Abstract
Purpose:
The purpose of this study was to further understand the relationship between cardiac function and flow, on the basis of sex, by quantifying cardiac flow characteristics and relating them to cardiac muscle performance in young adults.
Materials and Methods:
In this cross-sectional study, cardiac four-dimensional flow (4D flow) magnetic resonance imaging (MRI) and two-dimensional cine MRI were performed on 20 male and 19 female volunteers aged 20–35. Velocity-based metrics of flow, kinetic energy, vorticity, and efficiency indices were quantified, as well as cardiac strain metrics.
Results*:
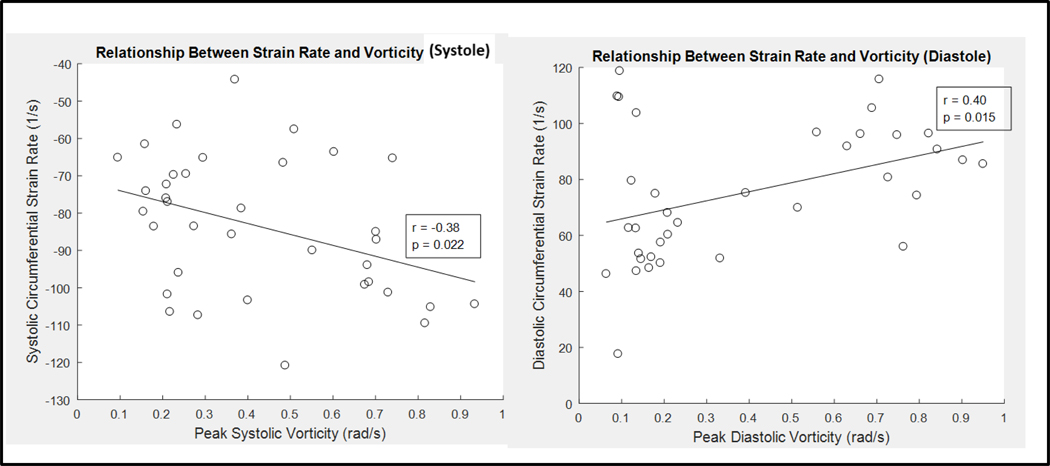
Peak systolic blood kinetic energy (male: 4.76 ± 2.66 mJ; female: 3.36 ± 1.43 mJ; p=0.047) was significantly higher in the male left ventricle (LV) than in the female LV. Peak systolic vorticity index (male: 0.008 ± 0.005 rad-m2/ml-s; female: 0.014 ± 0.007 rad-m2/ml-s; p=0.007), peak diastolic vorticity index (male: 0.007 ± 0.006 rad-m2/ml-s; female: 0.014 ± 0.010 rad-m2/ml-s; p=0.015), and cycle-average vorticity (male: 0.006 ± 0.001 rad-m2/ml-s; female: 0.011 ± 0.002 rad/s; p=0.001) were all significantly higher in the LV of women than they were in the LV of men. Radial, circumferential, and long-axis strain metrics were significantly higher in the female LV than in the male LV (p<0.05). Circumferential systolic and diastolic strain rates displayed moderate correlation to peak systolic (r=−0.38, p=0.022) and diastolic vorticity (r=0.40, p=0.015) values, respectively. *Results are reported as mean ± standard deviation.
Conclusion:
Left ventricular vorticity metrics were observed to be higher in women than in men and displayed moderate correlation to cardiac strain metrics. The methods and results of this study may be used to further understand the sex-based cardiac efficiency relationship between cardiac function and flow.
Summary Statement:
Left ventricular blood flow vorticity metrics were observed to be higher in women than in men and displayed moderate correlation to cardiac strain metrics. The methods and results of this study may be used to further understand the sex-based cardiac efficiency relationship between cardiac function and flow.
Introduction
To understand why the hearts of men and women respond differtly to physiological stresses and disease, efforts have been made to study sex differences in healthy baseline cardiac anatomy and function(1–3). sex differences have been detected in myocardial contractile performance, resting heart rate, cardiac growth, stroke volume response to exercise, and arterial blood pressure (1, 4). Differences in myocyte contraction have been supported by evidence of higher circumferential and longitudinal strain in the left ventricle of women than in the left ventricle of men using cardiovascular magnetic resonance feature tracking (5, 6). However, the relationship of such metrics as strain to the output of the heart (blood flow) has not yet been fully explained.
A method that has recently gained traction in the evaluation of cardiac function is flow analysis with Four-dimensional flow magnetic resonance imaging (4D Flow MRI). Through analysis of blood velocity and derived hemodynamic metrics, cardiac energetics and components of cardiac work can be analyzed. (7–14). Kinetic energy (KE) metric in particular may indicate the amount of energy that is dissipated in blood motion, and therefore can be used with flow parameters to provide ventricular efficiency indices. Furthermore, KE can be calculated with velocity information alone, making it analysis much less invasive.It has also been suggested that a healthy heart will remain efficient by minimizing the dissipation of KE through the formation of large vortex rings (11, 12, 17). Recent KE and vortex studies have provided insight in the flow dynamics of a variety of heart diseases(7, 9, 11–14, 17–20). Some work has also been done to compare the regional ventricular blood flow vortex development across gender and age (21). However, to our knowledge, no study to date has examined differences in both kinetic energy and vorticity metrics, and their relationship to cardiac strain, between the left ventricle of men and women with 4D flow MRI. Therefore, the purpose of this study was to determine sex differences in ventricular flow dynamics, coupled with cardiac strain, of healthy volunteers.
Methods
Human Subjects:
In this Institutional Review Board approved and Health Insurance Portability and Accountability Act – compliant study, data from thirty-nine healthy volunteers (twenty male age 25.8 ±, 2.7, nineteen female age 27.1 ± 2.9 years) were used. Data from nineteen of the healthy volunteers was analyzed retrospectively. Of this retrospective nineteen, fifteen have overlap from a study examining differences in cardiac flow between single ventricle patients and healthy volunteers(14). The remaining four were data sets (from the retrospective nineteen) were from a preliminary study aimed at setting up the analysis methods of this study. When differences were observed in our original retrospective cases, twenty additional volunteers were recruited prospectively, per the power analysis described in the statistical analysis section of this manuscript. Written informed consent was obtained, and each healthy subject underwent a health screening for cardiovascular disease before enrollment. Body surface area was calculated for each subject based on height and weight, except for the original four preliminary study subjects, whose heights were not recorded.
MRI Flow Acquisition:
For the 4D flow MRI acquisition, the subjects were scanned on a 3.0T clinical system (MR750 and Signa Premier, GE Healthcare) using an investigational 4D Flow MRI sequence known as PC-VIPR.(22, 23) 4D Flow MRI parameters were: 1.25mm isotropic spatial resolution, 320mm field of view, 6.2 ms repetition time, 160 cm/s velocity encoding, and11 minute scan time. A method for double gating to the electrocardiograph and respiratory cycles was used. This resportatory gating method was based on a bellows signal, and it provided a cardiac series of flow data for separate respiratory phases during a single free-breathing scan (24). A moving average filter was applied to the respiratory waveform to subdivide data into two 4D flow MRI datasets: above and below the moving average bellows signal. A 40% acceptance threshold above and below the moving average for each respiratory cycle was applied to mitigate potential motion during active respiration. Contrast agent was used in the 15 healthy volunteers from the study examining single ventricle flow in order to match the patient group in that study. However, contrast agent was not administered in the prospectively recruited subjects.
