Abstract
Objectives
We examined the use of voluntary HIV testing among state prisoners in the North Carolina prison system.
Methods
We calculated system-wide and facility-specific proportions and rates of adult inmates tested for HIV and estimated associations between testing status and inmate characteristics for prisoners in North Carolina.
Results
Of the 54016 inmates who entered prison between January 2004 and May 2006, 20820 (38%) were tested for HIV; of those tested, 18574 (89%) were tested at admission. Across the 8 intake prisons, more than 80% of inmates in both female facilities but less than 15% of inmates in 4 of 6 male facilities were tested. Prisoners with a documented history of heroin use, crack or cocaine use, conventional HIV risk behavior, or tuberculosis were at least 10% more likely to be tested than were inmates without these characteristics. However, more than 60% of men reporting conventional risk behaviors were not tested. Before covariate adjustment, Black men were 30% less likely than White men to be tested; in the multivariable regression model, this difference was attenuated to 13%.
Conclusions
Rates of HIV testing varied widely across intake prisons, and many male inmates with documented risk of infection were never tested.
The prevalence of HIV is disproportionately high among incarcerated individuals compared with the general US population.1 Although some evidence suggests that HIV is transmitted within prisons, most infections occur in the community.2,3 Given inmates’ limited access to community health care,4 prisons provide an important opportunity to conduct HIV testing.
Among the benefits of testing are that infected inmates can initiate medical care and, if appropriate, initiate highly active antiretroviral therapy (HAART). HAART is now widely available in prison systems, and prisoners have experienced declines in HIV-related mortality similar to those in the community.5,6 A positive HIV test may also initiate contact tracing to identify infection among inmates’ sexual or drug-using partners in the community and in prison.
HIV testing strategies vary across US state prison systems. According to Bureau of Justice statistics, 20 state prison systems have instituted mandatory HIV testing. The other 29 prison systems provide consent-based testing (data from Alaska were unavailable).7 Nearly all systems provide testing upon prisoners’ self-request. Among systems with consent-based testing, at least 2 provide opt-out testing (i.e., inmates are informed that they will be tested unless they actively decline)8 and 12 target testing to “high-risk” prisoners. Yet, little is known about the extent of HIV testing in prisons with consent-based testing or the degree to which testing in these systems includes prisoners with known risk factors. In addition, most existing US studies that examined the use of voluntary HIV testing were conducted before the era of HAART, and few have characterized the differences between testers and nontesters.9-14
In 2003, as part of its Advancing HIV Prevention initiative, the Centers for Disease Control and Prevention (CDC) recommended that correctional facilities offer HIV testing at the time of intake.15 With the CDC’s 2006 recommendations to improve access to HIV testing with the implementation of routine opt-out testing across health care settings, including correctional health care facilities,16 it is of renewed interest to examine the extent of HIV testing in prisons with consent-based testing. Low rates of testing may indicate missed opportunities to provide needed medical care and social support, reduce infectiousness via treatment, and provide counseling to reduce secondary transmission.
In our study, we examined the use of consent-based HIV testing in a large southern prison system, the North Carolina Department of Correction (NC DOC) Division of Prisons. We determined the proportion of inmates tested for HIV both during and after admission, examined differences in testing across intake prisons, and estimated associations between receipt of an HIV test and prisoner characteristics to detect disparities in testing, particularly among inmates with documented risk for infection.
METHODS
Before assignment to 1 of the 76 prisons in the NC DOC prison system, incoming inmates are admitted to 1 of 8 intake prisons that has a processing and diagnostic center. Two centers are designated for adult women, 4 for adult men, and 2 for younger men (i.e., younger than 22 years). Inmates receive a presentation about blood-borne diseases, including HIV. A medical evaluation is conducted including routine testing for syphilis and tuberculosis (TB). A nurse screens inmates for conventional HIV risk behaviors, and voluntary HIV testing is available; during the study period, it was NC DOC policy to offer inmates with known risk behaviors an HIV test. HIV testing is available anytime during incarceration by inmate self-request, by clinician recommendation, or after a blood exposure incident. Inmates testing positive are seen regularly by a physician who specializes in HIV treatment, and antiretroviral therapy is initiated per community recommendations. HIV testing is conducted with conventional enzyme-linked immunosorbent assay (ELISA) and Western blot tests. Inmates typically receive test results within 1 week. HCV antibody testing is provided to prisoners with clinical symptoms of hepatitis and to all prisoners with known HIV infection.
Assessments of inmates’ social (e.g., employment and marital status) and criminal histories are conducted by an NC DOC case analyst. The analyst relies on information from interviews with the prisoner and data generated both at arrest and during prior incarcerations.
Electronic Records and Data Linking
The NC DOC provided us electronic records of data collected routinely for all inmates entering the state prison system between January 1, 2004, and May 31, 2006. The records included demographic and social information, conviction offense and sentence, dates of imprisonment, mental health diagnoses, and results from education, substance abuse, and HIV-risk screenings. The dates and results of all tests for syphilis, HCV, and HIV conducted during the study period were provided in a separate database by Quest Diagnostics (Atlanta, GA), a private company contracted by the NC DOC to perform diagnostic lab work.
