Abstract
Objective:
To test the effect of a behavioral economics intervention in two food pantries on the nutritional quality of food available at the pantries and the foods selected by adults visiting food pantries.
Design:
An intervention (SuperShelf) was implemented in two food pantries (Sites A and B), with two other pantries (Sites C and D) serving as a control for pantry outcomes. The intervention aimed to increase the amount and variety of healthy foods (supply), as well as the appeal of healthy foods (demand) using behavioral economics strategies. Assessments included baseline and 4-month follow-up client surveys, client cart inventories, pantry inventories, and environmental assessments. A fidelity score (range 0–100) was assigned to each intervention pantry to measure the degree of implementation. A Healthy Eating Index score (HEI-2010, range 0–100) was generated for each client cart and pantry.
Setting:
Four Minnesota food pantries
Subjects:
Clients visiting intervention pantries before (n = 71) and after (n = 70) the intervention
Results:
Fidelity scores differed by intervention site (Site A=82, Site B=51). At Site A, in adjusted models, client cart HEI-2010 scores increased on average 11.8 points (p<0.0001), whereas there was no change at site B. HEI-2010 pantry environment scores increased in intervention pantries (Site A = 8 points, Site B = 19 points) and decreased slightly in control pantries (Site C = −4 points, Site D = −3 points).
Conclusions:
When implemented as intended, SuperShelf has the potential to improve the nutritional quality of foods available to and selected by pantry clients.
INTRODUCTION
In 2016, an estimated 1 in 8 households in the U.S. experienced food insecurity, (i.e., they lacked access to enough food for an active, healthy life for all household members).(1) While federal food assistance programs, such as the Supplemental Nutrition Assistance Program (SNAP), can increase food resources in some households, not everyone is eligible for these programs or receives enough benefits to avoid food insecurity.(2,3) In 2014, nearly 44 million people relied on food pantries to obtain food for their household. Though often considered an emergency resource, food pantries and other hunger relief agencies have increasingly come to serve clients facing persistent food insecurity.(3) These agencies serve food to low-income families with a disproportionate risk of insufficient diet(4,5) and diet-sensitive chronic disease,(3,6) making food pantries a worthwhile setting to address equity issues around healthy food access.(7,8)
The hunger relief network faces challenges both in supplying healthy food to clients, and in making those foods appealing to clients.(7,9–13) Pantry food sourcing relies in large part on food donations, food purchased at reduced costs, and items rescued from the food waste stream, which may not yield a consistent supply of healthy food without intentional efforts on the part of pantry staff.(7) The nutritional quality of food available in food pantries is not routinely monitored, nor are there standards for what is offered, but research has indicated that there is considerable room for improvement.(9,14–18) An analysis of Minnesota pantries using the United States Department of Agriculture (USDA) Healthy Eating Index-2010 (HEI-2010), which aligns with the Dietary Guidelines for Americans, found that the dietary component scores for total fruit, dairy, and whole grains of food pantry inventory were less than half of their optimal scores.(16,17) On the demand side, clients have reported that that they would like to see more healthy foods, like fruits, vegetables, dairy, and meats at the food pantry;(19–21) at the same time, they may not take what is offered if it is not appealing. Concerns over food safety, lack of produce variety, and the short shelf life of healthy perishables have been cited by clients,(7,20) which could be interpreted as low demand by food pantry staff, who report difficulty moving perishable food through the system in a timely way.(11,13) These challenges are interdependent: without an adequate and regular supply, clients cannot choose healthy foods, and without demonstrated client demand, pantries may not be motivated to solicit healthier donations or invest in infrastructure to support healthy food provisions.
The potential for hunger relief agencies to address health is just beginning to be explored.(8) Successful interventions in food pantries have led to improvements in client diabetes management,(6) food insecurity,(22) cooking skills,(23) and healthier food ordering by staff.(16) Meanwhile, national hunger relief organizations have called for strategies to promote healthy food supply and selection in pantries.(12,24–28) Many of these strategies use a behavioral economics approach to make the healthy choice the easiest choice.(28,29) Behavioral economics as a field considers that human decisions are susceptible to the way that choices are presented;(30) thus, behavior change can be “nudged” through careful “choice architecture.”(31)
Behavioral economics strategies have shown potential to influence food choices in many settings, including retail, restaurants, and cafeterias.(30–35) In theory, behavioral economics strategies are well-suited to the hunger relief setting because many behavioral economics constructs (e.g., defaults, order, tradeoffs, cues, and salience (30,36,37)) are relevant to the way that food pantries already operate. First, as charitable organizations, food pantries do not rely on paid advertisements or slotting fees from food companies promoting low-nutrient products, unlike in the retail setting.(38) Pantries, therefore, have the autonomy to change their layout, item placement, and signage without compromising their financial performance, provided they have the time and support to make changes. Second, choice-based pantries (estimated to be 72% of pantries who order from food banks in the region39) give clients some flexibility in what they take home, but still have default options and place limits on the types and quantities of food clients can select. This feature of the food pantry is analogous to setting the “price” of an item. Within the limits of its own food supply, food pantries have a unique opportunity to shape client food selection by carefully altering these defaults and food allowances, while maintaining choices for clients. Next, behavioral economics interventions may be a good option in a setting where people face many competing constraints on their time and resources; unlike education-focused interventions (e.g., cooking classes), implementing behavioral economics changes does not place any particular burden on clients as long as pantries continue their same basic operations. Finally, interventions in food pantries have the potential to reduce health disparities, as these efforts are specifically directed at improving nutrition among those with a high risk for diet-related disease.
In reality, pantries often have a limited capacity to make transformative changes, given the constraints of staff and volunteer time, reluctance to change, and limited resources to make infrastructure improvements. Small-scale behavioral economics experiments in food pantries, in which specific food have been promoted, do show promise in changing client selection of these foods.(28,40) This study tests a larger-scale food pantry transformation effort, SuperShelf, rooted in behavioral economics. The aims of this pilot study were to test whether implementing SuperShelf in two food pantries would result in: (1) an increase in the nutritional quality of food available to clients, and (2) an increase in the nutritional quality of food selected by clients. The hypothesis was that the nutritional quality of foods available to clients and selected by clients would be higher after the intervention compared with before. An exploratory aim of the study was to develop SuperShelf fidelity scoring tool for use in future evaluation studies.
