Abstract
Purpose:
The goal of this trial was to determine whether low-load blood flow restricted (BFR) exercise of appendicular muscles induces a cross-transfer of effect to the trunk extensor (TE) muscles, such that low-load TE exercise would enhance TE size and function to a greater extent than standard low-load exercise in people with recurrent low back pain (LBP). We also investigated the direct effects of BFR exercise in the appendicular muscles.
Methods:
32 adults with recurrent, non-specific LBP were randomized into two groups: Appendicular BFR Exercise (BFR Exercise) or Control Exercise (CON Exercise). All participants trained (2x/week) for 10-weeks, with a 12-week follow-up. Participants performed three sets of leg extension (LE), plantar flexion (PF), and elbow flexion (EF) exercises followed by low-load TE exercise without BFR. Outcome measures included MRI-derived muscle size (quadriceps and TE), strength (LE, PF, EF, and TE), and endurance (LE and TE).
Results:
There was no evidence for a cross-transfer of effect to the trunk extensors. There was also no statistically significant enhancement of limb skeletal muscle size or function of BFR relative to CON Exercise at any time point; though, moderate effect sizes for BFR exercise were observed for enhanced muscle size and strength in the leg extensors.
Conclusions:
Low-load BFR exercise of the appendicular muscles did not result in a cross-transfer of effect to the TE musculature. There was also no significant benefit of low-load BFR exercise on the appendicular muscle size and function, suggesting no benefit from low-load BFR exercise in adults with recurrent, non-specific LBP.
Keywords: Kaatsu, trunk extensor, muscle strength, muscle mass
INTRODUCTION
More than twenty-five years ago Sundberg and colleagues suggested that performing exercise under conditions of modest blood flow restriction (BFR; referred to in their seminal paper as “ischemic training”) resulted in enhanced skeletal muscle adaptations compared to standard exercise (1). Over the past several decades there has been growing interest in the potential for low-load BFR Exercise, also referred to as Kaatsu exercise, to enhance skeletal muscle adaptations to exercise (e.g., enhanced muscle mass, strength, endurance, etc.). Indeed, a number of studies have noted that low-load BFR exercise can serve as a potent stimulus for increases in muscle size, strength and endurance, relative to exercise without blood flow restriction (for reviews and meta-analyses see (2–7)). As such, BFR exercise has gained popularity as a novel exercise modality in both performance and rehabilitation settings.
In addition to the reported effects of BFR exercise listed above, there is evidence that BFR exercise might promote hypertrophy in muscles not exercising under “traditional” BFR conditions via systemic hypertrophy-promoting effects (8–11). For instance, Madarame and colleagues reported an increase in muscle size (12%) and strength (9.8%) of the elbow flexors after 10 weeks of low-load resistance exercise coupled with BFR of the legs, but not arms (8). This purported phenomenon, commonly referred to as a “cross-transfer of effect,” has been reported in several studies (8–11). The putative mechanism for this effect is increased systemic endocrine growth factors following BFR exercise (12–16). For instance, prior work suggests that resistance training with BFR amplifies normal exercise-induced high-energy phosphate depletion and muscle pH reduction, and maintains this altered metabolic milieu (6). A strong stimulation of the metaboreflex by these conditions could account for findings from numerous studies reporting that single bouts of BFR exercise increase serum growth hormone and IGF-1 levels (12–16) to levels comparable to, or greater than, those observed during resistance training at much higher intensities (17). However, this underlying scientific premise has also been called into question by data suggesting no systemic hormonal influence on hypertrophy or strength gains (18, 19). Accordingly, the overarching goal of this work was to rigorously determine whether a “cross transfer of effect” occurs in association with BFR resistance exercise. We chose to investigate the potential phenomenon within the context of the trunk extension musculature in a non-specific low back pain (LBP) population. The potential to apply the cross-transfer of BFR to the trunk muscles could have important therapeutic benefit in non-specific LBP.
Although the pathogenesis of non-specific LBP remains unknown, weakness and fatigability of the trunk extensor muscles are predictive of first time episodes of LBP, as well as recurrence (20–22). Dramatic atrophy of the lumbar multifidus muscle occurs following experimental disc and nerve root injuries (23), and patients with both recurrent and chronic non-specific LBP exhibit wasting of the trunk extensors (24–29). Collectively, these findings indicate that patients with non-specific LBP, particularly recurrent, non-specific LBP, exhibit deconditioned trunk extensor muscles (30). The vast majority of trunk extensor exercises for the rehabilitation of non-specific LBP are performed at low loads (31), mostly out of concern over the high mechanical and compressive loading on the spine (31, 32). There is a need to develop therapeutic exercise paradigms to induce adaptation in the trunk extensor musculature without high-mechanical and compressive loading on the spine. Thus, if BFR exercise of limb muscles were to induce a cross-transfer effect to the trunk extensors, the clinical significance and impact could be high. The, present study was to designed as a preliminary trial to determine whether low-load BFR exercise of appendicular muscles induces a cross-transfer of effect to the trunk extensor (TE) muscles, such that low-load TE exercise would enhance TE size and function to a greater extent than standard low-load exercise in people with recurrent, non-specific LBP. Accordingly, randomized assignment and blinding of study personnel to treatment group assignment were applied throughout the study. In addition, individuals in both exercise groups performed the appendicular exercises to volitional failure (to control for potential bias in the study design- see discussion for further comment). In doing so, we were also able to investigate the direct effects of BFR exercise in the appendicular muscles, which is impactful when one considers that many studies on BFR exercise have been criticized for being lower-quality studies (3).
METHODS
Study Design
This study was a single-blinded, single-site, randomized controlled trial, using a two-by-three (Group x Time) repeated measures factorial design. The Ohio University Institutional Review Board approved this study, and written informed consent was obtained from each individual prior to participating. This study protocol has previously been published in detail (33), and is registered on ClincialTrials.gov (NCT02308189). Subject recruitment began in December 2014, and the primary completion date of the study was November 2016. Participants were randomized, in a 1:1 ratio, into one of two groups (see CONSORT Diagram, Supplementary Digital Content 1, The Consolidated Standards of Reporting Trials (CONSORT) Flow Diagram). Group 1 received 10 weeks of resistance exercise training with BFR (BFR Exercise Group), while Group 2 received 10 weeks of resistance exercise training without BFR (CON Exercise Group). Randomization was stratified by sex, using a permuted-block design, for the purpose of maintaining balance across treatment groups. Study recruitment and eligibility testing, as well as randomization of subjects were performed by a project manager of the Ohio University Clinical and Translational Research Unit. Careful investigator bias control measures included: 1) study personnel conducting the outcome assessments (including image analysis) being blinded to group assignment throughout the length of the study, and 2) the statistician (MN) and principal investigator (BC) remaining blinded to group assignment throughout the study (they were unblinded after the data and statistical analyses were completed).
The chronological sequence of this study consisted of baseline testing, a 10-week exercise training intervention, and a 12-week follow-up period. Specifically, outcome measures were assessed at baseline, immediately following the completion of the exercise intervention (primary endpoint), and at week 12 of the follow-up period (secondary endpoint). Subjects were also asked to maintain their typical daily lifestyle (e.g. activity, diet, sleep patterns, etc.) throughout the course of the study to minimize confounding variability. Additionally, subjects were instructed to report for all outcome measure testing sessions in a well-hydrated state.
