Abstract
Objective:
To assess the feasibility and efficacy of in-restaurant interventions aiming to promote healthy choices via fundraising incentives benefiting school wellness programs and point-of-purchase nutrition promotion.
Design:
Twelve schools were randomly assigned to one of two intervention periods: Fundraising Incentive (FI) donated funds for visiting the study restaurant; Fundraising-Healthy Eating Incentive (F-HEI) included FI with additional funds given when selecting a healthier item. Both conditions included point-of-purchase nutrition promotions. Families were recruited to attend their designated intervention and complete a survey. Feasibility was assessed based on recruitment and participation, implementation fidelity, and intervention acceptability. Efficacy was assessed by comparing participant receipts between intervention periods and by comparing overall restaurant sales during intervention vs. two no-intervention time frames.
Setting:
Fast-casual restaurant in Southern California
Participants:
Parents with children attending participating schools.
Results:
Eighty-one families visited the restaurant during the intervention, with 66 completing surveys. All study activities were implemented successfully, but school family participation in the intervention was low (0.95%). Among participants completing surveys, all indicated satisfaction with the program. The percentage of healthier items ordered was significantly greater during both FI (χ2=5.97, p=.01) and F-HEI (χ2=8.84, p=.003) versus Comparison 2. Results were similar but did not reach statistical significance when comparing the interventions to Comparison 1.
Conclusions:
Results support potential efficacy of this program, but more research is needed to inform feasibility. Fidelity and acceptability data supported feasibility, but participation rates were low in this initial study. Methods evaluating this intervention with a greater proportion of parents should be considered.
Keywords: Restaurants, Healthy Eating, Fundraising Incentives, Obesity, School Wellness, Nutrition Environment, Nutrition Interventions
Introduction
The restaurant environment has been considered a likely contributing factor to rising obesity trends(1–3). In parallel with obesity rates, the share of food spending on food prepared away from home (FAFH) has increased significantly since the 1970s, including food purchased at fast-food and full-service restaurants(3). The consumption of FAFH is associated with diets higher in calories, saturated fats, sodium, and sugar, and lower in fruits, vegetables, fiber, and micronutrients(1–7).Fast-food and full-service restaurant consumption is associated with increased total daily energy intake. As a result, there is a need to identify and implement effective strategies to improve the nutrition environment of restaurants and dietary intake of restaurant diners.
Restaurant-based interventions to improve dietary choices have incorporated point-of-purchase nutrition information, increased healthy item availability, and/or financial incentives with mixed results(8,9), but few have investigated the impact of fundraising incentives aimed to improve food choices. In general, financial incentives have shown promise in promoting positive health behaviors. A review of randomized controlled trials revealed a positive effect of monetary incentives on food purchases, food consumption, and weight loss(10), and recent studies continue to support effects of monetary incentives on fruit and vegetable consumption, physical activity, and weight loss(11–15). Fundraising incentives that indirectly benefit the participant may also influence personal health behavior, specifically dietary behavior.
One recent study explored the impact of fundraising incentives (charitable donation) and targeted calorie messaging on beverage choices in a restaurant and determined that the donation had no effect(8). However, the selected charity was predetermined by the research team with no participant input. Thus, participants may not have been motivated to donate to the chosen charity which may have reduced the fundraising incentive’s impact.
No known studies have investigated the impact of school fundraising incentives to promote healthful eating in the restaurant setting. Successful restaurant-school partnerships may simultaneously benefit 1) schools by raising money for school initiatives, 2) school families through improved health behaviors and outcomes and 3) restaurants with the potential to develop brand loyalty among consumers.
Many schools already participate in “Dine Out” events where families earn donations for their school by dining at a restaurant. While existing programs offer potential financial benefits for restaurants and schools, one concern is potential unintended negative consequences on diet quality and energy intake if participating families increase their frequency of dining out.
We designed an alternative model to “Dine Out” events that incorporates fundraising incentives for purchasing healthier menu items aiming to retain the financial benefits of “Dine Out” events while promoting healthy eating. This pilot program collaborated with restaurants to promote healthier menu items and offer fundraising incentives benefiting participants’ school wellness programs, which provide nutrition and physical activity programming to students and have been shown to increase fruit and vegetable consumption and time spent participating in physical activity among school children(16). We examined the program’s feasibility, including acceptability among participants and implementation fidelity, as well as its initial efficacy in increasing the selection of healthier items when dining out.
Methods
Overview
A randomized pilot study was developed in collaboration with one school district and one fast-casual restaurant in Southern California targeting families with children attending elementary schools within the participating school district. Schools were randomized to one of two fundraising intervention conditions intended to promote healthier ordering behaviors among families when dining out. Feasibility (recruitment/participation, implementation fidelity, and intervention acceptability) was assessed using process evaluation and surveys completed by families. In addition, initial intervention efficacy was assessed in two ways. First, ordering of healthier items was compared between the two conditions among participating families. Ordering of healthier items among all restaurant customers was also compared during intervention periods versus two comparison periods when no intervention was in place. Institutional Review Board approval of all research methodology was obtained through IRB Company, Inc. (IRBCo).
