Abstract
Importance:
Parents of children with severe neurological impairment (SNI) manage complex medication regimens (CMR) at home.
Objective:
To help clinicians support parents and simplify CMR, we used the Medication Regimen Complexity Index (MRCI) to measure the complexity and potentially modifiable aspects of CMR, and examine the association between MRCI scores and subsequent acute visits.
Design:
Cross-sectional study conducted between 4/1/19 and 12/31/20.
Setting:
Single-center, large, hospital-based complex care clinic.
Participants:
Subjects ages 1–18 years with SNI and ≥5 prescribed medications.
Intervention:
Home medication regimen complexity was assessed using MRCI scores. The total MRCI score is comprised of 3 subscores (dosage form, dose frequency, and specialized instructions).
Main Outcomes and Measures:
Patient-level counts of subscore characteristics and additional safety variables (total doses per day, high-alert medications, potential drug-drug interactions) were analyzed by MRCI score groups (low, medium, and high score tertiles). Associations between MRCI score groups and acute visits were tested using Poisson regression, adjusted for age, complex chronic conditions, and recent healthcare use.
Results:
Of 123 patients, 59% were males with a median age of 9 years. The median MRCI score was 46 (IQR: 35–61; range: 8–139); for the low MRCI group it was 29 (IQR: 24–35), the medium group 46 (IQR: 42–50); and the high group 69 (IQR: 61–78). Median unique dosage forms per patient was 6 (IQR: 4–7); dose frequencies was 7 (IQR: 5–9); and instructions was 5 (IQR: 4–8), with counts increasing significantly across higher MRCI groups. Similar trends occurred for total daily doses (median 31; IQR: 20–45), high-alert medications (3; IQR: 1–5), and potential drug-drug interactions (3; IQR: 0–6). Rates of 30-day acute visits were 1.3 times greater (95% CI: 0.6, 2.8) in the medium versus low group, and 2.4 times greater (95% CI: 1.1, 5.4) in the high versus low group.
Conclusions & Relevance:
Higher MRCI scores were driven by multiple dose frequencies, complicated by different dosage forms and instructions, and associated with subsequent acute visits. These findings suggest that clinical interventions to manage CMR could target various aspects of these regimens, such as the simplification of dosing schedules.
Trial Registration:
Registered with ClinicalTrials.gov (NCT03849066).
INTRODUCTION
Complex medication regimens (CMR)—usually defined as the use of ≥5 medications (polypharmacy) and the presence of multiple different medication dosing schedules—are common among children with medical complexity, including children with severe neurological impairment (SNI).1–3 Amidst other competing care activities, parents and non-medical caregivers of children with SNI must manage and administer CMR in the home setting.2 In prior studies of medication safety, parents have reported concerns about medication administration, adherence, and adverse drug events (ADEs).4–8 The difficulty of administering CMR can be impacted by a variety of clinically modifiable medication-related factors, including the total number of medications, different dose frequencies, dosage forms (such as pills versus liquids), and specialized instructions, yet many pediatric polypharmacy studies still only measure basic medication counts.9–20 To guide clinicians’ efforts to simplify CMR and to provide tailored support and education for parents who administer CMR, clinicians need an easy and comprehensive way to identify and measure the various aspects of CMR that drive medication complexity.21, 22
The Medication Regimen Complexity Index (MRCI) is a validated tool that assesses medication regimen complexity in adult and geriatric populations with polypharmacy, and the MRCI tool has the potential to be extrapolated to the pediatric population.16, 19 The MRCI score is intended to differentiate, for example, between a lower-complexity patient taking 10 medications, each as a single pill with once daily dosing, and a higher-complexity patient taking 10 medications, but each with different dosage forms and requiring multiple doses per day. The total MRCI score is comprised of three subscores calculated from commonly available elements of patients’ medication scripts (dosage form, dose frequency, and specialized instructions). MRCI scores have been used to identify adult patients most likely to benefit from pharmacist-led medication therapy management programs and have also shown value in predicting subsequent healthcare utilization and ADEs.19, 23
In this study, we used the MRCI tool to identify, measure, and understand pediatric CMR within a prototypical population of children with SNI and polypharmacy. We aimed to: 1) measure the parent-facing complexity of CMR using total MRCI scores and subscores; 2) describe medication-level characteristics corresponding to MRCI subscore domains; 3) describe patient-level characteristics of CMR corresponding to MRCI subscore domains, as well as additional medication safety variables [e.g., total daily doses, high-alert medications, and potential drug-drug interactions (PDDI)], stratified by tertiles of total MRCI scores; and, 4) test the hypothesis that higher total MRCI scores are associated with increased subsequent acute healthcare utilization, controlling for patient age, counts of complex chronic conditions (CCCs), and recent healthcare utilization.23, 24
METHODS
Study Design
This was a cross-sectional analysis of all patients enrolled in a larger study measuring symptoms and polypharmacy in children with SNI, as described in prior publications.25, 26 We analyzed patients’ reconciled medication information captured in the electronic health record (EHR) during a routine primary care visit, as well as patients’ subsequent 30-day acute primary care, emergency, and inpatient healthcare utilization. This study followed the STROBE checklist when writing our report.27 The parent study was approved by the Colorado Multiple Institutional Review Board and registered with ClinicalTrials.gov (NCT03849066).25, 26
Identification, Consent, and Enrollment of Subjects
Between 4/1/2019 and 12/31/2020, we obtained parental written consent, enrolled, and assessed English- and Spanish-speaking patients between the ages of 1–18 years with SNI and polypharmacy (≥5 medications) who received primary care in a large, hospital-based special healthcare needs clinic. Consistent with previous definitions, children with SNI were defined to have neurological diagnoses expected to last ≥12 months and resulting in systemic or multi-system physiologic impairment requiring pediatric subspecialty care.1, 28 The presence of SNI and counts of complex chronic conditions (CCCs) were identified using published classification systems based on International Classification of Disease 10th Revision Clinical Modification (ICD-10-CM) diagnosis codes.1, 29
Medication Data
Prescription and over-the-counter medications were reconciled by the clinician at the time of the visit. All data elements necessary to calculate MRCI scores were available, including generic medication name, dose, dosage form, dose frequency, and additional specialized instructions. To reflect parent-facing medication complexity, we excluded clinic- or inpatient-administered medications (e.g., vaccines, botulinum toxin injections, etc.). Medication classes were assigned using the Anatomic Therapeutic Chemical classification system.30
Medication Regimen Complexity Index (MRCI) Score and Subscores
MRCI scores were calculated automatically from EHR data using the MRCI tool, scoring instructions, and examples, which are publicly available.31 Conceptually, the total MRCI score for a CMR is the sum of 3 weighted subscores (dosage form, dose frequency, and specialized instructions), with increasing weights corresponding to the difficulty of administration.16, 19 Each weighted dosage form score (e.g., tablet = 1, liquid = 2) was counted once per CMR. Each weighted dose frequency score (e.g., once daily = 1, twice daily = 2, every 12 hours = 2.5) was counted once per medication. Each weighted specialized instruction score (e.g., take multiple units = 1, taper/increase dose = 2) was counted once per medication. In the simplest scenario, a tablet administered once daily has a dosage form subscore of 1, dose frequency subscore of 1, and an instruction subscore of 0, for a total MRCI score of 2. The total MRCI score has no upper limit because it is dependent on the total number of medications, and higher MRCI scores indicate more complex regimens. Because meaningful MRCI score thresholds have not yet been established within the pediatric population, we classified MRCI scores by tertiles into “low,” “medium,” and “high” categories.
