Abstract
Objectives
Estimate the use of preventive dental care services by the Medicare population and determine if dollars spent on preventive dental care save dollars spent on expensive non-preventive procedures?
Methods
The 2002 Medicare Beneficiary Survey is used to estimate a multinomial logistic model to analyze the influence of predisposing, enabling and need variables in identifying those using preventive dental care, only non-preventive dental care, or no dental care in a multiple variable context. Regression models with similar controls are used to estimate the influence of preventive care on the use and cost of non-preventive and total dental care.
Results
Our analyses show that beneficiaries using preventive dental care had more dental visits but fewer visits for expensive non-preventive procedures and lower dental expenses than beneficiaries only having oral problems treated at the dentist.
Conclusions
Adding dental coverage for preventive care to Medicare could pay off in terms of both improving the oral health of the elderly population and in limiting the costs of expensive non-preventive dental care for the dentate beneficiary population.
Keywords: Dental, Utilization, Preventive, Expense, Out of Pocket
INTRODUCTION
For many retirees, paying for dental care treatment can be difficult [1–3]. According to the 2006 Health and Retirement Study (HRS) out of pocket dental expenditures were $776 for those with coverage and $1,126 for those without coverage for persons 51 years and above with a dental visit over the previous two year period. [4] These amounts are not trivial especially among those who live on a fixed income. Seventy percent of persons aged 65 and older in 2004 were not covered by any dental insurance. [5] Without assistance some poorer older Americans may choose to delay or avoid seeking dental care. Postponing dental care may lead to expensive complications. [6,7] As recently reported in the New York Times, “Left unchecked, a small cavity that would cost about $100 to fill can easily turn into a $1,000 root canal. Skip those $80 cleanings each year, and you may be looking at $2,000 worth of gum disease.” [8]
Studies of the impact of preventive dental care visits have primarily focused on younger populations. [9–11] Insufficient attention has been paid to the impact of preventive dental care within an elderly population as a means of limiting expensive non-preventive dental care procedures. Previous research on preventive dental care has either not focused strictly on the elderly [12] or has not used nationally representative data [13] for their findings.
Our study first investigates the factors that distinguish community-dwelling Medicare beneficiaries using preventive dental care services from those using only non-preventive dental care and from those not using any dental care. Previous studies have found increasing patterns of use over time [14], as well as racial/ethnic, education, and income differences in the use of dental care among elderly populations [15, 16]. Data from the 1996 Medical Expenditure Panel Survey showed similar differences in the use of preventive services over the entire community-based population. [17] Characteristics of the Medicare beneficiary population examined in our study covered a broad range of socio-economic, demographic measures including general health care status and health limitations from secondary data provided by the Centers for Medicare and Medicaid Services (CMS) 2002 Medicare Current Beneficiary Survey (MCBS). [18] By identifying the characteristics of older adults using preventive dental care, we hope to gain insight into the potential barriers to access such care and to those factors that might foster such care. We then examine the dental care use and costs for beneficiaries with and without preventive care during the year to determine whether investing in preventive care can impact the use and costs of more expensive non-preventive procedures.
METHODS
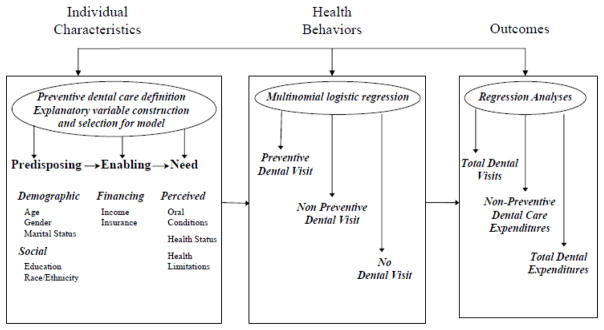
The Medicare Current Beneficiary Survey (MCBS) is a continuous, multipurpose survey of a nationally representative sample of aged, disabled, and institutionalized Medicare beneficiaries. [18] MCBS, which is sponsored by the Centers for Medicare & Medicaid Services (CMS), is the only comprehensive source of information on the health status, health care use, health insurance coverage, and socioeconomic and demographic characteristics of the entire spectrum of Medicare beneficiaries. [18] MCBS sampled persons are interviewed three times a year over 4 years to form a continuous profile of their health care experience. Interviews are conducted regardless of whether the sampled person resides at home or in a long-term care facility, using the version of the questionnaire appropriate to the setting. [18] Our study excludes beneficiaries in long-term care facilities during the entire survey year. We include beneficiaries who were in the community-dwelling population the entire survey year in addition to beneficiaries in the community population part of the year although we excluded data for them for the portion of the year they were in a long-term care facility. The model and analytic decision making process for the study is summarized in Figure 1.
