Abstract
Aims:
To explore factors associated with nurses' moral distress during the first COVID-19 surge and their longer-term mental health.
Design:
Cross-sectional, correlational survey study.
Methods:
Registered nurses were surveyed in September 2020 about their experiences during the first peak month of COVID-19 using the new, validated, COVID-19 Moral Distress Scale for Nurses. Nurses' mental health was measured by recently experienced symptoms. Analyses included descriptive statistics and regression analysis. Outcome variables were moral distress and mental health. Explanatory variables were frequency of COVID-19 patients, leadership communication and personal protective equipment/cleaning supplies access. The sample comprised 307 nurses (43% response rate) from two academic medical centres.
Results:
Many respondents had difficulty accessing personal protective equipment. Most nurses reported that hospital leadership communication was transparent, effective and timely. The most distressing situations were the transmission risk to nurses' family members, caring for patients without family members present, and caring for patients dying without family or clergy present. These occurred occasionally with moderate distress. Nurses reported 2.5 days each in the past week of feeling anxiety, withdrawn and having difficulty sleeping. Moral distress decreased with effective communication and access to personal protective equipment. Moral distress was associated with longer-term mental health.
Conclusion:
Pandemic patient care situations are the greatest sources of nurses' moral distress. Effective leadership communication, fewer COVID-19 patients, and access to protective equipment decrease moral distress, which influences longer-term mental health.
Impact:
Little was known about the impact of COVID-19 on nurses' moral distress. We found that nurses' moral distress was associated with the volume of care for infected patients, access to personal protective equipment, and communication from leaders. We found that moral distress was associated with longer-term mental health. Leaders should communicate transparently to decrease nurses' moral distress and the negative effects of global crises on nurses' longer-term mental health.
Keywords: communication, COVID-19, leadership, management, mental health, moral distress, nurses, pandemics, personal protective equipment, surveys
1 ∣. INTRODUCTION
Hospital nurses, as the frontline providers during the COVID-19 pandemic, faced unprecedented risk and challenges. Nurses lacked personal protective equipment (PPE) (American Nurses Association [ANA], 2020c) and experienced a lack of practice guidelines (Rosa et al., 2020). Nurses were delivering a crisis standard of care, balancing their duty to care for patients and their obligation to protect themselves and their families. Nurses' moral distress during the pandemic, and its relation to caring for patients with COVID-19 and a lack of PPE, has not been studied. In addition, the influence of leadership communication in mitigating nurse moral distress and the long-term effects of moral distress on nurses' mental health are not known. This paper addresses these knowledge gaps and advances theoretical understanding of the causes and consequences of nurse moral distress related to the COVID-19 pandemic.
2 ∣. BACKGROUND
2 1 ∣. Crisis standards of care and nurses' moral distress
Although recent epidemics such as SARS and Ebola presented ethical challenges to nursing care in other parts of the world (World Health Organization [WHO], 2015), COVID-19 is the first recent pandemic to appear in U.S. hospitals. Accordingly, U.S. hospitals were unprepared to initiate crisis standards of care necessary during a pandemic to guide healthcare providers during the process of allocating and using scarce medical resources (ANA, 2020a).
Crisis care standards entail a utilitarian ethical framework, which conflicts with the virtue-based ethical framework that typically drives the nursing care standard (Webster & Wocial, 2020). These conflicting frameworks lead to moral distress as nurses attempt to balance their desire to give the best care to individual patients with the need to provide the greatest good for the greatest number given limited resources.
The pandemic compounded moral distress that nurses routinely encounter in practice. Moral distress has been defined by multiple ethicists, often derived from Jameton (1984). The central concept is knowing the right thing to do but being constrained and unable to act, which threatens moral integrity. Moral distress is characterized by feeling powerless and unable to speak up or to be heard (Hamric, 2014). It is associated with the individual's duty to uphold professional ethical standards and responsibilities. We defined moral distress as occurring when an individual is unable to take what they believe to be a morally justifiable action, or unable to achieve an ethical outcome, resulting in compromised moral integrity and emotional distress (Hamric, 2014).
We utilize a framework presented by Epstein et al. (2019) in which sources of moral distress are conceptualized at three levels: patient, unit/team and hospital/system. An example of a patient source of distress is providing futile treatments. An example of a unit/team source is a lack of interdisciplinary collaboration. An example of a hospital/system source is inadequate staffing or supplies. This framework presents opportunities for managers to mitigate nurses' moral distress at the two upper levels (i.e. unit/team and hospital/system).
Changes in clinical practice due to COVID-19 presented new ethical challenges, heightening the potential for moral distress. Prominent changes included visitation restrictions, risk to personal and loved ones' safety, and reduced health care services (Morley et al., 2020). Now, we describe how these changes prompted moral distress at the three levels, per Epstein et al.'s (2019) framework. Patient sources of moral distress included transmission risk and the effect of PPE shortages. Lacking proper PPE, nurses faced the risk of contracting the virus. When professional obligation conflicted with their personal obligation to protect themselves and their families, feelings of powerlessness and moral distress may have resulted (Zuzelo, 2020). Moreover, providing care while wearing burdensome PPE changed care delivery, diminishing interactions with patients and compromising communication due to masks and shields (Wolf et al., 2016). Moral distress emerges when patient care is compromised due to PPE requirements.
