Abstract
Objective:
Our objectives were to characterize the association of longitudinal changes in maternal anthropometric measures with neonatal anthropometry and to assess to what extent late gestational changes in maternal anthropometry are associated with neonatal body composition.
Design:
In a prospective cohort of pregnant women, maternal anthropometry was measured at 6 study visits across pregnancy and after birth, neonates were measured and fat and lean mass calculated. We estimated maternal anthropometric trajectories and separately assessed rate of change in the second (15–28 weeks) and third trimester (28–39 weeks) in relation to neonatal anthropometry. We investigated the extent to which tertiles of third trimester maternal anthropometry change were associated with neonatal outcomes.
Setting:
Women were recruited from 12 U.S. sites (2009–2013).
Subjects:
2334 non-obese women with singleton pregnancies.
Results:
A higher rate of increase in gestational weight gain (GWG) was associated with larger birthweight infants with greater lean and fat mass. In contrast, higher rates of increase in maternal anthropometry measures were not associated with infant birthweight but were associated with decreased neonatal lean mass. In the third trimester, women with the tertile of lowest change in triceps skinfold (−0.57 to −0.06 mm per week) had neonates with 35.8g more lean mass than neonates of mothers with the middle tertile rate of change (−0.05 to 0.06 mm per week).
Conclusion:
The rate of change in third trimester maternal anthropometry measures may be related to neonatal lean and fat mass yet have a negligible impact on infant birthweight, indicating that neonatal anthropometry may provide additional information over birthweight alone.
Keywords: Anthropometry, Neonatal, body composition, gestational weight gain, longitudinal
Introduction
The relationship between gestational weight gain (GWG) and infant birthweight is well documented 1–3. In underweight, normal weight, and overweight women, GWG below recommendations is associated with small-for-gestational age birthweight while excess GWG is associated with large-for-gestational-age birthweight 1, 4 However, both GWG and birthweight are non-specific measures of maternal nutritional status and fetal size. They provide little insight into the extent to which the composition of maternal gains is associated with neonatal size and body composition. For example, GWG does not distinguish gains in maternal lean mass from gains in fat mass, each of which may be differentially associated with fetal growth and body composition 5. Similarly, birthweight does not adequately distinguish between neonatal fat and lean mass. As small- and large-for-gestational age infants are at an increased risk for short- and long-term risks of obesity, metabolic disorders,6, 7 and cognitive health8, understanding whether specific parameters of maternal weight gain impact neonatal body composition is important to inform future clinical guidance to prevent adverse birthweight and longer term outcomes.
Some investigators have studied relations between the total change in maternal fat and lean mass with birthweight 9–11 or GWG with neonatal lean and fat mass 5, 11, 12, but the association of readily assessable longitudinal changes in maternal body composition with neonatal body composition is unknown. Longitudinal changes may provide additional insight beyond total GWG alone based on the timing of maternal anthropometric changes. Maternal fat mass typically increases in mid-gestation with increased insulin-sensitivity,13 then decreases late in gestation with a slowing insulin response14, 15. The decreased insulinsensitivity is hypothesized to occur to mobilize maternal fat stores to support rapid fetal growth towards the end of gestation, when maternal nutritional intake alone would be insufficient 11. Diverging from this process may impact the appropriate accumulation of fetal fat and fat-free mass7. Therefore, components of GWG may provide a more sensitive and specific marker of infants at risk for inadequate or excessive birthweight.
Our objectives were to estimate the association of longitudinal changes in maternal anthropometric measures with neonatal body composition and birthweight, and to assess to what extent late gestational changes in maternal anthropometry are associated with neonatal body composition and size.
Methods
The NICHD Fetal Growth Studies-Singletons was a prospective cohort study of 2,334 non-obese pregnant women aged 18–40 years recruited from 12 U.S. sites between July 2009 and January 2013. Lowrisk, non-obese healthy women with spontaneously conceived pregnancies <14 weeks of gestation who were at no obvious risk for fetal growth restriction or overgrowth were selected for inclusion. Additional exclusion criteria included smoking, pre-gestational diabetes, chronic renal disease under medical supervision, autoimmune disease, psychiatric disorders, cancer, and HIV/AIDS 16, 17
At enrollment between 8 weeks 0 days and 13 weeks 6 days, research nurses conducted in-person interviews to obtain detailed demographic and health characteristics. Women were randomized into 1 of 4 follow-up schedules starting at 15 weeks to capture weekly data without subjecting each woman to weekly follow-up visits 16. Ultrasound exams were performed to collect fetal biometric measurements, including head circumference, abdominal circumference and femur length, that were then used to calculate estimated fetal weight 18.
