Abstract
Objective:
To evaluate whether a multi-pronged pilot intervention promoting healthier beverage consumption improved at-home beverage consumption and weight status among young children.
Design:
In this exploratory pilot study, we randomly assigned four child care centers to a control (delayed-intervention) condition or to a 12-week intervention that promoted consumption of healthier beverages (water, unsweetened low- or non-fat milk) and discouraged consumption of less-healthy beverages (juice, sugar-sweetened beverages, high-fat or sweetened milk). The multi-pronged intervention was delivered via child care centers; simultaneously targeted children, parents, and child care staff; and included environmental changes, policies, and education. Outcomes were measured at baseline and immediately post-intervention and included children’s (n=154) at-home beverage consumption (assessed via parental report) and overweight/obese status (assessed via objectively-measured height and weight). We estimated intervention impact using difference-in-differences models controlling for children’s demographics and classroom.
Setting:
Two Northern California cities, United States, 2013–2014.
Participants:
Children ages 2–5 years and their parents.
Results:
Relative to control group children, intervention group children reduced their consumption of less-healthy beverages from baseline to follow-up by 5.9 ounces/day (95% CI: −11.2,−0.6) and increased their consumption of healthier beverages by 3.5 ounces/day (95% CI: −2.6,9.5). Children’s likelihood of being overweight decreased by 3 percentage points in the intervention group and increased by 3 percentage points in the control group (difference-in-differences: −6 percentage points, 95% CI: −15,3).
Conclusions:
Our exploratory pilot study suggests that interventions focused comprehensively on encouraging healthier beverage consumption could improve children’s beverage intake and weight. Findings should be confirmed in longer, larger studies.
Keywords: Child care, early childhood, early care and education, obesity prevention, beverage consumption, beverage intake, nutrition, dietary behaviors, body mass, overweight, obesity, sugar-sweetened beverages, water, juice, milk
Introduction
More than one in four U.S. children ages 2 to 5 years are overweight or obese (1), increasing their risk for poor health outcomes and premature death in adulthood(2,3). Children’s beverage consumption habits are an important driver of childhood obesity. For example, consumption of sugar-sweetened beverages (SSBs) such as sodas, sports drinks, and fruit-flavored drinks increases risk of excess weight gain(4–6). Likewise, a recent meta-analysis found that consumption of 100% fruit juice is associated with a small amount of weight gain among children ages 1–6 years(7), and one study found that fruit juice consumption in early childhood is associated with higher SSB intake and higher body mass index (BMI) later in childhood(8). Conversely, consumption of healthier beverages, such as water, may help limit excess weight gain in children(9,10).
Experts agree that 2-to-5-year-olds should drink low- or non-fat milk and plain water, consume no more than 4–6 ounces/day of 100% fruit juice, and limit their consumption of SSBs (Supplemental Table 1)(11–13). While debate remains over whether to encourage children to drink sweetened milk(14), one expert panel advised against promoting sweetened milk(11), noting that its consumption is associated with increased energy intake(15). Despite these guidelines, many children consume juice, SSBs, and sweetened or high-fat milk(16–18). On any given day, 45% of children ages 2–5 years consume 100% fruit juice and 47% consume SSBs, with average intake at 53 calories/day for juice and more than 60 calories/day for SSBs(16). Given the limited progress in reversing the obesity epidemic among young children(1), new efforts are needed to improve young children’s beverage intake and limit their excess weight gain(16,18).
Child care facilities are an important setting for reaching young children and their parents with obesity prevention interventions. In the United States, approximately 11 million children under the age of 5 attend some type of child care every week(19), making these locations ideal both for shaping the dietary habits of large numbers of children and for reaching their parents with educational messages. Yet to date, few interventions delivered via child care settings have focused comprehensively on encouraging young children to drink water and low- or non-fat milk in lieu of SSBs and juice(20,21).
To fill this gap, we developed and implemented a multi-level, multi-pronged intervention that encouraged young children to consume water and low- or non-fat unsweetened milk instead of juice and SSBs. This study aimed to evaluate the pilot intervention’s impact on children’s weight (overweight/obese status [primary outcome], BMI, and BMI percentile) and beverage consumption, with a goal of determining the promise of the intervention and providing the data necessary to calculate sample size needs for larger trials. Based on previous studies of school-based water promotion interventions(9,22–25), we predicted that the intervention would increase children’s consumption of healthier beverages, reduce their consumption of less-healthy beverages, and lower their likelihood of having an unhealthy weight.
Methods
Participants
Child care centers and classrooms.
We recruited a convenience sample of four child care centers in Northern California for this pilot study. Centers were eligible if they were in San Mateo County, CA; were licensed(26); had enrolled at least ten children ages 2–5 years; had English or Spanish-speaking staff; served primarily English or Spanish-speaking families; and participated in the Child and Adult Care Food Program (CACFP, a federal nutrition assistance program providing funding for meals and snacks and a marker for centers that serve lower income children(27)). With help from district-level administrators, we identified four centers in two cities (two centers per city) to participate in the study. We ensured that recruited centers within each city were similar in number of students per classroom and in the type of program(s) offered (i.e., half- vs. full-day). Within each city, we randomly assigned one center to the intervention group and the other to the control (delayed intervention) group. A total of seven classrooms across the four centers participated: four classrooms in the intervention group and three classrooms in the control group.
Parents and children.
At each center, all eligible children and their parents were invited to participate. Children were eligible if they were 2–5 years old. Their parents were eligible if they spoke English or Spanish. Parents provided written informed consent for both their participation and their child’s participation.
Intervention
We designed the intervention to encourage children to consume age-appropriate beverages consistent with expert recommendations(11). The intervention promoted consumption of healthier beverages (i.e., water and unsweetened low- or non-fat milk) and recommended limiting consumption of less-healthy beverages (i.e., replacing juice with whole fruit and limiting SSBs, including sweetened milk, to no more than one serving per week).
