Summary
Background
Substantial evidence indicates that patient outcomes are more favourable in hospitals with better nurse staffing. One policy designed to achieve better staffing is minimum nurse-to-patient ratio mandates, but such policies have rarely been implemented or evaluated. In 2016, Queensland (Australia) implemented minimum nurse-to-patient ratios in selected hospitals. We aimed to assess the effects of this policy on staffing levels and patient outcomes and whether both were associated.
Methods
For this prospective panel study, we compared Queensland hospitals subject to the ratio policy (27 intervention hospitals) and those that discharged similar patients but were not subject to ratios (28 comparison hospitals) at two timepoints: before implementation of ratios (baseline) and 2 years after implementation (post-implementation). We used standardised Queensland Hospital Admitted Patient Data, linked with death records, to obtain data on patient characteristics and outcomes (30-day mortality, 7-day readmissions, and length of stay [LOS]) for medical-surgical patients and survey data from 17 010 medical-surgical nurses in the study hospitals before and after policy implementation. Survey data from nurses were used to measure nurse staffing and, after linking with standardised patient data, to estimate the differential change in outcomes between patients in intervention and comparison hospitals, and determine whether nurse staffing changes were related to it.
Findings
We included 231 902 patients (142 986 in intervention hospitals and 88 916 in comparison hospitals) assessed at baseline (2016) and 257 253 patients (160 167 in intervention hospitals and 97 086 in comparison hospitals) assessed in the post-implementation period (2018). After implementation, mortality rates were not significantly higher than at baseline in comparison hospitals (adjusted odds ratio [OR] 1·07, 95% CI 0·97–1·17, p=0·18), but were significantly lower than at baseline in intervention hospitals (0·89, 0·84–0·95, p=0·0003). From baseline to post-implementation, readmissions increased in comparison hospitals (1·06, 1·01–1·12, p=0·015), but not in intervention hospitals (1·00, 0·95–1·04, p=0·92). Although LOS decreased in both groups post-implementation, the reduction was more pronounced in intervention hospitals than in comparison hospitals (adjusted incident rate ratio [IRR] 0·95, 95% CI 0·92–0·99, p=0·010). Staffing changed in hospitals from baseline to post-implementation: of the 36 hospitals with reliable staffing measures, 30 (83%) had more than 4·5 patients per nurse at baseline, with the number decreasing to 21 (58%) post-implementation. The majority of change was at intervention hospitals, and staffing improvements by one patient per nurse produced reductions in mortality (OR 0·93, 95% CI 0·86–0·99, p=0·045), readmissions (0·93, 0·89–0·97, p<0·0001), and LOS (IRR 0·97, 0·94–0·99, p=0·035). In addition to producing better outcomes, the costs avoided due to fewer readmissions and shorter LOS were more than twice the cost of the additional nurse staffing.
Interpretation
Minimum nurse-to-patient ratio policies are a feasible approach to improve nurse staffing and patient outcomes with good return on investment.
Introduction
The years 2020–21 have been designated by WHO as the International Year of the Nurse and Midwife to honour the 200th anniversary of Florence Nightingale’s birth.1 Nightingale, through meticulous records and application of innovative statistics, documented that more British soldiers in military hospitals during the Crimean War died because of unsafe hospital conditions than of wounds in battle. Her solution was the introduction of trained nurses, shown by her research to be associated with reduced hospital deaths. Nurses are still saving lives in modern hospitals, and research suggests that patient harm can be further reduced by investments in nurse staffing.
The Lancet published in 2014 a landmark study showing that patients’ risk of dying after surgery varied by the number of patients for whom each nurse had responsibility.2 Studying outcomes of nearly half a million patients in nine European countries, investigators found that each additional patient added to nurses’ average workloads was associated with 7% higher odds of a patient dying within 30 days of admission. Evidence continues to grow that better hospital nurse staffing is associated with better patient outcomes, including fewer hospital acquired infections, shorter length of stay (LOS), fewer readmissions, higher patient satisfaction, and lower nurse burnout.2–14 Yet, substantial within-country variation in hospital nurse staffing persists, giving rise to calls for public policy interventions to establish minimum safe staffing standards in hospitals. In 2018, the International Council of Nurses, representing national nursing associations worldwide, issued their Position Statement on Evidence-Based Nurse Staffing, concluding that plenty of evidence supports taking action now to improve hospital nurse staffing, echoing Nightingale’s call to action over 150 years ago, that if we have evidence and fail to act, we are going backwards.15
The first jurisdictions to implement minimum nurse-to-patient ratios policies were the states of Victoria, Australia, and California, USA, in the late 1990s.16,17 The past 5 years have seen a resurgence of interest in establishing minimum nurse-to-patient ratio policies—Wales and Scotland (UK), Ireland, and Queensland (Australia) have implemented such policies18 and multiple US states are considering them.19 Queensland’s legislation is noteworthy because an independent prospective evaluation was included. Here, we report the results of that evaluation.
On July 1, 2016, Queensland established minimum nurse-to-patient ratios (the term nurse includes registered and enrolled nurses [nurses with a technical diploma who work under the supervision of a registered nurse]) for adult medical-surgical wards in 27 public hospitals. The legislation required that average nurse-to-patient ratios on morning and afternoon shifts be no lower than 1:4 and on night shifts no lower than 1:7. We collected survey data at the hospital level from thousands of nurses to link with data on patients’ clinical characteristics and outcomes from the period before and 2 years after implementation of ratios. Relative to comparison hospitals, we evaluated whether greater staffing improvements occurred at intervention hospitals, whether outcomes improved more at intervention hospitals, and whether the staffing improvements explained, at least partly, any advantage on patient outcomes.