Gestational weight gain was calculated as the difference between maternal weight and self-reported pre-pregnancy weight. Maternal weight was measured at each study visit without shoes or excessive clothing using a beam balance or digital scale. Antenatal weights from clinical visits were also abstracted from prenatal records. We included all weights (i.e., those measured at both routine prenatal and study visits) to increase the number of weight measurements per woman for improved precision of maternal weight gain estimates and trajectories. We plotted individual women’s weight change trajectory using all weights to ensure abstracted weights fell within plausible ranges when plotted with study-visit weights. If a chart abstracted and study-visit measured weight occurred on the same day, we included only the measured weights (n=2169 duplicate weights out of 45,540, 4.7%). Height was measured using a portable stadiometer (Seca Corporation, Hamburg, Germany; US office, Hanover, MD) and along with self-reported pre-pregnancy weight was used to calculate pre-pregnancy body mass index (BMI, kg/m2).
Research staff also collected additional maternal anthropometric measures at each of the 5 study visits. Mid-upper arm circumference was measured using a non-stretchable linen tape to the nearest 0.1cm. The triceps skinfold was measured at the point of mid-upper arm circumference and subscapular skinfold was measured at a 45 degree incline at the site inferior to inferior angle of the scapula using the Lange skinfold caliper (Beta Technology, Inc., Santa Cruz, CA).
Neonatal measurements were collected after delivery. Length was measured using a Seca 416 infantometer and weight was measured using an infant beam balance scale or an infant electronic (digital) scale. Neonatal abdominal flank skinfold was measured at midaxillary line just above the crest of the right ilium using Lange skinfold caliper (Beta Technology, Inc., Santa Cruz, CA). We calculated neonatal lean and fat mass using the following validated equations 19:
Fat Mass: 0.39055*Birthweight (kg) + 0.0453*Abdominal flank (cm) - 0.03237*Length (cm) + 0.5465
Lean Mass: Birthweight (kg) - Fat Mass (kg)
Fat Percentage: Fat mass (kg) / Birthweight (kg)*100
All maternal and neonatal anthropometric sites were measured in duplicate and average readings were used for analysis. If the second measure differed by a pre-specified value 20, 21, specific to each anthropometric measure, a third measure was performed and the average of the two closest measurements was used.
Statistical Analysis
In our analytic sample of 2334 women, we excluded a total of 423 (18%) observations due to the following reasons: loss to follow-up [157(6.7%)], the use of non-study approved calipers [160 (6.8%); one site], miscarriage or termination [12 (0.51%)], congenital malformations [63 (2.6%)], birthweight (<2000g) [11 (0.47%)] and implausible neonatal length values [9 (0.39%)]. The final sample included 1911 women. The relationships of longitudinal changes in maternal mid upper arm circumference, subscapular skinfold, triceps skinfold, arm muscle and arm fat areas, with neonatal lean mass, fat mass, fat percentage and birthweight were analyzed in two steps. In the first step, longitudinal trajectories of maternal anthropometry were assessed by fitting separate linear mixed models to each measure. We included terms for fixed and random effects to allow for estimation of the overall mean and individual trajectories, respectively, across gestation. For both the fixed and random effects, all linear mixed models included a quadratic term for gestational age to allow for model flexibility, selected based on the lowest Bayesian information criteria indicating model fit. We estimated individual anthropometric measures at 15, 28, and 40 weeks, and calculated the rate of change in each measure for the second (15–28 weeks) and third (28–40 weeks) trimesters. The cut point of 15 weeks was selected since there were no study visits at 14 weeks. Also, we divided the third trimester rates of gain into tertiles (<33rd and ≥66th percentiles) to assess to what extent rates of change in the lower or upper tertile were associated with neonatal size and body composition. In the second step, we used linear regression to assess the change in maternal anthropometry estimated at specific gestational ages based on the above model in relation to neonatal lean mass, fat mass, fat percentage and birthweight. We adjusted for maternal race, infant sex, parity, age, height, pre-pregnancy BMI, income, education, gestational age at delivery, baseline maternal anthropometry value, and the number days after delivery neonates were measured.
Separate trajectories for GWG were calculated using linear mixed models, as described above, to provide a comparison for individual anthropometric measures. Estimated fetal weight trajectories were also calculated using linear mixed models. In a secondary analysis, we eliminated part of the inherent correlation between GWG and fetal size by subtracting estimated fetal weight from maternal weight for a measure of net GWG. In an effort to isolate the association between maternal anthropometry and neonatal fat mass, independent of birthweight, we conducted sensitivity analyses accounting for neonatal size (i.e., birthweight). Due to the high correlation between birthweight and neonatal fat mass (0.84), we regressed birthweight on fat mass to obtain the residuals and used the residuals as the outcome in analyses with maternal anthropometry. Analyses were repeated after removing births <39 weeks’ gestation to determine if the trajectories were biased by earlier deliveries. To ensure that the observed relationships were not a function of the equations used to calculate neonatal lean and fat mass, we repeated the analyses using individual neonatal measures (length and abdominal flank skinfold). We tested for differences in the association between the rate of change in maternal anthropometry and neonatal anthropometry by maternal pre-pregnancy BMI, race, and the second trimester rate of change (third trimester models only). Analyses were conducted using SAS version 9.4 (SAS Institute, Inc. Cary, North Carolina, U.S.)22 and Stata software, version 13.0 (StataCorp, College Station, TX)23.
