Abstract
The association of different antihypertensive regimens with blood pressure (BP) control is not well-described among community-dwelling older adults with low comorbidity. We examined antihypertensive use and BP control in 10,062 treated hypertensives from Australia and the United States (U.S.) using baseline data from the ASPirin in Reducing Events in the Elderly (ASPREE) trial. Renin-angiotensin system (RAS) drugs were the most prevalently used antihypertensive in both countries (Australia: 81.7% of all regimens; U.S.: 62.9% of all regimens; P<0.001). Diuretics were the next most commonly used antihypertensive in both countries, but were more often included in regimens of U.S. participants (48.9%, vs. 33.3% of regimens in Australia; P<0.001). Among all antihypertensive classes and possible combinations, monotherapy with a RAS drug was the most common regimen in both countries, but with higher prevalence in Australian than U.S. participants (35.9% vs 20.9%; P<0.001). For both monotherapy and combination users, BP control rates across age, ethnicity, and sex were consistently lower in Australian than U.S. participants. After adjustment for age, sex, ethnicity, and BMI, significantly lower BP control rates remained in Australian compared to U.S. participants for the most commonly used classes and regimens (RAS blocker monotherapy: BP control=45.5% vs 54.2%; P=0.002; diuretic monotherapy: BP control=45.2% vs 64.5%; P=0.001; RAS blocker/diuretic combo: BP control=50.2% vs 65.6%; P=0.001). Our findings highlight variation in antihypertensive use in older adults treated for hypertension, with implications for BP control. Differences in BP control that were observed may be influenced, in part, by reasons other than choice of specific regimens.
Keywords: antihypertensive therapy, hypertension in older adults, blood pressure control
Introduction
Elevated blood pressure is common with aging and is an important modifiable risk factor for cardiovascular disease and stroke. High income countries such as the United States (U.S.) and Australia have rapidly growing geriatric populations, with adults aged 65 years and older accounting for approximately 15% of the total population in both countries.1,1 An estimated 60% or more of individuals older than 60 years of age have hypertension, with nearly half of those having controlled blood pressure.2–4 After publication of the 2017 ACC/AHA Hypertension Guideline, it is now estimated that 82% of US adults aged ≥75 years have uncontrolled blood pressure.5,6
The high prevalence of hypertension and its associated sequelae heightens the importance of identifying the most effective antihypertensives to control blood pressure in older adults without cardiovascular disease, as one means to help prolong their disability-free survival. Benchmarking of this type can assist clinicians in choosing antihypertensives most suitable at lowering cardiovascular events in older adults, and inform population-based health strategies to optimize treatment success. In this analysis we sought to characterize antihypertensive medication use and associated blood pressure control in a generalizable cohort of older adults from Australia and the U.S. who were enrolled in the ASPirin in Reducing Events in the Elderly (ASPREE) trial.7,8 Data from ASPREE provide an opportunity to compare hypertension treatment approaches and their effects on blood pressure control in nationally-representative samples of community-dwelling elderly with few comorbidities and preserved autonomy.
Methods
This cross-sectional analysis used baseline data from the ASPREE trial, a randomized, placebo-controlled study of daily low-dose aspirin to prolong disability-free survival in 19,114 healthy adults aged 70 and older in Australia and the U.S. (aged 65 and older for U.S. minorities). To be eligible for ASPREE, individuals had to be free of documented evidence of significant illness, including cardiovascular disease, dementia, or significant physical disability, and expected to live for at least another 5 years. Participants were recruited in the U.S. from academic and community medical centers and health systems, and in Australia from community-based general practice providers. Further details of the ASPREE study and main results have been extensively reported.9–11
All participants enrolled into the trial completed two baseline visits to finalize eligibility prior to randomization to 100 mg aspirin or placebo. At these visits, participants were asked about medical diagnoses and assessed for cognition, physical function, lifestyle, anthropometric measures, concomitant prescription medications, and other clinical parameters. Prescription medications were obtained via self-report with participants asked to present at the baseline visit with a list of all regularly-used medications and/or the medication bottles themselves.
Blood pressure for each participant was measured prior to randomization to aspirin or placebo at the first baseline visit by trained study staff. Blood pressure was measured according to standard operating procedures, in the seated position after at least 5 minutes of rest using an automated oscillometric device with an occluding cuff of appropriate size for the upper arm circumference. Since it was not designed as a blood pressure study, the ASPREE protocol did not require the specific model, only that it had to be a validated oscillometric device (OMRON HEM-7203, 7121, and 7130 models were exclusively used in Australia; in the U.S., any validated oscillometric device available to study staff could be used). Readings could be attended or unattended at the discretion of the study staff and based on the capabilities of the specific device used. Three separate and consecutive blood pressure readings one minute apart were recorded at the first visit and the average of all three measurements for each participant was used as the baseline blood pressure. Of the entire enrolled ASPREE cohort, 73.2% (14,213/19,114) had hypertension at baseline, defined as a either an average blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic, or taking at least one antihypertensive medication (regardless of blood pressure value), or both.12 The focus of this analysis is those hypertensive individuals who were receiving at least one antihypertensive agent (n=10,062), irrespective of their baseline blood pressure.
We categorized the antihypertensive drugs prescribed according to monotherapy, or combination therapies with two or more antihypertensives. Specific antihypertensive agents were classified as described previously, and according to the World Health Organization (WHO) Anatomical Therapeutic Chemical (ATC) Classification System [i.e., diuretics (C03), beta blocking agents (C07), calcium channel blockers (C08), agents acting on the renin-angiotensin system (C09), or other antihypertensives not included in these classes].13 This classification system includes up to five levels according to organ system and their therapeutic, pharmacological, and chemical properties.