Methods
Study design
This prospective panel study (RN4CAST-Australia) was quasi-experimental: we compared changes in measures of outcomes in a prospective panel of hospitals where assignment of the hospital to the treatment condition (the policy intervention) was non-random. We used nurse-reported data to measure medical-surgical nurse staffing levels and standardised patient data to measure outcomes at two timepoints: before implementation of ratios (baseline) and 2 years after implementation (post-implementation). We restricted our staffing measure to medical-surgical staffing and to nurses providing direct patient care. We compared two groups of hospitals: hospitals subject to the policy (intervention hospitals) and hospitals that discharged similar patients but were not subject to ratios (comparison hospitals). Intervention hospitals were chosen by the government to represent regions across the state. Therefore, our study accounted for pre-existing differences between intervention and comparison hospitals through statistical controls, including controls for hospital size and patient’s characteristics. We aimed to answer three main questions: first, whether changes in nurse staffing levels were different between intervention and comparison hospitals; second, whether changes in patient outcomes were different between intervention and comparison hospitals; and third, whether the staffing changes were associated with differential patient outcomes after accounting for differences in patient and hospital characteristics.
Ethics approval was obtained from the Queensland University of Technology (Kelvin Grove, QLD, Australia) and the University of Pennsylvania (Philadelphia, PA, USA). Use of the deidentified Queensland Hospital Admitted Patient Data Collection and linked death registry data was approved by Queensland Health in accordance with the Public Health Act 2005.
Study population and data sources
We used the standardised Queensland Hospital Admitted Patient Data Collection from the baseline period (July 1, 2015, to June 1, 2016) and 2 years after implementation of ratios (Jan 1 to Dec 31, 2018). The datafiles provide detailed information on patient demographics, diagnoses, procedures (with coding from the International Classification of Diseases, tenth edition, Australia modification), comorbidities, and discharge status. The files were linked with death records to measure 30-day mortality. Our focus was on adult patients in general medical-surgical wards—the clinical area targeted for change in nurse staffing ratios. Patients undergoing labour and delivery and patients being treated for psychiatric conditions were excluded.
We surveyed registered nurses and enrolled nurses—the types of nurses considered under the policy—before and after policy implementation to gather information on medical-surgical nurse staffing levels in the hospitals where they worked. Surveying bedside nurses, an approach supported by the organisational research literature,20 yields data on staffing levels with excellent predictive validity2,4 compared with single key-informant reports or administrative data, which often include non-direct care nurses (eg, management) and inflate staffing estimates. We provided respondents with a list of Queensland hospitals, so nurses could identify their hospital and the type of ward where they worked. This allowed us to attribute information from medical-surgical ward respondents to their hospital, aggregate their responses to produce hospital-level measures of medical-surgical ward staffing, and link them to independent data on patient outcomes and hospital size. The baseline survey data were collected between May 1 and May 31, 2016 (before ratio implementation on July 1, 2016). We repeated the survey 2 years after implementation between May 1 and May 31, 2018. We used a modified Dillman21 approach for email survey campaigns. In the baseline period, we sent emails and reminders to 26 871 nurses and received responses from 8732, giving an overall response rate of 32%. 2 years after implementation, we sent 30 658 emails and received responses from 8278 nurses, giving a response rate of 27%. Although a downward trend in survey responses has been well known in the past decade, these response rates were satisfactory and considered high for email-based surveys.22,23 These rates are consistent with or better than response rates for similar nurse surveys in the USA.3,4,24,25 The most important issue for the design of this study was to have a sufficient number of responses from nurses in each hospital to provide reliable staffing estimates. Although no threshold has been set for the number of respondents that ensures the reliability of the staffing measure we estimate, our previous work suggests that ten or more nurses per hospital suffice to provide staffing estimates that differ little from, and have the same effect as, measures estimated from 20, 30, or 40 or more nurses.2–4 The average number of medical-surgical nurse respondents per hospital was sufficient for the purposes of this study—our sample of hospitals (55, with 27 intervention hospitals and 28 comparison hospitals) included almost all hospitals in Queensland with more than 100 beds, represented by an average of 64 nurse respondents per hospital and as many as 588. Of key importance from the standpoint of representativeness, the 36 hospitals in our analyses accounted for 83% of all adult patient admissions to acute care hospitals statewide. Although nurse staffing on every ward probably affects patient outcomes, we restricted our attention to medical-surgical wards because doing so simplified the comparison across intervention and comparison hospitals, and these wards were the targeted setting for the policy.
Measures
Our measure of primary interest was hospital-level nurse-to-patient ratio on adult medical-surgical wards (hereafter referred to as nurse-to-patient ratios). By asking each nurse how many nurses and patients were on the ward during the last shift the nurse worked, and by averaging them to ward level and then hospital level, we produced a nurse staffing measure reflecting the average nurse-to-patient ratio across all medical-surgical wards in the hospitals. This method is consistent with the ratios legislation, which allows individual nurses to have a greater (or lesser) number of patients than the prescribed ratio, so long as the ward’s average is in compliance during the shift. As in other work,2,4 we expressed the ratio as the number of patients per nurse, allowing us to interpret model results in terms of the effect of each additional patient per nurse on each outcome.
Outcomes
Patient outcomes we assessed were patient 30-day mortality, 7-day readmission, and LOS. We used the Queensland Hospital Admitted Patient Data files to identify patient outcomes. These data were linked with death records, allowing us to capture deaths occurring within 30 days of admission, even those occurring outside the hospital. This eliminated bias due to hospital LOS variation arising from different discharge practices.26 To measure 7-day readmissions, we established the initial admission for each patient during each time period as the index admission. Patients who died during the index admission were excluded. For each index admission, we created a binary variable coded 0 if the patient was not admitted to any acute care hospital in the 7 days after discharge from index hospitalisation, and 1 if the patient was admitted within 7 days of discharge (except obstetric deliveries). LOS was measured continuously from admission to discharge. The minimum LOS was 1 day. Same-day and long-term (LOS >30 days) patients were excluded.