Increased workloads lead to understaffing. When nurses are prevented from spending adequate time with patients, they are unable to meet the duty to care. Per Epstein et al. (2019), understaffing is a hospital/system source of moral distress. When patients died without family members or clergy in attendance, spiritual end-of-life needs could not be honoured in the usual way (Webster & Wocial, 2020). Not attending to patients' spiritual needs originates in hospital-level policy but is experienced as patient-level moral distress.
2.2 ∣. The shortage of PPE contributed to nurses' moral distress
The widespread PPE shortage during the pandemic resulted in the unprecedented use and reuse of PPE (Webster & Wocial, 2020). Over half of 32,000 nurses surveyed in March-April 2020 reported a PPE shortage (ANA, 2020c). The Centers for Disease Control and Prevention provided guidelines on PPE reuse and the use of bandanas or scarves, presenting more risk than traditional guidelines (CDC, 2020). The realities of PPE shortages, of reusing PPE or using bandanas or scarves, were extraordinary in the U.S. The PPE shortage yielded unprecedented psychological burdens, including stress and anxiety, on healthcare providers (Arnetz et al., 2020; Young et al., 2020).
2.3 ∣. Leadership communication may reduce moral distress
While moral distress during pandemic nursing care is inevitable, effective manager communication with staff during a crisis may mitigate moral distress. We define communication, which is a core responsibility of the nurse manager, as providing staff with information about policies, procedures and expectations. As ‘communication is the nurse manager's most vital tool,’ optimal communication would include ‘openness, accuracy, timeliness, understanding, and satisfaction’ (Scott-Cawiezell et al., 2004, p. 243). The 2002–2004 SARS outbreak revealed that transparency and trust were ‘key elements in managing fear and uncertainty’ among healthcare workers (HCWs) amid constant new information and policy changes (Spalluto et al., 2020). Notably, just 44% of nurses reported in a March 2020 survey with 6500 respondents that their employer provided them with necessary information about COVID-19 (National Nurses United, 2020).
2.4 ∣. Nurses' mental health related to pandemic nursing care
Evidence to date from the COVID-19 pandemic reveals the negative psychological impacts of crisis care on nurses. A nationwide survey in April 2020 revealed that nearly half of HCWs reported anxiety, depression and PTSD (Young et al., 2020). A May-June 2020 survey found subthreshold insomnia, moderate-to-high chronic fatigue, high acute fatigue, and low-to-moderate intershift recovery, increased emotional exhaustion and depersonalization, moderate psychological distress and high post-traumatic stress among 400 nurses (Sagherian et al., 2020). These findings were worse among nurses who cared for COVID-19 patients (Sagherian et al., 2020).
Notably, to our knowledge, the literature on the mental health of HCWs generally, and nurses specifically, has not addressed nurses' moral distress, despite the unique circumstances that were expected to exacerbate it. Not only is moral distress, in real time, distressing to experience, but also it has many negative consequences, including anger, frustration, depression, helplessness, sadness, anxiety, emotional withdrawal, decreased job satisfaction, intention to leave and job attrition (Huffman & Rittenmeyer, 2012; Oh & Gastmans, 2015). It is likely, therefore, that the moral distress experienced by nurses during the pandemic contributed to subsequent poor mental health. The knowledge gaps, therefore, include the types and degree of moral distress experienced by nurses in the pandemic, factors associated with moral distress during the pandemic, and its relation to longer-term mental health. Empirical evidence about how access to PPE and communication by hospital leadership relate to nurse moral distress and longer-term mental health has not been available.
The purpose of this study was to examine several questions: how (1) the frequency of caring for patients with COVID-19, (2) access to PPE and cleaning supplies and (3) the quality of communication by hospital leadership about hospital policies for patient care delivery related to nurses' moral distress during the first peak of COVID-19 and to nurses' longer-term mental health. Additionally, we examined how nurses' moral distress related to their longer-term mental health.
3 ∣. THE STUDY
3 1 ∣. Aims
The study aims were to explore factors associated with nurses' moral distress during the first COVID-19 surge and their longer-term mental health.
3.2 ∣. Design
We utilized a cross-sectional correlational design. We surveyed nurses from two academic medical centres in a Northeastern U.S. city to measure key variables. Nurses were surveyed in late September 2020 about their experiences during the first peak month of COVID-19 (i.e. April 2020).
3.3 ∣. Participants
Participants were registered nurses (RNs) who provided direct patient care. A convenience sample was identified by each hospital's nurse scientist. To assure variation across participants in the frequency of caring for COVID-19 patients, nurses were recruited from units with and without COVID-19 patients as well as emergency department and float pool. The sampling frame size was calculated based on being able to afford the study incentives, which were $15 Starbucks digital gift cards. We projected a 25% response rate and invited 800 nurses to participate to obtain a sample of 200. For this study, the sample inclusion criterion was non-missing data for at least 10 of 13 items for the primary outcome variable (moral distress).
3.4 ∣. Data collection
Data were collected via an online survey administered through RedCap for 1 week, (the last week of September 2020). Email invitations from the principal investigator were distributed by hospital nurse scientists to eligible nurses. The email provided a link to the survey.
3.5 ∣. Ethical considerations
We considered whether it was ethical to ask nurses about sensitive moral distress and mental health without providing services. We concluded that, given the potential for actionable evidence from this survey to improve future moral distress and longer-term mental health for nurses, this research was ethically sound. The research protocol was determined to be exempt. An informed consent letter was included in the recruitment email, which noted that participation was anonymous and voluntary, and choosing not to participate would in no way affect employment. The survey opened with a statement that the content may trigger unpleasant recollections and participants may not want to take the survey.