Two-dimensional (2D) cine images were taken at increments throughout the heart of each volunteer in the short-axis, long-axis, two chamber, and four chamber orientations. Cine SSFP images had imaging parameters of 146×146mm field of view, 7mm slice thickness, flip angle of 45 degrees, TE of 1.18 ms, TR of 3.26 ms, and a X-Y spatial resolution of 1.37 mm.
4D Flow MRI Analysis:
Segmentation:
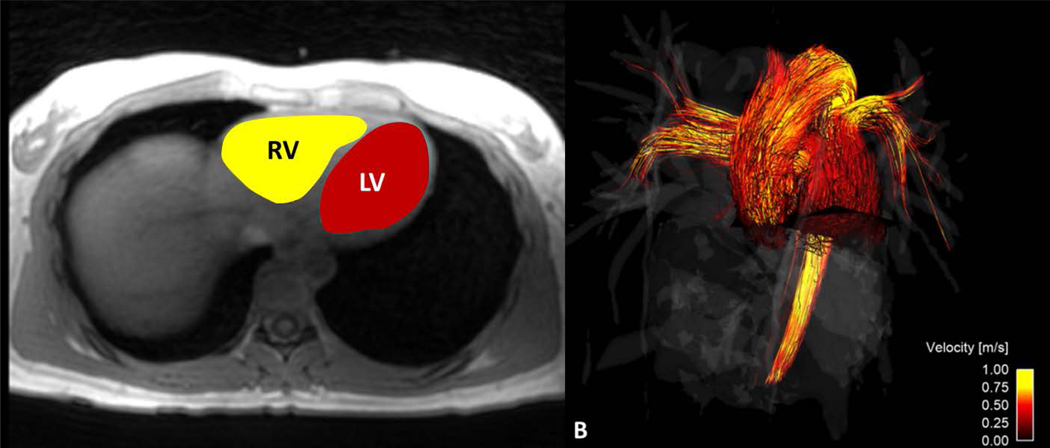
Time-averaged magnitude images from the 4D flow MRI data were exported in DICOM format to semiautomatic segmentation software (Mimics, Materialise, Leuven, Belgium) to segment the RV and LV of each subject. Time-averaged analysis was selected instead of time-resolved analysis a couple of reasons. First, the time-resolved images produced low ventricle boundary contrast, making reliable ventricular segmentation difficult. It has been shown in past work that usage of time-resolved images for ventricle segmentation can lead to much higher intra-observer error in flow analysis metrics(25). Second, time-averaged data processing is much quicker relative to the decrease in ventricle accuracy that is obtained vs. time-resolved processing. And, because data in this study were used for group comparison, the difference between group flow metrics was of more importance than the exact magnitude of individual metrics across the cardiac cycle. After segmentation, the time-averaged ventricular volumes were created by interpolating between the boundaries of the marked regions of each axial slice (Figure 1a). The ventricular volume data were exported in grayvalue format to be used for kinetic energy analysis.
Figure 1.
4D Flow MRI was used to calculate (A) kinetic energy in the right (RV) and left (LV) ventricles. Time-averaged 4D Flow MRI magnitude data were used to segment the RV and LV and (B) flow through the main pulmonary artery (MPA) and ascending aorta (Aao)
Flow:
Time-resolved 4D Flow MRI data were reconstructed into 14 time frames per cardiac cycle. For group analysis purposes, individual flow curves were registered by matching cardiac cycle time frames according to peak systole. Phase offsets for Maxwell terms and eddy currents were corrected automatically during reconstruction (22, 26). The eddy current correction was performed using 2nd order polynomial fitting of background tissue segmented based on thresholding of an angiogram. Velocity-weighted angiograms were calculated from the final velocity and magnitude data for all 14 time frames (23). Data were imported to Ensight (CEI, Apex, NC), where two-dimensional analysis planes were placed orthogonal to the ascending aorta (AAo) and main pulmonary artery (MPA) (Figure 1b). Flow (Q) measurements were made at each plane for each time frame of the cardiac cycle.
Kinetic Energy:
The KE within each ventricle was quantified through analysis of the MR image data files and ventricular volumes using Matlab (Mathworks, Natick, MA). This calculation was made with the standard KE equation, KE = ½ mv2. The mass of blood, m, was calculated by multiplying the density of blood (ρ = 1060 kg/m3) by the volume of each voxel within the ventricle. The velocity, v, of each voxel was obtained throughout the cardiac cycle from the 4D Flow MRI data. The KE from each voxel within the ventricular volume was then summed to obtain the total KE in both the RV (KERV) and LV (KELV) of each subject during all frames of the cardiac cycle. Lastly, QMPA and QAAo were normalized to KERV and KELV, respectively, as an index of cardiac efficiency.
Efficiency Index:
The aortic flow of each volunteer was normalized to the respective ventricular KE, as an index of cardiac efficiency. The resulting parameter was termed the efficiency index, with the intention of representing how much flow was generated per amount of kinetic energy dissipated. We hypothesized that a large amount of flow generated per a small amount of kinetic energy dissipated would indicate a more efficient system.
Vorticity:
Vorticity represents the magnitude of the three components of flow rotation,
where x, y, and z represent the three coordinate directions, and u, v, and w represent the velocity components in x, y, and z, respectively. As noted earlier, the degree of vortex formation may indicate the level of energy conservation in the ventricular flow. Using 4D Flow MRI data, the components of flow rotation were computed within each voxel of the segmented ventricular volumes. The magnitudes of the three components of vorticity were computed and summed throughout each ventricle. This time-averaged calculation was performed for each subject in Ensight (CEI, Apex, NC).
Cardiac Strain and Cardiac Function:
Strain was calculated from 2D short-axis MRI images based on the lengthening and shortening of the left ventricle wall using Segment 2.2 R6423 (http://segment.heiberg.se/) software. Strain analysis reproducibility with Segment has been demonstrated in past work. Global systolic and diastolic strains were calculated for longitudinal, circumferential and radial dimensions(29). Additionally, cardiac function metrics of stroke volume, end-diastolic volume, end-systolic volume, cardiac output, and ejection fraction were calculated using Segment software.
Statistical Analysis:
In order to determine the number of prospectively recruited subjects required to obtain 90% power to detect a difference of p<0.05, we used peak systolic vorticity index (rad/s/ml) differences in males and females. Based on our preliminary data (data from the original retrospective 19 volunteers) with an effect size of 0.0032 and a pooled standard deviation of 0.00425, we needed 18 subjects in each group to avoid type I errors for investigating sex differences. Power calculations were also performed on LV peak systolic KE and LV KE efficiency, and it was determined that two to three more subjects would be needed to be sufficiently powered to determine sex differences. Therefore, increasing the sample size to twenty in each group, we had high confidence in being sufficiently powered to determine sex differences in several fluid dynamic parameters.
