Abstract
Background:
Previously healthy firefighters with World Trade Center (WTC) dust exposure developed airway disease. Risk factors for irritant-associated asthma/COPD overlap are poorly defined.
Methods:
The study included 2,137 WTC-exposed firefighters who received a clinically-indicated bronchodilator pulmonary function test (BD-PFT) between 9/11/2001–9/10/2017. A post-BD FEV1 increase of >12% and 200 ml from baseline defined asthma, and post-BD FEV1/FVC ratio<0.7 identified COPD cases. Participants who met both criteria had asthma/COPD overlap. Eosinophil levels were measured on screening blood tests performed shortly after 9/11/2001 and prior to BD-PFT; a subgroup of participants also had serum IgE and 21 cytokines measured (N=215). Marginal Cox regression models for multiple events assessed the associations of eosinophil levels or serum biomarkers with subsequent diagnosis, with age, race, smoking, WTC-exposure, first post-9/11 FEV1/FVC ratio, and BMI included as covariates.
Results:
BD-PFT diagnosed asthma/COPD overlap in 99 individuals (4.6%), isolated-asthma in 202 (9.5%), and isolated-COPD in 215 (10.1%). Eosinophil concentration≥300 cells/μl was associated with increased risk of asthma/COPD overlap (HR: 1.85, 95% CI: 1.16–2.95), but not with isolated-asthma or isolated-COPD. Serum IL-4 also predicted asthma/COPD overlap (HR: 1.51 per doubling of cytokine concentration, 95% CI: 1.17–1.95). Greater IL-21 concentration was associated with both isolated-asthma and isolated-COPD (HR: 1.73, 95% CI: 1.27–2.35 and HR: 2.06, 95% CI: 1.31–3.23, respectively).
Conclusions:
In WTC-exposed firefighters, elevated blood eosinophils and IL-4 levels are associated with subsequent asthma/COPD overlap. Disease-specific Th-2 biomarkers present years before diagnosis suggest patient-intrinsic predisposition to irritant-associated asthma/COPD overlap.
Introduction
The collapse of the World Trade Center (WTC) on September 11, 2001 (9/11) exposed the Fire Department of the City of New York (FDNY) rescue and recovery workers to caustic dust and products of combustion.1 Subsequently, WTC-exposed rescue and recovery workers had high rates of airway injury, including excessive loss of lung function,2 obstructive ventilatory defect3 and airway hyper-reactivity.4 Firefighters with elevated post-exposure blood eosinophil concentrations were at increased risk of developing chronic obstructive pulmonary disease (COPD).5
Asthma/COPD overlap is a recently defined endotype of COPD,6–8 with patients experiencing a poorer quality of life and higher mortality compared with patients who have either isolated-COPD or isolated-asthma.9–11 Risk factors for asthma/COPD overlap are poorly defined, but among those with smoking-related COPD, elevated eosinophils in sputum and blood are biomarkers for this condition.12,13 There is a need for longitudinal studies to define risk factors for asthma/COPD overlap.14
The aim of this study was to determine early predictors of asthma/COPD overlap among WTC-exposed firefighters with at least one post-9/11 clinically-indicated pulmonary function test (PFT) with bronchodilator (BD) measurement (N=2,137). The main predictors of interest were blood biomarkers collected during participants’ post9/11 FDNY medical monitoring examination. We also examined these measurements in association with isolated isolated-asthma and with isolated-COPD as a way to understand the unique predictors of asthma/COPD overlap.
Methods
Study Population
The source population consisted of 9,598 male firefighters who were actively employed by the FDNY on 9/11, first arrived at the WTC between 9/11–9/24/2001, and had ≥3 post-9/11 forced expiratory volume at one second (FEV1) measurements from routine medical monitoring PFTs taken at FDNY.5 A subset of this population received at least one clinically-indicated BD-PFT performed according to American Thoracic Society (ATS) standards15 at a hospital-based pulmonary function laboratory between 9/11/2001 and 9/10/2017. We excluded 57 participants whose BD-PFT occurred before their first post-9/11 medical monitoring examination. The final study population included 2,137 firefighters (Figure 1). Participants provided written informed consent. The Montefiore Medical Center (FWA #00002558)/Albert Einstein College of Medicine (FWA #00023382) Institutional Review Board approved this study.
Figure 1. Firefighters who participated in the Asthma/COPD overlap study.
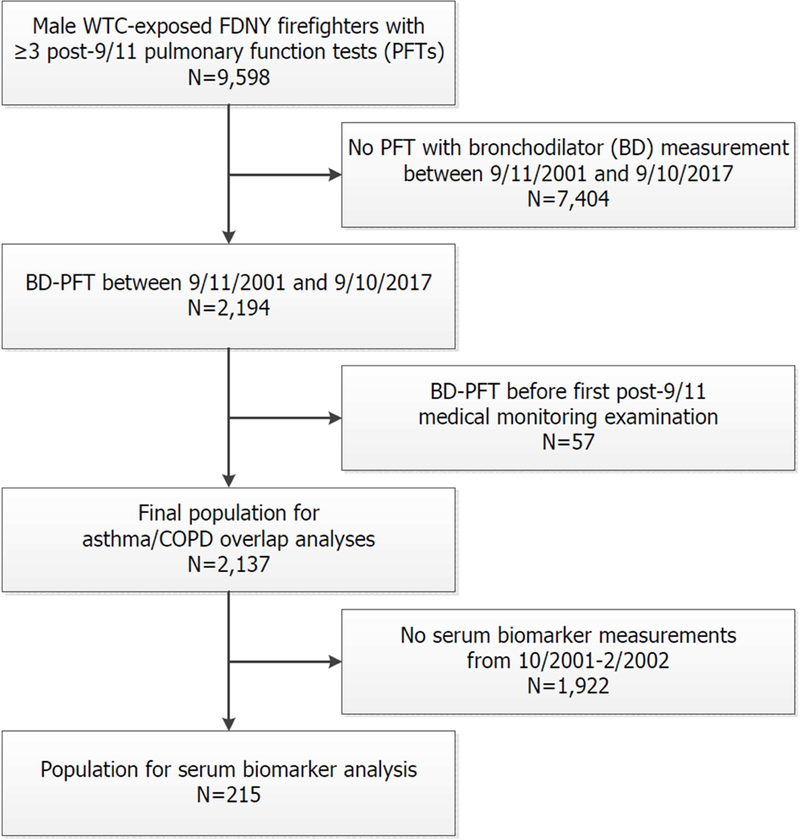
Shown is the source population of male firefighters who were employed by the Fire Department of the City of New York (FDNY) on 9/11/2001, present at the World Trade Center (WTC) site between 9/11/2001 and 9/24/2001, and had at least three routine monitoring pulmonary function tests (PFTs) taken between 9/11/2001 and 9/10/2017 for forced expiratory volume at one second (FEV1) slope measurement. The final study population included those who had received a post-9/11/2001 clinically-indicated PFT with bronchodilator measurement. The serum biomarker population was a subgroup who had biomarkers measured on serum drawn between 10/2001 and 2/2002.