Recruitment and Participation
Restaurant
Consumption of foods from different types of restaurants (e.g., quick-service/fast food, as well as full-service/sit down) is linked to less healthy nutritional intake (calories, sugar, saturated fat, sodium) among adults and children(3,17), with evidence that families consume foods from quick-service/fast-casual restaurants more often than full-service restaurants (18). In an effort to reach a broad range of families, we partnered with a local fast-casual Mexican-cuisine restaurant in San Diego County with a central location and convenient counter service and affordable menu. A research team member conducted a training session for on-site restaurant staff on research procedures prior to implementation. The restaurant owner received a $200 incentive for their participation.
Schools
All twelve elementary schools within the school district were invited to participate in the study in the form of a fundraiser, at a local restaurant, benefiting their school wellness program. The participating schools were then matched using the Mahalanobis method(19) based on student population size, percent of students eligible for free and reduced-price school lunches, and distance to the intervention restaurant. One school from each pair was randomly assigned to one of the two intervention groups.
Families
School families were recruited to visit the participating restaurant during the assigned intervention period via 1) e-mail blasts including an electronic flyer sent to parents of children attending elementary schools in the participating school district and 2) paper flyers delivered to all twelve schools and distributed to students prior to each intervention condition. The flyers included an identifying sticker for each school. Parents/guardians without a flyer were able to retrieve one from the research table in the restaurant prior to ordering. Restaurant staff collected flyers from participating families and attached the corresponding receipt to the flyer.
After ordering, parents/guardians visiting the study restaurant during the intervention were recruited to participate in an optional survey on-site to collect data on program acceptability and restaurant dining behaviors. Researchers positioned near point-of-purchase approached all families participating in the intervention and invited them to complete the survey. Eligibility criteria to participate in the survey included 1) being 18 years or older, 2) being a parent/guardian of a child who attended one of the participating elementary schools, 3) having ordered any item at the participating restaurant location during the intervention period, 4) able to read, write, and speak English or Spanish, and 5) agreeing to data collection procedures. The survey was administered in English or Spanish via paper or electronic tablet via QuickTapSurvey software (www.quicktapsurvey.com, TabbleDabble Inc., Toronto, Canada) and was designed to take less than ten minutes. Survey participants received a $10 gift card to the restaurant for completing the survey.
Intervention
Both the Fundraising Incentive (FI) and Fundraising-Healthy Eating Incentive (F-HEI) conditions consisted of a four-day restaurant-based intervention organized as a school “Dine Out” promotion incorporating fundraising incentives and nutrition information. Specifically, both conditions consisted of 1) a fundraising incentive for visiting the restaurant and ordering any item, 2) a poster promoting healthier menu options, and 3) nutrition information displayed at point-of-purchase. Fundraising incentives were provided as a donation to the school wellness program of the participant’s child and were calculated as a percentage of the family’s total bill. Incentive amounts were finalized using restaurant operator feedback. The incentive amounts and donation target (school wellness) were printed on the flyers distributed to families. Fifteen percent of the total bill was donated to the corresponding school for all receipts collected with a flyer. In the F-HEI condition, an additional 10% of the total bill was donated to the corresponding school for all receipts containing at least one of 16 promoted healthier menu items, which consisted of small plates (tacos) and main meals (bowls, tortas, burritos, salad) from the standard menu. This additional fundraising incentive was promoted on allstudy signage exhibited during F-HEI. During both conditions, a3×2 foot poster was displayed between the restaurant entrance and cashiers and highlighted a selection of the healthier items with pictures and nutrient information. The nutrition information at point of purchase, located at each of the cash registers, also included healthier menu items and nutrition information without photos.
In order to determine healthier menu items, Healthy Dining nutrition criteria were used(20) and menus were analyzed by a registered dietitian using Genesis R&D Food Formulation & Labeling Software (Genesis R&D Software 9.14.41 Database Structure version 9.8.2, ESHA Research, Salem, OR, 2015).
Measures
Feasibility
Feasibility analyses included assessments of recruitment and participation, implementation fidelity, and intervention acceptability.
To assess recruitment and implementation fidelity, process evaluation was carried out by the research team. Recruitment indicators included overall school and family participation, school population characteristics by intervention group, and demographic characteristics of survey participants. Additional variables that could affect participation and outcomes were also monitored including weather, holidays, and competing school and restaurant promotions (including restaurant menu specials).
Additional variables monitored by the research staff during recruitment and implementation included: number of flyers distributed and collected, number of e-mails distributed, intervention days of the week and times of day, restaurant staff training, nutrition promotion sign and poster placement, and customer traffic.
Intervention acceptability was measured via participants’ survey responses. The survey measured demographics, intervention acceptability, and behavioral data from parents/guardians who participated in the intervention.
