Abstract
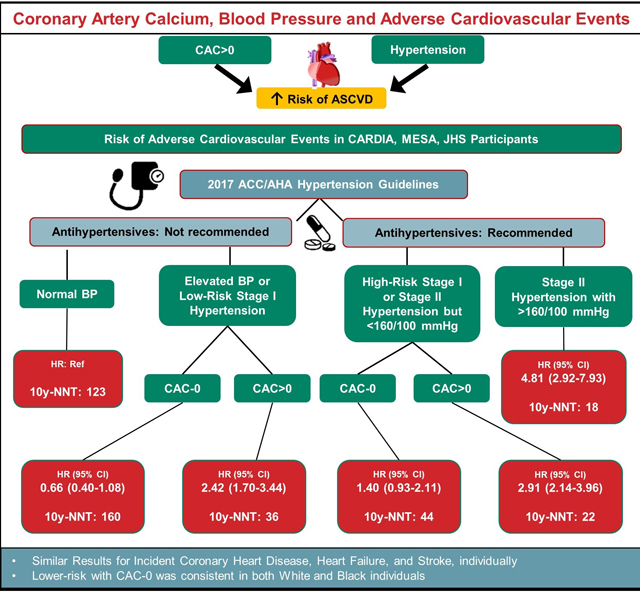
The 2017 ACC/AHA high blood pressure (BP) guidelines recommend risk assessment of atherosclerotic cardiovascular disease to inform hypertension (HTN) treatment in adults with elevated BP or low-risk stage I HTN. The use of coronary artery calcium (CAC) score to guide HTN therapy has not been adequately evaluated. Participants free of cardiovascular disease were pooled from Multi-Ethnic Study of Atherosclerosis, Coronary Artery Risk Development in Young Adults, and Jackson Heart Study. The risk for incident cardiovascular events (heart failure, stroke, coronary heart disease), by CAC status (CAC-0 or CAC>0) and BP treatment group was assessed using multivariable-adjusted Cox regression. The 10-year number needed to treat (NNT10) to prevent a single cardiovascular event was also estimated. This study included 6,461 participants (median age 53 years; 53.3% women; 32.3% Blacks). Over a median follow-up of 8.5 years, 347 incident cardiovascular events occurred. Compared with those with normal BP, the risk of incident cardiovascular event was higher among those with elevated BP/low-risk stage I HTN and CAC>0 (HR:2.4[95%CI:1.7–3.4]), and high-risk stage I/stage II HTN (BP:140–160/80–100mmHg) with CAC>0 (HR:2.9[95%CI:2.1–4.0]). A similar pattern was evident across racial subgroups and for individual study outcomes. Among those with CAC-0, the NNT10 was 160 for elevated BP/low-risk stage I HTN and 44 for high-risk stage I or stage II HTN (BP:140–160/80–100mmHg). Among those with CAC>0, the NNT10 was 36 and 22, respectively. Utilization of the CAC score may guide the initiation of HTN therapy and preventive approaches to personalize cardiovascular risk reduction among individuals where the current guidelines do not recommend treatment.
Keywords: Cardiovascular Risk, Coronary Artery Calcium, Coronary Heart Disease, Heart Failure, Hypertension, Outcomes, Stroke
Graphical abstract
Introduction
High blood pressure (BP) is associated with an increased risk of adverse cardiovascular events,1–3 and nearly half of the United States population across various age-groups have hypertension as per the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines.1–5 The stratification of patients based on the 10-year risk of adverse cardiovascular events using the ACC/AHA Pooled Cohort Equation has been proposed to guide the treatment of patients with elevated BP or low-risk stage I hypertension.2, 6 However, the equation does not accurately predict risk for atherosclerotic cardiovascular disease in racially diverse cohorts and provides only modest prognostic insight for risk stratification.7–9
The coronary artery calcium (CAC) score is a commonly used cardiac imaging marker that has been previously validated for predicting the risk of adverse cardiovascular events in multiethnic and racially diverse cohorts.10–13 The risk of cardiovascular mortality in hypertensive patients can be effectively assessed using the CAC score.10–13 However, the role of a CAC score of zero (CAC-0) to stratify the overall incident cardiovascular event risk, and specifically incident stroke, incident coronary heart disease (CHD), and incident heart failure in patients with previously untreated hypertension is not known.14 Furthermore, there are limited data on the role of CAC-0 to risk-stratify hypertensive patients within the racial sub-groups.14
We hypothesized that a CAC score of zero improves the adverse cardiovascular event risk stratification among individuals with elevated BP and low-risk stage 1 hypertension as per the 2017 ACC/AHA guidelines. We sought to evaluate the use of a CAC-0 score to evaluate the risk of adverse cardiovascular events in various strata of BP and to inform the appropriate use of BP-lowering medications in a multiethnic and diverse pooled cohort.
Methods
The data for this study were obtained from the National Heart, Lung, and Blood Institute (NHLBI) BioLINCC Data Repository and is available at https://biolincc.nhlbi.nih.gov/home/.
Study Population
The participant-level data was pooled from three prospective cohort studies: 1) the Coronary Artery Risk Development in Young Adults (CARDIA) Study,15 2) the Multi-Ethnic Study of Atherosclerosis (MESA),16 and 3) the Jackson Heart Study (JHS)17. In brief, the CARDIA study enrolled 5,115 Black and White individuals aged 18–30 years in 1985–1986 across 4 centers which included Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. The MESA is a multiethnic cohort study that enrolled 6,814 participants aged 45–84 years without any known cardiovascular disease between 2000–2002 in 6 United States communities. The JHS is a prospective cohort of 5,306 Black (3,883 with data available in NHLBI BioLINCC) individuals aged >20 years enrolled between 2000–2004 from the Jackson, Mississippi, tricounty area. In this study, we included participants from the three cohorts who were free of cardiovascular diseases (CHD, stroke, and heart failure) at baseline and had CAC scores available. We included the data from year 15 of CARDIA, visit 1 of MESA, and visit 2 of the JHS. We excluded individuals <40 years of age since the 10-year atherosclerotic cardiovascular disease (ASCVD) risk (estimated using pooled cohort equations) is recommended for use in adults ≥40 years of age. Given the objective of the study to assess the role of CAC to inform treatment initiation, we excluded individuals who were on antihypertensive treatment at baseline.
BP Measurements at Baseline
In the CARDIA study, the BP was recorded in the sitting position on the right arm using a Hawksley random-zero sphygmomanometer (WA Balm Co) after 5-minutes of rest. Measurements were repeated thrice at 1-minute intervals and the average of the last two readings was averaged. Similarly, in MESA, the BP was recorded in a seated position using Dinamap Pro-100 automated oscillometric sphygmomanometer after at least 5-minutes of rest. Three readings were taken and the average of the last two was used. In the JHS cohort, BP was recorded in the right arm in a sitting position using Hawksley random-zero sphygmomanometer after resting for at least 5-minutes. Two readings were recorded 1 minute apart and the average of the two readings was used.
Assessment of CAC Score
The CAC assessment protocols for participants of CARDIA, MESA, and JHS have been previously described.18–20 In brief, cardiac CT was performed using cardiac-gated electron-beam CT scanners (GE Imatron C-150XL, GE-Imatron, GE LightSpeed 16 Pro, GE LightSpeed Qxi, and Siemens Volume Zoom) at the respective study sites for the various cohorts. The images were viewed and scored as per standardized protocols using TeraRecon Aquarius Workstation (TeraRecon, Inc., San Mateo, CA).
Stratification Based on 2017 ACC/AHA Guidelines and CAC Score
The patients were classified as per the 2017 ACC/AHA BP treatment guidelines for antihypertensive medication initiation. The three broad groups included: 1) individuals with normal BP (<120/80 mmHg); 2) individuals with elevated BP (120–129/<80 mmHg) or low-risk stage I hypertension (130–139/80–89 mmHg); and 3) high-risk stage I hypertension (130–139/80–89 mmHg) or stage II hypertension (≥140/90 mmHg). The patients in the third group are recommended antihypertensive therapy under the current ACC/AHA guidelines. Based on the 2017 ACC/AHA guidelines, high-risk stage I hypertension was defined by additional features alongside BP cut-offs, which included any of the following: age ≥65 years with systolic BP ≥ 130 mmHg, diabetes mellitus, 10-year ASCVD risk ≥10% (estimated using pooled cohort equations), and having chronic kidney disease or estimated glomerular filtration rate <60 mL/min/1.72 m2. The pooled cohort equation for non-Hispanic Whites was used to compute the 10-year ASCVD risk in participants identifying as White, Hispanic, and Chinese Americans. For this study, besides the abovementioned treatment classification, the patients were further divided based on the presence of a CAC score of zero. The management of patients with BP ≥160/100 mmHg and those with normal BP is generally consistent across the multiple guideline recommendations, so they were not further stratified on the basis of CAC-0.21–23 The patients were classified into 6 overall groups: 1) normal BP; 2) elevated BP or low-risk stage I hypertension with CAC-0; 3) elevated BP or low-risk stage I hypertension with CAC>0; 4) high-risk stage I hypertension or stage II hypertension with BP <160/10 mmHg and CAC-0; 5) high-risk stage I hypertension or stage II hypertension with BP <160/10 mmHg and with CAC>0; 6) stage II hypertension with BP ≥ 160/100 mmHg (Figure S1). In sensitivity analysis for the primary outcome, we further stratified CAC score into the subgroups of CAC-0, CAC score 1–100, 100–400, and ≥400. In the additional sensitivity analysis, we further stratified those with normal BP into those with CAC-0 and CAC>0 (Figure S2).