Subjects
32 young adult subjects with recurrent, non-specific LBP were randomly assigned to an Exercise Control (ExCon; n=16) or BFR Exercise (ExBFR; n=14) Group (see CONSORT Diagram, Supplementary Digital Content 1, The Consolidated Standards of Reporting Trials (CONSORT) Flow Diagram). Table 1 describes the inclusion and exclusion criteria in detail. To be eligible for participation, individuals had to be between 18–50 years with recurrent, non-specific LBP. We operationally defined recurrent, non-specific LBP as individuals who answer “yes” to the following question: Have you had ≥2 episodes of LBP in the past 12 months with at least one episode causing a restriction of work or leisure time activity? A further criterion was poor TE muscle endurance (<176 secs on a modified Sorenson test) an isometric trunk extension endurance test. In a prospective study a mean time of 176 s was noted in those who went on to develop LBP as opposed to a mean time of 198 for those who did not (20). Individuals who had participated in progressive resistance exercise, within the previous 24 weeks (prior to screening), were also excluded. The criteria were designed to recruit a population with recurrent, non-specific LBP, but to exclude potential participants who are currently experiencing a level of LBP above where we had concerns about the pain interfering with a participant’s ability to appropriately perform the exercise prescription (e.g., exclusion criteria resulting in the exclusion of potential participants whose current pain level is greater than 4 on a 0–10 scale).
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria |
|---|
| 1. Between 18 and 50 years of age. |
| 2. Answer “yes” to the following questions: |
| ▪ Have you had two or more episodes of low back pain (LBP) in the past 12 months with at least one of the episodes causing a restriction of work or leisure time activity? |
| 3. Body mass index between 17 and 37 kg/m2. |
| 4. With no condition that could limit participation in supervised resistance training exercise based on the Physical Activity Readiness Questionnaire (PAR-Q). |
| 5. Sedentary lifestyle as measured by a classification of “low” or “moderate” levels of physical activity based on scoring criteria of the International Physical Activity Questionnaire (IPAQ). |
| 6. Exhibit low trunk extensor endurance defined as a time to task failure during the modified-Sorensen test of <176 seconds. |
| 7. Willing to maintain current diet and adhere to exercise programs described for the study and to not start any new dieting/weight management programs. |
| 8. Willing and able to return for all clinic visits and complete all study-related procedures. |
| 9. Able to read, understand, and complete study-related questionnaires. |
| 10. Able to read and understand, and willing to sign the informed consent form (ICF). |
| Exclusion criteria |
| 1. Participation in progressive resistance exercise within the previous 24 weeks prior to screening. |
| 2. Participation in any clinical trial within 24 weeks prior to screening. |
| 3. Hospitalization (medical confinement for 24 hours), or immobilization, or major surgical procedure requiring general anesthesia within 24 weeks prior to screening, or any planned surgical procedures during the study period. |
| 4. Limb amputation (except for toes) and/or any fracture within 24 weeks. |
| 5. Osteoarthritis, rheumatologic diseases or orthopedic disorders, which will not allow completion of the motions required for the resistance exercise. |
| 6. Conditions (such as myasthenia gravis, myositis, muscular dystrophy or myopathy, including drug-induced myopathy) leading to muscle loss, muscle weakness, muscle cramps or myalgia. |
| 7. Chronic or relapsing/remitting gastrointestinal disorders such as inflammatory bowel diseases, irritable bowel syndrome or gastrointestinal infections within 28 days of screening. |
| 8. Acute viral or bacterial upper or lower respiratory infection at screening |
| 9. Moderate or severe chronic obstructive pulmonary disease. |
| 10. Back pain greater than 4 (on a 10 point numeric pain rating scale) at screening. |
| 11. Leg length discrepancy > 3 cm. |
| 12. Current or recent (i.e., within 12 weeks) of narcotics or muscle relaxants. |
| 13. Currently pregnant (confirmed via a urine test) or planning to become pregnant within the next year at screening. |
| 14. Report unexplained weight loss over the past 30 days (> 10 pounds). |
| 15. Report having pending litigation related to low back pain or currently receiving disability for low back pain. |
| 16. Report having received treatment for low back pain from a health care practitioner in the past 6 weeks. |
| 17. History of spine surgery or hip arthroplasty. |
| 18. Cancer requiring treatment currently or in the past 3 years (except primary non-melanoma skin cancer or in situ cervical cancer). |
| 19. Moderate or severe asthma with current or recurring symptoms within the last 1-year. |
| 20. Known history of human immunodeficiency virus (HIV) antibody and/or positive hepatitis B surface antigen (HBsAg) and/or positive hepatitis C antibody (HCV) at screening. |
| 21. Neurological conditions resulting in impaired muscle function or mobility (e.g., stroke with residual paresis, paralysis, multiple sclerosis, or Parkinson Disease). |
| 22. Psychiatric conditions that warrant acute or chronic therapeutic intervention (e.g., major depressive disorder, bipolar disorder, panic disorder, schizophrenia) that in the investigators opinion may interfere with the conduct of study procedures |
| 23. History of cardiac conditions such as heart failure (NYHA class II-IV), angina (including unstable angina), myocardial infarction, cardiomyopathy, any cardiac arrhythmia (except stable sinus dysrhythmia or atrial fibrillation) or valvular heart disease (except asymptomatic mitral valve prolapse). |
| 24. History of peripheral vascular disease. |
| 25. Subjects with the following abnormal ECG findings at screening were excluded: Electrocardiogram findings indicative of left ventricular hypertrophy (LVH) (based on Cornell voltage criteria): A) For men: S in V3 plus R in a VL >2.8 mV (28 mm); For women: S in V3 plus R in a VL >2.0 mV (20 mm); or B) Electrocardiogram finding of QT prolongation defined as QTcF > 470 ms. |
| 26. Diabetics using insulin. |
| 27. Abnormal or uncontrolled blood pressure at the screening visit defined as diastolic BP >100 and/or systolic BP >160 mm Hg; if taking anti-hypertensive medication, have to be on stable doses of medication for more than 3 months. |
| 28. Current or recent history (within 1 year of screen) of heavy alcohol consumption (males 21 drinks/week, 4 drinks/day; females 14 drinks/week, 3 drinks/day) or drug abuse (as per the opinion of the principal investigator). |
| 29. Current or previous use of any drugs known to influence muscle mass or performance within 24 weeks. These may include, but are not limited to, anabolic steroids, IGF-1, growth hormone (GH), replacement androgen therapy, anti-androgen therapy. |
| 30. Use of systemic glucocorticoids within 12 weeks prior to screening. |
| 31. Having body dimensions that exceed the MRI or exercise equipment limits. |
| 32. Unable to undergo MRI (e. g. body containing any metallic medical devices or equipment, including heart pacemakers, metal prostheses, implants or surgical clips, any prior injury from shrapnel or grinding metal, exposure to metallic dusts, metallic shavings or having tattoos containing metallic dyes). |
| 33. Unable to reliably undergo exercise or strength tests described for this study (as per the opinion of the principal investigator). |
| Permitted Medications: |
| -- Use of the following concomitant medications was permitted during study participation if subjects had been on stable dose of the medication for 3 months prior to the study: Thyroid replacement medication; Estrogens and progestins for women; Anti-hypertensives; Vitamins and calcium supplements; Statins at dose levels that are well tolerated and do not cause myalgia; Oral anti-hyperglycemic drugs; Bisphosphonates |
| -- Use of the following concomitant medications as needed was permitted during study participation: Over the counter antihistamines and decongestants; Acetaminophen; Non-steroidal anti-inflammatory drugs (NSAIDS); Heat or Ice; Proton pump inhibitors; Antacids; Oral antibiotics (for fewer than 11 days); Laxatives; Protein supplements were allowed if they had been part of the subjects routine diet/nutritional intake prior to the study. |
| Prohibited Medications and Treatments: |
| -- Onset of treatment with the following concomitant medications is prohibited during study: Anti-obesity drugs, nutraceuticals, and dietary supplements that may affect body mass and body composition; Long acting-agonists; Any drug or supplement known to influence muscle mass or performance including but not limited to anabolic steroids, IGF-1, GH, replacement androgen therapy, anti-androgen therapy; Narcotics; Muscle relaxants; Any treatment specific for low back pain delivered by a health care practitioner (e.g., physician, physical therapist, chiropractor, massage therapist, or acupuncturist). |
Outcome Measures
Study outcomes were assessed at the Ohio Musculoskeletal and Neurologic Institute at Ohio University (Athens, Ohio, USA). Outcome measures were: 1) quadriceps femoris and lumbar erector spinae muscle cross-sectional area (CSA) measurements derived via magnetic resonance imaging (MRI), 2) voluntary isometric muscle strength of the leg extensors, elbow flexors, plantar flexors, and trunk extensors, 3) leg extensor and trunk extensor isometric muscle endurance, 4) low back pain, and 5) treatment acceptability. Methodological details are presented below.