3.6 ∣. Measures
The measures are described in the order they were presented in the survey. Two demographic variables were nursing unit type and years of RN experience (fill-in).
COVID-19 care frequency was measured by three questions: (1) did you care for at least one COVID-19 patient? (2) How frequently did you care for COVID-19 or presumed positive COVID-19 patients during the peak month? (response categories: several times in the month, weekly or daily), and (3) Thinking back on the peak month, how many COVID-19 or presumed COVID-19 positive patients did you care for in total? (response categories: 1–5, 6–10, 11–20, 21–50 and more than 50). We provided categories with differing numbers of patients because, above 10, we expected nurses to recall the exact number with less precision and we wanted to simplify their choices to reduce respondent burden about a potentially triggering question while showing the full range of frequencies.
PPE and cleaning supplies access were measured by asking: ‘During the peak COVID-19 month, did you have difficulty accessing PPE or cleaning supplies?’ Respondents who reported difficulty were offered a ‘check all that apply’ question for each of five types of PPE (N95 masks, surgical masks, face shields, gowns and gloves) and two types of cleaning supplies (disinfectant wipes and cleaning solution), which allowed them to report how they accessed these items. We use the term workaround for these access attempts. The three workarounds were: (1) Access required re-use or extended use; (2) Access required ‘improvised’ PPE or cleaning supplies (e.g. cloth masks or paper towels with alcohol); and (3) Individuals provided their own PPE or cleaning supplies. For each nurse, we summed the number of checked workarounds for (1) each type of PPE/cleaning supply, (2) all types, as well as (3) the subset comprising facial PPE (masks, shields). The maximum possible value for one type of PPE/cleaning supply was three. The maximum value for all PPE/cleaning supplies was 21 (seven types of PPE by three workarounds). The maximum value for the subset of facial PPE was nine.
The COVID-MDS comprises nine items reflecting classic moral distress situations that nurses face and four reflecting COVID-19-specific situations. The four COVID-19-specific situations were patient-level (caring for patients who: must experience hospitalization without family presence; die during a hospitalization without family and/or clergy present; present transmission risk to your family/household) and hospital-level (being assigned/floated to a new unit, requiring unfamiliar skills or procedures). For each item, respondents were queried on how often they experienced the situation in their job and the level of distress they felt when they experienced it. Likert response categories and their scoring values were: did not experience this (0), rarely experienced this (1), occasionally experienced this (2) and experienced this often (3). Regarding level of distress, the response categories and their scoring values were: none (0), mild (1), moderate (2) and severe (3). We multiplied the two values to create item-specific moral distress, ranging from 0 to 9. The total COVID-MDS score was calculated as the mean of the item scores. The COVID-19 subscale score was calculated as the mean of the four COVID-19-specific items. The scores were computed by omitting items with missing data for respondents who had up to three missing of the 13 total or one missing of the four COVID-19 items. These thresholds were selected to require at least 75% of the scale items with non-missing data to generate these key variables.
Nurses' mental health was measured by a composite of recently experienced symptoms (‘felt anxious,’ ‘had difficulty sleeping’ and ‘felt withdrawn’). The format was similar to the Patient Reported Outcome Measure Indicator Set. Our stem was ‘Over the past week how many days have you:’ Respondents could select a value from 0 to 7. We summed the number of days across the three symptoms as well as calculated the mean across these symptoms. The mean indicates the number of days they experienced each symptom. Our data do not indicate if multiple symptoms were experienced on the same day or not in the previous week.
In a survey section labelled ‘Leadership and Communication,’ we asked: ‘How often did hospital policies change during the peak month and how were they communicated to clinical staff?’ Then we presented three statements with the stem: ‘Communication from hospital leadership was:’ and queried the terms ‘transparent,’ ‘effective’ and ‘timely’. We developed these questions to measure nurses' perceptions about the most salient elements of communication in pandemic circumstances (Scott-Cawiezell et al., 2004; Spalluto et al., 2020) while keeping the instrument as short as possible. Six Likert response categories were used: from strongly disagree to strongly agree. For each nurse, an overall mean summary was calculated.
3.7 ∣. Validity and reliability/rigour
The new, validated, COVID-19 Moral Distress Scale (COVID-MDS) was utilized (Cramer et al., 2021; under review for publication). The COVID-MDS was created to provide a short moral distress scale and capture moral distress specific to the COVID-19 patient care situation. We referred to the measure of moral distress for healthcare professionals (MMD-HP) (Epstein et al., 2019), comprising 27 items, regarded as the gold standard but considered too lengthy. We created facsimile items reflecting the three dimensions of the MMD-HP: patient-level, team/unit and system-level causes (Epstein et al., 2019). COVID-19-specific items were created by the authors, who include a hospital nurse ethicist and a health system critical-care nurse administrator, based on their knowledge about the unique bases of moral distress from the pandemic circumstances and the literature (Morley et al., 2020). Psychometric evaluation demonstrated two hypothesized factors (classic moral distress and COVID-19-specific moral distress) through confirmatory analysis and concurrent validity related to volume of COVID-19 patients cared for. Internal consistency for each factor was established with a Cronbach's alpha ranging from .74 (COVID-19-specific) to .84 (traditional) (Cramer et al., 2021). Overall scale reliability was .88.
