Abstract
Objective:
To determine whether delayed or cancelled elective procedures due to COVID-19 resulted in higher rates of emergency department (ED) utilization and/or increased mortality.
Summary Background Data:
On March 15, 2020, the Veterans Affairs (VA) issued a nationwide order to temporarily pause elective cases due to COVID-19. The effects of this disruption on patient outcomes are not yet known.
Methods:
This retrospective cohort study used data from the VA Corporate Data Warehouse. Surgical procedures cancelled due to COVID-19 in 2020 (n=3,326) were matched to similar completed procedures in 2018 (n=151,863) and 2019 (n=146,582). Outcome measures included 30- and 90-day VA ED use and mortality in the period following the completed or cancelled procedure. We used exact matching on surgical procedure category and nearest neighbor matching on patient characteristics, procedure year, and facility.
Results:
Patients with elective surgical procedures cancelled due to COVID-19 were no more likely to have an ED visit in the 30- (Difference: −4.3 % pts; 95% CI: −0.078, −0.007) and 90 days (−0.9 % pts; 95% CI: −0.068, 0.05) following the expected case date. Patients with cancellations had no difference in 30- (Difference: 0.1 % pts; 95% CI: −0.008, 0.01) and 90-day (Difference: −0.4 % pts; 95% CI: −0.016, 0.009) mortality rates when compared to similar patients with similar procedures that were completed in previous years.
Conclusions:
The pause in elective surgical cases was not associated with short-term adverse outcomes in VA hospitals, suggesting appropriate surgical case triage and management. Further study will be essential to determine if the delayed cases were associated with longer-term effects.
Mini-Abstract
In this matched retrospective cohort study of 3,326 patients with cancelled elective procedures due to COVID-19, cancellations were not associated with increased short-term mortality or emergency department utilization in the 30- and 90-days following case cancellation. The pause in elective surgical cases was not associated with short-term adverse outcomes in VA hospitals, suggesting appropriate surgical case triage and management.
Introduction
The SARS-CoV-2 (COVID-19) pandemic caused an unprecedented interruption in healthcare delivery. Healthcare systems reallocated resources in anticipation of a surge and by mid-March, nearly every healthcare system had postponed, delayed, or cancelled elective surgical procedures. While it was almost universally acknowledged that curtailing procedures was necessary to reduce unnecessary exposure to the virus and to reallocate personnel, equipment, and resources for anticipated COVID-19 patients, there has been widespread concern that delays in care may have resulted in patient harm.1
On March 15, 2020, similar to many other healthcare systems, the Veterans Administration (VA) issued a nationwide order to temporarily pause elective cases for an indefinite period of time.2 The American College of Surgeons (ACS) issued triage guidance the next day to aid with decision making on which cases should proceed.3 However, the term “elective” is broad and ill-defined and there is no consensus on what types of cases should proceed, and under what circumstances. Suggestions and advice regarding how to triage cases varied across regions and disciplines.4 Up to 91 percent of surgical cases could be considered elective, but nearly all of these need to be completed at some point in the future.5 As such, these decisions were primarily left up to local clinicians and leaders instead of issuing blanket guidance. For many institutions, including VA, case-by-case decisions determined which procedures proceeded both immediately following the pause and later as surgical cases resumed.
The consequences of delays in surgery are not well-understood, however, research to date suggests that delays can have functional, psychologic, and economic ramifications for patients.4,6,7 Moreover, postponing care could lead to delays in diagnosis and treatment as disease burden continues to accumulate.8,9 As patients and healthcare systems continue to face challenges during the ongoing pandemic and grapple with the back log of cases in the post-surge phase, it is vital to ascertain how delays in elective procedures impacted patients. To assess short-term adverse outcomes, we examined the association of cancelled elective procedures with 30- and 90-day ED use and mortality among Veterans scheduled to have an elective procedure compared to similar patients with similar procedures in previous years.