Additional Medication Administration and Safety Characteristics of CMR
We assessed additional medication-safety related variables, including total daily doses, counts of high-alert medications, and counts of PDDIs.2, 32 Total daily dose counts were parameterized as: 1) minimum counts, based on scheduled medications and 2) maximum counts, based on scheduled medications plus PRN medications. High-alert medications have the potential to cause significant patient harm when used in error and were identified using published lists from the Institute for Safe Medication Practices.33 Finally, PDDI were identified using DrugBank’s interaction database.34 Interactions of moderate severity (“monitor and/or modify concomitant use”) and major severity (“avoid concomitant use”) were reported.34
Clinical and Healthcare Utilization Variables
Additional analytic variables were extracted from the patient’s EHR, including patient and parent demographic information; annual and visit ICD-10-CM diagnoses; and annual and subsequent 30-day acute healthcare utilization (acute primary care, emergency, and inpatient visits).
Statistical Analysis
Descriptive statistics and distributional graphs were used to describe the study population and the associated MRCI scores. Bivariate comparisons between patient characteristics/healthcare utilization and MRCI scores were evaluated using one-way ANOVA tests. Box plots were used to visualize the corresponding characteristics of CMR, stratified by MRCI score tertiles. Non-parametric tests of trend were used to assess for differences in median counts of characteristics of CMR across MRCI score categories. Multivariable Poisson regression was used to test the hypothesis that higher MRCI scores were associated with increased subsequent 30-day acute healthcare utilization, adjusting for variables known to be associated with acute healthcare utilization (age, number of CCCs, and acute healthcare utilization in the prior 30-days).24 Analyses were conducted using Stata 16.1, and significance was set at a 2-tailed P value <0.05.
RESULTS
Demographics and Characteristics of Study Patients and Parent Caregivers
Of the 123 patients with SNI included in the analysis, most patients were males (59%), white (76%) with a median age of 9 years (IQR: 5–13) and a high prevalence of ≥3 CCCs (60%) (Table 1). Patients frequently had ≥10 active medications (80%) directly prior to the clinical visit. Prior healthcare utilization was high, with numerous outpatient medical visits (42% with ≥20 annually), emergency visits (41% with ≥2 annually), and inpatient stays (50% with ≥2 annually). The parent caregivers for the study patients were primarily between 30 and 50 years-old (77%), female (86%), non-Hispanic or Latino (76%), white (79%), and had some college education (80%). Fifty percent of patients had ≥1 day per week of nurse-provided care.
Table 1.
Demographics and clinical characteristics of children with severe neurological impairment by MRCI score.
| % (N=123) |
MRCI Mean Score |
95% CI | One-Way ANOVA |
|
|---|---|---|---|---|
| Patient Age at Visit (years) | ||||
| 1–4 | 20.3 | 44.8 | (39.0, 50.6) | 0.198 |
| 5–8 | 27.6 | 54.9 | (49.2, 60.6) | |
| 9–12 | 28.5 | 49.1 | (40.5, 57.7) | |
| 13–17 | 23.6 | 45.2 | (37.1, 53.3) | |
| Patient Sex | ||||
| Male | 59.3 | 49.6 | (44.3, 54.9) | 0.659 |
| Female | 40.7 | 47.9 | (43.1, 52.7) | |
| Patient Race | ||||
| American Indian/Alaska Native | 0.8 | 69.0 | NA | 0.912 |
| Black/African American | 4.1 | 48.1 | (33.6, 62.6) | |
| White | 76.4 | 49.0 | (44.5, 53.5) | |
| More than one race | 13.8 | 48.7 | (41.6, 55.8) | |
| Not Specified | 4.9 | 45.6 | (29.4, 61.8) | |
| Patient Ethnicity | ||||
| Not Hispanic or Latino | 76.4 | 49.1 | (44.5, 53.7) | 0.883 |
| Hispanic or Latino | 23.6 | 48.4 | (42.9, 53.9) | |
| CCC Category | ||||
| 1–2 | 39.8 | 42.1 | (37.1, 47.1) | <0.001 |
| 3–4 | 44.7 | 49.5 | (44.2, 54.8) | |
| 5+ | 15.4 | 64.8 | (54.5, 75.1) | |
| Rx Count (Pre-Visit) | ||||
| 5–9 | 20.3 | 28.9 | (24.8, 33.0) | <0.001 |
| 10–14 | 35.8 | 41.0 | (37.1, 44.9) | |
| 15+ | 43.9 | 64.7 | (59.8, 69.6) | |
| Outpatient Visits in Past Year | ||||
| 1–9 | 24.4 | 38.2 | (32.6, 43.8) | 0.003 |
| 10–19 | 34.1 | 49.3 | (43.7, 54.9) | |
| 20–29 | 22.0 | 51.4 | (44.8, 58.0) | |
| 30+ | 19.5 | 59.0 | (47.6, 70.4) | |
| ED Visits in Past Year | ||||
| 0 | 43.1 | 46.6 | (41.5, 51.7) | 0.099 |
| 1 | 16.3 | 45.7 | (38.6, 52.8) | |
| 2 | 17.9 | 46.4 | (38.6, 54.2) | |
| 3+ | 22.8 | 57.6 | (47.5, 67.7) | |
| Inpatient Visits in Past Year | ||||
| 0 | 27.6 | 38.9 | (33.8, 44.0) | <0.001 |
| 1 | 22.8 | 43.8 | (37.0, 50.6) | |
| 2 | 19.5 | 56.8 | (48.3, 65.3) | |
| 3+ | 30.1 | 56.9 | (49.6, 64.2) | |
| Parent Education | ||||
| Some high school | 4.1 | 49.2 | (28.2, 70.2) | 0.838 |
| High school graduate | 14.8 | 45.0 | (38.0, 52.0) | |
| Some college or technical school | 39.3 | 50.3 | (43.4, 57.2) | |
| College graduate | 41.8 | 49.5 | (44.2, 54.8) | |
| Nurse-Provided Care | ||||
| 0 Days per Week | 48.0 | 45.8 | (40.5, 51.1) | 0.063 |
| 1–3 Days per Week | 17.9 | 47.9 | (37.7, 58.1) | |
| 4–7 Days per Week | 31.7 | 55.5 | (49.8, 61.2) | |
| Not Specified | 2.4 | 31.7 | (19.4, 44.0) |
Medication Regimen Complexity Index (MRCI) Scores and Subscores
The median total MRCI score for patients was 46 (IQR: 35–61; range: 8–139), and the low MRCI group had a median score of 29 (IQR: 24–35), the medium group 46 (IQR: 42–50); and the high group 69 (IQR: 61–78) (Figure 1). The median MRCI “dosage form” subscore was 14 (IQR: 9–18), the “dose frequency” subscore was 25 (IQR: 19–39), and the “additional instructions” subscore was 6 (IQR: 4–9). Each MRCI subscore contributed differentially to the MRCI total score (Figure 1), with the “dose frequency” subscore contributing most to medication complexity, particularly at higher total MRCI scores. Total MRCI scores varied significantly by certain demographic characteristics (number of CCCs, total number of medications) and preceding healthcare use (outpatient visits and inpatient visits) (Table 1). MRCI scores did not differ significantly by age, sex, race, ethnicity, annual emergency visits, parent education level, or days of parent- or nurse-provided care.