Baseline Characteristics
Demographic data were retrieved from the FDNY employee database. Participants’ height, weight, self-reported smoking status (current, former or never-smoker) and time of initial arrival at the WTC site were assessed during routine medical monitoring examinations at FDNY; both active duty firefighters and WTC-exposed retirees are scheduled to have a monitoring exam once every 12–18 months. We classified individuals as having high (morning of 9/11), moderate (afternoon on 9/11–9/12) or low (9/13–9/24) WTC exposure based on their WTC site arrival time.4 Current and former smokers were grouped together as ever-smokers in our analyses. Those who consistently self-reported no cigarette smoking were classified as never-smokers.
Blood and Serum Biomarkers
Eosinophil concentration was measured from blood drawn shortly after 9/11, during the first post-9/11 monitoring examination. The median first post-9/11 blood draw date was 1/10/2002 (interquartile range: 11/26/2001–12/27/2002). We also had pre-9/11 blood data (eosinophil concentration) for the 1,008 participants who had blood drawn at a pre-9/11 monitoring exam. Serum biomarkers from the first post-9/11 blood draw, including IgE and cytokines, were available for a subgroup of the study cohort (N=215). Serum was stored at −80°C; IL-4 and IFN- γ were assayed with EMD Milipore HSTCMAG28SPMX21 and IgE with HGAMMAG-303E.
Pulmonary Function
Participants’ most recent BD-PFT from the 9/11/2001–9/10/2017 period provided the pre- and post-bronchodilator FEV1 and forced vital capacity (FVC) measurements used to define our main outcome. A bronchodilator response of a >12% and 200 ml increase from baseline FEV1 diagnosed asthma.16 COPD was defined according to the GOLD criteria, which requires FEV1/FVC ratio<0.7 on a post-bronchodilator PFT.7 We classified individuals who had a bronchodilator response and FEV1/FVC≥0.7 as having isolated-asthma, and those who had FEV1/FVC<0.7 and no bronchodilator response as having isolated-COPD. Individuals who met the criteria for both asthma and COPD had asthma/COPD overlap. Total lung capacity (TLC) and residual volume (RV) measurements were also available from the BD-PFT data; these were measured prior to bronchodilator administration. We used spirometric measurements from 22,737 routine monitoring PFTs (always done without BD) taken between 9/11/2001 and 9/10/2017 to assess post-9/11 FEV1 trajectories. FEV1 values from post-9/11 monitoring PFTs that occurred prior to the BD-PFT were used to determine whether patients with asthma and/or COPD had accelerated (>64 ml/year) or expected (≤64 ml/year) FEV1 decline post-9/11, but prior to our outcome determination; for individuals who had neither diagnosis, all post-9/11 FEV1 values were included in the FEV1 decline rate calculation. Pre-9/11 FEV1 and FVC measurements were available from 1,265 spirometries performed at FDNY monitoring in the year prior to 9/11 (9/11/2000–9/10/2001).
Statistical Analyses
Demographic and other characteristics of the study population and serum biomarker subgroup were assessed as proportions and means (±SD), with independent sample t-tests or chi square tests used to evaluate differences, as appropriate. Longitudinal FEV1 % predicted, FEV1/FVC ratio and post-9/11 rate of FEV1 change were estimated in four subsets of the population defined by outcome (isolated-asthma, isolated-COPD, asthma/COPD overlap, or neither condition) using linear mixed effects models with random intercepts. Participants’ age on 9/11, height and race were included as fixed effects in the models with absolute FEV1 or FEV1/FVC ratio as the outcome. Mean FEV1 % predicted and FEV1/FVC ratio values in the four groups were estimated for each one-year period between 9/11/2000 and 9/10/2017, and mean rates of FEV1 change were determined using the post-9/11 spirometry data.
We performed log-rank Mantel-Cox tests to examine the univariable associations of post-9/11 FEV1 trajectory (accelerated vs. expected FEV1 decline), eosinophil concentration and smoking status with incident asthma/COPD overlap, followed by multivariable marginal Cox regression models for multiple events to evaluate shared and distinct risk factors for isolated-asthma, isolated-COPD, and asthma/COPD overlap. Censoring occurred at the time of the BD-PFT. Blood eosinophil concentration was assessed first as a binary (≥300 cells/μl vs. <300 cells/μl) and then as a continuous variable. We carried out two sensitivity analyses: one that excluded individuals with FEV1/FVC ratio<0.7 on a pre-9/11 monitoring PFT (N=69), and another that examined the relationship between pre-9/11 eosinophil concentration and the outcomes of interest (N=1,008). Absolute change in eosinophil concentration from pre- to post-9/11 was also investigated. A multivariable-adjusted Cox regression analysis for multiple events data was also performed in the serum biomarker subpopulation (N=215) in order to determine whether log2 transformed serum IgE and 21 cytokines were associated with isolated-asthma, isolated-COPD, or asthma/COPD overlap. After Bonferroni correction, the significance cut-off for the serum biomarker analyses was set at a two-sided p-value of 0.0024. For all other analyses, reported p-values are two-sided and considered significant at the <0.05 level. Multivariable models included age, race, smoking status, WTC exposure, first post-9/11 FEV1/FVC ratio and BMI as covariates. Covariates were selected based on theory. Data analyses were performed using SAS version 9.4. We created figures using Prism 7.
Results
Baseline Characteristics
Demographic and other characteristics of the 2,137 firefighters with clinically-indicated post-9/11 BD-PFT in the final study population (Figure 1) and those without BD-PFT are presented in Table 1. Compared with WTC-exposed firefighters who did not have a BD-PFT, the study population was slightly different in that it was older, had a higher BMI and post-9/11 blood eosinophil concentration, and a greater proportion of ever-smokers. These differences were more pronounced in those who would develop post-BD FEV1/FVC ratio<0.70. The serum biomarker subgroup was similar to the study population, with the exception of having a smaller proportion of ever-smokers.