To adjust for differences in patient mix across hospitals, our readmission and mortality models included risk scores for each outcome derived from models that regressed the different outcomes on 17 indicators (eg, diabetes, cancer, and so on) from the Charlson Comorbidity Index to account for confounding comorbidities,27–30 as well as sex, age, and dummy variables for the Diagnosis-Related Group (DRG). These scores were derived from separate logistic regression models in which we estimated a risk score for death or readmission based on the patient characteristics described. These models showed excellent discrimination (c statistics were approximately 0·90). Readmission models were restricted to short-term patients (LOS ≤30 days) with discharge to home. Models for LOS were also restricted to short-term patients and controlled for whether patients died during hospitalisation and for age, mortality risk, comorbidities, and DRG.
Statistical analysis
We first described the patients in intervention and comparison hospitals before and after implementation of ratios, including their sex, age, comorbidities, and outcomes (ie, mortality, readmissions, and LOS). We then provided the results of estimating multilevel random-intercept logistic regression models for mortality and readmissions and zero-truncated negative binomial regression models (LOS was a count variable) to produce odds ratios (ORs) for mortality and readmissions and incident rate ratios (IRRs) for LOS, indicating the differential change in out comes between patients in intervention and comparison hospitals, after accounting for hospital characteristics (ie, size and time-invariant factors) and patient characteristics. The specification of multilevel models for panels of macro units with observations on nested micro units is detailed in Fairbrother,31 and its elaboration in the context of a prospective panel study of nurses nested within hospitals is presented in Sloane and colleagues.24 Finally, after showing how nurse staffing had changed over time, we used similar models to estimate whether staffing improvements were associated with patient outcome improvements. We did not have missing data; all models were adjusted for clustering of patients in hospitals and controlled for hospital size. Using expected frequencies derived from our models, we estimated the counterfactual for each outcome, that is, what outcomes would we expect in intervention hospitals if ratios had not been implemented. We then used published cost data to make a rough estimate of return on investment derived by preventing additional LOS and readmissions.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
For this study, we included 231 902 patients (142 986 in intervention hospitals and 88 916 in comparison hospitals) assessed at baseline (2016) and 257 253 patients (160 167 in intervention hospitals and 97 086 in comparison hospitals) assessed in the post-implementation period (2018). Patients in intervention hospitals were slightly younger and less likely to be women than those in comparison hospitals (table 1). The differences in comorbidities between timepoints were minimal in most cases for patients in both intervention and comparison hospitals. Although slightly higher rates of diabetes without complications and cancer were observed in patients in comparison hospitals, all other comorbidities were somewhat more common in patients in intervention hospitals.
Table 1:
Patient characteristics by baseline or post-implementation time period and by intervention or comparison hospitals
| Comparison hospitals (n=28) |
Intervention hospitals (n=27) |
|||||
|---|---|---|---|---|---|---|
| Baseline | Post-implementation | Total | Baseline | Post-implementation | Total | |
| Number of patients | 88 916 | 97 086 | 186002 | 142 986 | 160 167 | 303 153 |
| Age, years | 63·1 (17·7) | 63·6 (17·6 | 63·4 (17·6 | 57·0 (20·6 | 58·3 (19·6 | 57·7 (19·6 |
| Sex* | ||||||
| Female | 45 344 (51·0%) | 49 762 (51·3%) | 95 106 (51·4%) | 67 066 (46·9%) | 76 862 (48·0%) | 143 928 (47·5%) |
| Male | 43 572 (49·0%) | 47 323 (48·7%) | 90 895 (48·9%) | 75 920 (53·4%) | 83 305 (52·0%) | 159 225 (52·5%) |
| Comorbidities | ||||||
| Acute myocardial infarction | 662 (0·7%) | 461 (0·5%) | 1123 (0·6%) | 1552 (1·4%) | 1744 (1·4%) | 3296 (1·4%) |
| Congestive heart failure | 1871 (2·4%) | 1910 (2·0%) | 3781 (2·0%) | 4224 (3·0%) | 4878 (3·0%) | 9102 (3·0%) |
| Cerebrovascular disease | 667 (0·8%) | 568 (0·6%) | 1235 (0·7%) | 1844 (1·3%) | 2200 (1·4%) | 4044 (1·3%) |
| Dementia | 1652 (1·9%) | 1403 (1·4%) | 3055 (1·6%) | 3726 (2·6%) | 3599 (2·2%) | 7325 (2·4%) |
| Chronic obstructive pulmonary disease | 1974 (2·2%) | 1905 (2·0%) | 3879 (2·4%) | 3579 (2·5%) | 5243 (3·3%) | 8822 (2·9%) |
| Mild liver disease | 686 (0·8%) | 758 (0·8%) | 1444 (0·8%) | 3894 (2·7%) | 4092 (2·6%) | 7986 (2·6%) |
| Diabetes | 8386 (9·4%) | 9129 (9·4%) | 17 515 (9·4%) | 12 136 (8·5%) | 12 890 (8·0%) | 25 026 (8·3%) |
| Diabetes with complications | 4302 (4·8%) | 5995 (6·2%) | 10 297 (5·5%) | 12 566 (8·8%) | 17 024 (10·6%) | 29 590 (9·8%) |
| Hemiplegia or paraplegia | 655 (0·7%) | 566 (0·6%) | 1221 (0·7%) | 3088 (2·2%) | 2938 (1·8%) | 6026 (2·0%) |
| Renal disease | 3201 (3·6%) | 2359 (2·4%) | 5560 (3·0%) | 8154 (5·7%) | 6435 (4·0%) | 14 589 (4·8%) |
| Cancer | 1366 (1·5%) | 1349 (1·4%) | 2715 (1·5%) | 1654 (1·2%) | 1730 (1·4%) | 3384 (1·4%) |
| Metastatic cancer | 1804 (2·0%) | 1830 (1·9%) | 3634 (2·0%) | 3105 (2·2%) | 3625 (2·3%) | 6730 (2·2%) |
Data are n (%) or mean (SD). Comorbidities present for fewer than 1% of patients are included in the analyses but excluded from this table. These include peripheral vascular disease, rheumatoid disease, peptic ulcer disease, moderate or severe liver disease, and AIDS.
