Abstract
Context
Several studies have reported increased risk of fragility fractures in patients with mild autonomous cortisol secretion (MACS), discordant to the degree of bone density deterioration.
Objective
To evaluate the effect of MACS on bone metabolism in patients with adrenal adenomas
Design
Cross-sectional study with prospective enrollment, 2014 – 2019
Setting
Referral center
Patients
213 patients with adrenal adenomas (22 Cushing syndrome (CS), 92 MACS and 99 nonfunctioning adrenal tumors (NFAT))
Main outcome measures
Osteocalcin, Procollagen I Intact N-Terminal (PINP), C-terminal telopeptide (CTX), sclerostin.
Results
Patients with CS demonstrated lower markers of bone formation when compared to patients with MACS and NFAT [CS vs MACS vs NFAT: mean osteocalcin 14.8 vs 20.1 vs 21.3 ng/mL (P<0.0001); mean PINP 34.8 vs 48.7 vs 48.5 μg/L (P=0.003)]. Severity of cortisol excess was inversely associated with sclerostin [CS vs MACS vs NFAT: mean sclerostin 419 vs 538 vs 624 ng/L, (P<0.0001)]. In a multivariable model of age, sex, BMI, cortisol and bone turnover markers, sclerostin was a significant predictor of low bone mass in patients with MACS (OR 0.63 [CI 95% 0.40–0.98] for each 100 ng/L of sclerostin increase).
After adrenalectomy, osteocalcin, CTX and sclerostin increased by a mean difference of 6.3 ng/mL, 0.12 ng/mL, and 171 pg/mL (P=0.02 for all), respectively.
Conclusions
Lower sclerostin level in patients with MACS reflects a reduction in osteocyte function or number associated with exposure to chronic cortisol excess. Increase in bone turnover markers after adrenalectomy suggests restoration of favorable bone metabolism.
Keywords: MACS, Cushing syndrome, non-functioning adrenal tumors, sclerostin, osteopenia, osteoporosis, bone turnover markers
1. INTRODUCTION
Incidentally discovered adrenal tumors are reported in approximately 5% of adults undergoing cross-sectional abdominal imaging, with roughly 95% representing benign adrenocortical adenomas 1. Overt adrenal hormonal excess is demonstrated in about 15% of patients with adenomas and includes mainly primary hyperaldosteronism and overt cortisol excess (Cushing syndrome, CS). Mild autonomous cortisol secretion (MACS), defined as an abnormal dexamethasone suppression test (cortisol >1.8 mcg/dl) 2 but without the classical external manifestations of overt CS, is more prevalent, affecting up to 48% of patients with adenomas 3–6.
Chronic exposure to subtle cortisol excess in patients with MACS has been reported to be detrimental to bone health7. The prevalence of vertebral fractures in patients with MACS was reported to be four times higher when compared to patients with non-functioning adrenal tumors (NFAT) 8–11. In a small retrospective comparative study of patients with MACS undergoing adrenalectomy versus those followed conservatively, the risk for new vertebral fractures was five-fold lower in subjects who underwent adrenalectomy 12. Several studies have shown that the risk of new fractures in patients with MACS is discordant with the degree of bone mineral density loss, suggesting that a reduction in bone quality rather than density contributes to the increased fracture risk 10,11,13. Patients with MACS were reported to have abnormal bone metabolism with low circulating concentrations of osteocalcin14–17, consistent with reduced bone formation. In addition, while several studies demonstrated elevated levels of carboxyterminal telopeptide of type 1 collagen [CTX] 14–17 reflecting increased bone resorption, other studies did not 15,18–20.
Abnormal bone metabolism may be a precursor to development of fragility fractures. However, small sample sizes, selective inclusion criteria, and heterogeneous definitions of MACS have collectively decreased the confidence and generalizability of reported results to date 15–17,19–23. Our study aimed to prospectively assess the effect of MACS on bone metabolism by evaluating bone turnover markers in patients with MACS, CS, and NFAT. In a subset of patients undergoing adrenalectomy, we also aimed to evaluate the effect of remission of hypercortisolism on bone metabolism.
2. SUBJECT AND METHODS
We prospectively enrolled patients evaluated for adrenal adenomas at Mayo Clinic in Rochester, Minnesota between 2014 and 2019. The study protocol was approved by the Mayo Clinic Institutional Review Board and all subjects provided written, informed consent. Clinical, imaging, and biochemical data were prospectively collected at the time of enrollment and the medical record was again reviewed at the time of study conclusion. Fasting blood was collected in the morning from eligible participants and stored at −80C. At the study conclusion, blood samples were analyzed for two markers of bone formation, osteocalcin (secreted by osteoblasts) and PINP (N-terminal propeptide of type 1 collagen, a cleaved byproduct of bone formation), a marker of bone resorption, CTX (C-terminal telopeptide of type 1 collagen, cleaved byproduct of osteoclast activity) and sclerostin (produced by osteocytes).
