Abstract
Background:
Early-life exposure to traffic-related air pollution may decrease fetal growth and increase childhood obesity risk. Our objective was to evaluate the relationship of early-life exposure to traffic-related air pollution with birthweight in term newborns and obesity at age 7-8 years in two prospective birth cohorts in Cincinnati, OH (the Health Outcomes and Measures of the Environment (HOME) Study and Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS)).
Methods:
We estimated elemental carbon attributable to traffic (ECAT) exposure at residential addresses during pregnancy with a validated land use regression model. We assessed birthweight among term infants using birth records or parent report (HOME Study n= 333 and CCAAPS n=590). We measured children’s weight and height at 7-8 years, and calculated age- and sex-specific BMI z-scores (HOME Study n= 198 and CCAAPS n=459). Using multivariable linear regression, we estimated the difference in term birthweight and BMI z-score per interquartile range (IQR) increase in ECAT concentrations in each cohort separately and in the pooled sample.
Results:
In adjusted models, ECAT exposure was not associated with lower birthweight (pooled sample β: 30g; 95% CI: −6, 66), or with higher BMI z-score (pooled sample β: −0.04; 95% CI: −0.15, 0.08). Infant sex modified the association between ECAT and birthweight (p=0.05). Among male newborns, higher ECAT concentrations were associated with higher birthweight (β: 61g; 95% CI: 9, 113), but we observed no association among female newborns (β: −9g; 95% CI: −58, 41).
Conclusions:
In contrast to some prior studies, early-life traffic-related air pollution exposure was not associated with lower birthweight or increased childhood adiposity in these two cohorts.
INTRODUCTION
Childhood obesity, a serious public health concern, has several risk factors, including genetics and socioeconomic characteristics, as well as exposure to environmental obesogens.1–3 One obesogen is ambient air pollution exposure, which is associated with weight status and patterns of weight gain throughout gestation, infancy, and childhood.4–15 Pre- and postnatal exposure to ambient and traffic-related air pollution has been shown to contribute to low birthweight and fetal growth restriction, greater infant weight gain, and excess childhood adiposity.6–8,10,12–14,16–19 Infants born low birthweight (< 2500 g) have an increased risk for infant mortality as well as cardiovascular disease and diabetes in adulthood.20–23 Furthermore, excess childhood adiposity is associated with adulthood obesity which increases mortality risk.24–26
Recent analyses suggest that the potential effect of traffic-related air pollution exposure on obesity risk varies for infants and children living near freeways versus non-freeways, leading researchers to hypothesize that specific traffic patterns and mixtures of vehicular exhaust may be independently associated with obesity risk.16,27 Identifying those vehicle types and roadway designs that present the greatest public health threat can guide effective intervention strategies.
Diesel traffic, which occurs at higher volumes on freeways, generates a higher concentration of fine and ultrafine particulates compared with gasoline engines, potentially posing a greater threat to the developing fetus and child’s health.28,29 Using a previously validated diesel source profile and land use regression model, we estimated a sensitive measure of traffic-related air pollution exposure from diesel combustion, elemental carbon attributable to traffic sources (ECAT), across different roadway classifications in the city of Cincinnati.30 Compared to elemental carbon exposure estimates used in previous studies, this novel ECAT measure may provide a better estimate of exposure to the hazardous fine particulates generated by diesel engines. We used this measure to investigate the relationship of residential traffic-related air pollution exposure during early-life with birthweight and childhood adiposity at age 7–8 years in the Health Outcomes and Measures of the Environment (HOME) Study and Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS). We hypothesized that higher residential ECAT exposure during early-life is associated with lower birthweight and higher childhood adiposity at school age.
METHODS
Study Participants
From March 2003 to January 2006, we recruited HOME Study participants from nine prenatal care clinics associated with three delivery hospitals in the greater Cincinnati, OH metropolitan area.31 To be eligible, women had to be living in the study region, 16 ± 3 weeks gestation, ≥ 18 years of age, residing in a home built in 1978 or prior, not living in a mobile or trailer home, HIV-negative, not taking medications for seizures or thyroid disorders, planning to continue prenatal care and deliver at the collaborating clinics and hospitals, planning to remain in the greater Cincinnati area for the next year, and fluent in English.31 Additionally, women could not have a diagnosis of any of the following disorders: diabetes, bipolar, schizophrenia, or cancer that resulted in radiation treatment or chemotherapy. Approval for the study was obtained from the institutional review boards of Cincinnati Children’s Hospital Medical Center and the participating delivery hospitals. Women provided written informed consent after study protocols were explained by trained research assistants.
We recruited CCAAPS study participants from the greater Cincinnati area using birth certificate data from 2001 to 2003. To be eligible, newborns had to reside at their time of birth either < 400 m or > 1500m from a major roadway (defined as > 1000 trucks daily), be > 35 weeks gestation at delivery, and have at least one atopic parent.30 The University of Cincinnati Institutional Review Board approved this study and all enrolled parents gave written informed consent before their own and their infants’ study participation.
Of 407 and 762 infants in the HOME Study and CCAAPS, respectively, we excluded twin pregnancies (n=18 for HOME; n=32 for CCAAPS), children born < 37 weeks gestation (HOME, n= 37; CCAAPS, n=33), those missing exposure information (HOME, n=17), covariates (HOME, n=2; CCAAPS, n=75), and those missing birthweight or gestational age (CCAAPS, n=32). For our main analyses, we excluded preterm infants (< 37 weeks) to reduce the effect of gestational age on birthweight and facilitate comparison between the two cohorts and with previous studies. The sample size for the analysis of birthweight was n=333 for the HOME Study and n=590 for CCAAPS. A total of n=198 (HOME) and n=459 (CCAAPS) children returned for the age 7–8 year follow up and had anthropometry data available for our analysis of childhood adiposity (see Figure, Supplemental Digital Content 1, flow diagram of participants included in each cohort and analysis). Due to differences in recruitment periods between the HOME Study and CCAPS, there is no overlap in the participants enrolled in both cohorts. We were not able to assess if siblings were enrolled in both studies.
