | 14.5% |
| Mountain | 158 | 11.4% | 17.7% |
| Pacific | 245 | 17.7% | 15.6% |
| New England | 69 | 5.0% | 20.2% |
* P<0.05; ** P<0.001
Dis-enrollment and Hospice Characteristics
Hospice dis-enrollment rates varied according to hospice characteristics (Table 2). Unadjusted analyses demonstrated that newer hospices (those with <5 years since Medicare certification) had higher disenrollment rates than older hospices (17.3% versus 14.6%, p=0.116), smaller hospices (those with ≤ 13 full-time equivalent employees) had higher dis-enrollment rates than larger hospices (16.1% versus 14.5%, p=0.230), hospices in competitive markets had higher dis-enrollment rates than those in less competitive markets (18.1 percent versus 14.9 percent, p=0.152), and hospices in rural areas had higher dis-enrollment rates than hospices in urban areas (16.1% versus 14.6%, p=0.282).
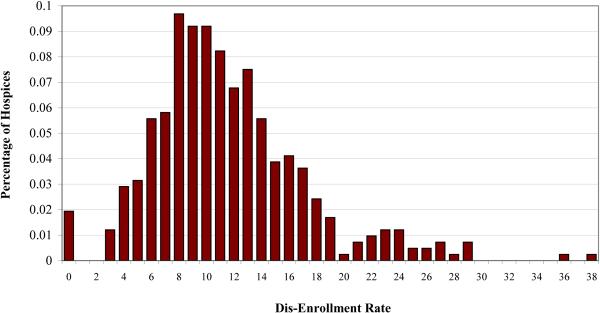
The mean dis-enrollment rate across all hospices in the sample was 15.3 percent (standard deviation = 24.5). However, there was substantial variation across hospices in this rate, which ranged from 0 percent dis-enrollment to 100 percent dis-enrollment. All hospices with 100 percent dis-enrollment had 3 or fewer observations per year. Excluding hospices with fewer than 10 observations per year, the mean dis-enrollment rate across hospices was 11.5 percent (standard deviation = 5.6) and ranged from 0 percent dis-enrollment to 38 percent dis-enrollment (Figure 1).
FIGURE 1.
Variability By Hospice in Patient Dis-Enrollment Rate*
* Includes hospices with at least 10 observations per year
Multivariate Results
In multivariate models, patients served by newer hospices (hospices within 5 years of initial Medicare certification date) were more likely to dis-enroll than those served by hospices that had been Medicare certified for 5 years or more (OR=1.14, 95%CI 1.03, 1.26) (Table 3). Compared with smaller hospices (those with ≤13 full-time equivalent employees), larger hospices (those with >13 full-time equivalent employees) had higher dis-enrollment rates (OR=1.11, 95%CI 1.02, 1.20). Patients served by hospices in highly competitive markets were more likely to dis-enroll compared with those in less competitive markets (OR=1.17, 95%CI 1.03, 1.35). The hospice's fiscal intermediary was also significantly associated with variation in patient dis-enrollment (χ2 = 18.6, p=0.017). Due to multi-collinearity between the hospice's fiscal intermediary and Census region (Cramer's V statistic=0.57) (Cramer 1946), Census region was excluded from the multivariate models. Hospice ownership and urban location were not significantly associated with patient dis-enrollment.
TABLE 3.