Results
The majority of women were married, had an income >50,000, 49.5% were nulliparous, and 50.3% were 20–29 years of age. The racial/ethnic distribution included 28.8% non-Hispanic white, 29.8% Hispanic and 21.4% and 20% of non-Hispanic black and Asian women, respectively (Table 1).
Table 1:
Demographic Characteristics in 1911 women
| Overall N (%) |
|
|---|---|
| Maternal Age, y | |
| <20 | 86 (4.50) |
| 20–29 | 962 (50.3) |
| 30–39 | 849 (44.4) |
| 40–44 | 14 (0.80) |
| Race/Ethnicity | |
| Non-Hispanic White | 550 (28.8) |
| Non-Hispanic Black | 409 (21.4) |
| Hispanic | 570 (29.8) |
| Asian and Pacific Islander | 382 (20.0) |
| Marital Status | |
| Never Married | 351 (18.4) |
| Married | 1506 (78.8) |
| Divorced/Widowed | 52 (2.80) |
| Income | |
| <$30,000 | 363 (19.0) |
| 30,000-$39,999 | 149 (7.80) |
| 40,000-$49,999 | 139 (7.27) |
| 50,000-$74,999 | 218 (11.4) |
| 75,000-$99,999 | 244 (12.8) |
| ≥$100,000 | 523 (27.4) |
| Parity | |
| 0 | 945 (49.5) |
| 1 | 659 (34.5) |
| ≥2 | 307 (16.0) |
| Timing of Neonatal Measurements (days from delivery), median (IQR) |
1 (1–2) |
Figure 1 depicts the estimated trajectories for each maternal anthropometric measure. Mid-upper arm circumference, subscapular skinfold, and triceps skinfold all increased from 15–28 weeks. From 28–40 weeks, the trajectory for mid-upper arm circumference increased slightly [mean (IQR) total change of 0.39cm (0.12, 0.64)] (Table 2), while triceps skinfold only increased until about 28 weeks [mean (IQR) change: 1.02 (0.21, 1.91)], then had a plateau that was followed by a slight decrease until 40 weeks [mean (IQR) change: −0.003 (−0.08, 0.08)].
Figure 1:
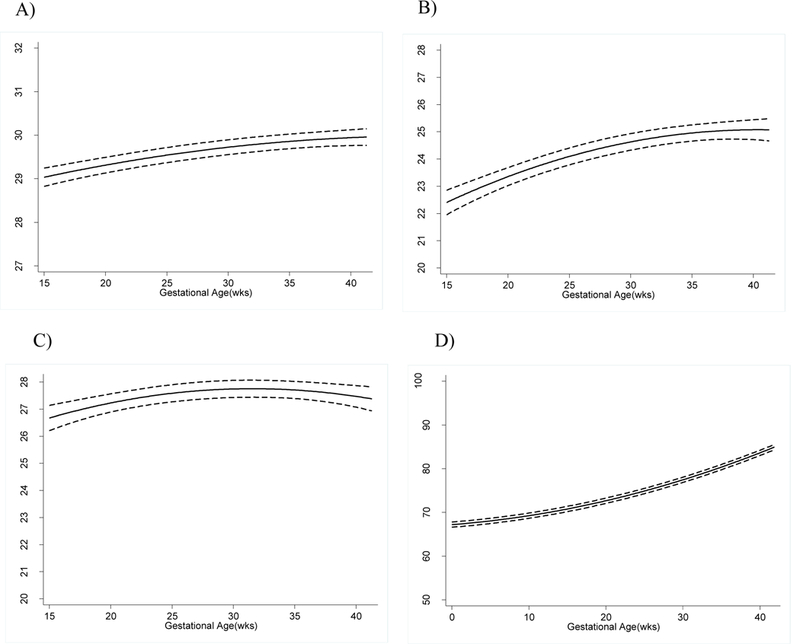
Trajectories estimated using linear mixed models for maternal A) mid-upper arm circumference B) subscapular skinfold C) triceps skinfold D) weight from 15 to 40 weeks gestation.