Methods
Data and Population
We used data from the VA Corporate Data Warehouse (CDW),10 a database of all VA electronic health records. We assessed Current Procedural Terminology (CPT) codes, procedure dates (i.e., scheduled, and completed or cancelled) and reasons for cancellations from the CDW surgery domain for calendar years 2018-2020. Cancellation reasons included changes in medical condition and other non-health reasons, but inconsistencies in data entry during the early period of the pandemic prevented data from being sufficiently precise to differentiate from COVID-19 and other reasons for cancellation.2
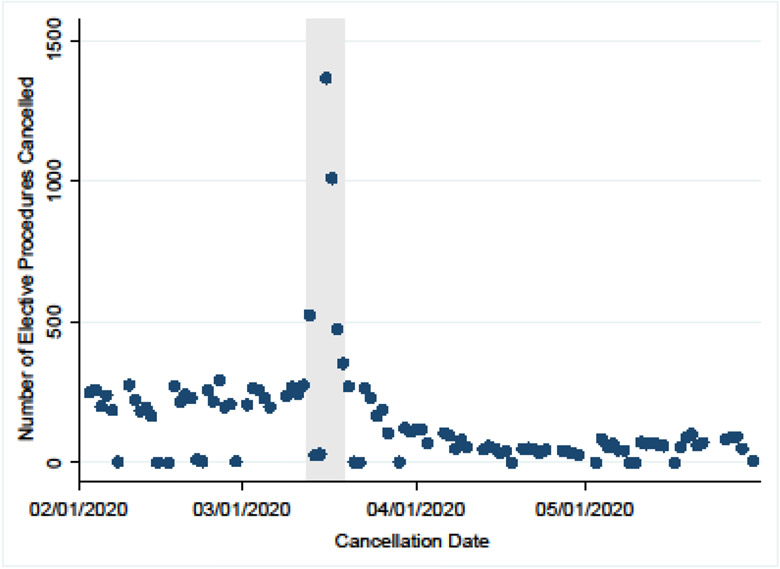
To examine the impact of cancellations due to the pandemic rather than changes in patient condition, we selected cases cancelled on March 13-19, 2020. Cancellations spiked dramatically during this seven-day period, which supports our claim that these cases were cancelled due to the nationwide order (Figure 1). The Supplementary Figure 1 illustrates that most cancelled cases were scheduled for that week, but some were scheduled for more than a month later. We limited cancellations to cases cancelled for the following reasons: environmental issue (2,585, 71.2%), clinic-related issue (279, 7.7%), and patient-related issue (517, 14.2%). We excluded surgical cases moved to earlier dates and cases labelled urgent or emergent — which should not have been affected by the national order — (29, 0.8%), and cancellations due to patient-health related issues (201, 5.5%). For comparison, nearly 30 percent of VA surgical cancellations were attributed to changes in medical condition prior to the pandemic.11 Twenty (0.6%) cancelled procedures with missing reasons or missing cancellation reasons were also excluded. In supplementary analyses, we limited the sample to only those cases cancelled on March 16th or 17th.
Figure 1. Time profile of the number of elective procedures cancelled between February 1 and May 31, 2020.
Note: Gray area indicates March 13-19, 2020.
The study cohort included patients with therapeutic and diagnostic elective procedures scheduled by all VA surgical service lines. We limited the sample to surgical procedures defined as CPT codes 10004-69979. We converted principal CPT codes to clinically meaningful procedures using the Agency for Healthcare Research and Quality’s (AHRQ) Clinical Classifications Software (CCS) and used the 179 classifications as surgical case categories.12 To classify the operative complexity of surgical procedures, we used invasive procedure complexity designations assigned by the VA Surgical Quality Improvement Program (VASQIP), a nationwide quality improvement effort responsible for measuring and improving the quality of surgical outcomes within the VA and the progenitor to the National Surgical Quality Improvement Program.13 VASQIP categorizes procedures using the following complexity designations: Standard, Intermediate, Complex, or Not in Complexity Matrix.
Finally, all-cause mortality data were extracted from the CDW, which is updated nightly. Date of death information come from numerous sources, including data in Social Security Administration Death Master File, from the Department of Defense, the National Cemetery Administration, VA medical facilities, and spousal or family notification. Lags between date of notification and date of death vary by source. The latest surgical case in the COVID-19 group was scheduled for June 2, 2020, and the latest data extraction on September 5, 2020 included death records as recent as September 3, 2020.