Hospice and Patient Characteristics Associated with Hospice Dis-enrollment
| Dis-enroll vs. Remain with Hospicea | Dis-enroll within 2 weeks vs. Remain with Hospiceb | Dis-enroll after 6 months vs. Remain with Hospicec | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Hospice Characteristics: | ||||||
| < 5 years since Medicare certification | 1.14 | (1.03, 1.26)* | 1.20 | (1.05, 1.38)* | 0.97 | (0.70, 1.34) |
| ≤ 13 full-time equivalent employees | 1.11 | (1.02, 1.20)* | 1.16 | (1.04, 1.29)* | 0.97 | (0.79, 1.20) |
| For-profit ownership | 0.97 | (0.88, 1.07) | 0.98 | (0.85, 1.12) | 0.99 | (0.77, 1.27) |
| Highly competitive market | 1.17 | (1.03, 1.35)* | 1.34 | (1.11, 1.60)* | 1.09 | (0.75, 1.59) |
| Urban location | 1.03 | (0.94, 1.13) | 1.10 | (0.97, 1.24) | 1.07 | (0.83, 1.38) |
| Fiscal intermediaryd (reference is Blue Cross Wisconsin) | ||||||
| Cahaba | 1.31 | (1.04, 1.64)* | 0.87 | (0.65, 1.16) | 2.42 | (1.47, 3.99)* |
| Blue Cross Iowa | 1.06 | (0.90, 1.25) | 0.88 | (0.70, 1.11) | 1.05 | (0.70, 1.59) |
| Blue Cross Maine | 1.31 | (1.10, 1.56)* | 0.99 | (0.80, 1.22) | 1.51 | (0.99, 2.32) |
| Blue Cross South Carolina | 1.22 | (1.06, 1.39)* | 1.18 | (0.99, 1.42) | 1.08 | (0.78, 1.50) |
| Blue Cross California | 1.11 | (0.98, 1.26) | 1.02 | (0.85, 1.22) | 1.07 | (0.79, 1.45) |
| U.S. Government California | 1.34 | (1.06, 1.69)* | 1.16 | (0.81, 1.68) | 1.49 | (0.80, 2.79) |
| Mutual of Omaha | 1.44 | (0.93, 2.20) | 0.95 | (0.66, 1.35) | 1.36 | (0.57, 3.28) |
| Other | 1.30 | (1.07, 1.58)* | 1.13 | (0.84, 1.53) | 1.78 | (1.05, 3.03)* |
| Patient Characteristics: | ||||||
| Age at death | 1.00 | (0.99, 1.00) | 0.99 | (0.99, 1.00)* | 1.01 | (1.00, 1.02)* |
| Race (reference is White non-Hispanic) | ||||||
| White Hispanic | 1.24 | (1.12, 1.38)** | 1.25 | (1.06, 1.48)* | 1.15 | (0.71, 1.85) |
| Black | 1.51 | (1.40, 1.63)** | 1.52 | (1.33, 1.74)** | 1.62 | (1.14, 2.29)* |
| Other | 1.61 | (1.39, 1.86)** | 1.86 | (1.53, 2.27)** | 1.48 | (0.84, 2.63) |
| Male | 1.09 | (1.03, 1.14)* | 1.16 | (1.05, 1.28)* | 1.08 | (0.87, 1.34) |
| Not married | 1.03 | (0.98, 1.07) | 0.96 | (0.88, 1.03) | 1.12 | (0.93, 1.35) |
| Site of Primary Cancere (reference is Lung) | ||||||
| Colon | 1.07 | (0.99, 1.15) | 1.04 | (0.91, 1.18) | 1.10 | (0.81, 1.50) |
| Prostate | 1.08 | (0.99, 1.18) | 0.97 | (0.84, 1.11) | 1.21 | (0.87, 1.68) |
| Breast | 1.11 | (1.02, 1.22)* | 0.98 | (0.85, 1.13) | 1.38 | (1.04, 1.83)* |
| Pancreas | 1.01 | (0.92, 1.12) | 1.08 | (0.92, 1.26) | 0.88 | (0.51, 1.54) |
| Bladder | 0.96 | (0.84, 1.09) | 1.10 | (0.88, 1.36) | 1.28 | (0.74, 2.22) |
| Lymph | 1.03 | (0.90, 1.19) | 1.32 | (1.08, 1.60)* | 1.84 | (1.04, 3.27)* |
| Ovarian | 0.98 | (0.85, 1.13) | 1.06 | (0.85, 1.32) | 0.79 | (0.45, 1.40) |
| Kidney | 1.18 | (1.03, 1.35)* | 1.17 | (0.94, 1.45) | 0.91 | (0.51, 1.62) |
| Uterine | 1.00 | (0.84, 1.20) | 0.99 | (0.75, 1.31) | 1.24 | (0.60, 2.56) |
| Other | 1.08 | (1.02, 1.15)* | 1.15 | (1.05, 1.26)* | 1.17 | (0.91, 1.51) |
| Comorbidity index | 1.05 | (1.04, 1.07)** | 1.10 | (1.07, 1.12)** | 1.07 | (1.00, 1.16) |
| Type of hospice care: home hospice only | 1.06 | (0.99, 1.14) | 0.87 | (0.78, 0.97)* | 0.80 | (0.57, 1.10) |
P<0.05
P<0.001
Models control for patient's year of death and days from hospice enrollment to death or dis-enrollment
Model control for patient's year of death
Model controls for patient's year of death and is conditional on surviving 6 months after hospice enrollment
Wald statistic for fiscal intermediary = 18.6, degrees of freedom=8, P-value=0.017
For dis-enrollment within 2 weeks, Wald statistic for fiscal intermediary = 10.4, degrees of freedom=8, P-value=0.237
