Abstract
Background:
Adherence to recommended laboratory testing practices is crucial for sexually transmitted infection (STI) prevention and control. The objective of this paper is to compare Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) testing practices of US clinical laboratories in 2013 prior to the updated 2014 CDC recommendations and in 2015 following the updated recommendations.
Methods:
A total of 236 clinical laboratories participated in surveys about their 2013 and 2015 CT and NG testing practices, including questions on specimen types collected and assays used.
Results:
There was an increase of 5 laboratories offering CT NAAT testing from 2013 to 2015 and an increase of 5 laboratories offering NG NAAT testing. There was a net increase of three laboratories accepting urine for CT and NG NAAT testing, the preferred specimen type for males. There was not a net increase in the total number of laboratories accepting vaginal swabs for CT NAAT testing (n=89 in 2013 and 2015), the preferred specimen type for females, but there was an increase of three laboratories accepting vaginal swabs for NG NAAT testing. The number of laboratories performing NG susceptibility testing decreased from 100 in 2013 to 89 in 2015 (X2 = 1.07, p > 0.10).
Conclusions:
There were no major changes in testing practices in the two year period from 2013 to 2015. However, there were some small shifts, including increases in the use of NAATs, acceptance of CDC preferred specimen types for CT/NG, and changes in usage of assays by manufacturer.
SUMMARY:
A survey of clinical laboratories in the US comparing 2013 CT/NG testing practices (prior to the release of the 2014 CDC testing recommendations) to 2015 CT/NG testing practices.
INTRODUCTION
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) are the most common notifiable bacterial sexually transmitted infections (STIs) in the United States.1 In 2018, 1.76 million cases of CT and 583,405 cases of NG were reported to the Centers for Disease Control and Prevention (CDC).1,2 A large number of cases remain undetected because many people with CT or NG are asymptomatic and do not seek testing.3,4 Untreated CT can lead to serious complications, including pelvic inflammatory disease (PID), infertility, and ectopic pregnancy in women and urethritis in men.5–7 Untreated NG can lead to PID in women and urethritis in men.4
Because of the high prevalence of asymptomatic CT and NG infections, screening is necessary to identify and treat these infections. Accurate detection of CT and NG infections relies upon appropriate laboratory diagnosis. In 2014, the CDC published updated recommendations regarding screening tests to detect CT and NG infections, including new recommendations regarding optimal specimen types (vaginal swabs for women and first catch urine for men) and the use of tests to detect rectal and oropharyngeal CT and NG.8 This paper compares CT and NG testing practices of US clinical laboratories in 2013 prior to the updated CDC recommendations and in 2015 following the release of the updated CDC recommendations to assess changes in testing practices.
METHODS
Sample and Survey Instrument
The survey was administered to US clinical laboratories and was based on the previous STD testing practices survey of clinical laboratories.9 The 2014 survey collected data on CT and NG testing activities conducted between January 1, 2013 and December 31, 2013, including types of specimens tested, types of test used (manufacturer), and testing for antimicrobial resistance. The 2016 survey collected data on testing activities performed January 1, 2015 through December 31, 2015. Throughout the report, the surveys and data reference the year of the data, rather than the year of the survey to maintain consistency. The survey was determined to be not human subjects research and exempt from Institutional Review Board review.
Data Analysis
Descriptive statistics were calculated for all survey items. Chi-square tests were conducted on data from 2013 and 2015 to determine if there were significant changes in testing practices between years. All statistical analysis was conducted in SPSS version 26.
RESULTS
The 2015 survey was sent to the 376 clinical laboratories that completed the APHL 2013 survey. Of those, 236 clinical laboratories responded to the 2015 survey (62.8% response rate). Only data from laboratories that completed both surveys are included in this report. Figure 1 shows the number of clinical laboratories from each state that completed the survey.
