INTRODUCTION
IGH-CRLF2 rearrangement is the most common mechanism of overexpression of cytokine receptor like factor 2 (CRLF2) in precursor B-cell acute lymphoblastic leukemia (B-ALL); however, P2RY8-CRLF2 rearrangement or alternative alterations leading to CRLF2 overexpression have also been observed, which are associated with increased relapse rate and progression1. Although many myeloid neoplasms, particularly acute myeloid leukemia (AML), are associated with various recurrent genetic rearrangements and fusions2, alterations leading to CRLF2 overexpression are exceedingly rare in AML. To date, no case of myeloid neoplasm with CRLF2 translocation has been reported. One case of MDS-EB1 with CRLF2 overexpression has been reported via multiple copies of an isodicentric Y chromosome, without evidence of CRLF2 rearrangement3. Here we report the first case of AML arising from an antecedent myelodysplastic syndrome (MDS), with a P2RY8-CRLF2 fusion, which responded to a myeloid regimen on a clinical trial of hypomethylating agent and immune checkpoint blockade combination therapy.
CASE REPORT
A 78-year-old man carried an initial diagnosis of myelodysplastic syndrome with excess blasts 1 (MDS-EB1) for one year, with a bone marrow showing 8% blasts by aspirate differential count and 5–9% blasts by CD34 immunostain (Appendix Figure A1A). He was monitored without any treatment or transfusions before presenting to Memorial Sloan Kettering Cancer Center (MSKCC) with worsening pancytopenia, including severe neutropenia. Bone marrow examination showed ~40% blasts that were medium in size with a rim of vacuolated cytoplasm, dispersed chromatin and inconspicuous nucleoli (Figure 1A), consistent with progression to AML. Flow cytometry confirmed the presence of an expanded blast population with predominantly abnormal myeloid immunophenotype, but a minute subset of blasts dimly expressed CD19 (Figure 1B). Despite this, the case is best classified as acute myeloid leukemia with myelodysplasia-related changes (AML-MRC) based on the 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemias2.
Figure 1. Acute myeloid leukemia with myelodysplasia-related changes with P2RY8-CRLF2 fusion.
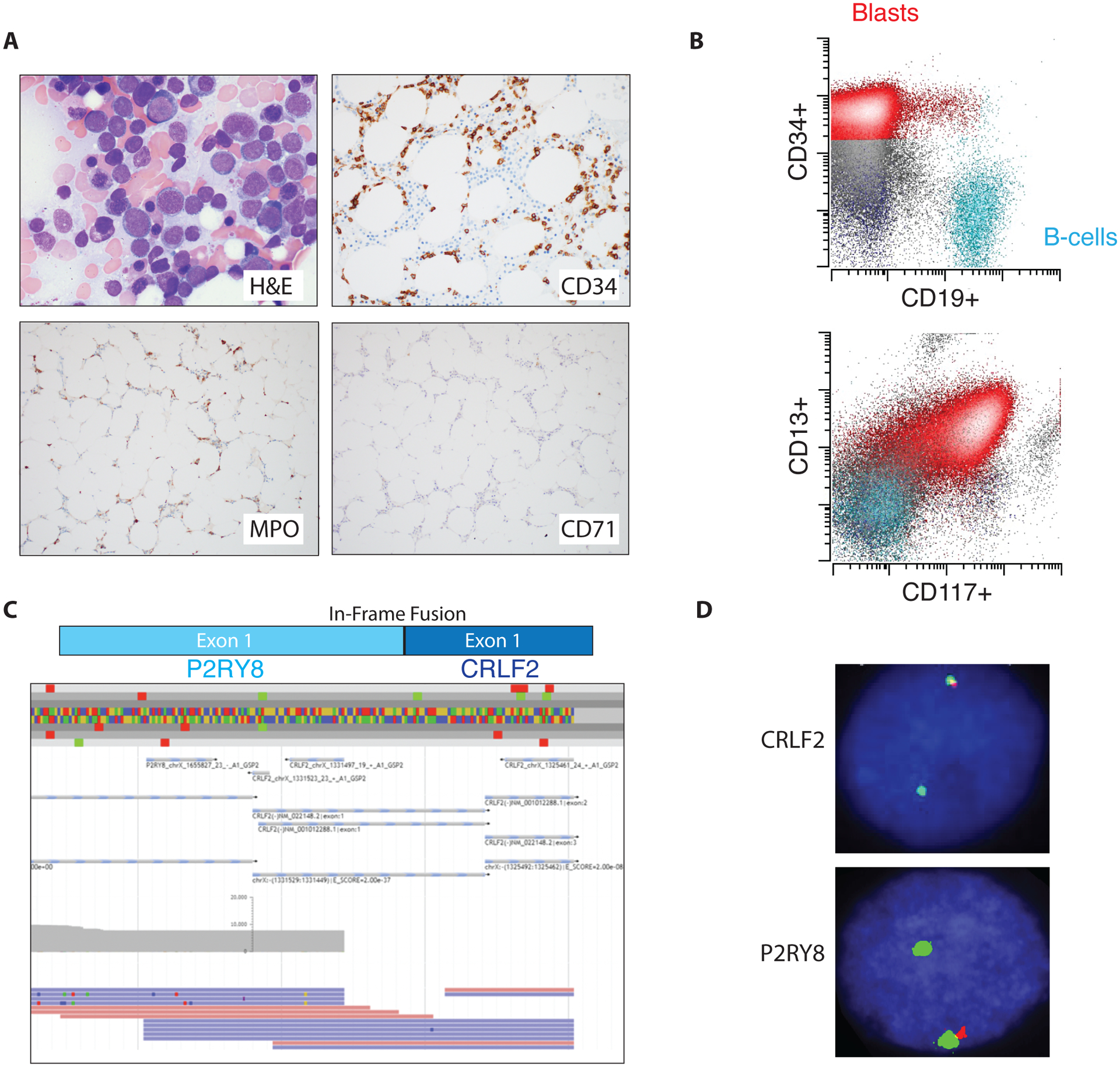
(A) Photomicrographs of the bone marrow biopsy showing acute myeloid leukemia (AML). (B) Flow cytometry of the bone marrow aspirate showing typical AML markers. (C) Anchored multiplex PCR (Archer FusionPlex) reads showing an in-frame fusion between P2RY8 and CRLF2. (D) Break-apart fluorescence in-situ hybridization probes for CRLF2 (top) and P2YR8 (bottom) consistent with interstitial deletion between the two genes resulting in fusion.
