Introduction
Deaths from fentanyl and from psychostimulants are increasing (Kariisa et al., 2019; O’Donnell et al., 2020) and new psychoactive substances (NPS) continue to emerge (US Drug Enforcement Administration [DEA], 2020). Methods of drug administration are also rapidly changing, with record-high increases in vaping of cannabis among adolescents (Miech et al., 2019). Further, the coronavirus disease 2019 (COVID-19) appears to be associated with drug overdoses and changes in use behavior (Volkow, 2020). While lagged indicators, such as national estimates of drug use, are useful for monitoring patterns of drug use and associated consequences, a national system to detect dangerous trends as they emerge is needed.
The New National Drug Early Warning System (NDEWS)
NDEWS was first funded by the National Institute on Drug Abuse (NIDA) in 2014 to expand the longstanding Community Epidemiology Workgroup (CEWG). In April 2020, the second iteration of the NIDA-funded NDEWS was awarded to our team from University of Florida, New York University, and Florida Atlantic University. NDEWS continues to examine lagged indicators but incorporates real-time surveillance to detect early signals of potential drug epidemics with an expanded Early Warning Network utilizing novel surveillance methods to rapidly harmonize data (Figure). A Scientific Advisory Group of 12 scientists across the US and 5 experts from the DEA, Centers for Disease Control and Prevention (CDC), and the Office of National Drug Control Policy (ONDCP) guides the new NDEWS.
Figure.
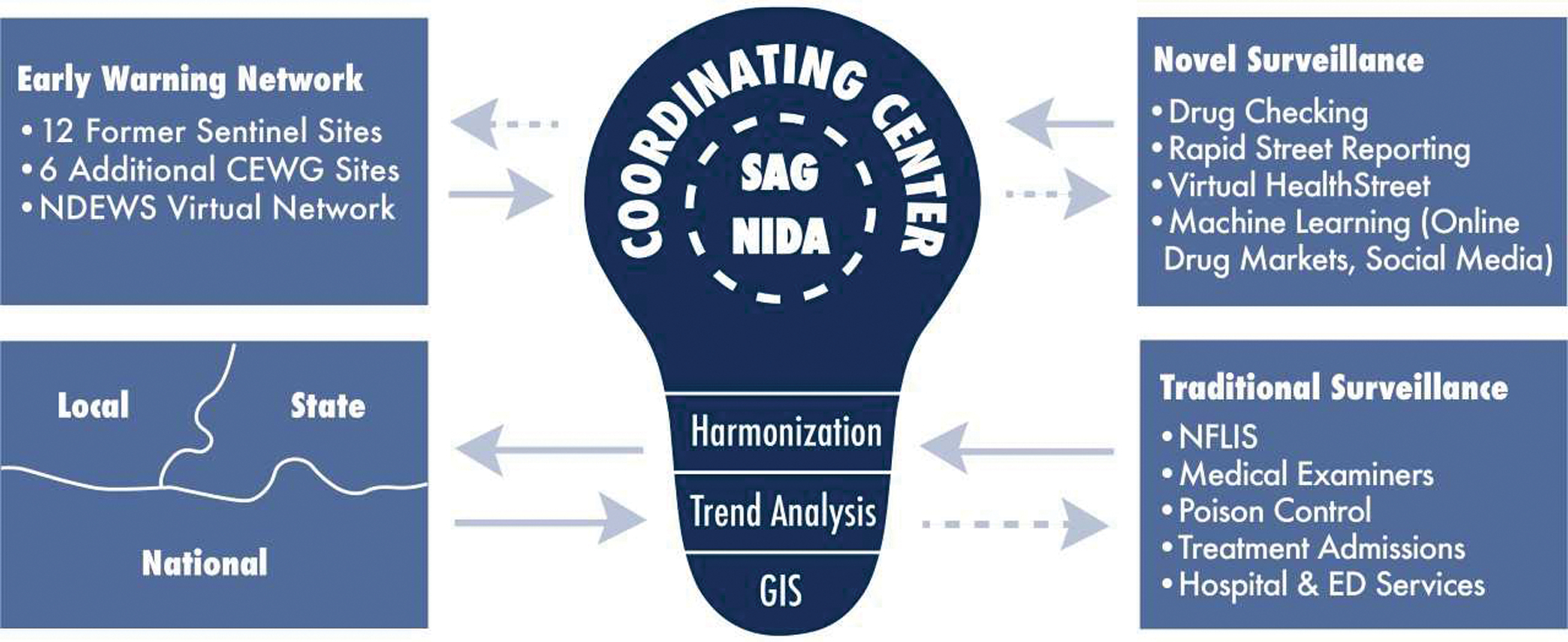
The National Drug Early Warning System
NDEWS: National Drug Early Warning System; CEWG: Community Epidemiology Workgroup; SAG: Scientific Advisory Group; NIDA: National Institute on Drug Abuse; GIS: geographic information system, NFLIS: National Forensic Laboratory Information System; ED: emergency department.