Measures
We examined 30- and 90-day ED use and 30- and 90-day mortality from patients’ scheduled surgery dates.
Covariates included patient age, sex, race, ethnicity, marital status, and VA priority group assignment (High disability: priority groups 1 and 4, Low/moderate disability: 2, 3, 6, Non-disabled, co-pay required: 7 and 8, and Low-income: 5). Clinical measures included Elixhauser comorbidity index score14 and quarterly Nosos score. The Nosos risk score indicates the patient’s healthcare expense level compared to the average risk score in the VA population (e.g., Nosos score of 1.5 indicates the patient is 50% more expensive compared to the average risk score).15 Finally, we included a covariate for the VA medical center associated with the scheduled or completed procedure.
Statistical Analysis
To assess whether procedural cancellations due to COVID-19 had immediate adverse consequences on patient health, we compared the outcomes of patients who had elective procedures cancelled due to COVID-19 (COVID-19 group) to the outcomes of similar patients who had the same procedure completed in March-June of 2018 and 2019 (comparison group).
We summarized patient sociodemographic and clinical characteristics for the COVID-19 group, the comparison group prior to matching, and the matched comparison group. Standardized differences were calculated to assess imbalance between the COVID-19 group and matched comparison groups. We used nearest neighbor matching with exact matching on surgical case category to estimate potential outcome means for patients who had procedures cancelled due to COVID-19.16 AHRQ CCS surgical case categories were matched exactly, and nearest neighbors were selected on patient covariates, VA facility, and procedure year based on Mahalanobis distance. COVID-19 cancelled procedures that had fewer than two exact matching cases needed for robust standard error estimation (52, 2.2%) or that had missing values (3, 0.1%) were dropped. We applied bias-correction for matching on two or more continuous covariates and estimated robust standard errors.17,18 Finally, we stratified the analyses by the following: whether the surgical case was assessed by the VASQIP, cases with intermediate operative complexity as defined by VASQIP, and cases with standard operative complexity as defined by VASQIP. All analyses were performed using Stata version 15.1 (StataCorp LLC). This study was approved by the Stanford University institutional review board.
Results
Sample Characteristics and Case Selection
Supplementary Table 1 presents descriptive statistics for the final analytic sample of 3,326 patients with cancelled elective procedures due to COVID-19 in 2020 and 298,445 matched patients with completed cases during March-June of 2018 and 2019. A slightly higher proportion of patients who had surgical procedures cancelled due to COVID-19 were Black (20.8%) compared to patients whose surgical procedures were completed (18.6%, p=.002). Although mean age for both groups was 64 years, patients who had surgeries cancelled on average had fewer Elixhauser comorbidities (mean: 3.3 v. 4.2, standardized difference: 0.34) and lower Nosos risk scores (mean: 1.7 v. 2.1, standardized difference: 0.18).
The surgical services with the most cancellations due to COVID-19 were ophthalmology, general surgery, and orthopedic cases (Table 1). Ophthalmology cases represented 25.7% of COVID-19 cancelled cases and 20.4% of matched completed cases in 2018 and 2019. Supplementary Table 2 lists the most frequently cancelled elective procedures, including lens and cataract procedures (779, 23.4%), knee arthroplasties (166, 5.0%), colonoscopies (166, 5.0%), and therapeutic procedures on muscles and tendons (149, 4.5%). Supplementary Table 3 describes the operative complexity for the completed and cancelled procedures. Complex procedures (27, 0.8%) represented small fractions of cancelled procedures, with standard complexity being the large majority (intermediate complexity: 483, 14.6%; standard complexity: 2792, 84.6%).
Table 1.