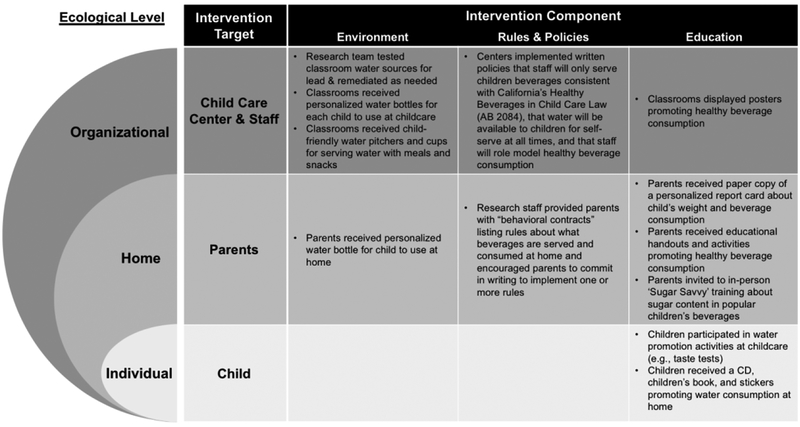
The 12-week intervention took place in Spring 2014. We designed the intervention to operate at multiple levels of the Social Ecological Framework(28,29) (Figure 1). The intervention targeted children, parents, and child care center staff and included three main components: 1) environmental changes, 2) implementation of rules and policies, and 3) educational activities. To enhance the feasibility, acceptability, and effectiveness of the intervention, we assembled a community advisory board (CAB), consisting of representatives from the county public health department, local child care organizations (e.g., Head Start, the local child care resource and referral agency, and the school districts overseeing the participating child care centers), child care providers, and parents with preschool-aged children. The CAB provided regular in-person and written feedback on intervention materials and implementation.
Figure 1.
Intervention activities used to promote children’s healthy beverage consumption by social ecological level, intervention target, and component.
Environmental changes.
Environmental changes focused on increasing children’s access to water at child care centers and at home. Prior to the intervention, the research team conducted water testing and remediation for lead in all intervention classrooms based on Environmental Protection Agency (EPA) recommendations(30). At baseline, no classrooms were serving water at all meals and snacks. To increase access to water during meal and snack times, the research team supplied classrooms with child-sized pitchers and cups so children could pour themselves water at meals and snacks. We also asked providers to serve children water at meals and snacks. We also observed that, at baseline, only one center had water available for children to self-serve outside of mealtimes. To increase children’s access to water outside of meal times, the research team provided all children with a child-sized reusable water bottle personalized with their name and photograph that they could use to serve themselves water throughout the day. Finally, to allow children to self-serve water outside of child care hours, we also provided each child with a second personalized water bottle to use at home.
Policies.
In 2010, California passed AB 2084, the Healthy Beverages in Childcare Policy(31). The policy, effective January 1, 2012, requires licensed child care facilities in California to: serve only milk that is low-fat (1%) or non-fat to children over two years of age; refrain from providing juice or beverages with added sugar including sweetened milk; and provide clean and safe drinking water at all times, including during meals and snacks. Despite AB 2084 having been in place for nearly two years at the time of the intervention, pre-intervention observations of classrooms indicated that only one center was complying with the requirement to provide water at all times. Observations also revealed that some centers served juice or allowed parents to send juice or SSBs with their children to child care and that no centers had integrated AB 2084 requirements into their written policies. These observations are consistent with previous research showing that there is often a delay between when policymakers pass new nutrition requirements and when child care centers come into full compliance with these requirements(32). To encourage implementation of AB 2084, the study principal investigator met with center directors and head teachers to explain the policy and to ask that centers comply with the new standards. Center directors also incorporated rules about beverage access and consumption into their written staff handbooks or wellness policies using language provided by the research team.
The intervention also encouraged families to adopt rules to promote healthier beverage consumption at home. Parents received written “behavioral contracts” listing rules about beverages they might consider adopting (e.g., limit children to no more than one serving of SSBs per week; serve whole fruit instead of fruit juice). Parents were encouraged to commit in writing to implementing one or more of these rules. Parents who returned completed contracts were eligible for a raffle for water bottles and gift cards.
Educational activities.
The intervention also included educational activities for both parents and children. Parents received personalized report cards describing their child’s weight and beverage consumption (developed using children’s baseline data and qualitative research on best practices for designing BMI report cards(33)), informational handouts (e.g., recipes for spa water), and interactive family activities (e.g., a worksheet for finding free water sources at the park). The research team delivered these written materials to parents via children’s mailboxes at the child care center. Parents were also invited to attend an in-person training in which study staff described how to determine the amount of added sugar in popular children’s beverages using the products’ nutrition labels.
Children participated in a wide variety of engaging, age-appropriate educational activities while at child care, including spa water taste tests (children sampled water infused with fruit or herbs), singing along to the “Drink More Water” children’s song developed specifically for the study(34), and reading the children’s book Potter the Otter: A Tale About Water(35). Research assistants or child care teachers facilitated these activities. To reinforce these lessons at home, children each received a CD with the “Drink More Water” children’s song, a copy of the Potter the Otter: A Tale About Water book, and stickers promoting water consumption.
Measures
We assessed outcomes at baseline (late 2013) and immediately following the 12-week intervention period (spring of 2014). We examined children’s weight status (overweight/obese vs. not), BMI percentile(36), raw (absolute) BMI(36,37), and children’s at-home beverage consumption.
Children’s anthropometrics.
Trained research assistants measured children’s anthropometrics using National Health and Nutrition Examination Survey (NHANES) protocols(38), measuring height to the nearest 0.1 centimeter using a portable stadiometer (Seca® North America; Chino, CA, USA) and weight to the nearest 0.01 kg using a digital scale (Tanita® Corporation; Arlington Heights, IL, USA). Measurements were collected at child care centers during the day. All measurements were taken twice. If the two measurements differed by more than 1 cm (height) or 0.1 kg (weight), a third was taken. We used the average of all measurements taken to compute BMI (kg/m2). We then calculated BMI percentile using the Centers for Disease Control and Prevention age- and sex-specific growth charts(39) and classified children as overweight/obese if their BMI percentile was at or above the 85th percentile for their age and sex.
Children’s at-home beverage consumption.