Muscle CSA:
MRI’s were obtained using a 0.25-Tesla Musculoskeletal MRI system (Esaote G-Scan Brio, Genoa, Italy). We acquired contiguous transverse T-1 weighted spin echo image slices in the trunk region between L2 and L5 and then, in a subsequent scan, the mid-thigh, with a slice thickness of 10 mm for both scans. To ensure the consistency within/among subjects, the isocenter was positioned at the midpoint of the L3/L4 intervertebral disc and 1/3 of the distance between the knee and the greater trochanter, respectively. Prior to all scans, subjects rested supine for at least 15 minutes to minimize the effects of fluid shifts on volumetric calculations. The post-testing MRI scan was obtained 3 days after the final training session to minimize the effects of exercise-induced fluid shifts. Scanned images were transferred to a computer for calculation of muscle anatomical CSA for the erector spinae and quadriceps femoris muscle groups (an average of three slices at the isocenter from both sides) using the MIPAV image analysis software. Extreme care was taken to insure that the slices chosen for analysis were of the same anatomical location at all time points (accomplished by matching the slices for anatomical features [i.e., fascial characteristics]). Intermuscular fat was subtracted from the calculations based on pixel intensity as we have previously described (34, 35).
Muscle Strength:
Voluntary muscle strength was quantified for the leg extensors, elbow flexors, plantar flexors, and the trunk extensors. For the leg extensors participants were seated in a MedX leg extension dynamometer (Ocala, FL), which allowed for strict control of hip and knee joint angles. The backrest was adjusted so subjects sat with a hip joint angle of 100°from flexion, and a seat belt was secured to prevent any movement of the hip joint. The limbs were attached to the force transducer (model U1T, HBM Inc., Marlborough, MA, USA), and the knee joint angle was set at 60 degrees from extension. For the elbow flexors subjects wore an arm isolator (Rogue Arm Blaster, Rogue Fitness, Columbus, OH, USA) and stood with their feet shoulder width apart with the arms attached to a force transducer (TSD121C, BioPac Systems) with the elbows positioned at 90 degrees. For the plantar flexors, subjects were seated in a custom-modified dynamometer with the legs positioned in the dynamometer with the hip, knee, and ankle joint angles all secured at 90 degrees, and force was measured by a force transducer (TSD121C, BioPac Systems). For the trunk extensors, subjects were seated in a lumbar extension dynamometer (MedX; Ocala, FL, USA) with the upper body positioned in the upright, neutral position, and force was measured via a force transducer (model U1T, HBM Inc., Marlborough, MA, USA). Femur and lap restraints were applied to stabilize the pelvis. During the strength assessments the exerted force was displayed on a computer monitor displayed in front of the subject. All force signals were amplified and recorded at 500 Hz using a 16-bit data acquisition card (MP150, BioPac Systems Inc., Santa Barbara, CA, USA). A minimum of thee trials for each task were performed, with additional trials provided as needed if subjects continually exert more force with each trial or if the highest two trials were not within 5%. Each contraction lasted approximately 5 seconds with at least a 60-second rest period. Muscle strength was defined as the highest value recorded in any trial.
Muscle Endurance:
The time to task failure of a sustained, submaximal isometric contraction of the leg extensors and the trunk extensors were determined (mechanical set-up the same as described for the strength assessment with the exception that the leg extension task was performed unilaterally with the non-dominant limb). During these tests, participants performed the tasks at 20% of their baseline muscle strength by matching a target line on a computer monitor until volitional task failure similar to our previous descriptions (36, 37). During the tasks, a target line was displayed on a computer monitor placed in front of the participant and the time to task failure will be quantified. Task failure was determined to occur when the feedback line drifted below the target force line by 5% for longer than 3 seconds despite verbal encouragement being provided to subjects to restore the position of the force line if they drifted away from the target force.
Treatment Acceptability:
Treatment acceptability was determined by administering the Treatment Evaluation Inventory Short Form survey at the end of every fourth exercise session (38).
Exercise Interventions
Supervised exercise training sessions were conducted twice per week for 10 weeks. For both training groups the exercise intensity was set at 25% of their maximal voluntary isometric strength. Our rationale for choosing an intensity of 25% is that it is similar to many studies on low-load exercise with blood flow restriction, including our own, that have shown positive muscle adaptations with intensity levels in the range of 25–30% of maximal strength (8, 11, 39, 40). To ensure that exercise intensity values were adjusted accordingly to strength progression, re-assessment of maximal strength was performed during the 5th week of the training schedule. Participants in the BFR Exercise Group performed three sets of leg extension (MedX leg extension dynamometer), plantar flexion (seated calf raises), and elbow flexion (arm curls on cable machine) exercises to task failure while BFR was applied to the proximal limbs by a KAASTU Master device (KAATSU Training Japan Co., Ltd., Tokyo, Japan). Subjects were allowed 30–60 seconds of rest between sets. While performing leg extension and plantar flexion exercises, the pressure cuff was placed on the upper thigh, just below the gluteal fold. While performing elbow flexion exercises, the pressure cuff was placed on the upper arm, just below the shoulder joint. The cuff pressure for each limb was determined on each day of exercise for an individual. The initial cuff pressure was applied in accordance with the KAATSU protocol (41), which involved setting the baseline pressure at ~ 30–40 mmHg and then applying additional pressure in increments of 20 mmHG. This inflation-deflation sequence continued until the circulation in the limbs was impeded, but not occluded. Specifically, the cuff pressure for the leg and arm was set when the capillary refill time of the leg, just above the knee, or the palms of the hands was between two and three seconds (41). The pressure cuffs remained inflated until the completion of all three sets of exercise, including the rest periods. The average cuff pressures for the first exercise session were 142.9±33.3 and 160.7±34.2 mmHg for the arms and legs, respectively. The inflation pressure was increased progressively throughout the 10-week training period based on subject tolerance and capillary refill time. The average cuff pressures for the last exercise session were 205.7±48.3 and 240.0±49.8 mmHg for the arms and legs, respectively. After completing the BFR exercises, participants in the BFR Exercise Group performed three sets of 15 repetitions of trunk extensor exercises at 25% of maximal voluntary isometric strength while seated in a MedX TE dynamometer. The CON Exercise Group performed an identical exercise protocol as the BFR Exercise Group, except that BFR was not applied to the appendicular limbs. An overview of the two exercise groups is illustrated in Table 2. We chose the specific exercises based on their being clinically viable and adaptable to BFR exercise.
Table 2.
Schematic overview of the exercise intervention groups.
| Group | Blood Flow Restriction |
Frequency | Exercise regimen |
|---|---|---|---|
| Control Exercise Group | No | Twice weekly | • 3 sets of leg extension, calf raises, and arm curls at 25% of individuals’ isometric MVC to failure (30-60 seconds rest between sets). • 3 sets of trunk extension at 25% for 15 repetitions (30-60 seconds rest between sets). • Up to 3-minutes rest between each exercise station. |
| BFR Exercise Group: | • Pressure cuffs applied to the upper leg during legs exercises and upper arms during arm curls. • Pressure is maintained throughout the 3 sets for the respective exercises. |
Twice weekly | • 3 sets of leg extension, calf raises, and arm curls at 25% of individuals’ isometric MVC with BFR to failure (30-60 seconds rest between sets) • 3 sets of trunk extension at 25% of individuals’ isometric MVC for 15 repetitions (30-60 seconds rest between sets) with BFR on upper arm. • Up to 3-minutes rest between each exercise station. |
Abbreviations: BFR, blood flow restriction; MVC, maximum voluntary contraction.