Table 1:
Population characteristics and longitudinal lung function
| Bronchodilator PFT Study Population N=2,137 |
|||||
|---|---|---|---|---|---|
| Variable | WTCd-exposed No Bronchodilator PFTa N=7,404 |
Post- Bronchodilator FEV1/FVC ≥ 0.7 N=1,823 |
Post- Bronchodilator FEV1/FVC< 0.7 N=314 |
Subpopulation with serum biomarkers N=215 |
Pr |
| Age on 9/11b | 39.9 ± 7.6 | 40.5 ± 6.7 | 44.0 ± 6.8 | 41.0 ± 6.8 | <0.001 |
| BMIbc | 28.7 ± 3.4 | 29.2 ± 3.5 | 28.5 ± 3.3 | 28.7 ± 3.3 | <0.001 |
| Smoking status, N (%)c | |||||
| Never | 5,031 (67.9) | 1,229 (67.4) | 142 (45.2) | 185 (86.0) | |
| Former | 2,143 (28.9) | 542 (29.7) | 148 (47.1) | 22 (10.2) | <0.001 |
| Current | 230 (3.1) | 52 (2.9) | 24 (7.6) | 8 (3.7) | |
| Race, N (%) | |||||
| White | 6,971 (94.2) | 1,719 (94.3) | 299 (95.2) | 208 (96.7) | |
| Black | 174 (2.3) | 36 (2.0) | 10 (3.2) | 4 (1.9) | <0.001 |
| Hispanic | 234 (3.2) | 66 (3.6) | 5 (1.6) | 3 (1.4) | |
| Other | 25 (0.3) | 2 (0.1) | 0 | 0 | |
| WTCd Arrival Time, N (%) | |||||
| Morning of 9/11 | 1,129 (15.3) | 366 (20.1) | 52 (16.6) | 37 (17.2) | |
| Afternoon on 9/11–9/12 | 5,322 (71.9) | 1,295 (71.0) | 223 (71.0) | 168 (78.1) | <0.001 |
| 9/13–9/24 | 953 (12.9) | 162 (8.9) | 39 (12.4) | 10 (4.7) | |
| Pre-9/11 Spirometry | |||||
| FEV1e (L)b | 4.43 ± 0.68g | 4.38 ± 0.69j | 3.94 ± 0.74jm | 4.32 ± 0.69p | <0.001 |
| FEV1 % predictedb | 105.9 ± 13.3g | 104.3 ± 13.7j | 95.2 ± 15.4jm | 103.3 ± 14.2p | <0.001 |
| FEV1/FVCf | 0.85 ± 0.05g | 0.85 ± 0.05j | 0.78 ± 0.07jm | 0.84 ± 0.05p | <0.001 |
| Post-9/11 Spirometry | |||||
| FEV1 (L)bc | 4.05 ± 0.65 | 3.96 ± 0.65 | 3.46 ± 0.73 | 3.92 ± 0.70 | <0.001 |
| FEV1 % predictedbc | 97.8 ± 12.9 | 95.4 ± 13.5 | 85.2 ± 15.3 | 94.4 ± 14.4 | <0.001 |
| FEV1/FVC | 0.84 ± 0.05 | 0.84 ± 0.05 | 0.74 ± 0.07 | 0.83 ± 0.06 | <0.001 |
| Post-9/11 FEV1 slope (ml/yr)b |
−35.1 ± 30.8 | −37.8 ± 32.4 | −47.5 ± 36.3 | −41.1 ± 37.0 | <0.001 |
| Blood eosinophil concentration | |||||
| Pre-9/11 eos/μl | 154 ± 109h | 162 ± 117k | 186 ± 144n | 153 ± 104q | <0.001 |
| Post-9/11 eos/μlbc | 184 ± 1.26i | 194 ± 1.36l | 231 ± 1.75o | 198 ± 132 | <0.001 |
Pulmonary function test
Mean ± standard deviation
Value on first post-9/11 monitoring exam
World Trade Center
Forced expiratory volume in one second
Forced vital capacity
N=6,836
N=3,295
N=7,388
N=1,686
N=857
N=1,780
N=285
N=151
N=304
N=209
N=109
ANOVA or chi square test comparing values in first three columns
Lung Function on Monitoring and BD-PFTs
Clinically-indicated BD-PFT diagnosed isolated-asthma in 202 individuals (9.4%), isolated-COPD in 215 (10.1%), and asthma/COPD overlap in 99 (4.6%) (Figure 2). At the time of BD-PFT, the asthma/COPD overlap subgroup had a lower pre-BD FEV1 % predicted, lower pre-BD FEV1/FVC ratio and higher RV/TLC ratio than any other diagnostic category (Table 2). Bronchodilator response was similar in asthma/COPD overlap and isolated-asthma patients (22.6±13.3% vs. 19.9±12.8% increase in FEV1, respectively, p=0.09).
Figure 2. Asthma/COPD overlap in WTC-exposed firefighters who had a bronchodilator PFT.
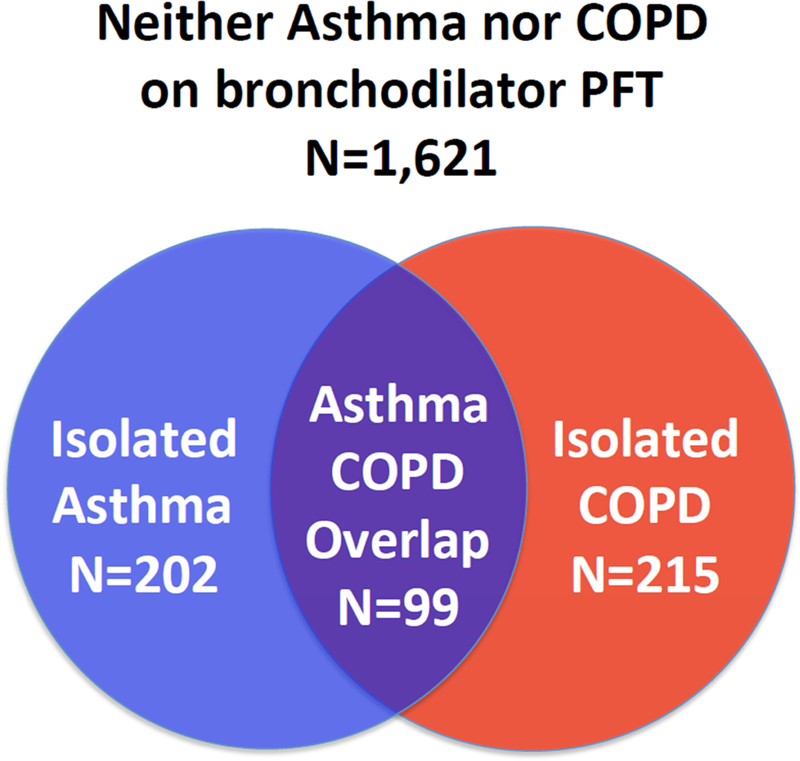
The Venn diagram demonstrates abnormalities on bronchodilator PFTs obtained via the WTC treatment program. Isolated-asthma was diagnosed in 202 individuals who had FEV1 bronchodilator response of greater than 12% and 200 ml. Isolated-COPD was diagnosed in 215 individuals who had a post-bronchodilator FEV1 /FVC ratio <0.70. Asthma COPD/overlap was diagnosed in 99 who had both a FEV1 bronchodilator response >12% and 200 ml, and a FEV1/FVC ratio <0.70. The remainder of the study population (1,621) did not have a bronchodilator response or airflow limitation.
