Abstract
IMPORTANCE
In response to the opioid epidemic, policies aiming to reduce opioid prescribing, misuse, and abuse may have the unintended consequence of restricting access to necessary opioid therapy for cancer-related pain. It is unknown how opioid prescribing patterns have changed among generalists and oncologists during this era.
OBJECTIVE
To examine trends in opioid prescription rates for Medicare Part D beneficiaries from 2013 to 2017 among oncologists and generalists.
DESIGN, SETTING, AND PARTICIPANTS
This repeated cross-sectional study of generalist physicians (internal medicine, family medicine, geriatric medicine, general practice) and oncology specialists (medical oncology, hematology-oncology, and radiation oncology) analyzed the Medicare Provider Utilization and Payment Data: Part D prescriber files from 2013 to 2017.
EXPOSURES
Generalist vs oncology specialty.
MAIN OUTCOMES AND MEASURES
Outcomes included physician-level rates of both opioid and long-acting opioid prescriptions per 100 Medicare Part D beneficiaries. Poisson regression was used to estimate annual predicted outcome rates and incidence rate ratios, adjusting for prescriber characteristics and state fixed effects.
RESULTS
We analyzed the prescribing patterns of 251 820 generalists and 14 210 oncologists. From 2013 to 2017, the annual adjusted predicted mean rate of opioid prescriptions per 100 Medicare beneficiaries decreased from 68.2 to 49.7 among generalists (adjusted incidence rate ratio [aIRR] = 0.73; 95% CI, 0.73–0.73) and from 77.8 to 58.8 among oncologists (aIRR = 0.76; 95% CI, 0.74–0.77). The rate of long-acting opioid prescriptions per 100 Medicare beneficiaries also decreased from 8.0 to 5.4 for generalists (aIRR = 0.67; 95% CI, 0.66–0.68) and from 18.6 to 13.3 for oncologists (aIRR = 0.72; 95% CI, 0.69–0.74).
CONCLUSIONS AND RELEVANCE
We found large declines in opioid prescription rates for Medicare beneficiaries by generalists and oncologists from 2013 to 2017. Opioid policy and advocacy appear to have been effective in reducing the extent of opioid prescribing in the Medicare population. Similar declines between generalists and oncologists raise concern that access to cancer pain management may have been inadvertently restricted. How much of the decrease in prescribing by oncologists is appropriate vs inappropriate deserves further investigation.
Opioid analgesics remain a cornerstone of pain management for many patients, particularly those with cancer-related pain.1 The use of opioids is often necessary, but the rapid rise in opioid misuse, opioid use disorder, and opioid overdose deaths in the general population is a major public health concern and contributes to decreasing life expectancy in the United States.2 The Centers for Disease Control and Prevention (CDC) released its Guideline for Prescribing Opioids for Chronic Pain in March 2016 to minimize un-necessary opioid use, and many of its recommendations were subsequently adopted on the local, state, and national level.3 Although it excluded patients undergoing active cancer treatment, it did include patients with chronic pain as a result of cancer.4 Outpatient opioid prescribing has steadily decreased in recent years owing to the efforts of the CDC and other federal and state policies restricting prescription opioid use.5
As restrictions on opioid prescribing expand, oncologists have raised concern that these initiatives may have the unintended consequence of restricting access to legitimate opioid therapy for the management of cancer-related pain.6 The undertreatment of pain in patients with cancer is well described; up to one-third of these patients may have inadequate pain relief.7 Because of oncologists’ concerns with guideline discrepancies,8 the CDC issued a statement in 2019 clarifying that their guideline “is not intended to deny clinically appropriate opioid therapy to any patients who suffer acute or chronic pain from conditions such as cancer.”9
Little is known about how opioid prescription rates have differed between oncologists and generalist physicians during the opioid epidemic. Therefore, this study examines trends in opioid prescribing in the Medicare Part D population from 2013 to 2017 within both oncology and generalist specialties. We focus on the Medicare population because most cancer survivors and patients who receive a diagnosis of incident cancer are Medicare beneficiaries.10
Methods
We conducted a repeated cross-sectional study examining adjusted annual rates of opioid prescriptions among generalists and oncologists using the publicly available Medicare Part D Prescriber Public Use Files from 2013 to 2017, the only years available for analysis. Medicare Part D prescriber data include annual records of Part D–covered prescription fills aggregated at the prescription drug level for each prescriber across the United States. We included physicians with generalist specialties (internal medicine, family medicine, geriatric medicine, general practice) and oncology specialties (medical oncology, hematology-oncology, and radiation oncology). We excluded physicians who rarely prescribed Medicare Part D–covered medications, including those with fewer than 100 Part D–covered prescription fills in a year for fewer than 11 Medicare beneficiaries. We also excluded nurse practitioners and physician assistants because these pre- scribers work in both general and oncology settings and could not be assigned by specialty. Because this study used publicly available data, institutional review board approval and informed consent were waived by the University of North Carolina at Chapel Hill.