Hemodynamic parameters measured from volunteer data that were noramly distributed were compared using a Student’s t-test. Normality of the data was tested for with both a D’Agostino & Pearson normality test and a Shapiro-Wilk normality test. For variables that were not definitively normally distributed, a Mann-Whitney test was used for statistical analysis. Note, however, that statistical analysis with both test types produced very similar results on statistical significance. Pearson correlation coefficient analyses were also performed to determine the strength of correlations between measured parameters. Results were visually plotted with cardiac-cycle averaged line plots and box plots to represent data spread. Summary results in the text were reported as mean ± standard deviation.
Results
4D Flow MRI
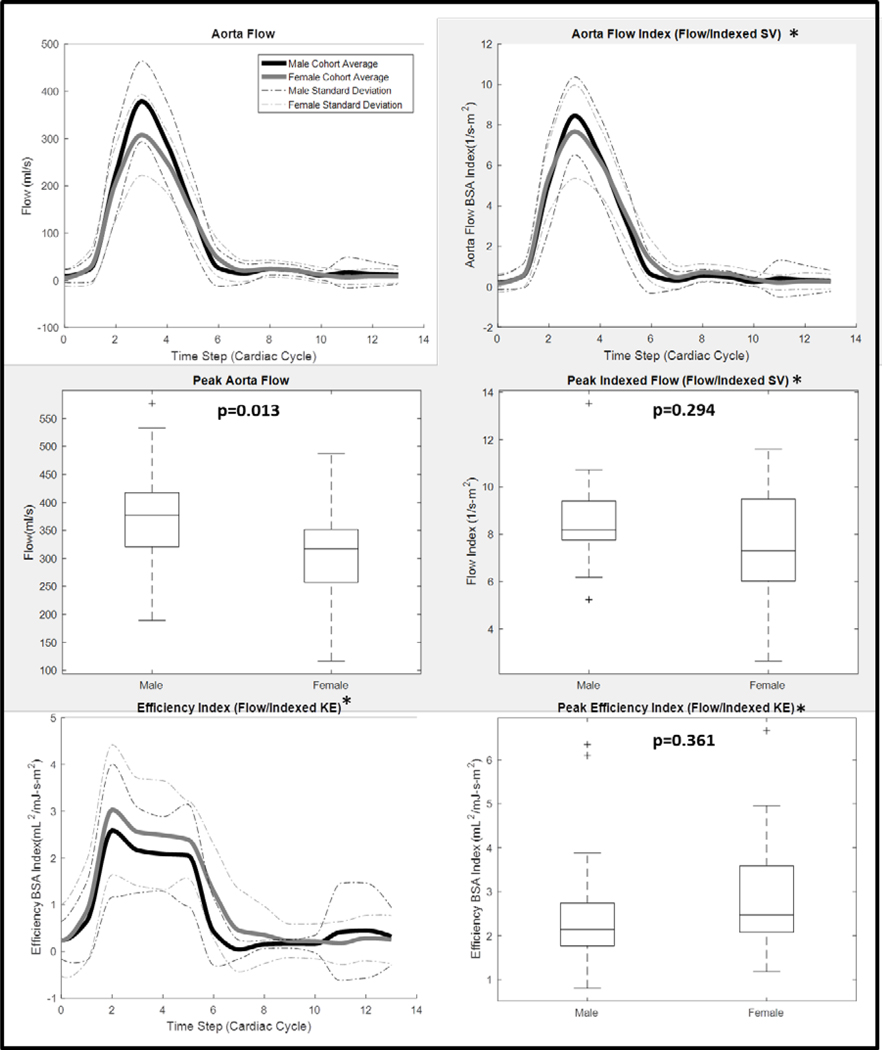
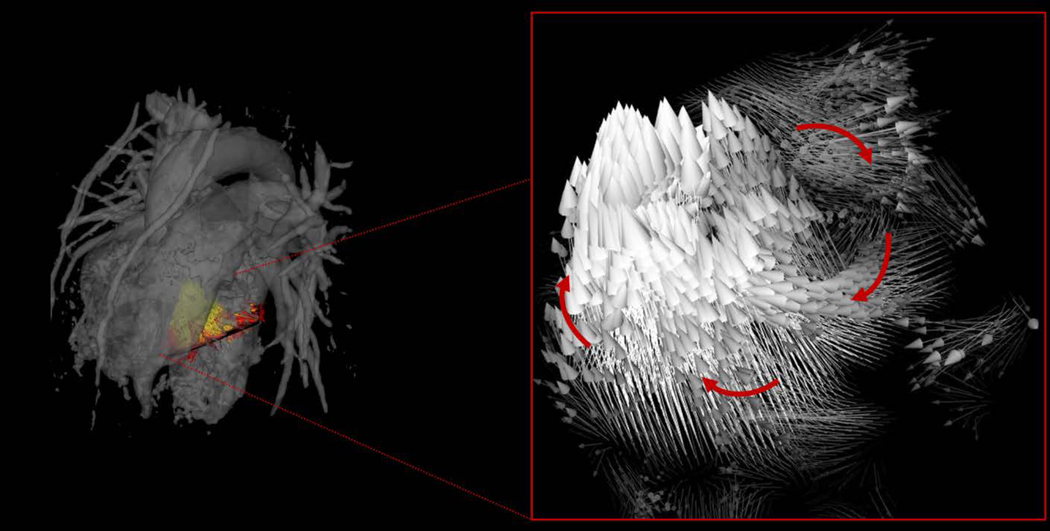
4D flow MRI-derived metrics were plotted across the group-average cardiac cycle for men and women, and peak flow parameters were compared between groups, as shown in Figures 2–4. As seen in figure 2, peak systolic blood kinetic energy (male: 4.76 ± 2.66 [mJ]; female: 3.36 ± 1.43 [mJ]; p=0.047) was significantly higher in the male LV than in the female LV. However, when KE was normalized to stroke volume index the peak systolic difference was not significant (male: 0.107 ± 0.061 [mJ-m2/mL]; female: 0.091 ± 0.040 [mJ-m2/mL]; p=0.353). Furthermore, although visible differences were observed in LV diastolic kinetic energy index between men and women (Figure 2, cardiac time step 8–10), they were not significant. Peak aortic flow (male: 378.96 ± 85.21 [ml/s]; female: 307.67 ± 85.50 [ml/s]; p=0.013) was significantly higher in the aorta of men than it was in women (Figure 3). Yet, when the flow was normalized by stroke volume index, peak systolic differences were not significant. Efficiency index was generally higher in women than in men (figure 3), although this difference was also not significant. When analyzing LV blood flow vorticity, significant differences were observed in peak systolic vorticity index (male: 0.008 ± 0.005 [rad-m2/ml-s]; female: 0.014 ± 0.007 [rad-m2/ml-s]; p=0.007), peak diastolic vorticity index (male: 0.007 ± 0.006 [rad-m2/ml-s]; female: 0.014 ± 0.010 [rad-m2/ml-s]; p=0.015), and cycle-average vorticity (male: 0.006 ± 0.001 [rad/s]; female: 0.011 ± 0.002 [rad/s]; p=0.001). As seen in Figure 4, all of these vorticity markers were higher in the LV of women than in the LV of men. A qualitative qualitative representation of blood velocity vectors was generated in a plane of a left ventricle, as seen in Figure 5.