COMPREHENSIVE GENOMIC/TRANSCRIPTOMIC PROFILING
Fluorescence in-situ hybridization (FISH) analysis performed on the marrow at the time of the initial diagnosis of MDS-EB1 was negative for recurring MDS related chromosome abnormalities, including deletion or loss of chromosomes 5, 7, 13, 17 and 20, gain of chromosome 8, and for KMT2A (MLL) translocations. At MSKCC, karyotype analysis of the AML bone marrow aspirate specimen showed a normal male karyotype, and FISH analysis was negative for the presence of KMT2A (MLL), EVI1, CBFB translocations, and TP53 deletion. A targeted next generation sequencing panel (MSK IMPACT Heme panel; Memorial Sloan Kettering Cancer Center, New York, NY) was performed on the bone marrow specimen obtained at the time of the AML diagnoses, which showed the alterations listed in Table 1, including mutations in ASXL1, KMT2D, RUNX1, SF3B1, TET2, PHF6, RAD21, and XBP1. Evaluation of this bone marrow sample using an anchored multiplex PCR-based, targeted RNA sequencing assay for detection of fusions (Archer FusionPlex, ArcherDx, Inc. Boulder, CO) revealed the presence of a fusion between exon 1 of P2RY8 and exon 1 of CRLF2 (Figure 1C). This fusion was confirmed in 22% of cells using FISH break apart probes for CRLF2 and P2RY8 (Xp22.33/Yp11.32, Cytocell, Tarrytown, NY; Figure 1D). The signal pattern was consistent with an interstitial deletion between the P2RY8 and CRLF2 genes within the pseudoautosomal region 1 (PAR1).
Table 1.
Comparison of molecular findings in the patient’s marrow samples obtained at the time of myelodysplastic syndrome with excess blasts-1 (MDS-EB1) and acute myeloid leukemia with myelodysplasia-related changes (AML-MRC).
| Mutational Profiling | Variant Allele Frequencies (VAF %) | |
|---|---|---|
| MDS-EB1 Marrow (May 2017) | AML-MRC Marrow (Sept 2018) | |
| ASXL1 c.1900_1922del (p.E635Rfs*15) | 14.4% | 19.8% |
| KMT2D c.10505_10506insTTTACCC (p.N3503Lfs*4) | 5.5% | 7.6% |
| RUNX1 c.497G>A (p.R166Q) | 5.8% | 17.5% |
| SF3B1 c.1774G>A (p.E592K) | 25.6% | 18.9% |
| TET2 c.4138C>T (p.H1380Y) | 8.3% | 17.1% |
| SETD1B c. 2502G>A (p.W834*) | 7.7% | <1.0% |
| PHF6 c.673C>T (p.R225*) | 0.0% | 20.2% |
| RAD21 c.371_372insTGAGGGCGGA (p.L124Ffs*6) | 0.0% | 5.7% |
| XBP1 exon 1 deletion | Not present | Present (VAF not available) |
To ensure that the P2RY8-CRLF2 rearrangement observed was present in the myeloid blasts rather than cells of other lineages, bone marrow mononuclear cells were separated by fluorescence activated cell sorting (FACS) to isolate the leukemic blasts, myelomonocytic cells and normal lymphocytes. FISH using the CRLF2 break apart probe revealed the CRLF2 rearrangement in a subset of the myeloid blasts (27.5%) and myelomonocytic cells (19.5%) but not in B-cells (Figure 2).
Figure 2. Confirmation of P2RY8-CRLF2 fusion in myeloid lineage.