Electronic prison and lab data were linked by using a unique prison identification number (PIN) assigned to all inmates upon first admission. The PIN was present in all prison records. The 3% of lab records with missing PINs were excluded from analyses. Prisoner records that were linked to a lab record were coded to indicate that the prisoner had been tested; the remaining prisoner records were coded as not tested.
Through a collaborative arrangement, the North Carolina Department of Health and Human Services provided data indicating whether inmates testing positive for HIV in prison had been previously diagnosed within the state and the original diagnosis date. Prisoners with an existing diagnosis, as indicated by state data, were excluded from our study population to focus the analyses on prisoners with unknown serostatus.
Before analysis, each inmate record was assigned a unique study identification number, and all other identifying information (name, birth date, and PIN) was removed from the data. Only records of inmates who were 18 years or older at the time of prison admission were included for analysis.
Coding of Infectious Diseases and Mental Health Conditions
Inmates were tested for HIV with an ELISA; reactive tests were followed by Western blot. HCV testing was conducted with antibody tests; prisoners with a Rapid Plasma Reagin titer of 1:8 or greater were coded as having “active” syphilis.17
All prisoners were assessed for TB via a Mantoux screening test at admission. Because the Mantoux results were not electronically available, electronic medication prescription data were used instead: prisoners prescribed anti-TB medications within 30 days of admission were coded as having TB.
Electronic records were used to identify prisoners diagnosed with a mental health disorder within 30 days of admission. All diagnoses were based on criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).18 Diagnoses chosen for analysis were limited to selected DSM-IV conditions: Axis I (psychosis, bipolar disorder, major depression, generalized anxiety disorder, dementia) and Axis II (developmental disorders and personality disorders) mental health disorders. Prisoners diagnosed with both Axis I and Axis II mental health disorders were coded for Axis I disorders only.
Statistical Analysis
We calculated the system-wide and prison-specific proportions of inmates tested for HIV during their admission. For the 12% of prisoners with multiple imprisonments during the study period, only their most recent admission was used. For all prisoners, admission was uniformly defined as spanning the first 21 days of imprisonment. All HIV tests performed on or after imprisonment day 22 were defined as postadmission tests. The postadmission incidence rate of HIV testing was estimated by dividing the total number of postadmission tests by the total number of postadmission person-days among those inmates not tested during admission. HIV testing proportions, which were based on testing at any time during imprisonment, were calculated for men and women separately by variable level.
Bivariate associations between testing status and inmate characteristics were estimated with gender-specific log binomial models; multivariate associations were estimated by adding: (1) variables with statistically significant (P<.05) bivariate associations, (2) indicator variables for intake facility, and (3) a dichotomous summary variable for risky behavior coded “yes” if the prisoner had any of the following conventional HIV risk behaviors: sex with multiple partners, sexual activity as or with a sex worker, sharing of needles, receipt of a blood transfusion during 1978 to 1985, men who have sex with other men (MSM; assessed only among men), and sex with MSMs and sex with injection drug users (both assessed only among women).
Information on conventional HIV risk behaviors was collected in only 1 of the 2 female intake prisons, so analysis of these behaviors among women was limited to a single facility. However, because these variables were not associated with HIV testing, they were not used in the covariate-adjusted model. Conventional risk behavior data were also missing for about 18% of men. To assess the effect of the missing data, we conducted a complete case analysis, an analysis restricted to intake facilities with minimal missing data, and an analysis based on multiple imputation of missing data. Imputation was carried out by using Amelia II algorithms (using version 2.5.0 of R) because of its facility with categorical variables.19,20 The multiple imputation model included the variables evaluated in the complete case analyses plus 6 variables of modest clinical interest (e.g., ever drink excessively, ever tired). Five imputation data sets were generated and analyzed by using PROC MIANALYZE in SAS version 9.1 (SAS Institute, Cary, NC). All other analyses were also conducted in SAS.
RESULTS
During the study period, 54664 inmates who were 18 years or older entered the NC DOC;17 of these prisoners were excluded from our analysis because they were admitted to a prison without a processing center. To focus our analysis on testing in prisoners with unknown serostatus, we excluded the 631 prisoners who were tested for HIV in prison despite state health department records indicating a preexisting HIV diagnosis.
Eighty-six percent of the inmates were male (Table 1). A greater proportion of men than women were Black, employed before their incarceration, and recidivists. The median sentence length was 12.2 months (25th, 75th percentiles=3.2, 24.3 months) for men and 3.2 months (25th, 75th percentiles=2.0, 14.2 months) for women.
TABLE 1.