Figure 2.
4D flow MRI data were used to calculate left ventricle blood flow kinetic energy throughout the cardiac cycle for 20 healthy men and 19 healthy women. Cardiac function data from 2D short-axis MR images were used, in conjunction with body surface areas, to create a kinetic energy index parameter. *Indexed data was reported on 35 of the 39 volunteers: BSA was not recorded for 4 subjects
Figure 4.
4D flow MRI data were used to calculate left ventricle blood flow vorticity throughout the cardiac cycle for 20 healthy men and 19 healthy women. Cardiac function data from 2D short-axis MR images were used, in conjunction with volunteer body surface areas, to create a vorticity index parameter. *Indexed data was reported on 35 of the 39 volunteers: BSA was not recorded for 4 subjects
Figure 3.
4D flow MRI data were used to calculate aorta flow throughout the cardiac cycle for 20 healthy men and 19 healthy women. Cardiac function data from 2D short-axis MR images were used, in conjunction with body surface areas, to create an aorta flow index parameter. *Indexed data was reported on 35 of the 39 volunteers: BSA was not recorded for 4 subjects
Figure 5.
4D flow MRI data were used to create velocity vector visualizations of left ventricle blood flow througout the cardiac cycle in healthy volunteers. Through this visualization, areas of vortex formation were observed, as emphasized with arrows.
Myocardial Strain
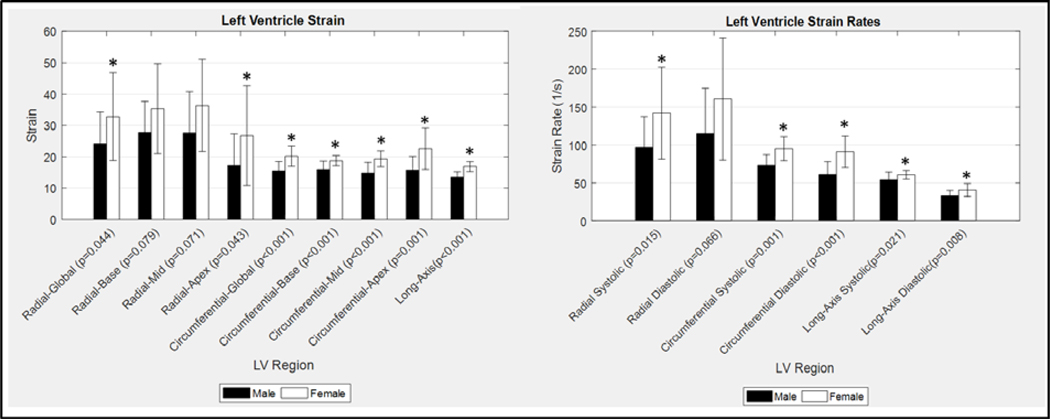
Myocardial strain metrics derived from 2D cine images were also recorded and compared between men and women. Figure 6 displays the LV radial, circumferential, and long-axis strain values of men and women, as well as the LV strain rates. Radial global (male: 24.18 ± 10.08; female: 32.81 ± 13.98; p=0.044), radial apex (male: 17.19 ± 10.17; female: 26.75 ± 15.85; p=0.043), circumferential global (male: 15.50 ± 3.01; female: 20.20 ± 3.25; p<0.001), circumferential base (male: 15.96 ± 2.65; female: 18.74 ± 1.63; p<0.001), circumferential mid (male: 14.81 ± 3.41; female: 19.32 ± 2.52; p<0.001), circumferential apex (male: 15.72 ± 4.42; female: 22.55 ± 6.56; p=0.001), and long-axis (male: 13.50 ± 1.75; female: 16.88 ± 1.58; p<0.001) LV strain were all significantly higher in women than they were in men. Additionally, radial systolic (male: 97.04 ± 40.37 [1/s]; female: 141.90 ± 60.43 [1/s]; p=0.015), circumferential systolic (male: 73.12 ± 13.96 [1/s]; female: 95.06 ± 15.72 [1/s]; p=0.001), circumferential diastolic (male: 61.16 ± 16.87 [1/s]; female: 90.95 ± 20.83 [1/s]; p<0.001), long-axis systolic (male: 53.96 ± 10.39 [1/s]; female: 60.77 ± 5.78 [1/s]; p=0.021), and long-axis diastolic (male: 33.08 ± 6.89 [1/s]; female: 40.63 ± 8.52 [1/s]; p=0.008) LV strain rates were all significantly higher in women than in men. Furthermore, circumferential systolic and diastolic strain rates displayed moderate correlation to peak systolic (r=−0.38, p=0.022) and diastolic vorticity (r=0.40, p=0.015) values, respectively (Figure 7). There were also many moderate correlations observed when comparing both strain and flow parameters with left ventricle mass and heart rate, as seen in tables 1 and 2. In particular, peak aortic flow and many strain rates were significantly correlated to both left ventricle mass and heart rate.
Figure 6.
Cardiac strain was calculated in the radial, circumferential, and long-axis orientation in the left ventricle of 20 healthy men and 19 healthy women. Additionally, systolic and diastolic strain rates were recorded. *Significant sex-based differences were observed, as noted.althy men and 19 healthy women. Additionally, systolic and diastolic strain rates were recorded. *Significant sex-based differences were observed, as noted.
Figure 7.
Left Ventricle strain rates obtained from 2D cine images were compared with left ventricle blood flow kinetic energy derived from 4D flow MRI data. A moderate relationship was observed in both systolic and diastolic phases of the cardiac cycle. Note that increased strain is correlated with increased vorticity in both systole (negative strain) and diastole (positive strain). The sign (positive vs. negative) of the strain metrics in systole and diastole are opposite in order to maintain consistency of wall motion with the designated coordinate direction (wall moving inward in systole and outward in diastole).
Table 1.
Cardiovascular magnetic resonance (CMR) strain and flow metric correlations with left ventricular mass (LVM).
| CMR Parameter | Correlation coefficient (r) | p-value |
|---|---|---|
| Radial Strain | −0.34 | 0.055 |
| Radial SSR | −0.39 | 0.029 |
| Radial DSR | 0.40 | 0.022 |
| Circumferential Strain | 0.56 | <0.001 |
| Circumferential SSR | 0.59 | <0.001 |
| Circumferential DSR | −0.61 | <0.001 |
| Longitudinal Strain | 0.58 | <0.001 |
| Longitudinal SSR | 0.37 | 0.037 |
| Longitudinal DSR | −0.43 | 0.013 |
| Peak Systolic KE | 0.47 | 0.004 |
| Peak Diastolic KE | 0.05 | 0.774 |
| Peak Aortic Flow | 0.64 | <0.001 |
| Peak Systolic Vorticity | −0.21 | 0.225 |
| Peak Diastolic Vorticity | −0.38 | 0.023 |
Abbreviations: SSR, systolic strain rate; DSR, diastolic strain rate; KE, kinetic energy
Table 2.