We assessed children’s at-home beverage consumption via parental report. Parents reported on their children’s at-home beverage consumption for past 24 hours (excluding times while the child was at child care) using a questionnaire adapted from a previously-validated instrument for assessing older children’s beverage consumption(40). Parents reported whether their child consumed beverages in 22 categories, including different types of milk, SSBs (e.g., fruit drinks, Kool-Aid, sports drinks, sodas), 100% fruit juice, tap water, and bottled water (Supplemental Table 2). For each beverage their child consumed, parents estimated the total amount the child drank in ounces. Most parents self-administered a written version of the questionnaire; the research team verbally administered questionnaires to parents with lower-literacy. To improve accuracy and completeness, research staff followed up with parents in-person or via phone regarding ambiguous or incomplete information.
We used parents’ survey responses to calculate children’s at-home beverage consumption, in ounces/day, of the following categories: each of the healthier beverages promoted by the intervention (total water, tap water, bottled water, unsweetened low- or non-fat milk), each of the less-healthy beverages discouraged by the intervention (100% juice, total SSBs excluding sweetened milk, unsweetened high-fat milk, sweetened milk), all healthier beverages combined, and all less-healthy beverages combined. We did not assess children’s beverage consumption while at child care.
Demographics.
Baseline questionnaires asked parents to report their marital status, educational attainment, ethnicity (Hispanic/Latino vs. not), household income, and number of household members. Parents also reported their child’s sex and date of birth, which we used to calculate the child’s exact age at the time of BMI measurements.
Intervention fidelity.
To provide insight on the extent to which classrooms implemented the water availability component of the intervention, we conducted weekly, unannounced “spot check” fidelity observations of intervention classrooms during meal or snack times. Trained observers recorded whether child care staff served water to children during the meal or snack, as encouraged by the intervention. In addition, we conducted day-long observations immediately post-intervention using the Environmental and Policy Assessment and Observation (EPAO) instrument(41) to assess compliance with various other aspects of the intervention (e.g., whether classrooms had water available for self-serve during outdoor playtime). Finally, we tracked the number of parents who returned a completed behavioral contract indicating they planned to implement one or more rule about beverages at home.
Analysis
To describe the sample, we calculated means, standard deviations, and proportions for child, parent, and household characteristics. To estimate intervention impact, we used generalized linear models with a difference-in-differences approach. For each outcome, we compared the change from baseline to follow-up (immediately post 12-week-intervention) in the intervention group to the change over the same period in the control group. The primary outcome was children’s overweight/obese status. Secondary outcomes were children’s at-home consumption of: each healthier beverage (i.e., total water, tap water, bottled water, unsweetened low- or non-fat milk), each less-healthy beverage (i.e., 100% juice, total SSBs excluding sweetened milk, unsweetened high-fat milk, sweetened milk), all healthier beverages combined, and all less-healthy beverages combined. We also assessed BMI percentile and absolute BMI (kg/m2) as exploratory outcomes. Due to the pilot nature of the study, we did not conduct power analyses.
Analytic models controlled for child’s age and sex (except for models assessing BMI-percentile and weight status, which are already age- and sex-specific) and parent/household demographic characteristics (marital status, Hispanic ethnicity, income, educational attainment, and household size). All models included indicators for time period (baseline vs. follow-up), study group (intervention vs. control), and an interaction between time period and study group.
Data were nested within children (repeated measures over time), classrooms, and centers. Classroom-level intraclass correlation coefficients (ICCs) ranged from <0.01 to 0.07 and center level ICCs ranged from <0.01 to 0.02 (Supplemental Table 3 presents ICCs for all outcomes at the child-, classroom-, and center-levels). To account for clustering, models clustered standard errors within children and included a set of indicator variables (i.e., fixed effects) for child care classrooms. Inclusion of classroom fixed effects also accommodated and corrected for any potential pair effects resulting from having conducted randomization within cities. Missing data comprised <15% of cases for all demographic variables. Analyses were conducted in Stata SE Version 15.1 (StataCorp LP, College Station, TX).
To describe intervention fidelity, we calculated the proportion of meals/snacks at which child care staff served water during the spot check fidelity observations. We also used EPAO observations to examine the number of intervention classrooms that complied with key intervention components (e.g., how many intervention classrooms served water at each meal). Finally, we calculated the proportion of parents who returned a behavioral contract to the research team indicating the rules about beverages they planned to implement.
Results
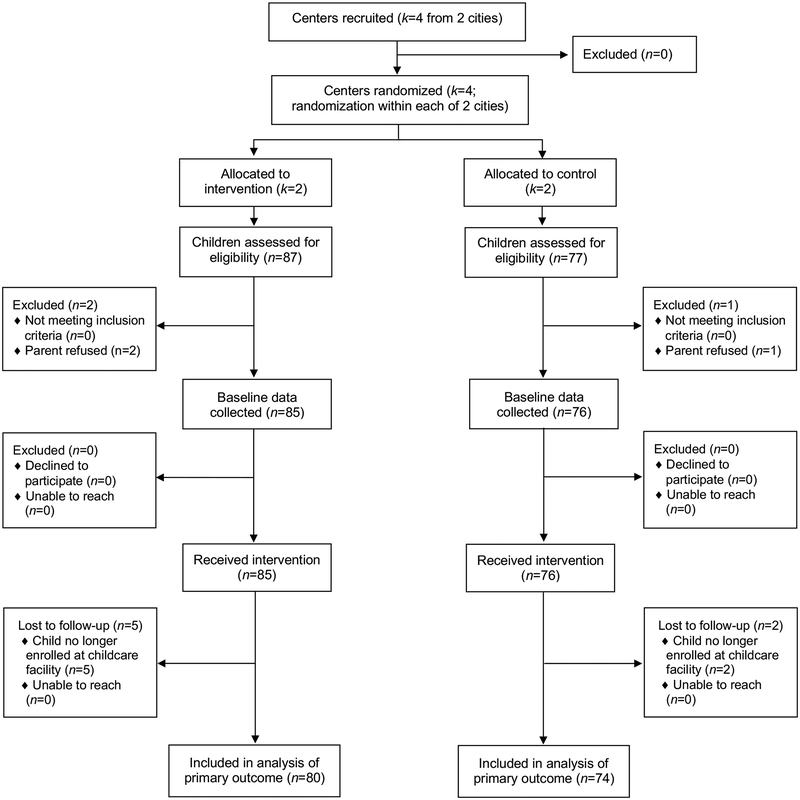
All centers approached for the study agreed to participate. Two centers (four classrooms; 87 total children) were randomized to receive the healthy beverages intervention and two centers (three classrooms; 77 total children) were randomized to the control (delayed intervention) group (Figure 2). Because the intervention was delivered via centers, all children (100%) in randomized centers received the intervention. Most parents (161, 98%) agreed to have their child’s height and weight measured. Of the 161 children measured at baseline, seven (4%) were lost to follow-up because the child was no longer enrolled at the facility, leaving 154 children with BMI data at both time points included in analyses of the primary outcome.