Figure 1. Behavioral Model of Dental Services Use and Analytic Framework.
Boldface and italicized text represent primary characteristics, factors and analytical analyses used in this adaptation of the Andersen model. Source: Adapted from Andersen and Davidson, 1997
Preventive Dental Care Definition
The rationale for separating beneficiaries with dental use into those with and without preventive care is that preventive services are elective and are better-suited than non-elective services such as fillings, crowns and root canals as a proxy for individuals who place a high priority on having good oral health. Beneficiaries who do not obtain at least one cleaning during the year but appear in the dentist’s office for a diagnostic procedure (examination and/or x-ray) are most likely there because they need a non-elective procedure. Such dental users not only may differ from those seeking elective, preventive services, but also may differ from non-users due to having better access to dental care. [19]
We defined preventive dental care similar to Swank, Vernon, and Lairson [12] to be having at least one dental visit in 2002 involving a cleaning. We considered more restrictive definitions including exams and/or x-rays or at least two cleanings during the year, but the most restrictive of these reduced the sample of those with preventive dental care by nearly 60 percent and produced a nearly four-fold increase in the sample of those with dental care use but without any preventive care. Statistical comparisons using z tests across a wide range of beneficiary attributes discussed below found (1) that the characteristics of those using preventive dental care did not differ markedly across alternative definitions of preventive care and (2) that the beneficiary group with dental use but without any cleanings was distinctly different from those with at least one cleaning and from those without any dental care during the year. Data on the type of service received at a dental visit were collected in question DU7 in the 2002 MCBS dental utilization and event questionnaire. [20]
Explanatory Variable Construction
We began with a core group of beneficiary characteristics from the MCBS using Andersen’s conceptual framework.[6] These included self-reported data on predisposing factors for age, gender, race/ethnicity, education, marital status, household size, and community status (full-year, part-year); an enabling factor for income, and a need factor for health status. Additional need and predisposing factors were constructed for smoking behavior; self-reported difficulty eating solid food because of teeth problems; health conditions ever diagnosed by a physician; and limitations in specific activities of daily living (ADLs), instrumental ADLs, and physical functioning. An enabling variable was constructed to measure dental coverage but only for beneficiaries who saw a dentist during the year.
Model Testing
Preliminary model testing for the likelihood of using preventive dental care with the core set of explanatory variables described above confirmed the addition of variables for teeth problems eating solid food and smoking behavior to the core model. We did not include the dental coverage variable among the explanatory variables in the model because of its high correlation with dental care utilization. Correlation within and across the four sets of general health care status categories for difficulties with ADLs, IADLs, physical limitations, and medical conditions necessitated additional model testing to determine which among the four measures provided the largest contribution to the model’s explanatory power. To reduce the correlation within each group of health limitation variables, we constructed dummy variables for the number of conditions or limitations within each group. Based on our preliminary testing we selected the number of physical function limitations for the multinomial logistic model.
Model Estimation
We then estimated a multinomial logistic model to analyze the influence of predisposing, enabling and need variables in identifying those using preventive dental care, only non-preventive dental care, or no dental care. A Wald test for combining alternatives in Stata [21] confirmed the split of the sample into 3,288 beneficiaries with preventive care, 1,265 with non-preventive care and 6,029 nonusers of dental services for the study. Finally, we estimated the impact of preventive dental care in regression models of total and non-preventive dental care use and expenditure. All estimates and statistics reported were computed by taking into account the complex sampling design of MCBS with the use of the software packages STATA and SUDAAN. [21,22]
RESULTS
Descriptive Analysis
There were 10,582 total participants in the 2002 MCBS representing 33,725,756 Medicare beneficiaries in the community-based population. Of these, more than half of the un-weighted participants were female (55%, N=5,847). Ten percent (N=1,080) of the participants were non-Hispanic black and 7 percent (N=792) were Hispanic. About half (N=5,275) of the participants were age 75 or more, 15 percent (N=1,621) were less than 65 and 35 percent (N=3,686) were between the ages of 65 and 74. Seven percent (N=755) were part-year community-based participants.
Preventive Dental Care Users
Table 1 shows the sample means of selected variables by type of dental care use. Users of preventive dental care compared to the other two beneficiary groups are generally more likely to be in the 65 to 79 age groups and less likely to be under 65 years of age or 80 years and older. They are better educated with higher incomes and are more likely to be non-smoking, white, non-Hispanic, married beneficiaries in very good or excellent health status, without teeth problems and with fewer health conditions and limitations than beneficiaries in the other two groups. Compared to beneficiaries who used only non-preventive dental care, they are more likely to have dental insurance coverage and they visit the dentist more often during the year (2.83 vs. 2.49 visits) but less often for more expensive non-preventive procedures (0.83 vs. 1.58 visits). As a result, they pay less in total ($560 vs. $822) and out of pocket ($408 vs. $623) for their total dental care and less in total ($263 vs. $581) and out of pocket ($189 vs. $433) for their non-preventive dental care.