Characteristics of Adult Prisoners Entering the North Carolina State Prison System: January 2004–May 2006
| Women, No. or % | Men, No. or % | |
|---|---|---|
| Total | 6804 | 47 212 |
| Age group, y | ||
| ≥45 | 12.4 | 14.0 |
| 35–44 | 33.8 | 25.9 |
| 25–34 | 36.3 | 34.2 |
| 18–24 | 17.6 | 25.9 |
| Race | ||
| Black | 42.2 | 55.5 |
| Other | 3.5 | 6.3 |
| White | 54.3 | 38.1 |
| Education | ||
| College | 13.5 | 7.3 |
| High school degree or GED | 46.2 | 47.0 |
| Less than high school | 40.3 | 45.6 |
| Employeda | 34.4 | 64.0 |
| Marrieda | 15.6 | 14.6 |
| IQ test result | ||
| ≤80 | 13.5 | 25.2 |
| 81–100 | 54.3 | 55.3 |
| ≥101 | 32.3 | 19.5 |
| Previous time served, mo | ||
| None | 60.5 | 44.0 |
| > 0–6 | 15.0 | 13.9 |
| 7–12 | 10.3 | 10.1 |
| ≥13 | 14.2 | 32.0 |
| Sentence length,b mo | ||
| ≥19 | 16.6 | 30.9 |
| 7–18 | 22.2 | 25.9 |
| 3–6 | 29.9 | 22.8 |
| < 3 | 31.3 | 20.4 |
| Drug-related conviction ever | 40.4 | 37.5 |
| Sex-related conviction ever | 1.3 | 6.2 |
| Cocaine or crack use ever | 63.0 | 32.7 |
| Heroin use ever | 5.8 | 1.9 |
| MSMc | … | 0.7 |
| Multiple sexual partnersc | 26.4 | 21.2 |
| Prostitutionc | 16.1 | 5.9 |
| Share needlesc | 9.0 | 3.0 |
| Blood transfusionc | 2.8 | 0.7 |
| Sex with needle sharerd | 15.6 | … |
| Sex with MSMd | 2.9 | … |
| Mental healthe | ||
| Axis I | 6.5 | 2.3 |
| Axis II | 4.5 | 2.7 |
| Hepatitis C | ||
| Positive | 7.6 | 3.2 |
| Negative | 2.1 | 1.1 |
| No test | 90.3 | 95.7 |
| Syphilis | ||
| Positive | 5.2 | 4.1 |
| Negative | 83.4 | 71.9 |
| No test | 11.4 | 23.9 |
| Tuberculosis | ||
| Positive | 1.0 | 3.8 |
| Negative | 99.0 | 96.2 |
Note. MSM = men who have sex with men.
Data missing for ≤20 observations per gender.
Data missing for 471 (6.9%) women and 2376 (5.0%) men.
Data not collected from 3976 (58%) women and 8333 (18%) men.
Data not collected from 3976 (58%) women and all men.
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety disorder, and dementia. Axis II: personality disorder, developmental disability.
Intake prison populations differed by median age and percentage non-White. In the 2 female facilities, the median ages were 33 and 35 years and the percentages non-White were 44.9% and 47.2%. In the male facilities, the median ages in the 2 prisons for young adults were 18 and 21 years and ranged between 33 and 36 years for the other 4 intake prisons. The proportion non-White in the male intake prisons ranged from 52.3% to 72.9%.
Thirty-four percent (n=18435) of all entrants received an HIV test during admission, but the percentage varied from 1% to 84% across processing centers: within each female processing center, more than 80% of entrants were tested for HIV; within 4 of the 6 male processing centers, fewer than 15% of the entrants were tested (Figure 1).
FIGURE 1.
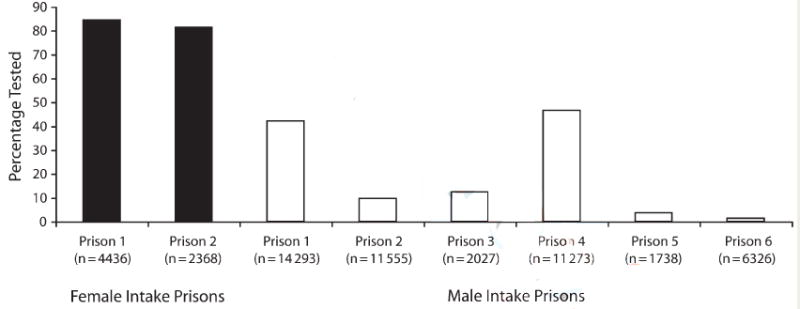
Proportion of newly admitted inmates tested for HIV within the 2 female and 6 male intake facilities of the North Carolina state prison system, January 2004 to May 2006.
Note. Total intake population in parentheses.
The 35581 inmates not tested for HIV during admission were imprisoned for a total of 20197 person-years during the study period. Among these inmates, 2236 (6.3%) were tested for HIV at a rate of 1.1 tests per 10 person-years in prison. Postadmission tests constituted 10.8% (2236 of 20671) of all HIV tests.