Some values do not add up to the total; categorisations with fewer than ten individuals were suppressed to maintain confidentiality.
Regarding the average number of patients per nurse, comparison hospitals averaged 6·13 patients per nurse (SD 0·75) at baseline and improved slightly after implementation to 5·96 patients per nurse (0·98). Intervention hospitals were better staffed on average at baseline (4·84 patients per nurse, SD 1·05) but improved by a greater margin to 4·37 patients per nurse (0·54) after implementation (table 2). The differences in these SDs, while unadjusted, indicate that the variation across intervention hospitals was reduced by half, whereas the variation across comparison hospitals increased somewhat over time. Regarding patient outcomes, 30-day mortality was somewhat higher overall at each timepoint for patients in intervention hospitals than for those in comparison hospitals, but although the percentage of patient deaths increased over time for patients in comparison hospitals, it decreased for those in intervention hospitals (table 2). Readmissions were slightly higher overall and in each timepoint for patients in intervention hospitals than for those in comparison hospitals, though the only change that occurred across timepoints—to the extent there was any change at all—was restricted to patients in comparison hospitals. Fewer than 2·8% of these patients were readmitted at baseline, whereas nearly 3% were readmitted post-implementation (table 2). By contrast, mean LOS was shorter and declined by a greater amount for patients in intervention hospitals than for those in comparison hospitals.
Table 2:
Patient mortality, readmissions, and length of stay, by timepoint and by intervention or comparison hospitals
| Comparison hospitals (n=28) |
Intervention hospitals (n=27) |
|||||
|---|---|---|---|---|---|---|
| Baseline | Post-implementation | Total | Baseline | Post-implementation | Total | |
| Patient outcomes | ||||||
| 30-day mortality, deaths per cases (%) | 952/88916 (1·07%) | 1092/97086 (1·12%) | 2044/186002 (1·10%) | 2290/142986 1·60%) | 2419/160167 (1·51%) | 4709/303 153 (1·55%) |
| 7-day readmissions, readmissions per cases (%) | 3226/115463 (2·79%) | 3660/123778 (2·96%) | 6886/239241 (2·88) | 5208/162910 (3·20%) | 5769/178699 (3·23%) | 10 977/341609 (3·21%) |
| Length of stay, mean (SD; cases) | 3·66 (3·83; 117809) | 3·51 (3·63; 126236) | 3·58 (3·73; 244045) | 3·45 (3·85; 176396) | 3·13 (3·42; 193318) | 3·29 (3·63; 369714) |
| Hospital staffing | ||||||
| Medical-surgical nurse staffing, mean patients per nurse (SD) | 6·13 (0·75) | 5·96 (0·98) | 6·04 (0·86) | 4·84 (1·05) | 4·37 (0·54) | 4·60 (0·80) |
Data are n/N (%), unless otherwise specified.
These results are tentative because they were not adjusted for differences in patient characteristics (eg, sex, age, and comorbidities) or differences in the size of intervention and comparison hospitals. To make these adjustments and assess differences across the two hospital groups over time, we used multilevel and multivariable models and, in the case of mortality and readmissions, converted percentages and percentage differences to odds and ORs. We first used the full sample of 55 hospitals to address whether the changes in outcomes were different in intervention versus comparison hospitals. We then used the sample of 36 hospitals with staffing data available to address whether, and to what extent, change in the outcomes in the two hospital groups were due to changes in staffing.
At baseline, patients in intervention hospitals had 34% higher 30-day mortality odds than those in comparison hospitals (adjusted OR 1·34, 95% CI 1·09–1·64, p=0·0052; table 3). After implementation, patients in comparison hospitals had higher, though not significantly, 30-day mortality odds (1·07, 0·97–1·17, p=0·18) than at baseline, whereas patients in intervention hospitals had significantly lower odds (0·89, 0·84–0·95, p=0·0003) than at baseline. The adjusted OR for the interaction between intervention hospitals and the implementation timepoint (0·84, 0·75–0·93, p=0·0016) implied that the difference in 30-day mortality odds between patients in intervention and comparison hospitals in the post-implementation period was significantly smaller than at baseline—only 12% higher (1·12, 0·91–1·37, p=0·28) and no longer significant (vs the significant difference of 34% higher at baseline).
Table 3:
Adjusted ORs and IRRs indicating the differences in mortality, readmissions, and length of stay between intervention and comparison hospitals (total n=55) and differential changes in those outcomes across timepoints
| 30-day mortality* |
7-day readmissions† |
Length of stay‡ |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | IRR (95% CI) | p value | |
| Intervention vs comparison at baseline | 1·34 (1·09–1·64) | 0·0052 | 1·15 (0·98–1·34) | 0·090 | 0·78 (0·72–0·84) | <0·0001 |
| Post-implementation vs baseline in comparison hospitals | 1·07 (0·97–1·17) | 0·18 | 1·06 (1·01–1·12) | 0·015 | 0·95 (0·93–0·98) | 0·0001 |
| Post-implementation vs baseline in intervention hospitals | 0·89 (0·84–0·95) | 0·0003 | 1·00 (0·95–1·04) | 0·92 | 0·91 (0·89–0·94) | <0·0001 |
| Interaction of intervention* post-implementation | 0·84 (0·75–0·93) | 0·0016 | 0·94 (0·88–0·99) | 0·049 | 0·95 (0·92–0·99) | 0·010 |
ORs for 30-day mortality and 7-day readmissions were estimated with random-intercept logistic regression models. IRRs for length of stay were estimated with zero-truncated negative binomial regression models. All models adjusted for the clustering of patients in hospitals and controlled for hospital size. DRG=Diagnosis-Related Group. IRR=incident rate ratio. OR=odds ratio.