For dis-enrollment after 180 days, Wald statistic for fiscal intermediary = 21.2, degrees of freedom=8, P-value=0.007
Wald statistic for site of primary cancer is =15.2, degrees of freedom=10, P-value=0.125
For dis-enrollment within 2 weeks, Wald statistic for site of primary cancer =19.7, degrees of freedom=10, P-value=0.032
For dis-enrollment after 180 days, Wald statistic for site of primary cancer =12.3, degrees of freedom=10, P-value=0.268
Sensitivity analyses using 4 years and 7 years since Medicare certification to characterize newer hospices (instead of 5 years) found similar effect sizes, although the estimated effect using 4 years was not significant. Thus, our main finding using 5 years to characterize newer hospices was not contradicted. Sensitivity analyses also demonstrated that the results were not sensitive to our characterization of a smaller hospice as one with 10 or 15 full-time equivalent employees of the hospice (instead of 13).
The patient characteristic most strongly associated with hospice dis-enrollment was reported race/ethnicity. Compared with patients reported to be White non-Hispanic, patients reported to be White Hispanic (OR=1.24, 95%CI 1.12, 1.38), Black (OR=1.51, 95%CI 1.40, 1.63) or Other race/ethnicity (OR=1.61, 95%CI 1.39, 1.86) were more likely to dis-enroll from hospice.
Characteristics Associated with Early and Late Hospice Dis-enrollment
Hospice characteristics associated with early and late dis-enrollment differed in a number of ways (Table 3). In the multivariable model of early dis-enrollment, patients served by newer hospices (OR=1.20, 95%CI 1.05, 1.38), smaller hospices (OR=1.16, 95%CI 1.04, 1.29) or hospices operating in competitive markets (OR=1.34, 95%CI 1.11, 1.60) were significantly more likely to dis-enroll. However, in the multivariable model of late dis-enrollment, there were no significant differences in dis-enrollment for patients served by newer hospices, smaller hospices, or hospices operating in competitive markets.Further, the hospice's fiscal intermediary was not significantly associated with early hospice dis-enrollment (χ2 = 10.4, 8df, p=0.237), but the hospice's fiscal intermediary was significantly associated with late hospice dis-enrollment (χ2 = 21.2, 8df, p=0.007).
Hospice Dis-enrollment and Immediate Hospitalization
In multivariable analysis, the factors independently associated with hospice dis-enrollment and immediate hospitalization were older age (OR=0.99, 95%CI 0.99, 1.00), being Black (OR=1.69, 95% CI 1.42, 2.01) or of Other race/ethnicity (OR=1.72, 95%CI 1.35, 2.18) compared with White non-Hispanic, having a higher Charlson comorbidity index value (OR=1.19, 95%CI 1.16, 1.23), being cared for by a newer hospice (OR=1.26, 95%CI 1.05, 1.51), being cared for being in a highly competitive market (OR=1.61, 95%CI 1.27, 2.05), and the hospice's fiscal intermediary (χ2 = 27.5, p=0.001).
DISCUSSION
We found that hospices have an average dis-enrollment rate of more than 15 percent for Medicare patients with terminal cancer, many of whom die within only a few weeks of hospice dis-enrollment. Dis-enrollment rates varied widely across hospices. Some hospices had no patients dis-enroll during the study period and other hospices had dis-enrollment rates as high as 38 percent. High dis-enrollment rates among this population of patients with terminal cancer is concerning, as hospice dis-enrollment is associated with greater likelihood of hospitalization and hospital death (Carlson et al. 2008b), higher Medicare expenditures (Carlson et al. 2008b), and may be a marker for poor quality of care at the end of life.