Among female prisoners, 85.7% were tested for HIV during admission or postadmission. Statistically significant bivariate associations with HIV testing were observed for race, previous time served, and sentence length. Compared with White women, “other” women (i.e., non-Whites and non-Blacks, including those coded as Indian, Asian or Oriental, other, or unknown) were less likely to be tested for HIV (relative risk [RR]=0.86; 95% confidence interval [CI]=0.80, 0.93). Also, women were less likely to be tested if they had never been imprisoned in the NC DOC previously (RR=0.92; 95% CI=0.90, 0.94). Compared with women with sentences of less than 3 months, women with sentences of 3 to 6 months or 7 to 18 months were more likely to be tested (3 to 6 months: RR=1.09; 95% CI=1.06, 1.11; 7 to 18 months: RR=1.07; 95% CI=1.04, 1.10), but those with sentences of 19 months or greater were less likely to be tested (RR=0.89; 95% CI=0.85, 0.93). In the 1 intake facility that assessed risk behavior (as discussed in the Methods section), women who affirmed a history of conventional HIV risk behaviors were no more likely to be tested than were women who denied such a history.
Among women prisoners, the covariate-adjusted models (Table 2), which accounted for prisoners’ intake facility, indicated that the largest discrepancy in testing was by race: women categorized as “other” were 14% less likely to be tested for HIV than were White women (RR=0.86; 95% CI=0.80, 0.93). There was a modest effect for intake prison (RR=0.94; 95% CI=0.92, 0.96).
TABLE 2.
Covariate-Adjusted Associations Between HIV Test Receipt and Characteristics of Adult Male and Female North Carolina State Prisoners: January 2004–May 2006
| Women, RR (95% CI) | Men, RR (95% CI) | |
|---|---|---|
| Age group, y | ||
| ≥45 | 0.98 (0.95, 1.02) | 0.95 (0.91, 0.99) |
| 35–44 | 0.99 (0.96, 1.01) | 0.98 (0.94, 1.02) |
| 25–34 | 1.00 (0.97, 1.02) | 0.95 (0.91, 0.99) |
| 18–24 (Ref) | 1.00 | 1.00 |
| Race | ||
| Black | 0.98 (0.96, 1.00) | 0.87 (0.85, 0.90) |
| Other | 0.86 (0.80, 0.93) | 0.99 (0.93, 1.05) |
| White (Ref) | 1.00 | 1.00 |
| Education | ||
| College | 0.98 (0.95, 1.01) | 1.04 (0.99, 1.09) |
| High school graduate or GED | 0.99 (0.97, 1.01) | 1.05 (1.03, 1.08) |
| Less than high school (Ref) | 1.00 | 1.00 |
| Employment | ||
| Unemployed | 1.02 (1.00, 1.04) | 0.97 (0.94, 0.99) |
| Employed (Ref) | 1.00 | 1.00 |
| Marital status | ||
| Not married or separated | 1.03 (1.00, 1.05) | 1.02 (0.99, 1.05) |
| Married (Ref) | 1.00 | 1.00 |
| IQ test result | ||
| ≤80 | 1.01 (0.98, 1.05) | 0.93 (0.90, 0.97) |
| 81–100 | 1.03 (1.01, 1.05) | 0.97 (0.95, 1.00) |
| ≥101 (Ref) | 1.00 | 1.00 |
| Previous time served, mo | ||
| None | … | 1.06 (1.03, 1.09) |
| > 0–6 | … | 1.04 (1.01, 1.08) |
| 7–12 | … | 1.02 (0.99, 1.06) |
| ≥13 (Ref) | … | 1.00 |
| Drug-related conviction evera | 1.03 (1.01, 1.05) | 0.98 (0.96, 1.00) |
| Sex-related conviction evera | 0.90 (0.81, 1.02) | 0.97 (0.92, 1.03) |
| Heroin use evera | 1.02 (0.98, 1.05) | 1.12 (1.05, 1.19) |
| Cocaine or crack use evera | 1.06 (1.03, 1.08) | 1.10 (1.08, 1.13) |
| Conventional HIV risk behaviorb | … | 1.10 (1.07, 1.13) |
| Mental healthc | ||
| Axis I | 0.98 (0.94, 1.02) | 0.99 (0.93, 1.06) |
| Axis II | 1.00 (0.97, 1.04) | 1.05 (0.99, 1.12) |
| Neither (Ref) | 1.00 | 1.00 |
| Syphilis | ||
| Positive | … | 1.00 (0.95, 1.05) |
| Negative (Ref) | … | 1.00 |
| Tuberculosis | ||
| Positive | 0.99 (0.90, 1.10) | 1.21 (1.16, 1.26) |
| Negative (Ref) | 1.00 | 1.00 |
Note. MSM = men who have sex with men; RR = relative risk. The model included a variable for intake facilities and covariates with reported estimates.
Referent = never.
Included MSM (men only), multiple sexual partners, prostitution, needle sharing, sex with MSM (women only), sex with injection drug user (women only), blood transfusion 1978–1985.
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety disorder, and dementia. Axis II: personality disorder, developmental disability.