Primary and Secondary Outcomes
The primary study outcome was a composite of the first occurrence of CHD (myocardial infarction, revascularization, or resuscitated cardiac arrest due to cardiac causes), stroke, or heart failure (HF). The secondary outcomes of interest were the individual outcomes of incident CHD, incident stroke, and incident HF. Expert panels in the respective cohorts adjudicated the individual study outcomes as described previously.24–27 The adjudication measures are detailed in Data Supplement.24–37
Statistical Analyses
The individual-level data were pooled, and the participants were categorized into the abovementioned groups. The baseline characteristics were summarized and compared using descriptive statistics. In brief, the continuous variables were summarized as the median and interquartile range (IQR) and compared using the Kruskal-Wallis test. Categorical data were summarized as counts and percentages and compared using the Chi-square test. Kaplan-Meier analyses were used to depict the cumulative incidence of the study outcomes stratified by antihypertensive therapy recommendation and CAC score and compared using the log-rank test. The follow-up time was censored at ten years since the ASCVD risk score estimated using the pooled cohorts equation predicts the risk of ASCVD till up to ten years. Multivariable-adjusted Cox regression models were used to assess the risk of the study outcomes across the various BP-CAC-based study groups, taking those with normal BP as the reference group. In the sensitivity analysis, we computed the risk of the primary and secondary study outcomes, taking those with normal BP and CAC-0 as the reference group. The analyses were repeated in the race-stratified sub-groups. The covariates in the model include age, sex, race, BMI, smoking status, diabetes mellitus, total cholesterol, statin use, high-density lipoprotein-cholesterol, study cohort, and chronic kidney disease. The interaction of race with the CAC-BP groups on the study outcomes was assessed using a multiplicative interaction term. The incidence rates across the various BP-CAC-based study groups in the overall population and across racial sub-groups were computed using Poisson regression models. The time-dependent area under the curve (AUC) was computed for 1) CAC-0 only; 2) 2017 ACC/AHA guidelines based study groups; and 3) CAC-BP-based study groups; as each one predicted the risk of the primary outcome. The Uno’s concordance statistic was computed to assess the change in risk prediction ability of the abovementioned three models. We also computed the 10-year number needed to treat (NNT10) to prevent the primary and secondary study outcomes in the overall population and in racial-subgroups. The NNT10 was computed assuming a 38% relative risk reduction in incident heart failure, 19% reduction in stroke, 17% reduction in CHD, and 25% relative risk reduction in the primary study outcomes based on the treatment effect of intensive BP control seen in the SPRINT trial.1, 6 Due to substantially smaller population counts and the relatively shorter follow-up periods in the Chinese American Americans and Hispanics, we did not compute NNT10 in this population. Based on prior data,13 we performed sensitivity analyses stratifying the population group by CAC score of 220. All statistical analyses were performed using SAS 9.4 (Cary, NC). All tests were two-sided with a significance level of 0.05.
Results
We identified 6,461 individuals free of incident cardiovascular disease. The median age was 53 (IQR: 45,64) years and the study population was composed of 53.3% females, 32.3% Blacks, 15.6% Hispanics, 8.9% Chinese American. Of them, ~66.0% (4,262), had a CAC score of zero. CARDIA, JHS, and MESA contributed 25.6%, 8.4%, and 66.0% of the study population, respectively. In our study, 54.8% had normal BP, 23.8% had elevated BP or low-risk stage I hypertension, 19.7% had high-risk stage I/ hypertension stage II with BP <160/100mmHg, and 1.7% had hypertension stage II with BP ≥160/100 mmHg (Table 1). The baseline patient characteristics of the study population stratified by the 2017 ACC/AHA high BP guideline-recommended treatment groups and CAC-0 status are described in Table 1. Participants with higher BP and those who were recommended antihypertensive therapy were relatively older, with a higher proportion of Blacks, Chinese Americans, and Hispanics, and had a higher prevalence of diabetes and obesity, and worse renal function (Table 1). The baseline participant characteristics of the study population with additional CAC based stratification of those with normal BP is described in Table S1.
Table 1.
Baseline Characteristics of the Study Population
| Characteristics | Normal BP | Elevated BP/Low-risk Stage 1 Hypertension | High-risk stage I/II Hypertension | Stage II Hypertension with BP >160/100 mmHg | P-value | |||
|---|---|---|---|---|---|---|---|---|
| CAC-0 | CAC>0 | CAC-0 | CAC>0 | |||||
| Number | 3,540 | 1,026 | 511 | 550 | 723 | 111 | ||
| Age (Years) | 50 (44–59) | 49 (44, 56) | 59 (51, 68) | 60 (50, 69) | 69 (62, 74) | 68 (59, 76) | <0.001 | |