Efficacy
Receipts
Two types of sales data were collected for analysis. First, sales receipts were collected from families who presented a flyer in the restaurant. The number of healthy items ordered and total number of items ordered by each participating dining party were recorded from receipts during each intervention, and the percent of items ordered that were the promoted healthy items (i.e. relative ordering of healthy items) was calculated for each dining party.
Sales
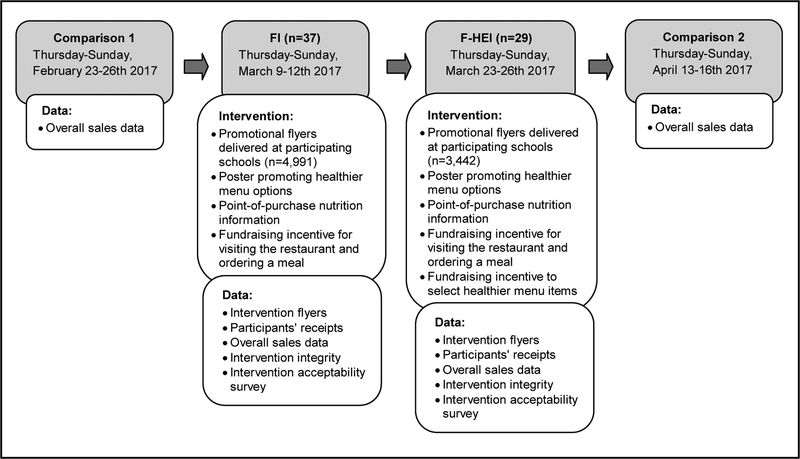
In addition, parallel variables were calculated from aggregate sales data (i.e. across all patrons in the restaurant) during each of the two intervention periods, as well as two four-day comparison periods in which no intervention was in place, one two weeks before the first intervention (FI) and one three weeks after the intervention periods ended. These no-intervention time periods are referred to herein as Comparison 1 and Comparison 2, respectively (Figure 1).
Figure 1.
Flow diagram of intervention and components of the restaurant-based fundraising and nutrition promotion on menu choices. FI indicates condition with Fundraising Incentive; F-HEI condition with Fundraising Healthy Eating Incentive. Process Evaluation data (placement of materials, weather, traffic, staff follow through, etc.) collected for implementation assessment.
Data Analysis
Feasibility.
Descriptive statistics (frequencies for categorical variables and means and standard deviations for continuous variables) were utilized to summarize recruitment and participation information, implementation fidelity, and intervention acceptability.
Efficacy.
Primary efficacy analyses were to compare relative ordering of healthy items between the two intervention groups (using receipt data and repeated in aggregate sales data for comparison), as well as to compare relative ordering of healthy items among all restaurant patrons during each intervention vs. comparison periods (in aggregate sales data). Chi square tests were used for each of these comparisons. The total donation gained from the fundraiser was also measured.
Sample size calculation.
In estimating the sample size needed to detect significant differences for efficacy analyses, we started with the effect size from a previous study examining changes in ordering of healthier menu items after healthy children’s menu changes(21), adjusting our estimate of the anticipated effect due to differences in the number of healthier menu options available. To detect an increase from 3% to 23% healthy items with alpha=.05 and power=.80, a sample of 44 orders per intervention time point was required (n=88). This sample size was feasible to expect in the receipt data based on enrollment in the study schools, historical target restaurant sales data, and estimated revenue from past Dine Out promotions.
Results
Feasibility
Recruitment and participation
All twelve schools from the school district agreed to participate in the research study. Characteristics of the school district population may be found in Table 1. The six schools participating in FI received a total of 4,991 flyers, based on student enrollment, and 49 (.98%) were collected at the restaurant during the intervention period. The remaining six schools received 3,442 flyers and 32 (.93%) were collected during F-HEI.
Table 1.
Characteristics of School Groups After Matching
| Group 1 (n=6 schools) | Group 2 (n=6schools) | School District Populationa (n=12 schools) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Number of students | 834.0 | 131.2 | 898.5 | 121.8 | 866.25 | 125.3 |
| Distanceb | 3.8 | 1.3 | 3.5 | 1.9 | 3.6 | 1.5 |
| Percent free and reduced lunch | 36.6 | 27.0 | 44.3 | 34.8 | 40.5 | 30.0 |
School district elementary school population.
Distance from school to restaurant.
Notes: Schools matched on enrollment, distance, and free and reduced meal eligibility using Mahalanobis. After matching the two groups did not differ on any of these characteristics (p>.05) although the present study was not powered to detect this difference. District data are from 2015–2016 Enrollment Demographics.
Participant receipts were collected from all orders submitted with a flyer. Eighty-one receipts were collected during the intervention periods, 49 during FI and 32 during F-HEI. Each receipt included an average of 4.4 total menu items ordered, with a range of 1–11 menu items. Three school staff submitted a flyer and ordered a menu item during F-HEI, which were included in the analysis. The school district raised $303.55 through the fundraising incentives for both intervention conditions combined.