METHODS
Intervention
SuperShelf was developed over five years in a collaborative partnership among representatives from a food shelf, a food bank, an integrated health care system, a university research team, and the university’s Extension services.(41) SuperShelf uses a progression of steps to transform food shelves, creating welcoming environments for communities to access appealing, healthy food. As a basis for achieving this, pantries must be client-centered in their approach, environment, and culture; this is signified, for example, by having a choice-based food distribution model (rather than providing pre-packed bags), having non-discriminatory practices, and taking advantage of existing opportunities to provide healthy and culturally-specific food to clients (e.g., a local food bank’s Cultural Equity program). In all of the food shelves, all food that clients receive is free.
The core components of the intervention are to (1) establish consistent access to healthy foods and meet specific stocking standards and (2) to increase the appeal of healthy foods using behavioral economics strategies. Succeeding in both of these components is expected to create a feedback loop between healthy food availability and food selection by allowing healthy perishables and other items to move through the pantry quickly, encouraging pantries to sustain their new procurement efforts for healthy items.
The intervention was delivered by trained SuperShelf consultants, who were SNAP-Ed educators at the University of Minnesota-Extension. In the first phase, consultants worked with pantry staff, particularly those responsible for ordering food, to increase the quantity and variety of healthy food available to clients (supply and stretch). Consultants examined the mix of existing food sources at the pantry, their purchasing priorities, and their donation patterns. They suggested tradeoffs in ordering so that more was spent on healthy food while still staying within budget, helped to create messages for soliciting healthy donations, and sought additional sources of healthy food (e.g., from retail rescue, community gardens, and produce distributions). Sourcing fruits and vegetables in all forms, including canned, frozen, and dried, was encouraged. A set of stocking standards (available at https://www.supershelfmn.org/resources) served as the benchmark for pantries for maintaining a consistent supply of healthy food, recognizing that adequate supply is a prerequisite for clients to make healthy food choices.(30)
In the second phase, the intervention introduced behavioral economics to increase the prominence and appeal of healthy food. In the first step (shift), the SuperShelf consultant worked with the pantry to sort all food into food groups and arrange it on the shelf in a particular order, with fruits/vegetables, dairy, protein, grains, and cooking/condiments first, followed by mixed meals, snacks, and desserts. It also addressed the “flow” of clients, or how they would move through the food pantry. Next, consultants examined the food allowances set by the pantry. These allowances often use less healthy defaults and may be more prescriptive than necessary (e.g., each household is offered one pancake mix, one pancake syrup, and one jelly per visit); allowances can therefore be altered to offer more choice and healthier choices. If, instead, pancake mix, syrup, and jelly are grouped together with the full range of condiments, some of which are healthier (like mustard, spices, and vegetable oil), then clients have an expanded set of options, even if they are still allowed the same number of options. This arrangement creates competition between healthy and less healthy items and eliminates the opportunity cost of rejecting a less-healthy default option. Along with these changes, in the final step (showcase), the food pantry is rearranged so that healthy food is displayed in a more appealing manner (e.g., in colorful bins and baskets instead of banana baskets), has more prominence (e.g., whole grains are placed at eye level), and is displayed attractively along with SuperShelf branded signage.
Evaluation and Measures
The SuperShelf pilot evaluation study took place in four food pantries in the greater-Minneapolis-St. Paul, MN metropolitan area. All four sites were client-choice panties. Two pantries were intervention sites (A and B) and two were control sites (C and D). Sites A and C were overseen by the same director within the same umbrella organization, as were Sites B and D, which reasonably balanced the arms of the study in terms of organizational practices and culture. These sites were chosen because they volunteered to undergo a SuperShelf transformation and the structure of having two food shelves in each of the organizations lent itself to well balanced control and intervention sites. The purpose of the control pantries was to monitor the local pantry environment and inventory patterns during the evaluation period. Control sites were particularly important for detecting potential seasonal changes that might affect inventory during the study period. Control measures were only collected at the pantry level in this pilot study.
Assessments were conducted before and after the intervention. At baseline (January – February, 2017), 71 clients were enrolled at the two intervention pantries during their visit to the pantry. Recruitment took place after clients selected their food to avoid influencing choice. After completing the informed consent process, the client took a survey while research staff conducted a cart inventory, recording the food that clients had just selected. The intervention, led by trained University of Minnesota-Extension Educators, took place between February and May 2017. A second sample of 70 clients was enrolled following the intervention (May-June, 2017) for the same measures as baseline. It would not have been feasible or ethical to repeat follow-up measures with the same set of clients, as food shelf visits are likely to be irregular and urgent (i.e., visits cannot be scheduled around research needs). Moreover, the repeated-cross sectional method made it unlikely that clients would change their food choices due to participation in research.
During recruitment periods, which took place over 3 to 6 days at each pantry, all clients visiting the food pantry were approached by research staff at the end of their visit. Clients were eligible to participate if they were at least 18 years old, were mentally capable of informed consent, and spoke English. Non-English speakers were eligible if a client companion or pantry volunteer was available to translate all study-related materials (n=2). Participants received a $10 gift card for participating. The study was approved by the Institutional Review Board at the University of Minnesota.
Pantry-level assessments, conducted before and after the intervention, included a detailed “snapshot” inventory of all foods on the shelf available to clients, a walkthrough assessment, and extensive photo documentation of the food shelf space to assess fidelity (i.e., the degree to which the intervention was implemented as intended).
Fidelity measure.
The aim of the fidelity measure was to understand implementation successes and challenges. Pantry walkthrough assessments were developed by our study team and conducted in which trained study staff were asked to assess features of pantry environment. Study staff also took extensive photographs at the time of the assessment. Photographs followed the path of clients as they moved through the pantry, documenting the overall physical space (e.g., shelf arrangement, presence of clutter), and specific elements of food displays (e.g., signage, close-ups of fresh produce). Because this was a pilot study meant to inform the next phase of work, creating the final fidelity scoring tool was an iterative process that was finalized after all data were collected. The original walkthrough assessment demonstrated low-interrater reliability and high subjectivity in response options; the research team’s photographs were, therefore, used post hoc to measure more specific and objective elements of the physical space. For example, the original walkthrough assessment asked, “To what extent do you agree that fresh fruits and vegetables are displayed in an appealing manner?” with response options ranging from strongly agree to strongly disagree. In the final fidelity scoring tool, this question was: “Select the strategies that are being used to display fruits and vegetables in an appealing manner,” with 1 point each (up to 3) given if fruits and vegetables were: a) sorted/organized; b) not bruised or moldy; c) stocked abundantly; and d) in baskets or colored bins.