2.1. Study Participants
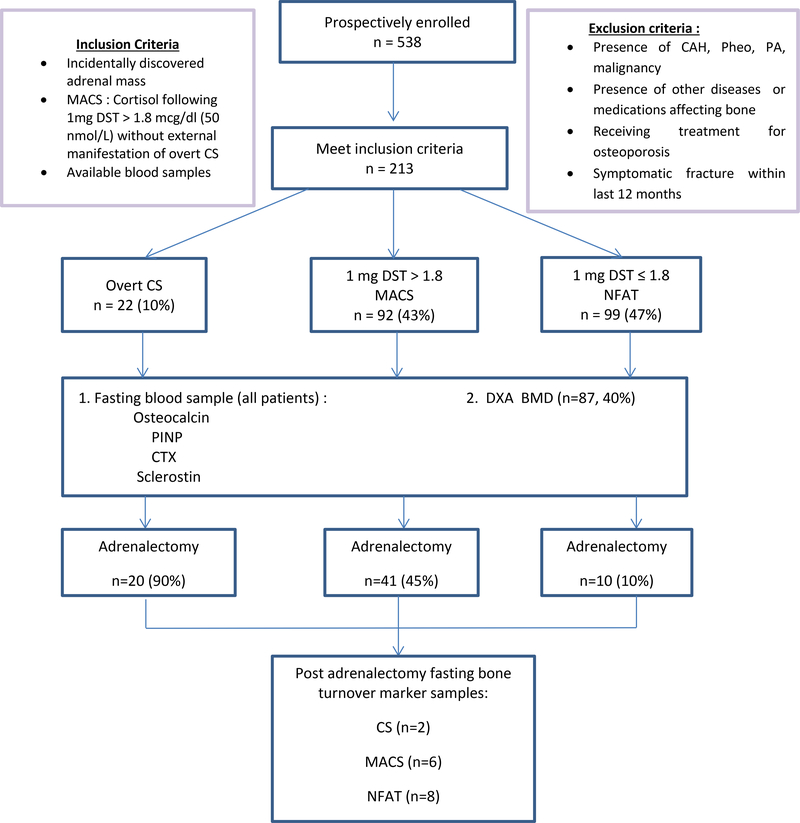
Patients were included in the study based on the following inclusion criteria: 1) adults with nonfunctioning adrenal adenoma, MACS, or CS, 2) available blood samples at the time of diagnosis (for the baseline cohort), 3) available blood samples at the time of diagnosis and also post-adrenalectomy (at least 6 weeks after adrenalectomy and/or at least 6 weeks without the provision of exogenous glucocorticoid therapy, when recovery of the hypothalamic-pituitary-adrenal (HPA) axis had been documented (8 AM serum cortisol was ≥10 mcg/dL (≥276 nmol/L) when assessed 24 hours after the last administered dose of glucocorticoid)), 4) absence of symptomatic fracture within the last 12 months, 5) absence of drugs affecting bone metabolism, dexamethasone metabolism or cortisol secretion, 6) absence of active extra-adrenal malignancy, 6) absence of other known diseases that may affect bone metabolism (such as hypogonadism, thyrotoxicosis, hyper/hypoparathyroidism, malabsorptive disorders, chronic renal failure (eGFR <30ml/min), chronic hepatic disease, depression, alcoholism, eating disorders, rheumatologic or hematologic diseases)(Figure 1). MACS was diagnosed when cortisol levels following 1 mg dexamethasone overnight suppression was >1.8 mcg/dL (>50 nmol/L) 2 without external manifestations of overt CS. CS was diagnosed based on the most recently published clinical practice guidelines 24. The diagnosis of osteopenia (−2.5 < T-score ≤ −1) at the hip and/or spine) or osteoporosis (T-score ≤ −2.5 at the hip and/or spine, or osteopenia with associated fragility fractures), presence of cardiovascular risk factors such as the presence of hypertension, dyslipidemia, pre-diabetes and type 2 diabetes mellitus (DM2) were collected for all patients in the cohort. Hypertension was defined as a documented diagnosis of hypertension treated with at least 1 antihypertensive medication. Composite diabetes included patients with a documented diagnosis of either DM2 (HbA1c ≥6.4%) or prediabetes (5.7% < HbA1c < 6.4%) and therapy with at least 1 glucose‐lowering medication. Dyslipidemia was defined as documented diagnosis and therapy with at least 1 lipid‐lowering medication.
FIGURE 1 : Flowchart on study process.
MACS :mild autonomous cortisol secretion; DST: dexamethasone suppression test; CAH: congenital adrenal hyperplasia; PA : primary aldosteronism; CS: Cushing syndrome; NFAT : non-functioning adrenal tumor; PINP : N-terminal propeptide of type 1 collagen; CTX: C-terminal telopeptide of Type 1 collagen; DXA BMD: dual-energy X-ray absorptiometry.