Figure 1:
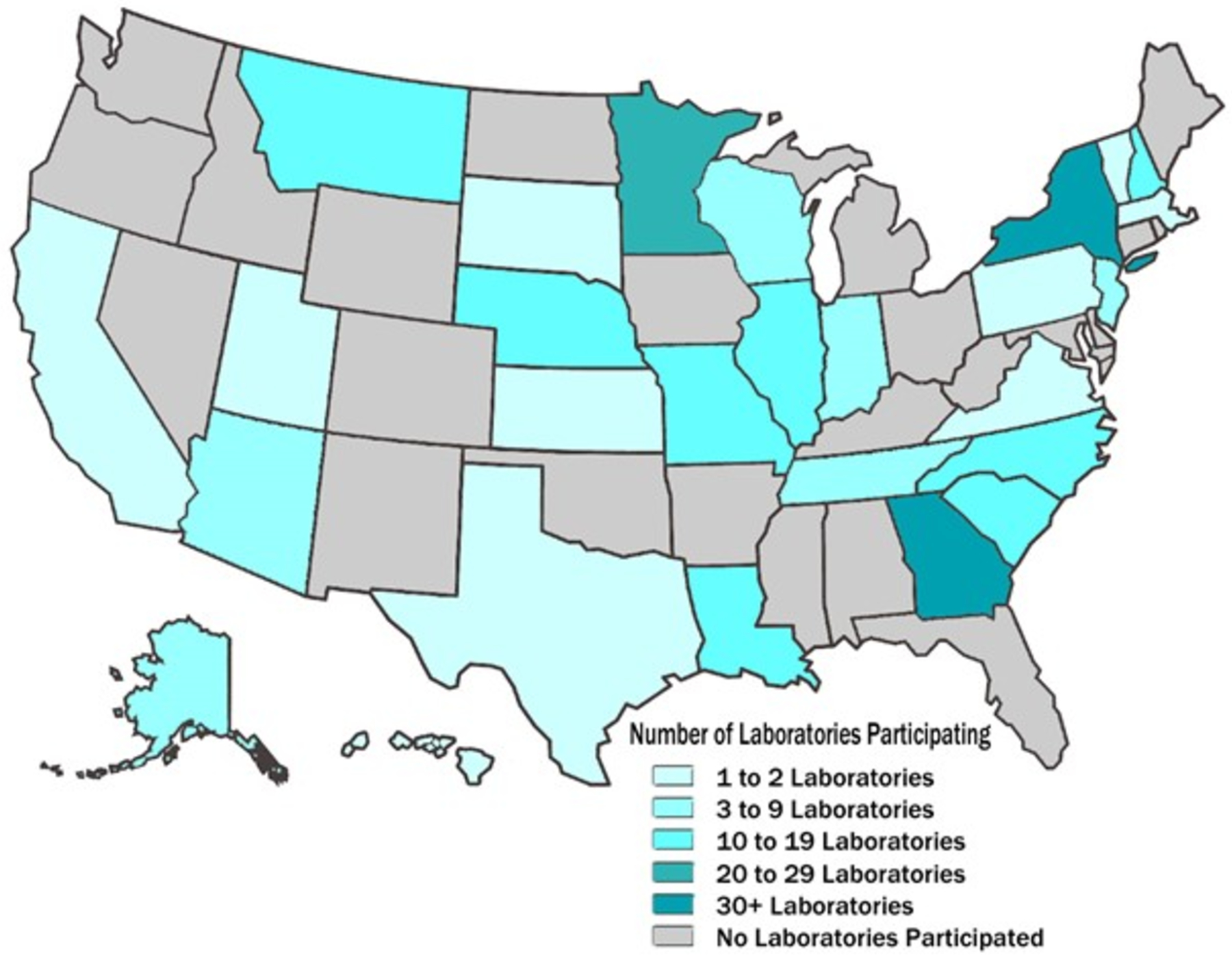
States Represented in Both 2013 and 2015 Surveys (N=236)
Chlamydia Testing Practices
Laboratories were asked to identify what types of chlamydia testing were performed in-house, referred to another laboratory, or not offered (Table 1). Over half of the laboratories offered CT NAAT testing in-house in 2013 and 2015. The number of laboratories offering in-house culture remained steady at 22 from 2013 to 2015, but the number of laboratories providing referrals for culture significantly decreased from 170 in 2013 to 143 in 2015 (X2 = 6.9, p ≤ 0.01). Other CT testing methods, such as DFA, EIA, hybrid capture or rapid testing were rarely (<5%) performed in-house, and less than half offered them through referral.
