Abstract
World Health Organization guidelines recommend that individuals living with HIV receive ≥6 months of isoniazid preventive therapy, including pregnant women. Yet, plasma isoniazid exposure during pregnancy, in the antiretroviral therapy era, has not been well described. We investigated pregnancy-induced and pharmacogenetic-associated pharmacokinetic changes and drug-drug-interactions between isoniazid and efavirenz in pregnant women. 847 women received isoniazid for 28 weeks, either during pregnancy or at 12 weeks postpartum, and 786 women received efavirenz. After adjusting for NAT2 and CYP2B6 genotype and weight, pregnancy increased isoniazid and efavirenz clearance by 26% and 15%, respectively. Isoniazid decreased efavirenz clearance by 7% in CYP2B6 normal metabolizers and 13% in slow and intermediate metabolizers. Overall, both isoniazid and efavirenz exposures were reduced during pregnancy, but the main determinants of drug concentration were NAT2 and CYP2B6 genotypes, which resulted in a 5-fold difference for both drugs between rapid and slow metabolizers.
Keywords: Pharmacokinetics, pregnancy, pharmacogenomics, drug-drug interaction
Introduction
HIV and tuberculosis are leading causes of morbidity and mortality among women of reproductive age, particularly among those living in low- and middle-income countries (LMIC)1,2. Pregnant women living with HIV have an increased susceptibility to TB infection and progression from latent TB infection to active disease3. To reduce the risk of HIV-associated TB, the World Health Organization (WHO) recommends 6 months of isoniazid preventive treatment (IPT) along with antiretroviral therapy4. This recommendation was also made for pregnant women, based on limited data. Both antiretrovirals and anti-TB regimens often include drugs that inhibit or induce liver enzymes, including cytochrome-P450 (CYP) isoenzymes, causing potential drug-drug interactions5. The situation is further complicated in pregnancy, which is associated with physiological changes, altered body weight and composition, changes in plasma protein concentrations, and other processes that can affect drug pharmacokinetics (PK)6–9.
The metabolism of both efavirenz (a commonly used antiretroviral to treat HIV) and isoniazid are affected by genetic polymorphisms in specific drug-metabolizing genes, and plasma drug levels can be further influenced by pregnancy. Studies to date, while small in number of participants and limited in geographic diversity have shown, a predicted 2-fold increase in CYP2B6 activity during pregnancy7. Dooley et al.10 observed a 19% increase in plasma efavirenz clearance during pregnancy compared to the postpartum period, and Olagunju et al.11 reported similar findings. Furthermore, an ancillary metabolic pathway of efavirenz, CYP2A6, is inhibited by isoniazid, thus potentially causing a drug-drug interaction12. There is currently little data regarding the effect of pharmacogenomics and pregnancy on isoniazid PK and on the drug-drug interaction between isoniazid and efavirenz in pregnancy and postpartum.
As part of the recently completely IMPAACT study P1078 TB APPRISE trial which investigated the safety and efficacy of administering IPT to pregnant women living with HIV, and reported a significantly higher rate of adverse pregnancy outcomes in women who received IPT during pregnancy13, we analyzed the key pharmacogenetic polymorphisms of efavirenz and isoniazid metabolism, the changes in the drug concentrations and PK of these two drugs during pregnancy, and their drug-drug interactions.
Methods
Participants and study design
This analysis used PK data collected in IMPAACT study P1078. The study design is reported in the primary manuscript13, summarised here and we report the PK procedure. IMPAACT study P1078 was a prospective, double-blind, placebo-controlled, randomized, noninferiority trial conducted in eight countries, and had a total of 13 sites. Local and collaborating institutional review boards approved the trial, and all women provided informed consent. Full details on ethics approval are provided in primary manuscript13.
HIV-positive pregnant women ≥ 18 years old were recruited if gestational age was 14 to 34 weeks, on WHO-recommended HIV treatment for prevention of mother-to-child transmission, weighing more than 35 kg. At study entry, women were randomized either to Arm A (immediate 28 weeks of 300-mg isoniazid daily treatment, then placebo) or Arm B (deferred isoniazid treatment, placebo until week 12 postpartum, then 28 weeks of 300-mg isoniazid). Adherence to isoniazid (or placebo) was monitored by self-report and pill count defined as the percentage of expected doses/pills taken during the entire treatment period, while ART adherence was self-reported.
Sample collection
Intensive samples were captured at pre-dose, 1, 2, 4, 6, 8, and 12 hours post-dosing, while sparse sampling occurred at least 2 hours post-dosing. Both sparse and intensive samples were captured on two visits; during pregnancy (between 28–40 weeks gestation) and week 16 postpartum (±4 weeks). Blood samples were centrifuged at 800 G for 10 minutes, and plasma was aliquoted into cryovials and immediately frozen at −70°C to await further processing. Plasma concentrations were determined by liquid chromatography-tandem mass spectrometry. Isoniazid calibration range from 0.105 to 25.0 mg/L, the inter-day accuracy and precision ranged from 92.2% to 104.5%, and 6.5% to 10.8%, respectively. Efavirenz calibration range from 0.0195 to 20.0 mg/L, the inter-day accuracy and precision ranged from 95.2% to 100.2%, and 3.2% to 11.3%, respectively.
Composite CYP2B6 genotype was defined based on combinations of four polymorphisms as follows: normal (1: 15582CC-516GG-983TT or 2: 15582CT-516GG-983TT); intermediate (3: 15582TT-516GG-983TT; 4: 15582CC-516GT-983TT; 5: 15582CC-516GG-983CT; 6: 15582CT-516GT-983TT; or 7: 15582CT-516GG-983CT); and slow metabolizer genotype (8: 15582CC-516TT-983TT; 9: 15582CC-516GT-983CT; 10: 15582CC-516GG-983CC, each with or without 11: −48GT; and 12: −48GG)14. Individuals with 983CC were considered ultra-slow metabolizers. (The term “normal” is used for consistency with standard nomenclature, not to suggest that others are abnormal.) For NAT2, genotypes were categorized based on combinations of rs1801279 (NAT2*14), rs1801280 (NAT2*5), rs1799930 (NAT2*6), and rs1799931 (NAT2*7), as slow, homozygous for the variant allele at any of the four loci (i.e., AA, CC, AA, AA, respectively), or heterozygous at 2 or more loci; intermediate, heterozygous at a single locus; or rapid, no variant allele at any locus (i.e., GG, TT, GG, GG, respectively)15,16. Genotyping was done in VANTAGE (Vanderbilt Technology for Advanced Genomics) using MassARRAY® iPLEX Gold (Agena Bioscience™, California, USA) and Taqman (ThermoFisher Scientific, Massachusetts, USA).
Data Analysis
Isoniazid and efavirenz concentrations were interpreted using population PK modelling using NONMEM version 7.4.317. Perl-speaks-NONMEM version 4.8.1, Pirana, and R with the package xpose4 were used to facilitate the model development process, data manipulation, and generation of model diagnostics18. To describe the PK of both isoniazid and efavirenz, one- and two-compartment models were tested with first-order absorption (with or without lag time or a chain of transit compartments), and first-order elimination. Since both drugs are mainly hepatically cleared, a well-stirred liver model19, was tested to capture the effect of first-pass metabolism. The liver hepatic blood flow Qh20 was assumed to be 90 L/h in a typical individual and adjusted for the effect of body size using allometric scaling21. The free fraction (fu) of efavirenz and isoniazid in plasma were fixed to 0.5%22 and 95%23, respectively. The pre-hepatic bioavailability of a typical individual was fixed to a reference value of 1.