Cardiovascular magnetic resonance (CMR) strain and flow metric correlations with heart rate (HR).
| CMR Parameter | Correlation coefficient (r) | p-value |
|---|---|---|
| Radial Strain | 0.50 | 0.002 |
| Radial SSR | 0.53 | 0.001 |
| Radial DSR | −0.56 | <0.001 |
| Circumferential Strain | −0.35 | <0.001 |
| Circumferential SSR | −0.56 | <0.001 |
| Circumferential DSR | 0.55 | <0.001 |
| Longitudinal Strain | −0.22 | 0.211 |
| Longitudinal SSR | −0.49 | 0.003 |
| Longitudinal DSR | 0.21 | 0.236 |
| Peak Systolic KE | −0.03 | 0.831 |
| Peak Diastolic KE | 0.25 | 0.125 |
| Peak Aortic Flow | −0.31 | 0.054 |
| Peak Systolic Vorticity | 0.43 | 0.006 |
| Peak Diastolic Vorticity | 0.46 | 0.003 |
Abbreviations: SSR, systolic strain rate; DSR, diastolic strain rate; KE, kinetic energy
Volumetric Data
Cardiac function data from the 2D short-axis cine images are recorded as male and female group averages in Table 3. Stroke volume (p<0.001), end systolic volume (p<0.001), end-diastolic volume (p<0.001), end systolic volume index (p=0.005), and end-diastolic volume index (p=0.012) were all significantly higher in men than they were in women. Stroke volume index was used to normalize ventricle blood flow KE, flow, and vorticity, as seen in Figures 2–4.
Table 3.
Cardiac function parameters obtained from two-dimensional short axis Magnetic Resonance Imaging. Stroke volume and body surface area were used to index flow parameters for men and women,
| Cardiac Parameter | Male | Female | p-value |
|---|---|---|---|
| Stroke Volume [mL] | 89.75 ± 15.26 | 69.32 ± 19.69 | 0.0009 |
| Stroke Volume BSA Index [ml/m2]* | 45.41 ±7.83 | 40.27± 11.06 | 0.138 |
| End Diastolic Volume [mL] | 168.35 ±27.24 | 124 ±27.10 | <0.001 |
| End Systolic Volume [mL] | 78.6 ±20.31 | 53.53 ±11.88 | <0.001 |
| Ejection Fraction [%] | 53.65 ±6.47 | 57.17 ±5.08 | 0.072 |
| Cardiac Output [L/min ] | 5.63 ±1.35 | 4.89 ± 1.50 | 0.130 |
| Heart Rate [bpm] | 63.05 ± 12.51 | 68.76 ± 10.32 | 0.137 |
| End Diastolic Volume Index [ml/m2]* | 84.99 ± 12.39 | 71.53 ±14.75 | 0.012 |
| End Systolic Volume Index [ml/m2]* | 39.58 ±9.37 | 30.84 ±7.18 | 0.005 |
| Cardiac Output Index [l/min-m2]* | 2.84 ±0.63 | 2.93 ±0.74 | 0.699 |
Indexed data was reported on 35 of the 39 volunteers: BSA was not recorded for 4 subjects
Discussion
The physiological differences in cardiac function between men and women are not fully understood. Although the development and application of many cardiac metrics on myocyte function and metabolism have shed light on sex differences in cardiac function (1, 4), a full connection between such metrics and cardiac flow has not been made. In an effort to further understand the connection between cardiac function and flow, as it relates to cardiac sex differences, this study used both traditional cardiac MRI and 4D flow MRI on 20 healthy men and 19 healthy women. We hypothesized that the young adult female heart would demonstrate increased indicators of myocardial function (increased myocardial strain, decreased energy use, more efficient flow patterns), as compared to the male heart. The major findings of this study were that women demonstrate increased systolic and diastolic 4D-flow MRI-derived vorticity and lower blood flow kinetic energy dissipation as compared to men. Additionally, the female heart showed increases in myocardial global strain and strain rates (systolic and diastolic), which may be related to the increased left ventricle vorticity observed with 4D flow MRI in women.
While there have been numerous studies that have probed sex differences in cardiac function, the majority of these studies have been either cross-sectional aging studies or in aged adults (30–35). Fewer studies have been strictly designed to determine sex differences in a young adult population, a time in life when women display a much lower incidence of CV disease (36, 37). In this study, we found that young women had smaller normalized LV volumes but increased systolic and diastolic function indicators (circumferential strain, blood flow vorticity) as measured by myocardial feature tracking strain and 4D flow MRI. These findings are consistent with a study by Petersen and colleagues, who used cardiac MRI in a large population and demonstrated smaller indexed LV volumes in older adult women compared to age-matched men(33). Previous work has also demonstrated that the female heart, prior to menopause, has augmented diastolic function (myocardial strain) compared to the age-matched male heart (34, 35), which corresponds to the results of this study which found increased diastolic strain rates and peak diastolic vorticity.
Sex dependent differences in systolic function in young adults have been equivocal when using standard clinical measurements (i.e. EF) (34, 35, 38). While we found that EF was slightly higher in women using cardiac MRI, this was not significant. However, myocardial strain has been used previously to discriminate systolic functional differences (5). This supports our findings of increased global myocardial strain and systolic strain rates in young adult women as compared to men. Additionally, we found that peak systolic vorticity is greater in the female LV as compared to the male LV, which is a potential measure that can help delineate sex-dependent systolic function. Taken together, our results agree well withmany of the previous findings of sex-dependent differences in cardiovascular function. However, the major contribution of this work is that it is the first to use 4D flow MRI and cardiac strain analysis to determine sex differences in myocardial function in a young healthy adult population.
4D flow MRI results revealed significantly higher peak systolic blood flow KE in the LV of men than in the LV of women. Considering published studies showing higher blood flow kinetic energy dissipation in the cardiac chambers of diseased patients than in more efficient healthy controls (11, 14, 18, 20), this may suggest that the LV of men is, in a way, less efficient that the LV of women. This may be further supported by the results of our efficiency index analysis, which showed that the ratio of flow to LV kinetic energy dissipation was generally higher in women than in men, although not statistically significant. It is, however, important to note that when KE was normalized to indexed stroke volume, the difference in peak systole was no longer significant.
In an effort to uncover more cardiac flow differences between sexes, metrics of ventricle blood flow vorticity were analyzed. Past studies have suggested that vortex core formation in the ventricular blood volume can be indicative of a more efficient, functioning heart (9, 13, 39–41). The presence of physiological vortex formation has been postulated to produce direct flow routes, which avoids excessive turbulence and energy dissipation, and may be a reflection of the heart’s ability to adapt to varying conditions. Whereas, in its absence, flow may develop a disordered motion, with an improper redirection of the blood during contraction, which may result in pathological peak pressure development (42). Previous work has determined that diastolic vorticity is a sensitive marker of diastolic function (39, 40, 43, 44). To our knowledge, what has been previously unexplored is systolic vorticity, and how it may be a mechanism of ventricular blood ejection. In this study, women exhibited augmented peak systolic vorticity, indexed to stroke volume, as compared to men. Subclinical systolic dysfunction is difficult to determine on the basis of measuring EF alone, while measures of myocardial deformation and 4D flow based metrics (i.e. vorticity) may provide a more sensitive modality for determining differences in systolic function that could be a marker for future outcomes in an otherwise healthy population. Taken together, increased myocardial function in young women compared to men may be a function of a lower energy dissipation of the blood in the LV during filling and ejection due to the greater vortical flow of the blood in the female heart. These metrics may shed light on sex-dependent changes in myocardial function with age, which may provide a clinical measure of cardiovascular disease risk.