Figure 2.
CONSORT flow diagram.
The sample was predominantly Hispanic/Latino and low-income, with two-thirds of parents reporting annual household income of $30,000 or less (Table 1).
Table 1.
Characteristics of children, parents and households by study group, n=154
| Intervention (n=80 children) |
Control (n=74 children) |
|||
|---|---|---|---|---|
| Characteristic | Mean or % | (SD) or (N) | Mean or % | (SD) or (N) |
| Children’s characteristics | ||||
| Age at baseline in years, mean (SD) | 4.10 | (0.59) | 4.32 | (0.44) |
| Male | 45% | (36) | 46% | (34) |
| Overweight/obese at baseline | 43% | (34) | 39% | (29) |
| Parent/household characteristics | ||||
| Hispanic ethnicity | 98% | (64) | 82% | (53) |
| Education of high school degree or less | 66% | (49) | 54% | (34) |
| Married | 66% | (47) | 65% | (40) |
| Annual Household Income ≤ $30,000 | 67% | (51) | 67% | (43) |
| No. household members, mean (SD) | 3.71 | (1.32) | 3.89 | (1.42) |
Notes. Characteristics are presented by study group for qualitative comparison, thus, p-values are not reported. Ns may not sum to total sample size due to missing data on some characteristics.
Beverage consumption.
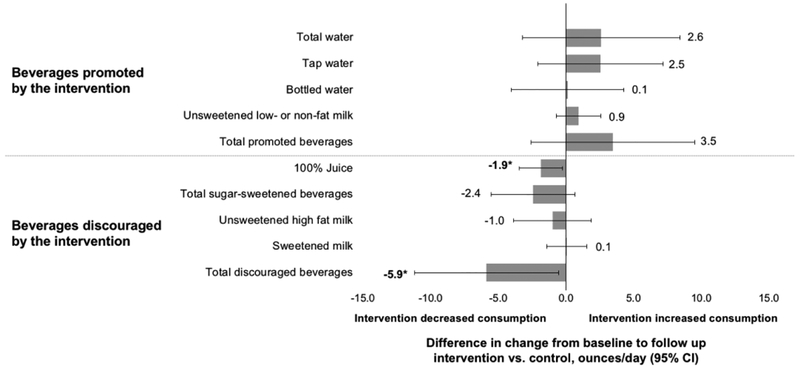
Results indicated that the intervention helped discourage children’s at-home consumption of less-healthy beverages. Children in the intervention group showed larger reductions in consumption of all less-healthy beverages combined compared to children the control group (difference-in-differences [DD]: −5.9 ounces/day, 95% CI: −11.2, −0.6) (Table 2, Figure 3). The intervention also significantly reduced juice consumption (DD: −1.9 ounces/day, 95% CI: −3.5, −0.2) and showed favorable but nonsignificant impacts on SSB consumption (DD: −2.4 ounces/day, 95% CI: −5.5, 0.7). Consumption of unsweetened high-fat milk decreased somewhat in the intervention group (−2.1 ounces/day, 95% CI: −4.3, 0.03), compared to a decrease of 1.1 ounces/day in the control group (95% CI: −3.4, 1.2), though the difference-in-differences between groups was not significant (DD: −1.0 ounces/day, 95% CI: −3.9, 1.9). Consumption of sweetened milk was stable over time in both groups.
Table 2.
Adjusted means and changes over time in children’s beverage consumption, weight status, and body mass by study group, n=154
| Difference | ||||
|---|---|---|---|---|
| Baseline | Follow-Up | Point Est. | (95% CI) | |
| Beverage consumption (ounces/day) | ||||
| All less-healthy beveragesa | ||||
| Intervention group | 13.1 | 10.8 | −2.3 | (−7.2, 2.6) |
| Control group | 13.9 | 17.5 | 3.6 | (−0.8, 7.9) |
| Difference | −5.9 | (−11.2, −0.6) | ||
| All healthier beveragesa | ||||
| Intervention group | 13.8 | 18.8 | 5.0 | (0.5, 9.4) |
| Control group | 8.3 | 9.8 | 1.5 | (−2.9, 5.9) |
| Difference | 3.5 | (−2.6, 9.5) | ||
| 100% juice | ||||
| Intervention group | 3.4 | 1.5 | −1.9 | (−3.4, −0.4) |
| Control group | 2.1 | 2.0 | −0.03 | (−1.2, 1.1) |
| Difference | −1.9 | (−3.5, −0.2) | ||
| Total SSBs excluding sweetened milk | ||||
| Intervention group | 2.5 | 4.3 | 1.8 | (−1.3, 4.8) |
| Control group | 0.5 | 4.7 | 4.2 | (1.4, 7.0) |
| Difference | −2.4 | (−5.5, 0.7) | ||
| Unsweetened high−fat (2% or whole) milk | ||||
| Intervention group | 4.8 | 2.7 | −2.1 | (−4.3, 0.03) |
| Control group | 9.5 | 8.4 | −1.1 | (−3.4, 1.2) |
| Difference | −1.0 | (−3.9, 1.9) | ||
| Sweetened milk | ||||
| Intervention group | 1.2 | 1.2 | 0.1 | (−1.2, 1.4) |
| Control group | 1.0 | 1.0 | 0.02 | (−0.9, 0.9) |
| Difference | 0.1 | (−1.4, 1.5) | ||
| Total watera | ||||
| Intervention group | 13.7 | 17.6 | 4.0 | (−0.3, 8.2) |
| Control group | 6.6 | 8.0 | 1.4 | (−2.9, 5.7) |
| Difference | 2.6 | (−3.2, 8.4) | ||
| Tap water | ||||
| Intervention group | 6.5 | 8.6 | 2.1 | (−1.7, 5.9) |
| Control group | 1.3 | 0.8 | −0.5 | (−3.5, 2.6) |
| Difference | 2.5 | (−2.1, 7.2) | ||
| Bottled water | ||||
| Intervention group | 7.0 | 8.7 | 1.7 | (−1.8, 5.2) |
| Control group | 5.5 | 7.0 | 1.6 | (−1.6, 4.7) |
| Difference | 0.1 | (−4.0, 4.3) | ||
| Unsweetened low− or non−fat milk | ||||
| Intervention group | 0.2 | 1.2 | 1.0 | (−0.5, 2.5) |
| Control group | 1.7 | 1.8 | 0.1 | (−0.9, 1.0) |
| Difference | 0.9 | (−0.7, 2.6) | ||
| Weight status & body mass index (BMI) | ||||
| Overweight/obese statusb | ||||
| Intervention group | 49% | 46% | −3% | (−10%, 3%) |
| Control group | 36% | 38% | 3% | (−4%, 9%) |
| Difference | −6% | (−15%, 3%) | ||
| BMI percentile | ||||
| Intervention group | 67.6 | 68.3 | 0.7 | (−1.3, 2.6) |
| Control group | 78.8 | 78.2 | −0.5 | (−3.6, 2.5) |
| Difference | 1.2 | (−2.5, 4.9) | ||
| Absolute BMI (kg/m2) | ||||
| Intervention group | 16.2 | 16.4 | 0.2 | (−0.1, 0.5) |
| Control group | 17.2 | 17.4 | 0.1 | (−0.2, 0.4) |
| Difference | 0.03 | (−0.2, 0.3) | ||