The intensive data was used to develop the base model since these women were monitored closely, dosing was observed, and richer sampling schedule allowed for the identification of the structural model. This model was then used to explore the sparse data and identify implausible values, which were flagged as outliers and removed from model development analysis. An extreme value of conditional weighted residuals (CWRES)24, i.e., absolute value ≥ 4, was used as a criterion to identify outliers. Since CWRES values for data observations arising from the postulated model are assumed to be normally distributed, randomly obtaining an absolute value ≥ 4 has a probability of <0.00633%, only a chance of 1 out of 10,000. We assumed that pharmacokinetics of both drugs were at steady state at the time of PK visit unless participant had been on efavirenz for less than 16 days25, or missed dose in the previous 3 days had been reported.
Random effects at occasion- (each dose), visit- (each PK sampling visit), and/or subject-level were included on the pharmacokinetic parameters if statistically significant using a lognormal distribution. Between-occasion-variability (BOV) was tested on absorption parameters, while between-visit-variability (BVV) and between-subject-variability (BSV) were tested on disposition parameters. A combination of proportional and additive error was used to model unexplained residual variability.
Model development was guided by evaluating the drops in objective function value (ΔOFV) of nested models. The OFV was assumed as χ2-distributed, hence with a 3.84 drop in OFV being significant at p<0.05 for one additional parameter (i.e., 1 degree of freedom). Besides statistical significance, a set of diagnostic plots, including visual prediction checks (VPCs) and physiological plausibility of the results were considered in model development decisions.
Since enzyme metabolic status has been widely reported to critically affect pharmacokinetics of both drugs, NAT2 genotype effect on isoniazid clearance and CYP2B6 and CYP2A6 genotype on efavirenz clearance were tested early in model development process12,26. Allometric scaling was applied on all clearance and volume of distribution parameters27 to account for body size effect. Other covariate effects on the PK parameters, including pregnancy and drug-drug interaction, were investigated using a stepwise approach with forward inclusion (p<0.05) and backward elimination (p<0.01).
Concentrations below limit of quantification (BLQ) were handled similarly to M6 method by Beal28, to mitigate the effect of the M6 method imputation the additive error for the imputed values was inflated by LLOQ/2. Only subset of participants were included in the genotype study, those with missing genotypic information where assigned a phenotype using mixture model.29. Participants with missing weight and height were assigned the typical values depending on whether pregnant or postpartum. The original protocol focused on IPT, hence did not include capturing ART PK information (i.e. efavirenz dosing time) for sparse sampling. This was later amended, resulting in 32% of the women having a missing efavirenz dosing time in at least one PK visit during the early phase of the trial. Women with missing dose times during one visit were assumed to take medication at the same time throughout the trial consistently; therefore, dosing time of the recorded visit was imputed on the missing visit. For women with missing dosing time at both visits, a median dosing time (i.e., 20:30) from the data was imputed.
Results
Study profile
PK samples were available from 847 women on 300-mg isoniazid (748 of whom were treated with efavirenz (600mg dose), 80 with nevirapine, 17 with lopinavir, and 2 with atazanavir based ART). Of the 847 on isoniazid, 32 underwent intensive sampling (at pre-dose, 1, 2, 4, 6, 8, and 12 hours post-dosing), providing 300 observations, while 815 underwent sparse sampling (at least 2 hours post-dosing), providing 1015 observations, of which 88 were identified as implausible outliers (outliers were identified per the description in Methods) and were removed from the model building process. 210 women had isoniazid profiles available during both pregnancy and postpartum, since they had started isoniazid at a late gestational age such that their 28 weeks of isoniazid had not elapsed prior to their postpartum PK visit.
The number of participants on efavirenz in the different arms (isoniazid or placebo treatment) varied because of ART switching over the course of the study, but the majority were on efavirenz. Of 786 women on efavirenz, 21 underwent intensive sampling, providing 266 observations, and 765 underwent sparse sampling, providing 1363 observations, of which 15 were identified as implausible outliers (outliers were identified per the description in Methods) then removed from the model building process. Baseline characteristics of all women are summarised in Table 1.
Table 1:
Demographic, clinical, and laboratory characteristics of women on isoniazid and efavirenz during pregnancy and at postpartum.
| Characteristics (median and range, or n and %) | Participants in isoniazid PK analysis | Participants in efavirenz PK analysis | ||
|---|---|---|---|---|
| Pregnancy (n=420) | Postpartum (n=637) | Pregnancy (n=712) | Postpartum (n=670) | |
| Age (years) | 29 (18 – 45) | 29 (19 – 42) | 29 (18–45) | 29 (18–45) |
| Weight (kg) | 68 (39 – 167) | 62 (38 – 165) | 67 (42 – 164) | 61 (37 – 114) |
| Body mass index (kg/m2) | 27 (18 – 61) | 24 (16 – 45) | 27 (18 – 61) | 25 (16 – 49) |
| Gestation/postnatal age (weeks) at PK sampling time | 26 (14 – 34) | 16 (7 – 23) | 26 (14 – 34) | 16 (7 – 23) |
| Baseline Viral load (copies/mL) | <40 (<40 – 237000) | <40 (<40 – 465000) | <40 (<40 – 237000) | <40 (<40 – 465000) |
| Drug regimen | ||||
| On isoniazid | 420 (100%) | 637 (100%) | 352 (49%) | 540 (80%) |
| On efavirenz | 371 (88%) | 563 (88%) | 712 (100%) | 670 (100%) |
| On nevirapine | 11 (3%) | 47 (8%) | - | - |
| On lopinavir/ritonavir | 5 (1%) | 5 (1%) | - | - |
| On atazanavir/ritonavir | 2 (0%) | 2 (0%) | - | - |
| Days on EFV at PK sampling time | 125 (18 – 3800) | 264 (1 – 4228) | 125 (18 – 3800) | 408 (1 – 4228) |
| Drug metabolizing genotype | NAT 2 acetylation status | CYP2B6 metabolizer status | ||
| Rapid | 52 (12%) | 70 (11%) | 168 (24%) | 146 (22%) |
| Intermediate | 140 (33%) | 202 (32%) | 299 (42%) | 264 (40%) |
| Slow | 159 (39%) | 199 (31%) | 118 (16%) | 102 (15%) |
| Ultra-slow | - | - | 1 (0%) | 2 (0%) |
| Missing | 69 (16%) | 166 (26%) | 126 (18%) | 156 (23%) |
| CYP2A6 metabolizer status | ||||
| Normal | 501 (70%) | 439 (65%) | ||
| Intermediate | 81 (11%) | 71 (11%) | ||
| Slow | 4 (1%) | 4 (1%) | ||
| Missing | 126 (18%) | 156 (23%) | ||
210 women had isoniazid profiles during both pregnancy and postpartum.
596 women had efavirenz profiles available during both pregnancy and postpartum.
Distribution of drug metabolizer genotypes
The distribution of drug metabolizer genotypes for NAT2, CYP2B6, and CYP2A6 (classified into three phenotypes as described in the Methods), stratified by country, is illustrated in Figure 1. Rapid isoniazid acetylator NAT2 genotypes (had site range of 4% – 31%) were the least prevalent group in all 8 countries, which varied considerably by sites. Intermediate metabolizer CYP2B6 (had site range of 43% – 63%), were frequent in all countries genotypes as were CYP2A6 normal metabolizer genotypes (had site range of 76% – 93%).