3.8 ∣. Data analysis
Sample characteristics and key variables were described with descriptive statistics. Nurse experience and ICU unit type were correlated to moral distress (results not shown). Linear regression models were estimated for moral distress and mental health. For moral distress, explanatory variables were frequency of COVID-19 patient care, leadership communication, and PPE/cleaning supplies access. For mental health, we utilized the same explanatory variables and added moral distress. These models controlled for nurse experience and unit type (ICU/other).
We addressed bias by evaluating the extent and patterns of missing data. The most missing data were observed for the leadership communication variables and the mental health symptoms, for which the same 19 observations (6.2%) were missing, which was considered modest. These respondents stopped answering the survey midway and these were later sections. There were no significant differences in moral distress for those with complete versus missing data. To retain observations for the regression, we replaced missing data on the leadership communication summary variable with the mean value from each hospital. Analyses were completed utilizing Stata 16 software (Stata Press, 2021).
4 ∣. RESULTS
The response rate was 43% (338/795). This sample comprised 307 who met the inclusion criterion. Respondents were predominately from acute care (41%); adult ICU (24%) and the ED (24%). The remainder were float pool (6.5%) or other (3.6%). The average RN years of experience were 8.69 (SD=6.8).
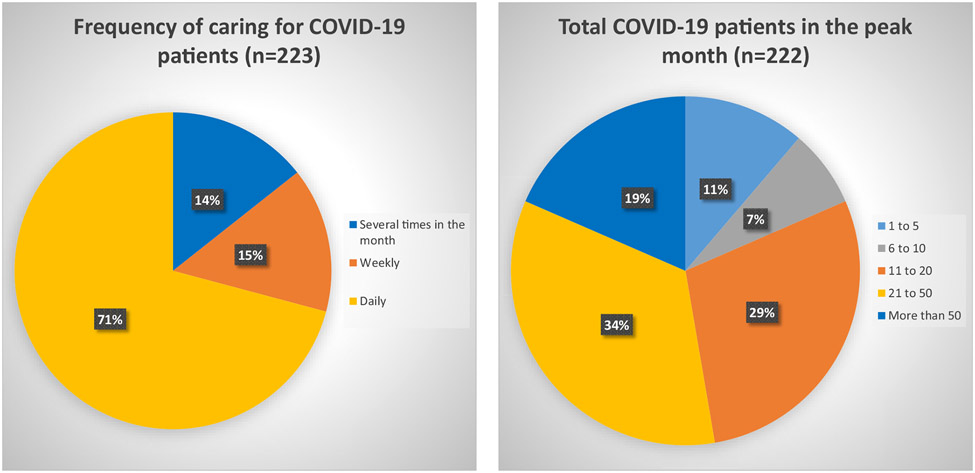
Most respondents (73%) had cared for at least one COVID-19 patient. Among these, 71% had cared for COVID-19 patients daily during the peak month (Figure 1). The largest proportion of respondents had cared for 21–50 patients with COVID-19 (34%).
FIGURE 1.
Frequency of COVID-19 patient care during the peak month.
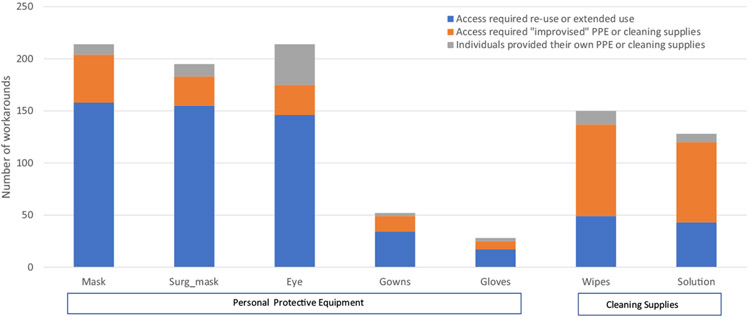
Over half (52.8%) of respondents had difficulty accessing PPE or cleaning supplies, principally masks and eye protection (i.e. face shields or goggles). Table 1 and Figure 2 display tallies for access workarounds by type of PPE/cleaning supply. Nearly all nurses reporting having difficulty accessing PPE reported reuse/extended use (one workaround) of N95 masks (98%) or surgical masks (96%). Ninety percent reported reuse/extended use of face shields. Of the three access workarounds (reuse/extended use, improvised use, providing your own), the greatest utilization was 1.3 workarounds per nurse for N95 and face shields/goggles. Gloves were the most accessible, evident from very few workarounds: 0.17 per nurse. Over half of the nurses with access difficulty had to improvise disinfectant wipes and cleaning solution. About one-quarter of nurses reported re-use/extended use of cleaning supplies. Overall, nurses reported trying, on average, 6 of 21 workarounds to access various types of PPE and cleaning supplies. They tried 4 of 9 workarounds, on average, to access facial PPE.
TABLE 1.
Workarounds for accessing PPE and cleaning supplies during the peak COVID-19 month (n = 171)
| Access required re-use or extended use |
Access required ‘improvised’ PPE or cleaning supplies (e.g. cloth masks or paper towels with alcohol) |
Individuals provided their own PPE or cleaning supplies |
|
|---|---|---|---|
| Type of PPE/cleaning supply | Frequency | Frequency | Frequency |
| N95 masks | 158 | 46 | 10 |
| Surgical masks | 155 | 28 | 12 |
| Eye protection including face shields or goggles | 146 | 29 | 39 |
| Gowns | 34 | 15 | 3 |
| Gloves | 17 | 8 | 3 |
| Disinfectant wipes | 49 | 88 | 13 |
| Cleaning solution | 43 | 77 | 8 |
| Total mask/eye/shield difficult to access, mean (SD) | 3.8 (1.6) | ||
| Total PPE/supplies difficult to access, mean (SD) | 6.1 (2.9) | ||
Note: Table data reflect subsample of nurses who reported difficulty accessing PPE or cleaning supplies.