The frequency of use of specific classes and regimens of antihypertensives was examined across the cohort, both as a total of all antihypertensives and regimens in the cohort (i.e. expressed as a percentage of a denominator of 100%), as well as within the specific categories of mono and combination therapies. Blood pressure was considered controlled if the participant was treated with antihypertensive medication(s) and with systolic blood pressure <140 mmHg and diastolic blood pressure <90 mmHg. We chose this threshold to define controlled blood pressure as it was the traditionally accepted blood pressure target for most adults at the time the baseline data were collected.
Data were analyzed using the statistical software Stata version 15.2. Descriptive statistics were used to present the antihypertensive drug prescription pattern and summarize hypertension control rates. Student t-test, ANOVA or Chi square tests were used to compare the distributions of baseline characteristics between subgroups of participants based on medication use (mono or combination therapy). Comparative analyses between Australian and U.S. participants for specific antihypertensive class/regimen and corresponding blood pressure control were conducted using logistic regression adjusting for key demographic characteristics (e.g., age, sex, BMI, race) which can influence choice of, and response to, specific antihypertensives. P-values less than 0.05 were considered significant.
Results
Demographics of Treated Hypertensive Participants
Overall, 14,213 of ASPREE’s 19,114 participants met criteria for hypertension at the baseline visit, and 70.8% (10,062/14,213) were receiving at least one antihypertensive agent. The baseline characteristics of the hypertensive participants taking at least one antihypertensive are summarized by country in Table 1. The proportion of Australian participants taking monotherapy or two or more antihypertensive agents was equally divided (50.7% and 49.3%, respectively). In contrast, the majority of U.S. participants used two or more antihypertensives (44.4% monotherapy, 55.7% two or more antihypertensive agents; P<0.001 for comparison of U.S. vs Australia for both monotherapy and two or more). Among those individuals treated with any antihypertensive at baseline (either monotherapy or in combination), 47% (4,732/10,062) had controlled blood pressure at enrollment, with a higher proportion of U.S. participants having controlled BP (US: 57%; AUS: 46%; P<0.001).
Table 1:
Characteristics of the hypertensive participants in ASPREE taking at least one antihypertensive.
| Overall N=10,062 | Australia N=8,748 | U.S. N=1,314 | ||||
|---|---|---|---|---|---|---|
| Variables | Monotherapy N=5,019 (49.9%) |
Combination (2+) N=5,043 (50.1%) |
Monotherapy N=4,435 (50.7%) |
Combination (2+) N=4,313 (49.3%) |
Monotherapy N=584 (44.4%) |
Combination (2+) N=730 (55.7%) |
| Age (years) | 74.9±4.7 | 74.9±4.7 | 75.1±4.5b | 75.2±4.5b | 73.2±5.6 | 73.1±5.7 |
| Male (%) | 41.7 | 39.6a | 42.5b | 41.4b | 35.3 | 28.9a |
| Race (%) | ||||||
| White/Caucasian | 91.1 | 88.3 | 97.9b | 97.8b | 39.0 | 32.3a |
| Black/African American | 4.5 | 7.6 | 0.02b | 0.02b | 38.2 | 52.6 |
| Hispanic | 3.0 | 2.5 | 0.7b | 0.7b | 20.4 | 13.4 |
| Asian | 0.8 | 1.0 | 0.7b | 1.0 | 1.7 | 1.0 |
| Other | 0.7 | 0.6 | 0.7 | 0.5 | 0.7 | 0.7 |
| Body Mass Index (kg/m2, mean±SD) | 28.4±4.8 | 29.7±5.1a | 28.4±4.5b | 29.6±5.0a,b | 29.08±5.4 | 30.6±5.8a |
| Obese (BMI≥30 kg/m2) | 32.5 | 43.3a | 31.9b | 42.3a,b | 36.8 | 49.1a |
| Estimated GFR (mg/dl, mean±SD) | 71.9±14.4 | 70.1±15.8a | 71.5±14.0b | 69.8±15.3a,b | 74.7±16.4 | 71.9±18.3a |
| In past 2 weeks any walk outside the home? (%) | 95.4 | 93.5a | 95.8b | 94.3a,b | 92.1 | 88.9a |
| Any difficulty in walking a distance of 1 mile/1.6 km (%) | 22.2 | 28.0a | 22.1 | 27.4a,b | 22.7 | 31.3a |
| Family History of CVD (%) | 61.8 | 65.1a | 62.4b | 65.8a,b | 57.5 | 61.1 |
| Medication history (%) | ||||||
| Lipid lowering medication | 40.3 | 46.6a | 39.3b | 45.7a,b | 48.3 | 51.9 |
| Previous regular aspirin | 11.2 | 14.5a | 7.7b | 9.7a,b | 37.3 | 42.7a |
| Number of Antihypertensives (%)c | a | a | a | |||
| One | 100.0 | - | 100.0 | - | 100.0 | - |
| Two | - | 69.8 | - | 70.5b | - | 65.7 |
| Three or more | - | 30.2 | - | 29.5b | - | 34.3 |
| Comorbidities (%) | ||||||
| Hypercholesterolemia | 68.5 | 69.6 | 70.2b | 71.6b | 55.8 | 58.0 |
| Diabetes | 10.1 | 14.7a | 9.0b | 12.8a,b | 18.2 | 25.8a |
| Depression | 15.1 | 14.7 | 15.6b | 15.0 | 10.8 | 13.2 |
| BP controlled <140/90 mmHg | 45.7 | 48.4a | 44.2b | 46.9a,b | 56.5 | 57.4 |
Significant differences (P<0.05) observed between participants using mono and two or more combination therapy
Significant differences (P<0.05) observed between Australian and U.S. participants
Data in the column represent the percent distribution within that column, of the total number listed in the column heading
In the U.S., hypertensive participants taking two or more antihypertensives compared to those taking monotherapy were more likely to be female and black, while in both countries combination users were more likely to be obese, have lower eGFR, more difficulty walking, and more likely to have a family history of cardiovascular disease. They were also more likely to report taking lipid-lowering medication, previous regular use of aspirin, and diabetes. We did not observe a significant difference in blood pressure control among U.S. participants receiving monotherapy compared to those taking two or more antihypertensive medications (57.4% vs. 56.5%); however, Australian participants receiving two or more antihypertensives had significantly better control rates than those on monotherapy (46.9% vs 44.2%, P=0.01).