Table 1.
Sample means for community-dwelling Medicare beneficiaries by use of dental care, 2002.
| Variable Description | All Beneficiaries | Population With Preventive Dental Visit | Population With Only Non Preventive Dental Visit | Population With No Dental Visit |
|---|---|---|---|---|
| Number of Beneficiariesa | 33,725,756 | 10,948,187 | 4,053,975 | 18,723,595 |
| Age less than 65 (percentage) | 12.48 | 8.15** | 15.96 | 14.25 |
| 65 to 69 | 16.68 | 18.50* | 15.97 | 15.77 |
| 70 to 74 | 24.29 | 27.35** | 24.26 | 22.51 |
| 75 to 79 | 20.89 | 23.67** | 19.30 | 19.61 |
| 80 and above | 25.66 | 22.34* | 24.50* | 27.86 |
| Female (percentage) | 55.71 | 57.10** | 52.61 | 55.57 |
| Black non-Hispanic (percentage) | 9.34 | 2.76** | 8.92* | 13.28 |
| Hispanic | 7.49 | 4.27** | 9.72 | 8.90 |
| White non-Hispanic | 78.96 | 90.03** | 76.19 | 73.09 |
| Other non-Hispanic | 3.99 | 2.72** | 4.94 | 4.53 |
| Person income < $10,000 (percentage) | 20.16 | 8.36** | 18.85* | 27.35 |
| $10,000–20,000 | 29.92 | 20.68** | 29.96* | 35.31 |
| $20,000–35,000 | 32.21 | 38.67** | 33.05* | 28.26 |
| Over $35,000 | 17.70 | 32.29** | 18.14* | 9.08 |
| Some or no high school (percentage) | 32.08 | 13.61** | 28.35* | 43.68 |
| High school graduate | 50.09 | 54.65* | 52.86* | 46.51 |
| College graduate | 17.64 | 31.60** | 18.54* | 9.28 |
| Married (percentage) | 52.03 | 61.07** | 54.96* | 46.10 |
| Widowed, divorced | 42.06 | 33.76** | 39.63* | 47.44 |
| Never married | 5.87 | 5.13* | 5.35 | 6.41 |
| Household Size One (percentage) | 34.89 | 31.65* | 33.01 | 37.20 |
| Size two | 49.90 | 58.37** | 50.56* | 44.81 |
| Size three or more | 15.18 | 9.98* | 16.43 | 17.96 |
| Health status fair/poor (percentage) | 27.14 | 17.02** | 28.08* | 32.86 |
| Good | 31.35 | 31.00 | 33.91 | 31.01 |
| Excellent/very good | 40.04 | 51.27** | 37.02 | 34.13 |
| Part year community resident (percentage) | 5.45 | 2.50* | 3.27* | 7.73 |
| Difficulty eating solid foods because of teeth (percentage) | 12.19 | 6.15** | 20.10* | 14.01 |
| Former smoker (percentage) | 47.51 | 49.96* | 48.43 | 45.82 |
| Current smoker | 13.73 | 7.76** | 13.82* | 17.20 |
| Never smoked | 38.76 | 42.46** | 37.65 | 36.75 |
| Dental coverage (percentage)b | 20.63 | 46.14** | 40.07* | 1.50 |
| Number of difficulties with activities of daily living (ADLs)c | 0.70 | 0.45** | 0.74 | 0.84 |
| Number of difficulties with instrumental ADLsd | 1.14 | 0.75** | 1.13* | 1.37 |
| Number of conditions ever diagnosed by physiciane | 2.84 | 2.58** | 3.02 | 2.95 |
| Number of physical limitationsf | 2.18 | 1.75** | 2.25* | 2.43 |
| Number of dental events | 1.28 | 2.83*** | 2.49 | 0 |
| Number of dental cleaning events | 0.53 | 1.63 | 0 | 0 |
| Number of dental events not cleaning, exam, or x-rays | 0.46 | 0.83*** | 1.58 | 0 |
| All dental events ($ payments) | 1.22 | 560.22*** | 821.60 | 0 |
| Dental cleaning events ($ payments) | 0.53 | 204.18 | 0 | 0 |
| Dental events not cleaning, exam, or x-rays ($ payments) | 0.46 | 262.61*** | 581.25 | 0 |
| All dental events (out of pocket (OOP) $ payments) | 207.22 | 407.57*** | 623.19 | 0 |
| Dental cleaning events (OOP $ payments) | 47.60 | 146.62 | 0 | 0 |
| Dental events not cleaning, exam, or x-rays (OOP $ payments) | 113.48 | 189.32*** | 432.77 | 0 |
Source: 2002 Medicare Current Beneficiary Survey community-based beneficiaries.