Models for mortality also included risk scores to control for each patient’s probability of dying given their age, sex, comorbidities present, and DRGs. Cases involving obstetric deliveries were excluded from the analyses.
Models for 7-day readmission also included risk scores to control for each patient’s probability of readmission given their age, sex, comorbidities present, and DRGs. These models were restricted to short-term patients alone (length of stay ≤30 days) with routine discharge to home and excluded readmission for obstetric delivery.
Models for length of stay also controlled for whether patients died during their hospital stay and for their age, sex, comorbidities, and DRGs; and were restricted to short-term patients alone.
The main ORs and interaction effects for readmissions and IRRs for LOS showed a similar pattern (table 3). Patients in intervention hospitals initially had 15% higher odds on readmissions than those in comparison hospitals (adjusted OR 1·15, 0·98–1·34, p=0·090), and patients in comparison hospitals had a 6% increase in odds of readmission from baseline to post-implementation (1·06, 1·01–1·12, p=0·015). At the same time, no change over time was observed for patients in intervention hospitals (1·00, 0·95–1·04, p=0·92). The adjusted OR for the interaction (0·94, 0·88–0·99, p=0·049) implied that the difference in odds of readmission between patients in intervention and comparison hospitals in the post-implementation period was significantly smaller than at baseline—only 8% higher (1·08, 0·92–1·26, p=0·35) and no longer indicating a significant difference. Patients in intervention hospitals initially had 22% shorter LOS than those in comparison hospitals (adjusted IRR 0·78, 95% CI 0·72–0·84, p<0·0001). For patients in comparison hospitals, we observed a decrease in the average LOS by a factor of 0·95 (0·93–0·98, p=0·0001), or 5%. For patients in intervention hospitals, the decrease in LOS was even greater and equal to 0·91 (95% CI 0·89–0·94, p<0·0001), or by 9%. The adjusted OR for the interaction (0·95, 0·92–0·99, p=0·010) suggests that the difference in LOS between patients in intervention and those in comparison hospitals in the post-implementation period was even greater than at baseline—26% shorter LOS (0·74, 0·68–0·81, p<0·0001).
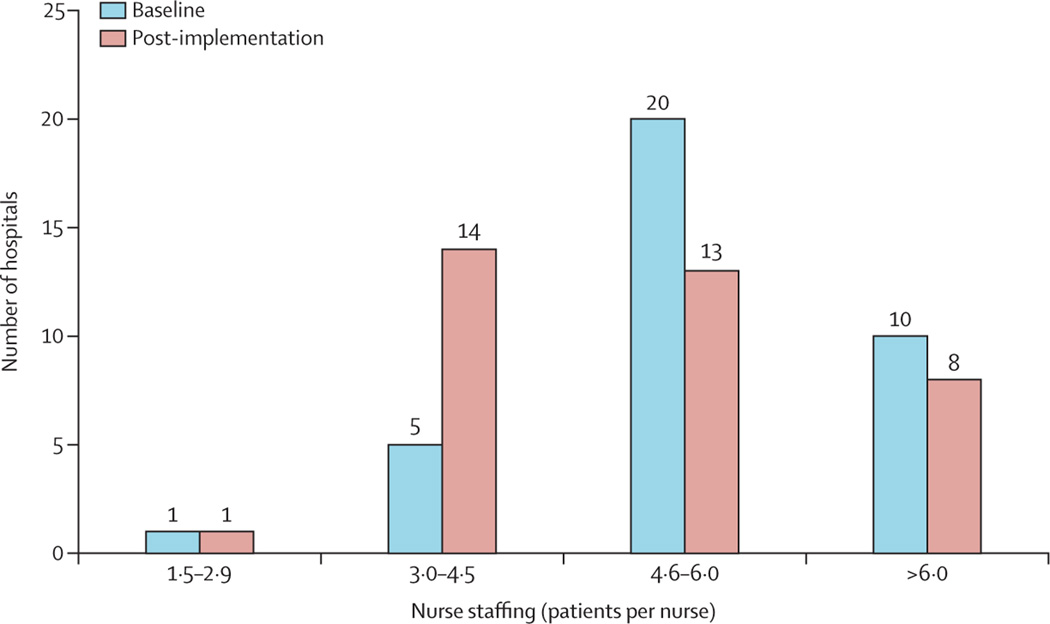
Subsequently, we focused on whether outcomes changes resulted from changes in staffing specifically. We eliminated the interaction between intervention and timepoint considered in the previous analyses and replaced it with an indicator of the staffing change over time and the effect on outcomes. The 36 hospitals for which we had reliable staffing measures included 21 (78%) of 27 intervention hospitals and 15 (54%) of 28 comparison hospitals. Staffing changed from baseline to post-implementation in these 36 hospitals ( figure). 30 (83%) hospitals had staffing that amounted to more than 4·5 patients per nurse at baseline, whereas the same was true for only 21 (58%) hospitals in the post-implementation period. Notably, only one comparison hospital had a marked decrease in the ratio of patients per nurse between timepoints (ie, from one ratio interval to a lower one in the figure) and, although average patients per nurse diminished by 0·47 in intervention hospitals, it diminished by 0·17 patients per nurse in comparison hospitals.
