Abstract
Purpose:
To obtain information on how family visitor restriction during the COVID-19 pandemic has impacted the workplace experience of physicians and nurses in the medical intensive care unit, and to assess differences by profession.
Materials and methods:
We developed a survey containing closed- and open-ended questions, applying both quantitative and qualitative analyses to our results.
Results:
Of the 74 respondents, 29 (38%) were nurses and 45 (62%) were physicians. Nurses reported positive changes to daily workflow and the ability to provide medical care, while physicians reported negative changes in these areas. Both groups reported decreased comprehension and increased distress among families, and decreased ability to provide end-of-life care. For the qualitative analysis, eight themes were identified: the patient’s room as space, creation of a new space through virtual communication, time, increased complexity of care, challenges around the use of technology, adjustments to team roles and responsibilities, desire for families to return, and internal tension.
Conclusion:
Intensive care physicians and nurses reported both positive and negative effects of family visitor restriction during the COVID-19 pandemic, with significant differences based on profession. Both groups expressed concern for an overall negative impact of visitor restriction on healthcare workers, patients, and their families.
Keywords: Caregivers, critical care, family, nurses, pandemics, physicians, visiting
Introduction
Family members are an integral part of the care team for patients in the intensive care unit (ICU), providing history to physicians and nurses, acting as surrogate decision makers, and assisting with patient care tasks such as reorientation. Family presence in the ICU has been associated with improved outcomes for patients (Fumagalli et al., 2006; Hendrickson, 1987), and has been shown to reduce psychological distress among family members (Chapman et al., 2016; Rosa et al., 2019). Restrictions on family visitation were previously common in hospitals across the United States (US), owing largely to concerns about infection control and patient physiologic stress, but multiple studies demonstrated that these concerns were unfounded (Netzer & Iwashyna, 2017). As such, limitations on family visiting hours in the ICU have been relaxed or removed altogether, and increased family presence is now a recommended best practice for patient- and family-centred care (Davidson et al., 2017; Gerritsen et al., 2017).
With the onset of the COVID-19 pandemic, family visitation at hospitals has been drastically reduced or eliminated as part of infection prevention efforts (Andrist et al., 2020). Epidemiologic data are sparse, but one study estimated that 98% of ICUs have implemented a “no visitor” policy as a result of COVID-19 (Valley et al., 2020). While complete visitor restriction during a pandemic offers the benefit of protecting healthcare workers (HCWs) from a source of infection transmission, experience from previous pandemics suggests that there are also potential negative effects, such as being put in the challenging position of conveying bad news over the phone and bearing the brunt of frustration or anger felt by families with regard to visitor restriction (Morley et al., 2020; Rogers, 2004; Wilder-Smith & Low, 2005). How the COVID-19 family visitor restriction has affected healthcare workers in the ICU is unknown.
We conducted a survey of HCWs in the ICU to assess the impact of family visitor restriction on the workplace experience. Our objectives were to gain an understanding of perceived changes to the workplace experience and to assess for differences in experience by profession.
Materials and Methods
Research Design
For this analysis, we sought to answer the following question: How has the restricted family visitation policy impacted HCWs in the ICU? We developed and administered a survey to answer this question, incorporating both quantitative and qualitative data. This design has previously been used in survey research designed to assess the experiences of nurses (Kelly et al., 2009).
Ethical Considerations
The protocol was submitted to the institutional review board at the University of North Carolina at Chapel Hill and was determined to be exempt from further review (20–0416).
Setting
Our study took place in the medical intensive care unit (MICU) of a 1000-bedded academic, tertiary referral, public medical centre in the southeastern United States (US). The MICU is a 30-bed unit containing both patients with COVID-19 in a strict isolation zone, and without COVID-19 in a usual infection prevention structure. The survey population included HCWs caring for both populations on separate days. Beginning on March 23rd, 2020, no family visitors were allowed into the medical centre with the exception of a few specific circumstances including paediatric patients, women in labour, and end-of-life care. For end-of-life care in the MICU, once a transition had been made to comfort measures only and/or a determination had been made that the patient was actively dying, one family member was allowed to come to the bedside for a single one-hour visit. In an effort to promote virtual communication in lieu of bedside communication with families, multiple tablet computers were procured to be used for remote communication between HCWs and families and/or patients and their families.
Survey Development
A physician workgroup examined the relevant literature, and in the absence of a validated instrument developed an exploratory survey with questions pertaining to the impact of family interaction on the daily workflow of ICU HCWs (defined here as the series of tasks that are necessary to provide patient care). Questions were developed a priori based on concepts thought by the study team to be relevant and important. The first 6 questions assessed participant demographics and role. The next 17 questions assessed changes in daily workflow, job-related satisfaction, and emotional distress. There were two types of closed-ended questions: questions with categorical response options, and questions with a continuous response option. For the continuous response option, participants responded on a scale ranging from 0 to 100, with 0 being the most negative response option, 50 being neutral, and 100 being the most positive response option. The two open-ended questions were: 1) If you are willing, please provide additional comments on how your daily workflow has been affected, and 2) Please provide any additional comments about what can be done to better support you right now. A pilot version of the survey was pretested in a small group of physicians to assess the clarity and revise structure.