We used univariate statistics to describe the generalist and oncologist physician cohorts. For the primary analysis, we used physician-level Poisson regression to estimate adjusted rates of 2 opioid prescription outcomes: number of opioid prescriptions per 100 Medicare beneficiaries and number of long-acting opioid prescriptions per 100 Medicare beneficiaries.11 We stratified our regression models by physician specialty (generalist or oncologist) and adjusted for calendar year, physician sex, mean age of the physician’s Medicare Part D patient population, mean Centers for Medicare and Medicaid Services hierarchical condition category comorbidity risk score for that population, and state fixed effects.12 Poisson model estimates were used to determine annual adjusted predicted incidence rates of each opioid prescription outcome for generalists and oncologists as well as annual adjusted incidence rate ratios (aIRRs) for each outcome by calendar year (compared with 2013).
Results
We analyzed 251 820 generalists and 14 210 oncologists who contributed 978 932 and 58 509 physician-year observations, respectively (Table). On average, oncologists’ Medicare patient populations were more clinically complex than patients treated by generalists, with mean (SD) hierarchical condition category risk scores of 2.2 (0.6) vs 1.5 (0.6), respectively, in 2017 (P < .001). Nearly all generalists and oncologists prescribed at least 1 Medicare Part D–covered opioid analgesic in each year of the study period.
Table.
Characteristics of Medicare Part D Generalist and Oncologist Opioid Prescribers, 2013–2017
| Characteristic | Year | ||||
| 2013 (n = 199 544) | 2014 (n = 204 243) | 2015 (n = 207 857) | 2016 (n = 213 502) | 2017 (n = 212 295) | |
| Prescriber type, No. (% of total) | |||||
| Generalists | 188 343 (94) | 192 823 (94) | 196 180 (94) | 201 537 (94) | 200 049 (94) |
| Oncologists | 11 201 (6) | 11 420 (6) | 11 677 (6) | 11 965 (6) | 12 246 (6) |
| Female, No. (% within specialty) | |||||
| Generalists | 67 773 (36) | 71 045 (37) | 74 010 (38) | 77 704 (39) | 78 423 (39) |
| Oncologists | 3068 (27) | 3229 (28) | 3441 (29) | 3571 (30) | 3736 (31) |
| Medicare patient age, mean (SD) | |||||
| Generalists | 70.7 (4.9) | 70.8 (4.8) | 70.9 (4.7) | 71.1 (4.6) | 71.3 (4.5) |