2.2. Measurements
2.2.1. Biochemical analysis
All patients were evaluated by a combination of various endocrine studies that included 1 and/or 8 mg overnight dexamethasone suppression test (DST), morning serum ACTH concentration, dehydroepiandrosterone sulphate (DHEA‐S), 24‐hour urinary free cortisol (UFC), and midnight salivary cortisol concentrations. Laboratory analyses were performed at Mayo Clinic Laboratories (Rochester, MN, USA). Serum cortisol and DHEA‐S were measured on an immunoenzymatic assay (Beckman Coulter UniCel™ DxI 800), plasma ACTH was measured on an automated electrochemiluminescent immunoassay (Roche Cobas 8000), and 24‐hour UFC and midnight salivary cortisol were measured by liquid chromatography‐tandem mass spectrometry (LC‐MS/MS).
2.2.2. Bone turnover markers
Eligible patients were requested to provide fasting blood samples for baseline assessment of bone formation [serum osteocalcin measured by an electrochemiluminescence immunoassay assay (Roche Cobas e411, intra- and interassay coefficients of variance (CV) were 1.7% and 3.9%,respectively ); serum amino-terminal propeptide of type I collagen (PINP) measured by radioimmunoassay (Orion Diagnostica, intra-and interassay CVs were 2.3% and 3.8%, respectively)], and resorption (serum C-telopeptide of type I collagen [CTX]) measured by an electrochemiluminescence immunoassay assay (Roche Cobas e411, intra- and interassay CVs were 1.9% and 7.8%, respectively) markers. Sclerostin (heparinized plasma sample) was measured by a quantitative, solid-phase, sandwich enzyme immunoassay, (R&D Systems, intra- and interassay CVs were 1.2% and 9.6%, respectively). CV values were obtained from kit inserts.
2.2.3. Assessment of bone health
Dual-energy X-ray absorptiometry (DXA) imaging was assessed at the lumbar spine, total hip and femoral neck using a Lunar Prodigy scanner (General Electric Healthcare, Waukesha, WI).
2.3. Statistics
Descriptive statistics were used to determine mean and standard deviation (SD) or median and ranges depending on data distribution, while categorical data are shown as a number (%). Associations between variables were assessed using one‐way ANOVA for continuous variables. P values less than .05 were considered significant. Data were analyzed using JMP SOFTWARE, VERSION 14 (SAS, Carey, NC, USA). We performed multivariate regression analyses to investigate the relationship between bone turnover markers and morning cortisol concentrations after overnight DST in predicting bone disease (osteopenia/osteoporosis), while controlling for confounding factors including age, sex and body mass index (BMI).
3. RESULTS
3.1. Demographic and endocrine data for patients with adrenal adenomas
A total of 213 patients [143, 67% women, median age 58 years (range 18–93)] with adrenal adenomas (median tumor size 2.4 cm (range 0.3 −14.4)) were included (Table 1). Of 213 patients, 22 (10%) were diagnosed with overt CS, 92 (43%) with MACS, and 99 (47%) with NFAT. Morning serum cortisol concentrations following dexamethasone administration (DST cortisol) were higher in patients with overt CS and MACS when compared to patients with NFAT (median 8.5 vs 3 vs 1.2 μg/dL, respectively). ACTH concentrations and DHEA-S index (DHEA-S level divided by the lower limit of the sex- and age-based reference range) were lower in patients with overt CS when compared to patients with MACS and NFAT [ACTH: median 5 vs 8.95 vs 15.5 pg/mL (P<0.0001) and DHEA-S index: median 0.65 vs 2.64 vs 4.62 (P<0.0001), respectively]. Urine free cortisol concentrations were highest in patients with CS, but were similar in other groups (CS vs MACS vs NFAT: median 108 vs 26 vs 22 μg/24h, normal < 45 μg/24h, P<0.0001), Table 1.
