Abstract
Background:
The COVID-19 pandemic caused disruptions in treatment for cancer. Less is known about its impact on new cancer diagnoses, where delays could cause worsening long-term outcomes. We quantified decreases in encounters related to prostate, lung, bladder and colorectal cancers, procedures that facilitate their diagnosis, and new diagnoses of those cancers in the COVID era compared to pre-COVID era.
Methods:
All encounters at Veterans’ Affairs (VA) facilities nationwide from 2016 through 2020 were reviewed. We quantified trends in new diagnoses of cancer, and in procedures facilitating their diagnosis, from January 1, 2018 onward. Using 2018–2019 as baseline, we estimated reductions in procedures and new cancer diagnoses in 2020. We calculated absolute and percentage differences in annual volume and observed to expected ratios of volume. We generated heat maps and funnel plots of volume changes.
Results:
From 2018 through 2020, there were 4.1 million cancer-related encounters, 3.9 million relevant procedures, and 251,647 new cancers diagnosed. Compared to the annual averages in 2018–2019, colonoscopies in 2020 decreased by 45% while prostate biopsies, chest CT scans, and cystoscopies decreased by 29%, 10%, and 21%, respectively. New cancer diagnoses decreased by 13% to 23%. These drops varied by state and continued to accumulate despite reductions in pandemic-related restrictions.
Conclusion:
We identified substantial reductions in procedures used to diagnose cancer and subsequent reductions in new diagnoses of cancer across the US due to the COVID-19 pandemic. A nomogram is provided to identify and resolve these unmet healthcare needs and avoid worse long-term cancer outcomes.
Keywords: COVID-19, Cancer Diagnosis, Cancer Screening, Prostate Cancer, Lung Cancer, Bladder Cancer, Colorectal Cancer
Precis:
The disruptions due to the COVID-19 pandemic have led to substantial reductions in procedures that could diagnose new cancers and subsequent reductions in new diagnoses of cancer in medical facilities across the US. To avoid the potential for worse long-term cancer outcomes due to delayed diagnoses, health systems must quantify their deficits and find ways to clear the backlog of undiagnosed cases.
Lay Summary:
The disruptions due to the COVID-19 pandemic have led to substantial reductions in new cancers being diagnosed. We quantify those reductions in a national healthcare system and offer a method for understanding the backlog of cases and the resources needed to resolve them.
Introduction
To slow COVID-19 transmission, safeguard patients, and preserve healthcare resources, a nationwide moratorium on elective clinical activities was instituted in March 2020.1, 2 The restrictions had immediate and anticipated impacts on treatment of patients with known cancer.3, 4 However, restrictions also included clinical procedures such as colonoscopies, prostate biopsies, computed tomography (CT) and cystoscopies that offer an opportunity to detect suspected or unexpected cancer. The moratorium-related decrease in access to care may have delayed identification of new cancers, leading to worse long-term outcomes.5–9 Current research examining this impact on screening and diagnosis of cancer has demonstrated significant decreases but has been limited to the early pandemic, without providing follow-up on how these encounters rebounded once restrictions were lifted.3, 10–13
Despite a gradual lifting of restrictions starting May 2020, recurrent COVID-19 outbreaks, new variants, regional variations in COVID transmission rates, institutional caution, and patient fears about COVID-19 exposure can be anticipated to keep healthcare visits and procedures well below 2019 levels across the US.3, 14 The accumulated backlog of procedures and resultant undiagnosed cancers due to the pandemic have not been determined at a national or regional level. There are few nationwide databases that provide near real-time, state-by-state data that can be used to assess this backlog. Without these data, an informed plan to allocate resources for recovery cannot be formulated.
We reviewed nationwide data from the Veterans Health Administration (VA), the largest healthcare system in the US, for the four most common cancers in that population: (1) prostate, (2) lung, (3) bladder, and (4) colorectal.15 The VA health system provides a large population that spans the entire US and includes broad racial, ethnic, and geographic diversity -an important cross-section of US healthcare. Given the standardized approach to care at VA facilities, changes in cancer management patterns are more reliably attributable to external pressures. Our analysis has four aims: (1) quantify the temporal trends in cancer-related clinical encounters, procedures that may facilitate the diagnosis of new cancers, and new cancers diagnosed in 2020 compared to baseline years (2018–2019), (2) estimate the accumulated backlog of unperformed procedures and undiagnosed cancers accrued in 2020, (3) identify geographic variation in deficits across the US, and (4) develop a tool to calculate additional capacity and time required to recover from these deficits.