| Female | 2028 (57.3) | 565 (55.1) | 184 (36.0) | 322 (58.6) | 270 (37.3) | 73 (65.8) | <0.001 | |
| Race | <0.001 | |||||||
| White | 1699 (48.0) | 380 (37.0) | 237 (46.4) | 144 (26.2) | 304 (42.1) | 33 (29.7) | ||
| Black | 996 (28.1) | 443 (43.2) | 150 (29.4) | 237 (43.1) | 211 (29.2) | 48 (43.2) | ||
| Chinese American | 326 (9.2) | 59 (5.8) | 46 (9.0) | 53 (9.6) | 80 (11.1) | 9 (8.1) | ||
| Hispanic | 519 (14.7) | 144 (14.0) | 78 (15.3) | 116 (21.1) | 128 (17.7) | 21 (18.9) | ||
| BMI (Kg/m2) | <0.001 | |||||||
| Normal | 1360 (38.4) | 238 (23.2) | 128 (25.1) | 121 (22.0) | 211 (29.2) | 30 (27.0) | ||
| Overweight | 1329 (37.5) | 392 (38.2) | 216 | 232 (42.3) | 289 (40.0) | 34 (30.6) | ||
| Obese | 848 (24.0) | 395 (38.5) | 167 (32.7) | 194 (35.3) | 222 (30.7) | 47 (42.3) | ||
| Waist Circumference (cm) | 90.5 (82, 100) | 95 (86, 104) | 97 (89, 107) | 97 (88, 106) | 98 (91, 107) | 100 (90, 108) | <0.001 | |
| Systolic BP (mmHg) | 108 (101, 113) | 126 (122, 131) | 126 (122, 129) | 140 (132, 159) | 141 (134, 150) | 169 (163, 177) | <0.001 | |
| Diastolic BP (mmHg) | 68 (62, 72) | 79 (73, 83) | 76 (70, 81) | 82 (73, 89) | 79 (73, 85) | 77 (71, 102) | <0.001 | |
| Total Cholesterol (mg/dL) | 189 (168, 213) | 194 (170, 216) | 197 (174, 221) | 198 (177, 223) | 198 (175, 223) | 195 (179, 229) | <0.001 | |
| LDL cholesterol (mg/dL) | 116 (95, 137) | 118 (97, 139) | 120 (99, 144) | 121 (101, 141) | 123 (103, 141) | 122 (104, 139) | 0.002 | |
| HDL cholesterol (mg/dL) | 50 (41, 60) | 50 (41, 60) | 47 (39, 59) | 48 (41, 60) | 47 (39, 58) | 52 (43, 62) | <0.001 | |
| Chronic Kidney Disease | 136 (3.8) | 15 (1.5) | 32 (6.3) | 53 (9.6) | 117 (16.2) | 20 (18.0) | <0.001 | |
| Diabetes Mellitus | 384 (10.9) | 63 (6.1) | 70 (13.7) | 190 (34.6) | 214 (29.6) | 32 (28.8) | <0.001 | |
| CAC Score | 0 (0, 0.9) | 0 (0, 0) | 49.5 (12, 203) | 0 (0, 0) | 91.1 (24, 320) | 19.4 (0, 173) | <0.001 | |
| Smoking Status | <0.001 | |||||||
| Never | 2,683 (75.8) | 743 (72.4) | 377 (73.8) | 428 (77.8) | 579 (80.1) | 92 (82.9) | ||
| Ex-Smoker | 398 (11.2) | 95 (9.3) | 60 (11.7) | 33 (6.0) | 65 (9.0) | 4 (3.6) | ||
| Current Smoker | 451 (12.7) | 184 (17.9) | 72 (14.1) | 88 (16.0) | 77 (10.7) | 14 (12.6) | ||
| Statin | 232 (6.6) | 44 (4.3) | 59 (11.6) | 42 (7.6) | 97 (13.4) | 9 (8.1) | <0.001 | |
| Study Outcomes | ||||||||
| Primary Outcome | 102 (2.9) | 20 (2.0) | 52 (10.2) | 36 (6.6) | 116 (16.0) | 21 (18.9) | <0.001 | |
| CHD | 72 (2.0) | 7 (0.7) | 35 (6.9) | 15 (2.7) | 74 (10.2) | 11 (9.9) | <0.001 | |
| Heart Failure | 26 (0.7) | 6 (0.6) | 14 (2.74) | 11 (2.0) | 31 (4.3) | 8 (7.2) | <0.001 | |
| Stroke | 18 (0.5) | 8 (0.8) | 9 (1.8) | 14 (2.6) | 29 (4.0) | 9 (8.1) | <0.001 | |
| Cohort | <0.001 | |||||||
| CARDIA | 1,090 (30.8) | 369 (36.0) | 61 (11.9) | 90 (16.4) | 26 (3.6) | 14 (12.6) | ||
| JHS | 244 (6.9) | 112 (10.9) | 55 (10.8) | 66 (12.0) | 57 (7.9) | 11 (9.9) | ||
| MESA | 2,206 (62.3) | 545 (53.1) | 395 (77.3) | 394 (71.6) | 640 (88.5) | 86 (77.5) | ||
Abbreviations: BP: Blood Pressure; BMI: Body mass index; CAC: Coronary Artery Calcium Score; CARDIA: Coronary Artery Risk Development in Young Adults Study; CHD: Coronary Heart Disease; GFR: Glomerular filtration rate; HTN: Hypertension; HDL: High-density lipoprotein; JHS: Jackson Heart Study; LDL: Low-density lipoprotein; MESA: Multi-Ethnic Study of Atherosclerosis.
Risk of Incident Adverse Cardiovascular Events
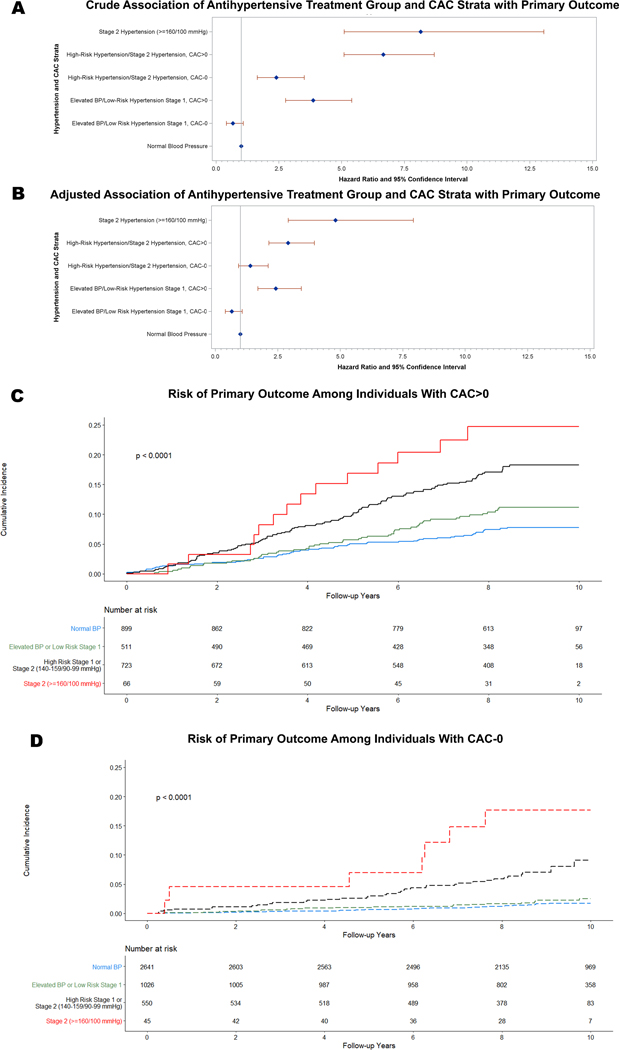
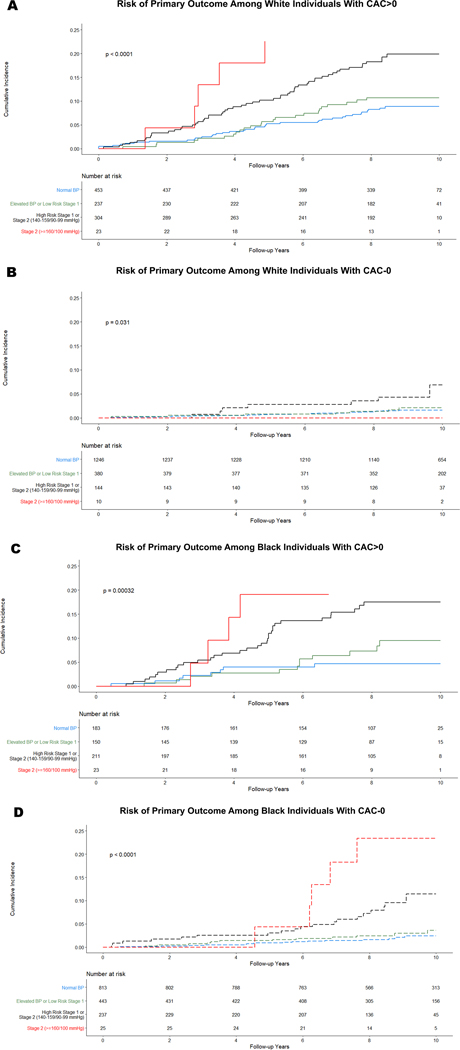
In our study population, there were 347 primary outcome events over a median follow-up period of 8.5 (IQR: 7.8–9.3) years. The event rate (per 1000-person years) for all study outcomes is described in Table 2. In multivariable-adjusted models, taking those with normal BP as the reference, the hazards for the incident adverse cardiovascular event was 0.66 (95% CI: 0.40–1.08), and 2.42 (95% CI: 1.70–3.44) in those with elevated BP/low-risk stage I hypertension, with CAC-0 and CAC>0, respectively. Similarly, taking those with normal BP group as the reference, the hazards for incident adverse cardiovascular event were 1.40 (95% CI: 0.93–2.11) and 2.91 (95% CI: 2.14–3.96) among those with high-risk stage I hypertension or stage II hypertension with BP <160/100 mmHg, with CAC-0 and CAC>0, respectively (Figure 1). The cohort stratified results for the primary outcome are presented in Table S3. The study outcomes were similar across racial subgroups (Figure 2, Table S4). There was no significant interaction of race and the CAC and BP-based risk stratification of the study outcomes (p>0.10). The time-dependent AUC curves for the prediction of risk of an incident cardiovascular event using classes of BP alone, CAC score alone, and CAC and high BP class combined are depicted in Figure S3. The Uno’s concordance statistic demonstrates that the combination of BP treatment classes with CAC-0 results in a significant improvement in the risk prediction for an incident cardiovascular event (p<0.001) than BP treatment classes or CAC-0 alone. Table S5 depicts the unadjusted and adjusted hazards for the primary outcome when those with CAC>0 were further stratified.
Table 2.