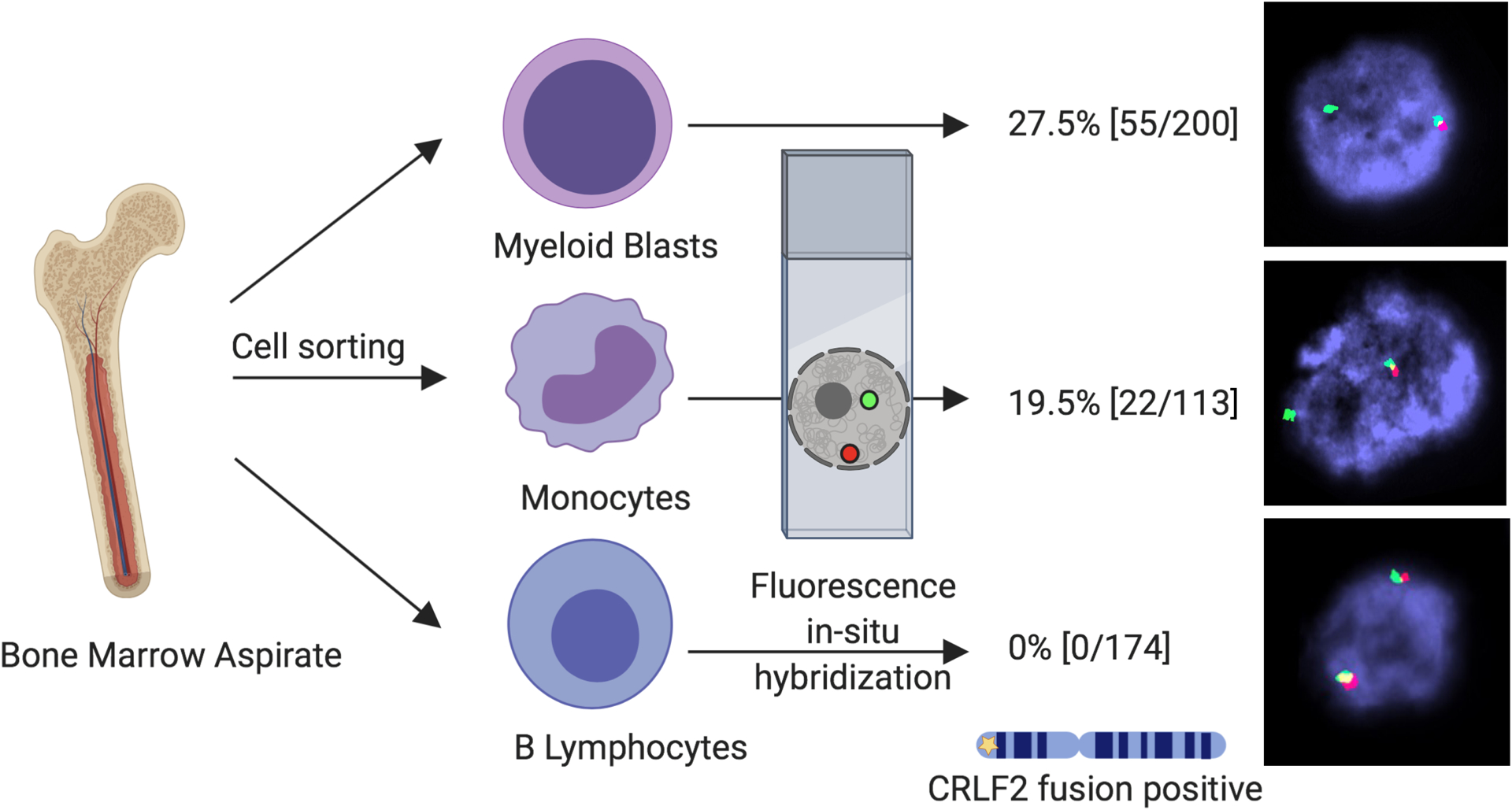
The bone marrow aspirate sample was sorted by fluorescence activated cell sorting (FACS) into the myeloid blast population, myelomonocytic cells and B lymphocytes. Breakapart fusion probes were applied to the sorted populations showing restriction of the P2RY8-CRLF2 fusion to the myeloid lineage including the blasts and myelomonocytes.
FISH evaluation of the prior bone marrow biopsy with MDS-EB1 was also performed, which showed the presence of the P2RY8-CRLF2 rearrangement in 10% of the cells (Appendix Figure A1C). Archer FusionPlex of the prior marrow with MDS-EB1 also identified the same fusion between exon 1 of P2RY8 and exon 1 of CRLF2 (Appendix Figure A1B). Oncoscan array of the MDS-EB1 biopsy did not reveal any unbalanced genomic changes, or copy-neutral loss of heterozygosity (CN-LOH)(data not shown), consistent with the normal FISH study observed by the outside institution a year prior. Targeted NGS sequencing (MSK IMPACT heme panel) of the MDS-EB1 bone marrow specimen also showed overlapping mutations with the AML bone marrow sample (Table 1), but with acquisition of new mutations (PHF6, RAD21, XBP1) in the AML sample, suggesting a myeloid primed hematopoietic stem cell/progenitor origin and clonal evolution with expansion of the clone with the P2RY8-CRLF2 rearrangement likely due to acquisition of a loss-of-function mutation in PHF6 mutation, which led to down-regulation of genes involved in normal B-cell development4.