Exposure Assessment
We used a previously validated land use regression (LUR) model (R² = 0.75) to estimate ECAT concentrations at each participant’s baseline address (at ~20 weeks gestation for HOME and ~6 months of age for CCAAPS).30 Briefly, between 2001 to 2006, research staff conducted ambient air sampling on a rotating basis across 24 sampling sites in the greater Cincinnati, OH region (see Figure, Supplemental Digital Content 2, with the geographical overlap in cohorts and air sampling locations).30 First, we quantified the concentration of particulate matter (PM2.5). Next, we analyzed the filters using X-ray fluorescence to determine the concentration of 39 elements and thermal-optical transmittance to quantify elemental and organic carbon concentrations. We used a multivariate receptor model, UNMIX, to determine traffic sources contributing to the total PM2.5 concentrations. We identified a diesel-specific traffic signature using elemental source profiles from separate samples obtained at cluster sources and used this signature to quantify the contribution of diesel traffic to the PM2.5 concentrations collected at each sampling site.32 For each sampling site, we calculated the concentration of elemental carbon generated from traffic-related diesel combustion (μg/m3) and constructed the land use regression model.30,32,33 Because the land use regression model was developed using the arithmetic mean of all 24-hour samples collected at each site, the ECAT concentrations were estimates of long-term exposure and did not incorporate temporal variations in exposure.30 We used the ECAT concentration at the residential address as an estimate of children’s early-life exposure to traffic-related air pollution.
Infant and Child Anthropometry
We abstracted the birthweight and gestational age of children from birth records in the HOME Study and relied on maternal report in CCAAPS. Trained research assistants measured weight and height when children were approximately 7–8 years of age in the HOME Study (range: 7.5–10y) and CCAAPS (range: 6.4–7.9y). Using WHO reference data (WHO, 2017), we calculated age and sex-specific body mass index (BMI) z-scores.34
Covariates
We collected sociodemographic and prenatal variables that may be related to both early-life ECAT concentrations and fetal or childhood growth. We identified potential confounders of the relationship of ECAT concentrations with fetal growth or child anthropometry a priori based on existing literature and constructed directed acyclic graphs to visualize confounding relationships (see Figure, Supplemental Digital Content 3 and Supplemental Digital Content 4, which illustrates variables confounding the association of ECAT with birthweight and childhood BMI).35,36 We assessed sociodemographic characteristics using standardized interviews administered at baseline; these included maternal race, marital status, age at delivery, education, and household income. The HOME Study assessed marital status at birth, while CCAAPS assessed marital status during late childhood.
We measured perinatal factors by medical chart review (HOME) or self-report (CCAAPS). These included: parity, maternal tobacco smoke exposure, maternal pre-pregnancy BMI, and weight gain during pregnancy. Prenatal smoking status was assessed by self-report (HOME & CCAAPS) and confirmed via serum cotinine concentrations in the HOME Study. The HOME Study collected parity while CCAAPS reported the number of children living at home under 18 years of age, which we used as a proxy for parity. The HOME Study abstracted maternal pre-pregnancy weight from medical charts and we used this to calculate pre-pregnancy BMI. CCAAPS did not collect information about maternal weight pre- or post-pregnancy. Thus, we were not able to adjust for pre-pregnancy BMI in the CCAAPS or pooled analyses. In CCAAPS, women self-reported the amount of weight gained during pregnancy and in HOME we abstracted this information from medical chart reviews.
Statistical Analysis
We used multivariable linear regression to evaluate the association of ECAT concentrations with a) birthweight or b) child BMI z-score at age 7–8 years in each cohort separately and in the pooled sample. In regression models we adjusted for maternal race, household income, maternal age at delivery, maternal education, parity, maternal exposure to tobacco, weight gain during pregnancy, and maternal pre-pregnancy BMI. In the multivariable linear regression with birthweight as the outcome we also adjusted for child sex. In each cohort we considered ECAT as both a continuous and categorical variable (terciles). We used restricted cubic splines to assess the linearity of the dose-response relationship of ECAT and birthweight or BMI z-scores. We did not adjust for birthweight in the analyses of BMI z-score at age 7–8 years because birthweight is on the causal pathway between ECAT exposure and childhood BMI.
Before pooling the cohorts, we assessed if the association of ECAT concentration with birthweight or BMI differed between cohorts. First, we assessed cohort heterogeneity by including terms for continuous ECAT concentrations, cohort, and their interaction term in adjusted models. Next, we compared multivariable models adjusting for cohort as a fixed effect to models adjusting for a random cohort effect (results not shown). For multivariable linear regression models in the pooled sample, we adjusted for cohort and covariates that were available in both cohorts.
We assessed the robustness of our models by comparing effect estimates from our final adjusted models with those from regression models not adjusting for maternal weight gain or pre-pregnancy BMI. We also conducted a sensitivity analysis including HOME Study infants born < 37 weeks gestation in our analysis and adjusting for gestational age in the regression model. We were not able to conduct this sensitivity analysis in CCAAPS because infants born prior to 35 weeks were not enrolled in the study.
In addition, we conducted secondary analyses examining whether associations of ECAT with birthweight or childhood BMI varied by maternal race (non-Hispanic White or non-Hispanic Black and Other Races), child sex, or household income (categorized as < $40,000 and > $40,000) in the individual cohorts and pooled sample. We first stratified participants based on maternal race, child sex, or household income and used adjusted linear regression models to estimate the relationship of ECAT with birthweight or BMI in each strata. Second, we assessed modification of the association between ECAT and each outcome by including a product interaction term between ECAT and the modifier of interest in a fully adjusted model. All analyses were performed using SAS v.9.4 (SAS Institutes, Inc.; Cary, NC) and R version 3.4.0 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
At baseline, the 923 participants included in this analysis across both cohorts were predominately non-Hispanic white (73%), age 25 – 35 years at time of delivery (59%), and non-smokers (89%), with a household income greater than $70,000 (37%), bachelor’s degree or higher (51%), and previous child (61%) (Table 1). Compared with the HOME Study, a greater proportion of CCAAPS participants were non-Hispanic white, multiparous, and gained more weight during pregnancy. Excluded HOME Study participants born < 37 weeks gestation were less likely to be non-Hispanic White compared to HOME Study participants included in our analysis (38% compared to 65%). Furthermore, excluded participants (n=37) had a lower median income than HOME Study participants included in the analysis (median=$40,000; 25th, 75th percentile=$17,500, $75,000 vs median=$55,000; 25th, 75th percentile=$22,500, $85,000), but had similar residential ECAT concentrations. There was not a difference in birthweight or BMI z-scores at age 7–8 years between the HOME Study and CCAAPS (see Table, Supplemental Digital Content 5, which contains birthweight and BMI z-score summary statistics for both cohorts). Overall, the mean birthweight in the pooled sample was 3,487g (SD = 479) and the mean BMI z-score was 0.56 (SD=1.29). The baseline characteristics of women who completed the follow-up visit when children were age 7–8 years old were similar to the full cohorts (Table 1).