Hospice dis-enrollment varied by non-clinical characteristics, including the type of hospice from which the patient received his/her care, the fiscal intermediary assigned to the patient's hospice, and the market in which the hospice operated. Specifically, we found that newer hospices (i.e., those within 5 years of initial Medicare certification) and smaller hospices (i.e., those with 13 or fewer full-time equivalent employees) had higher dis-enrollment rates than larger, more established hospices. Over the past several decades, the population served by hospice has become increasingly complex (National Hospice and Palliative Care Organization 2007) with multiple medical, nursing, and caregiver needs. Our finding that newer and smaller hospices had higher dis-enrollment rates suggests that these programs may not be able to adequately meet the needs of their patients or may lack the ability to appropriately select patients who meet Medicare hospice eligibility criteria. Further, our finding that patients served by newer hospices were more likely to dis-enroll and be immediately hospitalized may indicate that newer hospices have difficulty managing certain crisis clinical situations at home without hospitalization.
We found higher hospice dis-enrollment in highly competitive compared with less competitive hospice markets. It may be that in competitive markets patients who are not satisfied with their care switch hospices and experience a gap in service delivery as they transfer from one hospice to another. However, we found little evidence of patients switching hospices. Only 10 percent of patients who dis-enrolled from hospice later re-enrolled with a different hospice agency. A more likely explanation is that in competitive markets, hospices compete for patients and are under increased pressure not to refuse the enrollment of patients, as refusal might strain preferred relationships with the hospice's primary referral sources (i.e., hospitals, long-term care institutions, and physician practices). Additionally, in competitive environments, hospices may have extensive outreach or open access programs and may be initially enrolling patients who may not fully understand hospice services, who may not yet be hospice eligible, or who may require services that the hospice is not able to provide. This explanation is consistent with our finding that more competitive markets have higher early dis-enrollment rates (i.e., dis-enrollment within 2 weeks of enrollment) but do not have higher late dis-enrollment rates. Understanding the dynamics of competitive markets and the potential influence of hospice competition on patient dis-enrollment is critical as the number of hospices continues to increase (National Hospice and Palliative Care Organization 2007).
An important source of variation in hospice dis-enrollment rates was the hospice's fiscal intermediary. The role of fiscal intermediaries is to administer the MHB program for CMS by processing claims, reimbursing hospices for Medicare-covered services, tracking beneficiary eligibility, and performing audits of hospice enrollment and services. Although guidelines exist to aid hospices in determining which patients might have a life expectancy of 6 months or less if their disease follows its usual course (MHB eligibility requirements), some hospice eligible patients may have stable disease, slowly progressive disease, or improvement in their disease while on hospice and may live longer than 6 months. Such patients are often scrutinized and may be discharged from hospice for “failure to die in a timely fashion.” Fiscal intermediaries face competition for CMS contracts and thus have incentives to demonstrate to Medicare that they are reducing hospice expenditures and rigorously overseeing hospice utilization. Although variation across fiscal intermediaries in dis-enrollment rates could be due to systematic geographic variation in fiscal intermediary practices, we found only moderate correlation between fiscal intermediary and region, with some fiscal intermediaries covering all 9 Census regions. A more likely explanation for substantial variation across fiscal intermediaries in overall and late hospice dis-enrollment is that some fiscal intermediaries interpret the Medicare prognostic guidelines more narrowly and thus exert more pressure on hospices to dis-enroll long-stay patients than other fiscal intermediaries, resulting in variation across hospices in the dis-enrollment rates of patients who have been in hospice for longer than 6 months.