Survey Population and Administration
The survey was distributed via email in June 2020 to nurses, physicians, and advanced practice providers (APPs) working in the MICU. The survey opened on June 4th, 2020, and closed on June 16th, 2020. For nurses, both nurses working primarily at the bedside as well as nurse managers in the ICU were included. APPs are defined as a licensed, non-physician group of providers including nurse practitioners and physician assistants (Cooper et al., 1998). Each physician team in the MICU consists of an attending physician, a fellow (a physician who has completed internal medicine residency and is obtaining subspecialty training in critical care medicine), and one or more internal medicine residents (a physician who has completed medical school and is training to become certified in internal medicine). As each of these groups plays an important role in patient care, all were included in our survey population. Internal medicine residents, fellows, and attending physicians received an email if they had been scheduled for at least one shift since the initiation of the family visitor restriction. A directory was used to distribute the survey to all nurses and APPs in the MICU. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of North Carolina (Harris et al., 2009).
Quantitative Analysis
Quantitative data were analysed using Stata software (Stata/IC 15.1, College Station, TX). Data were summarised using descriptive statistics, with mean and standard deviation for continuous variables and frequency and percentage for categorical variables. For comparing responses between HCW types, a chi-square test was used to assess categorical variables. The chi-square test is used to test for an association between two categorical variables (Wechsler, 1997). For continuous variables, two methods were used to assess normality: 1) histograms were used to visually assess the distribution of each variable, and 2) the means and medians for each variable were compared, with a highly similar mean and median suggesting a normal distribution and a large difference in the mean and median suggesting a skewed distribution. One-way analysis of variance was used to compare mean values by category for continuous outcome variables with a normal distribution (Altman & Bland, 1996). The Kruskal-Wallis test was used to compare medians for continuous outcome variables with a skewed distribution (Sedgwick, 2012). A 2-sided significance level was set at <0.05.
Qualitative Analysis
We used conventional content analysis to analyse responses to the two open-ended questions. This method was selected because we found no existing theory or literature applicable to this research question (Hsieh & Shannon, 2005). Analysis began with repeated reading of the data to achieve immersion. Words and phrases that captured key thoughts and concepts were identified, and these were transformed into the initial coding scheme. From here, categories were created separately within the responses to each of the two open-ended questions. These categories were reviewed together for similarities and differences to ensure that all important concepts had been recognised while minimising redundancy and overlap. Finally, a single set of core themes emerged. Figure 1 displays our study design and the use of both quantitative and qualitative data to fully explore HCW perspectives on family visitor restrictions.
Fig. 1.
Study design using both quantitative and qualitative data.
Results
Survey invitations were sent to a total of 169 HCWs, and we received 76 completed surveys, for a 45% response rate. APPs were not included in the analysis due to very small sample size (n=2). Guidelines developed by experts in the field of survey research were consulted in the reporting of these results (Burns et al., 2008).
The mean age of respondents was 34.3 years (SD 7.5), and 50% were women. Participants had been in their role for an average of 4.2 years (SD 4.9), and the majority spent time providing care to both patients with and without COVID-19 (n=60, 81%). In terms of role type, 16 (22%) were attending physicians, 21 (28%) were residents, 8 (11%) were fellows, 28 (38%) were nurses working primarily at the bedside, and 1 (1%) was a nurse manager. Complete characteristics of respondents are shown in Table 1.
Table 1:
Baseline characteristics for entire cohort
| Variable | All providers (n=74) |
|---|---|
| Age, y, mean (SD) | 34.3 (SD 7.5) |
| Gender, No. (%) | |
| Male | 37 (50%) |
| Female | 36 (49%) |
| Gender non-conforming | 1 (1%) |
| Role, No. (%) | |
| Attending Physician | 16 (22%) |
| Resident Physician | 21 (28%) |
| Fellow Physician | 8 (11%) |
| Nurse practicing primarily at the bedside | 28 (38%) |
| Nurse manager | 1 (1%) |
| Years in role, y, mean (SD) | 4.2 (SD 4.9) |
| Schedule, No. (%) | |
| All days | 6 (8%) |
| Mostly days, some nights | 35 (47%) |
| An even mix of days and night | 21 (29%) |
| Mostly nights, some days | 7 (9%) |
| All nights | 5 (7%) |
| Have you directly participated in the care of a patient who has tested positive for SARS-CoV-2 (aka COVID19)? No. (%) | |
| Yes, I currently only provide care to patients with COVID19 | 10 (14%) |
| Yes, I currently mostly provide care to patients with COVID19, but also to some patients without COVID19 | 27 (36%) |
| I provide care to a mix of patients with and without COVID19 | 33 (45%) |
| No, I have not participated in the care of any patients with COVID19 | 4 (5%) |
For the quantitative analysis, all physicians were condensed into a single “physician” category, and all nurses were condensed into a single “nurse” category (an additional analysis was completed without condensing these categories, and trends within and between groups were unchanged). To identify any differences in perceived workplace experience based on profession, we used statistical testing (chi-square, one-way analysis of variance, and Kruskal-Wallis testing) to make comparisons between these two categories. Comparing physician and nurse estimates of average time spent with families before the total family visitor restriction, we found that physicians spent significantly more time than nurses communicating with families over the phone, whereas nurses spent significantly more time than physicians communicating with families at the bedside (Figure 2). Both groups reported an increase in time spent on the telephone with patient families, with a higher proportion of nurses reporting use of a web-based application to facilitate communication with patient families compared to physicians (93% vs. 71%, p=0.02). We then compared responses to questions utilizing the continuous 0–100 scale between physicians and nurses. When reporting changes to daily workflow, nurses reported an overall positive change and physicians reported a negative change (70.9 vs 26.0, p<0.0001). A similar trend was seen with perceived changes to the ability to provide medical care, with nurses reporting a positive change and physicians reporting a negative change (74.3 vs. 34.7, p<0.0001). Nurses reported an increase in job-related satisfaction while physicians reported a decrease (60.4 vs. 38.7, p<0.0001), and nurses reported an increase in the amount of interpersonal connection they felt with patients while physicians reported a decrease (58.7 vs. 31.4, p<0.0001). Both physicians and nurses reported a negative impact on end-of-life care, a perceived increase in family emotional distress, and a decrease in family comprehension during telephone updates. The results of questions with continuous response options are are shown in Table 2.