Table 1.
Maternal characteristics at baseline and follow-up at age 7-8 years among the HOME Study and CCAAPS Participants
| HOME | CCAAPS | |||
|---|---|---|---|---|
| Demographic Characteristic | Baseline n (%) |
Follow-up n (%) |
Baseline n (%) |
Follow-up n (%) |
| Total | 333 (100) | 198 (100) | 590 (100) | 459 (100) |
| Maternal Race | ||||
| Non-Hispanic White | 217 (65) | 121 (61) | 459 (78) | 359 (78) |
| Non-Hispanic Black /Other | 116 (29) | 77 (39) | 131 (20) | 100 (22) |
| Maternal Age at Delivery | ||||
| ≤ 25 years | 72 (22) | 49 (25) | 153 (26) | 115 (25) |
| > 25 - 35 years | 208 (62) | 121 (61) | 341 (58) | 268 (58) |
| > 35 years | 53 (16) | 28 (14) | 96 (16) | 76 (17) |
| Marital Status | ||||
| Married | 220 (66) | 122 (61) | 218 (83) | 208 (83) |
| Not Married | 113 (34) | 76 (38) | 44 (17) | 43 (17) |
| Household Income | ||||
| > $70,000 | 128 (38) | 71 (36) | 216 (36) | 183 (40) |
| $40,000 - 70,000 | 79 (24) | 44 (22) | 175 (30) | 126 (27) |
| $20,000 - 39,999 | 53 (16) | 29 (15) | 101 (17) | 76 (17) |
| < $20,000 | 73 (22) | 54 (27) | 98 (17) | 74 (16) |
| Maternal Education | ||||
| Bachelor’s Degree or Higher | 171 (51) | 93 (47) | 298 (51) | 241 (53) |
| Tech/ Some College | 85 (26) | 55 (28) | 157 (27) | 116 (25) |
| High School or Less | 77 (23) | 50 (25) | 135 (23) | 102 (22) |
| Infant Gender | ||||
| Male | 153 (46) | 87 (44) | 316 (54) | 248 (54) |
| Female | 180 (54) | 111 (56) | 274 (46) | 211 (46) |
| Parity | ||||
| 0 | 148 (44) | 90 (45) | 217 (37) | 163 (36) |
| 1+ | 185 (56) | 108 (55) | 373 (63) | 296 (64) |
| Maternal Smoking Status | ||||
| Smoker | 38 (11) | 24 (12) | 67 (11) | 44 (10) |
| Non-Smoker | 295 (89) | 174 (88) | 523 (89) | 415 (90) |
| Maternal Weight Gain During Pregnancy | ||||
| ≤ 25 lbs. | 118 (35) | 74 (37) | 189 (32) | 146 (32) |
| > 25 - 35 lbs. | 128 (38) | 68 (34) | 147 (25) | 114 (25) |
| ≥ 35 lbs. | 87 (26) | 56 (28) | 254 (43) | 199 (43) |
Abbreviations: HOME, Health Outcomes and Measures of the Environment; CCAAPS, Cincinnati Childhood and Air Pollution Study.
ECAT concentrations estimated at residential addresses were comparable across the two cohorts, (HOME median= 0.37 μg/m3; 25th, 75th percentile=0.30, 0.46 μg/m3 vs CCAAPS median=0.35 μg/m3; 25th, 75th percentile=0.30, 0.42 μg/m3; Figure 1). Pooled ECAT concentrations had an interquartile range (IQR) of 0.15 μg/m3 (pooled 25th and 75th percentile: 0.30, 0.45). Across both cohorts, median ECAT concentrations were higher among women who were unmarried; non-Hispanic black or other race; younger than 25 years of age; had an annual household income < $20,000; had a high school diploma, GED, or less; or smoked tobacco during pregnancy (see Table, Supplemental Digital Content 6, with descriptive statistics for ECAT concentrations).
Figure 1. Bean plot of the distribution of elemental carbon attributable to traffic (ECAT) concentrations among the HOME Study and CCAAPS.
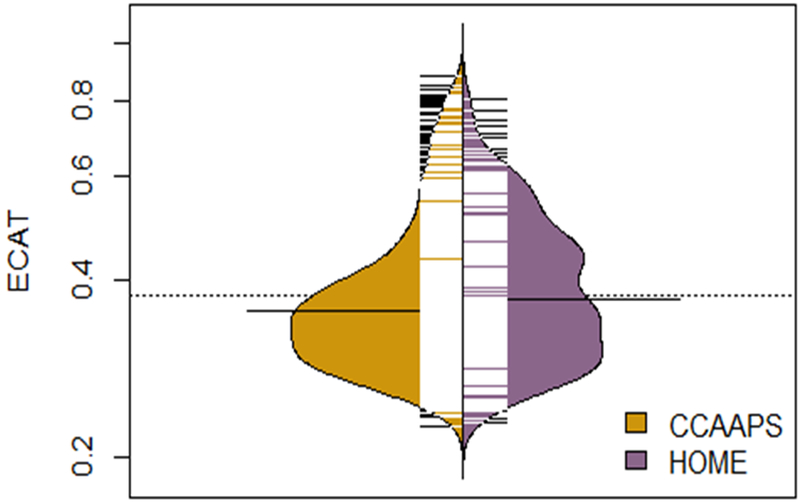
ECAT concentration (μg/m3) is on a natural-log y-axis. Each black and white mark represents a study participant and the bold black lines near the center indicate median concentrations in each cohort.
HOME, Health Outcomes and Measures of the Environment; CCAAPS, Cincinnati Childhood and Air Pollution Study
In both the individual cohort and pooled analyses, linearity tests using restricted cubic splines suggested ECAT concentrations had a linear relationship with both birthweight and BMI z-scores (results not shown, all non-linearity p-values > 0.45).