Table 1:
Types of CT Tests Offered by Year (N=236)
| 2013 | 2015 | |||||
|---|---|---|---|---|---|---|
| Type of CT Test | In-House N (%) |
Referral N (%) |
Not Offered N (%) |
In-House N (%) |
Referral N (%) |
Not Offered N (%) |
| Culture | 22 (9.3%) | 170 (72.0%) | 44 (18.6%) | 22 (9.3%) | 143 (60.6%) | 69 (29.2%) |
| DFA | 11 (4.7%) | 120 (50.8%) | 105 (44.5%) | 8 (3.4%) | 99 (41.9%) | 127 (53.8%) |
| Hybrid Capture | 3 (1.3%) | 82 (34.7%) | 151 (64.0%) | 2 (0.8%) | 79 (33.5%) | 153 (64.8%) |
| NAAT | 130 (55.1%) | 96 (40.7%) | 9 (3.8%) | 135 (57.2%) | 93 (39.4%) | 7 (3.0%) |
| Rapid test | 8 (3.4%) | 56 (23.7%) | 172 (72.9%) | 6 (2.5%) | 60 (25.4%) | 167 (70.8%) |
| MIF | 2 (0.8%) | 79 (33.5%) | 155 (65.7%) | 2 (0.8%) | 73 (30.9%) | 159 (67.4%) |
| EIA | 2 (0.8%) | 86 (36.4%) | 148 (62.7%) | 7 (3.0%) | 79 (33.5%) | 148 (62.7%) |
| CF | 1 (0.4%) | 78 (33.1%) | 157 (66.5%) | 0 (0.0%) | 78 (33.1%) | 156 (66.1%) |
| Other | 4 (1.7%) | 8 (3.4%) | 224 (94.9%) | 4 (1.7%) | 19 (8.1%) | 213 (90.2%) |
DFA = Direct Fluorescent Antibody; NAAT = Nucleic Acid Amplification Testing; MIF = Microimmunofluorescence;
EIA = Enzyme Immunoassay; CF = Complement Fixation
CT NAAT Testing
From 2013 to 2015, there was a net increase of five laboratories offering CT NAAT testing in-house (from 130 to 135), though this increase was not statistically significant (X2 = 0.21, p > 0.10). Of the 130 laboratories conducting NAAT testing in-house in 2013, 93.8% (n=122) offered NAAT testing in 2015, while 6.2% (n=8) no longer conducted testing in-house. Of the 106 laboratories that did not conduct NAAT testing in-house in 2013, 12.3% (n=13) offered NAAT testing in 2015 (Appendix Table 1).
Types of specimens accepted for CT NAAT
Of the laboratories that reported conducting CT NAAT testing in-house, over 90% accepted urine and endocervical swab specimens in 2013 and 2015 (Table 2). There was no net increase in 2015 in the total number of laboratories accepting vaginal swabs for NAAT testing [2013: 89/130 (69%); 2015: 89/135 (66%)]. From 2013 to 2015, there was a net increase of three laboratories accepting urine for CT NAAT testing [2013: 126/130 (97%); 2015: 129/135 (96%)].
Table 2:
Types of specimens accepted for CT NAAT (2013 N=130; 2015 N=135)*
| 2013 | 2015 | |
|---|---|---|
| Specimen | N (%) | N (%) |
| Urine | 126 (96.9%) | 129 (95.6%) |
| Endocervical Swab | 121 (93.1%) | 122 (90.4%) |
| Vaginal Swab | 89 (68.5%) | 89 (65.9%) |
| Male Urethral Swab | 93 (71.5%) | 74 (54.8%) |
| Rectal Swab | 22 (16.9%) | 27 (20.0%) |
| Throat Swab | 19 (14.6%) | 20 (14.8%) |
| Ocular/Conjunctival Swab | 14 (10.8%) | 15 (11.1%) |
| Endocervical Specimen in PAP media | 44 (33.8%) | 51 (37.8%) |
| Serum | 0 (0.0%) | 1 (0.7%) |
| Other | 4 (3.1%) | 5 (3.7%) |
Labs conducting CT NAAT testing in-house
The most common types of specimens received for CT NAAT in 2013 and 2015 were endocervical swabs (63.8% and 45.9%) and urine (30.0% and 29.6%). Only 11% of laboratories reported receiving vaginal swabs as their most common specimen type in 2013 and 2015.