Total RNA sequencing of the AML bone marrow specimen further confirmed the presence of the P2RY8-CRLF2 fusion along with overexpression of CRLF2 (Figure 3A). Principal component analysis comparing our patient to cohorts of AML or B-ALL from the TARGET study5 showed that the patient’s neoplasm clustered with other AML cases confirming the myeloid differentiation of the blasts (Figure 3B). Gene ontology analysis showed transcriptome-wide increases in cytokine-related signaling pathway genes potentially related to the P2RY8-CRLF2 fusion, as well as genes involved in regulating hematopoietic progenitor cell differentiation and the spliceosome (Figure 3C).
Figure 3. Transcriptomic analysis of P2RY8-CRLF2 fusion AML.
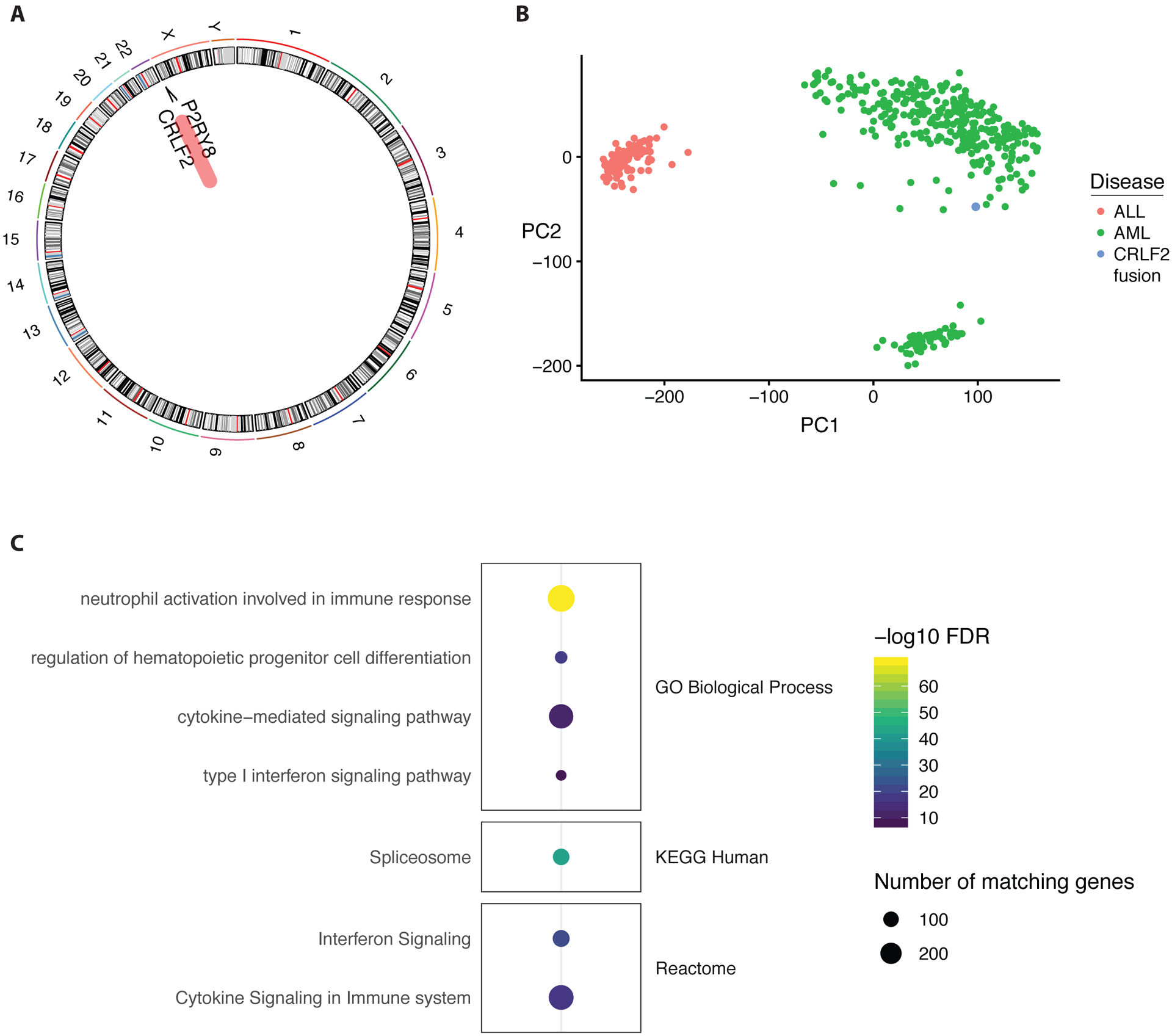
(A) Fusion analysis performed from polyA selected mRNA next-generation RNA sequencing. (B) Principal component analysis (PCA) plot showing two strongest principal components (PC1 on x-axis and PC2 on y-axis) from publicly available data from AML (green dots) and B-ALL (red dots) patient samples compared to our patient with P2RY8-CRLF2 fusion (blue dot). (C) Gene ontology analysis of the most highly expressed genes showing enrichment in hematopoietic differentiation, spliceosome, and immune signaling gene pathways. GO: Gene Ontology. KEGG: Kyoto Encyclopedia of Genes and Genomes
Since it is known that STAT5 is activated by P2RY8-CRLF2 fusion in B-ALL, we performed immunohistochemistry (IHC) using phosphorylation specific antibodies that showed increased STAT5 phosphorylation and partial ERK phosphorylation but not STAT3 phosphorylation (Figure 4A). Gene expression and IHC were largely correlated; however, the results are interpreted in the context of the importance of signaling in leukemia overall and these are not necessarily specific for P2RY8-CRLF2 fusion.