Lastly, although not the focus of this study, we consistently found higher hospice dis-enrollment of patients reported to be non-White compared with patients reported to be White non-Hispanic. Although this may be due to a higher likelihood of patients reported to be non-White to dis-enroll from hospice to pursue disease-focused treatments, as was found in a recent study (Johnson et al. 2008), we also found higher early dis-enrollment, late dis-enrollment, and dis-enrollment followed by immediate hospitalization for patients reported to be non-White compared with patients reported to be White non-Hispanic. It is therefore unlikely that a preference for disease-remittive treatments is the sole reason for higher dis-enrollment among patients reported to be non-White and suggests that hospices may not be meeting the needs of some patients groups. At the same time, the current analysis does not rule out that this is a group effect. That is, hospices that treat higher proportions of certain patients also have higher dis-enrollment rates for all of their patients.
This is the first study to describe hospice-level variation in dis-enrollment from the MHB. However, limitations of these results exist. First, our sample consists of Medicare fee-for-service patients with cancer from the SEER registries, and their experiences and dis-enrollment rates may differ from patients with non-cancer diagnoses, with cancer diagnoses living outside the SEER registry areas, or with other sources of insurance. However, patients with cancer comprise almost half of all patients who enroll with hospice each year (National Hospice and Palliative Care Organization 2007) and they are thus an important sub-group of hospice users. Future studies regarding the dis-enrollment patterns of patients with non-cancer diagnoses are warranted. Second, our measures of hospice size is based on the number of full-time equivalent employees of the hospice and may over or under estimate the hospice's size based on patient census. These data are also cross-sectional and thus we cannot rule out bias due to omitted variables. Finally, these data are from 1998–2002 and thus may not reflect the current hospice market. However, we believe that the continued growth in the hospice market from 2002-present underscores the importance of our findings regarding higher dis-enrollment rates for newer hospices and hospices operating in competitive markets.
Identifying the types of hospices and markets with high dis-enrollment rates is a critical first step in understanding the potentially modifiable hospice-level factors associated with dis-enrollment. Policy efforts should focus on reducing variation in dis-enrollment rates across hospices, as such variation may signal variation in quality of care or hospice-specific barriers to remaining with hospice continuously until death. Policy interventions to reduce variation across hospices in dis-enrollment could target both the hospice and the fiscal intermediary. Specifically, CMS could require hospices to report their dis-enrollment rates and to identify reasons for patient dis-enrollment (e.g., to pursue treatment not covered by the MHB, unsatisfied with hospice care, no longer eligible). Given that CMS is developing reporting requirements for hospices that participate in Medicare (Medicare Payment Advisory Commission 2008), including the reporting of hospice dis-enrollment rates and reasons for dis-enrollment could be a relatively simple intervention. Second, CMS could develop ways of ensuring more equal enforcement of hospice eligibility criteria across fiscal intermediaries. A recent MedPAC report on hospice (Medicare Payment Advisory Commission 2008) suggests that there is inadequate guidance for hospices regarding the identification of patients appropriate for hospice admission across diagnoses and disease categories. Improving the consistency of information regarding hospice eligibility may help reduce the number of individuals who are considered no longer eligible for hospice and yet die within weeks of hospice dis-enrollment.
Hospice dis-enrollment creates discontinuity of care in the end of life and may limit access to potentially important inter-disciplinary palliative care services for patients and families. As we continue to discuss policy solutions for improving access to hospice care (Carlson, Morrison, and Bradley 2008a), it is critical to consider patients who have involuntarily lost access to hospice services due to dis-enrollment. The number of individuals choosing hospice care continues to grow, and it is thus critical to understand the substantial variation across hospices in dis-enrollment rates and to address the organization-level barriers to keeping patients who wish to receive hospice care until death, enrolled with hospice until death.