Indicates that the mean in the column is significantly different than the mean for the population with no dental use at 5%.
Indicates that the mean in the column is significantly different than the mean for the population with only non-preventive dental visits and the mean for the population with no dental use at 5%.
Indicates that the mean in the column is significantly different than the mean for the population with only non-preventive dental visits.
Includes Medicare beneficiaries with missing values of race/ethnicity, education, marital status, household size, and health status.
Survey data limitations, as discussed in the methods section above, limit the ability of the MCBS to estimate dental insurance coverage reliably for the Medicare beneficiaries who did not see a dentist during the year.
Activities of daily living include bathing/showering, dressing, eating, getting in/out of bed/chair, walking, and using the toilet.
Instrumental activities of daily living include using the telephone, doing light housework, doing heavy housework, preparing meals, shopping for personal items, and managing money.
The list of conditions includes hardening of the arteries, hypertension/high blood pressure, myocardial infarction/heart attack, angina pectoris/coronary heart disease, other heart conditions, stroke/brain hemorrhage, skin cancer, other (non-skin) cancer, diabetes/high blood sugar, rheumatoid arthritis, mental retardation, osteoporosis/soft bones, broken hip, Parkinson’s disease, emphysema/asthma/cardiopulmonary disease, complete/partial paralysis, and lost arm or leg.
Physical limitations include any difficulty stooping/crouching, kneeling, lifting/carrying 10 pounds, extending arms above shoulders, writing/handling object, and walking ¼ mile or 2–3 blocks.
Non-Preventive Dental Care Users
Beneficiaries using only non-preventive dental care differ from those with no dental care by many of the characteristics that distinguish them from beneficiaries using preventive dental care. Compared to non-users, they are less likely to have physical limitations and are less likely to be 80 or older; a part-year community-dwelling resident; black, non-Hispanic; a current smoker; and to be in fair or poor health. They are more likely to have problems eating because of teeth problems, be married, and have a high school or college education and a higher income.
Regression Analysis
The multinomial logistic regression results in Table 2 provide the estimated odds of community-dwelling beneficiaries being in the preventive dental group (column 2), or being in the only non-preventive dental group (column 4), relative to being in the non-user group after controlling for characteristics distinguishing the three groups of beneficiaries. A second multinomial logistic regression has the same explanatory variables as the first only specifies beneficiaries only using non-preventive dental care as the base case. This equation provides the estimated odds of being in the preventive dental care group relative to being in the “only non-preventive” beneficiary group (column 3). As discussed above, these regressions also provided a test for the separation of the sample into three groups based on beneficiary characteristics examined in our study.
Table 2.
Multinomial logistic estimates
| Odds Ratio Point Estimates b | |||
|---|---|---|---|
| Population Characteristic | Preventive Dental Care vs. No Dental Care | Preventive Dental Care vs. Only Non-Preventive Care | Only Non-Preventive Dental Care vs. No Dental Care |
| Intercept | 5.46** | 8.65** | 0.63** |
| Age less than 65 | 1.14 | 0.84 | 1.35* |
| 65 to 69 | 0.98 | 1.08 | 0.90 |
| 70 to 74 | 0.94 | 1.01 | 0.93 |
| 75 to 79 | 1.18* | 1.20 | 0.98 |
| 80 and older | (1.00) | (1.00) | (1.00) |
| Male | 0.72** | 0.72** | 1.00 |
| Female | (1.00) | (1.00) | (1.00) |
| Black non-Hispanic | 0.32** | 0.38** | 0.84 |
| Hispanic | 0.74* | 0.55** | 1.35* |
| Other non-Hispanic | 0.62** | 0.63* | 1.00 |
| White non-Hispanic | (1.00) | (1.00) | (1.00) |
| Person income < $10,000 | 0.19** | 0.40** | 0.46** |
| $10,000–20,000 | 0.27** | 0.50** | 0.55** |
| $20,000–35,000 | 0.49** | 0.71** | 0.69** |
| Over $35,000 | (1.00) | (1.00) | (1.00) |
| Some or no high school | 0.21** | 0.50** | 0.42** |
| High school graduate | 0.49** | 0.74** | 0.66** |
| College graduate | (1.00) | (1.00) | (1.00) |
| Widowed, divorced | 0.85 | 1.01 | 0.85 |
| Never married | 1.32* | 1.63* | 0.81 |
| Married | (1.00) | (1.00) | (1.00) |
| Household size one | 1.46** | 1.29 | 1.13 |
| Size two | 1.31** | 1.27 | 1.03 |
| Size three or more | (1.00) | (1.00) | (1.00) |
| Has teeth problems eating solid food | 0.69** | 0.35** | 1.93** |
| Does not have problems | (1.00) | (1.00) | (1.00) |
| Health status fair/poor | 0.74** | 0.80 | 0.92 |
| Good | 0.95 | 0.84 | 0.94 |
| Excellent/very good | (1.00) | (1.00) | (1.00) |
| Three or more physical limitations a | 0.71** | 0.78 | 0.91 |
| Two | 0.90 | 0.83 | 1.09 |
| One | 1.03 | 0.99 | 1.05 |
| None | (1.00) | (1.00) | (1.00) |
| Current smoker | 0.44** | 0.61** | 0.71* |
| Former smoker | 0.86* | 0.91 | 0.94 |
| Never smoker | (1.00) | (1.00) | (1.00) |
| Part year community resident | 0.34** | 0.83 | 0.41** |
| Full year | (1.00) | (1.00) | (1.00) |
Source: 2002 Medicare Current Beneficiary Survey, community-based beneficiaries.