Sixty-six parent/guardians (representing 85% of families who participated in the interventions) agreed to complete the survey (n=37 during FI, n=29 during F-HEI). Demographic characteristics of the survey participants (Table 2) were comparable to the overall target population of parents living in the same Southern CA county(22). Forty-five percent of respondents identified as Hispanic or Latino, 42% were White, 7.5% were Asian, and 5.5% identified as other races. Two of the three schools with the lowest participation were the farthest from the restaurant (6 miles), one of which also had a competing fundraiser during the intervention period. The third lowest participating school had the greatest percentage of students receiving free and reduced-price lunches (96%).
Table 2.
Demographic Characteristics of Behavioral Survey Respondents
| Characteristica | FI | F-HEI | Total | |||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||
| Gender (n=66) | ||||||
| Male | 18 (48.6) | 11 (37.9) | 29 (43.9) | |||
| Female | 19 (51.4) | 18 (62.1) | 37 (56.1) | |||
| Mean age, years (n=66) | ||||||
| 18 to 25 | 2 (5.4) | 0 (0.0) | 2 (3.0) | |||
| 26 to 40 | 16 (43.2) | 15 (51.7) | 31 (47.0) | |||
| 41 to 55 | 15 (40.5) | 12 (41.4) | 27 (40.9) | |||
| Over 56 | 4 (10.8) | 2 (6.9) | 6 (9.1) | |||
| Ethnicity (n=66) | ||||||
| Hispanic | 13 (35.1) | 4 (13.8) | 17 (25.8) | |||
| Non-Hispanic | 23 (62.2) | 25 (86.2) | 48 (72.7) | |||
| Prefer not to answer | 1 (2.7) | 0 (0.0) | 1 (1.5) | |||
| Race (n=60) | ||||||
| White | 24 (72.7) | 21 (77.8) | 45 (75.0) | |||
| Native Hawaiian or Other Pacific Islander | 1 (3.0) | 1 (3.7) | 2 (3.3) | |||
| Asianb | 2 (6.1) | 2 (7.4) | 4 (6.7) | |||
| Multiracial and Other | 5 (15.2) | 3 (11.1) | 8 (13.3) | |||
| Prefer not to answer | 1 (3.0) | 0 (0.0) | 1 (1.7) | |||
| Education (n=66) | ||||||
| High school graduate or less | 6 (16.2) | 5 (17.2) | 11 (16.7) | |||
| Some college/ Associate degree | 14 (37.8) | 4 (13.8) | 18 (27.3) | |||
| Bachelor’s degree | 7 (18.9) | 12 (41.4) | 19 (28.8) | |||
| Graduate degree | 9 (24.3) | 8 (27.6) | 17 (25.7) | |||
| Prefer not to answer | 1 (2.7) | 0 (0.0) | 1 (1.5) | |||
| Eligible for free/reduced price meals (n=66) | ||||||
| Yes | 5 (13.5) | 6 (20.7) | 11 (16.7) | |||
| No | 29 (78.4) | 21 (72.4) | 50 (75.8) | |||
| Do not know | 2 (5.4) | 2 (6.9) | 4 (6.1) | |||
| Prefer not to answer | 1 (2.7) | 0 (0.0) | 1 (1.5) |
Individual n values vary due to missing data.
Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, or other Asian.
Implementation fidelity
The intervention conditions were implemented per protocol: each intervention occurred Thursday through Sunday with researchers collecting data during all shifts. Nutrition promotion materials were placed in designated areas, where they remained for the duration of the study. The restaurant staff collected flyers and receipts as they were trained to do by research staff. Although the restaurant promoted several other menu items separately from the study promotions, these promotions were ongoing for this restaurant and were consistent for both intervention conditions (e.g. Taco Tuesday ($1.00 off any taco); Happy Hour Specials). Competing events on at least one day of intervention were reported among four schools during FI and two schools during F-HEI (Fun Run, Farmer’s Market). Weather was consistent across conditions and was typical for the region and time of year; temperatures were in the 60s with sunny and cloudy skies.
Intervention acceptability
Program acceptability was demonstrated through survey responses with all respondents indicating that they were “somewhat” (14.3%) or “very” (85.7%) likely to participate in a similar fundraiser in the future. Half of all respondents indicated that they ordered a healthier menu item as advertised on the promotional materials. Among survey respondents who reported choosing a healthier menu item, all reported liking their meal, and nearly 86.5% indicated they were “very” or “somewhat” likely to order the menu item again.
Nearly all respondents (95.4%) from both intervention conditions agreed or strongly agreed that the general (15%) fundraising incentive motivated them to visit the restaurant, and 55.2% of respondents from F-HEI agreed or strongly agreed that the additional incentive motivated them to order a healthier menu item. Yet among those who ordered a healthier menu item in F-HEI, only 9% reported making their meal choice based on the fundraising incentive to order a healthier meal. A summary of survey questions and responses may be found in Table 3.
Table 3.