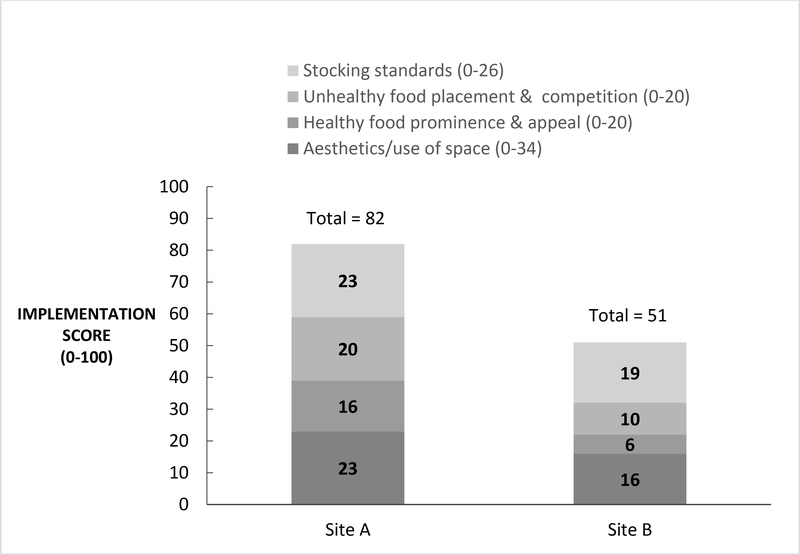
Inventory data also contributed to the fidelity scoring. From inventory data, a score was generated for the degree to which a pantry met specific SuperShelf stocking standards (e.g., 8 varieties of plain grains, 4 of which are whole grains). The final fidelity score (Supplement 1) has a range of 0–100 based on the sum of 4 subcomponents representing core SuperShelf intervention components: 1) aesthetics/use of space (34 points), 2) unhealthy food placement and competition (20 points), 3) healthy food prominence and appeal (20 points) and 4) meeting stocking standards (26 points).
Client measures.
Nutrient data were obtained by client cart inventories, which capture information on each product selected by the client at their visit. Staff took photographs of packaged foods to record the item name, brand, size, and quantity, and later entered this data into a database. Staff weighed and entered non-packaged food (e.g., loose vegetables) in the database in real time. Data were entered into Nutrient Data Systems for Research (NDSR), a nutrient analysis software application. A Healthy Eating Index-2010 (HEI-2010) score for each cart was calculated. The HEI-2010 is a valid and reliable USDA measure used to monitor how well a set of foods aligns with the Dietary Guidelines for Americans.(26,27) The HEI-2010 yields an overall score and 12 subcomponents of diet, including whole fruit, total fruit, total vegetables, whole grains, greens and beans, dairy, total protein foods, seafood and plant proteins, and fatty acid ratio. Three additional subcomponents (sodium, refined grains, and empty calories) are reverse coded so that higher scores indicate better alignment with standards. Data collection, data entry, and HEI-2010 scoring were based on protocols previously used by the principal investigator44. The HEI-2010 is a good instrument for the food pantry setting, as clients usually obtain a balance of items that contribute to all (or most) of the subcategories. Data from cart inventories were also used to calculate number of servings of fruits and vegetables and servings of whole grains clients selected at baseline and follow-up.
The client survey assessed demographics (age, gender, race/ethnicity, education, employment, household size), participation in federal food assistance programs, a two-item food insecurity screener,(45) frequency of pantry use, the portion of total food and produce a client received at the pantry. It included three items assessing (follow-up only) perceptions of changes in the last six months of a)The quality of the food offered at this food shelf b) The selection of different kinds of foods at this food shelf and c) the healthfulness of foods offered at this food shelf. Response option for all prompts were “Yes, I have noticed positive changes” or “No, I have not noticed any changes, or the changes have not been positive”. The survey also assessed client intention within the next 3 months to purchase or select any of 20 healthy, unprocessed types of foods. Food included fresh fruits and vegetables, brown rice, oatmeal, whole wheat flour, black beans, lentils, and spices.
Pantry measures.
In the two intervention pantries and two control pantries, HEI-2010 scores of pantry inventories (items on the shelf available to clients) was calculated from inventories conducted at a single time point before and after the intervention. Before each inventory, researchers asked pantries to stock the shelf the way that they would at the start of typical day that the pantry was open. An HEI-2010 score was calculated for each pantry before and after the intervention.
Analysis.
SAS Software v.9.4 (SAS Institute Inc., Cary, NC) was used for all analyses, and p-values <0.05 were considered statistically significant. For HEI-2010 scores, NDSR output files 04 and 09 were input into SAS code used to calculate HEI-2010 total and component scores, respectively for food shelf inventory and client carts.
The client level analysis assumed independence between the two samples (baseline and follow-up), as no more than three clients completed surveys at both time points. Client characteristics were analyzed combining the data from both food pantries. Pre and post survey responses were summarized using descriptive statistics (means and standard deviations or counts and proportions). Sample demographics and characteristics were compared between the pre and post samples using chi square tests or two-sample t-tests. Age group and education level were analyzed as ordinal variables with two-sample t-tests. The “prefer not to answer” and “missing” responses were not included in analyses.
For the primary outcome (change in client HEI-2010), pre/post changes in average client HEI-2010 scores and each HEI-2010 subcomponent were analyzed using multiple linear regression models controlling for client age, race, education, and food insecurity. First, HEI scores were examined separately by food pantry, and together in a multiple linear regression model to test for effect modification by food pantry. There was a significant interaction between the intervention and food pantry, thus HEI-2010 analyses were stratified by food pantry. Similarly, the number of servings of fruits and vegetables and servings of whole grains that clients took were compared from baseline to follow-up using multiple linear regression models (each food pantry separately), adjusting for household size. Results are reported as regression point estimates (β) and standard errors. At the food pantry level, change in HEI-2010 inventory scores and fruit and vegetable poundage were calculated to descriptively report changes in supply at the four sites.