Table 2:
The distribution of the total change in maternal anthropometry measures by Second Trimester and late gestation and of neonatal anthropometry measures at birth
| Second Trimester 15–28 weeks |
Third Trimester 28–40 weeks |
At Birth | |||
|---|---|---|---|---|---|
| Total Change Median(IQR) |
Rate of Change (per week) Median(IQR) |
Total Change Median(IQR) |
Rate of Change (per week) Median(IQR) |
Absolute Size Median(IQR) |
|
| Maternal Anthropometry | |||||
| Mid-upper arm circumference (cm) | 0.83 (0.53, 1.14) | 0.06 (0.04, 0.08) | 0.39 (0.12, 0.64) | 0.03 (0.01, 0.05) | |
| Subscapular Skinfold (mm) | 2.29 (1.99, 2.61) | 0.15 (0.13, 0.17) | 0.97 (0.53, 1.44) | 0.08 (0.04, 0.12) | |
| Tricep skinfold (mm) | 1.02 (0.21, 1.91) | 0.08 (0.02, 0.15) | −0.03 (−0.91, 0.92) | −0.003 (−0.08, 0.08) | |
| Maternal Weight Change (kg) | 5.78 (4.65, 6.94) | 0.44 (0.36, 0.53) | 7.43 (5.71, 9.18) | 0.61 (0.47, 0.76) | |
| Neonatal Anthropometry | |||||
| Abdominal flank (cm) Length (cm) | 40 (30, 50) | ||||
| Length (cm) | 50 (48, 52) | ||||
| Fat Mass (g) * | 395 (302, 508) | ||||
| Lean Masst‡ | 2895 (2698, 3106) | ||||
| Percent Body Fat (%)§ | 12.1 (9.6, 14.3) | ||||
| Birthweight | 3290 (3030, 3600) | ||||
| Measurement days, postnatal | 1 (1, 2) | ||||
0.39055*Birthweight(kg) + 0.0453*Abdominal flank(cm) − 0.03237*Length(cm) + 0.5465
Birthweight(kg) - Fat Mass(kg)
Fat mass(kg) / Birthweight (kg)*100
The rate of change of various maternal anthropometric measures in the second (15 to 28 weeks) and third trimesters (28 to 40 weeks) were differentially associated with neonatal body composition (Table 3). Changes in maternal mid-upper arm circumference and triceps skinfold, but not subscapular skinfold, were associated with neonatal anthropometry. Specifically, a faster rate of increase in triceps skinfold in both the second (β: −15.9, 95% CI: −27.1, −4.74) and third trimester (β: −13.1, 95% CI: −22.7, −3.37) was associated with decreased neonatal lean mass. In the third trimester, a faster rate of increase in mid-upper arm circumference (β: −28.1g, 95% CI: - 60.2, −4.13) was also associated with decreased neonatal lean mass. In comparison, an increase in the rate of change in maternal weight was consistently associated with an increase in all of the neonatal anthropometric measures including lean mass, fat mass, and birthweight, though the magnitude of the association was slightly reduced after fetal size was subtracted from maternal weight (net GWG change).
Table 3:
Association between the rate of change in maternal anthropometry and neonatal anthropometry†
| Neonatal Anthropometry | ||||
|---|---|---|---|---|
| Maternal Anthropometry | Lean Mass (g) β (95% CI) |
Fat Mass (g) β (95% CI) |
Fat Percent (%) β (95% CI) |
Birthweight (g) β (95% CI) |
| Mid-upper arm circumference (per 1mm change/week) | ||||
| Second Trimester (15-<28wks) | −25.8 (−54.0, 2.35) | 9.64 (−7.71, 26.4) | 0.33 (−0.06, 0.73) | −13.61 (−53.4, 26.2) |
| Third Trimester (28–40wks) | −28.1 (−60.2, −4.13)* | 15.07 (−4.06, 34.2) | 0.48 (0.03, 0.93)* | −13.7 (−59.4, 31.9) |
| Subscapular Skinfold (per 0.1 mm change/week) | ||||
| Second Trimester (15-<28wks | −36.3 (−79.0, 6.33) | −10.75 (−36.3, 14.76) | −0.21 (−0.80, 0.39) | −39.1 (−99.3, 21.2) |
| Third Trimester (28–40wks) | −22.4 (−46.9, 2.24) | −6.29 (−21.0, 8.49) | −0.12 (−0.46, 0.23) | −24.5 (−59.3, 10.3) |
| Triceps skinfold (per 0.1mm change/week) | ||||
| Second Trimester (15-<28wks) | −15.9 (−27.1, −4.74)* | −0.51 (−7.18, 6.16) | −0.041 (−0.12, 0.19) | −13.7 (−29.5, 2.10) |
| Third Trimester (28–40wks) | −13.1 (−22,7, −3.37)* | −2.65 (−8.45, 3.14) | −0.028 (−0.16, 0.11) | −13.3 (−27.1, 0.35) |
| Maternal Weight Change (per 0.1kg change/week) | ||||
| Second Trimester (15-<28wks) | 31.8 (23.2, 40.5)* | 21.3 (16.2, 26.5)* | 0.44 (0.32, 0.56)* | 54.5 (42.3, 66.6)* |
| Third Trimester (28–40wks) | 12.9 (7.60, 18.4)* | 9.42 (6.22, 12.6)* | 0.19 (0.12, 0.26)* | 22.7 (15.2, 30.3)* |
| Net Weight Changet‡ (per 0.1kg change/week) | ||||
| Second Trimester (15-<28wks) | 24.6 (18.1, 31.2)* | 16.7 (12.8, 20.6)* | 0.34 (0.25, 0.44)* | 42.4 (33.3, 51.6)* |
| Third Trimester (28–40wks) | 7.43 (2.85, 12.01)* | 6.06 (3.33, 8.79)* | 0.12 (0.06, 0.18)* | 13.8 (7.37, 20.3)* |
P<0.05