FIGURE 2.
Frequency of workarounds for personal protective equipment and cleaning supplies.
Note. n=162 nurses answered these questions. Nurses may have reported multiple types of workarounds for each type of personal protective equipment and cleaning supply.
Table 2 displays percent distributions for response categories of leadership communication about policy changes to clinical staff during the peak COVID-19 month and the mean and SD for the summary measure. Most nurses reported that hospital leadership communication was transparent (70%), effective (70%) and timely (78%). The summary mean value was 4.1, equivalent to a ‘tend to agree’ response, with the SD of 1.1 equivalent to a one-category change.
TABLE 2.
Leadership communication (N = 228 respondents)
| Transparent |
Effective |
Timely |
|
|---|---|---|---|
| Percentage | Percentage | Percentage | |
| Strongly disagree | 5.6 | 4.9 | 4.5 |
| Disagree | 5.6 | 4.9 | 4.2 |
| Tend to disagree | 18.8 | 20.1 | 13.5 |
| Tend to agree | 29.5 | 32.6 | 35.1 |
| Agree | 29.2 | 29.5 | 34.4 |
| Strongly agree | 11.5 | 8.0 | 8.3 |
| Leadership communication summary, mean (SD) | 4.1 (1.1) | ||
Table 3 displays moral distress item, subscale and summary scores. The average moral distress score was 1.9 (range: 0.0–7.8; hypothetical range 0–9). ICU nurses exhibited the highest moral distress (2.4), which was significantly higher than nurses on other nursing units (p < .001) except float pool nurses, whose moral distress was 2.0.
TABLE 3.
Moral distress
| Frequency |
Distress |
Multiplied score |
|
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| Experiencing poor communication between members of the care team that adversely affects patient care | 1.0 (0.9) | 0.9 (0.9) | 1.6 (1.9) |
| Being assigned an unsafe number of patients to care for at once considering the acuity level for each patient assigned to me | 0.8 (0.9) | 0.8 (1.0) | 1.4 (2.1) |
| Being asked to provide and continue aggressive and potentially futile treatments when I believe it is not in the best interest of the patient | 0.9 (1.0) | 0.9 (1.0) | 1.6 (2.4) |
| Lacking enough resources or bed capacity and therefore being required to ‘ration’ care (i.e. care is provided to some patients) | 0.5 (0.9) | 0.5 (0.9) | 1.0 (2.0) |
| Using technology and documentation that burdens me and compromises patient care | 0.5 (0.8) | 0.4 (0.7) | 0.7 (1.5) |
| Witnessing or experiencing uncivil behaviour among members of the care team | 0.4 (0.7) | 0.4 (0.8) | 0.7 (1.5) |
| Caring for patients who must experience hospitalization without family presence | 2.6 (0.9) | 1.7 (0.9) | 4.8 (2.8) |
| Caring for patients who die during a hospitalization without family and/or clergy present | 1.4 (1.1) | 1.5 (1.2) | 3.2 (3.1) |
| Being assigned/floated to a new unit, requiring unfamiliar skills or procedures | 1.0 (1.1) | 0.8 (1.0) | 1.7 (2.5) |
| Caring for COVID-19 patients that presents transmission risk to your family/household | 2.2 (1.1) | 1.9 (1.1) | 5.1 (3.4) |
| Witnessing orders for unnecessary or inappropriate care that do not adequately address patient needs | 0.7 (0.8) | 0.6 (0.8) | 1.0 (1.8) |
| Witnessing lack of respect among healthcare team for patients from vulnerable populations or minority groups | 0.4 (0.7) | 0.4 (0.8) | 0.7 (1.7) |
| Providing care to patients who have not been adequately informed or included in decisions about their own care | 0.7 (0.8) | 0.6 (0.8) | 1.0 (1.7) |
| COVID subscale, mean (SD) | 1.8 (0.7) | 1.9 (0.6) | 3.7 (2.2) |
| Summary score, mean (SD) | 1.0 (0.6) | 0.9 (0.6) | 1.9 (1.4) |
Note: n varies from 306 to 307 due to missing data.
Overall, nurses reported a higher frequency of experiencing COVID-19-specific morally distressing situations, equivalent to ‘occasionally’, and found those situations moderately distressing, as compared with non-COVID-19 situations, which were experienced rarely while generating moderate distress. COVID-19-specific situations that produced the most distress were transmission risk, caring for patients without family members present, and caring for patients who die without family/clergy present. Among non-COVID-19-specific situations presented in the survey, ones that produced the most moral distress were being required to ration care, being asked to provide aggressive, potentially futile treatments when the nurse believes it is not in the patient's interest, witnessing a lack of respect from care team members for patients from vulnerable/minority groups, and being assigned an unsafe number of patients.