Figure 1:
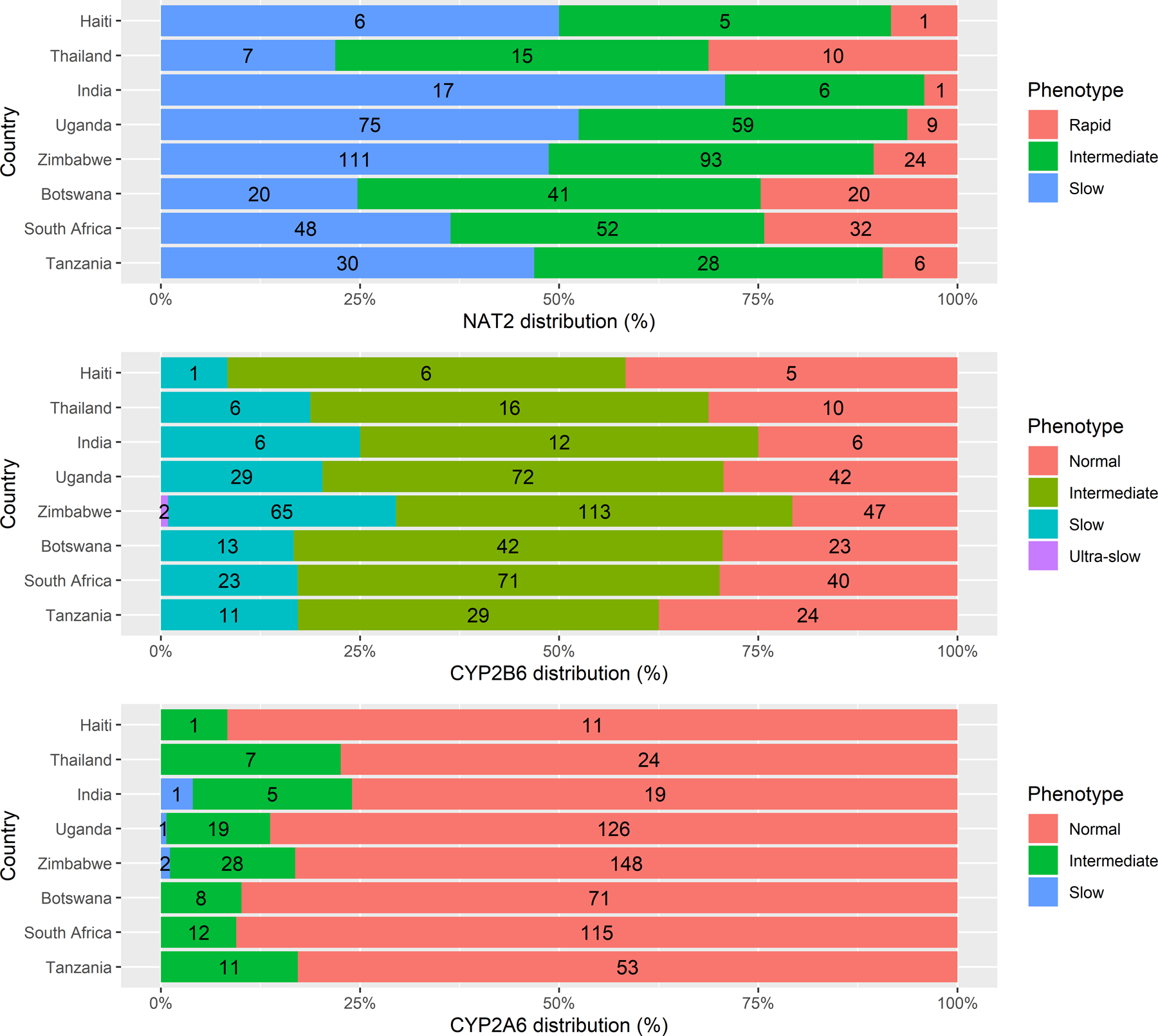
Distribution of the enzyme metabolizer genotypes for NAT2, CYP2B6, and CYP2A6 in the participants across the 8 countries involved in the study.
Structural model
A two-compartment disposition model best described the PK of both isoniazid and efavirenz with first-order-absorption through a chain of transit-compartments30. Drug elimination implemented with a well-stirred liver model19, was able to describe both hepatic clearance and first-pass extraction (EH) with the parameter of hepatic intrinsic clearance (CLint), as shown in Figure 2.
Figure 2:
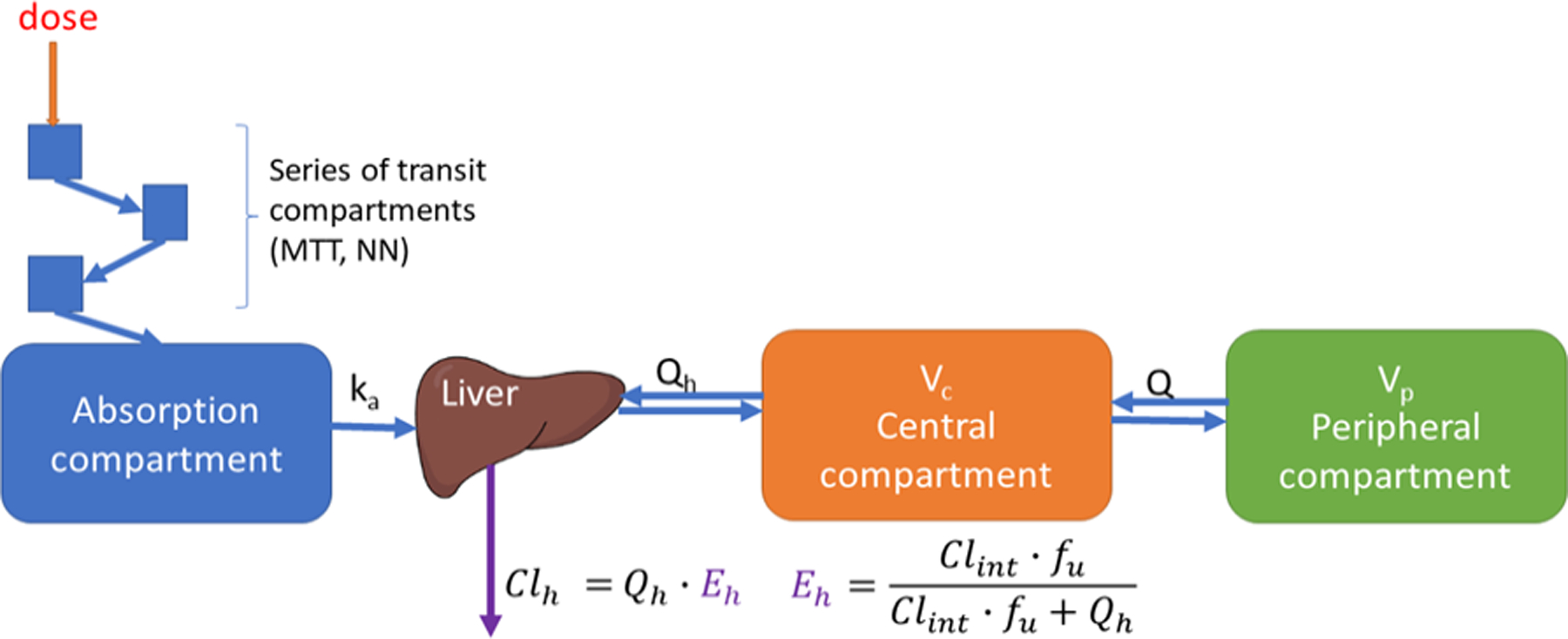
Schematic representation of the PK model of both efavirenz and isoniazid. The absorption is described with a series of transit-compartment to capture the delay in absorption, and a rate constant Ka. The hepatic extraction (Eh) is responsible for both first-pass metabolism and the systemic elimination with first-order kinetics. Vc represents the volume of distribution in the central compartment. Drug transfer between the central and peripheral compartment is defined by intercompartmental clearance Q/F, were F represents the oral bioavailability.
Isoniazid Pharmacokinetics - Covariate effects
Allometric scaling was applied to all clearance, volume, and liver parameters, to account for body size effect, improving the fit, and explaining part of between-subject variability (ΔOFV = −44). When fat-free mass replaced bodyweight for allometric scaling of clearance (but not volume) parameters, improved the fit of the model (ΔOFV = −6.27). NAT2 genotype significantly affected clearance of isoniazid (ΔOFV = −273, χ2 df=2 p ≪ 0.001), as CLint varied greatly between rapid, intermediate, and slow acetylators. After adjusting for body size and NAT2 genotype, pregnancy was found to increase clearance by 26% (ΔOFV = −49.6, χ2 df = 1 p ≪ 0.001). There was no significant difference in clearance between participants on the four different ART (efavirenz, nevirapine-, lopinavir/ritonavir-, and atazanavir/ritonavir-based) regimens (ΔOFV = −6.34, χ2 df = 3 p =0.0964). Inclusion of pregnancy on any other parameter, including the central compartment volume of distribution did not improve model fit. Parameter estimates for isoniazid are presented in Table 2.