In adjusted models, residential ECAT concentrations were not associated with birthweight in the HOME Study (difference per IQR increase in ECAT: 34g; 95% CI: −28, 95), CCAAPS (difference per IQR increase in ECAT: 20g; 95% CI: −23, 62), or the pooled sample (difference in birthweight: 30g; 95% CI: −6, 66). Nor did we find evidence of an association between residential ECAT concentrations and BMI z-score at age 7–8 years in the HOME Study (difference per IQR increase in ECAT: −0.07; 95% CI: −0.27, 0.13), CCAAPS (difference per IQR increase in ECAT: −0.02; 95% CI: −0.16, 0.12), or the pooled sample (difference per IQR increase in ECAT: −0.04; 95% CI: −0.15, 0.08). Similarly, we found no association between residential ECAT concentrations and birthweight or BMI z-scores when we categorized ECAT concentrations into terciles (Table 2 and Table 3). Results from models adjusting for cohort as a fixed effect were similar to those adjusting for a random cohort effect (results not shown). Furthermore, cohort did not modify the association between ECAT and birthweight or BMI (cohort and ECAT interaction term p-values = 0.83 and 0.28, for birthweight and BMI z-score analyses, respectively).
Table 2.
Adjusted difference in term birthweight across ECAT concentration terciles and per interquartile range increase in ECAT concentration (HOME Study and CCAAPS)
| HOME | CCAAPS | Pooled Sample | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ECAT Measure |
n | Difference (grams) |
95% CI | n | Difference (grams) |
95% CI | n | Difference (grams) |
95% CI |
| 1st Tercile | 111 | ref. | 196 | ref. | 307 | ref. | |||
| 2nd Tercile | 111 | −67 | (−186, 52) | 197 | 20 | (−66, 105) | 308 | 7 | (−65, 78) |
| 3rd Tercile | 111 | 8 | (−113, 129) | 197 | −29 | (−118, 59) | 308 | 17 | (−57, 91) |
| Per IQR | 333 | 34 | (−28, 95) | 590 | 20 | (−23, 62) | 923 | 30 | (−6, 66) |
Individual cohort models adjusted for maternal race (categorical), household income (continuous), maternal age at delivery (continuous), maternal education (categorical), parity (categorical), maternal exposure to tobacco (HOME Study: cotinine level (continuous) and CCAAPS: Non-smokers and Smokers (categorical), weight gain during pregnancy (continuous), and child sex (categorical). HOME model also adjusted for maternal pre-pregnancy BMI (continuous).
Pooled sample models adjusted for cohort (categorical), maternal race (categorical), household income (categorical), maternal age at delivery (continuous), maternal education (categorical), parity (categorical), smoking status (categorical: non-smokers and smokers), weight gain during pregnancy (continuous), and child sex (categorical).
ECAT and cohort interaction p-value = 0.83
Pooled ECAT interquartile range= 0.15 μg/m3
ECAT tercile sample size (concentration range): HOME (μg/m3) – 1st Tercile (0.23-0.33), 2nd Tercile (0.33-0.43), 3rd Tercile (0.43-0.81); CCAAPS – 1st Tercile (0.23- 0.31), 2nd Tercile (0.32-0.39), 3rd Tercile (0.39-0.88); Pooled sample (μg/m3) – 1st Tercile (0.23-0.32), 2nd Tercile (0.32-0.40), 3rd Tercile (0.40-0.88).
Abbreviations: ECAT, Elemental carbon attributable to traffic; HOME, Health Outcomes and Measures of the Environment; CCAAPS, Cincinnati Childhood and Air Pollution Study.
Table 3.
Adjusted difference in body mass index z-scores at age 7-8 years across ECAT concentration terciles and per interquartile range change in ECAT concentration (HOME Study and CCAAPS)
| HOME | CCAAPS | Pooled Sample | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ECAT Measure |
n | Difference (z-score) |
95% CI | n | Difference (z-score) |
95% CI | n | Difference (z-score) |
95% CI |
| 1st Tercile | 70 | ref. | 154 | ref. | 226 | ref. | |||
| 2nd Tercile | 62 | −0.26 | (−0.66, 0.14) | 156 | −0.19 | (−0.47, 0.09) | 218 | −0.07 | (−0.31, 0.17) |
| 3rd Tercile | 66 | −0.18 | (−0.59, 0.22) | 151 | −0.07 | (−0.36, 0.23) | 213 | −0.12 | (−0.36, 0.13) |
| Per IQR | 198 | −0.07 | (−0.27, 0.13) | 459 | −0.02 | (−0.16, 0.12) | 657 | −0.04 | (−0.15, 0.08) |
Individual cohort models adjusted for maternal race (categorical), household income (continuous), maternal age at delivery (continuous), maternal education (categorical), parity (categorical), maternal exposure to tobacco (HOME Study: cotinine level (continuous) and CCAAPS: Non-smokers and Smokers (categorical), and weight gain during pregnancy (continuous). HOME model also adjusted for maternal pre-pregnancy BMI (continuous).
Pooled sample models adjusted for cohort (categorical), maternal race (categorical), household income (categorical), maternal age at delivery (continuous), maternal education (categorical), parity (categorical), maternal exposure to tobacco (categorical: non-smokers and smokers), and weight gain during pregnancy (continuous).
ECAT and cohort interaction p-value = 0.28
Pooled ECAT interquartile range= 0.15 μg/m3
ECAT tercile sample size (concentration range): HOME (μg/m3) – 1st Tercile (0.23-0.33), 2nd Tercile (0.33-0.43), 3rd Tercile (0.43-0.81); CCAAPS – 1st Tercile (0.23- 0.31), 2nd Tercile (0.32-0.39), 3rd Tercile (0.39-0.88); Pooled sample (μg/m3) – 1st Tercile (0.23-0.32), 2nd Tercile (0.32-0.40), 3rd Tercile (0.40-0.88).
Abbreviations: ECAT, Elemental carbon attributable to traffic; HOME, Health Outcomes and Measures of the Environment; CCAAPS, Cincinnati Childhood and Air Pollution Study.
In sensitivity analyses, the association of ECAT concentration with birthweight or BMI was similar in fully adjusted models and models not adjusted for pregnancy weight gain or maternal pre-pregnancy BMI (see Tables, Supplemental Digital Content 7 and Supplemental Digital Content 8, characterizing the association in sensitivity analyses). Furthermore, inclusion of infants born < 37 weeks gestation in the HOME Study and adjustment for gestational age did not meaningfully alter the association between ECAT concentration and birthweight in adjusted models. In the individual cohort analyses, the association of ECAT concentration with birthweight or BMI z-score did not meaningfully vary across strata of maternal race, child sex, or household income (all interaction p-values > 0.12; see Tables, Supplemental Digital Content 9 and Supplemental Digital Content 10, which contain stratified analyses). In the pooled analysis, infant sex modified the association between ECAT concentrations and birthweight. Among male newborns, higher ECAT concentrations were associated with higher birthweight (61g; 95% CI: 9, 113), but we observed no association among female newborns (−9g; 95% CI: −58, 41) (infant sex and ECAT interaction p-value =0.05).