Figure:
Number of hospitals with various staffing levels at baseline and post-implementation
When staffing and changes in staffing were taken into account, the difference between intervention and comparison hospitals—the intervention effect—was significant only for LOS, while the overall change—the post-implementation effect—in readmissions and LOS remained significant (table 4). Most notably, the model showed that when staffing improves, or decreases by one patient per nurse, the odds on all three outcomes decrease significantly (table 4).
Table 4:
Adjusted ORs and IRRs indicating the differences in mortality, readmissions, and length of stay between intervention and comparison hospitals and the effect of changes in staffing on those outcomes across timepoints
| 30-day mortality* |
7-day readmissions† |
Length of stay‡ |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | IRR (95% CI) | p value | |
| Intervention effect | 1·26 (0·93–1·70) | 0·13 | 0·97 (0·84–1·11) | 0·61 | 0·79 (0·67–0·94) | 0·0065 |
| Post-implementation effect | 0·96 (0·91–1·01) | 0·12 | 1·03 (1·01–1·07) | 0·039 | 0·93 (0·91–0·95) | <0·0001 |
| Change in staffing, decrease of one patient per nurse | 0·93 (0·86–0·99) | 0·045 | 0·93 (0·89–0·97) | 0·0004 | 0·97 (0·94–0·99) | 0·035 |
DRG=Diagnosis-Related Group. IRR=Incident rate ratio. OR=odds ratio.
Models for mortality also included risk scores to control for each patient’s probability of dying given their age, sex, comorbidities present, and DRGs. Cases involving obstetric deliveries were excluded from the analyses.
Models for 7-day readmission also included risk scores to control for each patient’s probability of readmission given their age, sex, comorbidities present, and DRGs. These models were restricted to short-term patients alone (length of stay ≤30 days) with routine discharge to home and excluded readmission for obstetric delivery.
Models for length of stay also controlled for whether patients died during their hospital stay and for their age, sex, comorbidities, and DRGs; and were restricted to short-term patients alone.
Using the expected frequencies derived from our models, we estimated that, absent the policy, intervention hospitals could have expected to see 145 more deaths, 255 more readmissions, and 29 222 additional hospital days. It was estimated that 167 full-time equivalents were needed to meet ratio requirements (Mohle B, Queensland Nurses and Midwives’ Union, personal communication); at an average cost of AUD$100 000 (on the high end of the wage range) per full-time equivalent per year,32 the cost to fund these positions would amount to approximately $33 000 000 over the first 2 years post-implementation. Taking our estimates of LOS days and readmissions averted, we can estimate avoided costs. We used data from Australia’s Independent Hospital Pricing Authority33 on average hospital day costs in Queensland ($2312 in 2015–16) as the basis of our estimates. By preventing 255 readmissions with an average LOS of 2·7 days, the average costs avoided would be $1 589 594 (95% CI 1 179 120–2 358 240). By preventing 29 222 hospital days, the average costs avoided would be $67 561 264 (54 049 011–81 073 517).
Discussion
Our prospective panel study of Queensland hospitals revealed four key findings. First, the nurse-to-patient ratios mandate resulted in nurse staffing improvements at intervention hospitals that were significantly different from those in comparison hospitals, where staffing remained largely unchanged. This suggests that the improvements we observed were not part of a statewide secular trend of better nurse staffing; rather, the change was largely isolated to the hospitals prompted to improve by the policy. Second, intervention hospitals saw greater patient outcome improvements. Although intervention hospitals had patients who were sicker than those in comparison hospitals, and thus had somewhat worse baseline outcomes, their improvement in mortality, LOS, and readmissions was significantly better even after accounting for demographics, comorbidities, DRGs, and hospital size. Third, using data from medical-surgical ward nurses (the setting targeted by the policy), we found that changes in staffing in intervention hospitals accounted for a significant share of the outcome advantage for those hospitals. Finally, our estimates suggest that the policy resulted in significant cost savings.
This study also contributes to the understanding of the causal relationship between improved staffing and patient outcomes. The literature showing better outcomes in better staffed hospitals mostly involves cross-sectional studies; although they highlight clear associations, causality cannot necessarily be inferred.2–14 Some studies have examined longitudinal data and have determined that outcomes improve more when staffing similarly improves,23 but these studies relied on natural staffing change trends. Our study takes the additional step of informing whether direct state intervention yields better staffing, and whether those staffing improvements result in better patient outcomes. The answer to both questions was yes. Although probably not the only policy design that could stimulate staffing improvements and improved outcomes, Queensland’s policy implementation is a viable model offering lessons for other countries.
Our study has limitations. We refer to it as a quasi-experimental study, which is appropriate in the broad sense that it involves comparing a sample of comparison hospitals with intervention hospitals before and after the intervention—in this case an improvement in staffing—is observed in one group but not the other and in a natural setting rather than a controlled environment. However, the participating hospitals were not selected at random and were not assigned randomly to intervention and comparison groups—rather, intervention hospitals were chosen by the government. Moreover, comparison hospitals were not matched to intervention hospitals because we did not have the information needed for matching on many relevant characteristics and because the number of potential matches was insufficient for a very complete matching in any event. Therefore, we had to control for differences between hospitals using statistical controls rather than by design, or by using randomly selected and assigned hospitals. The higher prevalence of pre-existing conditions among patients in the intervention hospitals might have been due to the fact that intervention hospitals were larger (all comparison hospitals had fewer than 500 beds, whereas 22 [81%] of 27 intervention hospitals had fewer than 500 beds and five [19%] had more than 500 beds). However, our incorporation of patient-level measures of pre-existing conditions did adjust for a key observable factor that differentiated intervention from comparison hospitals, and the prospective panel design, with a focus on change over time, eliminated unobserved fixed effects that might have distinguished the two hospital groups. An additional limiting factor is that there were not enough medical-surgical nurses in some hospitals to reliably estimate the average staffing on medical-surgical wards, especially in small comparison hospitals. Nonetheless, most relevant patients were covered by the study hospital panel, suggesting that a nurse-to-patient ratio mandate would have a substantial public benefit.