Table 2:
Final PK parameter estimates for isoniazid
| Parameter | Typical Value (95% CIa) | Variabilityb, %CV (95% CIa) |
|---|---|---|
| CLintc (L/h) NAT2 Rapid | 72.3 (61.5 – 86.7) | 69.2 (64.2 – 74.2)* |
| CLintc (L/h) NAT2 Intermediate | 38.5 (34.6 – 43.2) | |
| CLintc (L/h) NAT2 Slow | 14.5 (13.1 – 16.0) | |
| Vcd (L) | 37.6 (33.9 – 40.7) | |
| Vpd (L) | 13.3 (10.5 – 16.9) | |
| Q/Fc (L/h) | 3.32 (2.53 – 4.54) | |
| ka (1/h) | 2.69 (1.91 – 3.51) | 145 (116 – 172)# |
| MTT (h) | 0.342 (0.209 – 0.459) | 116 (98.7 – 150)# |
| NN | 48.4 (22.2 – 83.8) | |
| QHc (L/h) | 90 FIXED | |
| fu (%) | 95 FIXED | |
| Prehepatic relative bioavailability | 1 FIXED | 12.3 (8.20 – 15.7)# |
| Proportional error (%) | 13.2 (11.3 – 15.3) | |
| Additive error (mg/L) | 0.0378 (0.0335 −0.0449) | |
| Pregnancy effect on CL (%) | +26.2 (19.8 – 33.2) |
Abbreviations: CLint clearance intrinsic; Vc apparent central volume of distribution for INH; VP apparent peripheral volume of distribution for INH; Q/F apparent intercompartmental clearance for INH; Ka first-order rate constant of INH absorption; MTT absorption mean transit time; NN Number of absorption transit compartment; QH blood liver flow40; fu unbound fraction of isoniazid in plasma50.
95% confidence intervals (CIs) were obtained with the SIR procedure
Variability was modelled with log-normal distribution and is presented as an approximate percentage CV.
Clearance parameters are allometrically scaled based on fat-free mass (typical value reported for 39 kg which was the median fat-free mass weight of the study population)
Volume pf distribution parameters are scaled based on weight (typical value reported for 67 kg which was the median weight of the study population).
Between subject variability.
Between occasion variability
Figure 3 displays the model-predicted individual exposures of isoniazid stratified by both NAT2 genotype and pregnancy status. The AUC0–24 of isoniazid boxplot shows that isoniazid exposure differs between the three genotypes, and decreased exposures were observed during antepartum compared to postpartum in all three genotypes. Combining all genotypes, the overall median (interquartile range) of isoniazid AUC0–24 antepartum was 8.05 (4.43–16.7) mg·h/L, compared to 11.1 (6.26 – 23.9) mg·h/L postpartum. Maximum concentrations (Cmax) during pregnancy and postpartum were 2.89 (1.97 – 4.13) mg/L and 3.69 (2.64 – 5.13) mg/L, respectively. The postpartum AUC0–24 was 1.4-fold greater compared to antepartum, while slow acetylator AUC0–24 was 5-fold greater compared to rapid acetylators. An isoniazid AUC0–24 of 10.52 mg∙h/L has been associated with 90% of early bactericidal activity in patients with active tuberculosis31.
Figure 3:
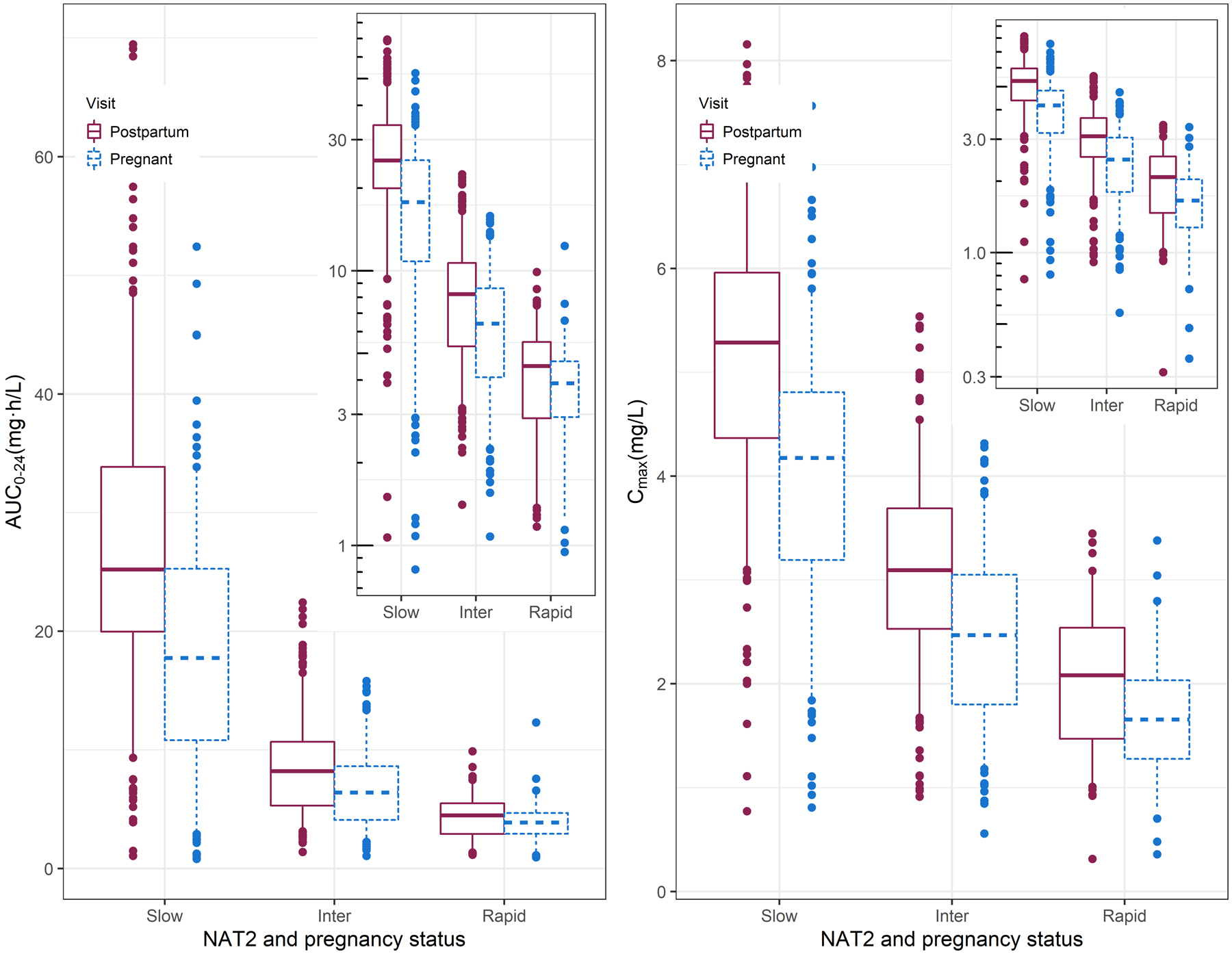
Isoniazid exposures stratified by NAT2 genotype and pregnancy. The box plot (with box representing median and inter-quartile range and whiskers the 5th-95th interval)) summarises isoniazid Cmax on the right and AUC0–24 on the left for the three genotypes (slow, intermediate, and rapid acetylator) for both the antepartum (red solid line) and postpartum (blue dashed lines) visit. AUC0–24 was calculated by integrating between the 0 and 24hr after dosing time points. The inset panel shows the same values on the log-scale.