Statistical Analyses
Sample size calculations for this study have been previously described (33). For the three skeletal muscle-related outcomes (i.e., muscular size, strength, and endurance), we computed a percent change score between values at pre-training and immediately after the 10-week intervention period, and between values at pre-training and the post-intervention 12-week follow-up period. Afterwards, we tested group percent differences using linear models, with covariates included to increase the power to detect a significant treatment effect, while also controlling for the potential confounding effects of the covariates (sex, standardized age [using a z-score transformation], standardized pre-treatment value). In this analysis the group difference (which we refer to in the results as “difference”) corresponds to the test of the interaction between time and group. One participant (control group) had extreme MRI values (standardized scores greater than three standard deviations [SD] away from the mean) and was excluded from the muscle size analyses. We subsequently identified this to be due to movement artifact in the MRI).
Next, we performed an Intention-to-Treat (ITT) analyses for all randomized participants who had baseline assessments and estimated parameters based on maximum likelihood estimation. We also performed an exploratory Per-Protocol Analyses (PPA), where we excluded participants who had: 1) failed to attend 75% of their exercise training sessions, 2) received prohibited concomitant interventions, or 3) developed an exclusionary medical condition while on study protocol. All data was expressed as mean ± SD unless otherwise noted (error bars in figures represent 95%CI). We performed all statistical tests at the 5% significance level (2-tailed), and because this was a proof-of-concept trial (i.e., exploratory in nature) we did not adjust the α level for multiple comparisons. To further aid in the interpretation of data we also report effect sizes (eta-squared [η2]) at the primary endpoint.
We also ran an analysis of covariance with group and time entered into the model with baseline values as covariates. The findings from this analysis were congruent with the percent change analysis described above. We chose to present the percent change results for simplicity and reader clarity. Unpaired T-tests were used to examine group differences at baseline.
Adverse Events
At each study-related visit we carefully documented any changes in health status. Adverse events (AEs) were documented and assessed for severity (grade) and attribution by the project’s medical director (TL) according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE) guidelines (42). In brief, the CTCAE displays Grades 1 through 5 with unique clinical descriptions of severity for each AE based on this general guideline:
Grade 1 Mild; asymptomatic or mild symptoms; clinical or diagnostic observations only; intervention not indicated.
Grade 2 Moderate; minimal, local or noninvasive intervention indicated; limiting age-appropriate instrumental activity of daily living (ADL).
Grade 3 Severe or medically significant but not immediately life-threatening; hospitalization or prolongation of hospitalization indicated; disabling; limiting self care ADL.
Grade 4 Life-threatening consequences; urgent intervention indicated.
Grade 5 Death related to AE.
The classification of potential relationship to the intervention (i.e., attribution) was as follows:
Definite: Temporal pattern + Known or expected AE response pattern + Confirmed by stopping the intervention + Reappearance of AE on re-challenge.
Probable: Temporal pattern + Known or expected AE response pattern + Confirmed by stopping the intervention + Could not be explained by participant’s clinical state.
Possible: Temporal pattern + Known or expected AE response pattern + Could have been produced by a number of other factors.
Unknown: Relationship for which no evaluation can be made.
Not related: AE for which sufficient information exists to indicate that the cause is unrelated to the study intervention.
RESULTS
A total of 574 individuals were screened for this study, and of those individuals screened, 35 met the eligibility criteria. Three chose not to participate, leaving 32 to be randomized in the study. Fifteen participants were randomized to the BFR Exercise Group (10 females and 5 males) and 17 participants were randomized to the CON Exercise Group (10 females and 7 males). Two participants were withdrawn from the study after the randomization process (n=1 female/group). The first was withdrawn due to the baseline strength testing session exacerbating their LBP (CON Exercise Group). The second was withdrawn during the follow-up period after they reported seeking physical therapy following the completion of the study exercise protocol (BFR Exercise Group). Thus results were analyzed for 14 participants in the BFR Exercise Group and 16 participants in the CON Exercise Group. Baseline characteristics of the subjects are detailed in Table 3 (no significant group differences were observed on any of the characteristics).
Table 3.
Descriptive statistics of the study participants at baseline.
| Group | Age (yrs) |
Height (cm) |
Weight (kg) |
Sorenson Time (secs) |
LBP (0-10) |
ES CSA (cm2) |
TE Strength (N-m) |
TE Endurance (Secs) |
Quadriceps CSA (cm2) |
LE Strength (N-m) |
LE Endurance (secs) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BFR Exercise | 28.4±9.2 | 168.5±8.8 | 75.7±16.7 | 74.3±38.9 | 2.9±0.8 | 19.8±3.7 | 221.2±86.1 | 379.7±334.5 | 51.5±10.2 | 904.1±277.5 | 154.0±62.6 |
| Control Exercise | 29.9±9.9 | 170.1±9.8 | 71.4±14.4 | 90.5±29.8 | 2.5±1.4 | 22.1±4.3 | 238.2±97.9 | 535.4±788.9 | 57.0±12.6 | 939.9±301.0 | 213.2±130.8 |
BFR: Blood flow restricted; LBP: Low back pain; ES: erector spinae; CSA: Cross-sectional area; TE: Trunk extensors; LE: Leg extensors.
Cross-transfer Effect of BFR Limb Exercise on Trunk Extensor Size and Function
Erector Spinae CSA
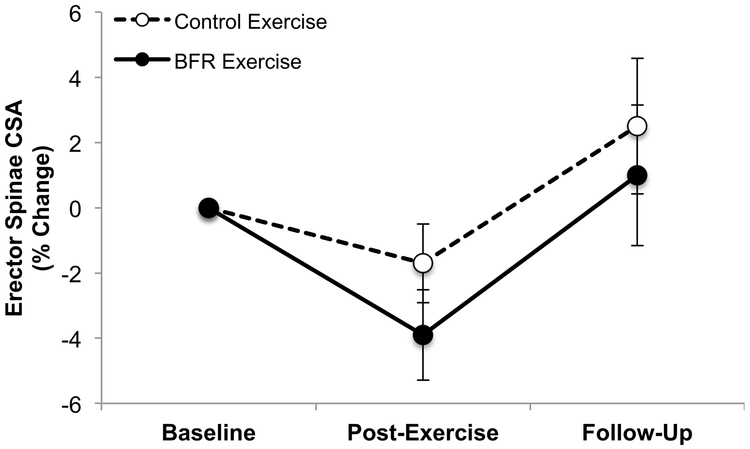
At the primary endpoint, there were no significant differences within or between groups (BFR Exercise Group: −3.9±2.7%, p=0.2; CON Exercise Group: −1.7±2.5%, p=0.5; group difference: p=0.5; η2=0.15) (Figure 1). At the secondary endpoint, there were again no significant differences within or between groups (BFR Exercise Group: 1.0±4.2%, p=0.8; CON Exercise Group: 2.5±4.3%, p=0.5; group difference: p=0.8) (Figure 1). When collapsed across exercise groups, no significant changes in erector spinae CSA muscles were observed at either the primary (−2.6±2.1%, p=0.2) or secondary (1.8±3.4%, p=0.6) endpoints.
Figure 1.
BFR exercise did not result in a significant cross-transfer of effect in erector spinae muscle CSA.
Error bars represents 95% CI.