Association of elective procedures cancelled due to COVID-19 and emergency department utilization
| Completed Proceduresa | COVID-19 Cancelledb | |||||
|---|---|---|---|---|---|---|
| No. | % 30-Day ED Visit Mean (SD) |
% 90-Day ED Visit Mean (SD) |
No. | 30-Day ED Difference (SE) [CI]c |
90-Day ED Difference (SE) [CI]c |
|
| COVID-19 Cancelled v. All Completed Procedures | 298445 | 0.104 (0.305) | 0.196 (0.397) | 3326 | −0.043 (0.018) [−0.078,−0.007] |
−0.009 (0.03) [−0.068,0.05] |
| COVID-19 Cancelled v. All Scheduled Procedures | 320474 | 0.103 (0.304) | 0.196 (0.397) | 3326 | −0.042 (0.018) [−0.076,−0.008] |
−0.011 (0.029) [−0.067,0.046] |
| VASQIP Cases | 86036 | 0.14 (0.347) | 0.235 (0.424) | 1040 | −0.098 (0.014) [−0.126,−0.071] |
−0.089 (0.028) [−0.145,−0.033] |
| Intermediate Operative Complexity | 36094 | 0.152 (0.359) | 0.252 (0.434) | 472 | −0.103 (0.018) [−0.138,−0.068] |
−0.142 (0.028) [−0.197,−0.087] |
| Standard Operative Complexity | 250292 | 0.094 (0.291) | 0.183 (0.387) | 2798 | −0.04 (0.019) [−0.078,−0.002] |
−0.012 (0.034) [−0.078,0.055] |
Abbreviations: ED, emergency department; VASQIP, VA Surgical Quality Improvement Program
Comparison group includes all matched completed elective procedures in March-June 2018 and 2019 unless stated otherwise.
Elective procedures cancelled on March 13-19, 2020.
Estimates are percentage point difference from the comparison group.
Risk of Emergency Department Use
Unadjusted 30- and 90-day ED use were lower among patients who had their procedures cancelled due to COVID-19 (90-day, 424/3,326, 12.8%) compared to patients who had procedures completed in 2018 or 2019 (63,335/315,713, 20.1%). Matching results show that procedure cancellations due to COVID-19 were associated with lower 30- and 90-day ED use (Table 1). Compared to similar patients who had the same procedure completed in 2018 and 2019, 30- and 90-day ED use among patients who had their cases cancelled were on average 4.3 (95% CI: −0.078,−0.007) and 0.9 (95% CI: −0.068, 0.05) percentage points lower, respectively. Compared to the mean ED visit rate in previous years, this represents a 41.3 and 4.6 percent drop relative to previous years. Patients who had intermediate operative complexity procedures cancelled were significantly less likely to have an ED visit within 30 days of their scheduled surgical cases.
Risk of Mortality
Twenty-six or 0.8% of patients who had cancelled procedures died within 90 days of the scheduled surgery date. The unadjusted 90-day mortality rate for patients whose surgical cases were not cancelled was 1.5% (4,649). Cancellations were not significantly associated with higher 30- and 90-day mortality (Table 2). Compared to matched patients, 30-day mortality rate for patients who had cancellations was, on average, 0.1 percentage points higher and not statistically significant (Difference=0.001; 95% CI: −0.008, 0.01). The estimate for 90-day mortality was also not statistically different between patients with cancellations and matched patients (Difference=−0.004 % pts; 95% CI: −0.016, 0.009). Cancellations were also not significantly associated with higher short-term mortality rates relative to surgical case completion in cases with intermediate operative complexity, although fewer of these cases were cancelled and estimates were less precise (30-day Difference=0.015; 95% CI: −0.072, 0.101; 90-day Difference=0.034; 95% CI: −0.054, 0.122). Cases assessed by VASQIP similarly did not show any statistically significant association (30-day Difference=−0.002; 95% CI: −0.041 to 0.037; 90-day Difference=−0.003; 95% CI: −0.043 to 0.036). The sensitivity analysis, which was limited to patients who had their cases cancelled only on March 16-17, produced similar results (see Supplemental Tables 4 and 5).