Regarding mental health, in the week before the survey (5 months after the first COVID-19 peak) nurses reported an average of 3.1 (SD = 2.1) days feeling anxiety, 1.8 (SD = 2.2) days feeling withdrawn and 2.7 (SD = 2.3) days of difficulty in sleeping. The total days nurses experienced the three symptoms was 7.6 (SD = 5.7), which ranged from 0 to 21; 21 would mean all three symptoms were experienced all 7 days. The mean number of days was 2.5 (SD = 1.9) in which one or more symptoms were experienced in the past week. Table 4 presents regression results for moral distress and longer-term mental health. In bivariate models, lower COVID-19 care frequency, better leadership communication, and less difficulty accessing PPE/supplies were significantly associated with less moral distress. In a multivariate regression model that controlled for nurse experience and unit type (dummy variable ICU yes/no), moral distress decreased with effective leadership communication and access to PPE/cleaning supplies, and increased with more than 20 COVID-19 patients in the peak month (p < .01). A typical variation in leadership communication (a 1 SD improvement), i.e. a one Likert response category shift, was associated with a .28 SD change in moral distress. An increase of 1 SD in the number of PPE workarounds used was associated with a .41-point increase in the moral distress score, a .29 SD. Nurses who cared for 21–50 patients had .42 higher moral distress score (.29 SD). Nurses who cared for more than 50 COVID-19 patients had .82 higher moral distress score (.58 SD). The explained variance (R-squared) for the multivariate model was .39. The two demographic control variables, years of RN experience and whether the nurse worked in the ICU, were both significantly related to moral distress. ICU nurses had .52 higher moral distress score (p = .001), equivalent to .36 SD. Each additional year of RN experience was associated with .02 lower moral distress (p = .016), equivalent to .01 SD.
TABLE 4.
Multivariate regression results—standardized continuous explanatory variables
| Bivariate |
Multivariate |
Multivariate with control variables |
||||
|---|---|---|---|---|---|---|
| Outcome variable | Coef. | p > ∣t∣ | Coef. | p > ∣t∣ | Coef. | P > ∣t∣ |
| Moral distress | ||||||
| COVID care frequency | ||||||
| 1–10 | −0.14 | .593 | −0.37 | .101 | −0.34 | .116 |
| 11–20 | 0.30 | .174 | −0.08 | .670 | 0.06 | .733 |
| 21–50 | 0.89 | <.001 | 0.40 | .034 | 0.42 | .024 |
| >50 | 1.20 | <.001 | 0.78 | .001 | 0.82 | <.001 |
| Leadership communication | −0.56 | <.001 | −0.41 | <.001 | −0.39 | <.001 |
| PPE/supplies access | 0.61 | <.001 | 0.46 | <.001 | 0.41 | <.001 |
| Mental health (longer term) | ||||||
| COVID care frequency | ||||||
| 1–10 | −0.66 | .074 | −0.64 | .079 | −0.62 | .085 |
| 11–20 | −0.64 | .050 | −0.75 | .017 | −0.69 | .030 |
| 21–50 | −0.32 | .300 | −0.69 | .024 | −0.72 | .019 |
| >50 | 0.78 | .042 | 0.37 | .326 | 0.28 | .463 |
| Leadership communication | −0.35 | .001 | −0.20 | .086 | −0.20 | .074 |
| PPE/supplies access | 0.25 | .026 | 0.2 | .869 | 0.03 | .821 |
| Moral distress (COVID-19 peak) | 1.67 | <.001 | 0.44 | .001 | 0.45 | .001 |
Note: Moral distress was queried about the first peak month of COVID-19 patients, i.e. April 2020. Mental health was queried about the week before the survey, i.e. late September 2020. The control variables were a dummy indicating intensive care unit or other unit type and years of registered nurse experience.
In bivariate models of longer-term mental health, having more than 50 COVID-19 patients in the peak month, better leadership communication, less difficulty accessing PPE/supplies and lower moral distress in the peak month were significantly associated with better mental health. In a multivariate model that controlled for experience and unit type, moral distress during the COVID-19 peak month and effective leadership communication were significantly associated with mental health (p < .01). A 1 SD increase in the moral distress scale score was associated with a .45 increase in the mental health score, equivalent to .24 SD. The explained variance (R-squared) for the multivariate model was .15.
5 ∣. DISCUSSION
We were motivated to examine how leadership communication, as a modifiable factor, might mitigate hospital nurses' moral distress and later mental health during the COVID-19 pandemic. Utilizing Epstein's three levels of moral distress, we conceptualized leadership communication as a mid-level strategy to mitigate moral distress. Accordingly, we hypothesized that transparent, timely and effective communication would reduce nurses' moral distress and mental health symptoms.
Consistent with Epstein's (2019) framework, we found that COVID-19 patient care volume and PPE workarounds increased moral distress, while effective leadership communication decreased it. Unique features of pandemic patient care were the greatest sources of nurses' moral distress. Increased moral distress resulted in poorer post-surge mental health. The largest effect on moral distress was noted for nurses who had cared for more than 50 COVID-19 patients in April 2020. This group had over half an SD higher moral distress score. Remaining significant explanatory variables, i.e. leadership communication, PPE workarounds, and having 21–50 COVID-19 patients, all had a similar, small to medium, effect on moral distress. Our multivariate model of moral distress explained 39% of the variance, a high degree of explained variance. Although most nurses reported positively about leadership communication, the responses covered the full range from strongly disagree to strongly agree. These findings add to the literature, which noted increased distress with increased COVID-19 patients, poor communication and less PPE, as noted in two systematic reviews. Among 8500 U.S. hospital nurses surveyed in February 2021 by the American Nurses Foundation (ANF) on what would better prepare them for future pandemics, the third most frequent response, was effective leadership communication, reported by 70% of respondents. One fifth intended to leave their position in the next six months. Notably, half of these nurses worked in Magnet or Pathway to Excellence hospitals, which are recognized for their excellent nursing standards and work environments, respectively (ANF, 2021).