Among male prisoners, 31.7% were tested for HIV during admission or postadmission. All 22 of the covariates, except MSM, needle sharing, and syphilis, were associated with test receipt (Table 3). Notably, men categorized as Black and “other” were, respectively, nearly 30% and 40% less likely to be tested for HIV than were Whites.
TABLE 3.
Associations Between HIV Test Receipt and Characteristics of Adult Male North Carolina State Prisoners: January 2004–May 2006
| No. | HIV Tested, % (No.) | RR (95% CI) | |
|---|---|---|---|
| Age group, y | |||
| ≥45 | 6 604 | 36.6 (2 415) | 1.94 (1.84, 2.03) |
| 35–44 | 12 243 | 38.3 (4 690) | 2.03 (1.94, 2.12) |
| 25–34 | 16 136 | 34.4 (5 557) | 1.82 (1.75, 1.90) |
| 18–24 (Ref) | 12 229 | 18.9 (2 309) | 1.00 |
| Race | |||
| Black | 26 221 | 27.7 (7 272) | 0.71 (0.70, 0.73) |
| Other | 2 992 | 23.6 (707) | 0.61 (0.57, 0.65) |
| White (Ref) | 17 999 | 38.9 (6 992) | 1.00 |
| Education | |||
| College | 3 464 | 35.7 (1 237) | 1.24 (1.18, 1.30) |
| High school graduate or GED | 22 209 | 33.8 (7 524) | 1.18 (1.14, 1.21) |
| Less than high school (Ref) | 21 539 | 28.8 (6 210) | 1.00 |
| Employment | |||
| Unemployed | 17 006 | 26.9 (4 581) | 0.78 (0.76, 0.81) |
| Employed (Ref) | 30 187 | 34.4 (10 385) | 1.00 |
| Marital status | |||
| Not married or separated | 40 295 | 31.4 (12 644) | 0.93 (0.90, 0.97) |
| Married (Ref) | 6 897 | 33.7 (2 325) | 1.00 |
| IQ test result | |||
| ≤80 | 11 893 | 26.4 (3 141) | 0.69 (0.66, 0.71) |
| 81–100 | 26 098 | 31.7 (8 280) | 0.82 (0.80, 0.85) |
| ≥101 (Ref) | 9 221 | 38.5 (3 550) | 1.00 |
| Previous time served, mo | |||
| None | 20 793 | 27.0 (5 604) | 0.74 (0.72, 0.77) |
| > 0–6 | 6 540 | 34.7 (2 269) | 0.96 (0.92, 1.00) |
| 7–12 | 4 777 | 34.2 (1 634) | 0.95 (0.90, 0.99) |
| ≥13 (Ref) | 15 102 | 36.2 (5 464) | 1.00 |
| Sentence length,a mo | |||
| ≥19 | 13 860 | 30.0 (4 161) | 0.79 (0.76, 0.82) |
| 7–18 | 11 610 | 31.1 (3 615) | 0.82 (0.79, 0.85) |
| 3–6 | 10 214 | 28.8 (2 938) | 0.75 (0.72, 0.78) |
| < 3 (Ref) | 9 152 | 38.2 (3 496) | 1.00 |
| Drug-related conviction ever | |||
| Yes | 17 698 | 30.0 (5 314) | 0.92 (0.89, 0.94) |
| No (Ref) | 29 514 | 32.7 (9 657) | 1.00 |
| Sex-related conviction ever | |||
| Yes | 2 902 | 28.2 (819) | 0.88 (0.83, 0.94) |
| No (Ref) | 44 310 | 31.9 (14 152) | 1.00 |
| Cocaine or crack use ever | |||
| Yes | 15 425 | 36.7 (5 667) | 1.26 (1.22, 1.29) |
| No (Ref) | 31 787 | 29.3 (9 304) | 1.00 |
| Heroin use ever | |||
| Yes | 872 | 39.7 (346) | 1.26 (1.16, 1.37) |
| No (Ref) | 46 340 | 31.6 (14 625) | 1.00 |
| MSM | |||
| Yes | 268 | 38.8 (104) | 1.10 (0.95, 1.28) |
| No (Ref) | 38 611 | 35.3 (13 622) | 1.00 |
| Multiple sexual partnersb | |||
| Yes | 8 224 | 29.3 (2 410) | 0.79 (0.77, 0.82) |
| No (Ref) | 30 655 | 36.9 (11 316) | 1.00 |
| Prostitutionb | |||
| Yes | 2 276 | 37.9 (863) | 1.08 (1.02, 1.14) |
| No (Ref) | 36 603 | 35.1 (12 863) | 1.00 |
| Shared needlesb | |||
| Yes | 1 163 | 34.9 (406) | 0.99 (0.91, 1.07) |
| No (Ref) | 37 716 | 35.3 (13 320) | 1.00 |
| Blood transfusionb | |||
| Yes | 277 | 45.1 (125) | 1.28 (1.12, 1.46) |
| No (Ref) | 38 602 | 35.2 (13 601) | 1.00 |
| Mental healthc | |||
| Axis I | 1 107 | 40.1 (444) | 1.28 (1.19, 1.37) |
| Axis II | 1 263 | 34.3 (433) | 1.09 (1.01, 1.18) |
| Neither (Ref) | 44 842 | 31.4 (14 094) | 1.00 |
| HCV | |||
| Positive | 1485 | 55.4 (822) | 0.89 (0.82, 0.97) |
| Negative (Ref) | 531 | 62.0 (329) | 1.00 |
| No test | 45 196 | 30.6 (13 820) | |
| Syphilis | |||
| Positive | 1 956 | 39.8 (778) | 1.01 (0.95, 1.07) |
| Negative (Ref) | 33 962 | 39.4 (13 380) | 1.00 |
| No test | 11 294 | 7.2 (813) | |
| Tuberculosis | |||
| Positive | 1797 | 35.5 (637) | 1.12 (1.05, 1.20) |
| Negative (Ref) | 45 415 | 31.63 (1 434) | 1.00 |
Note. MSM = men who have sex with men; RR = relative risk.