The costs saved because of reduced LOS and readmissions were estimated to be more than twice the costs of the additional staffing needed to comply with the policy while also yielding lower mortality. This information on Queensland offers insights for the jurisdictions that are debating minimum nurse-to-patient ratio policies (eg, New York and Illinois in the USA, and others in Australia) and for the international interest in interventions to improve nurse staffing. The most recent debate over nurse-to-patient ratios was in 2017, in Massachusetts (USA), which proposed a ratios mandate by ballot initiative.34 The state was flooded with advertising from interested stakeholders against ratios, arguing that the evidence for ratios was insufficient. Opponents raised concerns that there had not been a prospective evaluation of a staffing policy such as the one described in this report, and thus evidence of effectiveness was unclear. Likewise, opponents argued that little information existed about the return on investment from the additional nurses required as a result of a ratios mandate. Our findings fill these gaps.
An argument raised when California implemented ratios was that the policy was inflexible, applying ratios to all nurses at all times—when a nurse needed to go to lunch or take a break, other nurses were needed to cover the patient assignment. But other nurses were often at their limit and couldn’t take additional patients, even for a short period, and still comply with the law. This frustrated managers and made implementation difficult for many hospitals, especially early on. By contrast, Queensland mandated a minimum average staffing level at the ward level—an individual nurse could have more or fewer so long as the average number of patients per nurse didn’t exceed the ratio limits. This offered more flexibility in patient assignments. Our analysis suggests that Queensland’s flexible design is feasible and yields good outcomes. The Queensland evaluation design has prompted similar policy research in the USA, with similar findings.35,36
In conclusion, having enough nurses with manageable workloads has been shown to be important for good patient care and outcomes. The 2018 International Council of Nurses’ Position Statement on Evidence-Based Nurse Staffing16 recommends that governments should take action to ensure safe staffing levels. The results presented here suggest that minimum nurse-to-patient ratio policies are a feasible instrument to improve nurse staffing, produce better patient outcomes, and yield a good return on investment.
Research in context.
Evidence before this study
We searched PubMed for original research articles published in English between Jan 1, 1985, and March 1, 2020, with the following search terms (separately and in combination): “nursing”, “staffing”, “nurse-to-patient ratios”, and “staffing mandate”. We also did a manual search based on bibliographies of relevant papers. In 2014, The Lancet published the largest international study on the subject, involving hundreds of thousands of patients in 300 hospitals across nine countries, showing that patients in hospitals with better nurse staffing levels were less likely to die in hospital than those being treated in poorly staffed hospitals. This study capped decades of research linking staffing levels to outcomes including mortality, readmissions, length of stay, adverse events, and patient satisfaction. Most research, however, has been cross-sectional; the few longitudinal studies have been done in single or a small number of hospitals. The small number of evaluations of implemented policy were retrospective and relied upon administrative staffing data known to overestimate staffing levels by including nurses who are not in patient care roles (eg, managers).
Added value of this study
Despite being frequently debated, policy tools to achieve safe nurse staffing levels have rarely been implemented—only a few jurisdictions have done so over the past 30 years. In the places that implemented such policies, no prospective evaluations linked with patient outcomes have been done. The absence of such an evaluation has been cited as a reason why similar policies have not been adopted elsewhere. In 2016, Queensland, Australia, implemented a policy establishing minimum nurse-to-patient ratios in medical-surgical wards in 27 public hospitals that care for 83% of patients hospitalised across the state. We report the findings of a first-of-its-kind prospective evaluation of Queensland’s policy. In addition to evaluating the effect of the policy on mortality, we examined outcomes with cost implications (ie, readmissions and length of stay) relevant to financial considerations of health ministers and hospital administrators. The findings can directly inform debates in jurisdictions considering similar policies.
Implications of all the available evidence
These results support decades of research that suggested that making changes to improve staffing levels could result in better outcomes. Policy interventions establishing minimum nurse-to-patient ratios are feasible and yield significantly better outcomes for patients and a better return on investment to the public.
Acknowledgments
This study was supported by grants from Queensland Health and the National Institutes of Health, National Institute of Nursing Research (R01NR014855). The authors are independent and solely responsible for study design, data collection and analysis, findings, and interpretation, which do not necessarily represent views of Queensland Health. We would like to acknowledge Tim Cheney, Frances Hughes, Irene Hung, Beth Mohle, Shelley Nowlan, Natalie Spearing, and Kate Veach for their contributions to this work.
Funding Queensland Health, National Institutes of Health, National Institute of Nursing Research.
Footnotes
Declaration of interests
We declare no competing interests.
Data sharing
The nurse survey data cannot be shared in any form as a condition of survey respondent consent. The patient data cannot be shared by the investigators under the data use agreement with Queensland Health; however, the original admitted patient data collection can be requested directly from Queensland Health.
Contributor Information
Matthew D McHugh, School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA.
Linda H Aiken, School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA.
Douglas M Sloane, School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA.
Carol Windsor, School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia; Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia.
Clint Douglas, School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia; Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia; Metro North Hospital and Health Service, Royal Brisbane and Women’s Hospital, Herston, QLD, Australia.
Patsy Yates, School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia; Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia.
References
- 1.WHO. 2020—Year of the Nurse and the Midwife. 2021. https://www.who.int/campaigns/annual-theme/year-of-the-nurse-and-the-midwife-2020 (accessed April 29, 2021).