Note: The base case for the equation in the second and fourth columns is beneficiaries who did not visit the dentist during the year. The base case for the equation in the third column is beneficiaries who had only non-preventive dental care. The sample consists of 9,760 observations and excludes 822 persons with missing values of any independent variable from the initial analytic sample.
Indicates significant at the .05 level.
Indicates significant at the .01 level.
Psuedo-R2 = 0.13.
Includes some or a lot of difficulty stooping/crouching/kneeling, lifting/carrying 10 pounds, extending arms above shoulders, writing/handling object, and walking one quarter mile or two to three blocks.
Odds Ratio Point Estimate in second and fourth columns = estimate of [Probability of preventive dental visit (or only non-preventive dental care)/Probability of no dental care] for persons with row characteristic divided by [Probability of preventive dental visit (or only non-preventive care)/Probability of no dental care] for omitted characteristic from a multinomial logistic equation with beneficiaries without dental care as the reference group. Estimate in third column = estimate of [Probability of preventive dental visit/Probability of only non-preventive dental care] for persons with row characteristic divided by [Probability of preventive dental visit/Probability of only non-preventive dental care] for omitted characteristic from a similar multinomial logistic equation except with beneficiaries with only non-preventive dental care as the reference group.
To help interpret the estimated odds ratios in Table 2, the estimate for males (0.72) in column 2 indicates that the odds of a male beneficiary having a preventive dental visit are 72 percent of the odds of a female beneficiary after adjusting for other covariates, where the odds are defined as the probability of a preventive dental visit divided by the probability of not having any dental visit during the year. This means that, holding other attributes constant, male beneficiaries are about 70 percent as likely as female beneficiaries to have their teeth cleaned in the dentist’s office rather than to go without seeing a dentist during the year.
Preventive Dental Care vs. No Dental Care
Apart from the gender effect, column 2 of Table 1 shows that the odds of using preventive dental care relative to no dental care are lower for minority racial/ethnic groups compared to white non-Hispanics and for lower income and education groups compared to higher ones. A lower likelihood of using preventive dental care is also found for beneficiaries with teeth problems eating solid food relative to those with no such problems. This suggests that improved oral hygiene, including annual cleanings at a dentist’s office, offers protection against oral health problems. Beneficiaries with three or more physical limitations compared to those with none, in fair or poor health status compared to those in excellent or very good health status, and who are current or former smokers rather than never smoked, or part year rather than full year community-dwelling residents, are also less likely to use preventive dental care and are more likely to not visit the dentist during the year for any reason.
Curiously, the odds of never married beneficiaries using preventive dental care are half again larger than those of married beneficiaries. The relatively strong, positive effects of household sizes one and two compared to sizes three and larger might be masking marital status effects because of correlation between these variables.
Preventive Dental Care vs. Only Non-Preventive Care
In general, column 3 of Table 2 shows that the characteristics that distinguish preventive dental care users from non-users of dental care also distinguish them from beneficiaries who only go to the dentist for non-preventive procedures such as crowns, fillings, and root canals. This holds true across race/ethnicity, income, education, gender, marital status, teeth problem and smoking status categories. There were no differences between the two groups on the basis of age, household size, physical limitations, health status, and part year community status.