Early Warning Network
Scientists from 18 urban, suburban, and rural areas in the US, comprising the Early Warning Network, will regularly collect a standardized set of community-level indicators including drug availability, use and consequences of emerging drugs, morbidity, and mortality to compare sites. We will also collect data on self-reported use with accompanying biospecimens, drug seizures, prices, purity, diversion, and infectious diseases related to drug use, including COVID-19.
Novel and Rapid Surveillance
By focusing on leading-edge indicators, the resulting system is more responsive than reactive, relying on traditional, indirect sources, including data from the DEA’s National Forensic Laboratory Information System (NFLIS), Poison Control Centers, medical examiners/coroners, and emergency departments. New, direct sources, will include receiving data from drug checking and on-the-ground epidemiologic investigations within the 18 sites that include hair testing for exposure fentanyl and to over 100 NPS. Other direct sources of data will include outbreak investigations, a virtual community-based HealthStreet cohort of people self-reporting drug use, and web monitoring via machine-learning algorithms deployed to darknet drug markets and forums. Another focus will be on other known high-risk populations such as nightclub and dance festival attendees and “psychonauts” (Peacock et al., 2019).
Through a new NIDA Supplement, we have begun to examine the effect of COVID-19 on reporting and detection of overdose and other drug related outcomes through a longitudinal study of key informants involving medical examiners/coroners, funeral directors, emergency medical technicians, and syringe exchange workers, in Early Warning Network cities.
Dissemination and Training
Two additional goals are fundamental: dissemination and training. Dissemination is modeled after the Florida drug-Related Outcomes Surveillance and Tracking System (FROST). Results will also be disseminated to the community through our website (http://ndews.org/) and through webinars with an aim to reach people who use drugs and providers who care for people who use drugs. Our NIDA T32 Training Program and our NDEWS Research Lab is also training the next generation of scientists in surveillance science; students, fellows and junior scientists are conducting research, analyzing the data, writing, publishing and sharing results with the public and scientists in epidemiology, public health, forensic toxicology, psychology, artificial intelligence, and machine learning.
This system relies on trends found by the scientific network funded by the NIH and other agencies, as well as the community at large.
Acknowledgments
This research is supported by grants through the National Institute on Drug Abuse: U01DA051126 (Cottler) and T32DA035167. The National Institutes of Health provided financial support for the project and the preparation of the manuscript but did not have a role in the writing of the manuscript, nor the decision to submit the present research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflicts declared.
References
- Kariisa M, Scholl L, Wilson N, Seth P, Hoots B, 2019. Drug overdose deaths involving cocaine and psychostimulants with abuse potential – United States, 2003–2017. MMWR: Morb. Mortal Wky Rep 68, 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Patrick ME, O’Malley PM, Johnston LD, Bachman JG, 2019. Trends in reported marijuana vaping among US adolescents, 2017–2019. JAMA. 323, 475–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell J, Gladden RM, Goldberger BA, Mattson CL, & Kariisa M (2020). Notes from the field: opioid-involved overdose deaths with fentanyl or fentanyl analogs detected - 28 states and the District of Columbia, July 2016-December 2018. MMWR: Morb. Mortal Wky Rep 69, 271–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock A, Bruno R, Gisev N, Degenhardt L, Hall W, Sedefov R, White J, Thomas KV, Farrell M, Griffiths P, 2019. New psychoactive substances: challenges for drug surveillance, control, and public health responses. Lancet. 394, 1668–1684. [DOI] [PubMed] [Google Scholar]
- US Drug Enforcement Administration, 2020. National Forensic Laboratory Information System: NFLIS-Drug 2019 Midyear Report. Springfield, VA: (Accessed on 2 July 2020). https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/13408NFLISDrugMidYear2019.pdf [Google Scholar]
- Volkow ND, 2020. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 173 61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]