Figure 1. Distribution of MRCI subscores by total MRCI scores in children with severe neurological impairment.
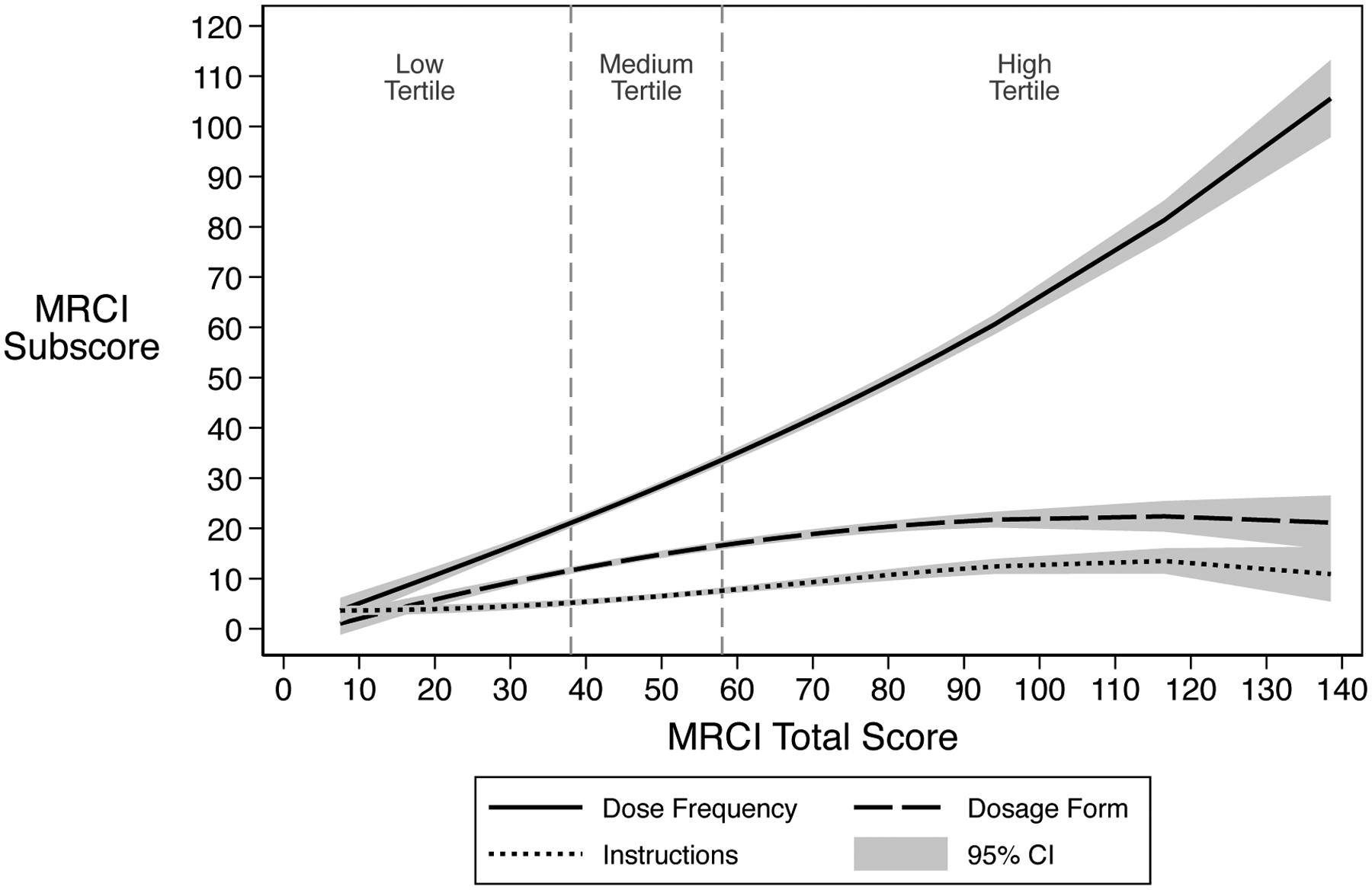
This graph displays fractional polynomial plots of MRCI subscores associated with total MRCI scores. The vertical reference lines display thresholds for the low, medium, and high MRCI total score tertiles.
Medication-Level Characteristics of CMR by MRCI Subscore Domains
Patients were prescribed a total of 1,772 prescriptions comprised of 210 distinct generic medications (Supplemental eTable 1). Regarding dose forms, capsules/tablets comprised 31.6% of medications and liquids comprised 26.0% of medications (Figure 2a). More than half (51.8%) of all scheduled individual medications required ≥2 doses per day (Figure 2b), most frequently antiepileptics (15.1% of scheduled medications with ≥2 doses per day), asthma medications (14.3%), antacids (8.9%), systemic steroids (6.5%), and anxiolytics (4.4%). Similarly, 60.6% of all PRN medications had recommended dose frequencies of ≥2 doses per day, while 33.3% were PRN without a specified dose frequency (Figure 2c). Finally, 34.8% of medications had ≥1 associated specialized instruction(s), most frequently indicating specific times of administration (13.2%), use of multiple units (11.4%), and medication mixing/dissolving instructions (8.2%) (Figure 2d).
Figure 2. Medication-level characteristics of complex medication regimens related to MRCI subscores in children with severe neurological impairment.