Efavirenz pharmacokinetics - Covariate effects
Efavirenz had a structural model similar to isoniazid, except the first-order absorption rate constant (ka) was unstable when sparse and intensive data were pooled together; so, the value observed in the intensive PK data analysis was used as a fixed constant. Allometric scaling with bodyweight on all clearance and volume parameters improved the model fit and explained part of the between-subject variability (ΔOFV = −28.6). Using fat-free mass instead of total bodyweight for clearance (but not volume) parameters further improved the model (ΔOFV = −12.5). CYP2B6 genotype significantly affected the clearance of efavirenz (ΔOFV = −399, χ2 df = 2 p ≪ 0.001). After adjusting for body size and CYP2B6 genotype, pregnancy was found to increase the clearance of efavirenz by 16% (ΔOFV = −75.5, χ2 df = 1 p ≪0.001). Clearance in women co-administrated isoniazid and efavirenz was 7% lower in normal metabolizers and 13% lower in slow and intermediate metabolizers (ΔOFV = −39.2, χ2 df = 2 p ≪0.001) regardless of pregnancy status. Effect of CYP2A6 phenotype on the clearance and bioavailability of efavirenz was investigated among CYP2B6 slow metabolizers, in whom CYP2A6 may be more important for efavirenz clearance, but no significant effect was observed. Parameter estimates for efavirenz are presented in Table 3.
Table 3:
Final parameter estimates for efavirenz
| Parameter | Typical Value (95% CIa) | Variability, %CV (95% CI) |
|---|---|---|
| CLintric (L/h) CYP2B6 normal | 2690 (2300 – 3030) | 53.8 (48.9 – 59.2)* |
| CLintric (L/h) CYP2B6 intermediate | 1940 (1790 – 2100) | |
| CLintric (L/h) CYP2B6 slow | 545 (487 – 624) | |
| Vcd (L) | 135 (109 – 165) | |
| Vpd (L) | 512 (487 – 623) | |
| Q/Fc (L/h) | 26.9 (19.8 – 36.5) | |
| Ka (1/h) | 1.75 FIXED | 180 (114.9– 227)# |
| MTT (h) | 1.78 (1.20 – 2.39) | 131 (103– 166)# |
| NN | 48.4 (11.3 – 64.7) | |
| QHc (L/h) | 90 FIXED | |
| Fu (%) | 0.5 FIXED | |
| Prehepatic relative Bioavailability | 1 FIXED | 23.2 (20.7 – 26.1)# |
| Proportional Error (%) | 6.91 (4.72 – 9.45) | |
| Additive Error (mg/L) | 0.353 (0.303 – 0.408) | |
| Pregnancy Effect on CL (%) | +15.9 (9.75 – 21.9) | |
| INH effect on CL/F (L/h) in CYP2B6 Fast metabolizers (%) | −6.87 (−12.1 – −1.13) | |
| INH effect on CL/F (L/h) in CYP2B6 Inter and slow metabolizers (%) | −13.4 (−17.3 – −9.06) |
Abbreviations: CLint clearance intrinsic; Vc apparent central volume of distribution for INH; VP apparent peripheral volume of distribution for INH; Q/F apparent intercompartmental clearance for INH; Ka first-order rate constant of INH absorption; MTT absorption mean transit time; NN Number of absorption transit compartment; QH blood liver flow; fu unbound fraction of efavirenz in plasma.
95% confidence intervals (CIs) were obtained with the SIR procedure
Variability was modelled with log-normal distribution and is presented as an approximate percentage CV.
Clearance parameters are allometrically scaled based on fat-free mass (typical value reported for 39 kg which was the median fat-free mass weight of the study population)
Volume pf distribution parameters are scaled based on weight (typical value reported for 67 kg which was the median weight of the study population).
Between subject variability.
Between occasion variability
The model-predicted individual exposures are shown in Figure 4, where panels A and B stratify by CYP2B6 genotype and pregnancy status, while panel C and D stratify by CYP2B6 genotype and isoniazid co-administration. Figure 4 shows that efavirenz varied between the three genotypes, and panel A and B shows a decrease in exposures during pregnancy. The overall exposure of efavirenz was higher postpartum compared to pregnancy with median (interquartile range) postpartum AUC0–24 of 70.6 (47.9 – 118) mg·h/L, compared to 55.8 (38.6 – 92.7) mg·h/L antepartum. Concentrations at 12 hours post-dosing (C12) antepartum and postpartum were 2.18 (1.48– 3.68) mg/L and 2.69 (1.87 – 4.71) mg/L, respectively. Among normal CYP2B6 metabolizers 13 (9%) women had postpartum efavirenz C12 of <1 mg/L compared to 25 (15%) women antepartum.
Figure 4:
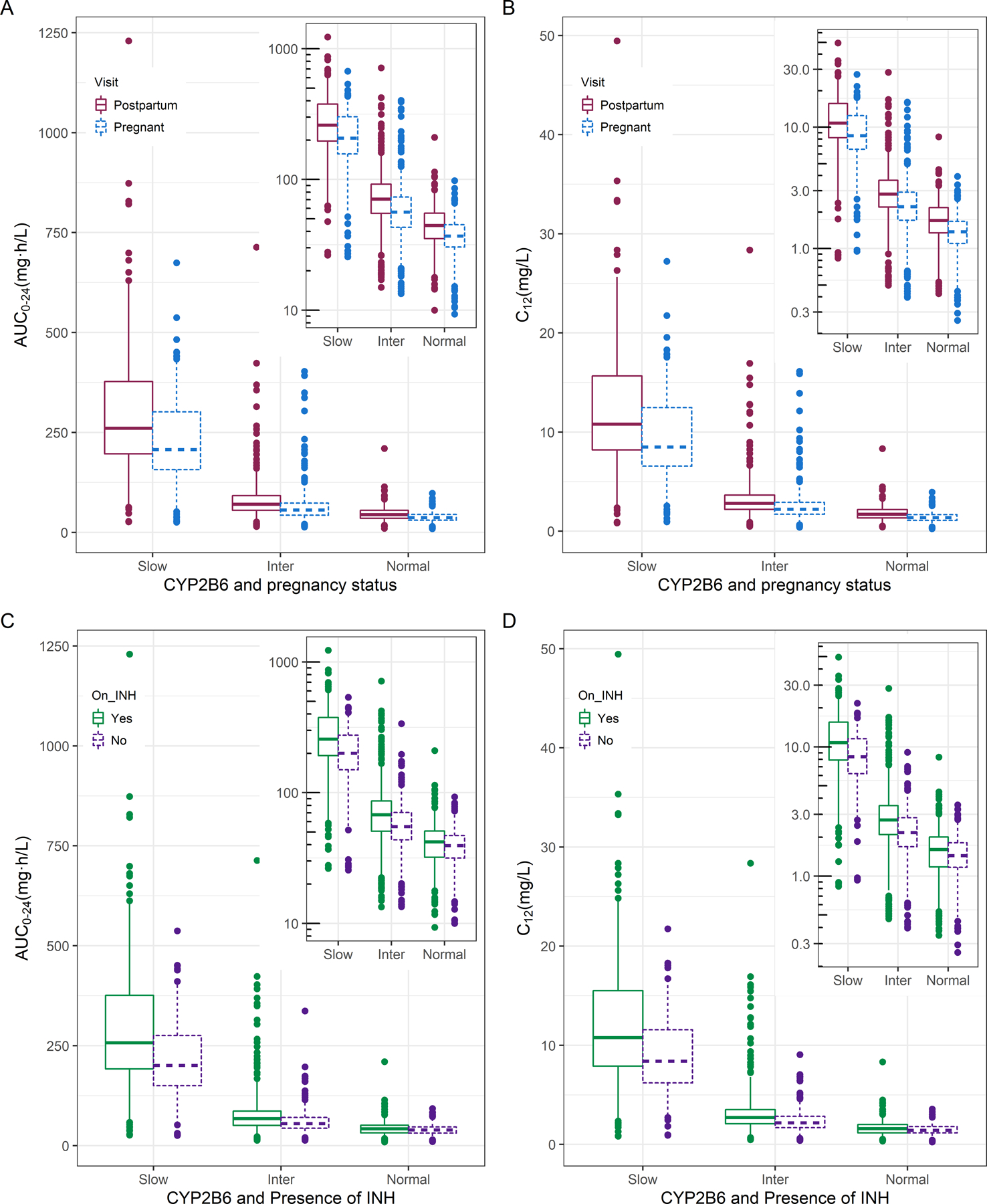
Efavirenz exposures stratified by CYP2B6 genotype, pregnancy and isoniazid co-administration Panel A and B displays box plot (with box representing median and inter-quartile range and whiskers the 5th-95th interval) summarizing AUC0–24 and C12 respectively for the three genotypes (slow, intermediate, and normal metabolizer) stratified by pregnancy (solid line) and postpartum (dashed lines) visit. While panel C and D stratify AUC0–24 and C12 respectively using INH co-administration
We observed a drug-drug interaction consisting of increased exposure of efavirenz in participants on concomitant isoniazid displayed in panel C and D of Figure 4. The difference in exposure in the slow and intermediate metabolizers was more apparent than in the normal metabolizers resulting in high concentration in slow CYP2B6 metabolizers. For example, choosing a threshold of 15 mg/L (similar to the upper quartile of C12 in CYP2B6 slow metabolizers co-administered isoniazid in Figure 4 panel D), among CYP2B6 slow metabolizers in the absence of isoniazid, efavirenz C12 was >15 mg/L in 4 (9%) individuals, compared to 45 (35%) individuals with presence of isoniazid. As a point of reference, a therapeutic range for plasma efavirenz concentrations of 1–4 mg/L has been suggested32, although concentrations somewhat <1 mg/L do not consistently predict treatment failure and concentrations >4 mg/L do not consistently predict toxicity. The overall median (interquartile range) of AUC0–24 was 66.8 (45.2 – 114) mg·h/L when isoniazid was present and 55.4 (39.7 – 98.1) mg·h/L when absent, corresponding to a 1.2-fold increase in efavirenz AUC0–24 due to the presence of isoniazid. All four panels in Figure 4 show that, while pregnancy and isoniazid affected efavirenz exposure, these effects were modest compared to CYP2B6 genotype, which resulted in a 5-fold difference between slow to normal metabolizers.