Notably, data from the strain analysis of this study may support our hypotheses on increased functional efficiency of the female heart even further. Results displayed that circumferential and long-axis strain, as well as systolic and diastolic strain rates, were all higher in the LV of women than in the LV of men. Therefore, the higher strain, particularly in the circumferential direction, may have contributed to the higher vorticity observed in the female left ventricle. In turn, the higher vorticity may have led to more efficient flow and less energy dissipation in the female ventricle than in the male ventricle. We postulate that strain in the circumferential direction is related to twisting (systole) and untwisting (diastole) of the ventricle, and the enhanced circumferential systolic and diastolic strain rate observed in the female myocardium may permit the development of greater vortical flow as compared to the male myocardium. This postulated relationship between cardiac strain and blood flow vorticity was supported by the observation of moderate correlations between circumferential strain rate and peak vorticity, in both systole and diastole, and may explain in the underlying cardiac functional advantage young women display compared to age-matched men. Furthermore, myocardial strain was observed to have an inverse correlation relationship with left ventricle mass. This may suggest that one mechanism for increased myocardial strain in women is lower ventricular mass, which may allow for larger myocardial deformation in thinner myocardium. Due to the addition of 4D flow MRI data with such strain analysis, this would be the first report to our knowledge to relate sex-dependent myocardial deformation to blood flow dynamics in the heart. These measures of cardiac function may provide novel markers of age-dependent changes in myocardial function between sexes.
There are some limitations to this study that warrant discussion. First of all, the subject group for this study was taken from two separate data sets. The first half of the data set was obtained from the control participants of a study examining cardiac flow differences between healthy volunteers and single ventricle patients (11, 14). The second portion of the data set was obtained prospectively for this study. Nonetheless, both portions of the subject group had the same age and health recruitment requirements, and both studies used the same MRI protocols. Second, due to the fact that this study focuses on sex differences in cardiac flow physiology, it must be acknowledged that hormonal differences between subjects, such as menstrual cycle, were not controlled for. Previous work has shown that the menstrual cycle phase may alter cardiovascular function (45–50), although these findings are equivocal. Lastly, the ventricular flow metrics presented in this study were derived from time-averaged analysis. Due to the large amount of ventricular wall motion over the cardiac cycle, this may have introduced some quantification error. However, it is important to note that time-averaged analysis is weighted heavily to diastolic ventricle volumes. Therefore, the ventricular volumes used for analysis in this study encompassed a majority of the ventricular flow regime throughout the cardiac cycle. The portion of the cardiac cycle in which analysis would be affected the most would be during peak diastole, when the actual ventricle volume in larger than the segmented ventricle volume. And, because flow is lowest in peak diastole, many of the key flow metrics presented in this work would be expected to be unaffected. Furthermore, the alternative time-resolved analysis has been shown to produce a high amount of inter-observer error due to lower resolution of ventricle boundaries(25). Combining these factors with the fact that time-averaged analysis provides a much more time-efficient analysis, the time-averaged approach was taken in this work.
In conclusion, significant sex-based differences were observed in flow and cardiac strain parameters. The methods and results of this study may be used to further understand the intricate relationship between cardiac function and flow, as it relates to differences between male and female cardiac physiology.
Key Points:
Cardiac flow data was obtained from twenty healthy men and nineteen healthy women using four-dimensional flow MRI
MRI-derived parameters of blood flow kinetic energy (higher in men), vorticity (higher in women), and cardiac strain (higher in women) were compared between sexes
Moderate positive correlations were observed between left ventricle blood flow kinetic energy and circumferential strain. Such metrics and relationships may indicate cardiac efficiency discrepancies between sexes
Abbreviations:
- RV
Right Ventricle
- LV
Left Ventricle
- KE
Kinetic Energy
- IRB
Institutional Review Board
- HIPAA
Health insurance portability and accountability act
- 4D Flow MRI
Four Dimensional Flow Magnetic Resonance Imaging
- KERV
Right Ventricular Kinetic Energy
- KELV
Left Ventricular Kinetic Energy
- Q
Flow
- MPA
Main Pulmonary Artery
- AAo
Ascending Aorta
- QAAo
Ascending Aorta Flow
- QMPA
Main Pulmonary Artery Flow
- SW
Stroke Work
- PC-VIPR
Phase Contrast with Vastly Undersampled Isotropic Projection Reconstruction
- TA
Time-Averaged
- DICOM
Digital Imaging and Communications in Medicine
References
- 1.Kolar F, Ostadal B. Sex differences in cardiovascular function. Acta Physiol (Oxf) 2013;207(4):584–587. doi: 10.1111/apha.12057 [DOI] [PubMed] [Google Scholar]
- 2.Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, Shah RU, Regitz-Zagrosek V, Grewal J, Vaccarino V, Wei J, Bairey Merz CN. Sex differences in cardiovascular disease - Impact on care and outcomes. Front Neuroendocrinol 2017;46:46–70. doi: 10.1016/j.yfrne.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aggarwal NR, Patel HN, Mehta LS, Sanghani RM, Lundberg GP, Lewis SJ, Mendelson MA, Wood MJ, Volgman AS, Mieres JH. Sex Differences in Ischemic Heart Disease: Advances, Obstacles, and Next Steps. Circ Cardiovasc Qual Outcomes 2018;11(2):e004437. doi: 10.1161/CIRCOUTCOMES.117.004437 [DOI] [PubMed] [Google Scholar]
- 4.Pianosi PT, Emerling E, Mara KC, Weaver AL, Fischer PR. Sex differences in fitness and cardiac function during exercise in adolescents with chronic fatigue. Scand J Med Sci Sports 2018;28(2):524–531. doi: 10.1111/sms.12922 [DOI] [PubMed] [Google Scholar]