Notes. BMI, body mass index; CI, confidence interval; SSB, sugar-sweetened beverage. The table shows unstandardized coefficients from generalized linear regressions controlling sociodemographics and, for dietary outcomes and absolute BMI, child’s age and sex. Models accounted for clustering by including classroom fixed effects and clustering standard errors within children. Classroom-level intraclass correlation coefficients (ICCs) ranged from <0.01 to 0.07 and center-level ICCs ranged from <0.01 to 0.02 (see Supplemental Table 3). Bolded coefficients and CIs are statistically significant at p<0.05.
To estimate changes in larger beverage categories (i.e., total water, all healthier beverages, and all less-healthy beverages), we first summed consumption across subcategories (e.g., tap and bottled water), then estimated the generalized linear regressions described above. Changes in consumption of the subcategories do not perfectly sum to the change in consumption of the larger beverage categories due to adjustment for covariates.
Results for proportion overweight/obese are reported as predicted probabilities of being in the overweight/obese category and as marginal effects (i.e., percentage point change in likelihood of being in the overweight/obese category).
Figure 3.
Effects of a healthy beverages intervention on children’s at-home consumption of 11 beverage categories, n=154.
Notes. Figure shows differences in change in consumption from baseline to follow-up, comparing the healthy beverages intervention group to the control group. Differences were estimated using generalized linear regressions, controlling for sociodemographics, child’s age, and child’s sex and accounting for clustering within children and classrooms. Changes in consumption of subcategories may not sum to the changes in larger categories due to adjustment for covariates. *p<0.05
Analyses also suggested that children in the intervention group had larger increases over time in their at-home consumption of healthier beverages than children in the control group. In total, the intervention group showed a larger increase in consumption of healthier beverages (+5.0 ounces/day, 95% CI: 0.5, 9.4) than the control group (+1.5 ounces/day, 95% CI: −2.9. 5.9), though this difference-in-differences was not statistically significant (DD: +3.5 ounces/day, 95% CI: −2.6, 9.5). Total water consumption increased somewhat more in the intervention group compared to the control group (DD: +2.6 ounces/day, 95% CI: −3.2, 8.4), as did consumption of unsweetened low- and non-fat milk (DD: +0.9 ounces/day, 95% CI: −0.7, 2.6), though again these difference-in-differences did not reach statistical significance.
Overweight/obese status and BMI.
At baseline, 43% of children in the intervention group and 39% of children in the control group were overweight/obese (Table 1). After adjusting for covariates, the likelihood of being overweight/obese declined from baseline to follow-up by 3 percentage points in the intervention group and increased by 3 percentage points in the control group (Table 2). Thus, the adjusted difference in changes over time between study groups was −6 percentage points; this difference-in-differences was not statistically significant (95% CI: −15, 3). There were no differences in changes over time in BMI percentile (DD: +1.2 percentiles, 95% CI: −2.5, 4.9) or absolute BMI (DD: +0.03 kg/m2, 95% CI: −0.2, 0.3).
Intervention fidelity.
Data triangulated across several sources suggested good intervention fidelity. First, child care staff served children water during nearly all (88%, n=37) of the 42 spot check fidelity observations the research team conducted during meal and snack times. Second, post-intervention observations conducted using the EPAO instrument indicated good compliance with key components of the intervention. For example, of the three classrooms that served lunch, all served children water with the meal. Three out of the four classrooms that served an afternoon snack served children water with the snack. Additionally, in all four classrooms, children were prompted by teachers to consume water during meals and during playtime. Likewise, in all four classrooms, water was visible to children in the classroom, available for self-serve in the classroom, and available for self-serve during outdoor playtime. None of the observed intervention classrooms served juice at any meal or snack, and none served any milk other than unsweetened low- or non-fat milk. One area where centers could have improved was serving water with breakfast: of the three classrooms that served breakfast, only one served children water with the meal. Finally, data also suggested parents were engaged with the intervention. More than half of parents (58% of the 81 parents participating in the intervention) returned signed behavioral contracts to the research team indicating which beverage rules they planned to implement at home.