Gonorrhea Testing Practices
The number of laboratories offering NG NAAT testing in-house increased slightly from 2013 to 2015, while the number of laboratories performing culture, Gramstain, and hybrid capture decreased slightly from 2013 to 2015 (Table 3). Other NG testing methods, such as hybrid capture or rapid testing were rarely (<3%) performed in-house, and less than a third offered them through referral.
Table 3:
Types of NG Test Offered by Location by Year (N=236)
| 2013 | 2015 | |||||
|---|---|---|---|---|---|---|
| Type of GC Test | In-House N (%) |
Referral N (%) |
Not Offered N (%) |
In-House N (%) |
Referral N (%) |
Not Offered N (%) |
| Culture | 180 (76.3%) | 39 (16.5%) | 17 (7.2%) | 175 (74.2%) | 38 (16.1%) | 23 (9.7%) |
| Gramstain | 170 (72.0%) | 24 (10.2%) | 42 (17.8%) | 153 (64.8%) | 27 (11.4%) | 56 (23.7%) |
| Hybrid Capture | 2 (0.8%) | 75 (31.8%) | 159 (67.4%) | 1 (0.4%) | 77 (32.6%) | 158 (66.9%) |
| NAAT | 131 (55.5%) | 99 (41.9%) | 6 (2.5%) | 136 (57.6%) | 95 (40.3%) | 5 (2.1%) |
| Rapid test | 3 (1.3%) | 57 (24.2%) | 176 (74.6%) | 5 (2.1%) | 59 (25.0%) | 172 (72.9%) |
| EIA | 0 (0.0%) | 81 (34.3%) | 155 (65.7%) | 0 (0.0%) | 75 (31.8%) | 161 (68.2%) |
| Other | 2 (0.8%) | 4 (1.7%) | - | 3 (1.3%) | 18 (7.6%) | - |
NAAT = Nucleic Acid Amplification Testing; EIA = Enzyme Immunoassay
NG NAAT Testing
From 2013 to 2015, there was a net increase of five laboratories offering NG NAAT testing in-house (from 131 to 136), though this increase was not statistically significant (X2 = 0.22, p > 0.10). Of the 131 laboratories conducting NG NAAT testing in-house in 2013, 94.7% (n=124) continued to offer NAAT testing in 2015, while 5.3% (n=7) no longer conducted testing in-house (Appendix Table 2). Of the 105 laboratories that did not conduct NG NAAT testing in-house in 2013, only 11.4% (n=12) offered NAAT testing in 2015.
Types of specimens accepted for NG NAAT
Of the laboratories that reported conducting NG NAAT testing in-house, over 90% reported accepting urine and endocervical swab specimens in 2013 and 2015 (Table 4). The total number of laboratories accepting vaginal swabs for NAAT testing only slightly increased from 2013 to 2015 [2013: 91/131 (70%); 2015: 94/136 (69%)]. There was also a slight increase in 2015 in the total number of laboratories accepting urine for NAAT testing [2013: 126/131 (96%); 2015: 129/136 (95%)].
Table 4:
Types of specimens accepted for NG NAAT (2013 N=131; 2015 N=136)
| 2013 | 2015 | |
|---|---|---|
| Specimen | N (%) | N (%) |
| Urine | 126 (96.2%) | 129 (94.9%) |
| Endocervical Swab | 122 (93.1%) | 126 (92.6%) |
| Vaginal Swab | 91 (69.5%) | 94 (69.1%) |
| Male Urethral Swab | 93 (71.0%) | 75 (55.1%) |
| Rectal Swab | 24 (18.3%) | 27 (19.9%) |
| Throat Swab | 21 (16.0%) | 23 (16.9%) |
| Ocular/Conjunctival Swab | 13 (10.0%) | 12 (8.8%) |
| Endocervical Specimen in PAP media | 45 (34.3%) | 53 (39.0%) |
| Other | 4 (3.1%) | 5 (3.7%) |
The most common types of specimens received for NG NAAT in 2013 and 2015 were endocervical swabs (62.3% and 45.6%) and urine (32.1% and 30.1%). Only 10% of laboratories in 2013 and 13% of laboratories in 2015 reported receiving vaginal swabs as their most common specimen type.