Figure 4. Immune signaling activation in P2RY8-CRLF2 fusion AML.
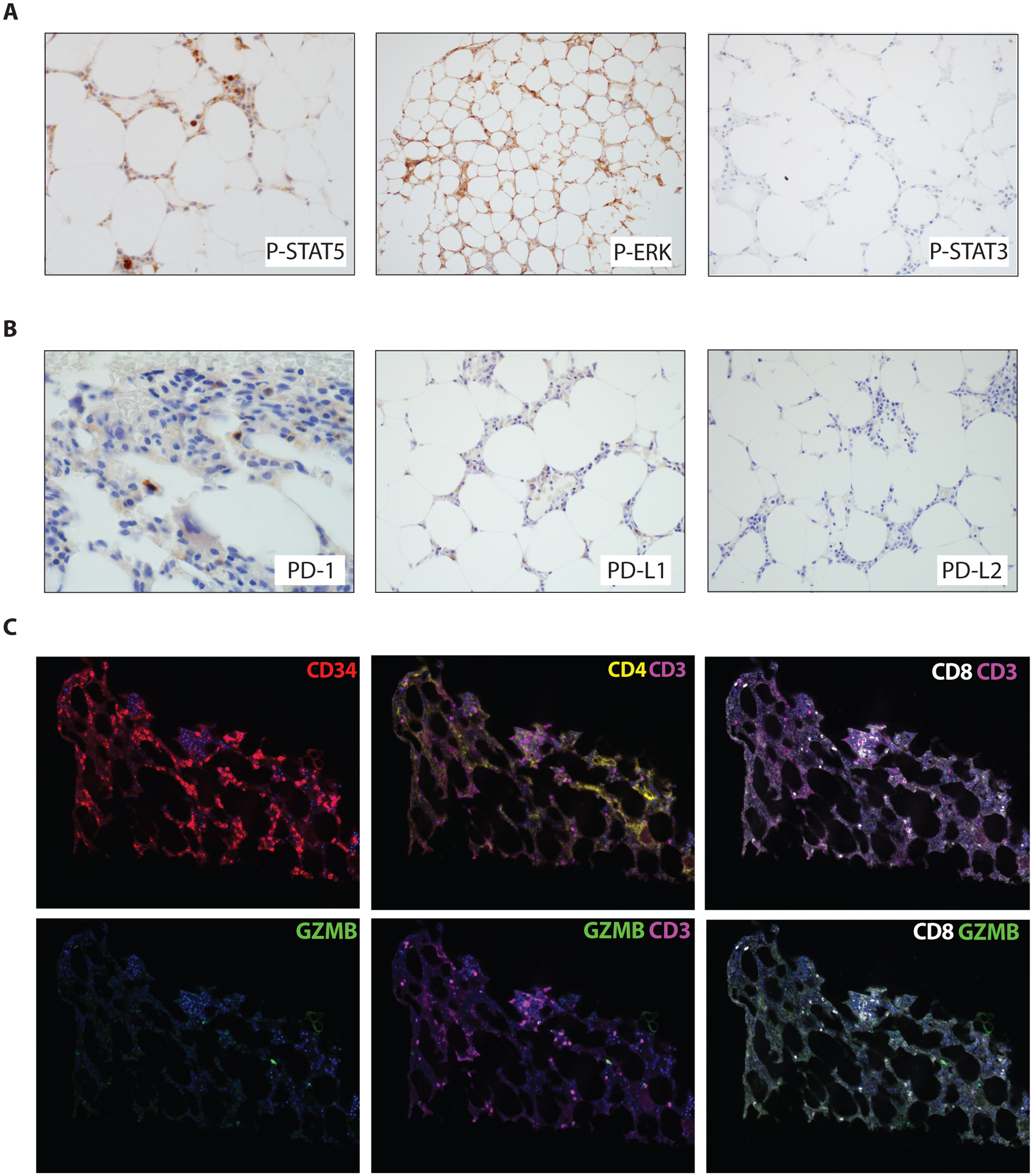
(A) Immunohistochemical photomicrographs of the bone marrow biopsy showing phospho-specific staining of STAT5 and ERK, but not STAT3. (B) Immunohistochemical photomicrographs of the bone marrow biopsy showing staining of PD-1 in scattered lymphoid cells. PD-L1 staining is equivocal, while PD-L2 is negative. (C) Using multiplex immunofluorescence microscopy, with digital image analysis, we find that the patient’s bone marrow is highly enriched with CD8+GZMB+ T-cells. CD34+ staining highlights the myeloblast population at the time of AML transformation. We further identify a population of CD3+CD4+ T-cells at baseline.