Trunk Extensor Strength
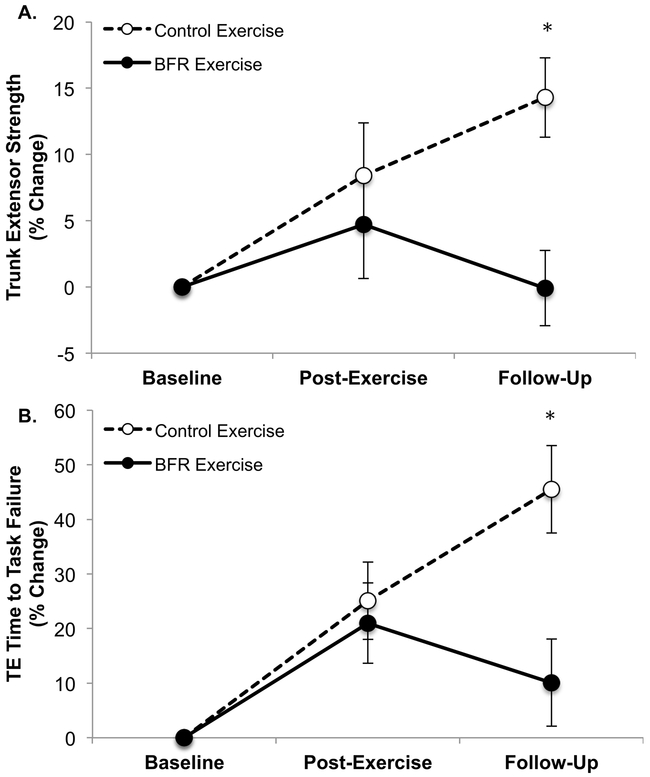
At the primary endpoint, neither the participants in the BFR Exercise Group, nor the CON Exercise Group, exhibited a significant change in strength relative to baseline BFR (Exercise Group: 4.7±7.9%, p=0.6; CON Exercise Group: 8.4±8.2%, p=0.3) (Figure 2A). Furthermore, there were no significant differences found between the groups (group difference: p=0.7; η2=0.05) (Figure 2A). In contrast, at the secondary time point, there was a significant increase in trunk extensor strength compared to baseline for the CON Exercise Group, but not for the BFR Exercise Group (BFR Exercise Group: −0.1±5.5%, p=0.9; CON Exercise Group: 14.3±6.2% p=0.03) (Figure 2A). The between group difference was also found to be significant (p=0.04). When we collapsed the two exercise groups, trunk extensor strength was not affected by exercise at either the primary endpoint (6.4±6.5%, p=0.3) or secondary endpoint (5.8±5.1%, p=0.3).
Figure 2.
BFR exercise did not result in a significant cross-transfer of effect in TE muscle strength (A) or endurance (B) (note that beneficial effects noted in the follow-up period are in the Control Exercise Group).
Error bars represents 95% CI.
Trunk Extensor Endurance
At the primary endpoint, neither the participants in the BFR Exercise Group, nor the CON Exercise Group, exhibited a significant percent change in time to task failure (BFR Exercise Group: 21.0±14.3%, p=0.2; CON Exercise Group: 25.1±14.6%, p=0.2), nor was there a difference between the groups (p=0.8, η2=0.03) (Figure 2B). In contrast, at the secondary endpoint, there was a significant increase in time to task failure for the CON Exercise Group (45.5±17.0%, p=0.01), but not the BFR Exercise Group (10.1±15.5%, p=0.5); however, there were no significant differences found between the groups (p=0.09) (Figure 2B).
Effects of BFR Limb Exercise on Appendicular Muscle Size and Function
Quadriceps Femoris Muscle CSA
We found no significant differences within or between groups at either time point (Figure 3). At the primary endpoint, there were no significant differences found within or between groups (BFR Exercise Group: 2.8±2.3%, p=0.2; CON Exercise Group: 0.6±2.2%, p=0.5; group difference: p=0.4); however, a moderate effect size (η2=0.19) was noted for the interaction term (Figure 3). At the secondary endpoint, there were again no significant differences found within or between groups (BFR Exercise Group: 3.5±2.5%, p=0.3; CON Exercise Group: 2.3±2.7%, p=0.4; group difference: p=0.7, η2=0.05) (figure 3). Due to a lack of a group effect for the MRI measure, we collapsed the two exercise groups to determine if exercise, regardless of whether BFR was administered, affected limb muscle size and function after controlling for the covariates (sex, standardized age, and standardized pre-treatment value). We did not observe a significant effect of exercise on CSA measured at the primary endpoint (1.6±1.8%, p=0.4), or secondary endpoint (2.9±2.2%, p=0.19).
Figure 3.
Blood flow restricted (BFR) exercise did not significantly increase quadriceps femoris muscle cross-sectional area (CSA).
Error bars represents 95% CI.
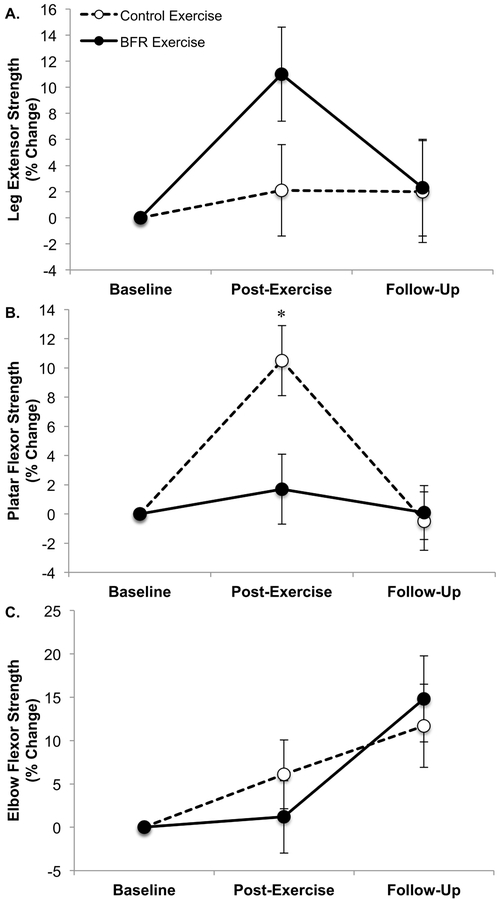
Appendicular Muscle Strength
There were no consistent patterns for strength changes among the three appendicular muscle groups at the primary or secondary endpoints (i.e., there was no systematic change [positive or negative] noted across the various muscle groups) (Figure 4). At the primary and secondary endpoints, leg extensor strength did not significantly increase for either the BFR Exercise Group, or the Exercise Control Group, and there were no significant differences between the groups (Primary Endpoint: BFR Exercise Group: 11.0±7.1%, p=0.1; CON Exercise Group: 2.1±7.3%, p=0.8; group difference: p=0.3; Secondary Endpoint: BFR Exercise Group: 2.3±7.2%, p=0.7; CON Exercise Group: 2.0±8.0%, p=0.80; group difference: p=0.9) (Figure 4A). There was a moderate effect size for strength enhancement in the BFR Exercise Group (η2=0.27) at the primary endpoint. In contrast, plantar flexor strength significantly increased in the CON Exercise Group, but not the BFR Exercise Group at the primary endpoint (Figure 4B), and there was a significant group difference (Primary Endpoint: BFR Exercise Group: 1.7±4.7%, p=0.7; CON Exercise Group: 10.5±5.0%, p=0.05; group difference: p=0.05; η2=0.84). At the secondary endpoint, there was no significant difference found within or between groups (Secondary Endpoint: BFR Exercise Group: 0.1±3.6%, p=0.9; CON Exercise Group: −0.5±4.2%, p=0.9; group difference: p=0.9). Finally, at the primary and secondary endpoint, elbow flexor strength did not significantly increase for either the BFR Exercise Group, or the CON Exercise Group, and there were no significant differences found between the groups (Primary Endpoint: BFR Exercise Group: 1.2±8.1%, p=0.9; CON Exercise Group: 6.1±8.2%, p=0.5; group difference: p=0.6; η2=0.08; Secondary Endpoint: BFR Exercise Group: 14.8±9.6%, p=0.08; CON Exercise Group: 11.7±9.9%, p=0.03; group difference: p=0.8) (Figure 4C). Overall, exercise (when collapsed across exercise groups) did not significantly affect any measure of appendicular muscle strength at the primary endpoint (leg extensor: 6.8±5.8%, p=0.3, η2=0.26; plantar flexor: 5.7±3.9%, p=0.15, η2=0.35; elbow flexor: 3.6±6.4%, p=0.6, η2=0.07) or secondary endpoint (leg extensor: 2.2±6.0%, p=0.7, η2=0.03; plantar flexor: −0.1±3.0%, p=0.9, η2<0.01; elbow flexor: 13.3±7.8%, p=0.1, η2=0.42).