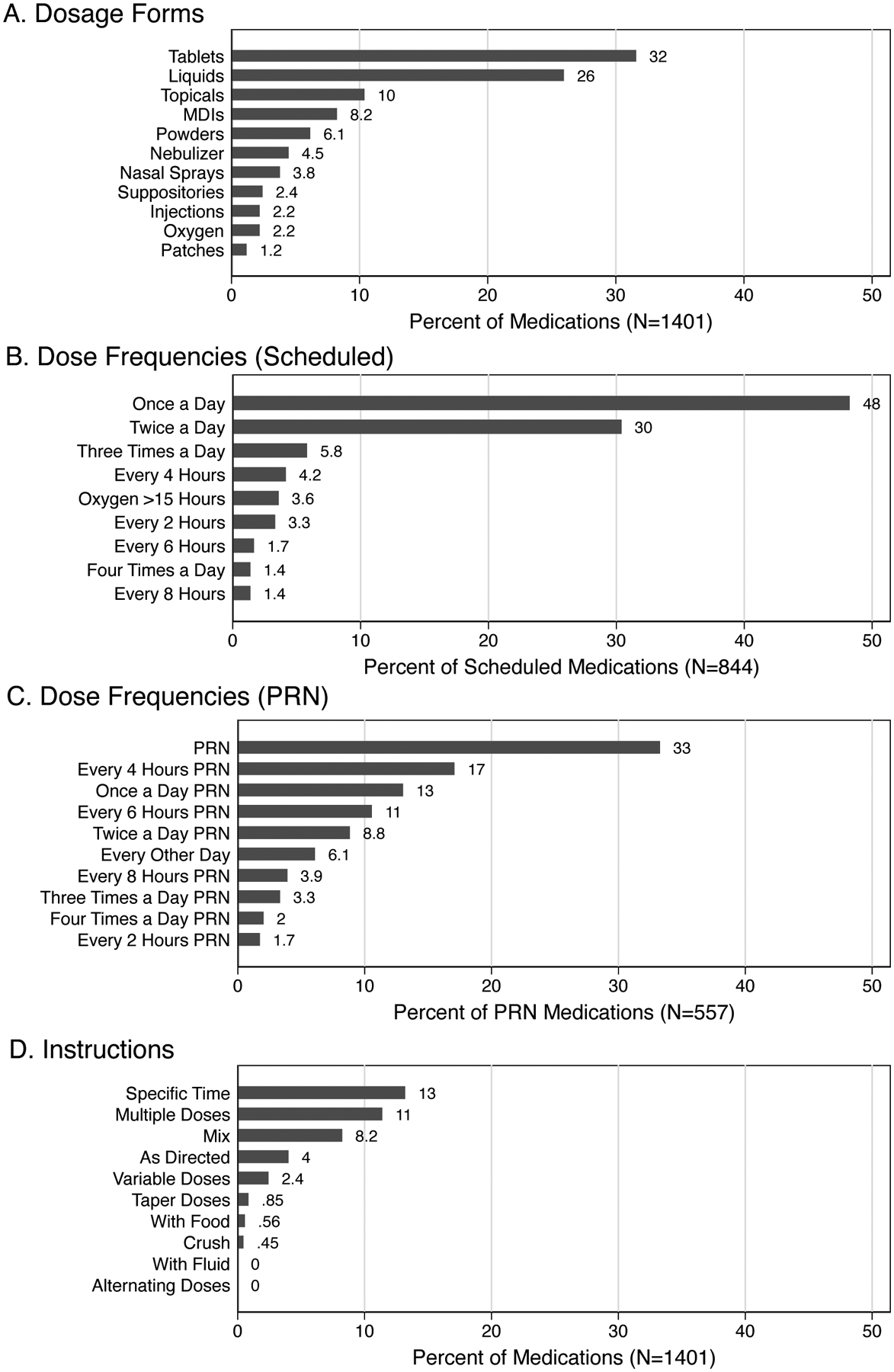
Panel A displays the percentage distribution of dosage forms among all medications. Panel B displays the percentage distribution of dose frequencies among all scheduled medications. Panel C displays the percentage distribution of dose frequencies among all PRN medications. Panel D displays the percentage distribution of additional instructions among all medications.
Patient-Level Characteristics of CMR by MRCI Total Scores
Overall, median counts of different dosage forms per day was 6 (IQR: 4–7), dose frequencies per day was 7 (IQR: 5–9), and additional instructions was 5 (IQR4–8) (Figure 3a). Similarly, median total scheduled doses of medication per day was 16 (IQR: 11–26), PRN medication doses per day was 12 (IQR: 7–20), and total doses of medication per day was 31 (IQR: 20–45) (Figure 3b). Finally, median counts of high-risk medications per participant was 3 (IQR: 1–5), moderate PDDIs was 3 (IQR: 0–6), and major PDDIs was 0 (IQR: 0–3) (Figure 3c). For each of the characteristics of CMR, the median counts increased significantly across higher MRCI score groups (Figure 3).
Figure 3. Characteristics of complex medication regimens at the patient-level by MRCI tertile in children with severe neurological impairment.