Behavioral Survey Results Summary
| Question | Response | FI | F-HEI | Total | |||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||||
| 1. Which of the following best describes your dining experience today? (n=66) | I dined at the restaurant | 27 (73.0) | 17 (58.6) | 44 (66.7) | |||
| I did not dine at the restaurant (includes takeout orders) | 10 (27.0) | 12 (41.4) | 22 (33.3) | ||||
| 2. How often do you eat meals prepared away from home (restaurants, coffee shops, delis, fast food, take-out, etc.)? (n=66) | A few times a year | 3 (8.1) | 1 (3.4) | 4 (6.1) | |||
| Once a month | 1 (2.7) | 2 (6.9) | 3 (4.5) | ||||
| A few times a month | 17 (45.9) | 13 (44.8) | 30 (45.5) | ||||
| 1–3 times a week | 13 (35.1) | 10 (34.5) | 23 (34.8) | ||||
| 4 or more times a week | 3 (8.1) | 3 (10.3) | 6 (9.1) | ||||
| 3. How often do you eat at this restaurant location? (n=66) | Never | 13 (35.1) | 11 (37.9) | 24 (36.4) | |||
| A few times a year | 16 (43.2) | 11 (37.9) | 27 (40.9) | ||||
| Once a month | 4 (10.8) | 2 (6.9) | 6 (9.1) | ||||
| A few times a month | 3 (8.1) | 4 (13.8) | 7 (10.6) | ||||
| 1–3 times a week | 1 (2.7) | 1 (3.4) | 2 (3.0) | ||||
| 4. Did you order one or more of the following menu items? (Select all that apply) (n=66) | (List of HD/KLW menu items)* | 19 (51.4) | 16 (55.2) | 33 (50.0) | |||
| No, I didn’t order any of these menu items | 17 (45.9) | 13 (44.8) | 32 (48.5) | ||||
| No response/Skipped response | 1 (2.7) | 0 (0.0) | 1 (1.5) | ||||
| 5. Why did you choose the menu item you ordered today? (Select all that apply) (n=66) | Taste: My child likes the foods in that meal | 21 (56.8) | 17 (58.6) | 38 (57.6) | |||
| Habit: This is what my child usually has at this restaurant | 5 (13.5) | 5 (17.2) | 10 (15.2) | ||||
| Cost: Selected the meal based on its price | 0 (0.0) | 4 (13.8) | 4 (6.1) | ||||
| Nutrition: Selected the meal because it was health | 7 (18.9) | 2 (6.9) | 9 (13.6) | ||||
| Promotion: I saw this meal promoted on a poster/sign/menu in the restaurant | 4 (10.8) | 4 (13.8) | 8 (12.1) | ||||
| Other reason (specify) | 4 (10.8) | 4 (13.8) | 8 (12.1) | ||||
| Donation: Selected the meal because the additional 10% will be donated to my school† | 0 (0.0) | 6 (20.7) | 6 (9.1) | ||||
| 6. Please indicate the overall liking of your meal. (n=66) | Like extremely | 5 (13.5) | 6 (20.7) | 11 (16.7) | |||
| Like very much | 13 (35.1) | 7 (24.1) | 20 (30.3) | ||||
| Like moderately | 9 (24.3) | 3 (10.3) | 12 (18.2) | ||||
| Neither like nor dislike | 1 (2.7) | 1 (3.4) | 2 (3.0) | ||||
| Not applicable | 5 (13.5) | 11 (37.9) | 16 (24.2) | ||||
| No response/Skipped response | 4 (10.8) | 1 (3.4) | 5 (7.6) | ||||
| 7. How likely are you to order this menu item again? (n=66) | Very likely | 26 (70.3) | 17 (58.6) | 43 (70.5) | |||
| Somewhat likely | 5 (13.5) | 5 (17.2) | 10 (16.4) | ||||
| Neutral | 4 (10.8) | 1 (3.4) | 5 (8.2) | ||||
| Somewhat unlikely | 0 (0.0) | 1 (3.4) | 1 (1.6) | ||||
| Very unlikely | 1 (2.7) | 1 (3.4) | 2 (3.3) | ||||
| Not applicable | 1 (2.7) | 4 (13.8) | 2 (3.3) | ||||
| 8. How likely are you to participate in a SchooLicious Dine Out Fundraiser in the future? (n=66) | Very likely | 30 (81.1) | 24 (82.8) | 54 (81.1) | |||
| Somewhat likely | 5 (13.5) | 4 (13.8) | 9 (13.6) | ||||
| No response/Skipped response | 2 (5.4) | 1 (3.4) | 3 (4.5) | ||||
| 9. To what extent do you agree or disagree with the following statements? | |||||||
| 9a. The 15% donation to my school from the Dine Out fundraiser motivated me to visit this restaurant today. (n=66) | Strongly agree | 26 (70.3) | 25 (86.2) | 51 (77.3) | |||
| Agree | 7 (18.9) | 4 (13.8) | 11 (16.7) | ||||
| Neutral | 3 (8.1) | 0 (0.0) | 3 (4.5) | ||||
| No response/Skipped response | 1 (2.7) | 0 (0.0) | 1 (1.5) | ||||
| 9b. The additional 10% donation to my school motivated me to order a healthy choice.‡(n=29) | Strongly agree | 13 (44.8) | 13 (44.8) | ||||
| Agree | 3 (10.3) | 3 (10.3) | |||||
| Neutral | 9 (31.0) | 9 (31.0) | |||||
| Disagree | 4 (13.8) | 4 (13.8) | |||||
Collapsed list of Healthy Dining (HD) and Kids Live Well (KLW) menu items.