Discussion
We performed the largest study of its kind, assessing isoniazid and efavirenz PK, genetic polymorphisms, and drug-drug interactions in a geographic diverse population of pregnant and postpartum women living with HIV in high TB burden regions of the world. We show that pregnancy modestly increases the clearance of both isoniazid and efavirenz, therefore increasing the risk of low (and possibly sub-therapeutic) drug exposure during pregnancy. Notably, though we also show that drug metabolizer genotypes profoundly affect plasma exposure of these two drugs, to an extent far greater than of pregnancy. For this reason, the risk of lower plasma drug exposure during pregnancy is likely greatest only in women who are CYP2B6 normal metabolizers or NAT2 rapid acetylator, since they clear the drug faster compared to the other genotypes and are already exposed to lower concentrations. Additionally, we report that efavirenz exposure is increased by isoniazid co-administration, especially in CYP2B6 intermediate and slow metabolizers. Lastly, high concentration observed in slow CYP2B6 and NAT2 genotype increases the risk of adverse effects.
The increase in clearance of isoniazid and efavirenz may be due to several physiological changes related to pregnancy, e.g., plasma albumin levels6, bodyweight and composition, plasma volume9, hepatic blood flow9, and induction or inhibition of drug metabolising enzymes. The pregnancy-induced increase in weight was accounted for in the model using allometric scaling, while no unbound concentration was captured, therefore we could not confirm or disprove the effect of pregnancy on the protein-binding of efavirenz. Antepartum increase in hepatic blood9, potentially increase the hepatic clearance of drugs with high hepatic extraction ratio, this may be more apparent in low binding drugs like isoniazid compared to efavirenz. The other reason for changes in drug clearance during pregnancy is induction or inhibition of drug-metabolizing enzymes. Pregnancy increases the activity of CYP2B67 and CYP3A46 (major and minor route of efavirenz metabolism33). Tsutsumi et al.8 observed a reduction in NAT2 activity during pregnancy, but the reduction was clinically not significant. The reported clearance increase is modest compared to the large between-subject variability in drug exposure due to host genetics. However, these changes may be of relevance for rapid/normal metabolizers, who already experience lower exposure, as further increase in clearance might increase their risk for sub-therapeutic concentrations.
Similar to previous reports12,34,35, we observed a drug-drug interaction between isoniazid and efavirenz, as isoniazid decreases the clearance of efavirenz, particularly for intermediate and slow efavirenz metabolizers. This is thought to be due to isoniazid’s inhibition of CYP2A636. However, for individuals who are CYP2B6 slow metabolizers, CYP2A6 assumes increased importance in clearing efavirenz, so that CYP2B6 slow metabolizers on isoniazid may have a higher risk of efavirenz toxicity. Our analysis did not detect any difference in isoniazid exposure between different ARTs (efavirenz-, nevirapine-, lopinavir/ritonavir-, and atazanavir/ritonavir-based), which contrasts with previous reports37,38. However, it may be that our analysis was not powered to detect these differences since 88% of the participants were on efavirenz-based ART.
Previously reported isoniazid exposures varied widely between studies. This might be due to effects of large between-subject and -occasion variability, different proportions of NAT2 acetylator genotypes, different drug formulations, drug-drug interactions, and instability of isoniazid in plasma39, which makes PK studies of isoniazid somewhat challenging. This wide range is well summarised in a recent review by Daskapan et al.40. Comparing our results with previous reports on non-pregnant populations40–42, we observed lower exposures of isoniazid for both pregnancy and postpartum visits, while the ratio in exposures between slow and rapid NAT2 genotype was similar (clearance for rapid acetylators was observed to be 4-fold faster than those of slow acetylators). It is unclear if the relatively low concentrations we observed at both visits are due to efavirenz exposure, as most women were on efavirenz-based regimen. It is also possible that the effect of pregnancy on isoniazid clearance takes time to reverse fully, and women in the postpartum visit may also have clearance levels higher than the general (non-pregnant, adult) population. It has been previously discussed that using postpartum period as a control to study effects of pregnancy may be suboptimal because of factors that include lactation and delayed reversal of pregnancy-related physiological changes43. Efavirenz exposures in our study were in line with previous reports in non-pregnant individuals33,44,45. Similarly, the ratio between normal and slow CYP2B6 metabolizers exposures was similar, with a C12 ratio of five.
In our study, we report genotype frequencies from a large cohort of patients with wide geographical representation. A frequency of NAT2 slow acetylators above 50% worldwide has been reported46. Studies have shown greater than two-fold difference in the prevalence of NAT2 slow acetylators in agriculturists (slow acetylators more prevalent) compared to pastoralists in central Asian population and sub-Saharan African populations47. A pooled analysis by Sabbagh et al.46 shows the highest level of within-population diversity of NAT2 genotype in Africans. In our study population, NAT2 slow acetylators were most prevalent, followed by intermediate. Among CYP genes in humans, CYP2B6 is one of the most polymorphic gene48. A meta-analysis by Zhou et al.49 reported CYP2B6 normal metabolizer status in 61%, 38%, 76%, 45%, and 58% in Europeans, Africans, East Asians, South Asians, and admixed Americans respectively. In comparison, 65%, 65%, 31%, 66%, and 72% distribution of CYP2A6 normal functioning gene were reported in Europeans, Africans, East Asians, South Asians, and admixed Americans, respectively. In the present study, Intermediate followed by normal metabolizer CYP2B6 genotypes were frequent in all countries, as were CYP2A6 normal metabolizer genotypes.