Figure 1 shows the overall distribution of antihypertensive use (mono, and two or more) and corresponding blood pressure control by age, sex, and race subgroups for U.S. and Australian-treated hypertensive participants. Monotherapy was more commonly used among Australian than U.S. participants, with significant differences in females and those aged 75–79 years. A significantly lower blood pressure control was observed in Australians compared to U.S. participants in several subgroups, including both sexes, and in whites, and irrespective of use of mono or combination antihypertensive therapies. Among different age strata, lower blood pressure control was observed in Australian participants aged ‘70–74’ and ‘75–79’ years compared to those U.S. participants on monotherapy in the same age group, and among participants aged ‘70–74’ years on two or more antihypertensives.
Figure 1:
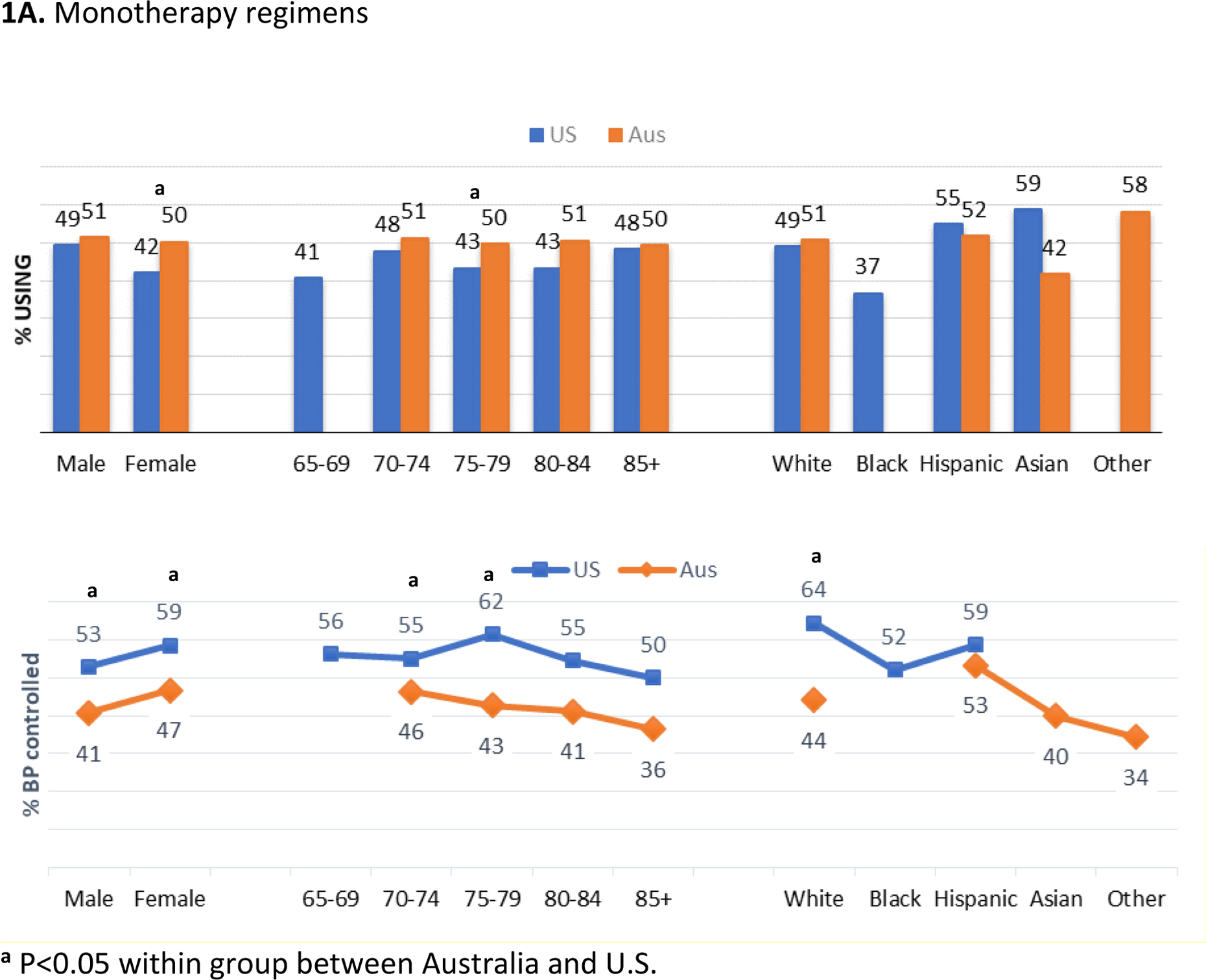
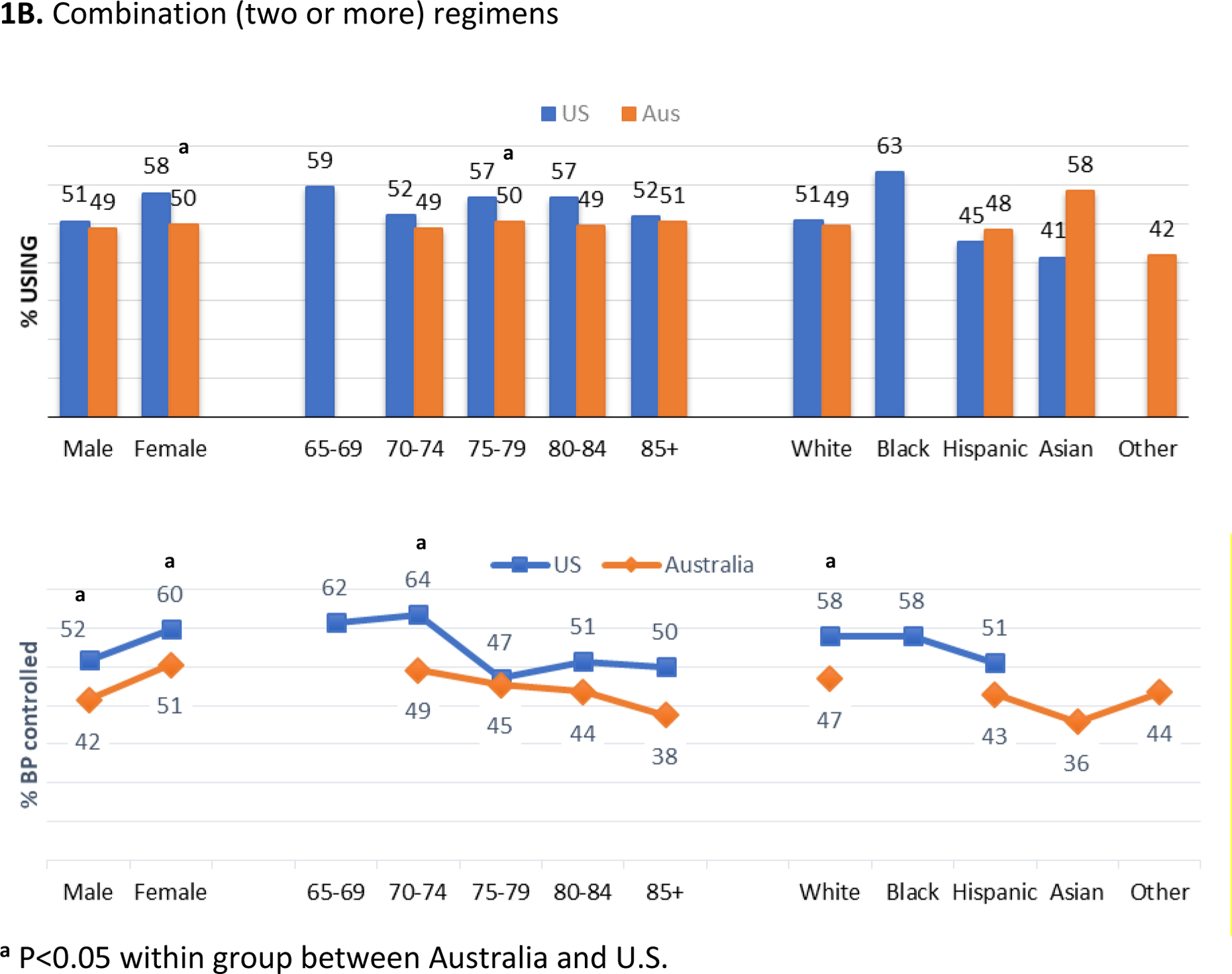
Use of antihypertensive drugs and associated blood pressure control by sex, age, and race among treated hypertensive participants by country (Note: groups with N <10 ignored)
Overall Frequency of All Antihypertensive Classes Used and Blood Pressure Control
When examining use of antihypertensives classes across all regimens, a renin-angiotensin-system (RAS) drug was most commonly employed (79.3%), followed by diuretic (35.4%), calcium channel blocker (CCB) (32.8%) and beta-blocker (15.4%). There was higher use of a RAS drug among Australians compared to U.S. participants (81.7% vs 62.9%; P<0.001), but lower use of diuretics (33.3% vs 48.9%; P<0.001), CCBs (32.5% vs 35.2%; P=0.02), and beta-blockers (13.6% vs 27.6%; P<0.001) (Figure 2a). After adjustment for age, sex, BMI, and race, blood pressure control rates were significantly higher in U.S. participants compared to Australian participants for regimens containing a RAS drug (56.4% vs 46.4%; P=0.001), diuretic (60.3% vs 47.8%; P<0.001), or beta-blocker (55.5% vs 45.7%; P=0.001) but similar for regimens with a CCB (54.6% vs 43.8%; P=0.12) (Figure 2b).