Fig. 2.
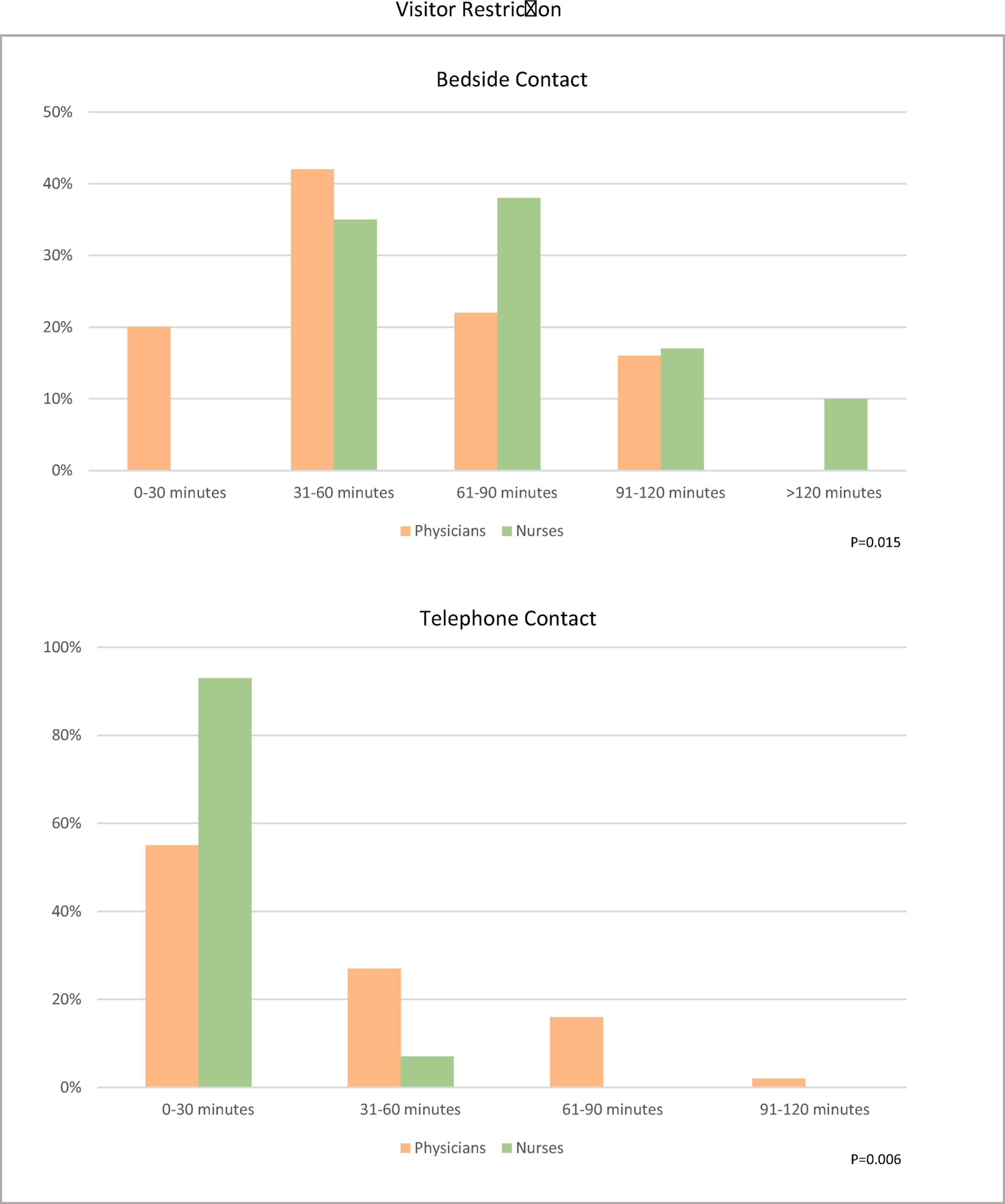
Average amount of bedside and telephone contact with families per day prior to visitor restriction.