Our study had some limitations, much of which we believe have been mitigated by use of a model-based approach analysis. Genotype data was not available in a subset of patients, 179 (21%) for isoniazid, and 173 (22%) for efavirenz, but this was addressed by imputation using a mixture model to assign individuals with missing information to a phenotype group. Blood draws during sparse sampling visits were scheduled for 2 hours after isoniazid dose. Because efavirenz is typically taken at night, this resulted in concentrations drawn 10–14 hours after efavirenz dose. Exact time of dose was not always reliably recorded for sparse sampling visits. For a portion of the study, timing of ART dosing was not recorded, so that information was imputed. While imputed data cannot be expected to be fully accurate, our approach was feasible to implement and expected to be robust since most women were taking efavirenz in the evening and were sampled the following morning, hence the slow terminal half-life (40 – 55 hours50) and accumulation of efavirenz minimized the impact of imprecise dosing time information. The uncertainty around self-reported or imputed dosing times and sampling schedule chosen for the sparse data may be the reasons for high variability observed in the absorption parameters, but this had a minor effect in our analysis since the structural model was built using the intensive data which had rich and reliable information for the entire PK profile. Similarly, the method we used for the identification and exclusion of implausible outlier values prevented these few samples from affecting the development of the PK models.
In conclusion, our study showed modest reductions in isoniazid and efavirenz exposure during pregnancy compared to postpartum. While the size of this effect is modest and unlikely to be of clinical significance for most patients, lower exposure may be important in normal CYP2B6 and rapid NAT2 acetylator, for whom the resulting concentrations may be sub-therapeutic, thus possibly leading to ineffective treatment and development of drug resistance. We also confirm the previously reported increased efavirenz exposure in individuals on concomitant isoniazid. This effect was overall modest but was most pronounced in CYP2B6 intermediate and slow metabolizers, who already had higher efavirenz levels and may therefore, be at higher risk of efavirenz-related toxicities.
Supplementary Material
Study Highlight.
What is the current knowledge on the topic?
Genetic variability greatly impacts isoniazid and efavirenz exposure, and it may affect interactions between these two commonly co-administered drugs. Very little knowledge is available on the effect of pregnancy on their PK.
What question did this study address?
We investigated the magnitude of pregnancy-induced changes in isoniazid and efavirenz pharmacokinetics, accounting for drug-drug-interactions and pharmacogenetics.
What this study adds to our knowledge?
Pregnancy increases clearance of isoniazid (by 26%) and efavirenz (by 15%), reducing both drugs exposures. Isoniazid co-administration reduces efavirenz clearance, and this reduction is larger in slow and intermediate CYP2B6 metabolizer.
How this might change clinical pharmacology or translational science
The modest pregnancy-related decreases in both drugs exposures may be of clinical importance in rapid NAT2 acetylator or CYP2B6 metabolizer, who already experience low exposure and are hence at risk of treatment failure. Isoniazid-induced increase in efavirenz exposure may raise the chance of toxicity amongst slow CYP2B6 metabolizers. Both findings suggest potential role for genetic testing and therapeutic-drug-monitoring.
Acknowledgement
The study team is very grateful to the women who participated in this study. We appreciate the contributions of the following individuals: Gary Maartens, and Marilyn Solomons from University of Cape Town. The IMPAACT team working at the sites in South Africa, Tanzania, Botswana, Zimbabwe, Uganda, Thailand, India, and Haiti. Kamunkhwala Gausi acknowledge her PhD funders, the Virtual consortium whose aim is to investigate the challenges of TB treatment for individuals on second-line ART whilst promoting African leadership and capacity building. Computations were performed using facilities provided by the University of Cape Town’s ICTS High Performance Computing team: hpc.uct.ac.za
Funding information
Overall support for the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT) was provided by the National Institute of Allergy and Infectious Diseases (NIAID) with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institute of Mental Health (NIMH), all components of the National Institutes of Health (NIH), under Award Numbers UM1AI068632 (IMPAACT LOC), UM1AI068616 (IMPAACT SDMC) and UM1AI106716 (IMPAACT LC), NICHD contract number HHSN275201800001I. Amita Gupta was also supported by NIH UM1AI069465.
The University of Cape Town Clinical PK Laboratory is supported in part via the Adult Clinical Trial Group (ACTG), by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health under award numbers UM1 AI068634, UM1 AI068636, and UM1 AI106701; as well as the Infant Maternal Pediatric Adolescent AIDS Clinical Trials Group (IMPAACT), funding provided by National Institute of Allergy and Infectious Diseases (U01 AI068632), The Eunice Kennedy Shriver National Institute of Child Health and Human Development, and National Institute of Mental Health grant AI068632.
References
- 1.WHO TUBERCULOSIS REPORT 2017 GLOBAL. (Geneva, 2017).at <http://apps.who.int/bookorders.> [Google Scholar]
- 2.Selwyn PA et al. A Prospective Study of the Risk of Tuberculosis among Intravenous Drug Users with Human Immunodeficiency Virus Infection. N. Engl. J. Med 320, 545–550 (1989). [DOI] [PubMed] [Google Scholar]
- 3.Singh N & Perfect JR Immune Reconstitution Syndrome and Exacerbation of Infections after Pregnancy. Clin. Infect. Dis 45, 1192–1199 (2007). [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Latent tuberculosis infection Updated and consolidated guidelines for programmatic management. (Geneva, 2018).at <https://www.who.int/tb/publications/2018/latent-tuberculosis-infection/en/> [PubMed] [Google Scholar]
- 5.Khoo SH, Gibbons S, Seden K & Back DJ SYSTEMATIC REVIEW : Drug-drug Interactions between Antiretrovirals and medications used to treat TB , Malaria , Hepatitis B & C and opioid dependence. 5656, (2014). [Google Scholar]
- 6.Pinheiro EA & Stika CS Drugs in pregnancy: Pharmacologic and physiologic changes that affect clinical care. Semin. Perinatol 151221 (2020).doi: 10.1016/j.semperi.2020.151221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickmann LJ, Isoherranen N, Trager WF, Levy RH & Keirns JJ Quantitative prediction of CYP2B6 induction by estradiol during pregnancy: potential explanation for increased methadone clearance during pregnancy. Drug Metab. Dispos 41, 270–4 (2013). [DOI] [PubMed] [Google Scholar]
- 8.Tsutsumi K et al. The effect of pregnancy on cytochrome P4501A2, xanthine oxidase, and N-acetyltransferase activities in humans. Clin. Pharmacol. Ther 70, 121–125 (2001). [DOI] [PubMed] [Google Scholar]
- 9.Jeong H Altered drug metabolism during pregnancy: hormonal regulation of drug-metabolizing enzymes. Expert Opin. Drug Metab. Toxicol 6, 689–99 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dooley KE et al. Pharmacokinetics of Efavirenz and Treatment of HIV-1 Among Pregnant Women With and Without Tuberculosis Coinfection. J. Infect. Dis 211, 197–205 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olagunju A et al. Pharmacogenetics of pregnancy-induced changes in efavirenz pharmacokinetics. Clin. Pharmacol. Ther 97, 298–306 (2015). [DOI] [PubMed] [Google Scholar]