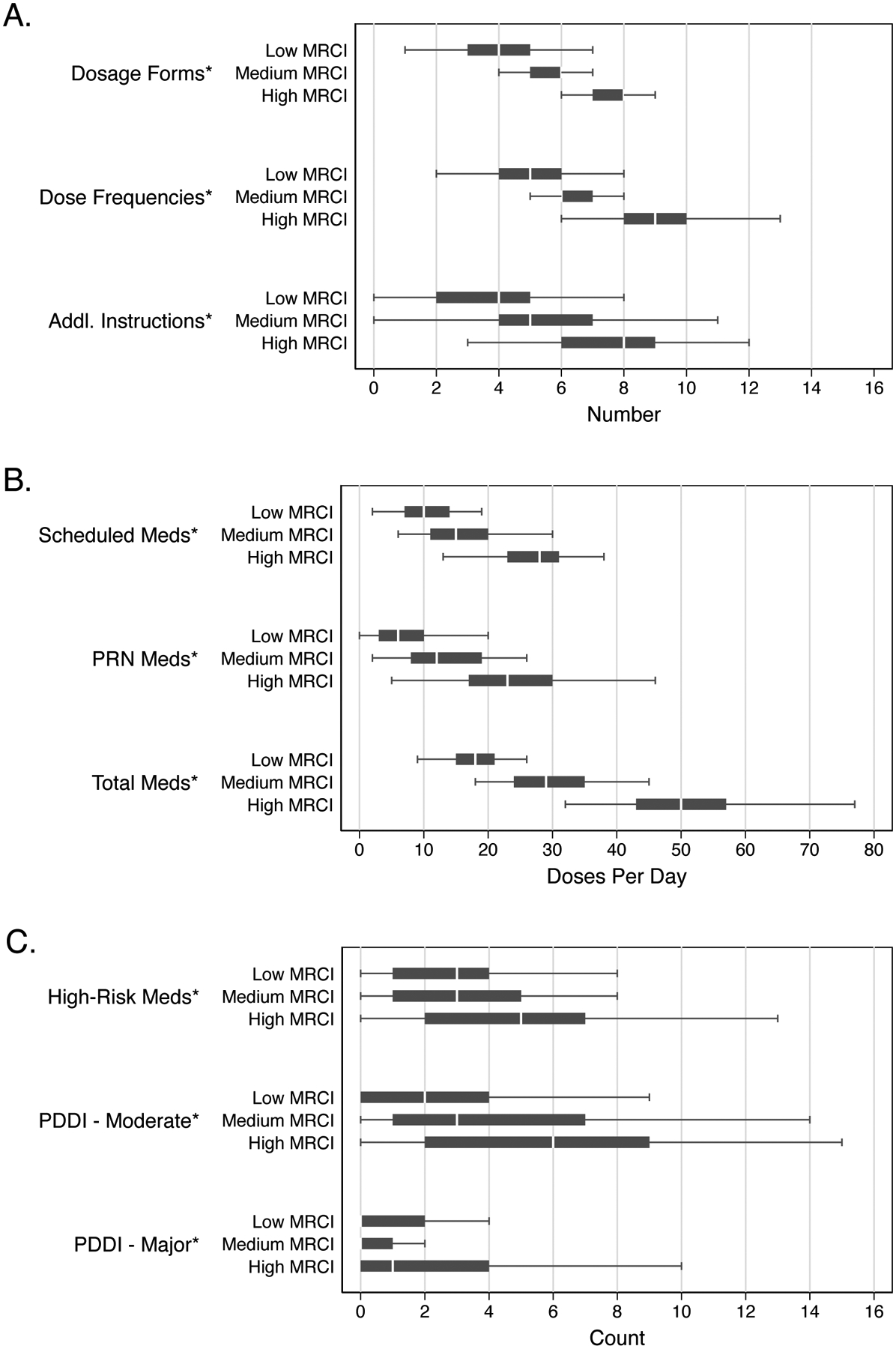
Panel A displays median counts and IQRs for unique dosage forms per patient, dose frequencies per patient, and additional instructions per patient. Panel B displays median counts and interquartile ranges (IQRs) for scheduled medication doses per patient per day excluding PRN medications, PRN medications per patient per day, and total doses per patient per day. Panel C displays median counts and IQRs for high-risk medications per patient, and moderate and major potential drug-drug interactions per patient. (*) denotes a significant increasing trend across MRCI score groups evaluated with non-parametric tests of trend, p<0.05.
Association Between MRCI Scores and 30-Day Acute Healthcare Utilization
Unadjusted 30-day incidence rates of acute healthcare utilization were 0.3 visits per person-month in the low MRCI group were, 0.4 visits per person-month in the medium MRCI group, and 0.7 visits per person-month in the high MRCI group (Table 2). After adjustments for age, number of CCCs, and preceding 30-day healthcare utilization, the incidence rate of subsequent 30-day acute visits was 1.3 times greater (95%CI: 0.6, 2.8) in the medium group and 2.4 times greater (95% CI: 1.1, 8.8) in the high group (Table 2).
Table 2.
Association between MRCI total scores and subsequent 30-day acute healthcare utilization in children with severe neurological impairment.
| N | Acute Visits | Unadjusted IRR (95% CI) | Adjusted IRR (95% CI) |
|
|---|---|---|---|---|
| Patient Age (years) | ||||
| 1–4 | 25 | 20 | 2.80 (1.31, 5.98) | 2.61 (1.16, 5.88) |
| 5–8 | 34 | 15 | 1.54 (0.69, 3.44) | 1.30 (0.58, 2.93) |
| 9–12 | 35 | 10 | Ref. | Ref. |
| 13–17 | 29 | 11 | 1.33 (0.56, 3.13) | 1.36 (0.57, 3.25) |
| CCC Category | ||||
| 1–2 | 49 | 16 | Ref. | Ref. |
| 3–4 | 55 | 25 | 1.39 (0.74, 2.61) | 1.05 (0.55, 2.01) |
| 5+ | 19 | 15 | 2.42 (1.20, 4.89) | 1.04 (0.45, 2.38) |
| MRCI Score Category | ||||
| Low MRCI | 41 | 11 | Ref. | Ref. |
| Medium MRCI | 41 | 15 | 1.36 (0.63, 2.97) | 1.26 (0.57, 2.78) |
| High MRCI | 41 | 30 | 2.72 (1.37, 5.44) | 2.42 (1.10, 5.35) |
| 30-Day Acute Visits (Pre-Visit) | 123 | 56 | 1.47 (1.21, 1.77) | 1.23 (0.99, 1.53) |
DISCUSSION
Children with SNI and polypharmacy displayed a broad range of medication regimen complexity, with MRCI scores ranging from 8 to 139, with a median MRCI score of 46. During non-acute routine clinical visits, children with SNI had substantially higher median MRCI scores than those reported in other analogous populations. Adults with autism spectrum disorder had mean MRCI scores of 14.6 (range: 0–89) and complex geriatric polypharmacy patients had average scores from 9.9 in the primary care setting to 30.3 at hospital discharge, with scores ≥22 predictive of unplanned 30-day readmissions.23, 35–41 A quarter of all medications were liquids (measuring liquids contributes to both complexity and higher risk for dosing errors) and 51% of all scheduled individual medications required ≥2 doses per day.8, 12, 42 Multiple different dose frequencies per patient were a driver of higher MRCI scores, which for those in the high MRCI group manifested as a median of 50 total daily doses per day. Additional characteristics of CMR directly impacting patient safety, including counts of high-alert medications and PDDIs, were also associated with higher MRCI scores. Finally, consistent with geriatric literature, higher MRCI scores in the current study were associated with increased subsequent 30-day acute healthcare utilization.19, 23, 43–46
These findings have several implications for the identification, clinical management, and ongoing monitoring of children with the most complex medication regimens.