- 2.Aiken LH, Sloane DM, Bruyneel L, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 2014; 383: 1824–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff DF. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care 2011; 49: 1047–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002; 288: 1987–93. [DOI] [PubMed] [Google Scholar]
- 5.Aiken LH, Sloane DM, Cimiotti JP, et al. Implications of the California nurse staffing mandate for other states. Health Serv Res 2010; 45: 904–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duffield C, Diers D, O’Brien-Pallas L, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res 2011; 24: 244–55. [DOI] [PubMed] [Google Scholar]
- 7.Lasater KB, McHugh MD. Nurse staffing and the work environment linked to readmissions among older adults following elective total hip and knee replacement. Int J Qual Health Care 2016; 28: 253–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011; 364: 1037–45. [DOI] [PubMed] [Google Scholar]
- 9.Silber JH, Rosenbaum PR, McHugh MD, et al. Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg 2016; 151: 527–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ball JE, Bruyneel L, Aiken LH, et al. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. Int J Nurs Stud 2018; 78: 10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cho E, Sloane DM, Kim EY, et al. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int J Nurs Stud 2015; 52: 535–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nantsupawat A, Srisuphan W, Kunaviktikul W, Wichaikhum OA, Aungsuroch Y, Aiken LH. Impact of nurse work environment and staffing on hospital nurse and quality of care in Thailand. J Nurs Scholarsh 2011; 43: 426–32. [DOI] [PubMed] [Google Scholar]
- 13.Rafferty AM, Clarke SP, Coles J, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud 2007; 44: 175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Twigg D, Duffield C, Bremner A, Rapley P, Finn J. The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: a retrospective analysis of patient and staffing data. Int J Nurs Stud 2011; 48: 540–48. [DOI] [PubMed] [Google Scholar]
- 15.International Council of Nurses. Evidence-based safe nurse staffing. Geneva: International Council of Nurses, 2018. [Google Scholar]
- 16.McHugh MD, Kelly LA, Sloane DM, Aiken LH. Contradicting fears, California’s nurse-to-patient mandate did not reduce the skill level of the nursing workforce in hospitals. Health Aff (Millwood) 2011; 30: 1299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerdtz MF, Nelson S. 5–20: a model of minimum nurse-to-patient ratios in Victoria, Australia. J Nurs Manag 2007; 15: 64–71. [DOI] [PubMed] [Google Scholar]
- 18.Van den Heede K, Cornelis J, Bouckaert N, Bruyneel L, Van de Voorde C, Sermeus W. Safe nurse staffing policies for hospitals in England, Ireland, California, Victoria and Queensland: a discussion paper. Health Policy 2020; 124: 1064–73. [DOI] [PubMed] [Google Scholar]
- 19.Lasater KB, Aiken LH, Sloane DM, et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf 2020; published online Aug 13. 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aiken M, Hage J. Organizational interdependence and intra-organizational structure. Am Sociol Rev 1968; 33: 912–30. [Google Scholar]
- 21.Dillman DA, Smyth JD, Christian LM. Internet, phone, mail, and mixed-mode surveys: the tailored design method. Hoboken, NJ: John Wiley & Sons, 2014. [Google Scholar]
- 22.Massey DS, Tourangeau R, eds. The nonresponse challenge to surveys and statistics. In: The annals of the American Academy of Political and Social Science; number 645. New York, NY: Sage, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Research Council. Chapter 1. The growing problem of nonresponse. In: Tourangeau R, Plewes TJ, eds. Nonresponse in social science surveys: a research agenda. Panel on a research agenda for the future of social science data collection, Committee on National Statistics. Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press, 2013. [Google Scholar]
- 24.Sloane DM, Smith HL, McHugh MD, Aiken LH. Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: a panel study. Med Care 2018; 56: 1001–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lasater KB, Jarrín OF, Aiken LH, McHugh MD, Sloane DM, Smith HL. A methodology for surveying organizational performance: a multistate survey of front-line providers. Med Care 2019; 57: 742–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahn KL, Brook RH, Draper D, et al. Interpreting hospital mortality data. How can we proceed? JAMA 1988; 260: 3625–28. [PubMed] [Google Scholar]
- 27.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994; 47: 1245–51. [DOI] [PubMed] [Google Scholar]
- 28.Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res 2008; 8: 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173: 676–82. [DOI] [PubMed] [Google Scholar]
- 30.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 2004; 57: 1288–94. [DOI] [PubMed] [Google Scholar]
- 31.Fairbrother M. Two multilevel modeling techniques for analyzing comparative longitudinal survey datasets. Political Sci Res Methods 2014; 2: 119–40. [Google Scholar]
- 32.Queensland Health. Wage rates—nursing stream. 2020. https://www.health.qld.gov.au/hrpolicies/salary/nursing (accessed April 29, 2021).
- 33.The Independent Hospital Pricing Authority. National hospital cost data collection cost report: round 20 financial year 2015–16. New South Wales, Australia: The Independent Hospital Pricing Authority, 2018. [Google Scholar]
- 34.Chen M. More nurses means better care—so why did this ballot measure fail? 2018. The Nation. https://www.thenation.com/article/archive/massachusetts-nurses-staffing-ballot/ (accessed April 29, 2021). [Google Scholar]
- 35.Lasater KB, Sloane DM, McHugh MD, et al. Evaluation of hospital nurse-to-patient staffing ratios and sepsis bundles on patient outcomes. Am J Infect Control 2020; published online Dec 10. 10.1016/j.ajic.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lasater KB, Aiken LH, Sloane DM, et al. Is hospital nurse staffing legislation in the public’s interest? An observational study in New York state. Med Care 2021; 59: 444–50. [DOI] [PMC free article] [PubMed] [Google Scholar]