Table 2:
Association of elective procedures cancelled due to COVID-19 and mortality
| Completed Proceduresa | COVID-19 Cancelledb | |||||
|---|---|---|---|---|---|---|
| No. | % 30-Day Mortality Mean (SD) |
% 90-Day Mortality Mean (SD) |
No. | 30-Day Mortality Difference (SE) [CI]c |
90-Day Mortality Difference (SE) [CI]c |
|
| COVID-19 Cancelled v. All Completed Procedures | 298445 | 0.0049 (0.0701) | 0.0123 (0.1101) | 3326 | 0.0008 (0.0045) [−0.008,0.0095] |
−0.0036 (0.0064) [−0.0162,0.009] |
| COVID-19 Cancelled v. All Scheduled Procedures | 320474 | 0.005 (0.0709) | 0.0125 (0.1111) | 3326 | 0.0017 (0.0047) [−0.0075,0.0109] |
−0.0025 (0.0066) [−0.0154,0.0104] |
| VASQIP Cases | 86036 | 0.0083 (0.0906) | 0.016 (0.1255) | 1040 | −0.0024 (0.0199) [−0.0413,0.0365] |
−0.0033 (0.0201) [−0.0426,0.0361] |
| Intermediate Operative Complexity | 36094 | 0.0083 (0.0908) | 0.0163 (0.1268) | 472 | 0.0146 (0.0442) [−0.0719,0.1012] |
0.0343 (0.0449) [−0.0536,0.1223] |
| Standard Operative Complexity | 250292 | 0.0039 (0.0624) | 0.0105 (0.1019) | 2798 | 0.0015 (0.0038) [−0.0059,0.0088] |
−0.003 (0.0063) [−0.0154,0.0094] |
Comparison group includes all matched completed elective procedures in March-June 2018 and 2019 unless stated otherwise.
Elective procedures cancelled on March 13-19, 2020.
Estimates are percentage point difference from the comparison group.
Completion Rate
In 2018 and 2019, 22.0% (4,070) of elective procedures cancelled in March-June were rescheduled and completed within 30 days of the initial case date; nearly one-third (5,918, 32.0%) were completed within 90 days at VA facilities. Rescheduling surgical cases cancelled due to COVID-19 lagged as the VA continues to adapt to the pandemic. Of the 3,326 cancelled cases, 67 (2.0%) procedures were completed within 30 days; 494 (14.9%) within 90 days (Table 3). Intermediate operative complexity procedures were slightly more likely to be rescheduled and completed than standard operative complexity procedures within 30 days (3.0 vs. 1.8%).
Table 3.
30- and 90-day completion frequency for elective procedures cancelled due to COVID-19.
| 30 days | 90 days | ||||
|---|---|---|---|---|---|
| Total | No. | % | No. | % | |
| COVID-19 Cancelleda | 3326 | 67 | 2.0 | 494 | 14.9 |
| VASQIP Cases | 1040 | 28 | 2.7 | 169 | 16.3 |
| Intermediate Operative Complexity | 472 | 14 | 3.0 | 68 | 14.4 |
| Standard Operative Complexity | 2798 | 51 | 1.8 | 411 | 14.7 |
Abbreviation: VASQIP, Veterans Affairs Surgical Quality Improvement Program
Elective procedures cancelled on March 13-19, 2020.
Discussion
Among 3,326 patients with cancelled elective procedures due to COVID-19, we did not find that cancellations in elective procedures were associated with increases in short-term patient mortality. Surgical procedures cancelled immediately around the order, despite having lower reschedule and completion rates compared to previous years, yielded similar mortality rates to procedures that had been completed. Further, cancelled elective surgical procedures were not associated with an increased probability of an ED visit soon after the scheduled date.
Overall, our results suggest first and foremost that clinicians engaged in effective decision making and were able to appropriately triage cases to balance the needs of patients and public health concerns. The vast majority of cancelled cases were low-acuity cases with low rates of intra- and post-operative surgical complications, in healthier patients, and concentrated in ophthalmology and orthopedics. While a few studies have examined the impact of postponing elective procedures on resource utilization, to our knowledge, this is the first study to examine what impact these delays have had on patient outcomes across a range of surgical and procedural specialties. While most cases were common, high-volume low-acuity procedures, we also did not find an association with 90-day mortality in intermediate-acuity case cancellations. With limited information and guidance about what should constitute an elective procedure and substantial uncertainty about the dangers of COVID-19 early in the pandemic, our results suggest that clinicians were able to select elective procedures could be safely delayed in a pandemic without immediate adverse consequences on patient survival.