RESULTS
Pantry and client characteristics
Pantry characteristics were balanced across the intervention and control arms of the study. Pantries in both arms were open to clients for an average of 16 hours per week. Intervention sites averaged 7 volunteers per day, while control sites averaged 8.5. Intervention sites reported serving an average of 23.5 clients per day compared with 16.3 clients in control pantries. The two arms were balanced in terms of food bank ordering frequency, and all four allowed clients to visit once a month.
Client survey demographics and characteristics are presented in Table 1. At baseline, clients were mostly female (66.7%) and racially/ethnically diverse (42.7% non-Hispanic black, 33.8% non-Hispanic white, 7.4% Asian, 10.3% Hispanic, and 5.9% Other). The average household size was 3.7 people. Most visited the food pantry once a month (77.9%). More than half of participants (55.4%) reported that about half or more of their total food in the last 6 months had been obtained at the food pantry. More than one-third (36.9%) reported that half or more of their total produce in the last 6 months had been obtained at the food pantry. There were no statistically significant differences in client characteristics between the baseline and follow-up samples.
Table 1.
Sample demographics and characteristics
| Baseline | Follow-up | ||
|---|---|---|---|
| % | % | p-value | |
| Age (n=71, 69)a | |||
| 18–29 | 9.9% | 13.0% | 0.86 |
| 30–39 | 19.7% | 23.2% | |
| 40–49 | 31.0% | 23.2% | |
| 50–59 | 25.4% | 27.5% | |
| 60–69 | 14.1% | 7.3% | |
| 70+ | 0.0% | 5.8% | |
| % Female (n=60, 70) | |||
| Female | 66.7% | 70.0% | 0.68 |
| Race (n=68, 67) | |||
| Non-Hispanic Black | 42.7% | 38.8% | 0.58 |
| Non-Hispanic White | 33.8% | 37.3% | |
| Asian | 7.4% | 13.4% | |
| Hispanic | 10.3% | 4.5% | |
| Other | 5.9% | 6.0% | |
| Has high-school education/GED or less (n=69, 69) | 43.5% | 53.6% | 0.23 |
| Employed (n=69, 69) | 47.8% | 46.4% | 0.87 |
| Food insecure (n=67, 63) | 79.1% | 81.0% | 0.79 |
| Currently participating in SNAP (n=58, 67) | 32.8% | 38.8% | 0.48 |
| Frequency of visiting this food shelf (n=68, 69) | |||
| More than once a month | 5.9% | 5.8% | 0.47 |
| Once a month | 77.9% | 69.6% | |
| Less than once a month/ First time visiting | 16.2% | 24.6% | |
| Portion of all food that comes from the food shelf in past 6 months (n=65, 68) | |||
| Less than Half | 44.6% | 54.4% | 0.26 |
| About Half or More | 55.4% | 45.6% | |
| Portion of produce that comes from the food shelf in past 6 month (n=65, 68) | |||
| Less than Half | 63.1% | 67.7% | 0.58 |
| About Half or More | 36.9% | 32.4% | |
| N (SD) | N (SD) | p-value | |
| Total # of Individuals in Household (n=71, 70) | 3.7 (2.3) | 3.8 (2.0) | 0.67 |
(Pre sample n, post sample n)
Implementation and fidelity
Each of the intervention sites worked to improve healthy food sourcing over 2–3 months, followed by a transformation day in which the food pantry was closed and rearranged according to SuperShelf principles. The final showcasing step, displaying appealing signage, was not implemented until July 2017 due to an unexpected delay in the sign orders; therefore, follow-up assessments were collected without the final signage four months after baseline assessments for both sites A and B. Total fidelity scores and subscores are presented in Figure 1. The post-intervention score for Site A was 82 out of 100, while the score for Site B was 51 of 100. Site A had the greatest room for improvement in the aesthetics/use of space subscore (68% of the maximum score). Site B scored less than 50% of the maximum score in all subcategories except stocking standards. Site A was overall considerably more successful in undergoing the core SuperShelf transformation elements, including rearranging the food pantry into food groups, changing the aesthetics of food presentation, putting the healthiest foods at eye level and creating competition for less healthy items by reworking its client shopping lists. Postimplementation meetings at Site B between the food pantry leadership, the SuperShelf team and the research team revealed several specific challenges, including: (i) lack of universal support among key staff meant to champion the transformation; (ii) staff turnover during the intervention period; and (iii) competing organizational priorities, which led to a lack of systemic adoption of SuperShelf standards into practices.
Figure 1.
Food Pantry Intervention Implementation Scores (0–100)
Client HEI-2010 scores
Table 2 presents change in Healthy Eating Index-2010 scores for clients at baseline and follow-up. Results for total HEI-2010 were similar in unadjusted models and models adjusting for age, race/ethnicity, education, and food insecurity status; only adjusted models are shown in tables. At Site A, the mean HEI-2010 score for the food selected by clients at baseline was 54.13, which increased to 65.90 following the intervention (p<0.0001 for difference). There were statistically significant increases in five of the twelve subcomponents: total vegetables (p<0.002), whole grains (p<0.04), fatty acid ratio (p<0.0008), sodium (p<0.0008) and empty calories (p<0.005). At Site B, there was no statistically significant difference in the total HEI-2010 score for the food selected by clients at baseline and follow-up (−0.86, p=0.72). Site B clients had a statistically significant increase only in the whole grain subcomponent scores (p<0.003).
Table 2.