Incidence Rate of Study Outcomes: Stratified by Antihypertensive Treatment Group and CAC Score
| Study Population Groups | Normal Blood Pressure | Elevated BP/Low Risk Hypertension Stage 1, CAC-0 | Elevated BP/Low-Risk Hypertension Stage 1, CAC>0 | High-Risk Hypertension/Stage 2 Hypertension, CAC-0 | High-Risk Hypertension/Stage 2 Hypertension, CAC>0 | BP≥160/100 |
|---|---|---|---|---|---|---|
| Incidence per 1000 person-years (95% Confidence Interval) | ||||||
| Primary Outcome | ||||||
| Overall | 2.78 (2.28–3.38) | 1.85 (1.19–2.87) | 12.34 (9.40– 16.20) | 7.45 (5.37–10.32) | 22.18 (18.48–26.61) | 25.97 (16.87–39.96) |
| Whites | 2.81 (2.15–3.67) | 1.51 (0.72–3.17) | 11.33 (7.58– 16.93) | 4.85 (2.31– 10.17) | 24.21 (18.61– 31.49) | 27.43 (12.92– 58.25) |
| Blacks | 2.25 (1.49–3.39) | 2.61 (1.48–4.61) | 9.86 (5.62–17.31) | 9.08 (5.79– 14.23) | 21.74 (15.46–30.56) | 26.60 (14.42– 49.06) |
| JHS | 2.84 (1.19–6.82) | 2.59 (0.64– 10.42) | 10.21 (3.88– 26.87) | 8.88 (3.32–23.77) | 20.96 (10.52–41.79) | - |
| CARDIA | 1.05 (0.66–1.68) | 1.05 (0.47–2.34) | 5.64 (2.31–13.74) | 5.16 (2.46–10.85) | 21.31 (9.88– 45.95) | 28.98 (11.67–71.96) |
| MESA | 4.48 (3.58–5.60) | 2.79 (1.59–4.91) | 14.65 (10.88– 19.71) | 8.25 (5.59–12.19) | 22.35 (18.39 27.15) | 28.85 (17.65–47.17) |
| Coronary Heart Disease | ||||||
| Overall | 1.94 (1.54–2.46) | 0.65 (0.31–1.36) | 8.31 (5.96–11.56) | 3.10 (1.87– 5.15) | 14.27 (11.36– 17.92) | 13.60 (7.53– 24.56) |
| Whites | 2.28 (1.70–3.07) | 0.64 (0.21–2.00) | 8.40 (5.29– 13.35) | 0.68 (0.10–4.87) | 15.85 (11.48–21.91) | 18.80 (7.79–45.41) |
| Blacks | 0.88 (0.46–1.69) | 0.86 (0.32–2.29) | 4.88 (2.20–0.83) | 4.24 (2.20–8.16) | 12.69 (8.18–19.68) | 9.55 (3.62–25.20) |
| JHS | 0.57 (0.08–4.03) | - | - | 2.18 (0.30–15.67) | 10.01 (3.79–26.43) | - |
| CARDIA | 0.70 (0.40–1.24) | 0.35 (0.09–1.39) | 5.60 (2.30–13.65) | 2.92 (1.09–7.82) | 14.47 (5.86–35.69) | 4.86 (0.68–34.49) |
| MESA | 3.42 (2.65–4.41) | 1.15 (0.48–2.77) | 10.10 (7.07–14.43) | 3.26 (1.76–6.06) | 14.12 (11.08–17.99) | 16.95 (9.19–31.28) |
| Heart Failure | ||||||
| Overall | 0.72 (0.49–1.05) | 0.55 (0.25–1.23) | 3.18 (1.89–5.37) | 2.23 (1.24–4.02) | 5.60 (3.94–7.96) | 9.03 (4.52–18.05) |
| Whites | 0.46 (0.24–0.89) | 0.43 (0.11–1.71) | 1.80 (0.68–4.78) | 2.74 (1.03–7.29) | 6.1 (3.68–10.08) | 3.53 (0.50–24.89) |
| Blacks | 1.17 (0.66–2.06) | 0.87 (0.32–2.31) | 4.80 (2.15–10.67) | 2.78 (1.25–6.19) | 4.97 (2.48–9.97) | 12.23 (5.10–29.29) |
| JHS | 2.27 (0.85–6.06) | 1.29 (0.18–9.21) | 7.63 (2.47–23.57) | 4.35 (1.09–17.27) | 4.97 (1.24–19.87) | - |
| CARDIA | 0.23 (0.09–0.62) | 0.35 (0.09–1.39) | - | 1.43 (0.36–5.69) | 5.16 (1.27–20.81) | 10.16 (2.46–41.92) |
| MESA | 1.03 (0.65–1.64) | 0.69 (0.22–2.14) | 3.61 (2.01–6.51) | 2.27 (1.09–4.76) | 5.69 (3.90–8.29) | 9.88 (4.47– 21.87) |
| Stroke | ||||||
| Overall | 0.49 (0.31–0.79) | 0.74 (0.37–1.47) | 2.05 (1.07–3.94) | 2.84 (1.68–4.80) | 5.23 (3.64–7.52) | 10.64(5.51–20.52) |
| Whites | 0.36 (0.17–0.76) | 0.64 (0.21–2.00) | 1.81 (0.68–4.84) | 1.36 (0.34–5.45) | 4.86 (2.77–8.53) | 7.32 (1.80–29.72) |
| Blacks | 0.68 (0.32–1.43) | 0.86 (0.32–2.30) | 0.80 (0.11–5.63) | 3.27 (1.56–6.84) | 6.86 (3.82–12.34) | 12.86 (5.41–30.60) |
| JHS | 0.57 (0.08–4.03) | 1.29 (0.18–9.15) | 2.54 (0.36–17.69) | 2.17 (0.30–15.43) | 10.25 (3.85–27.33) | - |
| CARDIA | 0.23 (0.09–0.62) | 0.35 (0.09–1.38) | - | 2.17 (0.70–6.71) | 5.14 (1.28–20.62) | 22.82 (8.41–61.89) |
| MESA | 0.75 (0.43–1.28) | 1.16 (0.48–2.78) | 2.63 (1.32–5.23) | 3.25 (1.75–6.03) | 4.83 (3.22–7.26) | 8.49 (3.49–20.66) |
Abbreviations: BP: Blood Pressure; CAC: Coronary Artery Calcium Score; CARDIA: Coronary Artery Risk Development in Young Adults Study; MESA: Multi-Ethnic Study of Atherosclerosis; JHS: Jackson Heart Study.
Note: The missing data are due to the inability to compute the incidence rate because of a low event rate.
Figure 1. Risk of Adverse Cardiovascular Events: Stratified by Antihypertensive Treatment Group and CAC Score.
Panel A and Panel B represent the forest plots of crude and multivariable-adjusted hazard ratio (blue diamond) with the 95% confidence interval (red error bars). Panel C and Panel D represents the Kaplan-Meier curves for the risk of cardiovascular events stratified by coronary artery calcium score (CAC). The P-Values in the Kaplan Meier Curves represent the log-rank test.
Figure 2. Race-Stratified Risk of Adverse Cardiovascular Events by Antihypertensive Treatment Group and CAC Score.
Panel A and Panel B represent the Kaplan-Meier curves for the risk of cardiovascular events stratified by coronary artery calcium score (CAC) among White individuals. Panel C and Panel D represent the Kaplan-Meier curves for the risk of cardiovascular events stratified by CAC among Black individuals. The P-Values in the Kaplan Meier Curves represent the log-rank test.
In our sensitivity analysis, taking those with normal BP and CAC-0 as the reference, the risk of the primary outcome was higher in those with normal BP and CAC>0 (HR: 3.41 [95% CI: 2.23–5.23]), elevated BP/low-risk stage I hypertension and CAC>0 (HR: 4.74 [95% CI: 3.04–7.41]), high-risk stage I hypertension/stage II hypertension (BP<160/100 mmHg) and CAC-0 (HR:2.69 [95% CI: 1.65–4.40]), and high-risk stage I hypertension/stage II hypertension (BP<160/100 mmHg) and CAC>0 (HR: 6.05 [3.96–9.24]), and stage II hypertension with BP≥160/100 mmHg (HR:9.47 [95% CI: 5.35–16.76]) (Table S6, Figure S4). The incidence rate for all study outcomes for this sensitivity analysis is depicted in Table S7.