Figure 2:
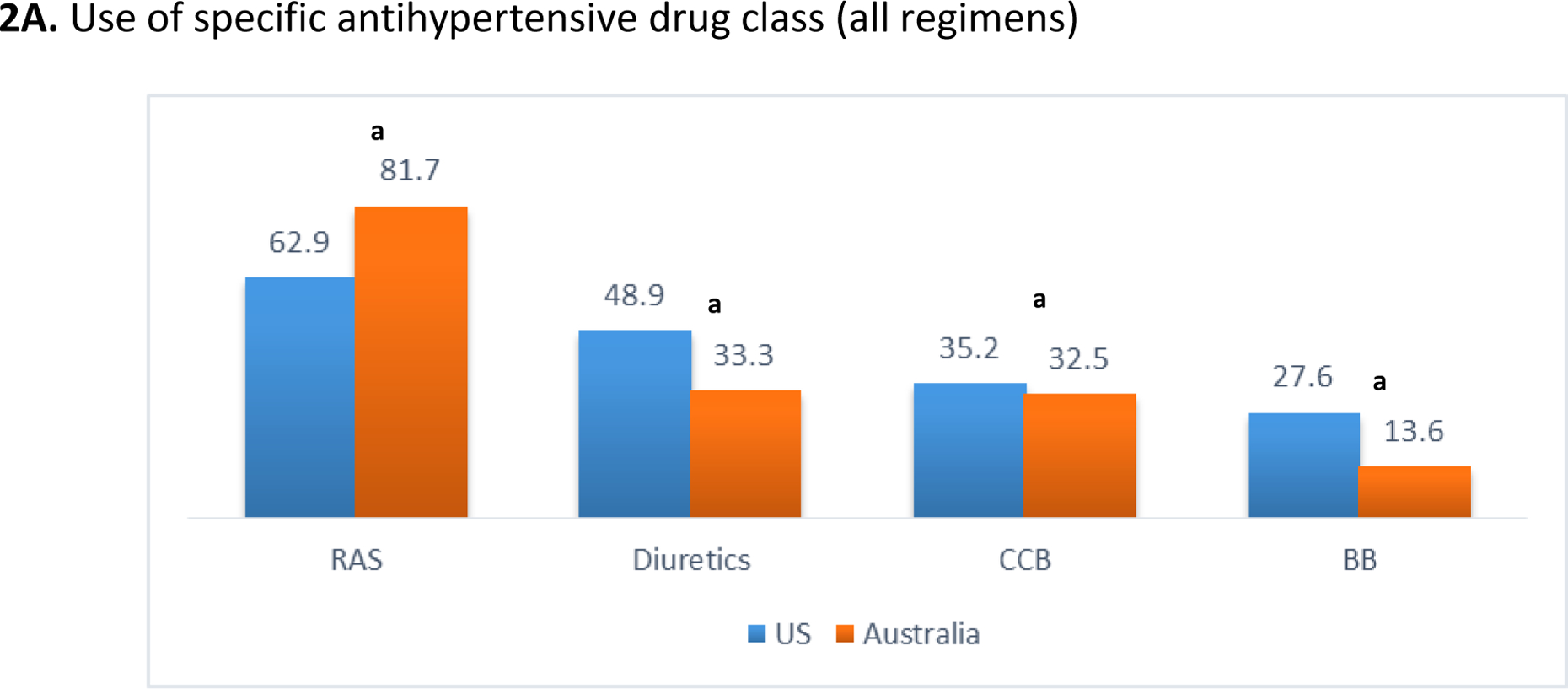
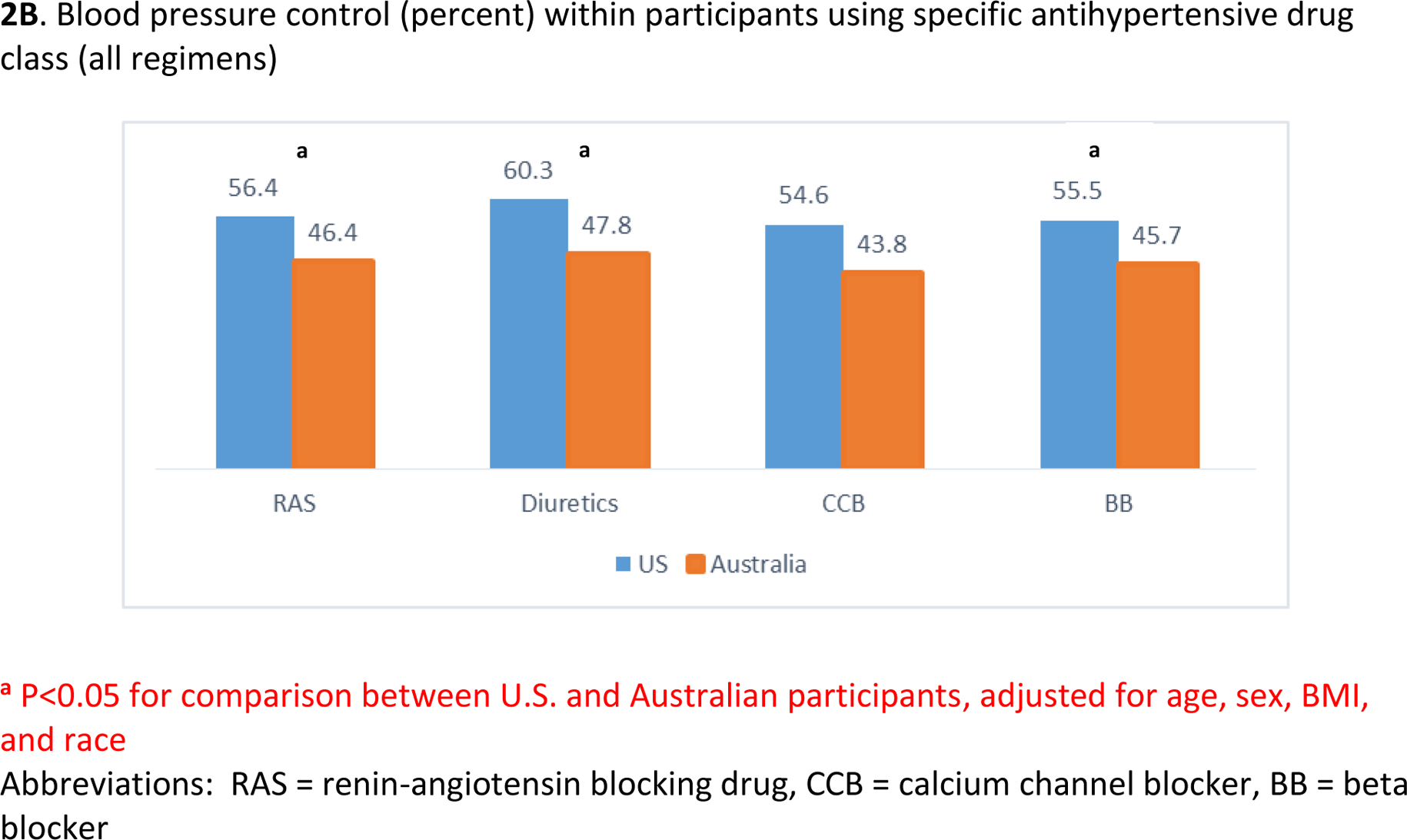
Distribution (percent) of specific antihypertensive drug classes (irrespective of mono or combination therapy), and corresponding blood pressure control rates by country
Among those individuals receiving monotherapy, a RAS drug was the most common in both countries; however, the percentage of those on monotherapy who received a RAS drug was much higher in Australian participants compared to U.S. participants (70.8% vs 47.1%; P<0.001) (Supplemental Appendix Table 1). This was also true for combination regimens, with RAS drugs more common in Australia than the U.S. (93.0% vs 75.6%; P<0.001). We found that the type of RAS drug used (irrespective of mono or combination therapy) differed by country – 62.8% of RAS drugs used by the Australian participants were angiotensin II receptor blockers (ARBs) (vs 36.8% in U.S.; P<0.001), while angiotensin converting enzyme (ACE) inhibitors accounted for 62.9% of the RAS drugs used by U.S. participants (vs 37.2% in Australians; P<0.001) (Supplemental Appendix Table 2). Of the monotherapies used other than a RAS drug, diuretics and beta blockers were more common in U.S. participants compared to Australian participants (diuretics: 21.2% vs 7.5%; P<0.001; beta blockers: 12.8% vs 6.7%; P<0.001), while use of CCBs were similar (16.8% vs 12.0%; P=0.35). A similar pattern of difference was observed for combination therapies, with the exception of CCBs, which also differed significantly between both countries. After controlling for age, sex, race, and BMI, breakdown by the different monotherapies or two or more antihypertensive combination therapies also showed a significant difference in blood pressure control favoring U.S. vs Australian-treated hypertensive participants with all classes except for those using beta blocker or CCB monotherapy, or CCB combination therapy (Supplemental Appendix Table 1).
Further investigation of the diuretic class revealed notable differences across the countries (Supplemental Appendix Table 2). Of the total proportion of all diuretics used, there was higher use of high-ceiling (i.e., loop) diuretics in the Australian participants compared to U.S. participants (9.3% vs 7.5%; P<0.001); whereas, there was much higher use of potassium-sparing agents (which included spironolactone) in the U.S. group (14.6% vs 4.2%; P<0.001). Low-ceiling diuretics, excluding thiazides (ATC code CO3B), the most common of which is indapamide, were more commonly used in Australian than U.S. participants (27.0% vs 6.8%; P<0.001). Finally, there was greater use of two diuretics in U.S. participants, compared to Australians (14.5% vs 6.1%; P<0.001).
Use of Specific Antihypertensive Classes within Monotherapy or Combination Therapy Regimens and Associated Blood Pressure Control Rates