Acknowledgments
Funding Sources: This work was supported by the National Cancer Institute (1R01CA116398-01A2); Dr. Carlson is a Brookdale Leadership in Aging Fellow and recipient of an NINR Career Development Award (1K99NR010495-01); Dr. Bradley is supported by the Patrick and Catherine Weldon Donaghue Medical Research Foundation Investigator Award (Grant #02-102). Dr. Morrison is the recipient of a Mid-Career Investigator Award in Patient Oriented Research (K24 AG022345) from the National Institute on Aging
Footnotes
Financial Disclosures: none
Conflicts of Interest: none
REFERENCES
- Baker LC. Measuring competition in health care markets. Health Serv Res. 2001;36(1 Pt 2):223–51. [PMC free article] [PubMed] [Google Scholar]
- Carlson MD, Gallo WT, Bradley EH. Ownership status and patterns of care in hospice: results from the National Home and Hospice Care Survey. Med Care. 2004;42(5):432–8. doi: 10.1097/01.mlr.0000124246.86156.54. [DOI] [PubMed] [Google Scholar]
- Carlson MD, Morrison RS, Bradley EH. Improving access to hospice care: informing the debate. J Palliat Med. 2008a;11(3):438–43. doi: 10.1089/jpm.2007.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson MDA, Herrin J, Du Q, Epstein AJ, Barry CL, Morrison RS, Bradley EH. Expenditures by Medicare for Hospice Users. Academy Health Annual Research Meeting; Washington D.C.. June 2008.2008b. [Google Scholar]
- Casarett DJ, Crowley RL, Hirschman KB. How should clinicians describe hospice to patients and families? J Am Geriatr Soc. 2004;52(11):1923–8. doi: 10.1111/j.1532-5415.2004.52520.x. [DOI] [PubMed] [Google Scholar]
- Casarett DJ, Marenberg ME, Karlawish JH. Predictors of withdrawal from hospice. J Palliat Med. 2001;4(4):491–7. doi: 10.1089/109662101753381638. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ. Impact of individual and market factors on the timing of initiation of hospice terminal care. Med Care. 2000;38(5):528–41. doi: 10.1097/00005650-200005000-00009. [DOI] [PubMed] [Google Scholar]
- Cramer H. Mathematical Methods of Statistics. Princeton University Press; Princeton: 1946. [Google Scholar]
- Johnson KS, Kuchibhatla M, Tanis D, Tulsky JA. Racial differences in hospice revocation to pursue aggressive care. Arch Intern Med. 2008;168(2):218–24. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]
- Kessler DP, McClellan MB. Is Hospital Competition Socially Wasteful? The Quarterly Journal of Economics. 2000;115(2):577–616. [Google Scholar]
- Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Medicare Payment Advisory Commission . Report to the Congress: Reforming the Delivery System, Chapter 8: Evaluating Medicare's Hospice Benefit. Washington, D.C.: 2008. [Google Scholar]
- Melnick GA, Zwanziger J, Bamezai A, Pattison R. The effects of market structure and bargaining position on hospital prices. J Health Econ. 1992;11(3):217–33. doi: 10.1016/0167-6296(92)90001-h. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute SEER-Medicare: Calculation of Comorbidity Weights. Available at: http://healthservices.cancer.gov/seermedicare/program/comorbidity.html; Accessed: May 2007.
- National Cancer Institute Surveillance, Epidemiology, and End Results database. Description available at: http://healthservices.cancer.gov/seermedicare/
- National Hospice and Palliative Care Organization NHPCO 2007 Facts and Figures. 2007 Accessed Februrary 2008, Available at: http://www.nhpco.org/files/public/Statistics_Research/NHPCO_facts-and-figures_Nov2007.pdf” [accessed on 2007]. Available at.
- National Hospice and Palliative Care Organization NHPCO Facts and Figures, Hospice Care In America Accessed December 2008. 2008 Available at http://www.nhpco.org/files/public/Statistics_Research/NHPCO_facts-and-figures_2008.pdf” [accessed on 2008]. Available at.
- Taylor DH, Steinhauser K, Tulsky JA, Rattliff J, Van Houtven CH. Characterizing Hospice Discharge Patterns in a Nationally Representative Sample of the Elderly, 1993–2000. Am J Hosp Palliat Care. 2008 doi: 10.1177/1049909107310136. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services . The International Classification of Diseases. 9th Revision. Clinical Modification: Public Health Service, Health Care Financing Administration; Mar, 1989. pp. 89–1260. DHHS Publication No (PHS) [Google Scholar]
- Wholey D, Feldman R, Christianson JB. The effect of market structure on HMO premiums. J Health Econ. 1995;14(1):81–105. doi: 10.1016/0167-6296(94)00039-7. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Melnick GA. The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California. J Health Econ. 1988;7(4):301–20. doi: 10.1016/0167-6296(88)90018-5. [DOI] [PubMed] [Google Scholar]