Prisoners with missing data who were tested for HIV = 32.0% (761 of 2376).
Prisoners with missing data who were tested for HIV = 14.9% (1245 of 8333).
Axis I: psychosis, bipolar disorder, major depression, generalized anxiety disorder, and dementia. Axis II: personality disorder, developmental disability.
In the covariate-adjusted analysis, male prisoners with a history of heroin use, cocaine or crack use, HIV-specific behaviors, and a medication history indicative of TB were at least 10% as likely to be tested for HIV as were those without these attributes (Table 2). Black men were 13% less likely to be tested for HIV than were White men (RR=0.87; 95% CI=0.85, 0.90). After adjustment for covariates, intake prison effects were still substantial. Compared with the referent group, males at intake prison 1, the relative risks of testing among males at intake prisons 2 through 6 were: prison 2, RR=0.33 (95% CI=0.31, 0.35); prison 3, RR=0.39 (95% CI=0.35, 0.44); prison 4, RR=0.90 (95% CI=0.87, 0.92); prison 5, RR=0.16 (95% CI=0.13, 0.19); and prison 6, RR=0.14 (95% CI=0.12, 0.15).
Except for attenuation of the RRs for “other” race, no previous time served, and positive syphilis results, results from the analysis restricted to intake facilities with minimal missing data (<2%) and the analysis based on multiple imputation were nearly identical to the results of the complete case analysis (see appendix table 4, available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
Because national guidelines promote widespread access to HIV testing, it is important to assess testing among high-risk populations including prisoners. We found that nearly 40% of prisoners were tested for HIV and that the vast majority of tests were conducted as part of the admission process. Although testing varied modestly by prisoner characteristics, it varied widely across intake prison. This observation is important given that previous studies of HIV testing have been conducted in smaller prison systems with only a single intake prison or without regard to multiple intake prisons.9-14
Little research is available that might explain the variation in facility testing rates. One study examining the relation between organizational structure and HIV testing in a national sample of correctional facilities found that organization size was a predictor of testing but other constructs were not.21 In our data, there was no apparent relation between organization size and testing practices.
Brief interviews with key informants in the NC DOC indicated that facility differences may reflect the priorities assigned by the chief medical professional at each prison, available resources, and, consequently, the manner and setting in which testing is offered. Given the nature of our study—a retrospective analysis of laboratory data—we had little information regarding testing practices during the study period. However, data collected in Fall 2008 suggest that at that time, the manner and setting of testing differed significantly across intake prisons: testing was either (1) offered privately, (2) offered in a group setting after an HIV presentation, or (3) simply available upon “sick call” request (see appendix table 2, available online). Notably, testing among female prisoners was tightly bound with reproductive health and in 1 prison was offered in an opt-out manner.
Testing practices in the NC DOC have been dynamic over time, making it difficult to draw inferences between practices in 2008 and our findings from the study period, 2004 to 2006. Nevertheless, it is reasonable to conclude from these data that testing rates are higher when testing is easily available and offered privately. Although not well studied, prisoners’ concerns about confidentiality and stigma likely play an important role in their willingness to be tested. Whereas these concerns are pertinent in any setting, they may have particular resonance among prisoners given the closed nature of their environment. More formal evaluation of these constructs as well as structural-level factors affecting facility testing rates will soon be underway in the NC DOC to better unify the provision of testing across intake prisons.
In nearly all state prison systems, including North Carolina’s, HIV testing is available throughout inmates’ incarceration. However, in our study population, the proportion of prisoners tested for HIV after the 21-day admission period was relatively small (6%). Where testing rates are low and sentences lengthy, providing periodic opportunities for prisoners to be tested for HIV could increase acceptance of testing, and repeat testing of prisoners testing negative at admission could be useful in monitoring intraprison transmission.2
Of concern, non-Whites were less likely to be tested for HIV than were Whites. Women with the racial category “other” were 14% less likely to be tested than were White women, and men categorized as “other” or Black were 40% and 30%, respectively, less likely to be tested than were White men.