Intervention Food Pantries’ Client-Level HEI-2010 Total and Component Scores at Baseline and Follow-up†
| Baseline (n =24, 29)‡ | Follow-up (n =30, 31) | ||
|---|---|---|---|
| Adjusted Mean (SE) | Adjusted Mean (SE) | p-value | |
| Total HEI-2010 score (0–100) | |||
| Site A | 54.13 (1.79) | 65.90 (1.91) | <.0001* |
| Site B | 56.97 (1.70) | 56.11 (1.65) | 0.72 |
| Total Vegetables (0–5) | |||
| Site A | 2.08 (0.19) | 2.99 (0.20) | 0.002* |
| Site B | 2.25 (0.30) | 2.01 (0.29) | 0.57 |
| Greens And Beans (0–5) | |||
| Site A | 2.39 (0.32) | 3.14 (0.34) | 0.12 |
| Site B | 1.4 (0.36) | 1.87 (0.35) | 0.36 |
| Total Fruit (0–5) | |||
| Site A | 1.33 (0.15) | 1.73 (0.16) | 0.08 |
| Site B | 2.21 (0.33) | 1.9 (0.31) | 0.51 |
| Whole Fruit (0–5) | |||
| Site A | 2.28 (0.22) | 2.62 (0.23) | 0.30 |
| Site B | 2.77 (0.35) | 2.7 (0.34) | 0.88 |
| Whole Grains (0–10) | |||
| Site A | 4.23 (0.48) | 5.71 (0.51) | 0.04* |
| Site B | 2.42 (0.59) | 5.02 (0.57) | 0.003* |
| Dairy (0–10) | |||
| Site A | 2.49 (0.26) | 2.63 (0.27) | 0.70 |
| Site B | 3.52 (0.56) | 3.04 (0.54) | 0.54 |
| Total Protein Foods (0–5) | |||
| Site A | 4.97 (0.03) | 4.95 (0.04) | 0.77 |
| Site B | 3.85 (0.26) | 3.88 (0.26) | 0.94 |
| Seafood And Plant Protein (0–5) | |||
| Site A | 2.83 (0.32) | 3.22 (0.34) | 0.48 |
| Site B | 2.15 (0.42) | 2.8 (0.41) | 0.29 |
| Fatty Acid Ratio (0–10) | |||
| Site A | 6.12 (0.42) | 8.34 (0.45) | 0.0008* |
| Site B | 7.55 (0.69) | 5.73 (0.67) | 0.07 |
| Sodium (0–10) | |||
| Site A | 4.64 (0.53) | 7.42 (0.57) | 0.0008* |
| Site B | 8.53 (0.59) | 8.09 (0.57) | 0.60 |
| Refined Grains (0–10) | |||
| Site A | 5.8 (0.53) | 5.77 (0.56) | 0.97 |
| Site B | 3.05 (0.66) | 2.14 (0.64) | 0.34 |
| Empty Calories (0–20) | |||
| Site A | 14.99 (0.55) | 17.36 (0.58) | 0.005* |
| Site B | 17.26 (0.60) | 16.94 (0.58) | 0.71 |
p<0.05
models adjusted for age, race, education, and food insecurity
(Site A n, Site B n)
Other client outcomes
At baseline, clients received an average of 34.0 kg (75.1 lbs) of food at their visit, and 30.6 kg (67.5 lbs) of food at follow-up. Increases in the servings of fruits and vegetables and whole grains were observed at both sites, although they were borderline statistically significant or not statistically significant. In models adjusted for age, race, education, food insecurity status, and household size, clients at Site A took on average 26.99 more servings of fruits and vegetables for their household at follow-up (p = 0.05) and 18.4 more servings of whole grains (p = 0.14). At site B, clients took on average 13.79 more servings of fruits and vegetables at follow-up (p = 0.42) and 11.54 more servings of whole grains (p =0.12). Clients did not report being more likely to purchase any of the 20 healthy food types in the next 3 months at follow-up. A follow-up only assessment indicated that 88% of clients noted positive changes in their overall satisfaction at the food shelf in the last 6 months.
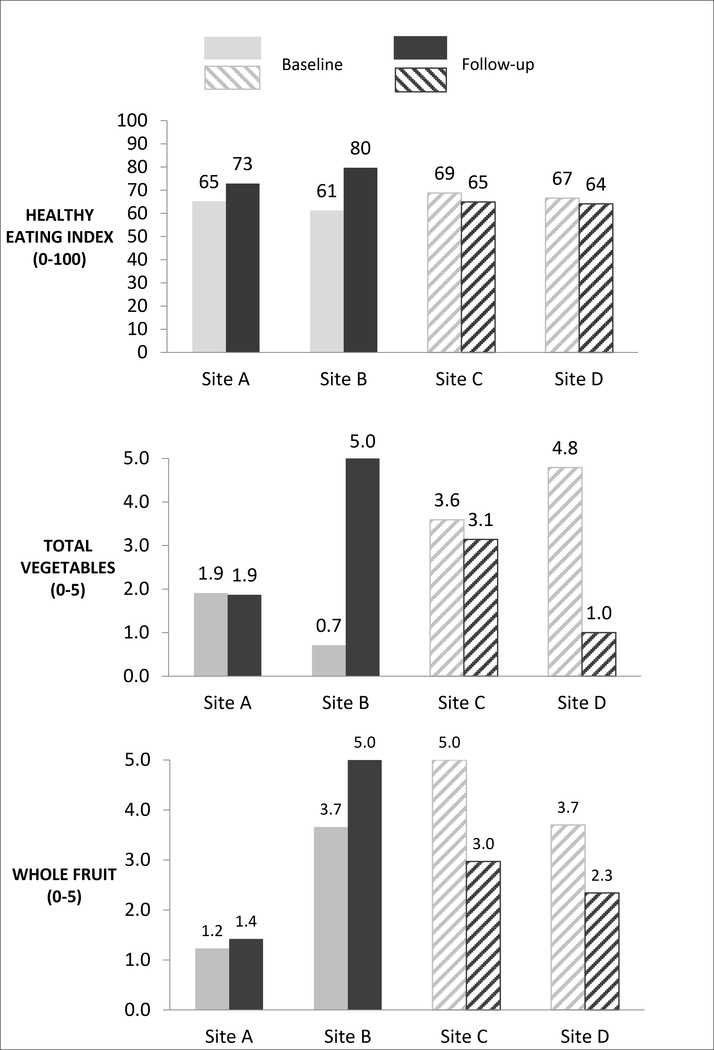
Pantry HEI-2010 scores
As presented in Figure 2, total HEI-2010 scores increased in both intervention pantries (8 points in Site A and 19 points in Site B). Total HEI-2010 scores decreased slightly in both control pantries (−4 points in Site C and −3 points in Site D). To further rule out seasonal effects, Figure 2 also displays changes in total vegetables and whole fruit, the subcomponents most likely to be affected by seasonal changes. These subcomponent scores stayed the same or increased in both intervention pantries while they decreased in both control pantries.