NG Culture and Susceptibility Testing
There was a net decrease in the number of laboratories offering NG culture in-house from 2013 to 2015 [2013: 180/236 (76%); 2015: 175/236 (74%); Table 3], though this difference was not significant (X2 = 0.28, p > 0.10).
The number of laboratories performing NG susceptibility testing decreased from 100 in 2013 to 89 in 2015 (X2 = 1.07, p > 0.10). The vast majority of laboratories offering NG susceptibility testing used a beta lactamase assay [2013: 79/100 (79%); 2015: 77/89 (86.5%)] (Table 5). For laboratories that offered NG susceptibility testing, the most common antimicrobials tested included penicillin [2013: 28/100 (28%); 2015: 23/89 (26%)], ceftriaxone [2013: 20/100 (20%); 2015: 19/89 (21%)], ciprofloxacin [2013: 17/100 (17%); 2015: 15/89 (17%)], and tetracycline [2013: 14/100 (14%); 2015: 18/89 (20%)].
Table 5:
NG Susceptibility Testing (2013 N=100, 2015 N=89)
| 2013 | 2015 | |
|---|---|---|
| Type of NG Susceptibility Testing | N (%) | N (%) |
| Agar dilution | 1 (1.0%) | 0 (0.0%) |
| Disc diffusion | 8 (8.0%) | 11 (12.4%) |
| Etest | 7 (7.0%) | 9 (10.1%) |
| Beta lactamase assay | 79 (79.0%) | 77 (86.5%) |
| Other | 5 (5.0%) | 7 (7.9%) |
Note: In 2013, laboratories could select only the primary method used. In 2015, laboratories could select all methods used.
CT and NG Testing By Manufacturer
Use of CT and NG tests shifted slightly from 2013 to 2015, which have been categorized by manufacturer rather than specific test due to any potential changes in the exact test method between the two surveys. Use of a Cepheid GeneXpert® test as the primary method of CT and NG testing significantly increased from 11.0% of laboratories in 2013 to about 17% in 2015. Use of a Roche Molecular Systems, Inc. test increased from 8.5% in 2013 to 9.3% in 2015 for CT testing and from 6.8% to 10.2% for NG testing. Use of a Hologic, Inc. test as the primary method of CT testing decreased from 24.6% in 2013 to 22.0% in 2015 for and from 32.6% in 2013 to 28.0% in 2015 for NG testing. Use of a BD Diagnostics test decreased from 10.6% in 2013 to 6.4% in 2015 for CT testing and from 13.1% in 2013 to 7.6% in 2015 for NG testing (Appendix Tables 3 and 4).
DISCUSSION
Results indicate that there were no major changes in CT and NG testing practices in the two year period from 2013 to 2015. However, there were some small shifts, including increases in the use of NAAT testing, acceptance of CDC preferred specimen types for CT/NG and changes in usage of assays by manufacturer.
There was a small increase overall in the total number of laboratories using CT and NG NAAT testing following the release of the 2014 CDC recommendations, which may indicate that laboratories are either not reading the CDC recommendations or are slow to adapt new protocols and testing practices. Although there was a slight increase in the number of laboratories testing preferred specimen types, overall most laboratories had still not shifted to testing preferred CT/NG specimen types for females. For female screening for CT/NG, the CDC recommends the use of vaginal swabs as the preferred specimen type.8 Vaginal swab specimens are as sensitive as cervical swab specimens, easier to collect, and there is no difference in specificity.10,11 First catch urine from women, while acceptable for screening, might detect up to 10% fewer infections when compared with vaginal swab samples.10,11 Because laboratories can only test the specimens they receive, these findings may point to a broader issue of lack of uptake of new testing and treatment recommendations by clinicians and healthcare providers.12
One limitation of this study is that questions about urine specimens were not differentiated between male and female specimens, thus, we do not know the proportion of male urine specimens tested (CDC recommended sample type for men) versus the proportion of female urine specimens tested (not the CDC recommended sample type for women). Another limitation is that representation of the clinical laboratories who responded to and completed the survey is not uniform, so these results may not accurately indicate testing practices across all areas of the US. Additional information is needed about testing practices in some areas, particularly in the southeast, where rates of STIs are very high. Furthermore, we evaluated laboratory practices that are over 5 years old. As a result, study findings may not reflect today’s laboratory practices. However, these data still provide an important snapshot of how testing practices changed following the release of CDC recommendations in many areas of the US.