Answer only applicable to F-HEI
Question only applicable to F-HEI.
Intervention Efficacy
Comparing Orders of Healthier Items between the Two Intervention Conditions
Of the 141 items ordered by participants during FI, 15.6% were healthier items, and of the 90 items ordered in F-HEI, 21.1% were healthier items. Although in the expected direction, the difference in ordering of healthier items between the two conditions was not statistically significant (χ2 =1.14, p=.29). Results were similar in the aggregate sales data (Table 4).
Table 4.
Relative orders of healthier menu items by study period
| Comparisons | n (%) Healthier Item Orders | Chi-square | p-value |
|---|---|---|---|
| Comparison 1 | 70 (6.9) | 1.59 | 0.21 |
| FI | 108 (8.4) | ||
| Comparison 1 | 70 (6.9) | 3.37 | 0.07 |
| F-HEI | 101 (9.1) | ||
| FI | 108 (8.4) | 5.97 | 0.01** |
| Comparison 2 | 55 (5.7) | ||
| F-HEI | 101 (9.1) | 8.84 | 0.003** |
| Comparison 2 | 55 (5.7) | ||
| FI | 108 (8.4) | 0.47 | 0.49 |
| F-HEI | 101 (9.1) | ||
| FIa | 22 (15.6) | 1.14 | 0.29 |
| F-HEIa | 19 (21.1) |
FI indicates Fundraising Incentive; F-HEI: Fundraising-Healthy Eating Incentive;
P<.01.
Receipt data: Comparison of % healthier item orders between FI and F-HEI performed using more precise receipt data. All other rows show comparisons using aggregate sales data.
Comparing Orders of Healthier Items during Intervention Periods vs. Comparison Periods
The percentage of healthier items ordered was significantly greater during both FI (χ2=5.97, p=.01) and F-HEI (χ2=8.84, p=.003) versus Comparison 2. Results were similar but did not reach statistical significance when comparing the interventions to Comparison 1.
Discussion
Results from this pilot study indicate initial promise of a collaborative healthy eating and school wellness fundraising program between schools and restaurants and also highlight areas for future research.
The study was implemented with full cooperation from the school district with all schools agreeing to participate. Among the families who took the survey, all indicated they would participate again in a similar program, most were motivated by the fundraising incentive to visit the restaurant (95%), and more than half were motivated by the additional incentive to order a healthier menu item (55%). Despite acceptability among this group, parents who did not participate in the intervention may not have approved of the program, a factor that could be explored in future research. Demographic characteristics of survey participants were comparable to both state and country demographics with respect to gender, race, education, and income(22) suggesting that the sample, while small, was representative of California and US school families. Given that San Diego area residents may be more health conscious than other parts of the United States(23), additional research is needed to inform generalizability beyond this area.
In terms of fidelity, all intervention procedures were followed, monitored, recorded, and analyzed as intended. Conducting nutrition research in the restaurant setting and collaborating with restaurant administration can be challenging due to differing priorities and goals. Establishing “buy-in” from the restaurant was imperative in implementing research methodology and collecting reliable data. We hypothesize this success was due to 1) consistent communication (and training) between the research team and the participating restaurant, 2) mutual benefit to all parties involved, and 3) starting small: implementing at one location over a relatively short timeline with the intent to scale up once roles, responsibilities and relationships were established.
Efficacy results provide initial promising evidence that fundraising incentives coupled with point-of-purchase promotions of healthier menu items may increase healthier items ordered in a collaborative school and restaurant-based intervention. Specifically, aggregate sales data provided some evidence that sales of healthier menu items were greater during intervention periods versus comparison periods. Given low rate of flyer turn-in, these results may reflect the influence of point-of-purchase promotions. There was no significant difference in healthier item orders between intervention periods suggesting the additional fundraising incentive was not an impactful strategy to increase healthier items ordered. However, healthier item promotional materials were displayed throughout both intervention periods potentially mitigating the effect of the healthier item fundraising incentive, and the sample size was limited in the analysis of participating school families’ receipts. While direct comparisons of FI and F-HEI did not reveal significant differences in the relative percentage of healthier items ordered, the significant difference in healthier orders during intervention versus comparison periods was most robust for F-HEI, with consistent evidence of increases in healthier items ordered regardless of the comparison period used. Because aggregate sales data included all customers rather than just those participating in the fundraising intervention, the conclusions made based on the sales data cannot be generalized to school families alone. These results could be considered a conservative assessment of the intervention, as patrons who are not from the target population are included in the sample and would have been exposed to the nutrition information component of the both conditions, but not the fundraising incentives.