Only Non-Preventive Dental Care vs. No Dental Care
The last column of Table 2 identifies characteristics that differentiate beneficiaries going to the dentist for oral problems, but not for cleanings, from those who did not venture into a dentist’s office during the year. As one might expect, the odds are nearly twice as high of having an oral problem treated compared to not going if the person reported a problem eating because of their teeth. Interestingly the odds are also higher for beneficiaries under age 65 compared to elderly beneficiaries and for Hispanics compared to white, non-Hispanic beneficiaries. The odds are lower for lower income and education groups compared to higher ones, as well as for current smokers compared to those who never smoked and for part year rather than full year community residents.
Dental Use and Expense
To be a good investment, preventive dental care should help beneficiaries avoid or at least minimize costly non-preventive dental procedures such as inlays, crowns, bridges, extractions, and root canals. The descriptive results above in Table 1 show that beneficiaries using preventive dental care had more dental visits but fewer visits for expensive non-preventive procedures and lower dental expenses than beneficiaries only having oral problems treated at the dentist. The findings in Table 3 confirm these results after controlling for other influences on dental use and expense by Medicare beneficiaries. Six regression equations were restricted to a sample of beneficiaries using dental care and were estimated in natural logarithm form for the number of events and for total and out of pocket expense for both total and non-preventive dental events. The key explanatory variable in the equations was a binary variable indicating that the beneficiary had at least one dental visit with a cleaning during the year. Other covariates in the model were the same as in the multinomial logistic models in Table 2 with the exception of an additional variable indicating dental insurance coverage. Table 3 displays only the coefficient estimates for the preventive dental care variable. In all cases the estimates are statistically significant and in the direction that is consistent with the descriptive findings. These results suggest that Medicare beneficiaries who use preventive dental care have more dental visits but pay less out of pocket and in total for dental care both overall and for expensive non-preventive procedures.
Table 3.
Estimates of the effect of preventive dental care on dental care use, dental expense, and out of pocket payments for community-dwelling Medicare beneficiaries with dental care use, 2002.
| Dental Care Use or Payments | Coefficient for Preventive Dental Care | Sample Size | R2 |
|---|---|---|---|
| Total dental events | |||
| Log of number of events | .176** (.026) | 4284 | .118 |
| Log of expense | −.328** (.052) | 4228 | .095 |
| Log of out of pocket payments | −.416** (.063) | 3906 | .051 |
| Non-preventive dental events | |||
| Log of number of events | −.060* (.030) | 2094 | .085 |
| Log of expense | −.250** (.065) | 2064 | .071 |
| Log of out of pocket payments | −.279** (.083) | 1893 | .050 |
Source: 2002 Medicare Current Beneficiary Survey community-based beneficiaries.
Note: The reference group for preventive dental care is beneficiaries with only non-preventive dental care. Other covariates in the equations include: age dummies, male, race/ethnicity categories, income categories, education categories, marital status, household size, teeth problems, health status, physical limitation categories, smoking status, dental coverage, and part year community resident. Estimated standard errors of the regression coefficient are in parentheses.
Indicates significant at the .05 level.
Indicates significant at the .01 level.
DISCUSSION
Our analysis characterized beneficiaries with and without preventive dental care and further identified the characteristics that distinguished the second group between those without any dental care and those only seeing a dentist to treat oral problems. We explored whether diagnostic care should be packaged with preventive care on the grounds that examinations and/or x-rays could detect oral disease. We found that among the 1,265 beneficiaries in the group classified as non-preventive dental users were 733 beneficiaries with at least one dental visit during the year with an examination and/or an x-ray. We relied on the Wald test for comparing alternatives to determine that these 733 beneficiaries should not be grouped with the 3,288 beneficiaries in the preventive group nor left as a separate group, but instead be merged with the other 532 beneficiaries in the non-preventive dental use group.
Our results are consistent with previous results confirming dental access problems for minority race/ethnicity groups and for persons with lower income and educational levels. [15,16] We also found that beneficiaries in worse overall health status with more physical and health limitations and difficulties with daily activities are concentrated in the group not visiting the dentist for any reason. Compounding these access problems is the limited supply of dentists and public financing for underserved populations. [23] Community outreach through the provision of transportation services, clinics, and provider networks targeted on the elderly may be required to bring missing dental services to these individuals much like similar programs targeted on rural communities [24]. Notably the beneficiaries who develop oral problems and who only visit the dentist for treating them display fewer of the attributes indicating access problems that are typical of the group of non-user beneficiaries.