In conclusion, only slight changes in testing practices were observed following the release of the 2014 CDC recommendations. The lack of major changes in testing practices observed may be due to the fact that the survey was given only one year after the CDC recommendations. Clinical laboratories may take more time to adjust to new recommendations since they need to be adopted not only by the laboratory, but also by those submitting specimens to the laboratory. Further research is needed to continue to monitor and evaluate STD testing changes in clinical laboratories as the CDC releases updated recommendations.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank the staff members at the clinical laboratories that completed this survey and John Papp at the Centers for Disease Control and Prevention for his review of this manuscript.
Conflicts of Interest and Source of Funding: AD is supported by the National Institute on Drug Abuse (K01DA044853) for career development. She also has received consulting fees from the Association of Public Health Laboratories. For the remaining authors, no conflicts of interest were declared. This publication was supported by Cooperative Agreement #5NU60OE000103, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
REFERENCES
- 1.Chlamydia - 2018 Sexually Transmitted Diseases Surveillance [Internet]. 2019. [cited 2020 Apr 20];Available from: https://www.cdc.gov/std/stats18/chlamydia.htm
- 2.Gonorrhea - 2018 Sexually Transmitted Diseases Surveillance [Internet]. [cited 2020 Apr 20];Available from: https://www.cdc.gov/std/stats18/Gonorrhea.htm
- 3.Stamm W. Chlamydia trachomatis infections of the adult. In: Holmes K, Sparling F, Stamm W, et al. , editors. Sexually Transmitted Diseases. New York, NY: McGraw-Hill Companies, Inc.; 2007. p. 575–94. [Google Scholar]
- 4.Hook EI, Handsfield H. Gonoccocal infections in the adult. In: Holmes K, Sparling F, Stamm W, et al. , editors. Sexually Transmitted Diseases. New York, NY: McGraw-Hill Companies, Inc.; 2007. p. 627–45. [Google Scholar]
- 5.Hoenderboom BM, van Benthem BHB, van Bergen JEAM, et al. Relation between Chlamydia trachomatis infection and pelvic inflammatory disease, ectopic pregnancy and tubal factor infertility in a Dutch cohort of women previously tested for chlamydia in a chlamydia screening trial. Sex Transm Infect 2019;sextrans-2018–053778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chow JM. The Association Between Chlamydia trachomatis and Ectopic Pregnancy: A Matched-Pair, Case-Control Study. JAMA 1990;263(23):3164. [PubMed] [Google Scholar]
- 7.Moi H, Blee K, Horner PJ. Management of non-gonococcal urethritis. BMC Infect Dis 2015;15(1):294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papp J, Schachter J, Gaydos C, Van Der Pol B. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae−-2014. MMWR Recomm Rep 2014;63(RR-02):1–24. [PMC free article] [PubMed] [Google Scholar]
- 9.Association of Public Health Laboratories. 2013 Chlamydia and Gonorrhea Clinical Laboratory Practices Survey [Internet]. 2018. Available from: https://www.aphl.org/aboutAPHL/publications/Documents/ID-2018Aug-2013-CTGC-Clin-Lab-Practices-Survey-Summary-Data-Report.pdf
- 10.Schachter J, Chernesky MA, Willis DE, et al. Vaginal Swabs Are the Specimens of Choice When Screening for Chlamydia trachomatis and Neisseria gonorrhoeae: Results From a Multicenter Evaluation of the APTIMA Assays for Both Infections: Sex Transm Dis 2005;32(12):725–8. [DOI] [PubMed] [Google Scholar]
- 11.Michel C-EC, Sonnex C, Carne CA, et al. Chlamydia trachomatis Load at Matched Anatomic Sites: Implications for Screening Strategies. J Clin Microbiol 2007;45(5):1395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis A, Gaynor A. Testing for Sexually Transmitted Diseases in US Public Health Laboratories, 2016: Sex Transm Dis 2020;47(2):122–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