Table 2:
Comparison of continuous responses by HCW type* Scores reported as Mean (Standard Deviation, SD) or Median (Interquartile Range, IQR)
| Has the absence of family visitors changed… | Physicians (n=45) | Nurses (n=29) | p-value |
|---|---|---|---|
| …your ability to provide medical care for patients in the medical intensive care unit (MICU)? | 26.0 (16.7) | 70.9 (22.7) | <0.0001 |
| …your ability to provide end-of-life care for patients in the medical intensive care unit (MICU)? | 16.4 (20.3) | 33.8 (27.6) | 0.009 |
| …your daily workflow? | 34.7 (20.7) | 74.3 (18.5) | <0.0001 |
| Following implementation of the family visitor restriction in the MICU… | Physicians (n=45) | Nurses (n=29) | p-value |
| …have you observed a change in family comprehension of their loved one’s medical situation when providing telephone updates? | 26.4 (20.2) | 33.4 (20.5) | 0.17 |
| …have you observed a change in family emotional distress when providing telephone updates? | 63.9 (22.0) | 62.7 (19.4) | 0.27 |
| …have you experienced a change in your own job-related emotional distress? | 58 (50–74) | 50 (36–71) | 0.08 |
| …have you experienced a change in your job-related satisfaction? | 38.7 (13.3) | 60.4 (22.9) | <0.0001 |
| …have you noticed a change in the amount of interpersonal connection you experience with your patients? | 31.4 (15.5) | 58.7 (22.7) | <0.0001 |
| …have you noticed a change in the amount of interpersonal connection you experience with patients’ families? | 23.8 (18.0) | 32.7 (18.4) | 0.12 |
| …has the amount of time you spend on the telephone with patients’ families changed? | 75.8 (19.3) | 71.2 (17.5) | 0.14 |
This table compares the results of questions with continuous response options between physicians and nurses. The first column shows the question that was asked. Participants responded to each question on a scale ranging from 0 to 100, with 0 being the most negative possible change, 50 being neutral or no change, and 100 being the most positive possible change. The second column shows the mean or median score for physicians. The third column shows the mean or median score for nurses. The fourth column shows the p-value for the comparison between the two groups.
Qualitative analysis for themes from the written responses was performed for the two open-ended survey responses. The following eight themes were identified:
Theme 1:
The patient’s room as space. Nurses found it easier to deliver care to patients with more space to manoeuvre.
“It’s easier practically to move around the room, and get to the patient in order to provide appropriate medical care. It’s also easier to provide appropriate medical care for pts.”
–Participant 4, Nurse
“The lack of visitors has allowed an easier workflow in getting in and out of rooms … I am able to get all tasks completed without reaching over family members…”
–Participant 46, Nurse
Physicians missed providing updates to family members in patients’ rooms while they were visiting.
“Harder to do family updates as part of natural workflow, I often relied on touching base with family when seeing patients in the afternoon.”
–Participant 9, Physician (Attending)
Theme 2:
Creation of a new virtual space for visitation. With family members not able to visit the bedside, nurses and physicians had to change how they communicated with family members.
“It has made us more conscious about providing daily updates for families, rather than waiting for the family to come by the unit.”
– Participant 14, Physician (Attending)
“… this has shown me there are more ways for family to communicate with the patient than I had thought of prior to the COVID restrictions. The iPads in the unit are very helpful in assisting video visits versus just over the phone.”
– Participant 58, Nurse
Virtual communication with families with Limited English Proficiency (LEP) presented additional challenges:
“…The Spanish-speaking family members are not receiving the same amount of updates and it is difficult as we used to be able to update the patient and the family at the same time previously with a bedside translator.”
– Participant 46, Nurse
Theme 3:
Time. Many nurses found that the no visitation rule saved them time, whereas physicians reported increased time burdens.
“Overall, absence of family has made it easier to provide care uninterrupted and more efficiently ….”
–Participant 22, Nurse
“I feel like I definitely have more time for patient care. I am not constantly being interrupted with a million questions from family members.”
–Participant 75, Nurse
“Significantly extra time with family contact given all patients need some level of update.”
– Participant 50, Physician (Resident)
Theme 4:
Increased complexity of care. Goals of care conversations and end-of-life care were challenging for nurses and physicians when family members are not allowed to visit.
“… I feel that end of life and suffering is drawn out as family members do not get to witness and thus understand the extent their family member is struggling.
– Participant 27, Nurse
“It feels harder for families to comprehend the severity of illness and gravity of their loved one’s situation when they aren’t present. …
– Participant 31, Physician (Fellow)
“…. It has been devastating to see family members say goodbye via FaceTime or have goals of care conversations which include making huge decisions, without saying goodbye. I couldn’t imagine.”
– Participant 39, Nurse
“… I feel that it is not fair that the patients do not have a loved one there holding their hand- it is me the bedside nurse that they have never met before sharing this intimate and important moment with them and I cannot even hold their hand without two pairs of gloves on.”
– Participant 41, Nurse
Theme 5:
The challenges around the use of technology. Both physicians and nurses voiced frustration with virtual communication, which was viewed as a distraction from direct patient care.
“…it takes an hour or more to reach each of the family members on the phone, and to fulfil additional family requests of video chat with the patients if patients are intubated/sedated or otherwise unable to communicate by themselves.”
– Participant 73, Physician (Resident)
“I spend an inordinate amount of time trying to get the system to work and get the family on the phone, which takes away from my patient care.”
– Participant 27, Nurse
“Using these platforms does not change the quality of care, however, it makes communicating with families more difficult.”
– Participant 72, Nurse
Theme 6:
Adjustments in team roles and responsibilities. Many HCWs noted a shift in the previous team dynamic shared by physicians and nurses. Nurses commented on increased communication bewteeen the physicians and families.
“The physicians that I have worked with in this pandemic have increased and really excelled in their efforts to call the families every day which is a huge difference from before because before if the family was not at the bedside sometimes they did not get updated. Honestly, by having the doctors update the family I have observed the families call a lot less to the nurses which is helpful since we have been so busy…”
– Participant 41, Nurse
Physicians in turn described a shift in not only how updates were provided, but which team members were responsible for providing the updates.
“My daily workflow often included going room to room updating families, getting to know them. Now it is done on the phone, primarily by the residents while we are in the [isolation] zone.”
Participant 74, Physician (Attending)
Theme 7:
A desire for family members to return. Many HCWs anticipated the return of family visitors after the pandemic. Some advocated for a return to the previous open visitation policy, whereas others voiced a preference for a new, adjusted policy.