For men, much of the difference in testing across racial category may be explained by differences in the racial composition and testing rate of the intake prisons. The intake prison with the greatest number of non-Whites (prison 2) tested less than 10% of all inmates. Whether racial composition could have affected facility testing rates is unclear. Nevertheless, after accounting for intake prison and other characteristics associated with testing, Black men and women characterized as “other” were still less likely to be tested for HIV than were Whites. Studies among other prisoner populations have also reported lower testing rates among prisoners who were not White.10,12,22 Given the higher prevalence of HIV among non-Whites than among Whites,7 greater testing of prisoners who are not White is an important step in improving case finding. More effort is needed to understand prisoners’ possible reluctance to be tested as well as the institutional barriers to testing.
Among men, prisoners reporting any conventional HIV risk behavior, heroin use, or crack or cocaine use were 10% more likely to be tested for HIV than were prisoners not disclosing these behaviors, and prisoners with TB disease were 20% more likely to be tested than were prisoners without TB. However, prisoners with active syphilis infection were no more likely to be tested for HIV than were those without syphilis infection, and although only a small proportion (<10%) of prisoners were tested for HCV, we found an inverse relation between HCV seropositivity and HIV testing. Given that syphilis, HCV, and HIV share routes of transmission, greater testing among syphilis- and HCV-infected populations may yield a relatively high proportion of HIV-infected individuals.
The CDC has recommended that HIV testing be available widely and offered routinely (i.e., via opt-out testing) in correctional health care facilities.15,16 Routine HIV testing in prisons could potentially have a profound impact on case identification. Routine HIV testing in the Rhode Island DOC detected about one third of all HIV infections in the state during the 1990s.23 In comparison, only 7% of new HIV cases in North Carolina are detected in correctional facilities (W. Jones, North Carolina Division of Public Health, personal communication, 2007). Increasing the availability and use of HIV testing in the NC DOC may be an efficient way to improve case finding in the state.
In light of our study findings and recommendations from the CDC, state legislators, community members and the NC state department of health, the NC DOC adopted a policy of routine opt-out testing beginning in November 2008. As in other prison systems, efforts to increase testing rates in the NC DOC should be approached with care: in the prison setting, which is designed to limit personal liberties, there is a fine line between encouragement and coercion. In a qualitative study of attitudes toward HIV testing among prisoners in 4 states, some inmates reported that HIV testing in their prison was mandatory despite their residing in prisons with a policy of voluntary testing.24 With such misperceptions (or inconsistent application of policy), state prison systems should ensure that consent-based HIV testing is truly voluntary. In the North Carolina prison system, we will be evaluating the testing process under this new policy of opt-out testing to ensure that testing is widely available to inmates but is not coercive.
Our study had some limitations. First, our study relied on routinely collected administrative data and did not include the full gamut of factors affecting testing (e.g., inmates’ perceptions of confidentiality and HIV stigma); moreover, the phrasing of some risk assessment items was vague. Second, validation of administrative data was not possible because of the retrospective design of this study. Third, approximately 23% of the data specific to HIV risk behaviors were missing. These data limited the scope of our analyses among women, but with most women tested for HIV, these variables would likely have demonstrated little association with testing. For the men, we assessed the effect of the missing data by comparing the results from a complete case analysis, a restricted population with minimal missing data, and an analysis using (multiply) imputed data; the effect estimates across analyses differed little. Fourth, data from the state department of health allowed us to exclude from the analyses prisoners testing positive for HIV who previously had been diagnosed in North Carolina; however, we were unable to identify and exclude prisoners who declined testing because of a previous diagnosis. Finally, informant interviews suggest that the systemwide testing policy was likely implemented differently across facilities. Unfortunately, information about providers’ practices and their interpretation of the testing policy was not available through this retrospective analysis of laboratory data.
Prisons have been recognized as an important point of contact with populations who are at increased risk of disease and who have little regular access to health care. To better utilize the opportunity to improve public health through the prison system, evaluations of prison health care services are greatly needed. In our study, we found that there were wide variations in testing rates across intake prisons, racial disparities in testing, and few tests provided after the admission process. The NC prison system has responded by adopting the CDC’s recommendation for opt-out testing and by working in partnership with university-based researchers to further evaluate the testing process. To fully realize the public health gains made by increased testing in the prison system, it is also essential that agencies outside the NC DOC, such as the state health department, help to provide adequate resources to prisoners after their release. Other state prison systems with consent-based testing could benefit from similar partnerships as the role of prisons expands in HIV case detection.
Supplementary Material
Acknowledgments
This work was funded by the NIH National Research Service Award (fellowship F30 MH077546-01).
The authors thank Peter Leone, MD, and Bill Miller, MD, for their thoughtful suggestions on an earlier version of this article. We also thank the administrators and staff of the NC Department of Correction for their assistance with this project. We dedicate this article to the late Andrew H. Kaplan, MD.