| Oncologists | 71.3 (3.3) | 71.4 (3.2) | 71.4 (3.2) | 71.6 (3.1) | 71.8 (3.0) |
| Medicare patient risk score, mean (SD)a | |||||
| Generalists | 1.4 (0.5) | 1.4 (0.5) | 1.5 (0.6) | 1.5 (0.6) | 1.5 (0.6) |
| Oncologists | 2.0 (0.4) | 2.0 (0.5) | 2.1 (0.5) | 2.2 (0.5) | 2.2 (0.6) |
| Any opioid prescription, No. (% within specialty) | |||||
| Generalists | 184 364 (98) | 188 056 (98) | 189 809 (97) | 192 952 (96) | 189 753 (95) |
| Oncologists | 11 145 (99.5) | 11 347 (99) | 11 600 (99) | 11 835 (99) | 12 088 (99) |
| Any long-acting opioid prescription, No. (% within specialty) | |||||
| Generalists | 131 464 (70) | 131 206 (68) | 129 746 (66) | 125 977 (63) | 116 497 (58) |
| Oncologists | 10 526 (94) | 10 688 (94) | 10 876 (93) | 11 057 (92) | 11 052 (90) |
Generalist prescribers include family medicine, internal medicine, geriatric medicine, and general practice specialties. Oncologist prescribers include medical oncology, hematology-oncology, and radiation oncology specialties. Physicians included in this table wrote a minimum of 100 Medicare Part D–covered prescription fills for at least 10 Medicare Part D beneficiaries in a given calendar year. All bivariate comparisons between generalists and oncologists were statistically significant in each study year at P < .001 and with absolute standardized mean differences >0.10.
Risk scores reflect the complexity of a prescriber’s Medicare Part D patient population and are calculated using the Centers for Medicare and Medicaid Services hierarchical conditions categories. Risk scores account for patient age, sex, Medicare coverage type, and diagnoses from the previous year.
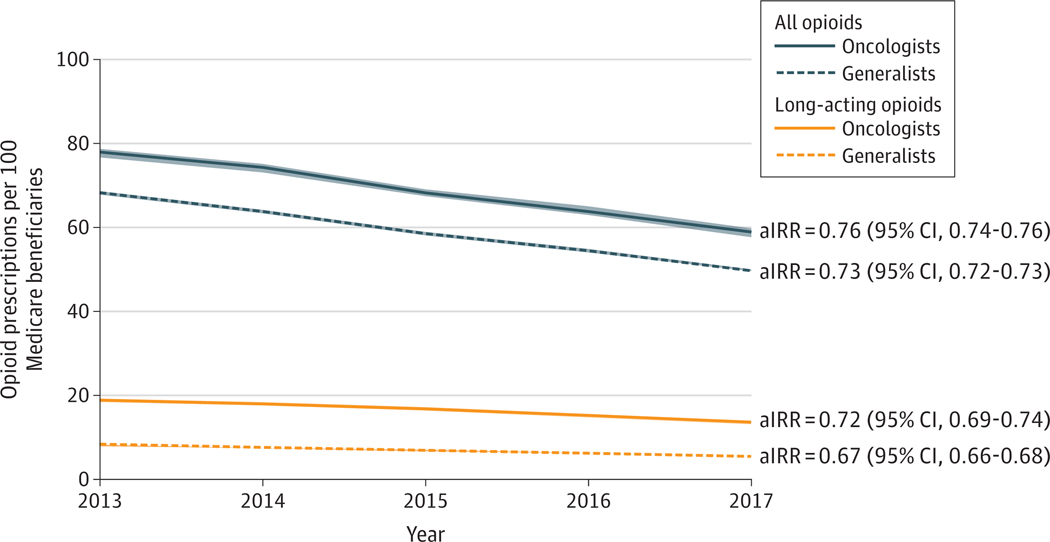
From 2013 to 2017, the annual adjusted predicted mean rate of opioid prescriptions per 100 Medicare beneficiaries (Figure; eTable in the Supplement) decreased from 68.2 to 49.7 among generalists (aIRR = 0.73; 95% CI, 0.73–0.73) and from 77.8 to 58.8 among oncologists (aIRR = 0.76; 95% CI, 0.74–0.77). The rate of long-acting opioid prescriptions per 100 Medicare beneficiaries also decreased from 8.0 to 5.4 for generalists (aIRR = 0.67; 95% CI, 0.66–0.68) and from 18.6 to 13.3 for oncologists (aIRR = 0.72; 95% CI, 0.69–0.74).