Discussion
We found that compared to a control group, children exposed to a focused healthy beverages intervention significantly decreased their consumption of less-healthy beverages. Children in the healthy beverages intervention also increased their consumption of healthier beverages compared to the control group, though these relative improvements were not statistically significant. Effects on overweight/obese status were favorable but also nonsignificant. Beverage consumption is a major contributor to childhood obesity(6,7) and early childhood is increasingly recognized as a critical period for establishing both healthy dietary behaviors and a healthy body weight(42). This is among the first interventions delivered via child care centers to focus exclusively and comprehensively on encouraging children to consume water and unsweetened low or non-fat milk in place of SSBs and 100% juice(20,21).
The intervention showed promise at increasing consumption of both water and unsweetened low- or non-fat milk, the beverages promoted by the intervention. Children in the intervention group increased their at-home water consumption by 2.6 ounces/day more than the control group. In addition to helping limit excess weight gain(9,10), this increase in water intake could potentially reduce children’s risk of inadequate hydration(43) and improve their cognitive functioning(44–47). Children in the intervention group also increased their at-home consumption of unsweetened low- or non-fat milk by about one ounce/day relative to the control group. Consumption of unsweetened low- or non-fat milk helps children meet recommended levels of calcium, potassium, and vitamin D intake while avoiding the excess sugar, saturated fat, and calories found in high-fat and sweetened milk(48).
The intervention also helped children limit their at-home consumption of the less-healthy beverages discouraged by the intervention. The intervention significantly reduced juice consumption and was also associated with a relatively large though nonsignificant reduction in SSB consumption. Reduced consumption of juice and SSBs could help children maintain a healthier weight(6,7) and may also reduce their risk of dental caries(49), diabetes, hyperlipidemia, and fatty liver disease(51). Consumption of high-fat milk also decreased in the intervention group relative to the control group, though not significantly. In total, the intervention significantly reduced children’s at-home consumption of all less-healthy beverages combined by nearly 6 ounce/day relative to the control group.
If sustained, this observed reduction in consumption of less-healthy beverages could help children maintain healthier weights. To contextualize the potential benefits of these changes in beverage intake, we used the United States Department of Agriculture’s online nutrition database Supertracker(52) to translate intervention impact on volume of beverages consumed into impact on calories and added sugar consumed (Supplemental Table 4). We summed intervention impacts across all beverage categories, accounting for both decreases in beverages like SSBs and juice as well as increases in beverages like unsweetened low- or non-fat milk. Assuming no other dietary changes, the intervention was estimated to help children avert more than 60 calories per day, well above the amount needed to achieve Healthy People 2020 goals for obesity prevalence among young children(53). The observed changes in beverage consumption could also result in children consuming nearly six fewer grams of added sugar per day, a notable finding given that 2–5 year-olds consume more than twice the daily recommended amount of added sugar(51).
Despite these encouraging changes in children’s beverage consumption habits, we did not observe statistically significant intervention effects on overweight/obese status, likely due to the study’s short duration and small sample size. One systematic review of childhood obesity prevention interventions suggested that follow-up periods of 7.5 months or longer may be needed to demonstrate changes in weight status(54). Future studies should follow children for a longer period to determine whether the improvements seen in beverage intake are sustained, and whether such changes ultimately impact children’s weight.
We note several limitations. First, while trained staff objectively measured height and weight, dietary behaviors were self-reported. Second, because our objective was to determine the promise of this intervention, we employed a relatively short follow-up period, and it is not clear if the observed changes in beverage consumption would be sustained over time. We also measured only children’s at-home beverage consumption, and did not assess their behaviors while at child care, meaning that we likely underestimated children’s total beverage consumption, particularly for children attending full-day child care programs. We also did not assess food intake, and cannot determine whether children compensated for any reductions in calorie intake from beverages by increasing their calorie intake from foods. Additionally, we recruited a relatively small sample of mostly low-income, Hispanic families from a convenience sample of four child care centers in a limited geographical area and our findings may not generalize to samples with different sociodemographic characteristics or in different geographic areas. Future studies should examine multi-pronged beverage-focused interventions in other populations, with longer follow-up periods, and with larger samples. Additional research could also help determine whether parents and child care centers can maintain the intervention’s environmental and policy changes in the absence of a research study(55).
There are several unique strengths to this pilot study. We designed a theory-informed intervention that simultaneously targeted factors at the child-, home-, and organizational social ecological levels. The multi-pronged intervention included a variety of creative strategies to address these multiple levels, including hands-on, engaging educational activities for both children and parents; meaningful environmental changes to promote children’s access to water and reduce their access to juice and SSBs, both while at home and at child care; and policy and rule changes across the two contexts. We also conducted regular in-person spot check fidelity observations to ensure child care centers’ compliance with the intervention, finding that child care staff were largely implementing the intervention as intended. Finally, this is among the first interventions focused intensively on improving young children’s beverage consumption as an obesity prevention strategy. Many effective obesity prevention interventions for young children have targeted both nutrition and physical activity simultaneously(56–65). This study suggests that focusing more narrowly on beverages may provide a simple yet effective means of promoting healthy weight in young children.
Conclusions
We developed and evaluated a beverage-focused intervention that targeted children, parents, and child care center staff using a variety of strategies. Our results suggest that such interventions have promise for improving children’s at-home beverage consumption and weight outcomes. Future studies should examine children over longer periods, include a larger number of child care centers serving diverse populations, and assess both food and beverage intake at child care centers as well as at home.
Supplementary Material
Acknowledgments:
We thank Keren Eyal, Maria Martin, Céline Stamets, Kiah Thorne, and Meagan Treviño for assistance with data collection and Emily Altman for assistance with data management.
Financial Support: This study was supported by a grant from the National Institutes of Health (K23 HD067305 to AIP). General support and training support for AHG were provided by the Carolina Population Center (P2C HD050924, T32 HD007168). AAH was supported through the Johns Hopkins Center for a Livable Future – Lerner Fellowship. CDB was supported in part by grants from the Maternal and Child Health Bureau, Health Resources and Services Administration, USDHHS (U45MC27709 and UA6MC27378) to the Division of Adolescent and Young Adult Medicine, Department of Pediatrics, University of California San Francisco. The funders had no role in the study design; the collection, analysis, or interpretation of the data; the writing of the report; or the decision to submit the manuscript for publication.