Risk of Incident Heart Failure, Stroke, and Coronary Heart Disease
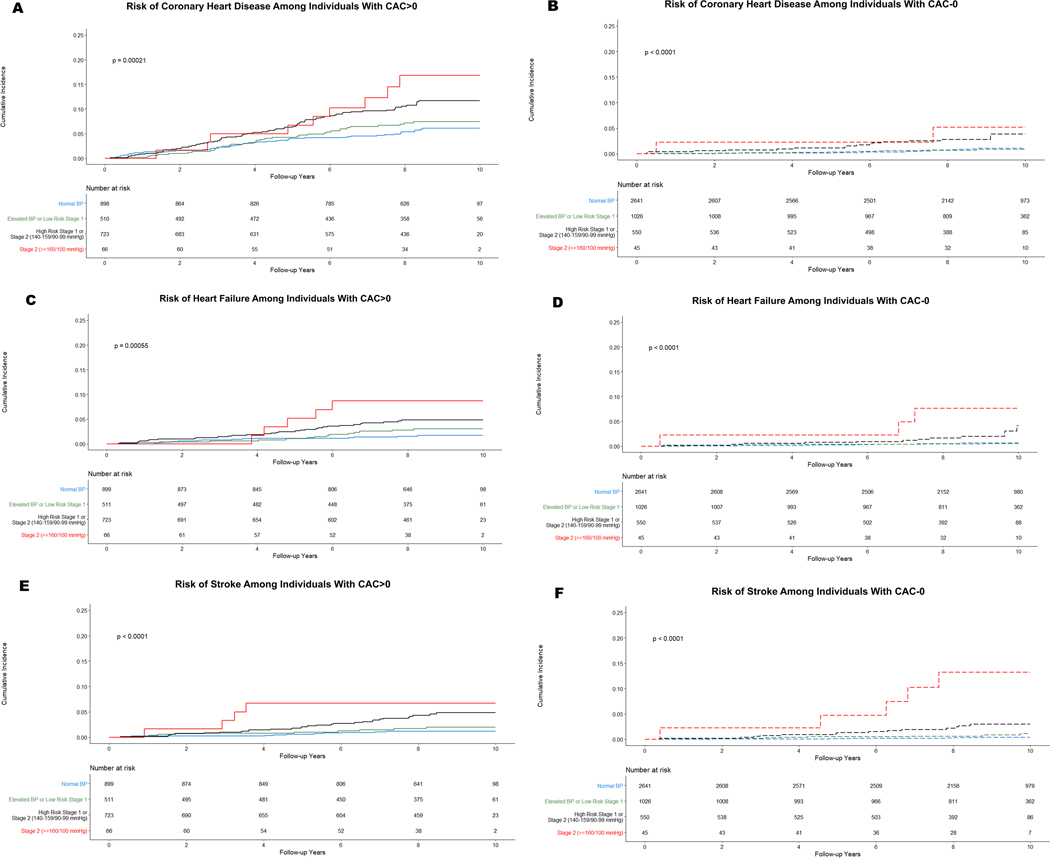
In our study cohorts, there were 96 HF events, 87 stroke events, and 214 CHD events. Controlling for covariates and taking those with normal BP as a reference, the risk of CHD was higher for those with elevated BP/low-risk stage I hypertension with CAC>0 (HR: 2.36 [95% CI: 1.55–3.60]), those with high-risk stage I hypertension/stage II hypertension (BP <160/100 mmHg) and with CAC>0 (HR: 2.64 [95% CI: 1.81–3.83]), and stage II hypertension with BP >160/100 mmHg (HR: 3.70 [95% CI: 1.89–7.25]) (Figure 3, Figure S5–S7). Those with elevated BP/low-risk stage I hypertension with CAC-0 had a lower risk of CHD (HR: 0.36 [95% CI: 0.17–0.79]) compared with those with normal BP. The risk of incident HF, compared with those having normal BP, was higher in individuals with CAC>0 and having low-risk elevated BP/stage I hypertension (HR: 2.15 [95% CI: 1.07–4.28]), those with high-risk stage I hypertension/stage II hypertension with BP <160/100 mmHg and CAC>0 (HR: 2.15 [95% CI: 1.20–3.83]), and stage II hypertension with BP >160/100 mmHg (HR: 3.90 [95% CI: 1.66–9.13]). The risk of incident stroke was higher in all BP treatment groups apart from those with CAC-0 and elevated BP/low-risk stage I hypertension (P<0.05 for all). The race stratified results for the HF, stroke, CHD outcomes are presented in Table S4. The incidence rate for the study outcomes across the BP and CAC-0 strata overall, in the racial subgroups, and by cohorts are depicted in Table 2.
Figure 3. Kaplan-Meir Curves for the Risk of Study Outcomes by Antihypertensive Treatment Group and CAC Score.
The figure represents the Kaplan-Meier curves for the risk of coronary heart disease (Panel A, B), heart failure (Panel C, D), and stroke outcome (Panel E, F) stratified by coronary artery calcium score (CAC). The P-Values in the Kaplan Meier Curves represent the log-rank test
In the sensitivity analysis, taking those with normal BP and CAC-0 as a reference, individuals with normal BP and CAC>0, elevated BP/low-risk stage I hypertension and CAC-0 or CAC>0, high-risk stage I hypertension/stage II hypertension (BP<160/100 mmHg) and CAC=0 or CAC>0, and those with stage II hypertension and BP ≥160/100 mmHg, had a higher risk of all secondary outcomes (Figure S8–S10, Table S6). The results of the sensitivity analyses using CAC score of 220 as cut-off are depicted in Table S8.
Number Needed to Treat to Prevent Incident Adverse Cardiovascular Events
Among patients with elevated BP/low-risk stage I hypertension (not recommended medication), the NNT10 for prevention of one incident adverse cardiovascular event was 160 and 36 in participants with CAC-0 and CAC>0, respectively. Among patients with high-risk stage I hypertension/stage II hypertension with BP <160/100 mmHg, the NNT10 for prevention of incident adverse cardiovascular events was 44 and 22 in participants with CAC-0 and CAC>0, respectively. The NNT10 for the primary outcome was 18 in those with BP ≥160/100 mmHg. For white participants with elevated BP/low-risk stage I hypertension, the NNT10 for preventing incident cardiovascular events was 193 and 37 in participants with CAC-0 and CAC>0, respectively. For Black participants with elevated BP/low-risk stage I hypertension, the NNT10 was 111 and 42. The NNT10 for prevention of incident adverse cardiovascular events in White participants with high-risk stage I hypertension/stage II hypertension with BP <160/100 mmHg was 58 and 20 in those with CAC-0 and CAC>0, respectively. In Black participants, the NNT10 for preventing incident cardiovascular event in those with stage I hypertension/stage II hypertension with BP <160/100 mmHg was 35 and 23 in those with CAC-0 and CAC>0, respectively. The NNT10 for preventing CHD, HF, and stroke across the various BP groups overall and among racial subgroups are depicted in Table 3.
Table 3.
Ten-Year Number Needed to Treat to Prevent One Study Outcome: Stratified by Antihypertensive Treatment Group and CAC Score
| Study Population Groups | Normal Blood Pressure | Elevated BP/Low-Risk Hypertension Stage 1, CAC-0 | Elevated BP/Low-Risk Hypertension Stage 1, CAC>0 | High-Risk Hypertension Stage 1/Stage 2 Hypertension, CAC>0 | High-Risk Hypertension Stage 1/Stage 2 Hypertension, CAC+ | BP≥160/100 |
|---|---|---|---|---|---|---|
| Primary Outcome | ||||||
| Overall | 123 | 160 | 36 | 44 | 22 | 18 |
| Whites | 114 | 193 | 37 | 58 | 20 | 18 |
| Blacks | 140 | 111 | 42 | 35 | 23 | 16 |
| Coronary Heart Disease | ||||||
| Overall | 259 | 679 | 79 | 155 | 50 | 49 |
| Whites | 214 | 608 | 73 | 841 | 45 | 36 |
| Blacks | 559 | 559 | 124 | 101 | 54 | 52 |
| Heart Failure | ||||||
| Overall | 315 | 405 | 86 | 64 | 55 | 31 |
| Whites | 480 | 452 | 143 | 57 | 49 | 82 |
| Blacks | 185 | 285 | 57 | 54 | 62 | 21 |
| Stroke | ||||||
| Overall | 895 | 477 | 268 | 177 | 108 | 56 |
| Whites | 1221 | 659 | 299 | 358 | 112 | 82 |
| Blacks | 568 | 326 | 568 | 132 | 85 | 41 |
Abbreviations: BP: Blood Pressure; CAC: Coronary Artery Calcium Score.