Table 2:
Bronchodilator pulmonary function test results
| Variable | Asthma COPD overlap, mean ± SD |
Isolated-asthma, mean ± SD |
Isolated-COPD, mean ± SD |
Neither diagnosis, mean ± SD |
|---|---|---|---|---|
| Pre-BDa FEV1b % predicted | 67.3±14.8 | 80.9±13.5f | 82.3±15.2f | 96.9±13.2f |
| Post-BD FEV1 % predicted | 81.3±14.5 | 96.2±13.7f | 85.9±15.0f | 100.5±13.5f |
| Pre-BD FVCc % predicted | 93.3±15.8 | 87.1±13.9f | 101.2±15.1f | 98.3±12.9f |
| Post-BD FVC % predicted | 101.8±14.0 | 96.0±13.3f | 103.4±15.1 | 98.5±12.9f |
| Pre-BD FEV1/FVC | 0.56±0.08 | 0.73±0.07f | 0.62±0.07f | 0.77±0.05f |
| Post-BD FEV1/FVC | 0.62±0.07 | 0.78±0.05f | 0.64±0.06f | 0.80±0.05f |
| Pre-BD RVd/TLCe | 0.40±0.10 | 0.33±0.09f | 0.33±0.08f | 0.28±0.07f |
Bronchodilator
Forced expiratory volume in one second
Forced vital capacity
Residual volume
Total lung capacity
p<0.05 vs. Asthma/COPD overlap subgroup
Both the pre-9/11 and first post-9/11 FEV1 % predicted in each subgroup were on average ≥80% on monitoring PFTs, but were lowest in those who went on to develop asthma/COPD overlap (Figure 3A). FEV1/FVC ratio on the first post-9/11 monitoring PFT was also lowest in this subgroup (Figure 3B). The annual post-9/11 FEV1 loss in individuals with asthma/COPD overlap was similar to that of the COPD subgroup (47.6 ml/year, 95% CI: 43.5–51.6, and 47.2 ml/year, 95% CI: 44.7–49.6, respectively), and greater than the rate of FEV1 loss in those with isolated-asthma (43.4 ml/year, 95% CI: 40.7–46.2) or neither outcome (36.8 ml/year, 95% CI: 35.9–37.6).
Figure 3. Lung function over time.
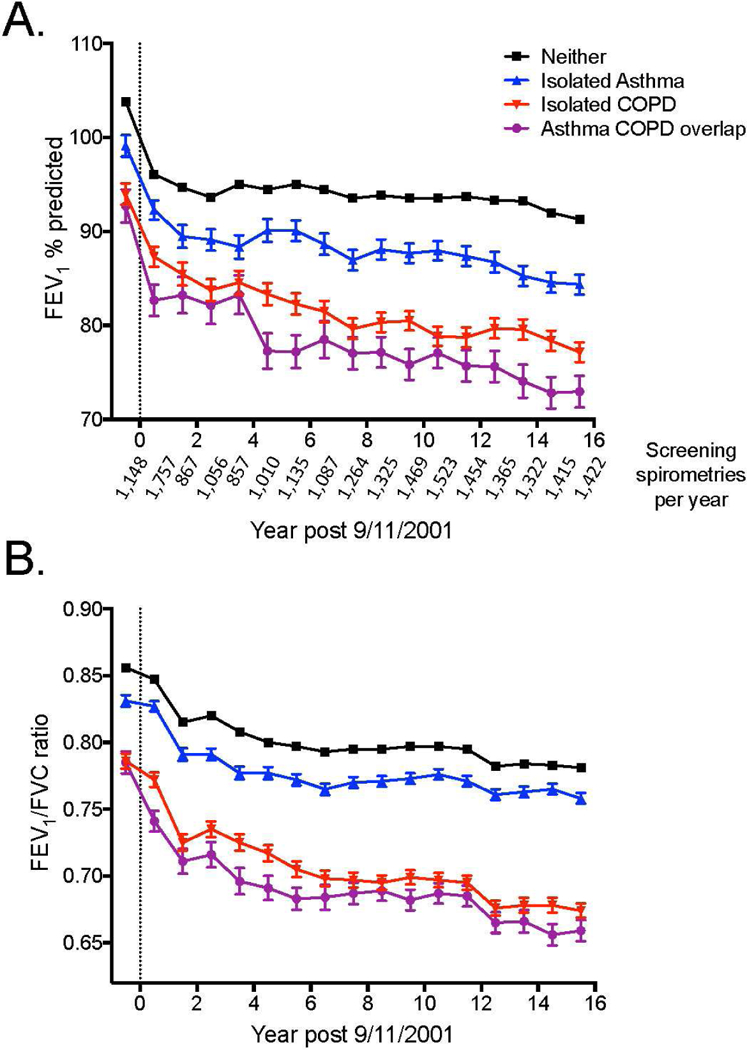
Panel A shows the mean (±SEM; SEM not shown if it is smaller than the size of the symbol) FEV1 % predicted in each year between 9/11/2000 and 9/10/2017 in the asthma/COPD overlap (purple), isolated COPD (red), isolated asthma (blue) and asthma-free and COPD-free (black) groups. The vertical line at 0 represents 9/11/2001. The number of spirometries per year is shown below the x axis. Panel B shows the mean FEV1/FVC ratio in the above groups in each year, adjusted for race, height and age, using the same number of spirometries per year as shown in panel A.