DISCUSSION
Our results do not suggest an association of residential traffic-related air pollution exposure during early-life with lower birthweight or higher BMI z-scores at age 7–8 years in these two Cincinnati, OH based cohorts. Results from our secondary analyses suggest that infant sex could potentially modify the association between residential traffic-related air pollution exposure and birthweight; however, these results warrant further investigation. We did not find that the relationship between ECAT and BMI z-scores varied by maternal race, child sex, or household income.
Exhaust generated from diesel combustion consists of fine (0.1–2.5μm) and ultrafine particles (< 0.1μm) which can adversely affect health and development by penetrating deep into the lungs, entering the bloodstream, and causing oxidative stress.37–39 The fetus may be particularly vulnerable to environmental pollutants, like diesel exhaust, because of immature detoxification pathways and increased sensitivity to environmental stressors.40 Prenatal traffic-related air pollution exposure could impact childhood adiposity by altering metabolic function during fetal development. Previous studies have reported that early-life traffic-related air pollution exposure is associated with an increase in leptin and adiponectin concentrations in cord blood, adipocytokines hypothesized to be related to fetal, infant, and child growth and obesity risk.27,41,42
In a larger sample, Bell et al. (2010) reported on average a 6g (95% CI: −11, 0) lower birthweight per IQR increase (1.1 μg/m3) in gestational exposure to ambient elemental carbon.43 Similarly, Kingsley et al. (2017) and Bell et al. (2007), among others, report an association between model-based and monitor-based PM2.5 exposure estimates and birthweight (12.1g lower birthweight per IQR [2.5 μg/m3], 95% CI: −24.2, −0.1; 14.7g lower birthweight per IQR [2.2 μg/m3], 95% CI:−17.1, −12.3, respectively).14,15,19,43 Several studies have also consistently reported an association between traffic density or estimated exposure to traffic-related air pollutants, including PM2.5, elemental carbon, and nitrogen oxides, and higher odds of term low birthweight.17,18,44
Our findings related to the association between traffic-related air pollution and birthweight may be impacted by our modest sample size, as well as lack of variation in exposure estimates. While the distribution of birthweight measurements in our analysis is comparable to previous studies, the ECAT concentrations are significantly lower and less variable than estimates of total elemental carbon concentrations from traffic sources in general. For example, our ECAT estimates only represent a portion of total elemental carbon. The mean ECAT concentration for the combined cohorts was 0.39 μg/m3 (SD= 0.12), while the mean of the total elemental carbon concentrations from motor vehicles in the Bell et al. (2010) study was 1.04 μg/m3 (SD= 0.60).43 Our study adds to this existing literature by focusing on lower exposure concentrations from a more specific traffic type.
Previous studies have also found an association of traffic-related air pollution with childhood obesity; however, results have varied based on exposure assessment method and timing. For example, similar to our results, both Fleisch et al. (2017) and Fioravanti et al. (2018) reported no association between exposure to estimated concentrations of traffic-related air pollutants, such as black carbon, particulate matter, or nitrogen oxides, and childhood obesity.45,46 However, Fleisch et al. (2017) did report an association between proximity to roadway and greater fat mass around age 7 years.45 While Kim et al. (2018) also reported no association between gestational exposure to freeway nitrogen oxides and childhood obesity, they did report an association between early-life exposure and BMI at age 10 when adjusting for later childhood exposure,16 a period of time when traffic-related air pollution exposure may also be associated with higher childhood BMI.9 However, results from Kim et al. (2018) only suggest an association between later childhood exposure to non-freeway traffic and higher BMI at age 10, but not freeway traffic.16
We speculate that differences in built environments surrounding distinct roadway types, such as greenspace and noise barriers, as well as access to recreational space in areas of dense roadways could influence exposure and childhood obesity risk; therefore, our findings could be influenced by residual confounding from our lack of consideration for these factors (see Figure, Supplemental Digital Content 11, which illustrates potential confounders that were not included in the analyses). Additionally, we did not account for exposure during childhood, which could vary from gestational or early-life exposure. For example, previous analyses of the CCAAPS cohort report that 54% of participants moved at least once during childhood; changes in residential address could impact longitudinal exposure to traffic-related air pollution.47 Future studies with spatio-temporal exposure models should consider including traffic exposure during childhood given that it could be an additional period of susceptibility.
Previous evidence suggests that maternal race, child sex, or household income could modify the association of air pollution exposure with fetal growth or childhood adiposity.15,44,48,49 Although the research is limited, prior studies suggest that the associations of particulate matter with lower birthweight and higher childhood BMI are stronger in males.10,49,50 Additionally, males may be more susceptible to preterm birth associated with exposure to some air pollutants.51 Our results suggesting that higher birthweight may be associated with ECAT exposure among males warrant further investigation. Future studies with larger sample sizes and other fetal growth measures are needed to better characterize sex-specific associations between traffic-related air pollution exposure and fetal growth.
There are some limitations to our present study. First, limiting our main analyses to term infants born at 37 weeks gestation or after may result in selection bias. Previous studies have reported a relationship of traffic-related pollution exposure with preterm birth.52,53 If traffic-related air pollution exposure is associated with preterm birth in the Cincinnati, OH region, then infants with higher ECAT exposure would be excluded from our analyses, which we expect to bias our results towards the null. Our sensitivity analysis which included HOME Study participants born preterm (i.e. < 37 weeks) does not suggest that the exclusion of preterm infants in the main analyses affected our results. However, the number of infants born preterm in the HOME Study is small and we were not able to examine associations among preterm infants in CCAAPS because infants born prior to 35 weeks were not enrolled in the study. Second, CCAAPS inclusion criteria also required infants to have at least one atopic parent. This criterion, however, does not appear to bias our findings given the two cohorts yielded similar results. Third, we assessed childhood obesity using body mass index which may not accurately reflect body composition. Fourth, we did not consider potential confounding due to maternal or child exercise and diet. Diet and exercise impact childhood adiposity and can be associated with traffic-related air pollution exposure through socioeconomic status. Moreover, we did not consider exposure to traffic noise or greenspace, which could have resulted in some residual confounding. Finally, we estimated early-life ECAT exposure based on one residential address, although women may have moved. Moreover, we used the land use regression model to estimate long-term ECAT exposure, therefore we were unable to differentiate effects of ECAT exposure during specific time periods and did not consider ECAT exposure during childhood. Housing characteristics and individual time-activity patterns could also contribute to misclassification of exposure, which on average is expected to bias our results towards the null.