Values are beta coefficients (95% CI); adjusted for race, infant sex, parity, age, height, pre-pregnancy BMI, gestational age at delivery, neonatal measurement date, and baseline anthropometry value; Neonatal lean mass, fat mass, and fat percent (n=1698), Birthweight (n=1759)
Calculated as the difference between maternal weight and estimated fetal weight’
Since late gestational changes in maternal anthropometric measures may indicate the mobilization of nutrient stores for fetal growth, we investigated the extent to which tertiles of change in the third trimester may be related to neonatal outcomes (Table 4). Women in the first tertile for triceps skinfold, with a rate of change between −0.57 to −0.06 mm per week, had neonates that had 35.8g more lean mass than neonates of mothers in the middle tertile (rate of change: −0.05 to 0.06 mm per week). Although, there was no significant overall association with birthweight. The remaining individual components of maternal anthropometry were not significantly associated with neonatal anthropometry. In contrast, a rate of change in the first tertile (−0.37 to 0.52 kg/week) of third trimester maternal weight gain compared to the middle tertile was associated with a −85.6g (95% CI: −128.1, −42.7) decrease in birthweight.
Table 4:
Association between the tertile of rate of change in maternal anthropometry in the third trimester (28–40wks) and neonatal anthropometry†
| Neonatal Anthropometry | ||||
|---|---|---|---|---|
| Maternal Anthropometry | Lean Mass (g) β (95% CI) |
Fat Mass (g) β (95% CI) |
Fat Percent (%) β (95% CI) |
Birthweight (g) β (95% CI) |
| Mid-Upper Arm Circumference (mm/week) | ||||
| −2.37 to 0.22 | 16.0 (−14.6, 46.6) | −9.05 (−27.2, 9.17) | −0.21 (−0.63, 0.23) | 12.6 (−30.6, 55.7) |
| 0.22 to 0.56 | Reference | Reference | Reference | Reference |
| 0.57 to 3.276 | −22.8 (−53.0, 7.46) | −8.72 (−26.7, 9.26) | −0.13 (−0.56, 0.29) | −26.7 (−69.4, 15.8) |
| Subscapular Skinfold (mm /week) | ||||
| −0.17 to 0.06 | 25.5 (−5.82, 56.9) | 6.75 (−12.0, 25.5) | 0.15 (−0.29, 0.59) | 33.9 (−10.3, 78.3) |
| 0.07 to 0.12 | Reference | Reference | Reference | Reference |
| 0.13 to 0.54 | 4.54 (−27.7, 36.8) | 2.21 (−17.1, 21.5) | 0.03 (−0.42, 0.48) | 12.8 (−32.8, 58.5) |
| Triceps Skinfold (mm /week) | ||||
| −0.57 to −0.06 | 35.8 (5.64, 65.9)* | 10.02 (−8.00, 28.1) | 0.18 (−0.24, 0.61) | 35.9 (−6.66, 78.6) |
| −0.05 to 0.06 | Reference | Reference | Reference | Reference |
| 0.07 to 0.63 | −4.78 (−35.3, 25.7) | 0.34 (−17.9, 18.5) | 0.09 (−0.33, 0.52) | −7.52 (−50.8, 35.7) |
| Weight Change (kg/week) | ||||
| −0.37 to 0.52 | −54.1 (−84.8, −23.5)* | −36.4 (−54.6, −18.2)* | −0.77 (−1.20, −0.34)* | −85.6 (−128.1, - 42.7)* |
| 0.51 to 0.71 | Reference | Reference | Reference | Reference |
| 0.72 to 1.73 | 25.1 (−5.00, 55.2) | 23.6 (5.70, 41.5)* | 0.45 (0.03, 0.87)* | 54.5 (12.1, 97.0)* |
| Net Weight Change‡ (kg/week) | ||||
| −0.06 to 0.04 | −14.7 (−45.5, 16.1) | −14.8 (−33.2, 3.59) | −0.30 (−0.73, −0.13)* | −25.3 (−68.7, 18.1) |
| 0.041 to 0.06 | Reference | Reference | Reference | Reference |
| 0.061 to 0.18 | 15.1 (−15.4, 45.3) | 19.4 (1.30, 37.5)* | 0.42 (−0.004, 0.85) | 40.8 (−2.05, 83.7) |
P<0.05
Values are beta coefficients (95% CI); adjusted for race, infant sex, parity, age, height, pre-pregnancy BMI, gestational age at delivery, and neonatal measurement date, and baseline anthropometry value; Neonatal lean mass, fat mass, and fat percent (n=1698), Birthweight (n=1759)
Calculated as the difference between maternal weight and estimated fetal weight
In sensitivity analyses accounting for birthweight, our results remained in a similar direction, but were now significant for mid-upper arm circumference and triceps skinfold. A faster rate of increase in maternal mid-upper arm circumference in both the second (β: 14.4, 95% CI: 4.89, 23.89) and third trimester (β: 17.1 95% CI: 4.05, 30.1) and triceps skinfold in the second trimester (β: 4.65, 95% CI: 0.89, 8.42) was associated with increased neonatal fat mass independent of birthweight (supplemental Table 1). When assessing tertiles of change using the residual method, the lowest tertile of change in maternal mid-upper arm circumference was associated with decreased neonatal fat mass independent of birthweight (β: −10.53, 95% CI: - 20.8, −0.27) (Supplemental Table 2).