Regarding the large COVID-19 patient frequency effect size, we theorize that caring for a large volume of COVID-19 patients inherently increases the nurse's exposure to morally distressing situations, heightens PPE access issues and requires dealing with rapid policy changes.
We theorize that there are several ways in which leadership communication might influence moral distress. Poor leadership communication may lead nurses to feel unsupported amid a crisis. Good leadership communication acknowledges the difficulty of the situation, its rapidly changing status and provides rationales for changing policies.
The association of PPE workarounds to moral distress is not surprising given the transmission risks that nurses faced. Uncivil behaviour among staff might have contributed to moral distress if limited PPE led to problematic interactions among co-workers or those deciding how to ration PPE. Circumstances of severe workarounds to obtain PPE is likely to correlate with concurring broader chaos in the healthcare setting, which fuels morally distressing situations even if they are not about transmission risk.
Research shows that in the early pandemic months, HCWs experienced high rates of anxiety, depression and sleep problems (Muller et al., 2020). Our novel contribution is demonstrating continued higher rates months later, during a time when this city had experienced stable, relatively low rates of COVID-19 for 4 months following the peak.
We found that the only explanatory variable significantly associated with longer-term mental health was moral distress in the peak COVID-19 month. Although considerable pre-pandemic literature links moral distress to concurrent poor nurse outcomes including anxiety and depression (Huffman & Rittenmeyer, 2012; Oh & Gastmans, 2015), to our knowledge the link between moral distress and longer-term mental health has not been established previously. This unfortunate finding may be due to the psychological trauma of moral distress. Additionally, without an indication that circumstances would improve, the prospect of a second wave of COVID-19 patients may have created anticipatory moral distress.
As noted by Spalluto et al. (2020), the SARS infectious outbreak from 2002 to 2004 yielded a near-identical scenario of increased stress, uncertainty, information overload, constant policy changes and insufficient health system resources. Our study reveals a similar circumstance, indicating that we have not learned from 2 decades of prior outbreaks. We are overdue to create resilient structures to meet future challenges.
5.1 ∣. Relevance to clinical practice and nursing management
Our findings have implications for managers. To mitigate moral distress, nurse managers should provide clearly communicated policies and guidelines. Consistent with our study, others have found that clear and timely communication about frequent policy changes, solicitation of questions and concerns from clinical nurses, and timely responses to those concerns enable nurses to practice with certainty and support, knowing their care is based on the best available information (Rosa et al., 2020).
Forthwith, managers should develop unit policies for a crisis standard of care and educate staff about them. Implementing a unit or health system-based plan may foster a relationship before a crisis between nurses and managers, increasing the potential for more open and effective communication to occur when a crisis happens. Nurses should be invited to leverage their unique vantage point to collaboratively create policies and protocols as well as solutions to mitigate moral distress.
Nurses caring for the highest frequency of COVID-19 patients and ICU nurses had the highest moral distress. Accordingly, managers should direct resources to these nurses. Morley et al. (2020) detail how to recognize moral distress and evidence-based recommendations for leaders. Webster and Wocial (2020) provide resources and self-care strategies for nurses experiencing moral distress, ranging from wellness tips to pro-bono teletherapy for COVID-19 frontline clinicians. The ANA has held numerous webinars for clinicians and managers and also provides a wellness website with links to apps, podcasts and hotlines (ANA, 2020b). Direct care nurses may benefit if a designated staff member, e.g. the staff development leader, curates such resources.
Our findings have implications for nursing education. Comprehensive ethics education should be mandated for all nurses but is not currently universally required. This education would give nurses tools to identify ethical implications and challenges of a crisis standard of care. This education should include the nature of moral distress and resources to address it.
Our findings have research implications. A paramount research focus is the cumulative effect on moral distress of pandemic patient care over many months, as well as effects of moral distress on post-pandemic mental health. The potential for a better nurse work environment to mitigate moral distress during a crisis is worthy of investigation given that transparent communication is one element of a favourable work environment. Interventions about communication timing and methods (i.e. daily huddles), and content may be developed and tested to ameliorate nurses' moral distress.
5.2 ∣. Limitations
Our study had several limitations. Our sample was a convenience sample from two urban academic medical centres in the Northeastern U.S. Results may not generalize to nurses working in other hospital types and regions. Even with a relatively high response rate of 43% for a 1 week survey conducted in the crisis circumstances of 2020, the response rate may have yielded bias from willing respondents' views and experiences. These responses may have differed from those of nurses who chose not to participate. There was potential recall bias of nurses recalling events and distress from 5 months earlier. Those events and distress, however, were likely to have made a distinct impression. The cross-sectional design prevents causal inference about the effects of moral distress on mental health. Unmeasured variables may have helped explain nurses' moral distress and longer-term mental health, such as nurses' pre-pandemic mental health, their resilience or their work environment. A more detailed measure of communication in future studies may provide additional insights for managers.
6 ∣. CONCLUSION
We examined moral distress and post-surge mental health in nurses caring for COVID-19 patients during April 2020. The data supported Epstein's framework by revealing that the three levels of moral distress contributed significantly to moral distress. Unique features of pandemic patient care generated the most moral distress. Transparent and timely leadership communication correlated to decreased moral distress, which in turn improved post-surge mental health. Given the lingering negative effects on nurses of suffering moral distress during a crisis, our findings should motivate and provide guidance for leaders in future crises.