First, MRCI scores are easily calculated, and can optimize the identification of patients who would benefit from clinical management ideally coordinated by primary care providers and pharmacists. Even within an already complex population of children with polypharmacy, correct identification of children with the most complex medication regimens is important for efficiency and safety, especially when clinical pediatric pharmacist support is limited.47, 48 Currently, no other standard measures of pediatric medication complexity are routinely employed to trigger CMR management. Evidence-based MRCI thresholds could flag a patient’s electronic health record in real time to indicate need for pharmacist review and medication therapy management interventions to simplify CMR.11, 49 Within healthcare systems, quantifying the volume of patients who would benefit from pharmacist-led interventions would help substantiate the need and value of providing dedicated pharmacist support within complex care programs and medical homes.20, 50
Next, primary care clinicians and pharmacists could use MRCI scores during clinical encounters to direct efforts to deprescribe and simplify CMR. Based on the MRCI subscores in this population of children with SNI, clinicians should first focus on ways to reduce total doses per day, through reductions in dose frequency or numbers of medications. In our experience, dose frequency reductions may be achieved by evaluating regimens for: 1) substitution with a therapeutic equivalent allowing for fewer doses per day; or, 2) dosage form optimization to change from immediate-release preparations to less frequent extended-release preparations, with the caveat that extended-release products cannot be crushed for enteral administration. Further reductions in total number of medications can be achieved by evaluating regimens for: 1) removal of therapeutic duplications; 2) opportunities to wean chronic medications used for well-controlled stable disease states, especially for legacy medications started years ago, where therapy may no longer be necessary; and 3) outgrown doses, used as an opportunity to determine if the drug is still needed, rather than simply increasing to a weight-appropriate dose.
Reductions in doses per day may not always be possible, so pharmacists may support parents through additional tailored solutions and specific education interventions. Pill-packs or pill boxes can be used to group medications that can be administered together at a common time, effectively reducing administration burden.51 When MRCI subscores reveal complexity due to multiple dosage forms or specialized instructions, pharmacist-led demonstrations and practice opportunities may improve parental confidence administering medications.2, 5, 52 A subset of liquid dosage forms require extemporaneous compounding; risks related to compounded medications may be reduced by switching to commercially available products, for example, tablets or capsules that can be crushed or opened. Standardization of specialized instructions, made available in multiple languages and with diagrams, could also reduce variability in clinicians’ free-text prescription instructions and improve parental understanding and confidence.8, 12, 42, 52
Finally, for children with CMR, studying the downstream clinical impact of interventions that reduce medication regimen complexity is difficult because no standard method is consistently used to measure pediatric CMR, either as an predictor or an outcome variable.20, 53 Moreover, in patient populations where medication changes occur frequently or simultaneously, without a composite measure of medication regimen complexity, determining the effect of a single medication change amidst a milieu of multiple medication changes is daunting. Rather, the composite MRCI score captures changes resulting from interventions affecting dosage forms, dose frequencies, and additional instructions, and MRCI scores may prove useful in tracking medication regimen complexity over time. Interventions to simplify and optimize CMR should be evaluated by longitudinally analyzing the relationship between MRCI scores and important clinical outcomes, such as patient- or parent-reported symptoms, exposure to PDDIs or high-alert medications, evidence of ADEs, or acute healthcare utilization.10, 23 For example, our finding that increased 30-day acute care utilization was associated the highest MRCI score group warrants further investigation. Given the confounding between complexity of the patient and CMR, we should not assume that reductions in MRCI scores would reduce acute healthcare utilization. Higher MRCI scores may instead reflect severity of illness rather than contributing directly to ADEs. Further evaluations of causality should employ a consistent measure of medication regimen complexity, such as MRCI scores, to reduce methodologic heterogeneity.20, 53
STUDY LIMITATIONS
Our study must be considered in the context of four limitations. First, this study was conducted at a single center in a primarily white, non-Hispanic, and English-speaking population with a focused and thus limited (albeit typical) set of severe neurological conditions. The utility of MRCI scores should be tested in diverse populations of children with medical complexity and different underlying disease processes. Second, the chosen thresholds for MRCI score groups were based on score percentiles rather than absolute cut points because no prior pediatric MRCI benchmarks were available. Until MRCI score data is generated for broader pediatric populations with different disease processes, the thresholds used in this study should not be used as absolute thresholds. Third, MRCI scores do not capture all unique pediatric-specific aspects of a medication regimen that may add significant complexity, such as compounded medications, use of enteral feeding tubes, or number of unique caregivers administering medications. Because these important CMR aspects often occur in the care of children, pediatric-specific modification and validation of the MRCI tool may be valuable. Finally, based on previous reports linking MRCI scores to acute care utilization due to ADEs, we used acute healthcare utilization as a proxy for medication-related issues (after adjusting for other markers of medical complexity). We did not, however, perform a causality assessment of ADEs.54
CONCLUSIONS
MRCI scores are easily calculated from readily available medication data in the EHR and can provide meaningful and actionable information. As MRCI scores increased, parents administered many more doses of medications per day, complicated by different dosage forms and specialized instructions. Higher MRCI scores were associated with increased subsequent acute healthcare utilization. These findings suggest that clinical interventions to manage CMR could target various aspects of these regimens, such as the simplification of dosing schedules.
Supplementary Material
Supplemental eTable 1. Medications used by MRCI tertile in children with severe neurological impairment.
KEY POINTS.
Question:
How complex are the medication regimens for children with neurological impairment?
Findings:
In this cross-sectional study of 123 neurologically impaired children, empirically measured Medication Regimen Complexity Index (MRCI) scores were high, driven by a median of 31 total daily doses of medication per patient; 7 different dose frequencies per patient; 6 unique dosage forms per patient; and 5 specialized instructions per patient. Higher MRCI scores were associated with increased subsequent acute healthcare utilization.
Meaning:
These findings suggest that clinical interventions to manage medication regimen complexity could target various aspects of these regimens, such as the simplification of dosing schedules.
ACKNOWLEDGEMENTS
Funding/Support:
Dr. Feinstein was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K23HD091295.
Role of the Funder/Sponsor:
The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations:
- ADE
adverse drug event
- CCC
complex chronic condition
- CMR
complex medication regimen
- EHR
electronic health record
- ICD-10-CM
International Classification of Disease, 10th Revision
- MRCI
Medication Regimen Complexity Index
- PRN
pro re nata (as needed)
- SNI
severe neurological impairment
Footnotes
Conflict of Interest Disclosures: Dr. Feinstein is Chair of the State of Colorado Medicaid Pharmacy and Therapeutics Committee. Dr. Blackmer has performed consultative services to Wolters Kluwer, Pediatric and Neonatal Lexi-Drugs. Dr. Blackmer also serves as a member of the Drug Utilization Review Board for Colorado Department of Health Care Policy and Financing. There are no other conflicts of interest relevant to this article to disclose.
Publisher's Disclaimer: Disclaimer: The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or the U.S. government.
Data Access, Responsibility, and Analysis: Dr. Feinstein had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Data Sharing Statement: All data collected as part of this study will be released in accordance with standard NIH data sharing policies and procedures after completion of the larger parent study described on ClinicalTrials.gov (NCT03849066).