Our results remained the same after limiting our analysis only to neonates born at gestational ages ≥39 weeks (the mean GA at delivery), providing confidence that the modeled maternal anthropometric trajectories were not biased by the inclusion of earlier deliveries. Our findings were consistent in analyses that included only individual neonatal anthropometric measures (length and abdominal flank skinfold used to calculate neonatal lean and fat mass, confirming the application of equations for calculating neonatal lean and fat mass for this population (data available on request). The association of maternal anthropometry with neonatal anthropometry did not differ by the second trimester rate of change (third trimester models only).
Discussion
Our study has demonstrated that the rate of change in maternal anthropometry may be related to neonatal lean and fat mass, yet has a negligible impact on infant birthweight indicating that neonatal anthropometry provides additional information over birthweight alone. Increases in maternal triceps skinfold thickness across the second and third trimesters, an indicator of an increase in maternal fat, was associated with decreased neonatal lean mass. As evidence suggests decreased lean mass is associated with an increased risk of a poorer metabolic profile later in life5, 8, our findings support the important insight into neonatal health provided by maternal anthropometric measures beyond total GWG alone.
The skinfold trajectories that we observed are similar to those documented in previous studies that described maternal skinfold changes in lean 24, 25, white 26, and homogenous ethnic populations9. Our study, which has documented an increase in neonatal lean and fat mass with an increased rate of GWG in the second and third trimester, is similar to studies that reported increased neonatal fat mass with excessive GWG in mid-late gestation 27 and at delivery28, but differ from other studies that reported increased neonatal fat and not lean mass with high maternal GWG only in the first half of pregnancy 12, 29.
The change in maternal fat skinfolds demonstrates the complex and dynamic state of pregnancy. Lipid metabolism is altered early in pregnancy to promote the storage of maternal fat, while later in pregnancy an increase in plasma fatty acid and glycerol concentrations corresponds to fat mobilization 14 Deviating from this expected pattern may reflect disrupted lipid metabolism or placental insufficiency 14, 30, ultimately limiting fetal gains. While we hypothesize that the lack of mobilization of maternal fat stores limits fetal lean mass acquisition, the exact mechanism and clinical importance of this relationship remains unclear and should be investigated in future studies. Furthermore, it is unclear why decreases in neonatal lean mass at birth were not reflected in birthweight, as reported in previous studies31, although previous studies have not been limited to normal and overweight women. One explanation may be the increase in birthweight due to neonatal fat mass, as indicated in our sensitivity analyses using the residual method, where an increased rate of maternal fat mass, particularly in the second trimester, was associated with increased neonatal fat mass independent of birthweight. The lack of significance may be also explained by potential error in neonatal anthropometric equations estimating body composition, though there was a trend in directionality towards decreasing birthweight associated with increasing maternal fat mass.
However, the existing evidence to support the biologic link between decreasing maternal skinfolds and fetal size is conflicting. Some studies report lower birthweight with increased triceps skinfold at 14 weeks gestation 9,32 and at delivery 33,34, while others report no difference in birthweight with increased maternal fat mass in the first half of pregnancy 35, 36. These variable findings may be explained by differences in techniques for measuring maternal fat mass or in the timing of skinfold measurements. Skinfolds measured at a single time-point 9,32 do not indicate the change in fat mass while measures of total pregnancy change 35, 36 will underestimate the associations seen with decreasing fat at the end of pregnancy.