“Relax some of the guidelines & let visitors come 3 times etc. if they wish.”
– Participant 36, Physician (Resident)
“I think the limited family members positively has impacted my care for patients. I think that post covid, establishing visitation hours would help both nursing staff, but also allow families to see their loves ones…”
– Participant 39, Nurse
Theme 8:
Internal tension. The concept of internal tension has previously been described in qualitative literature surrounding the experience of critical care nursing (Leung et al., 2017). This tension manifested as the simultaneous acknowledgement that while certain aspects of bedside care improved, other aspects pertaining to support and communication worsened.
“Providing care to critically ill patients without family members present has had it’s benefits along with some negatives. Family members are often not respectful of your space in already overcrowded rooms of pumps, ventilators, CRRT [continuous renal replacement therapy] and patient supplies. They … can often require more attention then the actual patient themselves. On the other hand, I think we have been struggling with not having the family present to see how hard we are working attending to their critically ill family members and how futile some interventions are. Face to face conversations with doctors and nurses go a long way, along with simple observance of the rooms and level of care being provided.”
-Participant 45, Nurse
Discussion
Previous research has shown that, when family members are present in the ICU, nurses are responsible for most of the family communication (Au et al., 2019). Studies have also shown that family presence in the ICU can negatively impact nurses’ workflow and environment due to perceived loss of control, interruptions in care, and increased workload (Berti et al., 2007; Monroe & Wofford, 2017). Therefore, it was not surprising that removing family members from the bedside improved nursing workflow. Additionally, nurses provide a great deal of emotional support to distressed families in the ICU, which can, in turn, lead to heightened nursing distress (Leung et al., 2019; Lief et al., 2018; Stayt, 2009). With the visitor restriction, nurses have had more time to focus on direct patient care without the added responsibility of providing information and support to family members at the bedside throughout the day. Interestingly, nurses reported no overall change in levels of job-related emotional distress, perhaps indicating that the positive changes to daily workflow were counterbalanced by other negative aspects of visitor restrictions such as challenges surrounding end-of-life care. Physicians in this study felt that visitor restrictions negatively impacted their workflow and increased their job-related emotional distress. Much of the emotional support and communication previously delivered by nurses are now being shifted to physicians by way of telephone updates, and our results indicate that this is both a time burden and an added source of stress.
Nurses had identified many barriers to effective family engagement in the ICU even before the onset of the COVID-19 pandemic (Hamilton et al., 2020; Hetland et al., 2018; Jakimowicz et al., 2017), and we feel that many of the issues identified in this study can help to mitigate these barriers. For example, HCWs described the addition of tablet computers as helping facilitate virtual family communication. Even after hospital visitor restrictions are relaxed, many family members will be unable to visit the ICU: it is increasingly common for family members to live in a different state than their loved one (Douglas et al., 2016), and prior studies have shown that over half of family caregivers are also actively employed or lack ready transportation (Carson et al., 2016; Cox et al., 2019). While in-person communication can and should return to being the primary mode of family engagement once visitors return, virtual communication will continue to be of benefit for caregivers who cannot be present but wish to remain engaged (Arabi et al., 2021). HCWs commented on the challenges of communicating with patients and families with Limited English Proficiency (LEP). Lack of access to professional interpreter services has been associated with worse patient health outcomes (Flores, 2006; Herzberg et al., 2021; Silva et al., 2016), and has also been shown to present unique challenges and stresses to nurses at the bedside (Choe et al., 2021; Coleman & Angosta, 2017). The rising demand for interpreters amidst the COVID-19 pandemic has prompted the development of innovative models to provide culturally competent and equitable care for patients with LEP, which has the potential to improve the experience of patients, families, and HCWs during the pandemic and beyond (Herzberg et al., 2021).
Our findings also revealed areas that need ongoing research and improvement. Many nurses and physicians commented on the effect of family absence, with families often positioned so that they are blocking the nurse’s paths to pumps or machines. Prior studies have demonstrated that modifying the arrangement of hospital rooms can improve nursing workflow (Lee et al., 2020), and re-organisation of ICU rooms could allow an optimal balance where HCWs and family members, both key components of the patient care team, can be present and maximise the benefit to the patient. Additionally, nurses indicated technological challenges with virtual communication. A dedicated facilitator to help schedule calls and coordinate virtual communication would reduce these frustrations both for HCWs and for patients and families. Even once families are able to return to the ICU, a coordinator to help schedule face-to-face family meetings between the healthcare team and family members would be beneficial; the current practice at our centre is for a physician member of the team, often a resident or fellow, to schedule these meetings. However, given the busy nature of patient care in the ICU, this system can make it challenging to set a meeting under circumstances that are optimal for both the family and HCWs (especially if multiple subspecialty teams are involved). One nurse-driven communication and support intervention resulted in a decreased ICU length of stay, which would likely offset the associated costs of added personnel (White et al., 2018).
Finally, families derive great benefit from the support offered by nurses at the bedside. In prior investigations, family members of patients in the ICU have reported that nurses helped convey information about the patient’s prognosis to the family (Kisorio & Langley, 2016; Wong et al., 2015), and to provide them with the confidence and support they need to make difficult treatment decisions (Adams et al., 2014). However, these tasks are time-consuming, and as demonstrated in our results can also impede more urgent and direct patient care tasks. Implementation of dedicated facilitators for family communication and support could potentially reduce this burden on the bedside nurses while still providing families with the information and support that they need. Patient and family outcomes associated with this type of program have previously been studied (Curtis et al., 2016; White et al., 2018), but less is known about the impact on HCWs and specifically nurses. While re-organisation of ICU rooms and addition of dedicated personnel would impose increased costs on hospital systems, these are exactly the types of changes that experts have recommended be made in response to lessons imposed by the COVID-19 pandemic in order to improve the experiences for HCWs, patients, and their families in the future (Arabi et al., 2021).