On the other hand, our analysis also had several strengths. Body mass index was calculated using anthropometric measurements taken by trained assistants and standardized protocols. In addition, we were able to compare our findings across the two cohorts which recruited participants from overlapping geographical areas during the same time period and assessed similar covariates. Lastly, we used a validated land use regression model that has been used in other health studies to estimate exposure at women’s residential addresses.30,33
CONCLUSION
In contrast to previous studies and our hypothesis, we did not find that traffic-related air pollution exposure was associated with lower birthweight or higher childhood adiposity at age 7–8 years in these two cohorts or the pooled sampled. Our results should be cautiously interpreted given prior research and the limitations of our study, including the modest sample size, relatively low ECAT concentrations, and our ability to examine ECAT only during the prenatal period. Future studies with larger sample sizes and temporally resolved traffic-related air pollution exposure models for intraurban areas may help clarify inconsistent research findings. Given the lifelong impact of low birthweight and childhood obesity, identifying specific sources of traffic pollution that increase obesity risk and built environment characteristics that can protect against exposure should be of great public health interest.
Supplementary Material
Supplemental Digital Content 1. Flow diagram of participants included in each cohort for the HOME Study and CCAAPS cohorts.
Supplemental Digital Content 2. Figure with map illustrating the geographical distribution of participants in HOME Study and CCAAPS. doc
Supplemental Digital Content 3. Figure with directed acyclic graph of variables confounding the association of ECAT with birthweight. doc
Supplemental Digital Content 4. Figure with directed acyclic graph of variables confounding the association of ECAT with childhood BMI. doc
Supplemental Digital Content 5: Summary statistics of term birthweight (grams) and BMI z-score for HOME Study and CCAAPS participants at enrollment. doc
Supplemental Digital Content 6. Table with median (25th and 75th percentile) maternal residential elemental carbon attributable to traffic (μg/m3) concentrations by covariate and cohort. doc
Supplemental Digital Content 7. Table with adjusted difference in term birthweight per interquartile range increase in maternal resident ECAT concentrations: Sensitivity analyses. doc
Supplemental Digital Content 8. Table with adjusted difference in BMI z-score at age 7–8 years per interquartile range change in maternal residential ECAT concentrations: Sensitivity analyses. doc
Supplemental Digital Content 9. Table with adjusted difference in term birthweight per interquartile range increase in residential ECAT concentrations stratified by maternal race, household income, and infant sex (HOME Study and CCAAPS). doc
Supplemental Digital Content 10. Table with adjusted difference in body mass index z-scores at age 7–8 years per interquartile range increase in residential ECAT concentration stratified by maternal race, household income and infant sex (HOME Study and CCAAPS). doc
Supplemental Digital Content 11. Directed acyclic graph of variables confounding the association of ECAT with birthweight and childhood BMI. doc
WHAT THIS STUDY ADDS: Our results add to the current research by using a novel marker of traffic-related air pollution, which is sensitive to diesel traffic, to characterize the association of traffic-related air pollution exposure with birthweight and child adiposity.
ACKNOWLEDGEMENTS:
The authors would like to acknowledge Christopher Wolfe for assisting with the production of figures.
SOURCES OF FUNDING: This work was supported by grants R01 ES024381, R01 ES020349, R01 ES011170, R21 ES023073, and P42 ES013660 from the US National Institute of Environmental Health Sciences (NIEHS, NIH). C.G. Sears is partially supported by the Institute at Brown for Environment and Society. The contents of this report are solely the responsibility of the authors and do not necessarily represent the official views of the sponsoring organizations.
Footnotes
CONFLICTS OF INTEREST: Dr. Lanphear reported serving as an expert witness in childhood lead poisoning cases, for which he has not received any compensation. Dr. Braun was financially compensated for serving as an expert witness for plaintiffs in litigation related to tobacco smoke exposures.
DATA SHARING: Interested investigators should contact Drs Joseph M.Braun [joseph_braun_1@brown.edu] and Kimberly Yolton [kimberly.yolton@cchmc.org] to discuss collaborative opportunities, obtain additional information about the HOME Study, and request a project proposal form. The HOME Study Data Sharing Committee meets regularly to review proposed research projects and ensure that they do not overlap with extant projects and are an efficient use of scarce resources
References
- 1.Wang Y Cross-national comparison of childhood obesity: the epidemic and the relationship between obesity and socioeconmoic status. International Journal of Epidemiology 2001;30:1129–1136. [DOI] [PubMed] [Google Scholar]
- 2.Silventoinen K, Rokholm B, Kaprio J, Sorensen TI. The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes (Lond) 2010;34(1):29–40. [DOI] [PubMed] [Google Scholar]
- 3.Romano ME, Savitz DA, Braun JM. Challenges and future directions to evaluating the association between prenatal exposure to endocrine disrupting chemicals and childhood obesity. Curr Epidemiol Rep 2014;1(2):57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dadvand P, Parker J, Bell ML, Bonzini M, Brauer M, Darrow LA, Gehring U, Glinianaia SV, Gouveia N, Ha EH, Leem JH, van den Hooven EH, Jalaludin B, Jesdale BM, Lepeule J, Morello-Frosch R, Morgan GG, Pesatori AC, Pierik FH, Pless-Mulloli T, Rich DQ, Sathyanarayana S, Seo J, Slama R, Strickland M, Tamburic L, Wartenberg D, Nieuwenhuijsen MJ, Woodruff TJ. Maternal exposure to particulate air pollution and term birth weight: a multi-country evaluation of effect and heterogeneity. Environ Health Perspect 2013;121(3):267–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong G, Qian Z, Liu M, Wang D, Ren W, Flick L, Fu J, Wang J, Chen W, Simckes M, Trevathan E. Ambient air pollution and the prevalence of obesity in Chinese children: the seven northeastern cities study. Obesity 2014;22(3):795–800. [Google Scholar]