Risk Factors for Asthma/COPD Overlap
Univariable analyses showed that the incidence of asthma/COPD overlap was elevated in participants with post-9/11 eosinophil concentration ≥300 cells/μl (HR: 1.69, 95% CI: 1.00–2.81, p<0.05) (Figure 4A), those with a history of smoking (HR: 1.67, 95% CI: 1.11–2.50, p=0.02) (Figure 4B) and those experiencing post-9/11 accelerated FEV1 decline (HR: 2.05, 95% CI: 1.22–3.43, p=0.006) (Figure 4C). In multivariable marginal Cox regression models for multiple events, asthma/COPD overlap was predicted by eosinophil concentration ≥300 cells/μl (Table 3a). Eosinophil concentration was not significantly associated with isolated-asthma or isolated-COPD. When isolated-asthma and asthma/COPD overlap were compared directly, asthma/COPD overlap was still associated with elevated eosinophils (Table 3b). Results were similar if analyses were restricted to those who had eosinophils measured less than 15 months after 9/11 (data not shown). A unique risk factor for isolated-asthma was high intensity WTC exposure, and for isolated-COPD was ever-smoking. Post-9/11 accelerated FEV1 decline was associated with all three outcomes. The observed associations did not change when eosinophil concentration was assessed as a continuous variable (data not shown).
Figure 4. Cumulative incidence of asthma/COPD overlap in WTC-exposed firefighters who had a bronchodilator PFT.
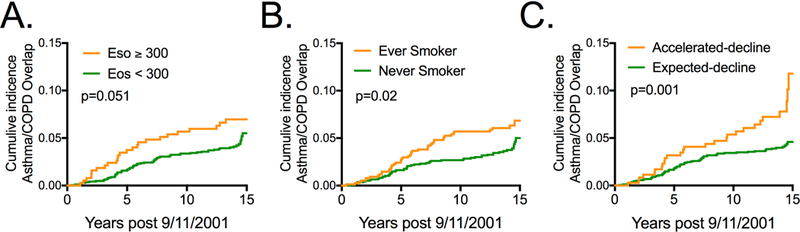
Panel A shows the cumulative incidence of asthma/COPD overlap in participants with blood eosinophil concentration ≥300 cells/μl (orange) and <300 cells/μl on first post-9/11 medical monitoring exam. The level of significance shown in each panel was determined by the log rank test. Panel B shows the cumulative incidence in those who reported ever smoking (orange) and never smoking (green). Panel C shows the cumulative incidence in participants who had an accelerated rate of post-9/11 FEV1 decline >64 ml/year (orange) and those with expected FEV1 decline ≤64 ml/year (green).
Table 3:
| Variables | Asthma/COPD Overlap vs. Neither |
Isolated-Asthma vs. Neither |
Isolated-COPD vs. Neither |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Eosinophils ≥ 300 cells/μlc | 1.85 | 1.16–2.95 | 0.009 | 0.93 | 0.63–1.36 | 0.69 | 1.16 | 0.82–1.64 | 0.39 |
| Accelerated FEV1 decline | 2.17 | 1.40–3.35 | <0.001 | 2.12 | 1.54–2.91 | <0.001 | 2.18 | 1.59–2.99 | <0.001 |
| Ever smoker | 0.92 | 0.58–1.44 | 0.70 | 0.77 | 0.56–1.05 | 0.09 | 1.60 | 1.18–2.17 | 0.003 |
| WTC exposure morning of 9/11 | 1.40 | 0.84–2.32 | 0.19 | 1.58 | 1.14–2.20 | 0.006 | 0.86 | 0.59–1.26 | 0.44 |
| Variables | Asthma/COPD Overlap vs. Isolated-Asthma |
Asthma/COPD Overlap vs. Isolated-COPD |
||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |||
| Eosinophils ≥ 300 cells/μlc | 2.00 | 1.11–3.62 | 0.02 | 1.60 | 0.89–2.85 | 0.12 | ||
| Accelerated FEV1 decline | 1.02 | 0.60–1.74 | 0.94 | 0.99 | 0.60–1.65 | 0.98 | ||
| Ever smoker | 1.19 | 0.69–2.05 | 0.52 | 0.57 | 0.34–0.98 | 0.04 | ||
| WTC exposure morning of 9/11 |
0.88 | 0.49–1.61 | 0.68 | 1.62 | 0.88–3.01 | 0.12 | ||
N=2,124 due to missing covariates
Adjusted for age, race, BMI, first post-9/11 FEV1/FVC
First post-9/11 measurement
To confirm that elevated post-9/11 eosinophil concentration and accelerated FEV1 decline were associated with incident asthma/COPD overlap, we carried out a sensitivity analysis excluding patients with a pre-exposure PFT that showed a FEV1/FVC ratio<0.7 (N=69). First post-9/11 eosinophil concentration ≥300 cells/μl and accelerated FEV1 decline both remained significant predictors of asthma/COPD overlap (HR: 1.67, 95% CI: 1.03–2.71, p=0.03 and HR: 2.15, 95% CI: 1.35–3.43, p=0.001, respectively). To assess if pre-exposure blood eosinophil levels were indicative of a predisposition to asthma/COPD overlap, we performed another sensitivity analysis using pre-9/11 eosinophil concentration in place of the post-9/11 measurement. The subgroup of participants who had had a pre-9/11 blood draw (N=1,008) had baseline characteristics and lung function similar to those of the full study population (data not shown). We found that pre-9/11 eosinophil concentration ≥300 cells/μl was also associated with the outcome (HR: 1.42, 95% CI: 1.22–1.66, p<0.001). Change in eosinophil concentration from pre- to post-9/11 was not associated with asthma/COPD overlap (data not shown).
In order to gain further insight into the immunological pathways associated with isolated-asthma, isolated-COPD, and asthma/COPD overlap, we examined serum Th1, Th-17 and Th2 biomarkers obtained within six months of 9/11. A multivariable marginal Cox regression analysis for multiple events in the serum biomarker subpopulation (N=215) showed that higher early post-9/11 IgE was associated with incident asthma/COPD overlap, but this result was not significant after adjustment for multiple comparisons (Table 4). We found that elevated IL-4 predicted asthma/COPD overlap and elevated IL-21 predicted both isolated-asthma and isolated-COPD, while elevated IFN-γ was a protective factor for isolated-asthma and isolated-COPD. Early post-9/11 levels of IL-5, IL-13, IL-17, IL-23 and IL-6 were not associated with any of the three mutually exclusive outcomes (data not shown).