TABLE 1:
Demographic data and bone turnover marker levels of patients with adrenal adenomas
| CS (n=22) | MACS (n=92) | NFAT (n=99) | P-value (CS vs MACS vs NFAT) | P-value (MACS vs NFAT) | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, median (range), years | 41.5 (18–61) | 59.5 (28–82) | 59 (28–93) | <0.0001 | 0.664 |
| Female, n (%) | 18 (86%) | 57 (62%) | 67 (68%) | 0.456 | 0.41 |
| BMI median (range), kg/m2 | 30.1 (21.9 – 54.6) | 31 (17 – 53) | 31 (15 – 51) | 0.06 | 0.525 |
| Weight, median (range), kg | 84 (62–113) | 89 (62–128) | 90 (63–126) | 0.29 | 0.94 |
| Computed tomography imaging | |||||
| Tumor size, median (range),cm | 3 (0.5–6.1) | 3.1 (0.5–14.4) | 1.7 (3–4.5) | <0.0001 | <0.001 |
| Unenhanced CT attenuation, n, median (range) Hounsfield units, n =151 |
n=13 10 (−55 to 36) |
n=68 8.25 (−20 to 36) |
n=70 7 (−27 to 41) |
0.416 | 0.32 |
| Endocrine work up | |||||
| Cortisol after overnight 1 mg dexamethasone, median, nmol/L (range), μg/dL (range) |
235 (61–689) 8.5 (2.2–25) |
83 (52–441) 3 (1.9–16) |
33 (25–49) 1.2 (0.9–1.8) |
<0.0001 | <0.001 |
| ACTH, n, median, pmol/L (range), pg/mL (range n=162 |
n=18 1.1 (1.09–2.94) 5 (4.99–13.4) |
n=78 1.97( 1.1–6.2) 8.95 (5–28.2) |
n=66 3.41 (2.0–6.16) 15.5 (9.27– 28) |
<0.0001 | <0.0001 |
| Urine cortisol, n, median μg/dL/24h (range) nmol/24h (range) n=156 |
n=21 108 (25–875) 298 (69–2415) |
n=74 26(2.6–84) 72(7.2–232) |
n=61 22(3.4–71) 61(9.4–196) |
<0.0001 | 0.049 |
| DHEA-S index, n, median (range), n =146 |
n=19 0.65 (0.18–7.03) |
n=71 2.63 (0.11–17.2) |
n=56 4.63 (0.58–16.41) |
<0.0001 | 0.007 |
| Cardiovascular Risk Factors | |||||
| Hypertension, n (%) | 16(73%) | 66(73%) | 63(64%) | 0.36 | 0.17 |
| Dyslipidemia, n (%) | 7(32%) | 57(63%) | 53(54%) | 0.03 | 0.18 |
| Diabetes Mellitus/IFG, n (%) | 9(41%) | 38(41%) | 40(41%) | 0.99 | 0.98 |
| Bone Disease | |||||
| DXA Bone density scans performed, n (%) | 8 (37%) | 48 (52%) | 31 (31%) | ||
| Osteopenia, n (%) | 5 (62%) | 27 (56%) | 16 (52%) | 0.84 | 0.69 |
| Osteoporosis, n (%) | 3 (38%) | 10 (21%) | 6 (19%) | 0.56 | 0.87 |
| Osteopenia and osteoporosis, n (%) | 8 (100%) | 37 (77%) | 22 (71%) | 0.09 | 0.54 |
| Bone Turnover Markers | |||||
| Osteocalcin, mean (SD), (range), ng/mL | 14.8 (16.3) (2.2–79.6) |
20.1 (10.2) (5.4–53.7) |
21.3 (12.1) (2.2–78.8) |
<0.0001 | 0.39 |
| PINP, mean (SD), (range), μg/L | 34.8 (23.6) (12.3–91.6) |
48.7 (23.5) (13.3–123) |
48.5 (22) (3–152) |
0.003 | 0.84 |
| CTX, mean (SD), (range), ng/mL | 0.3 (0.2) (0.09–0.93) |
0.4 (0.3) (0.05–1.28) |
0.4 (0.2) (0.10–1.16) |
0.15 | 0.5 |
| Sclerostin, mean (SD), (range), pg/mL | 419 (199) (73.2–683) |
538 (296) (111–873) |
624 (218) (202–1273) |
<0.0001 | 0.005 |
All P-values < 0.05 were considered statistically significant.
CS: Cushing syndrome; MACS: Mild autonomous cortisol secretion; NFAT: non-functioning adrenal tumors; BMI: body mass index; CT : computed-tomography; ACTH : Adrenocorticotrophic hormone; DHEA-S: dehydroepiandrosterone sulfate, IFG: impaired fasting glucose; DXA: Dual-energy X-ray absorptiometry, PINP: N-terminal propeptide of type 1 collagen; CTX: C-terminal telopeptide of Type 1 collagen; SD: standard deviation
No significant differences in the prevalence of composite diabetes and hypertension were noted between patients with overt CS, MACS and NFAT, while dyslipidemia was most frequently detected in patients with MACS, followed by NFAT, and was lowest in CS (MACS vs NFAT vs CS: 63% vs 54% vs 32%), respectively, P=0.03), reflecting demographic differences, Table 1.
Of the 87 patients (40%) with bone mineral density assessed at the time of diagnosis (8 with CS, 48 with MACS and 31 with NFAT), all patients with CS had low bone mass (5 with osteopenia and 3 with osteoporosis), 37 (77%) of patients with MACS had low bone mass (27 with osteopenia and 10 with osteoporosis), and 22 (71%) of patients with NFAT had low bone mass (16 with osteopenia and 6 with osteoporosis), Table 1.
3.2. Bone turnover markers
Unadjusted for confounding factors, in patients with overt CS, values for markers of bone formation (osteocalcin and PINP) were significantly lower when compared to patients with MACS and NFAT [CS vs MACS vs NFAT: mean osteocalcin 14.8 vs 20.1 vs 21.3 ng/mL (P<0.0001); mean PINP 34.8 vs 48.7 vs 48.5 μg/L (P=0.003)] (Table 1). No significant differences were noted in CTX measurements between the three groups (Table 1). Severity of cortisol excess was inversely associated with sclerostin measurements [CS vs MACS vs NFAT: mean sclerostin 419 vs 538 vs 624 ng/L, (P<0.0001)] (Table 1). In patients with MACS, sclerostin was a significant predictor of bone disease (osteopenia and/or osteoporosis) in a multivariable model which included age, sex, BMI, DST cortisol and bone turnover markers (OR 0.63 [CI 95% 0.40–0.98] for each 100 ng/L of sclerostin increase, P=0.04) (Table 2).