Our findings should be considered within the context of limitations. The accuracy of skinfold measures may be affected by skin compressibility and maternal characteristics. To limit this type of measurement error in the NICHD Fetal Growth Study, study personnel underwent training and followed a standardized protocol. Neonatal body compositions were not measured, but instead were calculated using validated equations 19. Applying these equations to a study with different population characteristics may induce error. However, recent evidence on the validity of anthropometric equations suggests low precision and accuracy of equations at birth, other than the one used in this study, 19 due to rapid infant growth and individual variability37. Still, our findings should be interpreted with caution and replicated using more accurate body composition equipment. Due to the observational nature of the study, we cannot make causal assumptions about the association between the mobilization of fat stores in late gestation and fetal growth.
This study was strengthened by the longitudinal design. Repeated skinfold measures enhanced the prediction of maternal anthropometric trajectories in a contemporary, diverse cohort. The multi-stage analytic approach enabled us to assess specific time-periods of change in relation to fetal development. An additional strength was the neonatal skinfold measures at birth to assess the composition of birthweight.
In conclusion, our findings suggest that the maternal components of GWG may provide additional insight about fetal growth and composition at birth beyond that supplied by GWG alone. However, future studies should aim to validate these findings using more accurate measures of body composition to determine if changes in maternal anthropometric measures would provide a more sensitive and specific predictor of fetal growth composition.
Supplementary Material
Acknowledgments
Financial Support: This project was supported by the intramural program at Eunice Kennedy Shriver National Institute of Child Health and Human Development and included American Recovery and Reinvestment Act funding via contract numbers HHSN275200800013C, HHSN275200800002I, HHSN27500006, HHSN275200800003IC, HHSN275200800014C, HHSN275200800012C, HHSN275200800028C, and HHSN275201000009C.
Footnotes
Authorship: The authors’ contributions were as follows: All authors designed the study. SJP wrote the manuscript; SJP, AMOV, PSA analyzed the data; WG, KLG, PSA, DW, JG, MH, RN were responsible for the data collection; all authors read and approved the final manuscript; and SJP and KLG had primary responsibility for the final content.
Ethics standard disclosure: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the local institutional review board. Written informed consent was obtained from all subjects/patients.
Conflicts of interest: The authors have declared that no conflicts of interest exist.
References
- 1.Rasmussen K, Yaktine A. Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: Institute of Medicine and National Research Council of the National Academies; Number of pages. [PubMed] [Google Scholar]
- 2.Nohr EA, Vaeth M, Baker JL, et al. Pregnancy outcomes related to gestational weight gain in women defined by their body mass index, parity, height, and smoking status. The American journal of clinical nutrition 2009;90:1288–94. [DOI] [PubMed] [Google Scholar]
- 3.Pugh SJ, Albert PS, Kim S, et al. Patterns of gestational weight gain and birthweight outcomes in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies-Singletons: a prospective study. Am J Obstet Gynecol 2017;217:346 e1–46 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludwig DS, Currie J. The association between pregnancy weight gain and birthweight: a within- family comparison. Lancet 2010;376:984–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Catalano PM, Mele L, Landon MB, et al. Inadequate weight gain in overweight and obese pregnant women: what is the effect on fetal growth? Am J Obstet Gynecol 2014;211:137 e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.SEWELL MF, Huston-Presley L, Super DM, et al. Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. Am J Obstet Gynecol 2006;195:1100–3. [DOI] [PubMed] [Google Scholar]
- 7.Catalano PM, Farrell K, Thomas A, et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. The American journal of clinical nutrition 2009;90:1303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewey KG, Begum K. Long-term consequences of stunting in early life. Matern Child Nutr 2011;7 Suppl 3:5–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villar J, Cogswell M, Kestler E, et al. Effect of fat and fat-free mass deposition during pregnancy on birth weight. Am J Obstet Gynecol 1992;167:1344–52. [DOI] [PubMed] [Google Scholar]
- 10.Mardones-Santander F, Salazar G, Rosso P, et al. Maternal body composition near term and birth weight. Obstet Gynecol 1998;91:873–7. [DOI] [PubMed] [Google Scholar]