ED visits following surgeries in both inpatient and ambulatory settings are common and well documented.19-21 With cancellations of procedures during the pandemic, the usual post-operative complications that drive these visits are no longer applicable, thus largely explaining why the national order to cancel elective surgical procedures was not associated with increased ED utilization when compared to previous years. While one might surmise that patients with cancelled procedures did not experience significant clinical consequences related to the delay (e.g., pain, infection) that would prompt acute, unscheduled visits to the ED, recent unpublished evidence and published data suggests that during the early stages of the pandemic, patients may have deferred visits to the ED in an attempt to reduce exposure to the virus.22 The Centers for Disease Control and Prevention found that ED visits declined 42 percent during the early months of the COVID-19 pandemic which is close to our estimate of a 46 percent drop in ED visits relative to the comparison group.23 Furthermore, it is possible that patients were substituting face-to-face ED visits with alternative virtual care modalities to address low-acuity concerns. These shifts in acute care utilization due to COVID-19 likely bias our estimates of ED visits when compared to previous years.
Though our results support the notion that elective cases can be safely delayed, the data does not capture the effects on other measures of health including well-being, functional capacity, pain, and economic consequences.4 Moreover, many of the surgical cases cancelled due to COVID-19 were for conditions that would take longer than 90 days to manifest as harmful in easily measurable ways. For example, patients that went without a cataract removal or knee arthroscopy may have experienced pain or reduced quality of life for longer than would normally be necessary but did not progress to the point of experiencing one of the more extreme outcomes measured in our study. Future studies should monitor longer-term outcomes for various procedure types.
Currently, there are limited data to guide healthcare systems in resuming elective cases. As our findings suggest, cancellations will undoubtedly result in an increasing backlog of cases that will pose significant future scheduling and clinical challenges. In the following months, it will be crucial to continue monitoring equitable access to elective surgery, particularly for socioeconomically disadvantaged patients who may be less able to advocate for themselves and more likely to be lost to follow-up. Variations in case completion rates should also be assessed to identify potential structural barriers to equitable access and ensure a fair allocation of services.
This study has several limitations. First, the VA population is different from the general population, and patients are more likely to be male, older, and have more comorbidities.24 While these differences would likely make this population more likely to suffer adverse outcomes associated with delays, it is unclear if other populations would have similar experiences with cancelled surgical cases due to COVID-19. Furthermore, our analysis was limited to VA data and did not include referrals to or care from non-VA or community providers due to lag in claims data. Surgeries performed at non-VA hospitals were therefore not included, though this was likely a rare occurrence given significantly limited access to outpatient specialty care in community settings during the pandemic. Similarly, ED visits to non-VA EDs were not captured and may undercount actual acute care visits. However, mortality outcomes were not impacted as death data was available regardless of location of death. Finally, despite a rich set of demographic and clinical factors used for matched controls, any matching procedure cannot rule out the possibility of residual confounding from unobserved factors.
Conclusion
This study gives evidence that elective procedure cancellation due to the COVID-19 pandemic was not associated with increased ED utilization or mortality in the VA. While this is encouraging, the full cost of delayed and deferred surgical cases is not reflected in these outcomes, as longer-term outcomes and delays in diagnostic procedures likely add to the burden patients face. With projections of a cyclical relapsing of the virus, it is likely surgery will continue to be impacted. While many questions remain, this analysis suggests surgical case triage and management has been effective in avoiding the most serious adverse outcomes that may have resulted from the surgical shutdown in the early stages of the COVID-19 pandemic.