Footnotes
Contributors D. L. Rosen originated the study and led the analyses and writing. V. J. Schoenbach and P. W. Stewart contributed to the writing and analyses. D. A. Wohl, C. E. Golin, and B. L. White contributed to the writing.
Human Participant Protection This project was approved by the biomedical institutional review board within the University of North Carolina, Chapel Hill, and the institutional review board of the North Carolina Department of Correction.
References
- 1.The Status of Soon-to-be-Released Inmates A Report to Congress. Vol. 1. Chicago, IL: National Commission on Correctional Health Care; 2002. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV transmission among male inmates in a state prison system–Georgia, 1992–2005. MMWR Morb Mortal Wkly Rep. 2006;55(15):421–426. [PubMed] [Google Scholar]
- 3.Macalino GE, Vlahov D, Sanford-Colby S, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons. Am J Public Health. 2004;94(7):1218–1223. doi: 10.2105/ajph.94.7.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000;90(12):1939–1941. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maruschak LM. HIV in Prisons, 2001. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2004. [Google Scholar]
- 6.National Center for Health Statistics. Health, United States 2004, with Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 7.Maruschak LM. HIV in Prisons, 2004. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2006. [Google Scholar]
- 8.Rosen DL, Schoenbach VJ, Kaplan AH. HIV testing in state prisons: balancing human rights and public health. Infectious Diseases in Corrections Report. 2006;9(4):1–5. [Google Scholar]
- 9.Cotten-Oldenburg NU, Jordan BK, Martin SL, Sadowski LS. Voluntary HIV testing in prison: do women inmates at high risk for HIV accept HIV testing? AIDS Educ Prev. 1999;11(1):28–37. [PubMed] [Google Scholar]
- 10.Behrendt C, Kendig N, Dambita C, Horman J, Lawlor J, Vlahov D. Voluntary testing for human immunodeficiency virus (HIV) in a prison population with a high prevalence of HIV. Am J Epidemiol. 1994;139(9):918–926. doi: 10.1093/oxfordjournals.aje.a117098. [DOI] [PubMed] [Google Scholar]
- 11.Hoxie NJ, Vergeront JM, Frisby HR, Pfister JR, Golubjatnikov R, Davis JP. HIV seroprevalence and the acceptance of voluntary HIV testing among newly incarcerated male prison inmates in Wisconsin. Am J Public Health. 1990;80(9):1129–1131. doi: 10.2105/ajph.80.9.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoxie NJ, Chen MH, Prieve A, Haase B, Pfister J, Vergeront JM. HIV seroprevalence among male prison inmates in the Wisconsin Correctional System. WMJ. 1998;97(5):28–31. [PubMed] [Google Scholar]
- 13.Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health. 2005;82(2):312–326. doi: 10.1093/jurban/jti055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kassira EN, Bauserman RL, Tomoyasu N, Caldeira E, Swetz A, Solomon L. HIV and AIDS surveillance among inmates in Maryland prisons. J Urban Health. 2001;78(2):256–263. doi: 10.1093/jurban/78.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Advancing HIV Prevention: Interim Technical Guidance for Selected Interventions. Atlanta, GA: CDC; 2003. [May 12, 2009]. Routine HIV testing of inmates in correctional facilities; pp. 25–30. Available at: http://www.cdc.gov/hiv/topics/prev_prog/AHP/resources/guidelines/pdf/AHPIntGuidfinal.pdf. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings MMWR. Atlanta: CDC; 2006. [PubMed] [Google Scholar]
- 17.World Health Organization. Detecting STI/RTI Sexually transmitted and other reproductive tract infections–A guide to essential practice. Geneva: World Health Organization; 2005. pp. 33–43. [Google Scholar]
- 18.Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 19.King G. Analyzing incomplete political science data: an alternative algorithm for multiple imputation. Am Polit Sci Rev. 2000;95:49–69. [Google Scholar]
- 20.Honaker J, Joseph A, King G, Scheve K, Singh N. Amelia: A Program for Missing Data. Cambridge, MA: Department of Government, Harvard University; 2000. [Google Scholar]
- 21.Oser CB, Tindall MS, Leukefeld CG. HIV testing in correctional agencies and community treatment programs: the impact of internal organizational structure. J Subst Abuse Treat. 2007;32(3):301–310. doi: 10.1016/j.jsat.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altice FL, Mostashari F, Selwyn PA, et al. Predictors of HIV infection among newly sentenced male prisoners. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(5):444–453. doi: 10.1097/00042560-199808150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Desai AA, Latta ET, Spaulding A, Rich JD, Flanigan TP. The importance of routine HIV testing in the incarcerated population: the Rhode Island experience. AIDS Educ Prev. 2002;14(5 suppl B):45–52. doi: 10.1521/aeap.14.7.45.23867. [DOI] [PubMed] [Google Scholar]
- 24.Kacanek D, Eldridge GD, Nealey-Moore J, et al. Project Start Study Group. Young incarcerated men’s perceptions of and experiences with HIV testing. Am J Public Health. 2007;97(7):1209–1215. doi: 10.2105/AJPH.2006.085886. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