- 11.Hediger ML, SCHOLL TO, SCHALL JI, et al. Changes in maternal upper arm fat stores are predictors of variation in infant birth weight. J Nutr 1994;124:24–30. [DOI] [PubMed] [Google Scholar]
- 12.Crozier SR, Inskip HM, Godfrey KM, et al. Weight gain in pregnancy and childhood body composition: findings from the Southampton Women’s Survey. The American journal of clinical nutrition 2010;91:1745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catalano PM, Tyzbir ED, Wolfe RR, et al. Carbohydrate metabolism during pregnancy in control subjects and women with gestational diabetes. Am J Physiol 1993;264:E60–7. [DOI] [PubMed] [Google Scholar]
- 14.Butte NF. Carbohydrate and lipid metabolism in pregnancy: normal compared with gestational diabetes mellitus. The American journal of clinical nutrition 2000;71:1256S–61S. [DOI] [PubMed] [Google Scholar]
- 15.Pitkin RM. Nutritional support in obstetrics and gynecology. Clinical obstetrics and gynecology 1976;19:489–513. [DOI] [PubMed] [Google Scholar]
- 16.Buck Louis GM, Grewal J, Albert PS, et al. Racial/ethnic standards for fetal growth: the NICHD Fetal Growth Studies. Am J Obstet Gynecol 2015;213:449 e1–49 e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grewal J, Grantz KL, ZHANG C, et al. Cohort Profile: NICHD Fetal Growth Studies-Singletons and Twins. International Journal of Epidemiology 2017:dyx161-dyx61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hadlock FP, Harrist RB, Carpenter RJ, et al. Sonographic estimation of fetal weight. The value of femur length in addition to head and abdomen measurements. Radiology 1984;150:535–40. [DOI] [PubMed] [Google Scholar]
- 19.Catalano PM, Thomas AJ, Avallone DA, et al. Anthropometric estimation of neonatal body composition. Am J Obstet Gynecol 1995;173:1176–81. [DOI] [PubMed] [Google Scholar]
- 20.Johnson TS, Engstrom JL, Gelhar DK. Intra- and interexaminer reliability of anthropometric measurements of term infants. J Pediatr Gastroenterol Nutr 1997;24:497–505. [DOI] [PubMed] [Google Scholar]
- 21.Ulijaszek SJ , Kerr DA. Anthropometric measurement error and the assessment of nutritional status. Br J Nutr 1999;82:165–77. [DOI] [PubMed] [Google Scholar]
- 22.SAS Institute . The SAS system for Windows. Release 9.4. Cary, NC: SAS Institute Inc., 2013. [Google Scholar]
- 23.StataCorp . Stata Statistical Software: Release 13. College Station, TX: StataCorp LP, 2013. [Google Scholar]
- 24.Taggart NR, Holliday RM, Billewicz WZ, Hytten FE, Thomson AM. Changes in skinfolds during pregnancy. Br J Nutr 1967;21:439–51. [DOI] [PubMed] [Google Scholar]
- 25.Ash S , Fisher CC , Truswell AS, et al. Maternal weight gain, smoking and other factors in pregnancy as predictors of infant birth-weight in Sydney women. Aust N Z J Obstet Gynaecol 1989;29:212–9. [DOI] [PubMed] [Google Scholar]
- 26.Maple-Brown LJ , Roman NM , Thomas A, et al. Perinatal factors relating to changes in maternal body fat in late gestation. J Perinatol 2013;33:934–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruchat SM , Allard C , Doyon M, et al. Timing of Excessive Weight Gain During Pregnancy Modulates Newborn Anthropometry. J Obstet Gynaecol Can 2016;38:108–17. [DOI] [PubMed] [Google Scholar]
- 28.Starling AP , Brinton JT , Glueck DH, et al. Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study. The American journal of clinical nutrition 2015;101:302–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davenport MH , Ruchat SM , Giroux I, et al. Timing of excessive pregnancy-related weight gain and offspring adiposity at birth. Obstet Gynecol 2013;122:255–61. [DOI] [PubMed] [Google Scholar]
- 30.King V , Parker M , Howard KP. Pegylation of magnetically oriented lipid bilayers. J Magn Reson 2000;142:177–82. [DOI] [PubMed] [Google Scholar]
- 31.Kent E , O’Dwyer V , Fattah C, et al. Correlation between birth weight and maternal body composition. Obstet Gynecol 2013;121:46–50. [DOI] [PubMed] [Google Scholar]
- 32.Lederman SA , Paxton A , Heymsfield SB, et al. Maternal body fat and water during pregnancy: do they raise infant birth weight? Am J Obstet Gynecol 1999;180:235–40. [DOI] [PubMed] [Google Scholar]
- 33.Briend A Do maternal energy reserves limit fetal growth? Lancet 1985;1:38–40. [DOI] [PubMed] [Google Scholar]
- 34.Toro-Ramos T , Sichieri R , Hoffman DJ. Maternal fat mass at mid-pregnancy and birth weight in Brazilian women. Ann Hum Biol 2016;43:212–8. [DOI] [PubMed] [Google Scholar]
- 35.Forsum E , Sadurskis A , Wager J. Resting metabolic rate and body composition of healthy Swedish women during pregnancy. The American journal of clinical nutrition 1988;47:942–7. [DOI] [PubMed] [Google Scholar]
- 36.Thame M , Trotman H , Osmond C, et al. Body composition in pregnancies of adolescents and mature women and the relationship to birth anthropometry. European journal of clinical nutrition 2007;61:47–53. [DOI] [PubMed] [Google Scholar]
- 37.Cauble JS , Dewi M , Hull HR. Validity of anthropometric equations to estimate infant fat mass at birth and in early infancy. BMC Pediatr 2017;17:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