Originality of Content: All presented information and materials are original.
REFERENCES
- 1.Thomson JE, Feinstein JA, Hall M, Gay JC, Butts B, Berry JG. Identification of Children With High-Intensity Neurological Impairment. JAMA Pediatr. August192019;doi: 10.1001/jamapediatrics.2019.2672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blackmer AB, Fox D, Arendt D, Phillips K, Feinstein JA. Perceived Versus Demonstrated Understanding of the Complex Medications of Medically Complex Children. J Pediatr Pharmacol Ther. 2021;26(1):62–72. doi: 10.5863/1551-6776-26.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feinstein JA, Hall M, Antoon JW, et al. Chronic Medication Use in Children Insured by Medicaid: A Multistate Retrospective Cohort Study. Pediatrics. April2019;143(4)doi: 10.1542/peds.2018-3397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edelstein H, Schippke J, Sheffe S, Kingsnorth S. Children with medical complexity: a scoping review of interventions to support caregiver stress. Child Care Health Dev. May2017;43(3):323–333. doi: 10.1111/cch.12430 [DOI] [PubMed] [Google Scholar]
- 5.Philips K, Zhou R, Lee DS, et al. Caregiver Medication Management and Understanding After Pediatric Hospital Discharge. Hosp Pediatr. November2019;9(11):844–850. doi: 10.1542/hpeds.2019-0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents’ medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. February2010;164(2):181–6. doi: 10.1001/archpediatrics.2009.269 [DOI] [PubMed] [Google Scholar]
- 7.Zandieh SO, Goldmann DA, Keohane CA, Yoon C, Bates DW, Kaushal R. Risk factors in preventable adverse drug events in pediatric outpatients. J Pediatr. February2008;152(2):225–31. doi: 10.1016/j.jpeds.2007.09.054 [DOI] [PubMed] [Google Scholar]
- 8.You MA, Nam SM, Son YJ. Parental Experiences of Medication Administration to Children at Home and Understanding of Adverse Drug Events. J Nurs Res. September2015;23(3):189–96. doi: 10.1097/jnr.0000000000000080 [DOI] [PubMed] [Google Scholar]
- 9.Ferreira JM, Galato D, Melo AC. Medication regimen complexity in adults and the elderly in a primary healthcare setting: determination of high and low complexities. Pharm Pract (Granada). Oct-Dec 2015;13(4):659. doi: 10.18549/PharmPract.2015.04.659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wimmer BC, Cross AJ, Jokanovic N, et al. Clinical Outcomes Associated with Medication Regimen Complexity in Older People: A Systematic Review. J Am Geriatr Soc. April2017;65(4):747–753. doi: 10.1111/jgs.14682 [DOI] [PubMed] [Google Scholar]
- 11.Dahmash DT, Shariff ZB, Kirby DJ, Terry D, Huynh C. Literature review of medication administration problems in paediatrics by parent/caregiver and the role of health literacy. BMJ Paediatr Open. 2020;4(1):e000841. doi: 10.1136/bmjpo-2020-000841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris LM, Dreyer BP, Mendelsohn AL, et al. Liquid Medication Dosing Errors by Hispanic Parents: Role of Health Literacy and English Proficiency. Acad Pediatr. May-Jun 2017;17(4):403–410. doi: 10.1016/j.acap.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bakaki PM, Horace A, Dawson N, et al. Defining pediatric polypharmacy: A scoping review. PLoS One. 2018;13(11):e0208047. doi: 10.1371/journal.pone.0208047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker C, Feinstein JA, Ma X, et al. Variation of the prevalence of pediatric polypharmacy: A scoping review. Pharmacoepidemiol Drug Saf. March2019;28(3):275–287. doi: 10.1002/pds.4719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. October102017;17(1):230. doi: 10.1186/s12877-017-0621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.George J, Phun YT, Bailey MJ, Kong DC, Stewart K. Development and validation of the medication regimen complexity index. The Annals of pharmacotherapy. September2004;38(9):1369–76. doi: 10.1345/aph.1D479 [DOI] [PubMed] [Google Scholar]
- 17.Wimmer BC, Bell JS, Fastbom J, Wiese MD, Johnell K. Medication Regimen Complexity and Polypharmacy as Factors Associated With All-Cause Mortality in Older People: A Population-Based Cohort Study. The Annals of pharmacotherapy. February2016;50(2):89–95. doi: 10.1177/1060028015621071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paquin AM, Zimmerman KM, Kostas TR, et al. Complexity perplexity: a systematic review to describe the measurement of medication regimen complexity. Expert opinion on drug safety. November2013;12(6):829–40. doi: 10.1517/14740338.2013.823944 [DOI] [PubMed] [Google Scholar]
- 19.Hirsch JD, Metz KR, Hosokawa PW, Libby AM. Validation of a patient-level medication regimen complexity index as a possible tool to identify patients for medication therapy management intervention. Pharmacotherapy. August2014;34(8):826–35. doi: 10.1002/phar.1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auger KA, Shah SS, Davis MM, Brady PW. Counting the Ways to Count Medications: The Challenges of Defining Pediatric Polypharmacy. J Hosp Med. August2019;14(8):506–507. doi: 10.12788/jhm.3213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sluggett JK, Ooi CE, Gibson S, et al. Simplifying Medication Regimens for People Receiving Community-Based Home Care Services: Outcomes of a Non-Randomized Pilot and Feasibility Study. Clinical interventions in aging. 2020;15:797–809. doi: 10.2147/CIA.S248377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bogler O, Roth D, Feinstein J, Strzelecki M, Seto W, Cohen E. Choosing medications wisely: Is it time to address paediatric polypharmacy? Paediatrics & Child Health. 2019:pxy188–pxy188. doi: 10.1093/pch/pxy188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoonover H, Corbett CF, Weeks DL, Willson MN, Setter SM. Predicting potential postdischarge adverse drug events and 30-day unplanned hospital readmissions from medication regimen complexity. Journal of patient safety. December2014;10(4):186–91. doi: 10.1097/PTS.0000000000000067 [DOI] [PubMed] [Google Scholar]
- 24.Zhou H, Roberts PA, Dhaliwal SS, Della PR. Risk factors associated with paediatric unplanned hospital readmissions: a systematic review. BMJ Open. January282019;9(1):e020554. doi: 10.1136/bmjopen-2017-020554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feinstein JA, Feudtner C, Blackmer AB, et al. Parent-Reported Symptoms and Medications Used Among Children With Severe Neurological Impairment. JAMA Netw Open. December12020;3(12):e2029082. doi: 10.1001/jamanetworkopen.2020.29082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feinstein JA, Feudtner C, Valuck RJ, et al. Identifying Important Clinical Symptoms in Children With Severe Neurological Impairment Using Parent-Reported Outcomes of Symptoms. JAMA Pediatr. November12020;174(11):1114–1117. doi: 10.1001/jamapediatrics.2020.2987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. October202007;370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 28.Thomson J, Hall M, Nelson K, et al. Timing of Co-occurring Chronic Conditions in Children With Neurologic Impairment. Pediatrics. January72021;doi: 10.1542/peds.2020-009217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feinstein JA, Russell S, DeWitt PE, Feudtner C, Dai D, Bennett TD. R Package for Pediatric Complex Chronic Condition Classification. JAMA Pediatr. April232018;172(6):596–598. doi: 10.1001/jamapediatrics.2018.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment, 2020.