Table 4:
Marginal Cox regression models predicting isolated-asthma, isolated-COPD, and asthma/COPD overlap in the subpopulation with serum drawn between 9/11/2001 and 3/10/2002ab
| Variables | Asthma/COPD Overlap vs. Neither |
Isolated-Asthma vs. Neither |
Isolated-COPD vs. Neither |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| IgEc | 2.31 | 1.14–4.67 | 0.02d | 1.21 | 0.92–1.58 | 0.16 | 1.14 | 0.81–1.62 | 0.45 |
| IFN-γc | 0.42 | 0.22–0.81 | 0.01d | 0.48 | 0.32–0.70 | <0.001 | 0.45 | 0.28–0.70 | <0.001 |
| IL-21c | 1.33 | 0.89–1.98 | 0.17 | 1.73 | 1.27–2.35 | <0.001 | 2.06 | 1.31–3.23 | 0.002 |
| IL-4 substituted for IL-21 in Marginal Cox regression model | |||||||||
| IL-4c | 1.51 | 1.17–1.95 | 0.002 | 1.68 | 1.08–2.61 | 0.02d | 1.35 | 0.96–1.91 | 0.08 |
N=215;
Adjusted for age, race, BMI, smoking status, WTC exposure level, first post 9/11 FEV1/FVC;
One log2 increase (doubling) of cytokine concentration.
A p value of 0.0024 was considered significant after bonferroni correction.
Discussion
The WTC-exposed FDNY firefighter population is a cohort comprised of previously healthy males. Importantly, asthma documented during pre-employment medical evaluation precludes employment as a FDNY firefighter. Those who develop reactive airways disease during their career are removed from active duty;17 therefore, the prevalence of pre-9/11 asthma in this cohort was low. The massive irritant exposure at the WTC site resulted in an acute drop in lung function, with rescue/recovery workers going on to experience air trapping as well as fixed and reversible airflow obstruction.2–4 In this study, we observed that elevated early post-9/11 blood eosinophil concentration predicted irritant-associated asthma/COPD overlap, but not isolated-asthma or isolated-COPD. A sensitivity analysis observed pre-911 elevated eosinophils were a risk factor for asthma/COPD overlap. This suggests a pre-WTC exposure predisposition to irritant-associated fixed and reversible airway injury. While we found some overlapping biomarkers of these outcomes, the observation that there are unique biomarkers of vulnerability to asthma/COPD overlap, isolated-asthma and isolated-COPD suggests the potential for different pathological processes for these three diagnoses; this could be explored in future studies.
The FDNY WTC-exposed cohort has advantages for investigating irritant-associated airways disease. Data from a centralized post-WTC medical treatment program enabled explicit diagnostic criteria for incident isolated-asthma, isolated-COPD and asthma/COPD overlap. Pre-9/11 lung function and blood data were available for a large subset of the cohort, enabling assessment of early indicators of susceptibility to subsequent airway injury. Our observation that pre-exposure eosinophil concentration was associated with later asthma/COPD overlap suggests patient-intrinsic vulnerability to the damaging effects of WTC dust exposure. How much the exposure itself contributed to the presentation is limited because not every assessment was performed pre-exposure.
Compared with those who developed isolated-asthma or isolated-COPD, asthma/COPD overlap patients had lower post-exposure FEV1 and FEV1/FVC ratio. An investigation in a cohort without WTC exposure found that low lung function in childhood was a risk factor for subsequent asthma/COPD overlap,18 and so our observed associations between early lung function measurements and this outcome may be evidence of similar biological mechanism(s). Both the asthma/COPD overlap and isolated-COPD subgroups have progressive airway injury, with greater post-9/11 FEV1 decline rates than individuals with isolated-asthma or neither diagnosis. The asthma/COPD overlap subgroup also experienced more air trapping, shown by higher RV/TLC at the time of BD-PFT. This is consistent with prior investigation of asthma/COPD overlap in never-smokers19 and could be evidence of the severity of small airways dysfunction associated with WTC exposure.20
Eosinophils and IgE are two Th-2 mediators that have been extensively studied as risk factors for asthma, COPD and asthma/COPD overlap.12,21–25 In this investigation, serum IgE was associated with asthma/COPD overlap but did not achieve significance after bonferroni adjustment for multiple comparisons. We did observe a significant association between serum levels of the Th-2 cytokine IL-4 and this outcome. IL-4 may be a biomarker on the causal pathway to irritant-iassociated asthma/COPD overlap, since inhibiting it with Dupilumab reduced asthma severity in non-WTC-exposed patients with or without high eosinophil levels.26,27 Further investigation is required to assess the Th-2 pathway(s) that are associated with FEV1 decline, airflow limitation and bronchodilator response following an intense irritant exposure.
The incident asthma observed in our study is a variant of irritant-induced asthma.28 That it was associated with high-intensity WTC exposure but not eosinophil concentration suggests that airway reactivity in this cohort is a form of noneosinophilic asthma.29 IFN-γ was a protective biomarker for this condition, and also for isolated-COPD. High IFN-γ is associated with low IL-4 in modulation of pulmonary lymphocyte-mediated innate immunity.30 Furthermore, asthma is associated with blunted IFN-γ response.31,32
The balance between Th-2 and Th-17 cytokines in airway inflammation is under active investigation.33–35 IL-21, which was found to significantly predict isolated-asthma and isolated-COPD in our cohort, is a component of the Th-17 pathway that is produced by innate lymphoid cells that regulate airway inflammation.36 Elevated levels are associated with airway inflammation in mouse models and humans.37–39 The data from the WTC-exposed FDNY cohort is consistent with a Th-2 and Th-17 response predicting airway remodeling and reactivity. These data support further investigation of the innate Th-17 response to pulmonary irritants.