Figure 2:
Food Pantry Inventory Total HEI-2010 and Seasonal HEI-Component Changes
DISCUSSION
Our results suggest that, when well-implemented, the SuperShelf intervention has the potential to improve the nutritional quality of food available to and selected by clients at a high risk for food insecurity. Following the intervention, both pantries had improved the nutritional quality of the foods available to clients, increasing their Healthy-Eating Index-2010 scores by 8 points (Site A) and 19 points (Site B). In the two control sites assessed at the same time, there was a slight decrease in overall HEI-2010 scores, as well as a decrease in the seasonal subcomponent scores on the HEI-2010. Seasonal effects are, therefore, unlikely to account for the score increase observed in the intervention pantries. Implementation fidelity was higher at Site A than site B. Client behavior change also differed by site. At Site A, where fidelity scores were higher, client HEI-2010 scores increased by nearly 12 points on average, whereas there was no change at Site B.
The magnitude of the change in client nutrition-related outcomes at Site A is notable. A nearly 12-point increase in the nutritional quality of foods selected by clients was highly statistically significant even with a small sample size. In another intervention study among food pantry clients in the same metropolitan area,(23) total HEI-2010 for overall diet increased 7.6 points following a 6-week cooking and nutrition education class for clients. Compared with an educational approach, a behavioral economics approach requires substantially less client time and effort, but has been thought to produce small effects.(46) If the effects of certain strategies are, in fact, meaningful, then behavioral economics strategies could offer a less burdensome approach to behavior change. While the current study did not measure overall client diet as the cooking class study did, another key finding of our study was that the majority of clients received about half or more of their total food from the food pantry. Considering that: a) a large effect of the intervention on food selected was observed, and b) the food selected at pantries comprised a large portion of clients’ total diets, it is plausible that the SuperShelf intervention could improve the overall nutritional quality of food pantry client’s diets. This hypothesis remains to be formally tested.
Understanding SuperShelf implementation is clearly essential to the next phases of this work. The SuperShelf intervention occurs in two phases, first addressing the availability of healthy foods (supply), then addressing the appeal of those foods (demand); results from this study indicate that the first phase may be easier to implement than the second. The first phase is lengthy and gradual, mostly involving decision-making staff or volunteers who make food sourcing decisions. The second phase is more conspicuous for both food pantry staff and clients, involving a transformation of the physical space and the way that clients move through the pantry. With the support of SuperShelf consultants, both intervention sites were successful in implementing the first phase of the intervention, as indicated by the high stocking standard scores (demonstrating adequate varieties of healthy foods) and increases in total HEI-2010 scores (demonstrating an overall improvement in nutritional quality). Site A was, however, more successful in implementing the core physical transformation elements, even without branded signage at the time of follow-up. While attractive signage contributes to the overall appeal of the food shelf, signage does not appear to be among the most essential components of the intervention. This is an important consideration for food pantries as they prioritize the costs of transforming their space.
In planning for the next phase of work, the SuperShelf team has built a set of practices to better identify pantry “readiness” prior to initiating the transformation process. These efforts have become essential as statewide momentum for improving nutrition in food pantries grows rapidly in a diverse set of food pantries. To date, more than seventy pantries in Minnesota have applied to participate in SuperShelf transformations. Meanwhile, national organizations such as Feeding America are increasingly cultivating efforts to provide and nudge food-insecure families towards healthy foods 24,28 Given the current heterogeneity in food pantries in developed countries18,47, assuring a process for pantries to meet the prerequisites for interventions – beginning with adopting a choice-based model and then adopting other elements of client-centredness – will be essential for dissemination of models like SuperShelf. Tools currently exist to assist food pantries in these first steps48 and the SuperShelf study team is currently developing more advanced tools to promote readiness (e.g. specific trainings on cultural equity).
With this growth of interest in SuperShelf, rigorous evaluation of its effects on clients continues to be necessary. A group-randomized study evaluating the SuperShelf model is currently underway in sixteen food pantries. Applications to participate include written responses gauging organizational alignment with SuperShelf core values41, ensuring organizational commitment with a letter from the Board of Directors and site pre-visits. This larger study will address many of the limitations of the current study, including lack of site randomization, the lack of client-level data for control sites, the small number of participants included in the study, and low/variable fidelity. Finally, the larger study will measure client total diet as its primary outcome, comparing 24-hour dietary recall data among a cohort of clients followed over one year. Approaches such as normalization process theory49 and principles-focused evaluation50 will be used to continue to assess implementation and its challenges.
In conclusion, SuperShelf resulted in a more nutritious set of foods available to clients in food pantries, but increasing healthy food availability alone appeared to be insufficient for changing client food selection. Behavioral economics strategies that emphasize healthy food and de-emphasize less healthy food are well-suited to be used in pantries ready to make a transformation. Properly implementing these strategies in this small, pilot study resulted in substantial improvements in the nutritional quality of food that clients took home. Coupled with the fact that pantry clients receive a significant share of their total food from the pantry, this intervention has the potential to result in measureable improvements in diet among a group that carries a disproportionate burden of diet-related chronic disease. As interest in SuperShelf grows, efforts continue to facilitate its implementation, and rigorously evaluate its effect on client health outcomes.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge Liz Riley at Valley Outreach and Sarah Schmidt at The Food Group for their invaluable contribution to the conceptualization and development of this work, as well Laura Bohen and Nathan Hesse at the University of Minnesota-Extension for their critical role in carrying out food pantry transformations. We would also like to acknowledge Grace Borg and Kristi Fordyce for their efforts in collecting the data for this study.
FINANCIAL SUPPORT
Research reported in this publication was supported by the Duke-UNC USDA Center for Behavioral Economics and Healthy Food Choice Research (BECR). The content is solely the responsibility of the authors and does not necessarily represent the official views of BECR. The study sponsors had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL STANDARDS DISCLOSURE
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the University of Minnesota. Informed consent was obtained from all subjects. Consent was witnessed and formally recorded.