Discussion
In this pooled cohort study encompassing >6,000 individuals, we observed significant heterogeneity in the incident cardiovascular risk captured by CAC score across different strata of BP. We observed that nearly a third of individuals with elevated BP or low-risk stage I hypertension who are not recommended initiation of antihypertensive therapy as per the 2017 ACC/AHA guidelines have a CAC>0, which corresponds to a higher risk of incident cardiovascular events compared with those having normal BP. Nearly half of the individuals with high-risk stage I hypertension or with stage II hypertension have CAC-0. The presence of CAC was predictive of an increased risk of adverse cardiovascular events across population treatment groups and identified individuals who may benefit from antihypertensive therapy or being treated to intensive BP goal. Refining risk assessment with the CAC score across BP groups also predicted the risk of incident heart failure, stroke, and coronary heart disease. The risk prediction ability of CAC-0 for guiding antihypertensive therapy is retained across racial subgroups. CAC-0 was independently associated with a lower risk of adverse cardiovascular events, even among those with normal BP. Cumulatively, the study findings suggest that the use of CAC scores, when available, can assist with personalizing the initiation of antihypertensive therapy in individuals with elevated BP or low-risk stage 1 hypertension.
Prior investigations have assessed the role of CAC score for risk assessment in hypertensive individuals.13, 14 Previously, Uddin et al. identified high-risk patient populations comparable to the SPRINT trial using a CAC score cut-off of 220 who may be candidates for aggressive BP control strategy.13, 14 The prevalence of CAC>0 has been found to increase with higher BP levels even among young, low-risk individuals.38 The utility of CAC scores in a population with elevated BP or low-risk stage 1 hypertension to identify those in the intermediate phenotype having a higher risk of incident adverse cardiovascular event, stroke, coronary heart disease, and heart failure are not known.39 McEvoy et al.40 previously assessed the utility of CAC score in those with hypertension as per the Joint National Committee-8 (JNC-8) guidelines. However, a clinically aligned contemporary understanding of CAC score in guiding antihypertensive therapy in light of the SPRINT trial and the 2017 ACC/AHA recommendations across diverse racial groups is not known. Racial/ethnic differences in the prevalence and the prognostic ability of CAC scores have been previously reported.11, 41 While these studies investigated the independent predictive ability of CAC scores in the general population, the risk refinement performance of CAC score in the racial subgroups to guide the initiation of antihypertensive therapy are not known.11, 12, 42 Our study findings suggest that while racial/ethnic minorities are at a higher risk of adverse cardiovascular events, the risk refinement for the initiation of antihypertensive therapy guided by CAC score has prognostic utility across racial subgroups. In our study of American cohorts, we observed that nearly a third of those not currently recommended treatment have an elevated CAC score (CAC>0). Assuming a similar proportion at a national level, nearly 7.1 million adults from 21.4 million43 not currently recommended treatment would be eligible for antihypertensive therapy. Our study found that CAC-0 may be a tool to guide shared patient-physician decision making in providing a personalized approach to risk reduction in patients with elevated BP or hypertension, especially those who are not recommended treatment under the current ACC/AHA guidelines. The personalized risk reduction in those with CAC>0 may include a comprehensive approach including antihypertensive therapy, lipid-lowering therapy, and glycemic control, healthy diet, physical activity, and smoking cessation.
The NNT10 for treatment among those with CAC>0 who are currently not recommended antihypertensive therapy under the ACC/AHA guidelines was relatively low. This indicates that a substantial risk reduction may be achieved if these individuals are initiated on pharmacotherapy and undergo intensive BP treatment. Several risk reduction approaches may be used alongside pharmacotherapy that may provide a comprehensive cardiovascular risk reduction in patients with elevated CAC scores who are otherwise deemed to be at a low-risk based on traditional risk factors.27 The comparable NNT10 of those with an elevated CAC in the elevated BP or hypertension across racial groups highlights the plausible efficacy of global use of CAC score to identify the ideal candidates for intensive BP control. Many patients with high-risk stage I hypertension or stage II hypertension with BP <160/100 mmHg had CAC-0. While the underlying cardiovascular risk is not obfuscated by CAC-0 in these otherwise high-risk individuals, there may be an advantage in utilizing this clinical information for therapeutic decisions. Prior to the SPRINT trial, hypertension guidelines had used a higher therapeutic cut-off for elderly individuals, recognizing the limited evidence of aggressive BP control in older individuals.1 Although there may be a small subset of elderly patients with CAC-0, clinicians may consider not escalating antihypertensive therapy among those who cannot tolerate higher BP lowering doses, such as older individuals with orthostatic hypotension. Furthermore, optimizing BP treatment in patients already on anti-HTN therapies should be addressed in future work.
We also observed that those with a CAC-0 and elevated BP/low-risk stage I hypertension had a lower risk of CHD than those with normal BP and CAC >0. Furthermore, CAC>0 is independently predictive of increased adverse cardiovascular risk, even among those with normal BP. This indicates that the CAC score captures underlying subclinical cardiovascular pathological changes, even in the setting of relatively lower cardiovascular risk. This subclinical disease may be captured by CAC>0 despite normal BP levels. The CAC-0 based risk stratification may therefore have utility in the primordial prevention of a broad complex of cardiovascular risk factors beyond a single risk factor, such as BP only.44 Since CAC>0 captures an overall risk of atherosclerotic cardiovascular disease and other preventive therapies like statins may find utility in this population. There exists a “prevention paradox” wherein a reasonable proportion of individuals developing cardiovascular events are at a lower predicted risk of cardiovascular disease, and large scale preventive efforts are not targeted towards this group.45, 46 Although ascertainment of “normal” BP may be difficult, the findings from this study and prior investigations44, 47 suggest that even those with “normal” BP may have a relatively high cardiovascular event risk. Hence, CAC-0 may have a role in primary cardiovascular prevention by identifying patients with normal BP in whom intensification of preventive approaches such as lipid-lowering therapy, glycemic control, healthy diet, physical activity, and smoking cessation should be targeted. The role of the CAC score in primary prevention of cardiovascular disease is an active area of interest,48, 49 with recent data indicating elevated CAC score being associated with an increased risk of incident hypertension.50
There are several public health implications of our study. The CAC score is increasingly being integrated into the control of traditional cardiovascular risk factors, such as dyslipidemia.51 Consequently, the CAC score may be available for many primary care patients. Given the estimated additional ~30 million individuals identified with hypertension by the 2017 ACC/AHA guidelines, the supplementation of the guideline-recommended treatment with the CAC score-driven approach may help in identifying those at the highest cardiovascular risk. This approach, in conjunction with other approaches such as blood biomarker-based strategy (N-terminal-pro-B-type natriuretic peptides and cardiac troponin) 6, 52 or use of other imaging markers (carotid ultrasound), may help amplify absolute cardiovascular risk reduction through personalized antihypertensive therapy.53 Further investigation is needed to compare the incremental benefit of CAC score-guided and biomarker-guided antihypertensive therapies. CAC-based therapeutic risk-stratification is an established, cost-effective approach to reduce adverse cardiovascular event risk. 54 Similarly, intensive BP control is a cost-effective risk reduction approach.55 Combining the CAC score-guided cardiovascular risk reduction and intensive BP control, especially in those at a presumed low cardiovascular risk and no pharmacotherapy recommendation under the current guidelines, may prove to be a cost-effective approach. The advantage of cardiovascular risk reduction through control of BP has been established across various patient substrates.47 However, the CAC score may inform the shared patient-physician therapeutic decision-making process in situations where there are limitations to aggressive antihypertensive treatment.53 There may also be clinical utility in the use of CAC score in the assessment of “residual” cardiovascular risk in patients adequately treated as per the ACC/AHA guidelines. This must be balanced against the risks associated with radiation exposure in the context of universal CAC screening among those with elevated BP or stage I hypertension.56 Also, this study does not advocate for universal CAC score-based screening of patients but rather use this important imaging biomarker when available.
Our study has several limitations. There are inherent differences in the composition and characteristics of the cohorts as the participants were recruited in different regions across the US. To account for these differences, we included the respective cohort as an adjustment covariate in our analyses. There were also temporal and procedural variations in the assessment of BP across the three cohorts. However, all cohorts recorded multiple BP readings in a sitting position, and we included the average of multiple measurements in our analysis. While we used multivariable-adjusted models in our analyses, residual confounding due to unmeasured confounders (such as BP measurement instruments) cannot be ruled out due to observational study design. The NNT10 was estimated in patients who were stratified according to the current guidelines. The study cohorts were initiated before the introduction of the current guidelines and there may not have been an incentive for intensification of antihypertensive therapy among participants during the follow-up period. Lastly, our findings may need verification in the setting of a randomized clinical trial to assess the efficacy of CAC score-guided management of hypertension compared with the current guideline-based practice.53 Prospective investigations are needed to assess the benefits, costs, and potential harms of CAC scans for a CAC score based approach to guide hypertension management.