TABLE 2:
Predictors of Osteopenia and Osteoporosis in patients with MACS
| Predictor | Multivariable analysis | ||
|---|---|---|---|
| Odds Ratio | 95% CI | P-value | |
| Age (for every 10 yrs increase) | 1.20 | 0.57–2.53 | 0.83 |
| Female sex | 1.35 | 0.18–9.87 | 0.77 |
| BMI (for every 5 kg/m2 increase) | 0.94 | 0.49–1.80 | 0.85 |
| Osteocalcin (for every ng/mL increase) | 1.10 | 0.92–1.32 | 0.26 |
| PINP (for every 1μg/L increase) | 0.97 | 0.90–1.07 | 0.62 |
| CTX (for every ng/mL increase) | 2.44 | 0.0–3189 | 0.8 |
| Sclerostin (for every 100 pg/mL increase) | 0.63 | 0.40–0.98 | *0.04 |
| Cortisol after 1mg DST (for every 1mcg/dL increase) | 0.92 | 0.74–1.16 | 0.51 |
All P-values < 0.05 were considered statistically significant.
BMI: Body mass index; PINP: N-terminal propeptide of type 1 collagen; CTX: C-terminal telopeptide of Type 1 collagen; DST: dexamethasone suppression test
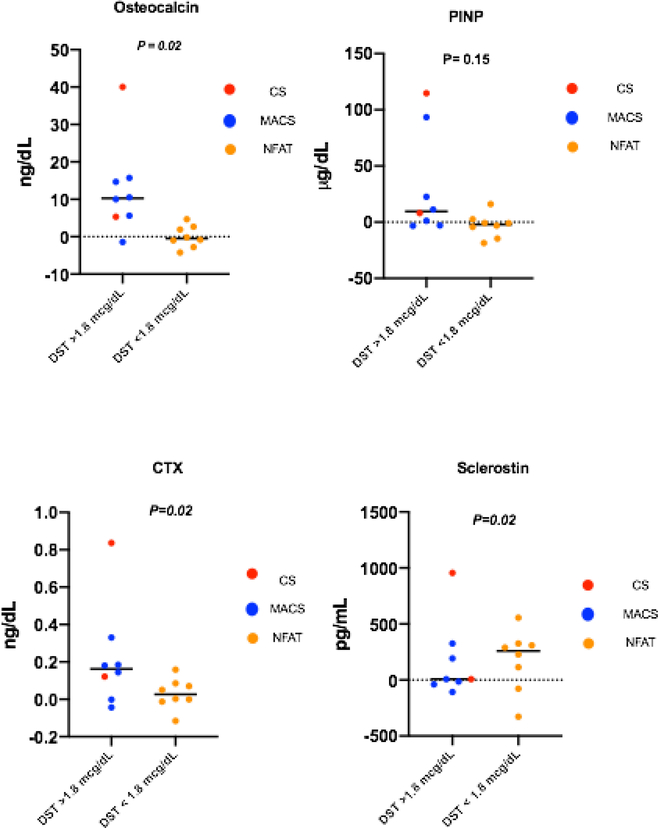
3.3. Post-adrenalectomy changes in bone metabolism
In 16 patients (2 patients with overt CS, 6 patients with MACS and 8 patients with NFAT), serum bone turnover markers were measured following adrenalectomy at a median of 37 weeks (range 6–92). Circulating levels of osteocalcin, CTX and sclerostin increased significantly by a mean difference of 6.3 ng/mL (SD=10.8, P= 0.02), 0.12 ng/mL (SD=0.2, P=0.02), and 171 pg/mL (SD=302.4, P=0.02), respectively. PINP concentrations demonstrated a non-significant increase after adrenalectomy (mean difference of 8.52 μg/L (SD=32.24, P=0.15) (Figure 2). In patients with MACS only (n=8), levels of osteocalcin and CTX increased significantly by a mean difference of 8.18 ng/mL (SD=6.74, P=0.04) and 0.14ng/mL (SD=0.12, P=0.05), respectively. Sclerostin and PINP levels increased post adrenalectomy, thought non-significantly, by a mean difference of 107 pg/mL (SD= 181, P=0.24) and 1.78μg/L (SD=35.4, P=0.75), respectively.
Figure 2: Mean difference of bone turnover markers pre- and post-adrenalectomy (remission).