We do not know whether the present results affected children’s eating behaviors specifically, given that incentives were targeted to adults and only standard menu items were promoted. In future research, it would be interesting to examine the effects of this type of intervention on different family members.
Healthy eating promotions in restaurants may raise the concern that the promotion may encourage families to dine out, being counter-productive to nutrition programming. In this study, only 6% of survey respondents reported that they dine out less than one time per month suggesting that these promotions did not attract infrequent diners. Additionally, 44% of respondents indicated that they eat away from home at least once per week, thus attracting a population who may benefit most from a restaurant-based healthy eating intervention.
Only 9% of survey respondents reported selecting the healthier menu item because of the fundraising incentive; coupled with the comparison of FI versus F-HEI, these results suggest that the additional incentive to order a healthier menu item did not motivate the targeted behavior change. Parents may have felt that the 15% donation was sufficient and that the additional 10% donation for ordering a healthier menu item was unnecessary. The majority of participants did agree that this initial incentive motivated them to visit the restaurant that day.
While the successful aspects of the present study highlight opportunities to continue research in this area on a larger scale in the future, limitations of the present study should be addressed prior to such expansion. As mentioned above, a primary limitation of this study is that the intervention participation rates were lower than anticipated for both intervention periods generating fewer receipts than the calculated sample size targets. Flyers were distributed at the individual level and collected at the family/order level potentially underestimating true participation rates. Nevertheless, there is clearly room to improve participation rates in the future.
Because different restaurants vary in terms of their consumer base and the healthfulness of the core items sold, it would be important to test this approach in a wider variety of restaurants to shed light on generalizability and the extent to which school family participation rates are tied to restaurant choice.
Likewise, we don’t know the extent to which this specific fundraising initiative was motivating to parents, which could be a factor contributing to low participation rates. While participants were aware that the funds were being raised for school wellness programs in general, parents may want to know and/or choose specifics of the fundraising goals (target and amount). Future research can shed light on this by talking with parents about their motivation to support different types of school fundraisers.
Finally, incentive amounts were finalized with restaurant operators; however, further dose response research may be completed to determine the optimum incentive amount required to motivate parents to select healthier menu items.
Improving recruitment in future studies can bolster benefits for participating schools. In this pilot, the total donation to school wellness programs from FI and F-HEI was $303.55 for all twelve participating schools, amounting to a minimal benefit for each school. Lower prices of meals at fast-casual restaurants result in a reduced donation amount as compared with table-service restaurants. While selecting higher price-points would increase per-order donations, volume of participants may be further reduced due to affordability of menu items.
Additionally, it was not possible to examine clustering of orders within schools within the sales data given that these data were aggregated (and included patrons who are not affiliated with the study schools). Future research should be designed to further investigate the promise of the present approach while being able to accommodate clustering in data analyses.
Creating public-private partnerships with the restaurant industry may be a useful strategy to expand healthier menu item availability and purchases and improve dietary habits of restaurant patrons. Overall, findings suggest that the use of the initial fundraising incentive plus healthy eating promotions (non-incentive-based strategies) to promote healthier items at point of purchase are promising avenues to pursue, although future research is needed to understand the extent to which refinements to the present study’s design (e.g., a wider variety of restaurants, different targeting of funds raised for schools, different incentive amounts) may bolster participation rates. Future studies could build on these techniques aiming to increase participation and the consumption of the healthier options beyond that observed in the present study.
Acknowledgments:
The authors thank Anita Jones-Mueller, Nicole Ring, the participating school district and its elementary schools and our restaurant partner.
Financial Support: This study was funded by the National Cancer Institute of the National Institutes of Health under Award Number 5R44CA192374. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder had no role in the design, analysis, or writing of this article.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Ethical Standards Disclosure
This study was conducted according to guidelines laid down by the Declaration of Helsinki and all procedures involving research study participants were approved by IRB Company, Inc. (IRB.co) in Buena Park, CA. A partial waiver of informed consent was used; participants were asked to read an information sheet prior to participation.
Contributor Information
Shawna L. McNally, Department of Research, Accents on Health, Inc. (dba Healthy Dining), 8745 Aero Dr. Suite 306, San Diego, CA 92123
Stephanie Anzman-Frasca, Department of Pediatrics, University at Buffalo, 3435 Main Street, Buffalo, NY 14214.
Kelly Bowman, Virginia Department of Education, James Monroe Building, 101 N 14th St., Richmond, VA 23219.
Mariana Beleche, Department of Research, Accents on Health, Inc. (dba Healthy Dining), 8745 Aero Dr. Suite 306, San Diego, CA 92123.
Sara C. Folta, Friedman School of Nutrition Science and Policy, Tufts University, 150 Harrison Ave, Boston, MA 02111
Anjali Patel, Department of Research, Accents on Health, Inc. (dba Healthy Dining), 8745 Aero Dr. Suite 306, San Diego, CA 92123.