- 6.Fleisch AF, Rifas-Shiman SL, Koutrakis P, Schwartz JD, Kloog I, Melly S, Coull BA, Zanobetti A, Gillman MW, Gold DR, Oken E. Prenatal exposure to traffic pollution: associations with reduced fetal growth and rapid infant weight gain. Epidemiology 2015;26(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray S, Edwards S, Miranda M. Assessing exposure metrics for PM and birth weight models. J Expo Sci Environ Epidemiol 2010;20(5):469–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hyder A, Lee H, Ebisu K, Koutrakis P, Belanger K, Bell M. PM2.5 exposure and birth outcomes: use of satellite- and monitor-based data. Epidemiology 2014;25(1):58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, Gilliland F, Lurmann F, Islam T, Berhane K. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environmental Health 2014;13(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lakshmanan A, Chiu Y, Coull B, Just A, Maxwell S, Schwartz J, Gryparis A, Kloog I, Wright R, Wright R. Associations between prenatal traffic-related air pollution exposure and birth weight: Modification by sex and maternal pre-pregnancy body mass index. Environ Res 2015;137:268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mao G, Nachman RM, Sun Q, Zhang X, Koehler K, Chen Z, Hong X, Wang G, Caruso D, Zong G, Pearson C, Ji H, Biswal S, Zuckerman B, Wills-Karp M, Wang X. Individual and Joint Effects of Early-Life Ambient Exposure and Maternal Prepregnancy Obesity on Childhood Overweight or Obesity. Environ Health Perspect 2017;125(6):067005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker JD, Woodruff TJ, Basu R, Schoendorf KC. Air pollution and birth weight among term infants in California. Pediatrics 2005;115(1):121–8. [DOI] [PubMed] [Google Scholar]
- 13.Rundle A, Hoepner L, Hassoun A, Oberfield S, Freyer G, Holmes D, Reyes M, Quinn J, Camann D, Perera FP, Whyatt R. Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy. Am J Epidemiol 2012;175(11):1163–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savitz DA, Bobb JF, Carr JL, Clougherty JE, Dominici F, Elston B, Ito K, Ross Z, Yee M, Matte TD. Ambient fine particulate matter, nitrogen dioxide, and term birth weight in New York, New York. Am J Epidemiol 2014;179(4):457–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bell M, Ebisu K, Belanger K. Ambient air pollution and low birth weight in Connecticut and Massachusetts. Environ Health Perspect 2007;115(7):1118–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim JS, Alderete TL, Chen Z, Lurmann F, Rappaport E, Habre R, Berhane K, Gilliland FD. Longitudinal associations of in utero and early life near-roadway air pollution with trajectories of childhood body mass index. Environ Health 2018;17(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen A- MN, Ballester F, Beelen RMJ, Chatzi L, Cirach M, Danileviciute A, Dedele A, Eijsden Mv, Estarlich M, Fernández-Somoano A, Fernández MF, Forastiere F, Gehring U, Grazuleviciene R, Gruzieva O, Heude B, Hoek G, Hoogh Kd, van den Hooven EH, Håberg SE, Jaddoe VWV, Klümper C, Korek M, Krämer U, Lerchundi A, Lepeule J, Nafstad P, Nystad W, Patelarou E, Porta D, Postma D, Raaschou-Nielsen O, Rudnai P, Sunyer J, Stephanou E, Sørensen M, Thiering E, Tuffnell D, Varró MJ, Vrijkotte TGM, Wijga A, Wilhelm M, Wright J, Nieuwenhuijsen MJ, Pershagen G, Brunekreef B, Kogevinas M, Slama R. Ambient air pollution and low birthweight: a European cohort study (ESCAPE). The Lancet Respiratory Medicine 2013;1(9):695–704. [DOI] [PubMed] [Google Scholar]
- 18.Wilhelm M, Ghosh JK, Su J, Cockburn M, Jerrett M, Ritz B. Traffic-related air toxics and term low birth weight in Los Angeles County, California. Environ Health Perspect 2012;120(1):132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kingsley SL, Eliot MN, Glazer K, Awad YA, Schwartz JD, Savitz DA, Kelsey KT, Marsit CJ, Wellenius GA. Maternal ambient air pollution, preterm birth and markers of fetal growth in Rhode Island: results of a hospital-based linkage study. J Epidemiol Community Health 2017;71(12):1131–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McIntire D, Bloom S, Casey B, Leveno K. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med 1999;340:1234–1238. [DOI] [PubMed] [Google Scholar]
- 21.Johnson RC, Schoeni RF. Early-life origins of adult disease: national longitudinal population-based study of the United States. Am J Public Health 2011(1541–0048 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vos L, Oren A, Bots M, Gorissen W, Grobbee D, Uiterwaal C. Birth size and coronary heart disease risk score in young adulthood. The Atherosclerosis Risk in Young Adults (ARYA) study. Eur J Epidemiol 2006;21:33–38. [DOI] [PubMed] [Google Scholar]
- 23.Hales C, Barker D, Clark P, Cox L, Fall C, Osmond C, Winter P. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ 1991;303(6809):1019–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deckelbaum R, Williams C. Childhood obesity: the health issue. Obes Res 2001;9(4):S239S–243S. [DOI] [PubMed] [Google Scholar]
- 25.Barker DJ. The developmental origins of adult disease. J Epidemiol Community Health 2003;58(2):114–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhaskaran K, dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. The Lancet Diabetes & Endocrinology 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alderete TL, Song AY, Bastain T, Habre R, Toledo-Corral CM, Salam MT, Lurmann F, Gilliland FD, Breton CV. Prenatal traffic-related air pollution exposures, cord blood adipokines and infant weight. Pediatr Obes 2018;13(6):348–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.U.S. EPA. Health Assessment Document for Diesel Engine Exhaust https://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=29060 Accessed December 2018.
- 29.Zhu Y, Pudota J, Collins D, Allen D, Clements A, DenBleyker A, Fraser M, Jia Y, McDonald-Buller E, Michel E. Air pollutant concentrations near three Texas roadways, Part I: Ultrafine particles. Atmospheric Environment 2009;43(30):4513–4522. [Google Scholar]
- 30.Ryan PH, Lemasters GK, Biswas P, Levin L, Hu S, Lindsey M, Bernstein DI, Lockey J, Villareal M, Khurana Hershey GK, Grinshpun SA. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect 2007;115(2):278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braun JM, Kalloo G, Chen A, Dietrich KN, Liddy-Hicks S, Morgan S, Xu Y, Yolton K, Lanphear BP. Cohort Profile: The Health Outcomes and Measures of the Environment (HOME) study. Int J Epidemiol 2017;46(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu S, McDonald R, Martuzevicius D, Biswas P, Grinshpun SA, Kelley A, Reponen T, Lockey J, Lemasters G. UNMIX modeling of ambient PM(2.5) near an interstate highway in Cincinnati, OH, USA. Atmos Environ (1994) 2006;40(S2):378–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sahu M, Hu S, Ryan PH, Le Masters G, Grinshpun SA, Chow JC, Biswas P. Chemical compositions and source identification of PM(2).(5) aerosols for estimation of a diesel source surrogate. Sci Total Environ 2011;409(13):2642–51. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization AnthroPlus software. Growth Reference 5 – 19 Years: Application Tools. http://www.who.int/growthref/tools/en Accessed November 2017.