TREATMENT AND FOLLOW-UP
Given the patient’s age and transformation to AML, a clinical trial was recommended. He was consented and enrolled onto a study regimen consisting of standard dosed decitabine plus investigational administration of the cytotoxic T-lymphocyte associated protein-4 (CTLA-4) antagonist, ipilimumab (NCT02890329). After two cycles of combination therapy, he achieved complete remission with incomplete count recovery and shortly thereafter a full complete remission (Table 2) with negative measurable residual disease (MRD) status by a flow cytometric assay with a detection limit of 1 in 2500 cells. This was accompanied by a robust molecular response with undetectable levels of the previously-detected PHF6, RUNX1, TET2 and RAD21 mutations, and a marked reduction in the variant allele frequencies for the mutations ASXL1 (0.4%) and SF3B1 (1.4%), likely representing MRD below the detection limit of flow cytometry. The patient continues to be in morphologic remission and in cycle 11 of investigational therapy at time of this report. Immunohistochemistry was performed on the checkpoint molecules including PD-1, PDL1 and PDL2 (Figure 4B). The PD-1 stain was positive in scattered T-cells. While the PDL1 stain showed equivocal results, gene expression by RNA-sequencing was at the 75th percentile compared to other profiled AML. Multiplexed immunofluorescence with a panel of antibodies against CD34, CD3, CD4, CD8 and Granzyme B (GZMB), as previously described6, was applied to his pre-treatment bone marrow, which revealed the presence of a dense tumor immune infiltrate that was CD8+ GZMB+, suggesting his marrow was enriched with activated CD8 T cells critical for response to checkpoint blockade (Figure 4C).
Table 2.
Complete blood count and bone marrow parameters over time
| Parameter (range) | MDS diagnosis | AML-MRC diagnosis | Post Cycle 2 | Post Cycle 4 |
|---|---|---|---|---|
| WBC K/μL (4.0–11) | 2.3 | 0.8 | 6.8 | 4.5 |
| Hgb g/dL (12.5–16.2) | 13.6 | 8.0 | 9.6 | 12.8 |
| PLT K/μL (150–400) | 40 | 54 | 104 | 143 |
| ANC K/μL (1.5–7.5) | 1.4 | 0.2 | 0.24 | 1.4 |
| BM Blasts | 8% | 40% | <5% | 2% |
WBC = white blood cells, Hgb = hemoglobin, PLT = platelets,
ANC = absolute neutrophil count, BM = bone marrow
DISCUSSION
CRLF2 is the protein product of a synonymous gene located in the pseudoautosomal region 1 (PAR1) on the short arm of the X chromosome and the Y chromosome. It forms a heterodimer with interleukin 7 receptor alpha (IL7RA) and is involved in lymphoid signaling pathways. Activation of this receptor leads to activation of Janus family tyrosine kinases (JAK) and STAT5. Deregulated expression of this gene has been described as the characteristic alteration in Philadelphia chromosome-like (Ph-like) B-ALL in adolescent and adult patients7,8. Russell et al. showed that this subgroup of B-ALL has either a translocation juxtaposing the CRLF2 to the IGH gene on chromosome 14 (t(X;14)(p22;q32) or t(Y;14)(p11;q32)) or a deletion of PAR1 region, resulting in overexpression of the CRLF2 gene9. Mulligan et al. reported that the interstitial deletion of PAR1 leads to juxtaposition of CRLF2 to the first, non-coding exon of P2RY8. This event was seen in up to 7% of childhood B-ALLs and in up to half of Down syndrome patients presenting with ALL10.
Dysregulated expression of CRLF2 has been shown to occur both as early events (founder or truncal alteration), mostly seen as IGH-CRLF2 fusion, and as late events, often observed as P2RY8-CRLF2 fusion. This has been observed in Down syndrome related ALL as well as non-Down syndrome ALL supporting the cooperation of CRLF2 events with other genetic alterations in progression of disease11. However, irrespective of the clone size, presence of this rearrangement is associated with higher relapse rate12. There have been suggestions that the increased relapse rate may be due to other concurrent alterations such as IKZF1 deletion13. However, other studies have shown the rearrangement as well as the CRLF2 overexpression to be independent predictors of worse outcome in B-ALL14,15.
Until now, only one case of myeloid neoplasm with CRLF2 overexpression has been reported. However, this case was associated with multiple copies of an isodicentric Y chromosome and not associated with P2RY8-CRLF2 rearrangement3. To our knowledge, our case represents the first P2RY8-CRLF2 rearrangement in myeloid neoplasms, which in our case was an AML arising from the underlying MDS. Although this rearrangement was previously thought to originate from B lymphocytes due to it being only observed in B-ALL, this was not the case for our patient. The flow sorted FISH analysis has shown that the P2RY8-CRLF2 was not present in the B-lymphocytes of this patient but only in the myeloid-lineage cells (myeloid blasts and myelomonocytic cells). In addition, based on the results from total RNA sequencing, our patient’s neoplasm clustered with other AML cases, providing further evidence for the myeloid differentiation of the blasts. Furthermore, the alterations observed in this patient, including the P2RY8-CRLF2 rearrangement, were present at the MDS stage suggesting a stem cell origin with selective pressure leading to development of AML.