Figure 4.
Effect of blood flow restricted (BFR) exercise on appendicular muscle strength of the leg extensors (A), plantar flexors (B), and elbow flexors (C). Panel D illustrates the effect of BFR exercise on leg extensor (LE) muscle endurance. For plantar flexor strength and leg extensor endurance the control exercise group exhibited a significant increase post-exercise (*plantar flexor p=0.05; leg extensor endurance p=0.04); however, the group difference was only significant for the plantar flexors (plantar flexor group difference p=0.05, η2=0.84; leg extensor endurance group difference (p=0.2; η2=0.39).
Error bars represents 95% CI.
Leg Extensor Endurance
We further examined whether BFR exercise influenced leg extensor muscular endurance at the primary and secondary endpoints. At the primary endpoint, time to task failure significantly increased for the CON Exercise Group, but not for the BFR Exercise Group (CON Exercise Group: 35.2±16.2%, p=0.04; BFR Exercise Group: 9.6±15.8%, p=0.6). However, there were no significant differences found between the groups (p=0.2), although a moderate effect size was observed for an enhancement in the CON Exercise Group (η2=0.39). At the secondary endpoint, there were no significant differences within or between groups (BFR Exercise Group: −2.1±9.5%, p=0.8; CON Exercise Group: 15.0±11.0%, p=0.19; group difference: p=0.2; η2=0.41). When we collapsed knee extensor endurance across groups, the primary endpoint was not significant, although a moderate mean increase was observed (22.1±12.4%, p=0.09), while at the secondary endpoint, we did not observe a similar effect (4.9±7.9%, p=0.6).
Per Protocol Analysis
In addition to the ITT analysis described above, we also performed a per protocol analysis (PPA) where we identified and excluded participants who failed to attend 75% of the exercise training sessions. This resulted in one male participant, from the CON Exercise Group, being excluded. After removing this participant, all analyses were repeated, and found that excluding this participant did not change the significance or interpretation of any of the results described above.
Adverse Events and Treatment Acceptability
There were a total of nine AEs reported in eight subjects. None of the AEs were deemed serious (5 mild and 4 moderate). Seven of the AEs were deemed clearly unrelated to the study protocol. Table 4 summarizes the AE’s. It should be noted that bruising at the site of cuff inflation, as well as general discomfort associated with the inflated pressure cuffs, were deemed expected and thus not documented as an AE.
Table 4.
Adverse events.
| Treatment Group |
AE | Severity | Attribution | Action Taken |
SAE | Comments |
|---|---|---|---|---|---|---|
| Experimental | Low Back Pain | Moderate | Likely Related | Discontinued Permanently | No | LBP exacerbated after 2 exercise sessions completed. Study physician deemed it DOMS. Subject chose to withdraw. |
| Not randomized | Ankle Sprain/strain | Mild | Clearly Unrelated | Discontinued Permanently | No | Subject was screen failed due to ankle injury from a fall prior to randomization. |
| Experimental | Leg bruising and edema | Mild | Clearly Unrelated | Reduced Dose | No | Participant injured leg due to a floor collapse (i.e., subject stepped through a floor). This trauma resulted in mild bruising and edema in one leg. Study physician recommended doing only unilateral exercises with the legs for two exercise sessions. |
| Experimental | Right radius fracture | Moderate | Clearly Unrelated | None | No | Participant fractured elbow during the follow-up period. Study physician recommended not assessing elbow flexion strength at the follow-up testing session (all other outcomes were assessed). |
| Experimental | Sinus infection | Mild | Clearly Unrelated | None | No | Resolved. No exercise sessions missed. |
| Experimental | Cervical neck pain | Moderate | Clearly Unrelated | Reduced Dose | No | Participant reported complaint of cervical neck pain prior to an exercise session week 8 of the intervention. Was not temporally related to a study intervention. The participant missed 1 exercise session prior to pain resolving. |
| Experimental | Diarrhea | Mild | Clearly Unrelated | Reduced Dose | No | Resolved after 24 hours. Missed 1 exercise session. |
| Control | Low Back Pain | Mild | Doubtfully related | Discontinued Permanently | No | The participant completed the exercise intervention portion of the study. When scheduling the follow-up testing session, the participant reported having received a LBP intervention (physical therapy) during the follow-up period. Participant was withdrawn from study. |
| Experimental | Salivary stent surgery planned | Moderate | Clearly Unrelated | None | No | During the follow-up period subject reported having a salivary stent placed. |
AE: Adverse event; SAE: Serious adverse event; DOMS: Delayed onset muscle soreness.
Average treatment acceptability scores (9–45 scale with a higher score reflective of better treatment acceptance) were relatively high in both groups (BFR Exercise Group: 31.4±5.7; CON Exercise Group: 34.5±4.0), and scores were not statistically different between groups (p=0.08).
DISCUSSION
We found that trunk muscle responses to low-load exercise were not enhanced following BFR exercise of the limb muscles for any of the outcome measures at any time point in this randomized, single-blinded trial. Thus, it appears that attempting to use the cross-transfer effect of BFR exercise is not a viable strategy for enhancing trunk muscle performance while maintaining lower mechanical loading of the spine. More surprising was our observation that BFR did not systematically enhance limb muscle mass and strength to a greater extent than low-load resistance exercise without BFR, despite numerous studies with contradictory findings (for reviews and meta-analyses see (2–7). We further discuss these findings below.
The lack of a cross-transfer of effect on the trunk muscles might be a function of an inadequate trunk muscle exercise stimulus. Though the trunk exercise was performed at 25% of isometric maximum, which has been associated with a positive cross-transfer effect (43), it is unknown how much of the isometric maximum or 25% max force was generated by the erector spinae and how much was generated by other muscles (e.g., hip extensors). Thus, the load on the erector spinae during the prescribed exercise protocol could have been insufficient to induce gains in size or strength, even with the addition of BFR, such as previously reported by Abe et al. (43). It could also be that the recurrent, non-specific LBP population studied here exhibits impaired central activation of the trunk muscles, thus limiting the response to training. However, in our opinion, the most likely explanation for a lack of cross-transfer of effect is a lack of systemic hormonal influence on hypertrophy or strength gains (18, 19). Curiously, our most robust finding was an increase in trunk extension strength and endurance in the control group during the follow-up period. We struggle to explain these findings.
As noted, the lack of an effect of BFR on the limb muscles was surprising. Numerous studies over the past 15–20 years have reported that low-load BFR resistance exercise facilitates exercise-induced gains in muscle mass and strength (8, 13, 39, 44, 45). Two recent meta-analyses indicated the superiority of BFR resistance training when compared to an equivalent low-load resistance training program without BFR (2, 5) and another meta-analysis suggested that low-load blood flow restricted exercise was equally as effective as high-load resistance exercise at generating muscle hypertrophy (4). Thus, our findings that low-load BFR resistance exercise was no better than low-load resistance exercise is contrary to much of the extant literature. There are a few potential reasons for this.