Methods
Data Source
This time-series study examines data from Computerized Patient Record System (CPRS), the VA’s electronic medical record. The information is stored in the Department of Veterans Affairs Informatics and Computing Infrastructure (VINCI), one of the only nationwide, real-time, patient-level datasets. Data from >9 million veterans at 1,244 VA medical facilities offers a unique opportunity to examine the temporal and geographic variation in cancer care across the US, providing administrative, demographic, and clinical information on all inpatient and outpatient visits. The Institutional Review Board of the University of Maryland School of Medicine and Baltimore VA Medical Center Research and Development Committee approved this study.
Study population
All patients with a clinical encounter in a US-based VA facility from January 1, 2018 through December 31, 2020 were evaluated. We included all patients with an encounter for our cancers of interest, a procedure that might identify one of these cancers, or a new diagnosis of our cancers of interest. Encounters were searched for International Classification of Diseases-10 (ICD-10, see Supplemental Table 1) or Current Procedural Terminology (CPT, see Supplemental Table 2) codes related to the four most common cancers in the VA population (prostate, lung, bladder, and colorectal), or CPT codes for diagnostic and screening procedures related to the identification of these cancers: prostate biopsies, chest computed tomography (CT) scans (classified as screening or diagnostic), cystoscopies, colonoscopies, sigmoidoscopies, and fecal occult blood tests (FOBTs).3, 10 Patients were considered to have a new cancer diagnosis if they had no encounter with a diagnosis code for the same cancer over a period of 2 years prior to the new diagnosis. To ensure this, we reviewed all encounters from January 1, 2016 to December 31, 2017. Patients were included regardless of age, gender, race, or geographic location, and we did not exclude patients based on death or disenrollment.
Outcomes
Outcomes of interest included (1) cancer-related healthcare encounters, (2) cancer-related diagnostic or screening procedures and (3) new cancer diagnoses. Cancer-related encounters were defined as any healthcare encounter (inpatient or outpatient) with an associated ICD-10 diagnosis code for our four cancers of interest. Cancer-related diagnostic and screening procedures included prostate biopsies, chest CT scans (screening and diagnostic), cystoscopies, colonoscopies, sigmoidoscopies, and FOBTs.
Statistical analyses
Outcome measures were grouped by the month and year of the patient encounter. Using pre-COVID baseline data from January 1, 2018 to December 31, 2019, a monthly baseline, accounting for seasonal variation, was calculated. We then calculated monthly encounters from January 1, 2020 to December 31, 2020 as a percentage of baseline and as a raw deficit. In addition to monthly deficits, the annual deficit for 2020 for each outcome was calculated as a raw number and as a percentage of the baseline annual volume. Annual deficits were calculated for each state to examine geographic variation.
A heat map of the US for each diagnostic and screening procedure was generated to examine geographic variation by state. Observed to expected (O/E) ratios were calculated for the annual number performed for each diagnostic and screening procedure in each state, with the observed being the number of procedures performed in 2020 and the expected being the average annual number of procedures from 2018–2019. Funnel plots compared O/E ratios in each state by expected procedure numbers.
To compute the duration and magnitude of the increase in relevant procedures required to recover from the current backlog, we created a nomogram that can be used to compute (1) the number of months needed to clear the backlog, given the current backlog (expressed as percentage of baseline monthly procedures) and state (or institutional) capacity to increase monthly procedures (expressed as a percentage), (2) the monthly capacity above baseline needed to clear the backlog, given the current backlog and the number of months over which a state (or institution) wants to clear the backlog. Statistical analyses were generated with R (v. 4.0.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
From January 1, 2018 to December 31, 2020, there were 4.1 million cancer-related encounters, 3.9 million relevant diagnostic and screening procedures, and 251,647 patients with new diagnoses for cancer in the VA. New cancer diagnoses included prostate (n=139,960 patients), lung (n=51,224), colorectal (n=27,697), and bladder (n=32,766). Patients undergoing our diagnostic or screening procedures for the four cancers of interest had a median age of 67 years and were predominantly male (92%), with 22% Black and 6.1% Latino patients. Compared to patients undergoing these procedures in 2018–2019, 2020 patients had similar ages, although fewer in the 60–69 year-old range (29% vs. 36%; p<0.001; Table 1). Although statistically significant, the differences in demographic characteristics were not clinically important.