- 31.Electronic Data Capture and Coding Tool for Medication Regimen Complexity. Accessed6/19/2021, https://pharmacy.cuanschutz.edu/research/MRCTool
- 32.Antoon JW, Hall M, Herndon A, et al. Prevalence of Clinically Significant Drug-Drug Interactions Across US Children’s Hospitals. Pediatrics. November2020;146(5)doi: 10.1542/peds.2020-0858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institute for Safe Medication Practices. High-Alert Medications in Community/Ambulatory Settings. https://www.ismp.org/recommendations/high-alert-medications-community-ambulatory-list
- 34.Wishart DS, Knox C, Guo AC, et al. DrugBank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. January12006;34(Database issue):D668–72. doi: 10.1093/nar/gkj067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barnette DJ, Hanks C, Li W, Porter K. Patient-Level Medication Regimen Complexity in an Adolescent and Adult Population with Autism Spectrum Disorders. Pharmacotherapy. June2019;39(6):636–644. doi: 10.1002/phar.2202 [DOI] [PubMed] [Google Scholar]
- 36.Ferreira JM, Galato D, Melo AC. Medication regimen complexity in adults and the elderly in a primary healthcare setting: determination of high and low complexities. Pharmacy Practice. 2015;13(4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Advinha AM, de Oliveira-Martins S, Mateus V, Pajote SG, Lopes MJ. Medication regimen complexity in institutionalized elderly people in an aging society. International journal of clinical pharmacy. 2014;36(4):750–756. [DOI] [PubMed] [Google Scholar]
- 38.Mansur N, Weiss A, Beloosesky Y. Looking beyond polypharmacy: quantification of medication regimen complexity in the elderly. The American journal of geriatric pharmacotherapy. 2012;10(4):223–229. [DOI] [PubMed] [Google Scholar]
- 39.Libby AM, Fish DN, Hosokawa PW, et al. Patient-level medication regimen complexity across populations with chronic disease. Clinical therapeutics. 2013;35(4):385–398. e1. [DOI] [PubMed] [Google Scholar]
- 40.Patel CH, Zimmerman KM, Fonda JR, Linsky A. Medication Complexity, Medication Number, and Their Relationships to Medication Discrepancies. The Annals of pharmacotherapy. July2016;50(7):534–40. doi: 10.1177/1060028016647067 [DOI] [PubMed] [Google Scholar]
- 41.Linnebur SA, Vande Griend JP, Metz KR, Hosokawa PW, Hirsch JD, Libby AM. Patient-level medication regimen complexity in older adults with depression. Clin Ther. November12014;36(11):1538–1546 e1. doi: 10.1016/j.clinthera.2014.10.004 [DOI] [PubMed] [Google Scholar]
- 42.Yin HS, Parker RM, Sanders LM, et al. Pictograms, Units and Dosing Tools, and Parent Medication Errors: A Randomized Study. Pediatrics. July2017;140(1)doi: 10.1542/peds.2016-3237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Willson MN, Greer CL, Weeks DL. Medication regimen complexity and hospital readmission for an adverse drug event. Annals of Pharmacotherapy. 2014;48(1):26–32. [DOI] [PubMed] [Google Scholar]
- 44.Wimmer BC, Bell JS, Fastbom J, Wiese MD, Johnell K. Medication regimen complexity and polypharmacy as factors associated with all-cause mortality in older people: a population-based cohort study. Annals of pharmacotherapy. 2016;50(2):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alves-Conceicao V, Rocha KSS, Silva FVN, Silva ROS, Silva DTd, Lyra-Jr DPd. Medication regimen complexity measured by MRCI: a systematic review to identify health outcomes. Annals of Pharmacotherapy. 2018;52(11):1117–1134. [DOI] [PubMed] [Google Scholar]
- 46.Harris SC, Jean SJ. Characterization of the medication regimen complexity index in high-utilizer, adult psychiatric patients. Mental Health Clinician. 2020;10(4):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eiland LS, Benner K, Gumpper KF, et al. ASHP-PPAG Guidelines for Providing Pediatric Pharmacy Services in Hospitals and Health Systems. J Pediatr Pharmacol Ther. May-Jun 2018;23(3):177–191. doi: 10.5863/1551-6776-23.3.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lampkin SJ, Gildon B, Benavides S, Walls K, Briars L. Considerations for Providing Ambulatory Pharmacy Services for Pediatric Patients. J Pediatr Pharmacol Ther. Jan-Feb 2018;23(1):4–17. doi: 10.5863/1551-6776-23.1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bowers BL, Heffern C, Billings S. Implementation of a medication therapy management program in a primary care clinic. Journal of the American Pharmacists Association : JAPhA. May-Jun 2019;59(3):383–389. doi: 10.1016/j.japh.2019.02.009 [DOI] [PubMed] [Google Scholar]
- 50.Lenz M, Clark JA, Gates BJ. Medication Regimen Complexity in Patients Receiving Consultant Pharmacy Services in Home Health Care. Sr Care Pharm. February12020;35(2):81–84. doi: 10.4140/TCP.n.2020.81 [DOI] [PubMed] [Google Scholar]
- 51.Amazon.com. Pill Pack. Accessed1/28/2021, https://www.pillpack.com
- 52.Williams TA, Wolf MS, Parker RM, et al. Parent Dosing Tool Use, Beliefs, and Access: A Health Literacy Perspective. J Pediatr. December2019;215:244–251 e1. doi: 10.1016/j.jpeds.2019.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rinke ML, Bundy DG, Velasquez CA, et al. Interventions to reduce pediatric medication errors: a systematic review. Pediatrics. August2014;134(2):338–60. doi: 10.1542/peds.2013-3531 [DOI] [PubMed] [Google Scholar]
- 54.Organization WH. The use of the WHO-UMC system for standardised case causality assessment. Accessed4/13/2021, https://www.who.int/publications/m/item/WHO-causality-assessment
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental eTable 1. Medications used by MRCI tertile in children with severe neurological impairment.