It could be that the recurrent, non-specific LBP population had problems in the activation of limb muscles, as individuals with recurrent, non-specific LBP have been reported to exhibit impairments in quadriceps activation capacity following aerobic exercise (46). It could also be that our exercise protocol differed from many of those performed in previous studies. Here, subjects in both exercise groups were asked to perform the exercise to volitional concentric task failure, while in numerous BFR exercise studies exercise dose has been based on repetition or volume (8, 13, 39, 44, 45). Our rationale was to match the groups for volitional effort. Consistent with our findings, Farup and colleagues (2015) as well as Fahs and colleagues (2015) observed that low-load BFR exercise and low-load resistance exercise without restriction, when performed to volitional failure (3x/week for 6-weeks), resulted in equal muscle hypertrophy (47). We would argue that protocols not matching for volitional effort (but rather repetitions or volume) do not directly address the question of whether there is added value to the adaptive response associated with blood flow restriction per se, but are rather evaluating whether or not low-load exercise when performed to task failure can induce muscle growth and strength gains. With this stated, it should be noted that moderate effect sizes were noted for BFR exercise enhancing muscle size and strength in the leg extensors (η2=0.19 and 0.27, respectively). As such, it is probable that we were underpowered to detect these differences. However, these potentially positive effects (based on effect size interpretation) must be considered alongside the lack of positive effect sizes for BFR exercise in relation to leg extensor muscle endurance as well as muscle strength of the plantar and elbow flexor muscles.
It is also worth noting that our study implemented rigorous control measures that are lacking from much of the previous work on BFR exercise (48, 49). For instance, we designed our trial to match for volitional effort (as discussed above), randomized our subjects, and blinded our outcome assessors, data analysts, and statistician. While we cannot be certain that our discrepant results are due to our bias control measures, it is plausible inasmuch that numerous biases are believed to affect the scientific literature and it has been suggested that these biases are creating crisis (50). Accordingly, we advocate for the inclusion of strong bias controls in future studies and publications in the BFR exercise field.
Lastly, we should note that in the current study both control and BFR exercise groups performed the training at 25% of their maximum strength. Our findings should be interpreted within this context. Specifically, the usage of low-intensity exercise in the appendicular muscles of the control group should be questioned because the limbs have minimal restriction for mechanical load in this scenario. This design does not impact the BFR exercise findings per se, but certainly this approach limits the opportunity for the exercise control group to exhibit positive direct and cross-transfer of effect findings.
In conclusion, we did not observe changes in muscle morphology and performance that would support the cross-transfer effect of limb BFR exercise to the trunk extensor muscles of individuals with recurrent, non-specific LBP. Thus, it appears that BFR exercise would provide no added rehabilitative benefit for adults with recurrent, non-specific low back pain. In addition, we did not observe BFR exercise to increase limb muscle outcome measures at any time point. Contrary to prior reports, these findings indicate that BFR exercise does not enhance muscle mass and strength to a greater extent than low-load resistance exercise without blood flow restriction. These results are contrary to the majority of prior reports on BFR exercise training.
Supplementary Material
Supplemental digital content 1. The Consolidated Standards of Reporting Trials (CONSORT) Flow Diagram.
ACKNOWLEDGEMENTS AND GRANTS
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health (NIH), under Award number R21AR063909 (to BC Clark), supported the research reported in this publication. The content is solely the responsibility of the authors and does not represent the official views of the NIH. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the ACSM.
Footnotes
CONFLICT OF INTEREST
Brian Clark has received research funding from the National Institutes of Health, Regeneron Pharmaceuticals, Astellas Pharma Global Development, Inc., RTI Health Solutions, Ohio Department of Higher Education, and the Osteopathic Heritage Foundations. In the past 5-years Brian Clark has received consulting fees from Regeneron Pharmaceuticals, Abbott Laboratories, and the Gerson Lehrman Group. Additionally, Brian Clark is co-founder with equity and scientific director of AEIOU Scientific, LLC. In the past five years, David Russ has received research funding and consulting fees from Abbott Nutrition. The other authors declare no conflicts of interest.
Publisher's Disclaimer: Medicine & Science in Sports & Exercise® Published ahead of Print contains articles in unedited manuscript form that have been peer reviewed and accepted for publication. This manuscript will undergo copyediting, page composition, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered that could affect the content.
REFERENCES
- 1.Sundberg CJ, Eiken O, Nygren A, Kaijser L. Effects of ischaemic training on local aerobic muscle performance in man. Acta Physiol Scand. 1993;148(1):13–9. [DOI] [PubMed] [Google Scholar]
- 2.Slysz J, Stultz J, Burr JF. The efficacy of blood flow restricted exercise: A systematic review & meta-analysis. Journal of science and medicine in sport. 2016;19(8):669–75. [DOI] [PubMed] [Google Scholar]
- 3.Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD. Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med. 2017;51(13):1003–11. [DOI] [PubMed] [Google Scholar]
- 4.Lixandrao ME, Ugrinowitsch C, Berton R et al. Magnitude of Muscle Strength and Mass Adaptations Between High-Load Resistance Training Versus Low-Load Resistance Training Associated with Blood-Flow Restriction: A Systematic Review and Meta-Analysis. Sports Med. 2018;48(2):361–78. [DOI] [PubMed] [Google Scholar]
- 5.Loenneke JP, Wilson JM, Marin PJ, Zourdos MC, Bemben MG. Low intensity blood flow restriction training: a meta-analysis. Eur J Appl Physiol. 2012;112(5):1849–59. [DOI] [PubMed] [Google Scholar]
- 6.Manini TM, Clark BC. Blood flow restricted exercise and skeletal muscle health. Exerc Sport Sci Rev. 2009;37(2):78–85. [DOI] [PubMed] [Google Scholar]
- 7.Pope ZK, Willardson JM, Schoenfeld BJ. Exercise and blood flow restriction. J Strength Cond Res. 2013;27(10):2914–26. [DOI] [PubMed] [Google Scholar]
- 8.Madarame H, Neya M, Ochi E, Nakazato K, Sato Y, Ishii N. Cross-transfer effects of resistance training with blood flow restriction. Med Sci Sports Exerc. 2008;40(2):258–63. [DOI] [PubMed] [Google Scholar]
- 9.Ozaki H, Yasuda T, Ogasawara R, Sakamaki-Sunaga M, Naito H, Abe T. Effects of high-intensity and blood flow-restricted low-intensity resistance training on carotid arterial compliance: role of blood pressure during training sessions. Eur J Appl Physiol. 2013;113(1):167–74. [DOI] [PubMed] [Google Scholar]
- 10.Thiebaud RS, Loenneke JP, Fahs CA et al. The effects of elastic band resistance training combined with blood flow restriction on strength, total bone-free lean body mass and muscle thickness in postmenopausal women. Clin Physiol Funct Imaging. 2013;33(5):344–52. [DOI] [PubMed] [Google Scholar]
- 11.Yasuda T, Ogasawara R, Sakamaki M, Bemben MG, Abe T. Relationship between limb and trunk muscle hypertrophy following high-intensity resistance training and blood flow-restricted low-intensity resistance training. Clin Physiol Funct Imaging. 2011;31(5):347–51. [DOI] [PubMed] [Google Scholar]