Trial registration for this study is available at ClinicalTrials.gov (). The Committee on Human Research at the University of California San Francisco approved this study.
Footnotes
Conflicts of Interest: None.
Ethical Standards Disclosure: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Committee on Human Research at the University of California San Francisco. Written informed consent was obtained from all subjects.
References
- 1.Skinner AC, Ravanbakht SN, Skelton JA, et al. (2018) Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Must A & Strauss RS (1999) Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord 23, s2. [DOI] [PubMed] [Google Scholar]
- 3.Reilly JJ & Kelly J (2011) Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int J Obes 35, 891–898. [DOI] [PubMed] [Google Scholar]
- 4.Ebbeling CB, Feldman HA, Chomitz VR, et al. (2012) A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med 367, 1407–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Ruyter JC, Olthof MR, Seidell JC, et al. (2012) A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med 367, 1397–1406. [DOI] [PubMed] [Google Scholar]
- 6.Malik V, Pan A, Willett WC, et al. (2013) Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am J Clin Nutr 98, 1084–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auerbach BJ, Wolf FM, Hikida A, et al. (2017) Fruit juice and change in BMI: A meta-analysis. Pediatrics 139, e20162454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sonneville Kendrin R, Long Michael W, Rifas Shiman Sheryl L, et al. (2014) Juice and water intake in infancy and later beverage intake and adiposity: Could juice be a gateway drink? Obes 23, 170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muckelbauer R, Libuda L, Clausen K, et al. (2009) Promotion and provision of drinking water in schools for overweight prevention: Randomized, controlled cluster trial. Pediatrics 123, e661–e667. [DOI] [PubMed] [Google Scholar]
- 10.Wang YC, Ludwig DS, Sonneville K, et al. (2009) Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med 163, 336–43. [DOI] [PubMed] [Google Scholar]
- 11.Story M (2013) Recommendations for Healthier Beverages. Robert Wood Johnson Foundation. [Google Scholar]
- 12.National Academies of Sciences, Engineering, and Medicine (2017) Strategies to Limit Sugar-Sweetened Beverage Consumption in Young Children: Proceedings of a Workshop. National Academies Press. [PubMed] [Google Scholar]
- 13.Heyman MB & Abrams SA (2017) Fruit juice in infants, children, and adolescents: Current recommendations. Pediatrics 136, e20170967. [DOI] [PubMed] [Google Scholar]
- 14.Patel AI, Moghadam SD, Freedman M, et al. (2018) The association of flavored milk consumption with milk and energy intake, and obesity: A systematic review. Prev Med 111, 151–162. [DOI] [PubMed] [Google Scholar]
- 15.Briefel RR, Wilson A, Cabili C, et al. (2013) Reducing calories and added sugars by improving children’s beverage choices. J Acad Nutr Diet 113, 269–275. [DOI] [PubMed] [Google Scholar]
- 16.Bleich SN, Vercammen KA, Koma JW, et al. (2018) Trends in beverage consumption among children and adults, 2003–2014. Obes 26, 432–441. [DOI] [PubMed] [Google Scholar]
- 17.Kit BK, Fakhouri TH, Park S, et al. (2013) Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr 98, 180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kay MC, Welker EB, Jacquier EF, et al. (2018) Beverage consumption patterns among infants and young children (0–47.9 months): Data from the Feeding Infants and Toddlers Study, 2016. Nutrients 10, 825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ChildCare Aware of America (2018) About Child Care. http://usa.childcareaware.org/families-programs/about-child-care/.
- 20.Cradock A, Poole M, Agnew K, et al. (In press) A systematic review of strategies to increase drinking water access and consumption among 0- to 5-year olds. Obes Rev. [DOI] [PubMed] [Google Scholar]
- 21.Vercammen K, Frelier J, Lowery C, et al. (2018) A systematic review of strategies to reduce sugar-sweetened beverage consumption among 0‐year to 5‐year olds. Obes Rev 19, 1504–1524. [DOI] [PubMed] [Google Scholar]
- 22.Kenney EL, Gortmaker SL, Carter JE, et al. (2015) Grab a cup, fill it up! An intervention to promote the convenience of drinking water and increase student water consumption during school lunch. Am J Public Health 105, 1777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elbel B, Mijanovich T, Abrams C, et al. (2015) A water availability intervention in New York City public schools: Influence on youths’ water and milk behaviors. Am J Public Health 105, 365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel AI, Grummon AH, Hampton KE, et al. (2016) A trial of the efficacy and cost of water delivery systems in San Francisco Bay Area middle schools, 2013. Prev Chronic Dis 13, E88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwartz AE, Leardo M, Aneja S, et al. (2016) Effect of a school-based water intervention on child body mass index and obesity. JAMA Pediatrics 170, 220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.California Department of Social Services (2018) Child Care Licensing. California Department of Social Services. http://www.cdss.ca.gov/inforesources/Child-Care-Licensing (accessed July 2017). [Google Scholar]
- 27.Yaktine A & Moats S (2011) Child and Adult Care Food Program: Aligning dietary guidance for all. Food and Nutrition Board, Institute of Medicine of the National Academies. [PubMed] [Google Scholar]
- 28.Story M, Kaphingst KM, Robinson-O’Brien R, et al. (2008) Creating healthy food and eating environments: Policy and environmental approaches. Annu Rev Public Health 29, 253–272. [DOI] [PubMed] [Google Scholar]
- 29.Sallis J, Owen N & Fisher EB Ecological Models of Health Behavior In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed., pp. 465–485. San Francisco, CA: Jossey-Bass. [Google Scholar]
- 30.Environmental Protection Agency (2017) Lead and Copper Rule. Drinking Water Requirements for States and Public Water Systems. https://www.epa.gov/dwreginfo/lead-and-copper-rule (accessed May 2018). [Google Scholar]
- 31.Brownley J (2010) Child day care facilities: nutrition. Health and Safety Code, vol. 1596.808. [Google Scholar]
- 32.Lee DL, Gurzo K, Yoshida S, et al. (2018) Compliance with the New 2017 Child and Adult Care Food Program Standards for Infants and Children before Implementation. Child Obes 14, 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson H, Linchey J & Madsen K (2015) Critical elements of a school report to parents on body mass index. Prev Chronic Dis 12, E136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zamenes A (2014) Drink More Water! https://www.youtube.com/watch?v=QrWquDo7TzE (accessed March 2019).