In univariable analyses, we found that in addition to high eosinophil concentration and accelerated FEV1 decline, ever-smoking was associated with asthma/COPD overlap. After adjusting for confounders, such as post-9/11 lung function, smoking was a unique risk factor for isolated-COPD but not isolated-asthma or asthma/COPD overlap. Therefore, the relationship between smoking and asthma/COPD overlap in this cohort was confounded by the other covariates. High WTC exposure level was not associated with isolated-COPD or asthma/COPD overlap, which suggests that an intense but brief irritant exposure did not increase risk of airway remodeling. In this cohort, isolated-COPD was not associated with eosinophil levels. In a population with smoking-related COPD, however, elevated blood eosinophil concentration was a biomarker of increased exacerbation.40 The variability of eosinophil effect reported in the literature may be related to the proportion of the study cohorts with an asthma component.41,42
There are several limitations to this investigation. The FDNY firefighters are overwhelmingly white, male, and experienced a massive irritant exposure, potentially limiting generalizability of these findings; however, most findings from the FDNY cohort have been replicated in other WTC-exposed cohorts. Our definitions of isolated asthma, asthma/COPD overlap and isolated COPD depend on results from the most recent BD-PFT. It is possible that those with isolated COPD, defined as FEV1/FVC < 0.7 and no bronchodilator response in this study, have asthma/COPD overlap since we did not proceed to methacholine challenge testing in the subgroup. Similarly those with asthma/COPD overlap, defined as FEV1/FVC < 0.7 and a bronchodilator response, may not have persistent with FEV1/FVC < 0.7 with permanent airway remodeling. A third limitation may be the use of eosinophils ≥300 or <300 cells/μl in our analyses. We modeled post-9/11 eosinophils as a continuous variable and still observed a significant association with asthma/COPD overlap. This suggests cut-point selection did not drive the analyses. Lastly, this study was vulnerable to selection bias. The study population with clinically-indicated BD-PFT was systematically different from those without BD-PFT, with more intense WTC exposure, higher eosinophil levels and post-WTC exposure lower lung function. This precludes assessment of rates of asthma/COPD overlap in the entire cohort, since undiagnosed cases are likely. Nevertheless, analyses within the BD-PFT population provide a valid assessment of risk factors for specific diagnoses within a symptomatic subgroup.
The data from the FDNY WTC Health Program is a valuable resource for understanding irritant-associated airways disease in a previously healthy population. High eosinophil concentrations, uniquely associated with asthma/COPD overlap in this population, may reflect biological pathways that predispose one to exaggerated inflammation and/or poor counter-regulatory responses to inflammation, leading to reversible and fixed airflow obstruction. There may be potential for early interventions that involve targeting specific inflammatory pathways in an attempt to improve lung function outcomes.
Acknowledgements
Funding:
This study was supported by NIOSH contracts #200–2011-39383, #200–2011-39378, #200–2017-93426 and #200–2017-93326, NIOSH grants U01 OH011302 and U01 OH011300, and NHLBI grant R01HL119326
All authors received support from grants and/or contracts from the National Institute of Occupational Safety and Health and/or NIH/NHLBI.
Role of sponsors:
The sponsors had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, the preparation, review, and approval of the manuscript, or the decision to submit the manuscript for publication.
Abbreviation list
- ATS
American Thoracic Society
- BD
Bronchodilator
- BMI
Body mass index
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- FDNY
Fire Department of the City of New York
- FEV1
Forced expiratory volume at one second
- FVC
Forced vital capacity
- GOLD
Global Initiative for Obstructive Lung Disease
- HR
Hazard ratio
- μl
Microliter
- ml
Milliliter
- PFT
Pulmonary function test
- RV
Residual volume
- SD
Standard deviation
- SEM
Standard error
- TLC
Total lung capacity
- WTC
World Trade Center
Footnotes
Conflicts of interest and financial disclosures:
All authors received support from grants and/or contracts from the National Institute of Occupational Safety and Health and/or NIH/NHLBI.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lioy PJ, Weisel CP, Millette JR, et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environmental health perspectives. 2002;110(7):703–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldrich TK, Gustave J, Hall CB, et al. Lung function in rescue workers at the World Trade Center after 7 years. The New England journal of medicine. 2010;362(14):1263–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiden MD, Ferrier N, Nolan A, et al. Obstructive airways disease with air trapping among firefighters exposed to World Trade Center dust. Chest. 2010;137(3):566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aldrich TK, Vossbrinck M, Zeig-Owens R, et al. Lung Function Trajectories in World Trade Center-Exposed New York City Firefighters Over 13 Years: The Roles of Smoking and Smoking Cessation. Chest. 2016;149(6):1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeig-Owens R, Singh A, Aldrich TK, et al. Blood Leukocyte Concentrations, FEV1 Decline, and Airflow Limitation: A 15-Year Longitudinal Study of WTC-Exposed Firefighters. Annals of the American Thoracic Society. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christenson SA, Steiling K, van den Berge M, et al. Asthma-COPD overlap. Clinical relevance of genomic signatures of type 2 inflammation in chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine. 2015;191(7):758–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. American journal of respiratory and critical care medicine. 2017;195(5):557–582. [DOI] [PubMed] [Google Scholar]
- 8.Cosentino J, Zhao H, Hardin M, et al. Analysis of Asthma-Chronic Obstructive Pulmonary Disease Overlap Syndrome Defined on the Basis of Bronchodilator Response and Degree of Emphysema. Annals of the American Thoracic Society. 2016;13(9):1483–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baarnes CB, Andersen ZJ, Tjonneland A, Ulrik CS. Incidence and long-term outcome of severe asthma-COPD overlap compared to asthma and COPD alone: a 35-year prospective study of 57,053 middle-aged adults. International journal of chronic obstructive pulmonary disease. 2017;12:571–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. The Journal of asthma : official journal of the Association for the Care of Asthma. 2011;48(3):279–285. [DOI] [PubMed] [Google Scholar]
- 11.Lange P, Colak Y, Ingebrigtsen TS, Vestbo J, Marott JL. Long-term prognosis of asthma, chronic obstructive pulmonary disease, and asthma-chronic obstructive pulmonary disease overlap in the Copenhagen City Heart study: a prospective population-based analysis. The Lancet. Respiratory medicine. 2016;4(6):454–462. [DOI] [PubMed] [Google Scholar]