- 5.Lawton JS, Cupps BP, Knutsen AK, Ma N, Brady BD, Reynolds LM, Pasque MK. Magnetic resonance imaging detects significant sex differences in human myocardial strain. Biomed Eng Online 2011;10:76. doi: 10.1186/1475-925X-10-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andre F, Steen H, Matheis P, Westkott M, Breuninger K, Sander Y, Kammerer R, Galuschky C, Giannitsis E, Korosoglou G, Katus HA, Buss SJ. Age- and gender-related normal left ventricular deformation assessed by cardiovascular magnetic resonance feature tracking. J Cardiovasc Magn Reson 2015;17:25. doi: 10.1186/s12968-015-0123-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Wakeel N, Fernandes JF, Amiri A, Siniawski H, Goubergrits L, Berger F, Kuehne T. Hemodynamic and energetic aspects of the left ventricle in patients with mitral regurgitation before and after mitral valve surgery. J Magn Reson Imaging 2015;42(6):1705–1712. doi: 10.1002/jmri.24926 [DOI] [PubMed] [Google Scholar]
- 8.Arvidsson PM, Töger J, Heiberg E, Carlsson M, Arheden H. Quantification of left and right atrial kinetic energy using four-dimensional intracardiac magnetic resonance imaging flow measurements. J Appl Physiol (1985) 2013;114(10):1472–1481. doi: 10.1152/japplphysiol.00932.2012 [DOI] [PubMed] [Google Scholar]
- 9.Bermejo J, Benito Y, Alhama M, Yotti R, Martínez-Legazpi P, Del Villar CP, Pérez-David E, González-Mansilla A, Santa-Marta C, Barrio A, Fernández-Avilés F, Del Álamo JC. Intraventricular vortex properties in nonischemic dilated cardiomyopathy. Am J Physiol Heart Circ Physiol 2014;306(5):H718–729. doi: 10.1152/ajpheart.00697.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlsson M, Heiberg E, Toger J, Arheden H. Quantification of left and right ventricular kinetic energy using four-dimensional intracardiac magnetic resonance imaging flow measurements. Am J Physiol Heart Circ Physiol 2012;302(4):H893–900. doi: 10.1152/ajpheart.00942.2011 [DOI] [PubMed] [Google Scholar]
- 11.Han QJ, Witschey WR, Fang-Yen CM, Arkles JS, Barker AJ, Forfia PR, Han Y. Altered Right Ventricular Kinetic Energy Work Density and Viscous Energy Dissipation in Patients with Pulmonary Arterial Hypertension: A Pilot Study Using 4D Flow MRI. PLoS One 2015;10(9):e0138365. doi: 10.1371/journal.pone.0138365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanski M, Arvidsson PM, Töger J, Borgquist R, Heiberg E, Carlsson M, Arheden H. Left ventricular fluid kinetic energy time curves in heart failure from cardiovascular magnetic resonance 4D flow data. J Cardiovasc Magn Reson 2015;17:111. doi: 10.1186/s12968-015-0211-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pierrakos O, Vlachos PP. The effect of vortex formation on left ventricular filling and mitral valve efficiency. J Biomech Eng 2006;128(4):527–539. doi: 10.1115/1.2205863 [DOI] [PubMed] [Google Scholar]
- 14.Rutkowski DR, Barton G, François CJ, Bartlett HL, Anagnostopoulos PV, Roldán-Alzate A. Analysis of cavopulmonary and cardiac flow characteristics in fontan Patients: Comparison with healthy volunteers. J Magn Reson Imaging 2019. doi: 10.1002/jmri.26583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PREC O KATZ LN. Determination of kinetic energy of the heart in man. Am J Physiol 1949;159(3):483–491. [DOI] [PubMed] [Google Scholar]
- 16.Katz AM. Physiology of the Heart: Wolters Kluwer Health, 2015. [Google Scholar]
- 17.Gürel E, Prinz C, Van Casteren L, Gao H, Willems R, Voigt JU. The Impact of Function-Flow Interaction on Left Ventricular Efficiency in Patients with Conduction Abnormalities: A Particle Image Velocimetry and Tissue Doppler Study. J Am Soc Echocardiogr 2016;29(5):431–440. doi: 10.1016/j.echo.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 18.Sjöberg P, Heiberg E, Wingren P, Ramgren Johansson J, Malm T, Arheden H, Liuba P, Carlsson M. Decreased Diastolic Ventricular Kinetic Energy in Young Patients with Fontan Circulation Demonstrated by Four-Dimensional Cardiac Magnetic Resonance Imaging. Pediatr Cardiol 2017;38(4):669–680. doi: 10.1007/s00246-016-1565-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong J, Chabiniok R, Pushparajah K, Sammut E, Tibby SM, Celermajer D, Giese D, Hussain T, Greil G, Schaeffter T, Razavi R. Kinetic Energy Ejection Fraction: A Better Marker Of Cardiac Function In The Single Ventricle Circulation. Journal of the American College of Cardiology 2015;65(10). [Google Scholar]
- 20.Jeong D, Anagnostopoulos PV, Roldan-Alzate A, Srinivasan S, Schiebler ML, Wieben O, François CJ. Ventricular kinetic energy may provide a novel noninvasive way to assess ventricular performance in patients with repaired tetralogy of Fallot. J Thorac Cardiovasc Surg 2015;149(5):1339–1347. doi: 10.1016/j.jtcvs.2014.11.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Föll D, Taeger S, Bode C, Jung B, Markl M. Age, gender, blood pressure, and ventricular geometry influence normal 3D blood flow characteristics in the left heart. Eur Heart J Cardiovasc Imaging 2013;14(4):366–373. doi: 10.1093/ehjci/jes196 [DOI] [PubMed] [Google Scholar]
- 22.Gu T, Korosec FR, Block WF, Fain SB, Turk Q, Lum D, Zhou Y, Grist TM, Haughton V, Mistretta CA. PC VIPR: a high-speed 3D phase-contrast method for flow quantification and high-resolution angiography. AJNR Am J Neuroradiol 2005;26(4):743–749. [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson KM, Lum DP, Turski PA, Block WF, Mistretta CA, Wieben O. Improved 3D phase contrast MRI with off-resonance corrected dual echo VIPR. Magn Reson Med 2008;60(6):1329–1336. doi: 10.1002/mrm.21763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schrauben EM, Anderson AG, Johnson KM, Wieben O. Respiratory-induced venous blood flow effects using flexible retrospective double-gating. J Magn Reson Imaging 2015;42(1):211–216. doi: 10.1002/jmri.24746 [DOI] [PubMed] [Google Scholar]
- 25.Hussaini SF, Rutkowski DR, Roldán-Alzate A, François CJ. Left and right ventricular kinetic energy using time-resolved versus time-average ventricular volumes. J Magn Reson Imaging 2017;45(3):821–828. doi: 10.1002/jmri.25416 [DOI] [PubMed] [Google Scholar]
- 26.Walker PG, Cranney GB, Scheidegger MB, Waseleski G, Pohost GM, Yoganathan AP. Semiautomated method for noise reduction and background phase error correction in MR phase velocity data. J Magn Reson Imaging 1993;3(3):521–530. [DOI] [PubMed] [Google Scholar]
- 27.Heiberg E, Sjögren J, Ugander M, Carlsson M, Engblom H, Arheden H . Design and validation of Segment--freely available software for cardiovascular image analysis. BMC Med Imaging 2010;10:1. doi: 10.1186/1471-2342-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heyde B, Jasaityte R, Barbosa D, Robesyn V, Bouchez S, Wouters P, Maes F, Claus P, D’hooge J. Elastic image registration versus speckle tracking for 2-D myocardial motion estimation: a direct comparison in vivo. IEEE Trans Med Imaging 2013;32(2):449–459. doi: 10.1109/TMI.2012.2230114 [DOI] [PubMed] [Google Scholar]