REFERENCES
- 1.Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household Food Security in the United States in 2016.; 2017. Accessed May 2, 2018 https://www.ers.usda.gov/webdocs/publications/84973/err-237.pdf?v=42979
- 2.Mabli J, Ohls J, Dragoset L, Castner L, Santos B. Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Insecurity. USDA Food and Nutrition Service; 2013. Accessed May 3, 2018 https://www.urban.org/sites/default/files/publication/28506/412065-How-Much-Does-SNAP-Reduce-Food-Insecurity-.PDF [Google Scholar]
- 3.Weinfeld N, Mills G, Borger C, et al. Hunger in America 2014. Feeding America; 2014. Accessed November 6, 2015 http://help.feedingamerica.org/HungerInAmerica/hunger-in-america-2014-full-report.pdf [Google Scholar]
- 4.Duffy P, Zizza C, Jacoby J, Tayie FA. Diet quality is low among female food pantry clients in Eastern Alabama. J Nutr Educ Behav. 2009;41(6):414–419. doi: 10.1016/j.jneb.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 5.Simmet A, Depa J, Tinnemann P, Stroebele-Benschop N. The Dietary Quality of Food Pantry Users: A Systematic Review of Existing Literature. J Acad Nutr Diet. 2017;117(4):563–576. doi: 10.1016/j.jand.2016.08.014 [DOI] [PubMed] [Google Scholar]
- 6.Seligman HK, Lyles C, Marshall MB, et al. A pilot food bank intervention featuring diabetes-appropriate food improved glycemic control among clients in three states. Health Aff Proj Hope. 2015;34(11):1956–1963. doi: 10.1377/hlthaff.2015.0641 [DOI] [PubMed] [Google Scholar]
- 7.Byker Shanks C Promoting Food Pantry Environments that Encourage Nutritious Eating Behaviors. J Acad Nutr Diet. 2017;117(4):523–525. doi: 10.1016/j.jand.2016.12.020 [DOI] [PubMed] [Google Scholar]
- 8.Long CR, Rowland B, Steelman SC, McElfish PA. Outcomes of disease prevention and management interventions in food pantries and food banks: protocol for a scoping review. BMJ Open. 2017;7(10):e018022. doi: 10.1136/bmjopen-2017-018022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross M, Campbell EC, Webb KL. Recent trends in the nutritional quality of food banks’ food and beverage inventory: Case studies of six California food banks. J Hunger Environ Nutr. 2013;8(3):294–309. doi: 10.1080/19320248.2013.816992 [DOI] [Google Scholar]
- 10.Shimada T, Ross M, Campbell EC, Webb KL. A model to drive research-based policy change: Improving the nutritional quality of emergency food. J Hunger Environ Nutr. 2013;8(3):281–293. doi: 10.1080/19320248.2013.821963 [DOI] [Google Scholar]
- 11.Campbell EC, Ross M, Webb KL. Improving the nutritional quality of emergency food: A study of food bank organizational culture, capacity, and practices. J Hunger Environ Nutr. 2013;8(3):261–280. doi: 10.1080/19320248.2013.816991 [DOI] [Google Scholar]
- 12.Campbell EC, Webb KL, Ross M, Crawford PB, Hudson H, Hecht K. Nutrition-Focused Food Banking. Institute of Medicine; 2015. Accessed November 16, 2015 http://healthyfoodbankhub.feedingamerica.org/resource/nutrition-focused-food-banking/ [Google Scholar]
- 13.Rochester JS, Nanney MS, Story M. Assessing foodshelves’ ability to distribute healthy foods to foodshelf clients. J Hunger Amp Environ Nutr. 2011;6(1):10–26. doi: 10.1080/19320248.2011.549363 [DOI] [Google Scholar]
- 14.Hoisington A, Manore MM, Raab C. Nutritional quality of emergency foods. J Am Diet Assoc. 2011;111(4):573–576. doi: 10.1016/j.jada.2011.01.007 [DOI] [PubMed] [Google Scholar]
- 15.Akobundu UO, Cohen NL, Laus MJ, Schulte MJ, Soussloff MN. Vitamins A and C, calcium, fruit, and dairy products are limited in food pantries. J Am Diet Assoc. 2004;104(5):811–813. doi: 10.1016/j.jada.2004.03.009 [DOI] [PubMed] [Google Scholar]
- 16.Nanney MS, Grannon KY, Cureton C, et al. Application of the Healthy Eating Index-2010 to the hunger relief system. Public Health Nutr. 2016;FirstView:1–9. doi: 10.1017/S136898001600118X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grannon KY, Hoolihan C, Wang Q, Warren C, King R, Nanney MS. Comparing the Application of the Healthy Eating Index– 2005 and the Healthy Eating Index–2010 in the Food Shelf Setting. Published online In Press. [Google Scholar]
- 18.Simmet A, Depa J, Tinnemann P, Stroebele-Benschop N. The Nutritional Quality of Food Provided from Food Pantries: A Systematic Review of Existing Literature. J Acad Nutr Diet. 2017;117(4):577–588. doi: 10.1016/j.jand.2016.08.015 [DOI] [PubMed] [Google Scholar]
- 19.Greer AE, Cross-Denny B, McCabe M, Castrogivanni B. Giving Economically Disadvantaged, Minority Food Pantry Patrons’ a Voice: Implications for Equitable Access to Sufficient, Nutritious Food. Fam Community Health. 2016;39(3):199–206. doi: 10.1097/FCH.0000000000000105 [DOI] [PubMed] [Google Scholar]
- 20.Verpy H, Smith C, Reicks M. Attitudes and behaviors of food donors and perceived needs and wants of food shelf clients. J Nutr Educ Behav. 2003;35(1):6–15. [DOI] [PubMed] [Google Scholar]
- 21.Campbell E, Hudson H, Webb K, Crawford PB. Food preferences of users of the emergency food system. J Hunger Environ Nutr. 2011;6(2):179–187. doi: 10.1080/19320248.2011.576589 [DOI] [Google Scholar]
- 22.Martin KS, Wu R, Wolff M, Colantonio AG, Grady J. A novel food pantry program: food security, self-sufficiency, and diet-quality outcomes. Am J Prev Med. 2013;45(5):569–575. doi: 10.1016/j.amepre.2013.06.012 [DOI] [PubMed] [Google Scholar]
- 23.Caspi C, Friebur R, Davey C, Nanney MS. Results of a pilot intervention to improve dietary outcomes among adults experiencing food insecurity. J Hunger Environ Nutr. Published online April 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feeding America Health & Hunger. Accessed January 3, 2018 https://hungerandhealth.feedingamerica.org/