Table 2 shows the frequency distribution of all antihypertensive drug classes and regimens, categorized by monotherapy and combinations, utilized in the cohort. A RAS drug used as a single antihypertensive agent was the most common regimen, followed by ‘RAS plus a diuretic’ combination, in both U.S. and Australia. The RAS monotherapy was more frequently used in Australia compared to U.S. (35.9% versus 20.9%, P<0.001). After RAS monotherapy, the regimen used most commonly as a single agent were diuretics (9.4%) in the U.S., whereas it was CCB (6.1%) in Australia. In treated hypertensives taking more than one antihypertensive, the most common combination after ‘RAS plus diuretic’ was an ‘RAS plus CCB’ in both U.S. and Australia. Although there were no differences in frequency of the most common 3 drug regimen (RAS + diuretic + CCB) in both countries (6.0% vs 6.9%), the use of 3 or more antihypertensive in combination was slightly higher overall in U.S. participants than Australian participants (19% vs 14.6%; P<0.001).
Table 2:
Distribution of treated hypertensive participants by antihypertensive drug use as monotherapy, or as a specific combination (two, three or more) and associated control rates. Note, percentages are reported as a total of all antihypertensive regimens utilized in the cohort.
| Medication | Australia (N=8748) | US (N=1314) | P-valuea | |||
|---|---|---|---|---|---|---|
| % usage (n) | % Controlled (95% CI) | % usage (n) | % Controlled (95% CI) | usage | control | |
| Monotherapy | ||||||
| RAS | 35.9 (3139) | 45.5 (43.7–47.2) | 20.9 (275) | 54.2 (48.3–60.1) | <0.001 | 0.002 |
| DU | 3.8 (332) | 45.2 (39.8–50.5) | 9.4 (124) | 64.5 (56.1–72.9) | <0.001 | 0.001 |
| CCB | 6.1 (533) | 34.9(30.8–38.9) | 7.5 (98) | 57.1 (47.3–66.9) | 0.292 | 0.107 |
| BB | 3.4 (295) | 46.8 (41.1–52.3) | 5.7 (75) | 52.0 (40.7–63.3) | <0.001 | 0.057 |
| Other mono therapy | 1.6 (136) | 44.1 (35.8–52.5) | 0.9 (12) | 50.0 (21.7–78.3) | 0.369 | 0.169 |
| Two drug combination | ||||||
| RAS+ DU | 15.6 (1368) | 50.2 (47.5–52.8) | 13.9 (183) | 65.6 (58.7–72.5) | 0.131 | 0.001 |
| RAS+CCB | 12.3 (1072) | 46.2 (43.2–49.2) | 7.3 (96) | 49.0 (39.0–59.0) | 0.004 | 0.514 |
| RAS+BB | 2.8 (242) | 40.9 (34.7–47.1) | 3.2 (42) | 52.4 (37.3–67.5) | 0.102 | 0.069 |
| DU +BB | 0.7 (60) | 50.0 (37.3–62.7) | 4.6 (60) | 65.0 (52.9–77.1) | <0.001 | 0.338 |
| Other 2 combinations | 3.4 (297) | 42.8 (37.1–48.4) | 7.5 (99) | 54.6 (44.7–64.4) | <0.001 | 0.379 |
| Three or more drug combination | ||||||
| RAS +DU +CCB | 6.9 (601) | 45.3 (41.3–49.2) | 6.0 (79) | 58.2 (47.4–69.1) | 0.023 | 0.52 |
| RAS+ DU +BB | 1.8 (156) | 49.4 (41.5–57.2) | 4.3 (57) | 59.7 (46.9–72.4) | <0.001 | 0.966 |
| Other ≥3 combinations | 5.9 (517) | 45.5 (41.2–49.7) | 8.7 (114) | 50.0 (40.8–59.2) | 0.375 | 0.144 |
Abbreviations: RAS = renin-angiotensin blocking drug, DU = diuretic, CCB = calcium channel blocker, BB = beta blocker
P-value for comparison between U.S. and Australian participants adjusted for age, sex, BMI, and race
After adjustment for age, sex, ethnicity, and BMI, significantly lower BP control rates remained in Australian compared to U.S. participants (Table 2) for the most commonly used classes and regimens (RAS blocker monotherapy: BP control=45.5% vs 54.2%; P=0.002; diuretic monotherapy: BP control=45.2% vs 64.5%; P=0.001; RAS blocker/diuretic combo: BP control=50.2% vs 65.6%; P=0.001).