- 35.Singh S (2012) Potter the Otter: A Tale About Water. United States: FIRST 5 Santa Clara County. [Google Scholar]
- 36.Cole TJ, Faith MS, Pietrobelli A, et al. (2005) What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Eur J Clin Nutr 59, 419. [DOI] [PubMed] [Google Scholar]
- 37.Berkey CS & Colditz GA (2007) Adiposity in adolescents: Change in actual BMI works better than change in BMI z-score for longitudinal studies. Ann Epidemiol 17, 44–50. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (2007) National Health and Nutrition Examination Survey (NHANES) Anthropometry Manual. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- 39.Centers for Disease Control and Prevention, National Center for Health Statistics (2000) CDC growth charts: United States. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- 40.Grummon AH, Hampton KE, Hecht A, et al. (2017) Validation of a brief questionnaire against direct observation to assess adolescents’ school lunchtime beverage consumption. J Nutr Educ Behav 49, 847–851.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ward D, Hales D, Haverly K, et al. (2008) An instrument to assess the obesogenic environment of child care centers. Am J Health Behav 32, 380–386. [DOI] [PubMed] [Google Scholar]
- 42.Birch L, Parker L & Burns A (editors) (2011) Early Childhood Obesity Prevention Policies. Washington, DC: National Academies Press. [Google Scholar]
- 43.Kenney EL, Long MW, Cradock AL, et al. (2015) Prevalence of inadequate hydration among US children and disparities by gender and race/ethnicity: National Health and Nutrition Examination Survey, 2009–2012. Am J Public Health 105, e113–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Benton D & Burgess N (2009) The effect of the consumption of water on the memory and attention of children. Appetite 53, 143–146. [DOI] [PubMed] [Google Scholar]
- 45.D’Anci KE, Constant F & Rosenberg IH (2006) Hydration and cognitive function in children. Nutr Rev 64, 457–464. [DOI] [PubMed] [Google Scholar]
- 46.Masento NA, Golightly M, Field DT, et al. (2014) Effects of hydration status on cognitive performance and mood. Br J Nutr 111, 1841–1852. [DOI] [PubMed] [Google Scholar]
- 47.Edmonds CJ & Jeffes B (2009) Does having a drink help you think? 6–7-year-old children show improvements in cognitive performance from baseline to test after having a drink of water. Appetite 53, 469–472. [DOI] [PubMed] [Google Scholar]
- 48.United States Department of Health and Human Services & United States Department of Agriculture (2015) Dietary Guidelines for Americans 2015–2020. 8th Edition.. [Google Scholar]
- 49.Marshall TA, Levy SM, Broffitt B, et al. (2003) Dental caries and beverage consumption in young children. Pediatrics 112, e184–191. [DOI] [PubMed] [Google Scholar]
- 50.Malik VS, Popkin BM, Bray GA, et al. (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care 33, 2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vos MB, Kaar JL, Welsh JA, et al. (2017) Added sugars and cardiovascular disease risk in children: A scientific statement from the American Heart Association. Circulation 135, e1017–e1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.United States Department of Agriculture (2018) Food-A-Pedia Supertracker. https://www.supertracker.usda.gov/foodapedia.aspx?CatgoryID=−1&FoodDescription=soda (accessed June 2018). [Google Scholar]
- 53.Wang YC, Hsiao A, Orleans CT, et al. (2013) The Caloric Calculator: Average caloric impact of childhood obesity interventions. Am J Prev Med 45, e3–e13. [DOI] [PubMed] [Google Scholar]
- 54.Bluford DAA, Sherry B & Scanlon KS (2007) Interventions to prevent or treat obesity in preschool children: A review of evaluated programs. Obes 15, 1356–1372. [DOI] [PubMed] [Google Scholar]
- 55.Glasgow RE, Vogt TM & Boles SM (1999) Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am J Public Health 89, 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alkon A, Crowley AA, Neelon SEB, et al. (2014) Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health 14, 215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fitzgibbon ML, Stolley MR, Schiffer L, et al. (2005) Two-year follow-up results for Hip-Hop to Health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 146, 618–625. [DOI] [PubMed] [Google Scholar]
- 58.Eliakim A, Nemet D, Balakirski Y, et al. (2007) The effects of nutritional-physical activity school-based intervention on fatness and fitness in preschool children. J Pediatr Endocrinol Metab 20, 711–718. [DOI] [PubMed] [Google Scholar]
- 59.Puder JJ, Marques-Vidal P, Schindler C, et al. (2011) Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): Cluster randomised controlled trial. BMJ 343, d6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zask A, Adams JK, Brooks LO, et al. (2012) Tooty Fruity Vegie: An obesity prevention intervention evaluation in Australian preschools. Health Promot J Austr 23, 10–15. [DOI] [PubMed] [Google Scholar]
- 61.De Coen V, De Bourdeaudhuij I, Vereecken C, et al. (2012) Effects of a 2-year healthy eating and physical activity intervention for 3–6-year-olds in communities of high and low socio-economic status: The POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutr 15, 1737–1745. [DOI] [PubMed] [Google Scholar]
- 62.Herman A, Nelson BB, Teutsch C, et al. (2012) “Eat healthy, stay active!”: A coordinated intervention to improve nutrition and physical activity among head start parents, staff, and children. Am J Health Promot 27, e27–e36. [DOI] [PubMed] [Google Scholar]
- 63.Yin Z, Parra-Medina D, Cordova A, et al. (2012) Míranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child Obes 8, 429–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhou Z, Ren H, Yin Z, et al. (2014) A policy-driven multifaceted approach for early childhood physical fitness promotion: Impacts on body composition and physical fitness in young Chinese children. BMC Pediatrics 14, 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Salazar G, Vasquez F, Concha F, et al. (2014) Pilot nutrition and physical activity intervention for preschool children attending daycare centres (JUNJI): Primary and secondary outcomes. Nutr Hosp 29, 1004–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.