Perspectives
The CAC score is an effective tool to identify individuals across racial subgroups with elevated BP or low-risk stage I hypertension who are at a higher risk of incident CHD, stroke, heart failure, and adverse cardiovascular events and may benefit from antihypertensive pharmacotherapy. Refinement of risk assessment using the CAC score may help identify additional candidates who may benefit from antihypertensive therapy.
Supplementary Material
Novelty and Significance.
What is New?
Nearly a third of individuals with elevated blood pressure (BP) or low-risk stage I hypertension, who are not recommended treatment as per 2017 ACC/AHA high BP Guidelines, have an elevated coronary artery calcium score (CAC) score, which translates to a higher risk of adverse cardiovascular events.
What is Relevant?
Those with elevated BP/low-risk stage I hypertension and CAC>0 have a high-risk of incident coronary heart disease, incident heart failure, and incident stroke.
The increased adverse cardiovascular risk associated with CAC>0 was consistent in both White and Black individuals.
Summary
In the pooled cohort of over 6,000 participants, CAC>0 was independently predictive of increased adverse cardiovascular event risk across 2017 ACC/AHA hypertension guideline treatment groups and identifies individuals who may benefit from antihypertensive therapy or intensive BP control alongside comprehensive cardiovascular risk reduction approaches.
Acknowledgments
We would like to thank the participants of the CARDIA, MESA, and JHS Studies. We would like to thank the respective cohort investigators for making the data publically available through NHLBI BioLINCC.
Sources of Funding
This work was supported by the National Institutes of Health Mentored Patient-Oriented Research Award [5K23HL146887–02] to Dr. Pankaj Arora.
Footnotes
Disclosures
None of the authors had any conflicts of interest or financial disclosures to declare.
References
- 1.Wright JT Jr, Whelton PK, Reboussin DM. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2294. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, Wright JT Jr., 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation. 2018;138:e484–e594 [DOI] [PubMed] [Google Scholar]
- 3.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S. Heart disease and stroke statistics-2020 update: A report from the american heart association. Circulation. 2020;141:e139–e596 [DOI] [PubMed] [Google Scholar]
- 4.Kalra R, Parcha V, Patel N, Bhargava A, Booker KS, Arora G, Arora P. Increased awareness, inadequate treatment, and poor control of cardiovascular risk factors in american young adults: 2005–2016. Eur J Prev Cardiol. 2020:2047487320905190 [DOI] [PubMed] [Google Scholar]
- 5.Parcha V, Patel N, Kalra R, Arora G, Arora P. Prevalence, awareness, treatment, and poor control of hypertension among young american adults: Race-stratified analysis of the national health and nutrition examination survey. Mayo Clin Proc. 2020;95:1390–1403 [DOI] [PubMed] [Google Scholar]
- 6.Pandey A, Patel KV, Vongpatanasin W, Ayers C, Berry JD, Mentz RJ, Blaha MJ, McEvoy JW, Muntner P, Vaduganathan M, Correa A, Butler J, Shimbo D, Nambi V, deFilippi C, Seliger SL, Ballantyne CM, Selvin E, de Lemos JA, Joshi PH. Incorporation of biomarkers into risk assessment for allocation of antihypertensive medication according to the 2017 acc/aha high blood pressure guideline: A pooled cohort analysis. Circulation. 2019;140:2076–2088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, Ikram MA, Stricker BH, Hofman A, Franco OH. Comparison of application of the acc/aha guidelines, adult treatment panel iii guidelines, and european society of cardiology guidelines for cardiovascular disease prevention in a european cohort. JAMA. 2014;311:1416–1423 [DOI] [PubMed] [Google Scholar]
- 8.Rana JS, Tabada GH, Solomon MD, Lo JC, Jaffe MG, Sung SH, Ballantyne CM, Go AS. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol. 2016;67:2118–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeFilippis AP, Young R, Blaha MJ. Calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;163:68–69 [DOI] [PubMed] [Google Scholar]
- 10.Hecht H, Blaha MJ, Berman DS, Nasir K, Budoff M, Leipsic J, Blankstein R, Narula J, Rumberger J, Shaw LJ. Clinical indications for coronary artery calcium scoring in asymptomatic patients: Expert consensus statement from the society of cardiovascular computed tomography. J Cardiovasc Comput Tomogr. 2017;11:157–168 [DOI] [PubMed] [Google Scholar]
- 11.Orimoloye OA, Budoff MJ, Dardari ZA, Mirbolouk M, Uddin SMI, Berman DS, Rozanski A, Shaw LJ, Rumberger JA, Nasir K, Miedema MD, Blumenthal RS, Blaha MJ. Race/ethnicity and the prognostic implications of coronary artery calcium for all-cause and cardiovascular disease mortality: The coronary artery calcium consortium. J Am Heart Assoc. 2018;7:e010471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nasir K, Shaw LJ, Liu ST, Weinstein SR, Mosler TR, Flores PR, Flores FR, Raggi P, Berman DS, Blumenthal RS, Budoff MJ. Ethnic differences in the prognostic value of coronary artery calcification for all-cause mortality. J Am Coll Cardiol. 2007;50:953–960 [DOI] [PubMed] [Google Scholar]
- 13.Uddin SMI, Mirbolouk M, Kianoush S, Orimoloye OA, Dardari Z, Whelton SP, Miedema MD, Nasir K, Rumberger JA, Shaw LJ, Berman DS, Budoff MJ, McEvoy JW, Matsushita K, Blaha MJ, Graham G. Role of coronary artery calcium for stratifying cardiovascular risk in adults with hypertension. Hypertension. 2019;73:983–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinberg RL, Rubenfire M, Brook RD. Coronary artery calcium scoring in patients with hypertension. J Hum Hypertens. 2020;34:609–616 [DOI] [PubMed] [Google Scholar]
- 15.Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, Jacobs DR Jr,., Liu K, Orden S, Pirie P, et al. Recruitment in the coronary artery disease risk development in young adults (cardia) study. Control Clin Trials. 1987;8:68S–73S [DOI] [PubMed] [Google Scholar]
- 16.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR Jr., Kronmal R, Liu K, Nelson JC, O’Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–881 [DOI] [PubMed] [Google Scholar]
- 17.Taylor HA Jr., Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in african americans: Design and methods of the jackson heart study. Ethn Dis. 2005;15:S6–4-17 [PubMed] [Google Scholar]
- 18.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac ct in population-based studies: Standardized protocol of multi-ethnic study of atherosclerosis (mesa) and coronary artery risk development in young adults (cardia) study. Radiology. 2005;234:35–43 [DOI] [PubMed] [Google Scholar]
- 19.Carr JJ, Jacobs DR Jr., ,Terry JG, Shay CM, Sidney S, Liu K, Schreiner PJ, Lewis CE, Shikany JM, Reis JP, Goff DC Jr., Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol. 2017;2:391–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sung JH, Yeboah J, Lee JE, Smith CL, Terry JG, Sims M, Samdarshi T, Musani S, Fox E, Ge Y, Wilson JG, Taylor HA, Carr JJ. Diagnostic value of coronary artery calcium score for cardiovascular disease in african americans: The jackson heart study. Br J Med Med Res. 2016;11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr., ,Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr., Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (jnc 8). JAMA. 2014;311:507–520 [DOI] [PubMed] [Google Scholar]
- 22.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, Authors/Task Force M. 2018 esc/esh guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension: The task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension. J Hypertens. 2018;36:1953–2041 [DOI] [PubMed] [Google Scholar]
- 23.Whelton PK, Carey RM, Aronow WS, Casey DE Jr., , Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., , Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, Wright JT Jr., 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation. 2018;138:e426–e483 [DOI] [PubMed] [Google Scholar]