For those beneficiaries who used dental care during the year, our results suggest that preventive dental care reduces dental bills and out of pocket payments primarily because it is associated with fewer expensive non-preventive dental procedures. Our descriptive analysis shows that if the beneficiary group receiving preventive dental care required the same non-preventive dental care as the “only non-preventive” group, they would have paid $216 more per capita or $2.4 billion more in total in 2002 out of their own pockets for their dental bills. This analysis does not account for the majority of community dwelling beneficiaries who did not see a dentist during the year.
Data were not available from the MCBS to identify the general oral health status of the non-user group or the percentage of them who were missing their teeth (edentulous). Demographic and socio-economic characteristics of the non-user group suggest that the prevalence of edentulous beneficiaries in this group is higher than a national average of about one-third of non-institutionalized adults 65 years of age and older. [16, 25] Our limited use-driven measure of dental coverage also did not provide a clear indication of how many of the non-users lacked insurance coverage, a strong correlate with dental use [5, 26]. We were only able to identify dental coverage if either (1) the beneficiary received third party payments for dental expenses or (2) reported having a “dental only” private or public insurance plan. Beneficiaries were not asked directly in the MCBS whether or not they had dental insurance coverage, so the MCBS was unable to measure dental coverage accurately for persons who did not see a dentist during the survey year. Only six percent of those with dental coverage were identified by having a “dental only” plan, and slightly more than one percent (1.3) of non-users were identified as covered by having such a plan.
Model limitations include potential omission of relevant variables such as oral health status, dentate status, and provider supply that could bias model coefficients. The potential for selection bias exists in the dental use and expenditure models from the limited dental coverage variable. Future plans to use MCBS longitudinal data to model the effect of preventive dental care should offer more insight into this study’s findings.
Clearly the dentate portion of the non-user group would consider their lack of preventive dental care a good investment because they have no dental expenses. What is unclear is how many of them either currently have untreated oral diseases or conditions or will ultimately develop oral problems in the future that either diminish their quality of life or will eventually require expensive treatments. The Douglas, et al study found relatively high percentages of untreated coronal decay, root caries, and severe periodontal pocketing among a representative sample of community-dwelling elders age 70 and older living in six New England states [27]. A more definitive answer to the question posed by our study needs to be addressed with longitudinal data to determine whether periodic preventive dental care in the dentist’s office pays off in terms of fewer expensive problems and procedures over time. In the meantime, our limited short-term duration study suggests that it does. The policy implication of our study is that at a minimum adding dental coverage of preventive care to Medicare could pay off in terms of both improving the oral health of the elderly population and in limiting the costs of expensive non-preventive dental care for the dentate beneficiary population.
Acknowledgments
This investigation was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health. (1R03DE016850-01A2, Preventive Dental Care Services and General Health Care)
The authors wish to thank Pat Stewart and Diane McNally of the University of Maryland School of Pharmacy Pharmaceutical Research Computing (PRC) for their analytical and programming support.
References
- 1.Marcus M, Schoen MH, May S. An Alternative Method for Financing Care for the Non-Institutionalized Geriatric Patient. Geriodontology. 1984 May;3(4):31–33. doi: 10.1111/j.1741-2358.1984.tb00045.x. [DOI] [PubMed] [Google Scholar]
- 2.Bomberg TJ, Ernst NS. Improving Utilization of Dental Care Services by the Elderly. Geriodontics. 1986 April;2(2):57–60. [PubMed] [Google Scholar]
- 3.Manski RJ, Goodman HS, Reid BC, Macek MD. Dental Insurance Visits and Expenditures Among Older Adults. American Journal of Public Health. 2004 May;94(5):759–764. doi: 10.2105/ajph.94.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manski RJ, Moeller JR, Chen H, StClair PA, Schimmel J, Magder L, Pepper JV. Dental Care Expenditures and Retirement. Journal of Public Health Dentistry. doi: 10.1111/j.1752-7325.2009.00156.x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manski RJ, Brown E. Dental Use, Expenses, Private Dental Coverage, and Changes, 1996 and 2004. Rockville (MD): Agency for Healthcare Research and Quality; 2007. MEPS Chartbook No. 17. http://www.meps.ahrq.gov/mepsweb/data_files/publications/cb17/cb17.pdf. [Google Scholar]