- 12.Luetkemeyer AF et al. Combined effect of CYP2B6 and NAT2 genotype on plasma efavirenz exposure during rifampin-based antituberculosis therapy in the STRIDE study. Clin. Infect. Dis 60, 1860–1863 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta A et al. Isoniazid Preventive Therapy in HIV-Infected Pregnant and Postpartum Women. N. Engl. J. Med 381, 1333–46 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holzinger ER et al. Genome-wide association study of plasma efavirenz pharmacokinetics in AIDS Clinical Trials Group protocols implicates several CYP2B6 variants. Pharmacogenet. Genomics 22, 858–67 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boukouvala sotiria et al. Database of arylamine N-acetyltransferases (NATs). Democritus Univ. Thrace (2016).at <https://nat.mbg.duth.gr/> [Google Scholar]
- 16.McDonagh EM et al. PharmGKB summary: very important pharmacogene information for N-acetyltransferase 2. Pharmacogenet. Genomics 24, 409–25 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boeckmann AJ, Beal SL & Sheiner LB NONMEM User’s Guide, Part V. Introductory Guide. NONMEM Proj. Gr 48 (2011).doi: 10.1017/CBO9781107415324.004 [DOI] [Google Scholar]
- 18.Keizer RJ, Karlsson MO & Hooker A Modeling and Simulation Workbench for NONMEM: Tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst. Pharmacol 2, e50 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gordi T et al. A semiphysiological pharmacokinetic model for artemisinin in healthy subjects incorporating autoinduction of metabolism and saturable first-pass hepatic extraction. Br. J. Clin. Pharmacol 59, 189–98 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang J, Jamei M, Yeo KR, Rostami-Hodjegan A & Tucker GT Misuse of the well-stirred model of hepatic drug clearance. Drug Metab. Dispos 35, 501–502 (2007). [DOI] [PubMed] [Google Scholar]
- 21.Mehvar R Clearance concepts: Fundamentals and application to pharmacokinetic behavior of drugs. J. Pharm. Pharm. Sci 21, 88s–102s (2018). [DOI] [PubMed] [Google Scholar]
- 22.Alghamdi WA, Al-Shaer MH & Peloquin CA Protein binding of first-line antituberculosis drugs. Antimicrob. Agents Chemother 62, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sturkenboom MGG et al. Quantification of isoniazid, pyrazinamide and ethambutol in serum using liquid chromatography-tandem mass spectrometry. J. Appl. Bioanal 1, 89–98 (2015). [Google Scholar]
- 24.Hooker AC, Staatz CE & Karlsson MO Conditional weighted residuals (CWRES): A model diagnostic for the FOCE method. Pharm. Res 24, 2187–2197 (2007). [DOI] [PubMed] [Google Scholar]
- 25.Eckhardt BJ & Gulick RM Drugs for HIV Infection. Infect. Dis. (Auckl) 2, 1293–1308.e2 (2017). [Google Scholar]
- 26.Parkin DP et al. Trimodality of isoniazid elimination: Phenotype and genotype in patients with tuberculosis. Am. J. Respir. Crit. Care Med 155, 1717–1722 (1997). [DOI] [PubMed] [Google Scholar]
- 27.Anderson BJ & Holford NHG Mechanism-Based Concepts of Size and Maturity in Pharmacokinetics. Annu. Rev. Pharmacol. Toxicol 48, 303–332 (2008). [DOI] [PubMed] [Google Scholar]
- 28.Beal SL Ways to fit a PK model with some data below the quantification limit. J. Pharmacokinet. Pharmacodyn 28, 481–504 (2001). [DOI] [PubMed] [Google Scholar]
- 29.Keizer RJ, Zandvliet AS, Beijnen JH, Schellens JHM & Huitema ADR Performance of Methods for Handling Missing Categorical Covariate Data in Population Pharmacokinetic Analyses. AAPS J. 14, 601–611 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Savic RM, Jonker DM, Kerbusch T & Karlsson MO Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J. Pharmacokinet. Pharmacodyn 34, 711–726 (2007). [DOI] [PubMed] [Google Scholar]
- 31.Donald PR et al. The influence of dose and N-acetyltransferase-2 (NAT2) genotype and phenotype on the pharmacokinetics and pharmacodynamics of isoniazid. Eur. J. Clin. Pharmacol 63, 633–639 (2007). [DOI] [PubMed] [Google Scholar]
- 32.Marzolini C et al. Efavirenz plasma levels can predict treatment failure and central nervous system side effects in HIV-1-infected patients. [DOI] [PubMed]
- 33.Desta Z et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2B6 and Efavirenz-Containing Antiretroviral Therapy. Clin. Pharmacol. Ther 106, 726–733 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dooley KE et al. Pharmacokinetics of Efavirenz and Treatment of HIV-1 Among Pregnant Women With and Without Tuberculosis Coinfection. J. Infect. Dis 211, 197–205 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertrand J et al. Dependence of Efavirenz- and Rifampicin-Isoniazid-Based Antituberculosis Treatment Drug-Drug Interaction on CYP2B6 and NAT2 Genetic Polymorphisms: ANRS 12154 Study in Cambodia. J. Infect. Dis 209, 399–408 (2014). [DOI] [PubMed] [Google Scholar]
- 36.Wen X, Wang J-S, Neuvonen PJ & Backman JT Isoniazid is a mechanism-based inhibitor of cytochrome P450 1A2, 2A6, 2C19 and 3A4 isoforms in human liver microsomes. Eur. J. Clin. Pharmacol 57, 799–804 (2002). [DOI] [PubMed] [Google Scholar]
- 37.Sekaggya-Wiltshire C et al. Low anti-tuberculosis drug concentrations in HIV-Tuberculosis co-infected adults with low body weight. In Internantional Work. Clin. Pharmacol. Tuberc. Drugs 51–52 (Internantional workshop on clinical pharmacology of Tuberculosis Drugs, Hague, Netherlands, 2018).at <http://regist2.virology-education.com/abstractbook/2018/abstractbook_11tbpk.pdf> [Google Scholar]
- 38.Chirehwa MT et al. Effect of efavirenz-based antiretroviral therapy and high-dose rifampicin on the pharmacokinetics of isoniazid and acetyl-isoniazid. J. Antimicrob. Chemother 74, 139–148 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poole NF & Meyer AE Stability of Isoniazid in Aqueous Solutions and Plasma. Exp. Biol. Med 104, 560–562 (1960). [DOI] [PubMed] [Google Scholar]
- 40.Daskapan A et al. A Systematic Review on the Effect of HIV Infection on the Pharmacokinetics of First-Line Tuberculosis Drugs. Clin. Pharmacokinet 58, 747–766 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zabost A et al. Correlation of N-acetyltransferase 2 genotype with isoniazid acetylation in polish tuberculosis patients. Biomed Res. Int 2013, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seng K-Y et al. Population pharmacokinetic analysis of isoniazid, acetylisoniazid, and isonicotinic acid in healthy volunteers. Antimicrob. Agents Chemother 59, 6791–9 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kock M. de, Tarning J, Barnes KI & Denti P Response to “Lactation Status and Studies of Pyrimethamine Pharmacokinetics in Pregnancy”. CPT Pharmacometrics Syst. Pharmacol 6, 731–731 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Orrell C et al. Effect of mid-dose efavirenz concentrations and CYP2B6 genotype on viral suppression in patients on first-line antiretroviral therapy. Int. J. Antimicrob. Agents 47, 466–472 (2016). [DOI] [PubMed] [Google Scholar]
- 45.Dickinson L et al. Pharmacokinetic and Pharmacodynamic Comparison of Once-Daily Efavirenz (400 mg vs. 600 mg) in Treatment-Naive HIV-Infected Patients: Results of the ENCORE1 Study. Clin. Pharmacol. Ther 98, 406–416 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sabbagh A, Darlu P, Crouau-Roy B & Poloni ES Arylamine N-Acetyltransferase 2 (NAT2) Genetic Diversity and Traditional Subsistence: A Worldwide Population Survey. PLoS One 6, e18507 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patin E et al. Sub-Saharan African coding sequence variation and haplotype diversity at the NAT2 gene. Hum. Mutat 27, 720 (2006). [DOI] [PubMed] [Google Scholar]
- 48.Zanger UM & Klein K Pharmacogenetics of cytochrome P450 2B6 (CYP2B6): Advances on polymorphisms, mechanisms, and clinical relevance. Front. Genet 4, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou Y, Ingelman-Sundberg M & Lauschke VM Worldwide Distribution of Cytochrome P450 Alleles: A Meta-analysis of Population-scale Sequencing Projects. Clin. Pharmacol. Ther 102, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Squibb B-M SUSTIVA ® (efavirenz) capsules and tablets. Full prescribing information. (Princeton, NJ, 2010). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