- 25.Developing a Food Bank Nutrition Policy. Presented at the: Accessed November 6, 2015 http://www.mchnutritionpartners.ucla.edu/sites/default/files/CWH%20Food%20Bank%20Policy%20Online%20Course%20Mar%209%202015.pdf
- 26.Healthy Options Healthy Meals. Choose Healthy Options Program (CHOP) Implementation Guide. MAZON: A Jewish Response to Hunger and Greater Pittsbergh Community Food Bank; Accessed November 8, 2015 http://mazon.org/our-response/our-initiatives/healthy-options-healthy-meals/ [Google Scholar]
- 27.Webb K, Campbell E, Ross M, Vollmer L. Guide to Drafting a Food Bank Nutrition Policy. UC Berkeley Center for Weight and Health; 2015. [Google Scholar]
- 28.Nudges: Making the Healthy Choice the Easy Choice. Feeding America Accessed May 19, 2016 http://healthyfoodbankhub.feedingamerica.org/wp-content/uploads/mp/files/tool_and_resources/files/nudges-toolkit.pdf
- 29.Ashe M, Graff S, Spector C. Changing places: Policies to make a healthy choice the easy choice. Public Health. 2011;125(12):889–895. doi: 10.1016/j.puhe.2011.04.010 [DOI] [PubMed] [Google Scholar]
- 30.Roberto C, Kawachi I. Behavioral Economics and Public Health. Oxford University Press [Google Scholar]
- 31.Thaler Richard, Sunstein Cass. Nudge: Improving Decisions about Health, Wealth, and Happiness. Penguin Books; 2009. [Google Scholar]
- 32.Bucher T, Collins C, Rollo ME, et al. Nudging consumers towards healthier choices: a systematic review of positional influences on food choice. Br J Nutr. 2016;115(12):2252–2263. doi: 10.1017/S0007114516001653 [DOI] [PubMed] [Google Scholar]
- 33.Payne CR, Niculescu M, Just DR, Kelly MP. Shopper marketing nutrition interventions. Physiol Behav. 2014;136:111–120. doi: 10.1016/j.physbeh.2014.03.029 [DOI] [PubMed] [Google Scholar]
- 34.Skov LR, Lourenco S, Hansen GL, Mikkelsen BE, Schofield C. Choice architecture as a means to change eating behaviour in self-service settings: a systematic review. Obes Rev. 2013;14(3):187–196. doi: 10.1111/j.1467-789X.2012.01054.x [DOI] [PubMed] [Google Scholar]
- 35.Thorndike AN, Bright O-JM, Dimond MA, Fishman R, Levy DE. Choice architecture to promote fruit and vegetable purchases by families participating in the Special Supplemental Program for Women, Infants, and Children (WIC): randomized corner store pilot study. Public Health Nutr. 2017;20(7):1297–1305. doi: 10.1017/S1368980016003074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ammerman AS, Hartman T, DeMarco MM. Behavioral Economics and the Supplemental Nutrition Assistance Program: Making the Healthy Choice the Easy Choice. Am J Prev Med. 2017;52(2):S145–S150. doi: 10.1016/j.amepre.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 37.Richards MR, Sindelar JL. Rewarding Healthy Food Choices in SNAP: Behavioral Economic Applications. Milbank Q. 2013;91(2):395–412. doi: 10.1111/milq.12017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayala GX, D’Angelo H, Gittelsohn J, et al. Who is behind the stocking of energy-dense foods and beverages in small stores? The importance of food and beverage distributors. Public Health Nutr. 2017;20(18):3333–3342. doi: 10.1017/S1368980016003621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cureton C, King RP, Warren C, et al. Factors associated with the healthfulness of food shelf orders. Food Policy. 2017;71:124–131. doi: 10.1016/j.foodpol.2017.08.002 [DOI] [Google Scholar]
- 40.Wilson NLW, Just DR, Swigert J, Wansink B. Food pantry selection solutions: a randomized controlled trial in client-choice food pantries to nudge clients to targeted foods. J Public Health Oxf Engl. Published online May 12, 2016. doi: 10.1093/pubmed/fdw043 [DOI] [PubMed] [Google Scholar]
- 41.SuperShelf: Transforming food shelves to bring good food to all. SuperShelf. Accessed May 8, 2018 https://www.supershelfmn.org
- 42.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB, Basiotis PP. Development and Evaluation of the Healthy Eating Index-2005: Technical Report. Center for Nutrition Policy and Promotion, U.S. Department of Agriculture; 2007. Accessed February 10, 2016 http://www.cnpp.usda.gov/HealthyEatingIndex.htm [Google Scholar]
- 43.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–580. doi: 10.1016/j.jand.2012.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caspi CE, Grannon KY, Wang Q, Nanney MS, King RP. Refining and implementing the Food Assortment Scoring Tool (FAST) in food pantries. Public Health Nutr. 2018;21(14):2548–2557. doi: 10.1017/S1368980018001362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–32. doi: 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 46.Guthrie JF. Integrating Behavioral Economics into Nutrition Education Research and Practice. J Nutr Educ Behav. 2017;49(8):700–705.e1. doi: 10.1016/j.jneb.2016.09.006 [DOI] [PubMed] [Google Scholar]
- 47.Stroebele-Benschop N, Simmet A, Depa J. Nutrition Status of Those Receiving Unprepared Food from Food Banks: Overview of Food Bank Users in High-Income Countries and Their Diet In: Preedy V, Patel VB, eds. Handbook of Famine, Starvation, and Nutrient Deprivation: From Biology to Policy. Springer International Publishing; 2017:1–22. doi: 10.1007/978-3-319-40007-5_10-1 [DOI] [Google Scholar]
- 48.Healthy Client Choice. More Than Food. Accessed January 3, 2019 https://www.ittakesmorethanfood.org/getting-started-with-healthy-client-choice/
- 49.May C, Finch T. Implementing, Embedding, and Integrating Practices: An Outline of Normalization Process Theory. Sociol- J Br Sociol Assoc. 2009;43(3):535–554. doi: 10.1177/0038038509103208 [DOI] [Google Scholar]
- 50.Patton MQ. Principles-Focused Evaluation: The GUIDE. Guilford Press; 2018. Accessed June 6, 2018 https://www.guilford.com/books/Principles-Focused-Evaluation/Michael-Quinn-Patton/9781462531820/reviews [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.