- 6.Shay K. Infectious Complications of Dental and Periodontal Diseases in the Elderly Population. Clinical Infectious Diseases. 2002 May;34:1215–1223. doi: 10.1086/339865. [DOI] [PubMed] [Google Scholar]
- 7.Andersen RM, Davidson PL. Ethnicity, Aging, and Oral Health Outcomes: A Conceptual Framework. Advances in Dental Research. 1997 May;11(2):203–209. doi: 10.1177/08959374970110020201. [DOI] [PubMed] [Google Scholar]
- 8.Konrad W. How to Manage Dental Costs, With or Without Insurance. New York Times. 2009 September 5;B6 [Google Scholar]
- 9.Lewis C, Teeple E, Robertson A, Williams A. Preventive Dental Care for Young, Medicaid-Insured Children in Washington State. Pediatrics. 2009 July;124(1):e120–e127. doi: 10.1542/peds.2008-3089. [DOI] [PubMed] [Google Scholar]
- 10.Lewis C, Mouradian W, Slayton R. Dental Insurance and Its Impact on Preventive Dental Care Visits for U.S. Children. Journal of the American Dental Association. 2007;138(3):369–380. doi: 10.14219/jada.archive.2007.0170. [DOI] [PubMed] [Google Scholar]
- 11.Kenney GM, McFeeters JR, Yee JY. Preventive Dental Care and Unmet Dental Needs Among Low-Income Children. American Journal of Public Health. 2005 August;95(8):1360–1366. doi: 10.2105/AJPH.2004.056523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swank ME, Vernon SW, Lairson DR. Patterns of Preventive Dental Behavior. Public Health Reports. 1986;101(2):175–184. [PMC free article] [PubMed] [Google Scholar]
- 13.Branch LG, Antczak AA, Stason WB. Toward Understanding the Use of Dental Services by the Elderly. Special Care in Dentistry. 1986;6(1):38–41. doi: 10.1111/j.1754-4505.1986.tb00949.x. [DOI] [PubMed] [Google Scholar]
- 14.Manski RJ, Moeller JF, Maas WR. Dental Services: An Analysis of Utilization over 20 Years. Journal of the American Dental Association. 2001 May;132:655–664. doi: 10.14219/jada.archive.2001.0243. [DOI] [PubMed] [Google Scholar]
- 15.Davidson PL, Andersen RM. Determinants of Dental Care Utilization for Diverse Ethnic and Age Groups. Advances in Dental Research. 1997 May;11(2):254–262. doi: 10.1177/08959374970110020801. [DOI] [PubMed] [Google Scholar]
- 16.Vargas CM, Kramarow EA, Yellowitz JA. Aging Trends No. 3. Hyattsville, MD: National Center for Health Statistics; 2001. The Oral Health of Older Americans. [PubMed] [Google Scholar]
- 17.Manski RJ, Moeller JF. Use of Dental Services. An Analysis of Visits, Procedures, and Providers, 1996. Journal of the American Dental Association. 2002 February;133:167–175. doi: 10.14219/jada.archive.2002.0140. [DOI] [PubMed] [Google Scholar]
- 18.http://www.cms.hhs.gov/MCBS/
- 19.Dolan TA, Atchison K, Huynh TN. Access to Dental Care Among Older Adults in the United States. Journal of Dental Education. 2005 September;69(9):961–974. [PubMed] [Google Scholar]
- 20.http://www.cms.hhs.gov/MCBS/Downloads/2002_CCQ_du.pdf
- 21.Statacorp. Stata Statistical Software: Release 7.0. College Station, TX: Stata Corporation; [Google Scholar]
- 22.Research Triangle Institute. SUDAAN Software for analysis of correlated data. Release 6.40. Research Triangle Park, NC: Research Triangle Institute; 1995. [Google Scholar]
- 23.Mertz E, O’Neil E. The Growing Challenge of Providing Oral Health Care Services to All Americans. Health Affairs. 2002 September/October;21(5):65–77. doi: 10.1377/hlthaff.21.5.65. [DOI] [PubMed] [Google Scholar]
- 24.Department of Health and Human Services. The Outreach Sourcebook, Volume 9, Rural Health Demonstration Projects (Health Resources and Services Administration, Office of Rural Health Policy) Rockville, MD: 2003. Project 16—Something to Smile About: Preventive Dental Care Project for Garrett County Maryland; pp. 57–59. [Google Scholar]
- 25.Marcus SE, Kaste LM, Brown LJ. Prevalence and Demographic Correlates of Tooth Loss Among the Elderly in the United States. Special Care in Dentistry. 1994 May;14(3):123–127. doi: 10.1111/j.1754-4505.1994.tb01117.x. [DOI] [PubMed] [Google Scholar]
- 26.Manski RF, Macek MD, Moeller JF. Private Dental Coverage: Who Has It and How Does It Influence Dental Visits and Expenditures? Journal of the American Dental Association. 2002 November;133(11):1551–1559. doi: 10.14219/jada.archive.2002.0087. [DOI] [PubMed] [Google Scholar]
- 27.Douglass CW, et al. Oral Health Status of the Elderly in New England. Journal of Gerontology. 1993 March;48(2):M39–M46. doi: 10.1093/geronj/48.2.m39. [DOI] [PubMed] [Google Scholar]