ACKNOWLEDGEMENTS
The authors wish to thank the staff nurses who completed the survey and Morgan Peele for her analytic support.
Funding information
Dr. Clark's postdoctoral fellowship and Ms. French's and Ms. Rosenbaum's predoctoral fellowship are supported by funding from the National Institute of Nursing Research, National Institutes of Health [Aiken, PI; T32NR007104].
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- American Nurses Association. (2020a). Crisis standard of care: COVID-19 pandemic, https://www.nursingworld.org/~496044/globalassets/practiceandpolicy/work-environment/health--safety/coronavirus/crisis-standards-of-care.pdf
- American Nurses Association. (2020b). Well being initiative, https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/the-well-being-initiative/
- American Nurses Association. (2020c). What 32,000 nurses want you to know about treating COVID-19. https://www.nursingworld.org/~4987e5/globalassets/covid19/ana_covid19infographic_dataset1_20200424-final.pdf
- American Nurses Foundation. (2021). Year One COVID-19 Impact Assessment. https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/year-one-covid-19-impact-assessment-survey/
- Arnetz JE, Goetz CM, Sudan S, Arble E, Janisse J, & Arnetz BB (2020). Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. Journal of Occupational and Environmental Medicine, 62(11), 892–897. 10.1097/JOM.0000000000001999 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Coronavirus disease 2019 (COVID-19): Using personal protective equipment (PPE). https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html
- Cramer Smith, Rogowski, & Lake. (2021). Measuring moral distress in nurses during a pandemic: Development of the COVID-MDS. Paper presented at the AcademyHealth Annual Research Meeting, virtual. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, & Hamric AB (2019). Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empirical Bioethics, 10(2), 113–124. 10.1080/23294515.2019.1586008 [DOI] [PubMed] [Google Scholar]
- Hamric AB (2014). A case study of moral distress. Journal of Hospice and Palliative Nursing, 16(8), 457–463. 10.1097/NJH.0000000000000104 [DOI] [Google Scholar]
- Huffman DM, & Rittenmeyer L (2012). How professional nurses working in hospital environments experience moral distress: A systematic review. Critical Care Nursing Clinics, 24(1), 91–100. 10.1016/j.ccell.2012.01.004 [DOI] [PubMed] [Google Scholar]
- Jameton A (1984). Nursing practice: The ethical issues. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Morley G, Sese D, Rajendram P, & Horsburgh CC (2020). Addressing caregiver moral distress during the COVID-19 pandemic. Cleveland Clinic Journal of Medicine, 10.3949/ccjm.87a.ccc047. PMID: 32518134. [DOI] [PubMed] [Google Scholar]
- Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SØ, Stroobants S, Van de Velde S, & Vist GE(2020). The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research, 293, 113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Nurses United. (2020). Survey of nation's frontline registered nurses shows hospitals unprepared for COVID-19. Retrieved 7/16/2021, 2021, from https://www.nationalnursesunited.org/press/survey-nations-frontline-registered-nurses-shows-hospitals-unprepared-covid-19
- Oh Y, & Gastmans C (2015). Moral distress experienced by nurses: A quantitative literature review. Nursing Ethics, 22(1), 15–31. 10.1177/0969733013502803 [DOI] [PubMed] [Google Scholar]
- Rosa WE, Schlak AE, & Rushton CH (2020). A blueprint for leadership during COVID-19. Nursing Management, 51(8), 28–34. 10.1097/01.NUMA.0000688940.29231.6f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagherian K, Steege LM, Cobb SJ, & Cho H (2020). Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. Journal of Clinical Nursing, 10.1111/jocn.15566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Schenkman M, Moore L, Vojir C, Connolly RP, Pratt M, & Palmer L (2004). Exploring nursing home staff's perceptions of communication and leadership to facilitate quality improvement. Journal of Nursing Care Quality, 19(3), 242–252. [DOI] [PubMed] [Google Scholar]
- Spalluto LB, Planz VB, Stokes LS, Pierce R, Aronoff DM, McPheeters ML, Omary RA (2020). Transparency and trust during the coronavirus disease 2019 (COVID-19) pandemic. Journal of the American College of Radiology, 17(7), 909–912. 10.1016/j.jacr.2020.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Press. (2021). Stata 16 for Windows.
- Webster L, & Wocial LD (2020). Ethics in a pandemic. https://www.myamericannurse.com/ethics-in-a-pandemic-2/ [Google Scholar]
- Wolf LA, Perhats C, Delao AM, Moon MD, Clark PR, Zavotsky KE (2016). “It's a burden you carry”: describing moral distress in emergency nursing. Journal of Emergency Nursing, 42(1), 37–46. 10.1016/j.jen.2015.08.008 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2015). Ethics in epidemics, emergencies and disasters: research, surveillance and patient care. https://www.who.int/publications/i/item/ethics-in-epidemics-emergencies-and-disasters-research-surveillance-and-patient-care-training-manual
- Young KP, Kolcz DL, O'Sullivan DM, Ferrand J, Fried J, & Robinson K (2020). Health care workers' mental health and quality of life during COVID-19: Results from a mid-pandemic, national survey. Psychiatric Services, 72,122–128. 10.1176/appi.ps.202000424 [DOI] [PubMed] [Google Scholar]
- Zuzelo PR (2020). Making do during a pandemic: Morally distressing and injurious events. Holistic Nursing Practice, 34, 259–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.