Figure. Annual Predicted Incidence Rates of Opioid Prescriptions per 100 Medicare Beneficiaries.
Analyses were estimated using Poisson regression with prescriber-level data, with SEs clustered for prescriber and adjusting for prescriber sex, mean patient age, mean risk score, and state fixed effects. The 95% CIs are represented as light-colored bands around each predicted rate line. Adjusted incidence rate ratios (aIRRs) reported for each specialty opioid category represent the relative change in adjusted incidence rate in 2017 compared with 2013. For all 4 categories, aIRRs were statistically significant at P < .001.
Discussion
This study of opioid prescribing patterns among generalists and oncologists for Medicare Part D beneficiaries during the opioid epidemic reveals several interesting findings. Among the data we analyzed from 251 820 generalists and 14 210 oncologists, we found large declines in Medicare Part D opioid prescription rates—similar to decreases seen nationally during this same period.13 Most striking were the similar relative decreases among generalists and oncologists in both total (27.1% and 24.4%, respectively) and long-acting (32.5% and 28.5%, respectively) opioid prescription rates per 100 Medicare beneficiaries from 2013 to 2017. We also found oncologists to have a higher rate of total and long-acting opioid prescriptions than generalists. More of the decrease in overall opioid prescription rates for generalists was attributed to fewer long-acting opioid prescriptions compared with oncologists. This differential behavior may reflect a recognition among generalists of the potential harm of long-acting opioid products in patients with noncancer pain.14
Although these data are unable to assess the clinical appropriateness of opioid therapy for individual patients, the similar relative decrease in opioid prescription rates between generalists and oncologists raises concern that access to legitimate opioid-based pain management for patients with cancer pain has been inadvertently restricted during the opioid epidemic. How much of this decline is due to physician reluctance to prescribe opioids or patient reluctance to use opioids for fear of addiction, vs difficulty prescribing opioids due to new restrictions, vs clinically appropriate reductions in opioid prescribing among patients with cancer deserves further investigation. In fact, 92% of oncology practices surveyed by the American Society for Clinical Oncology reported concern that restrictions on opioid prescribing would result in the undertreatment of cancer-related pain, and 40% had patients who had experienced trouble filling opioid prescriptions; the most commonly cited barriers included requirements for prior authorization, pill limits, and caps on maximum doses.15
Limitations
This study has some limitations. First, we do not know the clinical indications for these opioid prescriptions, and it is likely that some of the opioid prescriptions filled by generalists were for patients with cancer. Conversely, some prescriptions written by oncologists may have been for patients who were not undergoing active cancer treatment but who had not yet transitioned back to a generalist for medical management. We also lack data on how many prescriptions were written or consumed; our data include only prescriptions filled by Medicare beneficiaries. Additionally, we cannot judge the appropriateness of prescribing practices over time given the lack of clinical data. Subsequent investigations will be necessary to see how prescribing patterns change following the 2019 CDC clarification.9
Conclusions
In conclusion, we found that opioid prescribing in the Medicare population decreased as the policy and advocacy response to the opioid crisis amplified from 2013 to 2017. However, similar declines among generalists and oncologists raise concern that access to legitimate opioid-based cancer pain management may have been inadvertently restricted. The ex- tent to which these decreases among Medicare beneficiaries treated by oncologists are appropriate vs inappropriate deserves further investigation.
Supplementary Material
Key Points.
Question How have opioid prescribing patterns for Medicare patients changed during the opioid epidemic among generalists and oncologists?