- 35.Greenland S, Pearl J, Robins J. Causal diagrams for epidemiologic research. Epidemiology 1999;10(1):37–48. [PubMed] [Google Scholar]
- 36.Pearl J Causal diagrams for empirical research. Biometrika 1995;82(4):669–688. [Google Scholar]
- 37.Oberdörster G, Utell M. Ultrafine particles in the urban air: to the respiratory tract--and beyond? Environ Health Perspect 2002;110:A440–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Riedl M, Diaz-Sanchez D. Biology of diesel exhaust effects on respiratory function. J Allergy Clin Immunol 2005;115(2):221–228. [DOI] [PubMed] [Google Scholar]
- 39.Xing YF, Xu YH, Shi MH, Lian YX. The impact of PM2.5 on the human respiratory system. Journal of Thoracic Disease. 2016;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suk W, Ruchirawat K, Balakrishnan K, Berger M, Carpenter D, Damstra T, de Garbino J, Koh D, Landrigan P, Makalinao I, Sly P, Xu Y, Zheng B. Environmental threats to children’s health in Southeast Asia and the Western Pacific. Environ Health Perspect 2003;111(10):1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lavigne E, Ashley-Martin J, Dodds L, Arbuckle TE, Hystad P, Johnson M, Crouse DL, Ettinger AS, Shapiro GD, Fisher M, Morisset AS, Taback S, Bouchard MF, Sun L, Monnier P, Dallaire R, Fraser WD. Air Pollution Exposure During Pregnancy and Fetal Markers of Metabolic function: The MIREC Study. Am J Epidemiol 2016;183(9):842–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simpson J, Smith AD, Fraser A, Sattar N, Lindsay RS, Ring SM, Tilling K, Davey Smith G, Lawlor DA, Nelson SM. Programming of Adiposity in Childhood and Adolescence: Associations With Birth Weight and Cord Blood Adipokines. J Clin Endocrinol Metab 2017;102(2):499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bell M, Belanger K, Ebisu K, Gent J, Lee H, Koutrakis P, Leaderer BP. Prenatal exposure to fine particulate matter and birth weight: variations by particulate constituents and sources. Epidemiology 2010;21(6):884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ebisu K, Bell M. Airborne PM2.5 chemical components and low birth weight in the northeastern and mid-Atlantic regions of the United States. Environ Health Perspect 2012;120(12):1746–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fleisch AF, Luttmann-Gibson H, Perng W, Rifas-Shiman SL, Coull BA, Kloog I, Koutrakis P, Schwartz JD, Zanobetti A, Mantzoros CS, Gillman MW, Gold DR, Oken E. Prenatal and early life exposure to traffic pollution and cardiometabolic health in childhood. Pediatr Obes 2017;12(1):48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fioravanti S, Cesaroni G, Badaloni C, Michelozzi P, Forastiere F, Porta D. Traffic-related air pollution and childhood obesity in an Italian birth cohort. Environmental Research 2018;160:479–486. [DOI] [PubMed] [Google Scholar]
- 47.Brokamp C, LeMasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol 2016;26(4):428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miranda ML, Maxson P, Edwards S. Environmental contributions to disparities in pregnancy outcomes. Epidemiologic Reviews 2009;31:67–83. [DOI] [PubMed] [Google Scholar]
- 49.Chiu Y, Hsu H, Wilson A, Coull B, Pendo M, Baccarelli A, Kloog I, Schwartz J, Wright R, Taveras E, Wright R. Prenatal particulate air pollution exposure and body composition in urban preschool children: Examining sensitive windows and sex-specific associations. Environmental Research 2017;158(798–805). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jedrychowski W, Perera F, Mrozek-Budzyn D, Mroz E, Flak E, Spengler JD, Edwards S, Jacek R, Kaim I, Skolicki Z. Gender differences in fetal growth of newborns exposed prenatally to airborne fine particulate matter. Environ Res 2009;109(4):447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ghosh R, Rankin J, Pless-Mulloli T, Glinianaia S. Does the effect of air pollution on pregnancy outcomes differ by gender? A systematic review. Environ Res 2007;105(3):400–8. [DOI] [PubMed] [Google Scholar]
- 52.Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B. Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the south coast air basin of California. Environ Health Perspect 2009;117(11):1773–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ji X, Meng X, Liu C, Chen R, Ge Y, Kan L, Fu Q, Li W, Tse LA, Kan H. Nitrogen dioxide air pollution and preterm birth in Shanghai, China. Environ Res 2018;169:79–85. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Flow diagram of participants included in each cohort for the HOME Study and CCAAPS cohorts.
Supplemental Digital Content 2. Figure with map illustrating the geographical distribution of participants in HOME Study and CCAAPS. doc
Supplemental Digital Content 3. Figure with directed acyclic graph of variables confounding the association of ECAT with birthweight. doc
Supplemental Digital Content 4. Figure with directed acyclic graph of variables confounding the association of ECAT with childhood BMI. doc
Supplemental Digital Content 5: Summary statistics of term birthweight (grams) and BMI z-score for HOME Study and CCAAPS participants at enrollment. doc
Supplemental Digital Content 6. Table with median (25th and 75th percentile) maternal residential elemental carbon attributable to traffic (μg/m3) concentrations by covariate and cohort. doc
Supplemental Digital Content 7. Table with adjusted difference in term birthweight per interquartile range increase in maternal resident ECAT concentrations: Sensitivity analyses. doc
Supplemental Digital Content 8. Table with adjusted difference in BMI z-score at age 7–8 years per interquartile range change in maternal residential ECAT concentrations: Sensitivity analyses. doc
Supplemental Digital Content 9. Table with adjusted difference in term birthweight per interquartile range increase in residential ECAT concentrations stratified by maternal race, household income, and infant sex (HOME Study and CCAAPS). doc
Supplemental Digital Content 10. Table with adjusted difference in body mass index z-scores at age 7–8 years per interquartile range increase in residential ECAT concentration stratified by maternal race, household income and infant sex (HOME Study and CCAAPS). doc
Supplemental Digital Content 11. Directed acyclic graph of variables confounding the association of ECAT with birthweight and childhood BMI. doc