- 29.Morais P, Marchi A, Bogaert JA, Dresselaers T, Heyde B, D’hooge J, Bogaert J. Cardiovascular magnetic resonance myocardial feature tracking using a non-rigid, elastic image registration algorithm: assessment of variability in a real-life clinical setting. J Cardiovasc Magn Reson 2017;19(1):24. doi: 10.1186/s12968-017-0333-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosen BD, Cushman M, Nasir K, Bluemke DA, Edvardsen T, Fernandes V, Lai S, Tracy RP, Lima JA. Relationship between C-reactive protein levels and regional left ventricular function in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis. J Am Coll Cardiol 2007;49(5):594–600. doi: 10.1016/j.jacc.2006.09.040 [DOI] [PubMed] [Google Scholar]
- 31.Fernandes VR, Edvardsen T, Rosen BD, Carvalho B, Campos O, Cordeiro MA, Kronmal R, Bluemke DA, Lima JA. The influence of left ventricular size and global function on regional myocardial contraction and relaxation in an adult population free of cardiovascular disease: a tagged CMR study of the MESA cohort. J Cardiovasc Magn Reson 2007;9(6):921–930. doi: 10.1080/10976640701693824 [DOI] [PubMed] [Google Scholar]
- 32.Merz CN, Moriel M, Rozanski A, Klein J, Berman DS. Gender-related differences in exercise ventricular function among healthy subjects and patients. Am Heart J 1996;131(4):704–709. [DOI] [PubMed] [Google Scholar]
- 33.Petersen SE, Aung N, Sanghvi MM, Zemrak F, Fung K, Paiva JM, Francis JM, Khanji MY, Lukaschuk E, Lee AM, Carapella V, Kim YJ, Leeson P, Piechnik SK, Neubauer S. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J Cardiovasc Magn Reson 2017;19(1):18. doi: 10.1186/s12968-017-0327-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daimon M, Watanabe H, Abe Y, Hirata K, Hozumi T, Ishii K, Ito H, Iwakura K, Izumi C, Matsuzaki M, Minagoe S, Abe H, Murata K, Nakatani S, Negishi K, Yoshida K, Tanabe K, Tanaka N, Tokai K, Yoshikawa J, Investigators JNVfEMPJS. Gender differences in age-related changes in left and right ventricular geometries and functions. Echocardiography of a healthy subject group. Circ J 2011;75(12):2840–2846. [DOI] [PubMed] [Google Scholar]
- 35.Okura H, Takada Y, Yamabe A, Kubo T, Asawa K, Ozaki T, Yamagishi H, Toda I, Yoshiyama M, Yoshikawa J, Yoshida K. Age- and gender-specific changes in the left ventricular relaxation: a Doppler echocardiographic study in healthy individuals. Circ Cardiovasc Imaging 2009;2(1):41–46. doi: 10.1161/CIRCIMAGING.108.809087 [DOI] [PubMed] [Google Scholar]
- 36.Colditz GA, Willett WC, Stampfer MJ, Rosner B, Speizer FE, Hennekens CH. Menopause and the risk of coronary heart disease in women. N Engl J Med 1987;316(18):1105–1110. doi: 10.1056/NEJM198704303161801 [DOI] [PubMed] [Google Scholar]
- 37.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet 1999;353(9147):89–92. doi: 10.1016/S0140-6736(98)10279-9 [DOI] [PubMed] [Google Scholar]
- 38.Natori S, Lai S, Finn JP, Gomes AS, Hundley WG, Jerosch-Herold M, Pearson G, Sinha S, Arai A, Lima JA, Bluemke DA. Cardiovascular function in multi-ethnic study of atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol 2006;186(6 Suppl 2):S357–365. doi: 10.2214/AJR.04.1868 [DOI] [PubMed] [Google Scholar]
- 39.Elbaz MS, van der Geest RJ, Calkoen EE, de Roos A, Lelieveldt BP, Roest AA, Westenberg JJ. Assessment of viscous energy loss and the association with three-dimensional vortex ring formation in left ventricular inflow: In vivo evaluation using four-dimensional flow MRI. Magn Reson Med 2017;77(2):794–805. doi: 10.1002/mrm.26129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fenster BE, Browning J, Schroeder JD, Schafer M, Podgorski CA, Smyser J, Silveira LJ, Buckner JK, Hertzberg JR. Vorticity is a marker of right ventricular diastolic dysfunction. Am J Physiol Heart Circ Physiol 2015;309(6):H1087–1093. doi: 10.1152/ajpheart.00278.2015 [DOI] [PubMed] [Google Scholar]
- 41.Hong GR, Pedrizzetti G, Tonti G, Li P, Wei Z, Kim JK, Baweja A, Liu S, Chung N, Houle H, Narula J, Vannan MA. Characterization and quantification of vortex flow in the human left ventricle by contrast echocardiography using vector particle image velocimetry. JACC Cardiovasc Imaging 2008;1(6):705–717. doi: 10.1016/j.jcmg.2008.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sengupta PP, Pedrizzetti G, Kilner PJ, Kheradvar A, Ebbers T, Tonti G, Fraser AG, Narula J. Emerging trends in CV flow visualization. JACC Cardiovasc Imaging 2012;5(3):305–316. doi: 10.1016/j.jcmg.2012.01.003 [DOI] [PubMed] [Google Scholar]
- 43.Schäfer M, Browning J, Schroeder JD, Shandas R, Kheyfets VO, Buckner JK, Hunter KS, Hertzberg JR, Fenster BE. Vorticity is a marker of diastolic ventricular interdependency in pulmonary hypertension. Pulm Circ 2016;6(1):46–54. doi: 10.1086/685052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schäfer M, Humphries S, Stenmark KR, Kheyfets VO, Buckner JK, Hunter KS, Fenster BE. 4D-flow cardiac magnetic resonance-derived vorticity is sensitive marker of left ventricular diastolic dysfunction in patients with mild-to-moderate chronic obstructive pulmonary disease. Eur Heart J Cardiovasc Imaging 2018;19(4):415–424. doi: 10.1093/ehjci/jex069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shenouda N, Priest SE, Rizzuto VI, MacDonald MJ. Brachial artery endothelial function is stable across a menstrual and oral contraceptive pill cycle but lower in premenopausal women than in age-matched men. Am J Physiol Heart Circ Physiol 2018;315(2):H366–H374. doi: 10.1152/ajpheart.00102.2018 [DOI] [PubMed] [Google Scholar]
- 46.Priest SE, Shenouda N, MacDonald MJ. Effect of sex, menstrual cycle phase, and monophasic oral contraceptive pill use on local and central arterial stiffness in young adults. Am J Physiol Heart Circ Physiol 2018;315(2):H357–H365. doi: 10.1152/ajpheart.00039.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW. Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med (Maywood) 2010;235(1):111–118. doi: 10.1258/ebm.2009.009186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.D’Urzo KA, King TJ, Williams JS, Silvester MD, Pyke KE. The impact of menstrual phase on brachial artery flow-mediated dilatation during handgrip exercise in healthy premenopausal women. Exp Physiol 2018;103(2):291–302. doi: 10.1113/EP086311 [DOI] [PubMed] [Google Scholar]
- 49.Yazar Ş, Yazıcı M. Impact of Menstrual Cycle on Cardiac Autonomic Function Assessed by Heart Rate Variability and Heart Rate Recovery. Med Princ Pract 2016;25(4):374–377. doi: 10.1159/000444322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abidi S, Nili M, Serna S, Kim S, Hazlett C, Edgell H. Influence of sex, menstrual cycle, and oral contraceptives on cerebrovascular resistance and cardiorespiratory function during Valsalva or standing. J Appl Physiol (1985) 2017;123(2):375–386. doi: 10.1152/japplphysiol.00035.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]