All P-values <0.05 were considered statistically significant
CS: Cushing syndrome; MACS: mild autonomous cortisol secretion; NFAT: non-functioning adrenal tumor; DST: dexamethasone suppression test; PINP: N-terminal propeptide of type 1 collagen; CTX: C-terminal telopeptide of Type 1 collagen
4. DISCUSSION
In our study, we demonstrated that sclerostin was the only biomarker that distinguished patients with MACS from patients with NFAT. We also showed that sclerostin concentrations were inversely proportional to the degree of hypercortisolism. Concentrations of osteocalcin, PINP and CTX were similar in patients with MACS and NFAT. In a multivariable analysis, sclerostin was a significant predictor of low bone mass in patients with MACS. Sclerostin has been recognized as a key negative regulator of bone formation, and glucocorticoid therapy has been reported to stimulate the expression of the SOST gene, which encodes sclerostin28. Contrary to this observation, our study showed that plasma sclerostin levels are significantly decreased in patients with endogenous hypercortisolism. This could be explained by the differences of chronic endogenous cortisol excess versus transient/acute effect of exogenous glucocorticoid therapy on bone metabolism. In bone, sclerostin is exclusively produced by osteocytes30 and chronic glucocorticoid exposure can induce autophagy in osteocytes31 and increase oxidative stress32. Decreased sclerostin concentrations in patients with MACS may be explained by the decrease in osteocyte function and/or number rather than by a direct, inhibitory effect on sclerostin production. Similar observation of low sclerostin was reported in one other study which included 21 patients with endogenous overt cortisol excess 29, though no other studies have explored the role of sclerostin in MACS.
Our study confirmed previous reports that osteocalcin concentrations inversely correlate with the degree of cortisol excess in overt CS 25,26. This is consistent with existing knowledge that cortisol excess inhibits the differentiation of osteoblasts from precursor mesenchymal cells and increases osteoblast apoptosis 27. In our study, we did not identify differences in concentrations of osteocalcin, PINP and CTX in patients with MACS versus patients with NFAT. Several studies have reported low osteocalcin concentrations in patients with MACS 14–17,20,22,23. However, other studies did not confirm a reduction in bone formation as measured by osteocalcin 18,19,21 and PINP 14,15. Similar discrepancies have been reported in assessment of bone resorption, with CTX concentrations being increased14,17,23, normal15,19 or reduced20, and urinary deoxypyridinoline concentrations reported within the normal range in patients with MACS 15,16,19,21,22. These conflicting results may be attributed to small sample sizes, selection criteria based on age and gonadal status, as well as differences in definition of MACS.
In a small cohort of patients undergoing adrenalectomy, we observed an increase in bone turnover markers after surgery. The increase in osteocalcin and PINP concentrations are consistent with improvement in osteoblast activity. The noted rise in CTX levels is consistent with increased turnover with bone remodeling. The increase in sclerostin concentrations noted after adrenalectomy likely reflects recovery of osteocytic function after the cessation of metabolic stress, or to an increase in the number of osteocytes after the removal of the apoptotic effect of cortisol excess. This is further supported by the reported improvement in FGF23 levels in patients with treated endogenous hypercortisolism. FGF23 is also produced by osteocytes, and its rise after cure from hypercortisolism reflects restoration of osteocyte numbers and/or function28.
5. STRENGTHS AND LIMITATIONS
We acknowledge that despite the prospective enrollment, evaluation of patients did not follow a pre-specified protocol which explains that not all patients had a uniform approach to testing. Our study lacks a control group without adrenal tumors that would have allowed for a comparative assessment of patients with NFAT who may still have subtle cortisol secretion not detected by current standard of care testing 35. The length of time patients had hypercortisolism prior to diagnosis is also unknown and could potentially affect the degree of disruption to bone metabolism. In addition, although all patients were recruited from within the Mayo Clinic, only one of the clinics routinely obtained DXA imaging in all patients with MACS. Strengths of this study are consecutive enrollment, relatively large cohort size, uniform diagnosis based on the established 2016 ESE/ENSAT guidelines, and the same assays used for laboratory measurements. While BMD assessments were obtained in only in 40% of patients, all DXA imaging was performed using the same approach at a single institution. Finally, inclusion of a small cohort of patients with measurements pre- and post-adrenalectomy patients further supports the effect of cortisol secretion on bone metabolism.
6. CLINICAL IMPLICATIONS
MACS has been reported to have a detrimental effect on bone health, with a higher prevalence of vertebral fractures when compared to NFAT. Several studies have shown that the risk of new fractures in patients with MACS is discordant to BMD, suggesting that a reduction in bone quality rather than only bone mineral density contributes to the increased fracture risk 10,11,13. Hence, existing screening tools to evaluate for osteopenia and osteoporosis via DXA may not be able to detect patients at risk of developing fragility fractures early enough to intervene. Whilst adrenalectomy has been reported to decrease the risk of new fractures, the appropriate selection of patients with MACS who would benefit most from adrenalectomy remains challenging.
Our study found sclerostin to be a predictor for osteopenia or osteoporosis in a multivariable model of age, sex, BMI, DST cortisol, and bone turnover markers. Measurements of sclerostin may help identify patients with MACS who are at risk of having osteopenia or osteoporosis; however, it is unclear whether sclerostin concentrations are predictive of future fragility fractures. Measurements of sclerostin concentrations during the evaluation of patients with MACS may be of value in selectively identifying those patients most likely to benefit from adrenalectomy. However, larger longitudinal studies are needed to validate sclerostin as a diagnostic and prognostic biomarker of skeletal health in patients with MACS.