PHF6 mutations are rare in de novo AML but relatively common in AML-MRC and exceedingly rare in B-ALL16,17. PHF6 along with DNMT3A are the most common mutations in mixed phenotype acute leukemias (MPAL) with T-lineage differentiation18. PHF6 is a critical component in lineage determination of precursor cells especially between T and B lineages, and it is believed that a functioning PHF6 is required for B-cell differentiation leading to selective abundance of this mutation in T-ALL and MPAL with T-lineage differentiation18,19. This notion is further supported by the observation that PHF6 suppression leads to impaired tumor progression in B-ALL4. It has also been shown that PAX5 deficient pro-B cells can undergo myeloid lineage differentiation in the presence of transcription factors such as GATA or CEBPA20. In our patient, the immunophenotype and RNA expression data unequivocally point towards myeloid differentiation. Although it is difficult to ascertain the functional consequences of the P2RY8-CRLF2 rearrangement and the acquired PHF6 mutation at the time of AML transformation, we hypothesize that the two may interact in a way that led to the development of AML instead of B-ALL.
Remarkably, this patient with AML-MRC and PHF6, RUNX1, TET2, and RAD21 mutations had an MRD-negative CR by flow cytometry after just 4 cycles of combination decitabine with ipilimumab. While the complete results from clinical trials of these agents are needed to evaluate the efficacy and safety of this combination, this patient’s exceptional response could suggest the unique molecular characteristics of his tumor may have been important, namely the P2RY8-CRLF2 fusion. Recent evidence in head and neck cancers with oncogenic chromosomal rearrangements suggests that gene fusions may be a source of immunogenic neoantigens and stimulate T-cell responses that could be unleashed after immune checkpoint blockade21. This patient’s T-cells were positive for PD-1, suggesting a relation to the response to CTLA-4 blockade. Further research is needed to define whether this mechanism of action could be at play with other fusions or in the case of subclonal alterations such as in this patient.
Supplementary Material
Appendix Figure 1. Presence of the P2RY8-CRLF2 fusion in earlier bone marrow biopsy with myelodysplastic syndrome (MDS). (A) Photomicrographs of the bone marrow biopsy showing MDS with excess blast-1 (MDS-EB1). (B) Anchored multiplex polymerase chain reaction (Archer FusionPlex) reads showing an in-frame fusion between P2RY8 and CRLF2. (C) Breakapart fluorescence in situ hybridization probes for CRLF2 (top) and P2YR8 (bottom) consistent with interstitial deletion between the 2 genes resulting in fusion.
CONTEXT SUMMARY.
Key Objective
Is there utility to fusion discovery of known fusions in novel disease contexts?
Knowledge Generated
P2RY8-CRLF2 fusions have been observed in B-acute lymphoblastic leukemia but we report the first detection of this fusion in acute myeloid leukemia arising from myelodysplastic syndrome. Cell sorting, molecular characterization and immunostaining characterized the myeloid origin of this fusion and subsequent signaling effects.
Relevance
This patient was treated with the novel combination of decitabine and ipilimumab with an outstanding response. Immune cell infiltrates in the bone marrow on treatment suggests the response was related to the immune checkpoint inhibition. Further study of P2RY8-CRLF2 fusions and response to immunotherapy is warranted and could have implications for fusion discovery in novel disease contexts.
ACKNOWLEDGMENTS
This study was supported by the Comprehensive Cancer Center Core Grant (P30 CA008748) at Memorial Sloan-Kettering Cancer Center (MSKCC) from the National Institutes of Health, USA. We also want to acknowledge the members of the MSKCC diagnostic molecular laboratory, cytogenetics laboratory, flow cytometry laboratory, and immunohistochemical stain laboratory for their support in performing the relevant assays.
RESEARCH SUPPORT
U.A. has no conflict of interest. J.T. is supported by the Conquer Cancer Foundation of the American Society of Clinical Oncology, the American Association for Cancer Research, the American Society of Hematology (ASH), the Robert Wood Johnson Foundation, and the NIH/NCI (1K08CA230319-01). W.X. has received research support from Stemline therapeutics. C.H. has received honorarium from Invivoscribe, Inc. . J.S.G. is supported by the Conquer Cancer Foundation of the American Society of Clinical Oncology, the Leukemia & Lymphoma Society and UM1 CA186709.
Footnotes
DECLARATION
This study was performed in accordance with the Helsinki declaration. Patient consent has been obtained and the study has been approved by the Memorial Sloan Kettering Cancer Center institutional review board under protocol 12–245.