Limitations
Our study has several limitations. It is possible that our results were impacted by non-response by those who did not feel impacted by the changes so that responses captured here are more extreme or somehow not fully representative of our study population (Cheung et al., 2017). Because a validated instrument to address our research question does not exist, the survey used here was developed by the study team and has not been validated formally. Our survey development working group including only physicians and did not include nurses or other HCWs, and so additional relevant topics may not have been considered. Participants were asked to estimate their communication times before the pandemic but not during the pandemic. We did not include APPs in our final analysis due to the very small sample size, although in doing so we may have missed valuable information. Finally, the study was performed in a MICU at a single centre in the US, and our findings may not be generalisable outside of this setting.
Conclusion
Restricted family visitation during the COVID-19 pandemic has resulted in both positive and negative changes to the workplace experience for HCWs in the ICU. While some differences exist based on profession, both groups expressed concern for an overall negative impact of visitor restriction on HCWs, patients, and families. However, our findings also highlighted numerous areas for improvement that have the potential to benefit HCWs, patients, and families during the pandemic and after visitor restrictions are lifted.
Implications for Clinical Practice.
Nurses reported positive changes to daily workflow and ability to provide medical care in the absence of family visitors, driven by increased time and physical space to provide direct patient care.
Physicians reported negative changes to daily workflow and ability to provide medical care in the absence of family visitors, driven by disruptions in family communication.
Both physicians and nurses noted an increase in family emotional distress and a decrease in family comprehension during telephone updates, and a negative impact on ability to provide end-of-life care.
Nurses and physicians in a medical intensive care unit reported divergent perspectives on some aspects of family visitor restriction, but both groups expressed concern for an overall negative impact of visitor restriction on healthcare workers, patients, and their families.
Funding Sources:
This project was supported by institutional training grant 2Y32HL007106-41 and KL2TR002490.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams JA, Anderson RA, Docherty SL, Tulsky JA, Steinhauser KE, & Bailey DE Jr. (2014). Nursing strategies to support family members of ICU patients at high risk of dying. Heart Lung, 43(5), 406–415. 10.1016/j.hrtlng.2014.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman DG, & Bland JM (1996). Statistics Notes: Comparing several groups using analysis of variance. BMJ, 312(7044), 1472–1473. 10.1136/bmj.312.7044.1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrist E, Clarke RG, & Harding M (2020). Paved With Good Intentions: Hospital Visitation Restrictions in the Age of Coronavirus Disease 2019. Pediatr Crit Care Med. 10.1097/pcc.0000000000002506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arabi YM, Azoulay E, Al-Dorzi HM, Phua J, Salluh J, Binnie A, Hodgson C, Angus DC, Cecconi M, Du B, Fowler R, Gomersall CD, Horby P, Juffermans NP, Kesecioglu J, Kleinpell RM, Machado FR, Martin GS, Meyfroidt G, Rhodes A, Rowan K, Timsit J-F, Vincent J-L, & Citerio G (2021). How the COVID-19 pandemic will change the future of critical care. Intensive Care Medicine, 47(3), 282–291. 10.1007/s00134-021-06352-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au SS, Ordons A. L. R. d., Ali AA, Soo A, & Stelfox HT (2019). Communication with patients’ families in the intensive care unit: A point prevalence study. Journal of Critical Care 10.1016/j.jcrc.2019.08.031 [DOI] [PubMed] [Google Scholar]
- Berti D, Ferdinande P, & Moons P (2007). Beliefs and attitudes of intensive care nurses toward visits and open visiting policy. Intensive Care Medicine, 33(6), 1060–1065. 10.1007/s00134-007-0599-x [DOI] [PubMed] [Google Scholar]
- Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff T, & Cook DJ (2008). A guide for the design and conduct of self-administered surveys of clinicians. Cmaj, 179(3), 245–252. 10.1503/cmaj.080372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson SS, Cox CE, Wallenstein S, Hanson LC, Danis M, Tulsky JA, Chai E, & Nelson JE (2016). Effect of Palliative Care-Led Meetings for Families of Patients With Chronic Critical Illness: A Randomized Clinical Trial. Jama, 316(1), 51–62. 10.1001/jama.2016.8474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DK, Collingridge DS, Mitchell LA, Wright ES, Hopkins RO, Butler JM, & Brown SM (2016). Satisfaction With Elimination of all Visitation Restrictions in a Mixed-Profile Intensive Care Unit. American Journal of Critical Care, 25(1), 46–50. 10.4037/ajcc2016789 [DOI] [PubMed] [Google Scholar]