- 12.Pierce JR, Clark BC, Ploutz-Snyder LL, Kanaley JA. Growth hormone and muscle function responses to skeletal muscle ischemia. J Appl Physiol. 2006;101(6):1588–95. [DOI] [PubMed] [Google Scholar]
- 13.Abe T, Yasuda T, Midorikawa T et al. Skeletal muscle size and circulating IGF-1 are increased after two weeks of twice daily “KAATSU” resistance training. Int J KAATSU Training Research. 2005;1(1):6–12. [Google Scholar]
- 14.Abe T, Kearns CF, Sato Y. Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J Appl Physiol (1985). 2006;100(5):1460–6. [DOI] [PubMed] [Google Scholar]
- 15.Takarada Y, Nakamura Y, Aruga S, Onda T, Miyazaki S, Ishii N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J Appl Physiol (1985). 2000;88(1):61–5. [DOI] [PubMed] [Google Scholar]
- 16.Reeves GV, Kraemer RR, Hollander DB et al. Comparison of hormone responses following light resistance exercise with partial vascular occlusion and moderately difficult resistance exercise without occlusion. J Appl Physiol (1985). 2006;101(6):1616–22. [DOI] [PubMed] [Google Scholar]
- 17.Kraemer WJ, Marchitelli L, Gordon SE et al. Hormonal and growth factor responses to heavy resistance exercise protocols. J Appl Physiol (1985). 1990;69(4):1442–50. [DOI] [PubMed] [Google Scholar]
- 18.West DW, Burd NA, Tang JE et al. Elevations in ostensibly anabolic hormones with resistance exercise enhance neither training-induced muscle hypertrophy nor strength of the elbow flexors. J Appl Physiol (1985). 2010;108(1):60–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.West DW, Kujbida GW, Moore DR et al. Resistance exercise-induced increases in putative anabolic hormones do not enhance muscle protein synthesis or intracellular signalling in young men. J Physiol. 2009;587(Pt 21):5239–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biering-Sorensen F Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976). 1984;9(2):106–19. [DOI] [PubMed] [Google Scholar]
- 21.Takala EP, Viikari-Juntura E. Do functional tests predict low back pain? Spine (Phila Pa 1976). 2000;25(16):2126–32. [DOI] [PubMed] [Google Scholar]
- 22.Alaranta H, Luoto S, Heliovaara M, Hurri H. Static back endurance and the risk of low-back pain. Clin Biomech (Bristol, Avon). 1995;10(6):323–4. [DOI] [PubMed] [Google Scholar]
- 23.Hodges P, Holm AK, Hansson T, Holm S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine. 2006;31(25):2926–33. [DOI] [PubMed] [Google Scholar]
- 24.Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9(4):266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gibbons LE, Videman T, Battie MC. Isokinetic and psychophysical lifting strength, static back muscle endurance, and magnetic resonance imaging of the paraspinal muscles as predictors of low back pain in men. Scand J Rehabil Med. 1997;29(3):187–91. [PubMed] [Google Scholar]
- 26.Hides J, Gilmore C, Stanton W, Bohlscheid E. Multifidus size and symmetry among chronic LBP and healthy asymptomatic subjects. Man Ther. 2008;13(1):43–9. [DOI] [PubMed] [Google Scholar]
- 27.Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine (Phila Pa 1976). 1996;21(23):2763–9. [DOI] [PubMed] [Google Scholar]
- 28.Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976). 1994;19(2):165–72. [DOI] [PubMed] [Google Scholar]
- 29.Storheim K, Holm I, Gunderson R, Brox JI, Bo K. The effect of comprehensive group training on cross-sectional area, density, and strength of paraspinal muscles in patients sick-listed for subacute low back pain. Journal of spinal disorders & techniques. 2003;16(3):271–9. [DOI] [PubMed] [Google Scholar]
- 30.Verbunt JA, Seelen HA, Vlaeyen JW et al. Disuse and deconditioning in chronic low back pain: concepts and hypotheses on contributing mechanisms. Eur J Pain. 2003;7(1):9–21. [DOI] [PubMed] [Google Scholar]
- 31.McGill SM. Low Back Disorders. Champaign, IL: Human Kinetics; 2007. [Google Scholar]
- 32.Marras WS, Ferguson SA, Burr D, Davis KG, Gupta P. Spine loading in patients with low back pain during asymmetric lifting exertions. Spine J. 2004;4(1):64–75. [DOI] [PubMed] [Google Scholar]
- 33.Amano S, Ludin AF, Clift R et al. Effectiveness of blood flow restricted exercise compared with standard exercise in patients with recurrent low back pain: study protocol for a randomized controlled trial. Trials. 2016;17:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monzon A, Hemler PF, Nalls M et al. Segmentation of magnetic resonance images of the thighs for a new NIH initiative. SPIE: Medical Imaging. 2007;6212:65123L. [Google Scholar]
- 35.Manini TM, Clark BC, Nalls MA, Goodpaster BH, Ploutz-Snyder LL, Harris TB. Reduced physical activity increases intermuscular adipose tissue in healthy young adults. Am J Clin Nutr. 2007;85(2):377–84. [DOI] [PubMed] [Google Scholar]
- 36.Williams PS, Hoffman RL, Clark BC. Preliminary evidence that anodal transcranial direct current stimulation enhances time to task failure of a sustained submaximal contraction. PLoS One. 2013;8(12):e81418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams PS, Hoffman RL, Clark BC. Cortical and spinal mechanisms of task failure of sustained submaximal fatiguing contractions. PLoS One. 2014;9(3):e93284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelley M, Heffer R, Gresham F, Elliott S. Development of a modified treatment evaluation invesntory. J Psychopath Behav Assess. 1989;11(3):235–47. [Google Scholar]
- 39.Patterson SD, Ferguson RA. Enhancing strength and postocclusive calf blood flow in older people with training with blood-flow restriction. J Aging Phys Act. 2011;19(3):201–13. [DOI] [PubMed] [Google Scholar]
- 40.Clark BC, Manini TM, Hoffman RL et al. Relative safety of 4 weeks of blood flow-restricted resistance exercise in young, healthy adults. Scand J Med Sci Sports. 2011;21(5):653–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.KAATSU Global I. KAATSU Equipment User Manaual. 2017. Available from: http://kaatsu-canada.net/images/userManual.pdf.
- 42.NCI [Internet]. U.S. Department of Health and Human Services. Available from: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. [DOI] [PubMed]
- 43.Abe T, Loenneke JP, Fahs CA, Rossow LM, Thiebaud RS, Bemben MG. Exercise intensity and muscle hypertrophy in blood flow-restricted limbs and non-restricted muscles: a brief review. Clin Physiol Funct Imaging. 2012;32(4):247–52. [DOI] [PubMed] [Google Scholar]
- 44.Takarada Y, Takazawa H, Sato Y, Takebayashi S, Tanaka Y, Ishii N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J Appl Physiol (1985). 2000;88(6):2097–106. [DOI] [PubMed] [Google Scholar]
- 45.Yamanaka T, Farley RS, Caputo JL. Occlusion training increases muscular strength in division IA football players. J Strength Cond Res. 2012;26(9):2523–9. [DOI] [PubMed] [Google Scholar]
- 46.Hart JM, Weltman A, Ingersoll CD. Quadriceps activation following aerobic exercise in persons with low back pain and healthy controls. Clin Biomech (Bristol, Avon). 2010;25(8):847–51. [DOI] [PubMed] [Google Scholar]
- 47.Farup J, de Paoli F, Bjerg K, Riis S, Ringgard S, Vissing K. Blood flow restricted and traditional resistance training performed to fatigue produce equal muscle hypertrophy. Scand J Med Sci Sports. 2015;25(6):754–63. [DOI] [PubMed] [Google Scholar]
- 48.Smart NA, Waldron M, Ismail H et al. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. International journal of evidence-based healthcare. 2015;13(1):9–18. [DOI] [PubMed] [Google Scholar]
- 49.Clark GT, Mulligan R. Fifteen common mistakes encountered in clinical research. Journal of prosthodontic research. 2011;55(1):1–6. [DOI] [PubMed] [Google Scholar]
- 50.Fanelli D, Costas R, Ioannidis JP. Meta-assessment of bias in science. Proc Natl Acad Sci U S A. 2017;114(14):3714–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content 1. The Consolidated Standards of Reporting Trials (CONSORT) Flow Diagram.