REFERENCES
- 1.Schmah J, Fedders B, Panzer-Grumayer R, et al. : Molecular characterization of acute lymphoblastic leukemia with high CRLF2 gene expression in childhood. Pediatr Blood Cancer 64, 2017. [DOI] [PubMed] [Google Scholar]
- 2.Arber DA, Orazi A, Hasserjian R, et al. : The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127:2391–405, 2016 [DOI] [PubMed] [Google Scholar]
- 3.Mangaonkar AA, Patnaik MM, Oliver GR, et al. : Multiple isodicentric Y chromosomes in myeloid malignancies: a unique cytogenetic entity and potential therapeutic target. Leuk Lymphoma 60:821–824, 2019 [DOI] [PubMed] [Google Scholar]
- 4.Meacham CE, Lawton LN, Soto-Feliciano YM, et al. : A genome-scale in vivo loss-of-function screen identifies Phf6 as a lineage-specific regulator of leukemia cell growth. Genes Dev 29:483–8, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma X, Liu Y, Liu Y, et al. : Pan-cancer genome and transcriptome analyses of 1,699 paediatric leukaemias and solid tumours. Nature 555:371–376, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel SS, Weirather JL, Lipschitz M, et al. : The microenvironmental niche in classic Hodgkin lymphoma is enriched for CTLA-4- positive T-cells that are PD-1-negative. Blood, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rochman Y, Leonard WJ: Thymic stromal lymphopoietin: a new cytokine in asthma. Curr Opin Pharmacol 8:249–54, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vesely C, Frech C, Eckert C, et al. : Genomic and transcriptional landscape of P2RY8-CRLF2-positive childhood acute lymphoblastic leukemia. Leukemia 31:1491–1501, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russell LJ, Capasso M, Vater I, et al. : Deregulated expression of cytokine receptor gene, CRLF2, is involved in lymphoid transformation in B-cell precursor acute lymphoblastic leukemia. Blood 114:2688–98, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Mullighan CG, Collins-Underwood JR, Phillips LA, et al. : Rearrangement of CRLF2 in B-progenitor- and Down syndrome-associated acute lymphoblastic leukemia. Nat Genet 41:1243–6, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potter N, Jones L, Blair H, et al. : Single-cell analysis identifies CRLF2 rearrangements as both early and late events in Down syndrome and non-Down syndrome acute lymphoblastic leukaemia. Leukemia 33:893–904, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Attarbaschi A, Morak M, Cario G, et al. : Treatment outcome of CRLF2-rearranged childhood acute lymphoblastic leukaemia: a comparative analysis of the AIEOP-BFM and UK NCRI-CCLG study groups. Br J Haematol 158:772–7, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Morak M, Attarbaschi A, Fischer S, et al. : Small sizes and indolent evolutionary dynamics challenge the potential role of P2RY8-CRLF2-harboring clones as main relapse-driving force in childhood ALL. Blood 120:5134–42, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dou H, Chen X, Huang Y, et al. : Prognostic significance of P2RY8-CRLF2 and CRLF2 overexpression may vary across risk subgroups of childhood B-cell acute lymphoblastic leukemia. Genes Chromosomes Cancer 56:135–146, 2017 [DOI] [PubMed] [Google Scholar]
- 15.Fang Q, Zhao X, Li Q, et al. : IKZF1 alterations and expression of CRLF2 predict prognosis in adult Chinese patients with B-cell precursor acute lymphoblastic leukemia. Leuk Lymphoma 58:127–137, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Van Vlierberghe P, Patel J, Abdel-Wahab O, et al. : PHF6 mutations in adult acute myeloid leukemia. Leukemia 25:130–4, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mori T, Nagata Y, Makishima H, et al. : Somatic PHF6 mutations in 1760 cases with various myeloid neoplasms. Leukemia 30:2270–2273, 2016 [DOI] [PubMed] [Google Scholar]
- 18.Xiao W, Bharadwaj M, Levine M, et al. : PHF6 and DNMT3A mutations are enriched in distinct subgroups of mixed phenotype acute leukemia with T-lineage differentiation. Blood Adv 2:3526–3539, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang J, Ding L, Holmfeldt L, et al. : The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature 481:157–63, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heavey B, Charalambous C, Cobaleda C, et al. : Myeloid lineage switch of Pax5 mutant but not wild-type B cell progenitors by C/EBPalpha and GATA factors. EMBO J 22:3887–97, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang W, Lee K-W, Srivastava RM, et al. : Immunogenic neoantigens derived from gene fusions stimulate T cell responses. Nature Medicine 25:767–775, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Figure 1. Presence of the P2RY8-CRLF2 fusion in earlier bone marrow biopsy with myelodysplastic syndrome (MDS). (A) Photomicrographs of the bone marrow biopsy showing MDS with excess blast-1 (MDS-EB1). (B) Anchored multiplex polymerase chain reaction (Archer FusionPlex) reads showing an in-frame fusion between P2RY8 and CRLF2. (C) Breakapart fluorescence in situ hybridization probes for CRLF2 (top) and P2YR8 (bottom) consistent with interstitial deletion between the 2 genes resulting in fusion.