- 12.Gao J, Zhou W, Chen B, Lin W, Wu S, Wu F. Sputum cell count: biomarkers in the differentiation of asthma, COPD and asthma-COPD overlap. International journal of chronic obstructive pulmonary disease. 2017;12:2703–2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Konno S, Taniguchi N, Makita H, et al. Distinct Phenotypes of Smokers with Fixed Airflow Limitation Identified by Cluster Analysis of Severe Asthma. Annals of the American Thoracic Society. 2018;15(1):33–41. [DOI] [PubMed] [Google Scholar]
- 14.Woodruff PG, van den Berge M, Boucher RC, et al. American Thoracic Society/National Heart, Lung, and Blood Institute Asthma-Chronic Obstructive Pulmonary Disease Overlap Workshop Report. American journal of respiratory and critical care medicine. 2017;196(3):375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. The European respiratory journal. 2005;26(2):319–338. [DOI] [PubMed] [Google Scholar]
- 16.Global Initiative for Asthma. Global strategy for asthma management and prevention (2017 update). Vancouver, USA: Global Initiative for Asthma;2017. [Google Scholar]
- 17.Niles JK, Webber MP, Gustave J, et al. The impact of the World Trade Center attack on FDNY firefighter retirement, disabilities, and pension benefits. American journal of industrial medicine. 2011;54(9):672–680. [DOI] [PubMed] [Google Scholar]
- 18.Bui DS, Burgess JA, Lowe AJ, et al. Childhood Lung Function Predicts Adult Chronic Obstructive Pulmonary Disease and Asthma-Chronic Obstructive Pulmonary Disease Overlap Syndrome. American journal of respiratory and critical care medicine. 2017;196(1):39–46. [DOI] [PubMed] [Google Scholar]
- 19.Gelb AF, Yamamoto A, Verbeken EK, Nadel JA. Unraveling the Pathophysiology of the Asthma-COPD Overlap Syndrome: Unsuspected Mild Centrilobular Emphysema Is Responsible for Loss of Lung Elastic Recoil in Never Smokers With Asthma With Persistent Expiratory Airflow Limitation. Chest. 2015;148(2):313–320. [DOI] [PubMed] [Google Scholar]
- 20.Friedman SM, Maslow CB, Reibman J, et al. Case-control study of lung function in World Trade Center Health Registry area residents and workers. American journal of respiratory and critical care medicine. 2011;184(5):582–589. [DOI] [PubMed] [Google Scholar]
- 21.Hastie AT, Martinez FJ, Curtis JL, et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. The Lancet. Respiratory medicine. 2017;5(12):956–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kitaguchi Y, Komatsu Y, Fujimoto K, Hanaoka M, Kubo K. Sputum eosinophilia can predict responsiveness to inhaled corticosteroid treatment in patients with overlap syndrome of COPD and asthma. International journal of chronic obstructive pulmonary disease. 2012;7:283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cosio BG, Soriano JB, Lopez-Campos JL, et al. Defining the Asthma-COPD Overlap Syndrome in a COPD Cohort. Chest. 2016;149(1):45–52. [DOI] [PubMed] [Google Scholar]
- 24.Hirai K, Shirai T, Suzuki M, et al. A clustering approach to identify and characterize the asthma and chronic obstructive pulmonary disease overlap phenotype. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2017;47(11):1374–1382. [DOI] [PubMed] [Google Scholar]
- 25.Tamada T, Sugiura H, Takahashi T, et al. Biomarker-based detection of asthma-COPD overlap syndrome in COPD populations. International journal of chronic obstructive pulmonary disease. 2015;10:2169–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wenzel S, Castro M, Corren J, et al. Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting beta2 agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet (London, England). 2016;388(10039):31–44. [DOI] [PubMed] [Google Scholar]
- 27.Wenzel S, Ford L, Pearlman D, et al. Dupilumab in persistent asthma with elevated eosinophil levels. The New England journal of medicine. 2013;368(26):2455–2466. [DOI] [PubMed] [Google Scholar]
- 28.Tarlo SM, Lemiere C. Occupational asthma. The New England journal of medicine. 2014;370(7):640–649. [DOI] [PubMed] [Google Scholar]
- 29.Carr TF, Zeki AA, Kraft M. Eosinophilic and Noneosinophilic Asthma. American journal of respiratory and critical care medicine. 2018;197(1):22–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bal SM, Bernink JH, Nagasawa M, et al. IL-1beta, IL-4 and IL-12 control the fate of group 2 innate lymphoid cells in human airway inflammation in the lungs. Nature immunology. 2016;17(6):636–645. [DOI] [PubMed] [Google Scholar]
- 31.Message SD, Laza-Stanca V, Mallia P, et al. Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 production. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(36):13562–13567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silver JS, Kearley J, Copenhaver AM, et al. Inflammatory triggers associated with exacerbations of COPD orchestrate plasticity of group 2 innate lymphoid cells in the lungs. Nature immunology. 2016;17(6):626–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choy DF, Hart KM, Borthwick LA, et al. TH2 and TH17 inflammatory pathways are reciprocally regulated in asthma. Science translational medicine. 2015;7(301):301ra129. [DOI] [PubMed] [Google Scholar]
- 34.Dillon MB, Schulten V, Oseroff C, et al. Different Bla-g T cell antigens dominate responses in asthma versus rhinitis subjects. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2015;45(12):1856–1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu W, Liu S, Verma M, et al. Mechanism of TH2/TH17-predominant and neutrophilic TH2/TH17-low subtypes of asthma. The Journal of allergy and clinical immunology. 2017;139(5):1548–1558.e1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coquet JM, Schuijs MJ, Smyth MJ, et al. Interleukin-21-Producing CD4(+) T Cells Promote Type 2 Immunity to House Dust Mites. Immunity. 2015;43(2):318–330. [DOI] [PubMed] [Google Scholar]
- 37.Lajoie S, Lewkowich I, Herman NS, et al. IL-21 receptor signalling partially mediates Th2-mediated allergic airway responses. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2014;44(7):976–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qaseem AS, Singh I, Pathan AA, et al. A Recombinant Fragment of Human Surfactant Protein D Suppresses Basophil Activation and T-Helper Type 2 and B-Cell Responses in Grass Pollen-induced Allergic Inflammation. American journal of respiratory and critical care medicine. 2017;196(12):1526–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ricciardolo FLM, Sorbello V, Folino A, et al. Identification of IL-17F/frequent exacerbator endotype in asthma. The Journal of allergy and clinical immunology. 2017;140(2):395–406. [DOI] [PubMed] [Google Scholar]
- 40.Watz H, Tetzlaff K, Wouters EF, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a posthoc analysis of the WISDOM trial. The Lancet. Respiratory medicine. 2016;4(5):390–398. [DOI] [PubMed] [Google Scholar]
- 41.Papi A, Kostikas K, Wedzicha JA, et al. Dual Bronchodilation Response by Exacerbation History and Eosinophilia in the FLAME Study. American journal of respiratory and critical care medicine. 2017. [DOI] [PubMed] [Google Scholar]
- 42.Song JH, Lee CH, Kim JW, et al. Clinical implications of blood eosinophil count in patients with non-asthma-COPD overlap syndrome COPD. International journal of chronic obstructive pulmonary disease. 2017;12:2455–2464. [DOI] [PMC free article] [PubMed] [Google Scholar]