Findings In this cross-sectional study of the prescribing patterns of 251 820 generalists and 14 210 oncologists, analyzing Medicare Part D prescriber files, the annual adjusted mean rate of opioid prescriptions per 100 Medicare beneficiaries decreased from 68.2 to 49.7 among generalists (adjusted incidence rate ratio = 0.73) and from 77.8 to 58.8 among oncologists (adjusted incidence rate ratio = 0.76) between 2013 and 2017.
Meaning Oncologists and generalists had similar trends in decreasing opioid prescription rates, raising concern that access to appropriate opioid-based cancer pain management may be inadvertently restricted during the opioid epidemic.
Acknowledgments
Meeting Presentation: This article was presented during the 2020 ASCO Virtual Scientific Program; May 29–31, 2020.
Footnotes
Conflict of Interest Disclosures: Dr Roberts is supported by grant KL2TR002367 from the National Center for Advancing Translational Science. Dr Royce is supported by grant K12CA120780 from the UNC Oncology Clinical Translational Research Training Program. No other disclosures are reported.
Contributor Information
Ankit Agarwal, Department of Radiation Oncology, University of North Carolina at Chapel Hill.
Andrew Roberts, Department of Population Health, University of Kansas Medical Center, Kansas City; Department of Anesthesiology, University of Kansas Medical Center, Kansas City.
Stacie B. Dusetzina, Department of Health Policy, Vanderbilt University School of Medicine, Nashville, Tennessee.
Trevor J. Royce, Department of Radiation Oncology, University of North Carolina at Chapel Hill.
REFERENCES
- 1.Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol. 2014;32(16):1739–1747. doi: 10.1200/JCO.2013.52.4629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dowell D, Haegerich T, Chou R. No shortcuts to safer opioid prescribing. N Engl J Med. 2019;380 (24):2285–2287. doi: 10.1056/NEJMp1904190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroenke K, Alford DP, Argoff C, et al. Challenges with implementing the Centers for Disease Control and Prevention opioid guideline: a consensus panel report. Pain Med. 2019;20(4):724–735. doi: 10.1093/pm/pny307 [DOI] [PubMed] [Google Scholar]
- 5.Bohnert ASB, Guy GP Jr, Losby JL. Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention’s 2016 opioid guideline. Ann Intern Med. 2018;169 (6):367–375. doi: 10.7326/M18-1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ASCO. ASCO policy statement on opioid therapy: protecting access to treatment for cancer-related pain. May 2016. Accessed May 11, 2020 https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2016-ASCO-Policy-Statement-Opioid-Therapy.pdf.
- 7.Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–4154. doi: 10.1200/JCO.2014.56.0383 [DOI] [PubMed] [Google Scholar]
- 8.Meghani SH, Vapiwala N. Bridging the critical divide in pain management guidelines from the CDC, NCCN, and ASCO for cancer survivors. JAMA Oncol. 2018;4(10):1323–1324. doi: 10.1001/jamaoncol.2018.1574 [DOI] [PubMed] [Google Scholar]
- 9.Post TA. CDC issues clarification on guideline for prescribing opioids for chronic pain in patients with cancer and sickle cell disease. April 9, 2019. Accessed May 11, 2020 https://www.ascopost.com/News/59920. [Google Scholar]
- 10.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1029–1036. doi: 10.1158/1055-9965.EPI-16-0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. Risk adjustment. July 2018. Accessed May 11, 2020 https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors.
- 13.Centers for Disease Control and Prevention. US opioid prescribing rate maps. March 5, 2020. Accessed May 11, 2020 https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html.
- 14.Klimas J, Gorfinkel L, Fairbairn N, et al. Strategies to identify patient risks of prescription opioid addiction when initiating opioids for pain: a systematic review. JAMA Netw Open. 2019;2(5): e193365. doi: 10.1001/jamanetworkopen.2019.3365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Society of Clinical Oncology. The state of cancer care in America, 2017: a report by the American Society of Clinical Oncology. J Oncol Pract. 2017;13(4):e353–e394. doi: 10.1200/JOP.2016.020743 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.