Discussion
Hypertension, defined by blood pressure and/or use of antihypertensive medication, was highly prevalent among Australian and U.S. participants enrolled in the ASPREE trial. Although individuals were recruited into ASPREE on the basis of being otherwise healthy and free of documented cardiovascular disease, the high prevalence of hypertension is consistent with observations in the general population in the age group enrolled.6,14 Less than half of participants had blood pressure that was controlled according to the threshold of <140/90 mmHg.
Examination of patterns of antihypertensive use across the cohort revealed similarities and differences across countries. For example, the use of RAS drugs was common in participants of both countries, although overall monotherapy (and specifically monotherapy with a RAS drug) was more common in Australian participants. Diuretics, either as a monotherapy or in combination, were utilized more frequently in U.S. participants.
The differences in antihypertensive use could stem from the influence of previous research studies conducted within the two countries and the demographics of the enrolled cohort. In Australia, the Second Australian National Blood Pressure Study (ANBP-2), which recruited mostly white participants from community general practice providers similar to ASPREE, found a lower rate of cardiovascular events or death from any cause in those randomized to an angiotensin converting enzyme inhibitor compared to diuretic.15 In the U.S., significantly more minorities were enrolled into ASPREE, and diuretics figured prominently in U.S.-based hypertension trials which included large numbers of minorities such as the Antihypertensive and Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT) and the Action to Control Cardiovascular Risk in Diabetes (ACCORD).16,17 Examination of diuretic use in more detail (Supplemental Appendix Table 2) suggests the possibility of more intensive diuretic regimens occurring in U.S. participants.
An additional explanation for prescribing differences may be attributed to adherence to hypertension guidelines at the time of recruitment into ASPREE. Australian blood pressure guidelines during that period specified initial monotherapy and then addition of a second agent, while combination therapies were subject to restricted use indications under the Australian Pharmaceutical Benefits Scheme.18 Previous research conducted during this time period has shown that more than half of antihypertensive prescriptions initiated in Australia conformed to Australian guidelines.19 In contrast, U.S. guidelines have more liberally promoted initial combination therapy.20,21
The differences we observed in use of antihypertensive classes and regimens may have contributed to differences observed in blood pressure control rates in our cohort, which were slightly lower in Australian compared to U.S. participants across subgroupings of age, sex, and race (Figure 1), and in both monotherapy and combination therapy groups. This occurred despite higher rates of obesity, diabetes, and smoking in U.S. participants, as previously reported,8 which should have made it more difficult to control blood pressure in this group. It is possible that dose intensity of regimens may have been different across participants of both countries, but unfortunately, we lack detailed information to explore that hypothesis. Similarly, the significantly higher use of ARBs in Australian participants, which have dose-response effects that are less pronounced than ACE inhibitors and CCBs,22,23 could have led to lower rates of blood pressure control if mostly initial doses were used. Further evidence supporting this is that we did not observe any differences in blood pressure control between participants from the U.S. and Australia who used CCBs. Finally, we think it is unlikely that measurement differences between the two countries existed as standard operating procedures were followed, sites were regularly monitored, and there were no differences in the mean blood pressures of hypertensive participants from both countries who were not receiving antihypertensive medication (data not shown).
The strengths of our study include the large size of the cohort and although not designed as a blood pressure study, repeated standardized blood pressure measurements using automatic oscillometric devices were performed according to standard operating procedures. Both the U.S. and Australia share similar blood pressure profiles within the community;24 since ASPREE enrolled a sample of older, generally healthy adults with access to healthcare, it is likely that our findings are highly generalizable and reflective of the broader healthy community-dwelling elderly hypertensive populations in both countries.
Our findings must be interpreted within the context of important limitations; namely, the cross-sectional nature of the analysis. We lack data on dose, so it is not known whether the lower control rates in Australian participants compared to the U.S. can be attributed to differences in dosing intensity. Adherence with antihypertensives could be different between the groups, although there was no indication of this within the main ASPREE study based on adherence to the aspirin/placebo intervention. Although the average of three blood pressure measurements in one sitting were used, they are nonetheless from only one visit, albeit using standard operating procedures which incorporated appropriately recommended technique. Variability within the blood pressure machines could be a factor since we did not use the same machines across all sites; however, all machines were inspected and validated regularly. Finally, medications were self-reported or retrieved through the medical record when possible, which allows the possibility of ascertainment bias in the completeness of the prescription record.