Supplementary Material
Acknowledgments
Funding/Support:
This study was funded by a grant from the US Department of Veterans Affairs Health Services and Research Development Service Individual Investigator Research (IIR) Award (IIR 16-266, grant no. 1101HX002362-01A2; PI, Anita Vashi). Dr. Tran is a Big Data Scientist Training Enhancement Program (BD-STEP) Advanced Fellow funded by the VA Office of Academic Affiliations.
Role of Funder:
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Fu SJ, George EL, Maggio PM, et al. The consequences of delaying elective surgery: surgical perspective. Ann Surg. 2020;272:e79–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Veterans Affairs Office of Inspector General. Appointment management during the COVID-19 pandemic (VAOIG-20-02794-218). September 1, 2020. Available at https://www.va.gov/oig/pubs/VAOIG-20-02794-218.pdf. Accessed November 9, 2020.
- 3.American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures (dated March 17, 2020). Available at https://www.facs.org/covid-19/clinical-guidance/triage. Accessed November 9, 2020.
- 4.Søreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020. April 30 [Epub ahead on print]. Accessed on 11/9/2020. Available at: 10.1002/bjs.11670. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prin M, Guglielminotti J, Mtalimanja O, et al. Emergency-to-elective surgery ratio: a global indicator of acccess to surgical care. World J Surg. 2018;42:1971–1980. [DOI] [PubMed] [Google Scholar]
- 6.Vogel TR, Dombrovskiy VY, Lowry SF. In-hospital delay of elective surgery for high volume procedures: the impact on infectious complications. J Am Coll Surg. 2010;211:784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herrod PJJ, Adiamah A, Boyd-Carson H, et al. Winter cancellations of elective surgical procedures in the UK: a questionnaire survey of patients on the economic and psychological impact. BMJ Open. 2019;9:e028753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107:785–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pellino G, Spinelli A. How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum. 2020;63:720–722. [DOI] [PubMed] [Google Scholar]
- 10.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33:1203–1211. [DOI] [PubMed] [Google Scholar]
- 11.Argo JL, Vick CC, Graham LA, et al. Elective surgical case cancellation in the Veterans Health Administration system: identifying areas for improvement. Am J Surg. 2009;198:600–606. [DOI] [PubMed] [Google Scholar]
- 12.HCUP CCS-Services and Procedures. Healthcare Cost and Utilization Project (HCUP). May 2018. Agency for Healthcare Research and Quality, Rockville, MD. Available at www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. Accessed November 9, 2020. [Google Scholar]
- 13.Massarweh NN, Kaji AH, Itani KMF. Practical guide to surgical data sets: Veterans Affairs Surgical Quality Improvement Program (VASQIP). JAMA Surg. 2018;153:768–769. [DOI] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 15.Rosen AK, Wagner TH, Pettey WBP, et al. Differences in risk scores of Veterans receiving community care purchased by the Veterans Health Administration. Health Serv Res. 2018;53:5438–5454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abadie A, Drukker D, Herr JL, et al. Implementing matching estimators for average treatment effects in Stata. Stata J. 2004;4:290–311. [Google Scholar]
- 17.Abadie A, Imbens GW. Large sample properties of matching estimators for average treatment effects. Econometrica. 2006;74:235–267. [Google Scholar]
- 18.Abadie A, Imbens GW. Bias-corrected matching estimators for average treatment effects. J Bus Econ Stat. 2011;29:1–11. [Google Scholar]
- 19.Kocher KE, Nallamothu BK, Birkmeyer JD, et al. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood). 2013;32:1600–1607. [DOI] [PubMed] [Google Scholar]
- 20.Fox JP, Vashi AA, Ross JS, et al. Hospital-based, acute care after ambulatory surgery center discharge. Surgery. 2014;155:743–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernandez-Boussard T, Graham LA, Desai K, et al. The fifth vital sign: postoperative pain predicts 30-day readmissions and subsequent emergency department visits. Ann Surg. 2017;266:516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baum A, Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324:96–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wagner TH, Almenoff P, Francis J, et al. Assessment of the Medicare Advantage risk adjustment model for measuring Veterans Affairs hospital performance. JAMA Netw Open. 2018;1:e185993–e185993. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.