Table 1.
Demographic characteristics of patients undergoing screening or diagnostic procedures for cancer in 2018–2020.
| Year of Procedure | |||
|---|---|---|---|
| N | 1,618,014 (80.1%) | 400,729 (19.9%) | |
| Age, years, median (IQR) | 67 (59, 72) | 66 (56, 72) | < 0.001 |
| Age (category) | < 0.001 | ||
| <40 | 49,727 (3.1%) | 19,289 (4.8%) | |
| 40–49 | 66,806 (4.1%) | 23,398 (5.8%) | |
| 50–59 | 320,447 (19.8%) | 87,451 (21.8%) | |
| 60–69 | 578,090 (35.7%) | 117,444 (29.3%) | |
| ≥70 | 602,944 (37.3%) | 153,147 (38.2%) | |
| Sex | < 0.001 | ||
| Female | 120,946 (7.5%) | 36,399 (9.1%) | |
| Male | 1,497,068 (92.5%) | 364,330 (90.9%) | |
| Race | < 0.001 | ||
| White | 1,160,450 (77.1%) | 276,782 (74.6%) | |
| Black | 323,822 (21.5%) | 84,555 (22.8%) | |
| Other | 20,312 (1.4%) | 9,905 (2.7%) | |
| Ethnicity -Latino | 93,555 (6%) | 25,037 (6.5%) | < 0.001 |
| Location | < 0.001 | ||
| Inpatient | 10,510 (0.6%) | 3,346 (0.8%) | |
| Outpatient | 1,607,504 (99.4%) | 397,383 (99.2%) | |
| Procedure | < 0.001 | ||
| Prostate biopsy | 31,242 (1.9%) | 8,670 (2.2%) | |
| Chest CT scan | 579,748 (35.8%) | 138,139 (34.5%) | |
| Cystoscopy | 83,437 (5.2%) | 22,058 (5.5%) | |
| Colonoscopy | 923,587 (57.1%) | 231,862 (57.9%) | |
Numbers represent frequency (%) unless otherwise specified. Other race represents Asian, American Indian, Pacific Islander, or Unknown. IQR-interquartile range, CT-computed tomography.
Cancer-related encounters dropped precipitously during April and May of 2020 compared to the same months in 2018 and 2019, with encounters for prostate cancer falling from an average of 63,496 in April 2018–2019 to 46,938 in April 2020 (26% decrease, Figure 1A). Encounters rebounded to near baseline levels by the summer. In April 2020, encounters for cancers of the lung, bladder and colorectum decreased by 10%, 27%, and 19% from baseline, respectively. In addition, prostate biopsies, chest CT scans, cystoscopies, colonoscopies, and FOBT decreased by 80%, 64%, 74%, 93%, and 54% respectively, from baseline volumes in April 2018 and 2019 (Figure 1B). Unlike cancer-related encounters, which rebounded after a few months, the procedures continued to remain below baseline throughout 2020. Colonoscopy had the largest decrease, resulting in an estimated deficit of 24,871 unperformed procedures in April and 5,840 in December (Figure 1C). The decrease in procedures during 2020 without a rebound sufficient to make up for the deficits during the moratorium resulted in an estimated total annual deficit of 133,231 colonoscopies (45% of annual baseline colonoscopy volume), 7,838 prostate biopsies (29%), 62,793 chest CT scans (12%), 20,680 cystoscopies (21%), and 49,334 FOBTs (13%, Figure 1D). Screening chest CT scans had a similar initial deficit but rebounded so no annual deficit existed for 2020.
Figure 1.