7. CONCLUSIONS
In conclusion, patients with MACS demonstrate lower sclerostin concentrations reflecting a reduction in osteocyte function or number due to exposure to chronic cortisol excess. Overt CS is associated with reduced bone formation as demonstrated by lower osteocalcin and PINP concentrations. Increase in bone turnover markers after adrenalectomy suggests restoration of favorable bone metabolism.
ACKNOWLEDGEMENTS
Jolaine M. Hines, Immunochemical Core Laboratory, Mayo Clinic, 200 First Street SW, Rochester, MN 55905
This research was partly supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH) USA under award K23DK121888 (to I.B). The views expressed are those of the author(s) and not necessarily those of the National Institutes of Health USA.
Footnotes
DISCLOSURE STATEMENT
IB reports advisory board participation with Corcept and HRA Pharma outside the submitted work. This research was supported by the James A. Ruppe Career Development Award in Endocrinology (IB) and the Catalyst Award for Advancing in Academics from Mayo Clinic (IB).
REFERENCES
- 1.Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest.s 2006;29(4):298–302. [DOI] [PubMed] [Google Scholar]
- 2.Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175(2):G1–G34. [DOI] [PubMed] [Google Scholar]
- 3.Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR. The clinically inapparent adrenal mass: update in diagnosis and management. Endocrine reviews. 2004;25(2):309–340. [DOI] [PubMed] [Google Scholar]
- 4.Barzon L, Sonino N, Fallo F, Palu G, Boscaro M. Prevalence and natural history of adrenal incidentalomas. European journal of endocrinology / European Federation of Endocrine Societies. 2003;149(4):273–285. [DOI] [PubMed] [Google Scholar]
- 5.Bancos I, Chortis V, Lang K, et al. The natural history of adrenal incidentaloma - results from the international prospective multi-centre EURINE-ACT study. Endocrine Abstracts (2017) 49 GP122 2017. [Google Scholar]
- 6.Prete A, Taylor Angela E, Sitch Alice J, et al. Mild autonomous cortisol excess in adrenal incidentalomas - metabolic disease burden and urinary steroid metabolome in 1201 prospectively recruited patients. Endocrine Abstracts (2017) 50 OC21. 2017. [Google Scholar]
- 7.Athimulam S, Bancos I. Evaluation of bone health in patients with adrenal tumors. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):125–132. [DOI] [PubMed] [Google Scholar]
- 8.Athimulam S DD KS, Drake M, Bancos I. The Impact of Mild Autonomous Cortisol Secretion on Bone Metabolism. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiodini I, Guglielmi G, Battista C, et al. Spinal volumetric bone mineral density and vertebral fractures in female patients with adrenal incidentalomas: the effects of subclinical hypercortisolism and gonadal status. J Clin Endocrinol Metab. 2004;89(5):2237–2241. [DOI] [PubMed] [Google Scholar]
- 10.Chiodini I, Morelli V, Masserini B, et al. Bone mineral density, prevalence of vertebral fractures, and bone quality in patients with adrenal incidentalomas with and without subclinical hypercortisolism: an Italian multicenter study. J Clin Endocrinol Metab. 2009;94(9):3207–3214. [DOI] [PubMed] [Google Scholar]
- 11.Chiodini I, Viti R, Coletti F, et al. Eugonadal male patients with adrenal incidentalomas and subclinical hypercortisolism have increased rate of vertebral fractures. Clin Endocrinol (Oxf). 2009;70(2):208–213. [DOI] [PubMed] [Google Scholar]
- 12.Salcuni AS, Morelli V, Eller Vainicher C, et al. Adrenalectomy reduces the risk of vertebral fractures in patients with monolateral adrenal incidentalomas and subclinical hypercortisolism. Eur J Endocrinol. 2016;174(3):261–269. [DOI] [PubMed] [Google Scholar]
- 13.Morelli V, Eller-Vainicher C, Salcuni AS, et al. Risk of new vertebral fractures in patients with adrenal incidentaloma with and without subclinical hypercortisolism: a multicenter longitudinal study. J Bone Miner Res. 2011;26(8):1816–1821. [DOI] [PubMed] [Google Scholar]
- 14.Osella G, Terzolo M, Reimondo G, et al. Serum markers of bone and collagen turnover in patients with Cushing’s syndrome and in subjects with adrenal incidentalomas. J Clin Endocrinol Metab. 1997;82(10):3303–3307. [DOI] [PubMed] [Google Scholar]
- 15.Torlontano M, Chiodini I, Pileri M, et al. Altered bone mass and turnover in female patients with adrenal incidentaloma: the effect of subclinical hypercortisolism. J Clin Endocrinol Metab. 1999;84(7):2381–2385. [DOI] [PubMed] [Google Scholar]
- 16.Chiodini I, Torlontano M, Carnevale V, et al. Bone loss rate in adrenal incidentalomas: a longitudinal study. J Clin Endocrinol Metab. 2001;86(11):5337–5341. [DOI] [PubMed] [Google Scholar]