- Cheung KL, ten Klooster PM, Smit C, de Vries H, & Pieterse ME (2017). The impact of non-response bias due to sampling in public health studies: A comparison of voluntary versus mandatory recruitment in a Dutch national survey on adolescent health. BMC Public Health, 17(1), 276. 10.1186/s12889-017-4189-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe AY, Thomson JE, Unaka NI, Wagner V, Durling M, Moeller D, Ampomah E, Mangeot C, & Schondelmeyer AC (2021). Disparity in Nurse Discharge Communication for Hospitalized Families Based on English Proficiency. Hosp Pediatr, 11(3), 245–253. 10.1542/hpeds.2020-000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JS, & Angosta AD (2017). The lived experiences of acute-care bedside registered nurses caring for patients and their families with limited English proficiency: A silent shift. J Clin Nurs, 26(5–6), 678–689. 10.1111/jocn.13567 [DOI] [PubMed] [Google Scholar]
- Cooper RA, Henderson T, & Dietrich CL (1998). Roles of nonphysician clinicians as autonomous providers of patient care. Jama, 280(9), 795–802. 10.1001/jama.280.9.795 [DOI] [PubMed] [Google Scholar]
- Cox CE, White DB, Hough CL, Jones DM, Kahn JM, Olsen MK, Lewis CL, Hanson LC, & Carson SS (2019). Effects of a Personalized Web-Based Decision Aid for Surrogate Decision Makers of Patients With Prolonged Mechanical Ventilation: A Randomized Clinical Trial. Ann Intern Med 10.7326/m18-2335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis JR, Treece PD, Nielsen EL, Gold J, Ciechanowski PS, Shannon SE, Khandelwal N, Young JP, & Engelberg RA (2016). Randomized Trial of Communication Facilitators to Reduce Family Distress and Intensity of End-of-Life Care. Am J Respir Crit Care Med, 193(2), 154–162. 10.1164/rccm.201505-0900OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, Cox CE, Wunsch H, Wickline MA, Nunnally ME, Netzer G, Kentish-Barnes N, Sprung CL, Hartog CS, Coombs M, Gerritsen RT, Hopkins RO, Franck LS, Skrobik Y, Kon AA, Scruth EA, Harvey MA, Lewis-Newby M, White DB, Swoboda SM, Cooke CR, Levy MM, Azoulay E, & Curtis JR (2017). Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med, 45(1), 103–128. 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- Douglas SL, Mazanec P, Lipson A, & Leuchtag M (2016). Distance caregiving a family member with cancer: A review of the literature on distance caregiving and recommendations for future research. World journal of clinical oncology, 7(2), 214–219. 10.5306/wjco.v7.i2.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G (2006). Language Barriers to Health Care in the United States. New England Journal of Medicine, 355(3), 229–231. 10.1056/NEJMp058316 [DOI] [PubMed] [Google Scholar]
- Fumagalli S, Boncinelli L, Lo Nostro A, Valoti P, Baldereschi G, Di Bari M, Ungar A, Baldasseroni S, Geppetti P, Masotti G, Pini R, & Marchionni N (2006). Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit: results from a pilot, randomized trial. Circulation, 113(7), 946–952. 10.1161/circulationaha.105.572537 [DOI] [PubMed] [Google Scholar]
- Gerritsen RT, Hartog CS, & Curtis JR (2017). New developments in the provision of family-centered care in the intensive care unit. Intensive Care Med, 43(4), 550–553. 10.1007/s00134-017-4684-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton R, Kleinpell R, Lipman J, & Davidson JE (2020). International facilitators and barriers to family engagement in the ICU: Results of a qualitative analysis. Journal of Critical Care 10.1016/j.jcrc.2020.04.011 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickson SL (1987). Intracranial pressure changes and family presence. J Neurosci Nurs, 19(1), 14–17. 10.1097/01376517-198702000-00003 [DOI] [PubMed] [Google Scholar]
- Herzberg EM, Barrero-Castillero A, & Matute JD (2021). The healing power of language: caring for patients with limited english proficiency and COVID-19. Pediatr Res, 1–3. 10.1038/s41390-021-01487-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetland B, McAndrew N, Perazzo J, & Hickman R (2018). A qualitative study of factors that influence active family involvement with patient care in the ICU: Survey of critical care nurses. Intensive Crit Care Nurs, 44, 67–75. 10.1016/j.iccn.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qual Health Res, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jakimowicz S, Perry L, & Lewis J (2017). An integrative review of supports, facilitators and barriers to patient-centred nursing in the intensive care unit. J Clin Nurs, 26(23–24), 4153–4171. 10.1111/jocn.13957 [DOI] [PubMed] [Google Scholar]
- Kelly M, Lyng C, McGrath M, & Cannon G (2009). A multi-method study to determine the effectiveness of, and student attitudes to, online instructional videos for teaching clinical nursing skills. Nurse Educ Today, 29(3), 292–300. 10.1016/j.nedt.2008.09.004 [DOI] [PubMed] [Google Scholar]
- Kisorio LC, & Langley GC (2016). End-of-life care in intensive care unit: Family experiences. Intensive and Critical Care Nursing, 35, 57–65. 10.1016/j.iccn.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Lee J, Lee H, & McCuskey Shepley M (2020). Exploring the spatial arrangement of patient rooms for minimum nurse travel in hospital nursing units in Korea. Frontiers of Architectural Research, 9(4), 711–725. 10.1016/j.foar.2020.06.003 [DOI] [Google Scholar]