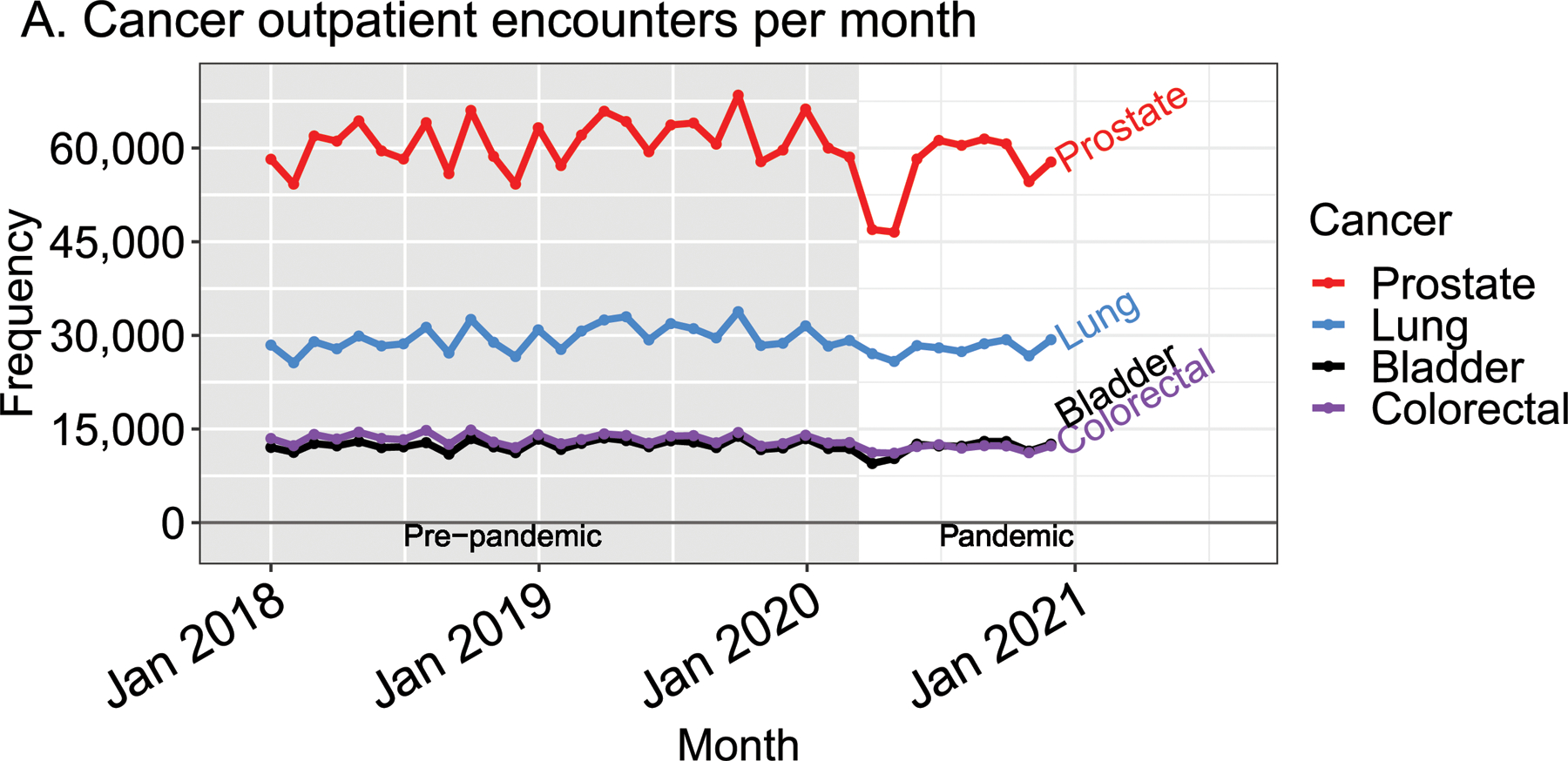



Temporal trends in (A) cancer encounters and (B) diagnostic and screening procedures in the VA health system from 2018 to 2020. The estimated (C) monthly and (D) cumulative deficit in procedures based on 2018–2019, seasonally adjusted baseline is presented. The grey, shaded region indicates the pre-pandemic era, defined as prior to March 11, 2020. CT -computed tomography; FOBT -fecal occult blood test.