- 24.de Lemos JA, Ayers CR, Levine BD, deFilippi CR, Wang TJ, Hundley WG, Berry JD, Seliger SL, McGuire DK, Ouyang P, Drazner MH, Budoff M, Greenland P, Ballantyne CM, Khera A. Multimodality strategy for cardiovascular risk assessment: Performance in 2 population-based cohorts. Circulation. 2017;135:2119–2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Budoff MJ, Young R, Burke G, Jeffrey Carr J, Detrano RC, Folsom AR, Kronmal R, Lima JAC, Liu KJ, McClelland RL, Michos E, Post WS, Shea S, Watson KE, Wong ND. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ascvd) events: The multi-ethnic study of atherosclerosis (mesa). Eur Heart J. 2018;39:2401–2408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah RV, Spahillari A, Mwasongwe S, Carr JJ, Terry JG, Mentz RJ, Addison D, Hoffmann U, Reis J, Freedman JE, Lima JAC, Correa A, Murthy VL. Subclinical atherosclerosis, statin eligibility, and outcomes in african american individuals: The jackson heart study. JAMA Cardiol. 2017;2:644–652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gooding HC, Ning H, Gillman MW, Shay C, Allen N, Goff DC Jr., Lloyd-Jones D, Chiuve S. Application of a lifestyle-based tool to estimate premature cardiovascular disease events in young adults: The coronary artery risk development in young adults (cardia) study. JAMA Intern Med. 2017;177:1354–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McClelland RL, Jorgensen NW, Budoff M, Blaha MJ, Post WS, Kronmal RA, Bild DE, Shea S, Liu K, Watson KE, Folsom AR, Khera A, Ayers C, Mahabadi AA, Lehmann N, Jockel KH, Moebus S, Carr JJ, Erbel R, Burke GL. 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: Derivation in the mesa (multi-ethnic study of atherosclerosis) with validation in the hnr (heinz nixdorf recall) study and the dhs (dallas heart study). J Am Coll Cardiol. 2015;66:1643–1653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Longstreth WT Jr., Gasca NC, Gottesman RF, Pearce JB, Sacco RL. Adjudication of transient ischemic attack and stroke in the multi-ethnic study of atherosclerosis. Neuroepidemiology. 2018;50:23–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogunmoroti O, Oni E, Michos ED, Spatz ES, Allen NB, Rana JS, Virani SS, Blankstein R, Aronis KN, Blumenthal RS, Veledar E, Szklo M, Blaha MJ, Nasir K. Life’s simple 7 and incident heart failure: The multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Effoe VS, Wagenknecht LE, Echouffo Tcheugui JB, Chen H, Joseph JJ, Kalyani RR, Bell RA, Wu WH, Casanova R, Bertoni AG. Sex differences in the association between insulin resistance and incident coronary heart disease and stroke among blacks without diabetes mellitus: The jackson heart study. J Am Heart Assoc. 2017;6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keku E, Rosamond W, Taylor HA Jr., Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L, Sarpong D. Cardiovascular disease event classification in the jackson heart study: Methods and procedures. Ethn Dis. 2005;15:S6–62-70 [PubMed] [Google Scholar]
- 33.Kamimura D, Cain LR, Mentz RJ, White WB, Blaha MJ, DeFilippis AP, Fox ER, Rodriguez CJ, Keith RJ, Benjamin EJ, Butler J, Bhatnagar A, Robertson RM, Winniford MD, Correa A, Hall ME. Cigarette smoking and incident heart failure: Insights from the jackson heart study. Circulation. 2018;137:2572–2582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yano Y, Reis JP, Tedla YG, Goff DC Jr., Jacobs DR Jr., Sidney S, Ning H, Liu K, Greenland P, Lloyd-Jones DM. Racial differences in associations of blood pressure components in young adulthood with incident cardiovascular disease by middle age: Coronary artery risk development in young adults (cardia) study. JAMA Cardiol. 2017;2:381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reis JP, Auer R, Bancks MP, Goff DC Jr., Lewis CE, Pletcher MJ, Rana JS, Shikany JM, Sidney S. Cumulative lifetime marijuana use and incident cardiovascular disease in middle age: The coronary artery risk development in young adults (cardia) study. Am J Public Health. 2017;107:601–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nwabuo CC, Appiah D, Moreira HT, Vasconcellos HD, Yano Y, Reis JP, Shah RV, Murthy VL, Allen NB, Sidney S, Muntner P, Lewis CE, Lloyd-Jones DM, Schreiner PJ, Gidding SS, Lima JA. Long-term cumulative blood pressure in young adults and incident heart failure, coronary heart disease, stroke, and cardiovascular disease: The cardia study. Eur J Prev Cardiol. 2020:2047487320915342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang J, Chang Y, Kim S, Sung KC, Shin H, Ryu S. Increased burden of coronary artery calcium from elevated blood pressure in low-risk young adults. Atherosclerosis. 2019;282:188–195 [DOI] [PubMed] [Google Scholar]
- 39.Elshazly MB, Abdellatif A, Dargham SR, Rifai MA, Quispe R, Cainzos-Achirica M, Martin SS, Yeboah J, Psaty BM, Post WS, Nasir K, Budoff MJ, Blumenthal RS, Blaha MJ, McEvoy JW. Role of coronary artery and thoracic aortic calcium as risk modifiers to guide antihypertensive therapy in stage 1 hypertension (from the multiethnic study of atherosclerosis). Am J Cardiol. 2020;126:45–55 [DOI] [PubMed] [Google Scholar]
- 40.McEvoy JW, Martin SS, Dardari ZA, Miedema MD, Sandfort V, Yeboah J, Budoff MJ, Goff DC Jr., Psaty BM, Post WS, Nasir K, Blumenthal RS, Blaha MJ. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation. 2017;135:153–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaikh K, Nakanishi R, Kim N, Budoff MJ. Coronary artery calcification and ethnicity. J Cardiovasc Comput Tomogr. 2019;13:353–359 [DOI] [PubMed] [Google Scholar]
- 42.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345 [DOI] [PubMed] [Google Scholar]
- 43.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr., Whelton PK Potential us population impact of the 2017 acc/aha high blood pressure guideline. Circulation. 2018;137:109–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, Nasir K, Szklo M, Blumenthal RS, Blaha MJ. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol. 2020;5:1011–1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, Ellis SG, Lincoff AM, Topol EJ. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904 [DOI] [PubMed] [Google Scholar]
- 46.Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, Jacques PF, Rifai N, Selhub J, Robins SJ, Benjamin EJ, D’Agostino RB, Vasan RS. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–2639 [DOI] [PubMed] [Google Scholar]
- 47.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913 [DOI] [PubMed] [Google Scholar]
- 48.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Munoz D, Smith SC Jr., Virani SS, Williams KA Sr., Yeboah J, Ziaeian B 2019 acc/aha guideline on the primary prevention of cardiovascular disease: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation. 2019;140:e596–e646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Greenland P, Michos ED, Redmond N, Fine LJ, Alexander KP, Ambrosius WT, Bibbins-Domingo K, Blaha MJ, Blankstein R, Fortmann SP, Khera A, Lloyd-Jones DM, Maron DJ, Min JK, Muhlestein JB, Nasir K, Sterling MR, Thanassoulis G. Primary prevention trial designs using coronary imaging: A national heart, lung, and blood institute workshop. JACC Cardiovasc Imaging. 2020;S1936–878X(20)30650–1. doi: 10.1016/j.jcmg.2020.06.042. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 50.Sung KC, Lee MY, Kim JY, Park JB, Cho EJ, Avolio A. Prediction of incident hypertension with the coronary artery calcium score based on the 2017 acc/aha high blood pressure guidelines. Hypertens Res. 2020;43:1293–1300 [DOI] [PubMed] [Google Scholar]
- 51.Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72:434–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sandoval Y, Bielinski SJ, Daniels LB, Blaha MJ, Michos ED, DeFilippis AP, Szklo M, deFilippi C, Larson NB, Decker PA, Jaffe AS. Atherosclerotic cardiovascular disease risk stratification based on measurements of troponin and coronary artery calcium. J Am Coll Cardiol. 2020;76:357–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Greenland P, Michos ED, Redmond N, Fine LJ, Alexander KP, Ambrosius WT, Bibbins-Domingo K, Blaha MJ, Blankstein R, Fortmann SP, Khera A, Lloyd-Jones DM, Maron DJ, Min JK, Muhlestein JB, Nasir K, Sterling MR, Thanassoulis G. Primary prevention trial designs using coronary imaging. A National Heart, Lung, and Blood Institute Workshop. 2020:3554. [DOI] [PubMed] [Google Scholar]
- 54.Roberts ET, Horne A, Martin SS, Blaha MJ, Blankstein R, Budoff MJ, Sibley C, Polak JF, Frick KD, Blumenthal RS, Nasir K. Cost-effectiveness of coronary artery calcium testing for coronary heart and cardiovascular disease risk prediction to guide statin allocation: The multi-ethnic study of atherosclerosis (mesa). PLoS One. 2015;10:e0116377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z, Berlowitz DR, Conroy MB, Fine L, Oparil S, Morisky DE, Kazis LE, Ruiz-Negron N, Powell J, Tamariz L, Whittle J, Wright JT Jr., , Supiano MA, Cheung AK, Weintraub WS, Moran AE, Group SR. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377:745–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim KP, Einstein AJ, Berrington de Gonzalez A. Coronary artery calcification screening: Estimated radiation dose and cancer risk. Arch Intern Med. 2009;169:1188–1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.