- 17.Tauchmanova L, Pivonello R, De Martino MC, et al. Effects of sex steroids on bone in women with subclinical or overt endogenous hypercortisolism. Eur J Endocrinol. 2007;157(3):359–366. [DOI] [PubMed] [Google Scholar]
- 18.Hadjidakis D, Tsagarakis S, Roboti C, et al. Does subclinical hypercortisolism adversely affect the bone mineral density of patients with adrenal incidentalomas? Clin Endocrinol (Oxf). 2003;58(1):72–77. [DOI] [PubMed] [Google Scholar]
- 19.Bardet S, Rohmer V, Boux de Casson F, et al. [Bone mineral density and biological markers of bone repair in patients with adrenal incidentaloma: effect of subclinical hypercortisolism]. Rev Med Interne. 2002;23(6):508–517. [DOI] [PubMed] [Google Scholar]
- 20.Sartorio A, Conti A, Ferrero S, et al. Evaluation of markers of bone and collagen turnover in patients with active and preclinical Cushing’s syndrome and in patients with adrenal incidentaloma. Eur J Endocrinol. 1998;138(2):146–152. [DOI] [PubMed] [Google Scholar]
- 21.Chiodini I, Tauchmanova L, Torlontano M, et al. Bone involvement in eugonadal male patients with adrenal incidentaloma and subclinical hypercortisolism. J Clin Endocrinol Metab. 2002;87(12):5491–5494. [DOI] [PubMed] [Google Scholar]
- 22.Francucci CM, Pantanetti P, Garrapa GG, Massi F, Arnaldi G, Mantero F. Bone metabolism and mass in women with Cushing’s syndrome and adrenal incidentaloma. Clin Endocrinol (Oxf). 2002;57(5):587–593. [DOI] [PubMed] [Google Scholar]
- 23.Guo W, Li F, Zhu C, et al. Effect of hypercortisolism on bone mineral density and bone metabolism: A potential protective effect of adrenocorticotropic hormone in patients with Cushing’s disease. The Journal of international medical research. 2018;46(1):492–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nieman LK, Biller BM, Findling JW, et al. Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2015;100(8):2807–2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szappanos A, Toke J, Lippai D, et al. Bone turnover in patients with endogenous Cushing’s syndrome before and after successful treatment. Osteoporos Int. 2010;21(4):637–645. [DOI] [PubMed] [Google Scholar]
- 26.Sereg M, Toke J, Patocs A, et al. Diagnostic performance of salivary cortisol and serum osteocalcin measurements in patients with overt and subclinical Cushing’s syndrome. Steroids. 2011;76(1–2):38–42. [DOI] [PubMed] [Google Scholar]
- 27.Chang JK, Li CJ, Liao HJ, Wang CK, Wang GJ, Ho ML. Anti-inflammatory drugs suppress proliferation and induce apoptosis through altering expressions of cell cycle regulators and pro-apoptotic factors in cultured human osteoblasts. Toxicology. 2009;258(2–3):148–156. [DOI] [PubMed] [Google Scholar]
- 28.Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE. Glucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a longitudinal study of gene expression in bone tissue from glucocorticoid-treated mice. Arthritis Rheum. 2008;58(6):1674–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Lierop AH, van der Eerden AW, Hamdy NA, Hermus AR, den Heijer M, Papapoulos SE. Circulating sclerostin levels are decreased in patients with endogenous hypercortisolism and increase after treatment. J Clin Endocrinol Metab. 2012;97(10):E1953–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Bezooijen RL, Roelen BAJ, Visser A, et al. Sclerostin is an osteocyte-expressed negative regulator of bone formation, but not a classical BMP antagonist. J Exp Med. 2004;199(6):805–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xia X, Kar R, Gluhak-Heinrich J, et al. Glucocorticoid-induced autophagy in osteocytes. J Bone Miner Res. 2010;25(11):2479–2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Almeida M, Han L, Ambrogini E, Weinstein RS, Manolagas SC. Glucocorticoids and tumor necrosis factor alpha increase oxidative stress and suppress Wnt protein signaling in osteoblasts. J Biol Chem. 2011;286(52):44326–44335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Staa TP, Leufkens HGM, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. Journal of Bone and Mineral Research. 2000;15(6):993–1000. [DOI] [PubMed] [Google Scholar]
- 34.Manolagas SC, Weinstein RS. New developments in the pathogenesis and treatment of steroid-induced osteoporosis. J Bone Miner Res. 1999;14(7):1061–1066. [DOI] [PubMed] [Google Scholar]
- 35.Lopez D, Luque-Fernandez MA, Steele A, Adler GK, Turchin A, Vaidya A. “Nonfunctional” Adrenal Tumors and the Risk for Incident Diabetes and Cardiovascular Outcomes: A Cohort Study. Ann Intern Med. 2016;165(8):533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]