References
- 1.Currie J, Vigna SD, Moretti E, et al. (2010) The effect of fast food restaurants on obesity and weight gain. Am Econ J Econ Policy 2, 32–63. [Google Scholar]
- 2.Seguin RA, Aggarwal A, Vermeylen F, et al. (2016) Consumption frequency of foods away from home linked with higher body mass index and lower fruit and vegetable intake among adults: a cross-sectional study. J Environ Public Health. Published online: 26 January 2016. doi: 10.1155/2016/3074241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin BH, Guthrie J (2012) Nutritional quality of food prepared at home and away from home, 1977–2008. EIB-105, USDA, Economic Research Service; https://www.ers.usda.gov/publications/pub-details/?pubid=43699 (accessed August 2019). [Google Scholar]
- 4.Morland KB, Evenson KR (2009) Obesity prevalence and the local food environment. Health Place 15, Suppl. 2, 491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowman SA, Vinyard BT (2004) Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr 23, Suppl. 2, 163–8. [DOI] [PubMed] [Google Scholar]
- 6.Ayala GX, Rogers M, Arredondo EM, et al. (2008) Away-from-home food intake and risk for obesity: examining the influence of context. Obesity 16, Suppl. 5,1002–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lachat C, Nago E, Verstraeten R, et al. (2012) Eating out of home and its association with dietary intake: a systematic review of the evidence. Obes Rev 13, Suppl. 4, 329–46. [DOI] [PubMed] [Google Scholar]
- 8.Policastro P, Palm T, Schwartz J, et al. (2017) Targeted calorie message promotes healthy beverage consumption better than charity incentive. Obesity 25, Suppl. 8, 1428–1434. [DOI] [PubMed] [Google Scholar]
- 9.Valdivia Espino JN, Guerrero N, Rhoads N, et al. (2015) Community-based restaurant interventions to promote healthy eating: a systematic review. Prev Chronic Dis 12, 140455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wall J, Mhurchu CN, Blakely T, et al. (2006) Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev 64, 518–31. [DOI] [PubMed] [Google Scholar]
- 11.Harkins KA, Kullgren JT, Bellamy SL, et al. (2017) A trial of financial and social incentives to increase older adults’ walking. Am J Prev Med. Published online: 3 January 2017. doi: 10.1016/j.amepre.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 12.French SA, Rydell SA, Mitchell NR, et al. (2017) Financial incentives and purchase restrictions in a food benefit program affect the types of foods and beverages purchased: results from a randomized trial. Int J Behav Nutr Phys Act 14, 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardiner CK, Bryan AD (2017) Monetary incentive interventions can enhance psychological factors related to fruit and vegetable consumption. Ann Behav Med 51, 599–609. [DOI] [PubMed] [Google Scholar]
- 14.Polacsek M, Moran A, Thorndike AN, et al. (2017) A supermarket double-dollar incentive program increases purchases of fresh fruits and vegetables among low-income families with children: the healthy double study. J Nutr Educ Behav. Published online: 7 November 2017. doi: 10.1016/j.jneb.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Volpp KG, John LK, Troxel AB, et al. (2008) Financial incentive-based approaches for weight loss: a randomized trial. JAMA 300,2631–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (2018) Adult Obesity Facts: Obesity is common, serious, and costly. https://www.cdc.gov/obesity/data/adult.html (accessed August 2019). [Google Scholar]
- 17.Powell LM, Nguyen BT (2013) Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatr 167, 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell L, Nguyen B, Han E. (2012) Energy intake from restaurants: demographics and socioeconomics, 2003–2008. American Journal of Preventative Medicine.43(5), 498–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song M, Herman R. (2010) A practical guide on designing and conducting impact studies in education: lessons learned from the what works clearinghouse (phase I). Washington, DC: American Institutes for Research; 2010. http://www.air.org/sites/default/files/downloads/report/Song__Herman_WWC_Lessons_Learned_2010_0.pdf (accessed August 2019). [Google Scholar]
- 20.Nutrition criteria: the Healthy Dining recommended nutrition criteria. Healthy Dining Finder. https://www.healthydiningfinder.com/About-This-Site/nutrition-criteria (accessed August 2019). [Google Scholar]
- 21.Anzman-Frasca S, Mueller MP, Sliwa S, et al. (2015) Changes in children’s meal orders following healthy menu modifications at a regional U.S. restaurant chain. Obesity (Silver Spring) 23, Suppl. 5, 1055–62. [DOI] [PubMed] [Google Scholar]
- 22.US Census Bureau (2018) QuickFactsCalifornia. https://www.census.gov/quickfacts/fact/table/CA,US/IPE120216#viewtop (accessed August 2019). [Google Scholar]
- 23.American College of Sports Medicine (2017) American Fitness Index announces fittest cities in the United States. ACSMs Health Fit J 21, Suppl. 4, 2. doi: 10.1249/FIT.0000000000000302 [DOI] [Google Scholar]