- Leung D, Blastorah M, Nusdorfer L, Jeffs A, Jung J, Howell D, Fillion L, & Rose L (2017). Nursing patients with chronic critical illness and their families: a qualitative study. Nurs Crit Care, 22(4), 229–237. 10.1111/nicc.12154 [DOI] [PubMed] [Google Scholar]
- Leung YW, Maslej MM, Ho C, Razavi S, Uy P, Hosseini MA, Avery J, Rodin G, & Peterkin A (2019). Cocreating Meaning Through Expressive Writing and Reading for Cancer Caregivers. J Palliat Care, 825859719871538. 10.1177/0825859719871538 [DOI] [PubMed] [Google Scholar]
- Lief L, Berlin DA, Maciejewski RC, Westman L, Su A, Cooper ZR, Ouyang DJ, Epping G, Derry H, Russell D, Gentzler E, Maciejewski PK, & Prigerson HG (2018). Dying Patient and Family Contributions to Nurse Distress in the ICU. Ann Am Thorac Soc 10.1513/AnnalsATS.201804-284OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe M, & Wofford L (2017). Open visitation and nurse job satisfaction: An integrative review. J Clin Nurs, 26(23–24), 4868–4876. 10.1111/jocn.13919 [DOI] [PubMed] [Google Scholar]
- Morley G, Sese D, Rajendram P, & Horsburgh CC (2020). Addressing caregiver moral distress during the COVID-19 pandemic. Cleve Clin J Med 10.3949/ccjm.87a.ccc047 [DOI] [PubMed] [Google Scholar]
- Netzer G, & Iwashyna TJ (2017). Fair Is Fair: Just Visiting Hours and Reducing Inequities. Ann Am Thorac Soc, 14(12), 1744–1746. 10.1513/AnnalsATS.201706-471OI [DOI] [PubMed] [Google Scholar]
- Rogers S (2004). Why can’t I visit? The ethics of visitation restrictions - lessons learned from SARS. Critical care (London, England), 8(5), 300–302. 10.1186/cc2930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa RG, Falavigna M, da Silva DB, Sganzerla D, Santos MMS, Kochhann R, de Moura RM, Eugênio CS, Haack T. d. S. R., Barbosa MG, Robinson CC, Schneider D, de Oliveira DM, Jeffman RW, Cavalcanti AB, Machado FR, Azevedo LCP, Salluh JIF, Pellegrini JAS, Moraes RB, Foernges RB, Torelly AP, Ayres L. d. O., Duarte PAD, Lovato WJ, Sampaio PHS, de Oliveira Júnior LC, Paranhos J. L. d. R., Dantas A. d. S., de Brito PIPGG, Paulo EAP, Gallindo MAC, Pilau J, Valentim HM, Meira Teles JM, Nobre V, Birriel DC, Corrêa eCastro L, Specht AM, Medeiros GS, Tonietto TF, Mesquita EC, da Silva NB, Korte JE, Hammes LS, Giannini A, Bozza FA, Teixeira C, Investigators, f. t. I. V. S. G., & Network, t. B. R. i. I. C. (2019). Effect of Flexible Family Visitation on Delirium Among Patients in the Intensive Care Unit: The ICU Visits Randomized Clinical TrialEffect of Flexible Family Visitation on Delirium Among Patients in the Intensive Care UnitEffect of Flexible Family Visitation on Delirium Among Patients in the Intensive Care Unit. Jama, 322(3), 216–228. 10.1001/jama.2019.8766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgwick P (2012). Non-parametric statistical tests for independent groups: numerical data. BMJ : British Medical Journal, 344, e3354. 10.1136/bmj.e3354 [DOI] [Google Scholar]
- Silva MD, Genoff M, Zaballa A, Jewell S, Stabler S, Gany FM, & Diamond LC (2016). Interpreting at the End of Life: A Systematic Review of the Impact of Interpreters on the Delivery of Palliative Care Services to Cancer Patients With Limited English Proficiency. J Pain Symptom Manage, 51(3), 569–580. 10.1016/j.jpainsymman.2015.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stayt LC (2009). Death, empathy and self preservation: the emotional labour of caring for families of the critically ill in adult intensive care. J Clin Nurs, 18(9), 1267–1275. 10.1111/j.1365-2702.2008.02712.x [DOI] [PubMed] [Google Scholar]
- Valley TS, Schutz A, Nagle MT, Miles LJ, Lipman K, Ketcham SW, Kent M, Hibbard CE, Harlan EA, & Hauschildt K (2020). Changes to Visitation Policies and Communication Practices in Michigan Intensive Care Units During the COVID-19 Pandemic. American Journal of Respiratory and Critical Care Medicine. 10.1164/rccm.202005-1706LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler S (1997). Statistics at Square One. Ninth Edition, revised by M. J. Campbell, T. D. V. Swinscow, BMJ Publ. Group, London, 1996. No. of pages: 140. Price: £11. ISBN 0–7279-0916–9. Statistics in Medicine, 16(22), 2629–2630. [DOI] [Google Scholar]
- White DB, Angus DC, Shields A-M, Buddadhumaruk P, Pidro C, Paner C, Chaitin E, Chang C-CH, Pike F, Weissfeld L, Kahn JM, Darby JM, Kowinsky A, Martin S, & Arnold RM (2018). A Randomized Trial of a Family-Support Intervention in Intensive Care Units. New England Journal of Medicine, 378(25), 2365–2375. 10.1056/NEJMoa1802637 [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A, & Low JG (2005). Risk of respiratory infections in health care workers: lessons on infection control emerge from the SARS outbreak. Southeast Asian J Trop Med Public Health, 36(2), 481–488. [PubMed] [Google Scholar]
- Wong P, Liamputtong P, Koch S, & Rawson H (2015). Families’ experiences of their interactions with staff in an Australian intensive care unit (ICU): a qualitative study. Intensive Crit Care Nurs, 31(1), 51–63. 10.1016/j.iccn.2014.06.005 [DOI] [PubMed] [Google Scholar]