Conclusions
Our findings highlight variation in antihypertensive use in older adults treated for hypertension, with implications for blood pressure control. In the nationally representative ASPREE study cohort, differences were observed in the use of monotherapy and in specific medication classes, between participants of both countries, with higher frequencies of RAS drug use and monotherapy regimens and less diuretic use in Australians compared to U.S. participants. Even after adjustment for covariates affecting choice of, and response to antihypertensives, significantly lower blood pressure control rates remained in Australian compared to U.S. participants for the most commonly used classes and regimens. Differences in observed BP control may be partly influenced by reasons additional to the choice of specific regimen.
Supplementary Material
Funding:
This work was supported by the National Institute on Aging and the National Cancer Institute at the National Institutes of Health (grant number U01AG029824); the National Health and Medical Research Council (grant numbers 334037 and 1127060); Monash University (Australia); and the Victorian Cancer Agency (Australia).
Footnotes
International Standard Randomized Controlled Trial Number Register (ISRCTN83772183) and clinicaltrials.gov (NCT01038583).
Disclosure: A. G. Bayer provided aspirin and matching placebo.
References
- 1.Australian Institute of Health and Welfare. Older Australia at a glance. 2018. https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/contents/demographics-of-older-australians/australia-s-changing-age-and-gender-profile Accessed February 20, 2020.
- 2.United States Census Bureau. Facts for Features: Older Americans Month: May 2017. https://www.census.gov/newsroom/facts-for-features/2017/cb17-ff08.html Accessed February 20, 2020.
- 3.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–968. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension 2017;70:736–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet 2019;394:639–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khera R, Lu Y, Lu J, Saxena A, Nasir K, Jiang L, Krumholz HM. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ 2018;362:k2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, Whelton PK. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation 2018;137:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson MR, ASPREE Investigator Group. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials 2013;36:555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNeil JJ, Woods RL, Nelson MR, Murray AM, Reid CM, Kirpach B, Storey E, Shah RC, Wolfe RS, Tonkin AM, Newman AB, Williamson JD, Lockery JE, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Trevaks RE, Orchard SG, Beilin LJ, Donnan GA, Gibbs P, Johnston CI, Grimm RH, on behalf of the ASPREE Investigator Group. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J Gerontol A Biol Sci Med Sci 2017;72:1586–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, Storey E, Shah RC, Lockery JE, Tonkin AM, Newman AB, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Donnan GA, Gibbs P, Johnston CI, Ryan J, Radziszewska B, Grimm R, Murray AM, for the ASPREE Investigator Group. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med 2018;379:1499–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, Reid CM, Lockery JE, Kirpach B, Shah RC, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Johnston CI, Ryan J, Radziszewska B, Jelinek M, Malik M, Eaton CB, Brauer D, Cloud G, Wood EM, Mahady SE, Satterfield S, Grimm R, Murray AM, for the ASPREE Investigator Group. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 2018;379:1509–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, Kirpach B, Shah RC, Ives DG, Storey E, Ryan J, Tonkin AM, Newman AB, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Donnan GA, Gibbs P, Johnston CI, Radziszewska B, Grimm R, Murray AM, for the ASPREE Investigator Group. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med 2018;379:1519–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chowdhury EK, Nelson MR, Ernst ME, Margolis KL, Beilin LJ, Johnston CI, Woods RL, Murray AM, Wolfe R, Storey E, Shah RC, Lockery JE, Tonkin AM, Newman AB, Williamson JD, Abhayaratna WP, Stocks NP, Fitzgerald SM, Orchard SG, Trevaks RE, Donnan GA, Grimm R, McNeil J, Reid CM; ASPREE Investigator Group. Factors associated with treatment and control of hypertension in a healthy elderly population free of cardiovascular disease: a cross-sectional study. Am J Hypertens 2019. December 6 Pii:hpz192.doi: 10.1093/ajh/hpz192 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lockery JE, Rigby J, Collyer TA, Stewart AC, Woods RL, McNeil JJ, Reid CM, Ernst ME; ASPREE investigator Group. Optimising medication data collection in a large-scale clinical trial. PLoS One 2019. December 27;14(12):e0226868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoare E, Kingwell BA, Jennings GLR. Blood pressure down under, bud down under what? US and Australian hypertension guideline conversation. Hypertension 2018;71:972–975. [DOI] [PubMed] [Google Scholar]
- 16.Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GA, Johnston CI, et al. Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003;348:583–592. [DOI] [PubMed] [Google Scholar]
- 17.Officers ALLHAT and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981–2997. [DOI] [PubMed] [Google Scholar]
- 18.The ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Heart Foundation of Australia. Guide to management of hypertension 2008 (Updated December 2010) [online]
- 20.Schaffer AL, Pearson S, Buckley NA. How does prescribing for antihypertensive products stack up against guideline recommendations? An Australian population-based study (2006–2014). Br J Clin Pharmacol 2016;82:1134–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Presure: the JNC 7 report. JAMA 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 22.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 23.Weber MA. Angiotensin receptor blockers Chapter C137. In, Hypertension primer: the essentials of high blood pressure: basic science, population science, and clinical management. Izzo JL Jr, Sica DA, Black HR, eds. 4th edition 2008. Lippincott Williams & Wilkins. [Google Scholar]
- 24.Mehlum MH, Liestøl K, Kjeldsen S, Wyller TB, Julius S, Rothwell PM, Mancia GM, et al. Blood pressure-lowering profiles and clinical effects of angiotensin receptor blockers versus calcium channel blockers. Hypertension 2020; epub ahead of print 10.1161/HYPERTENSIONAHA.119.14443 [DOI] [PubMed] [Google Scholar]
- 25.Iburg KM. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1345–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