The annual procedural deficits generated during 2020 varied by state, though no consistent patterns were detected by geographic region (Figure 2) or state size (Figure 3). Two-thirds of states had deficits >25% of their annual baseline prostate biopsy volume. For chest CT scans, 44% of states had minimal deficits (<10%) and 10% had >25% deficits. For cystoscopies, 36% of states had deficits of >25%. Colonoscopies had the largest deficits; 29% of states had >50% deficits and only one state (Connecticut) had a <20% decrease. The funnel plots demonstrated that decreased procedure performance occurred in both large and small states.
Figure 2.
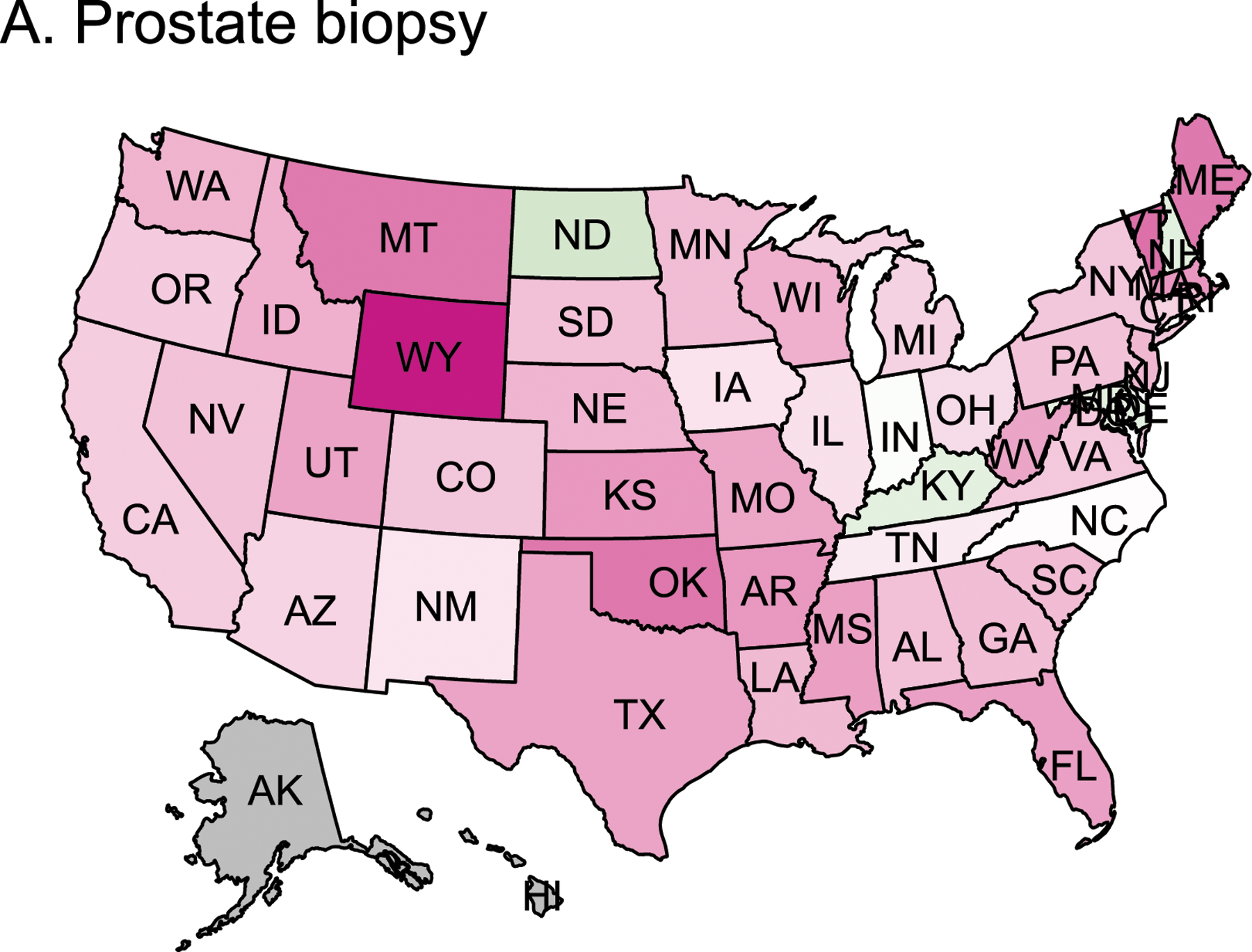
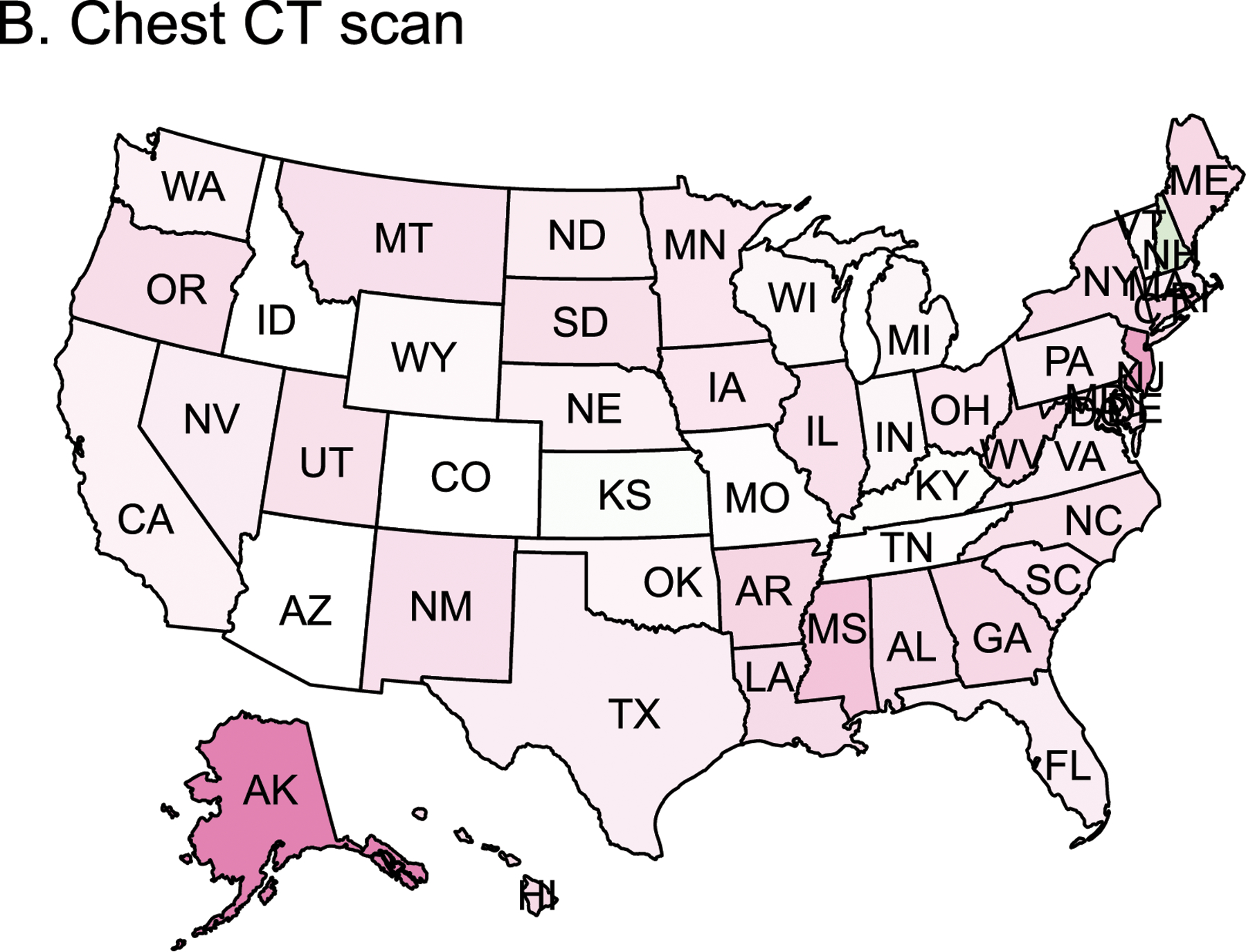

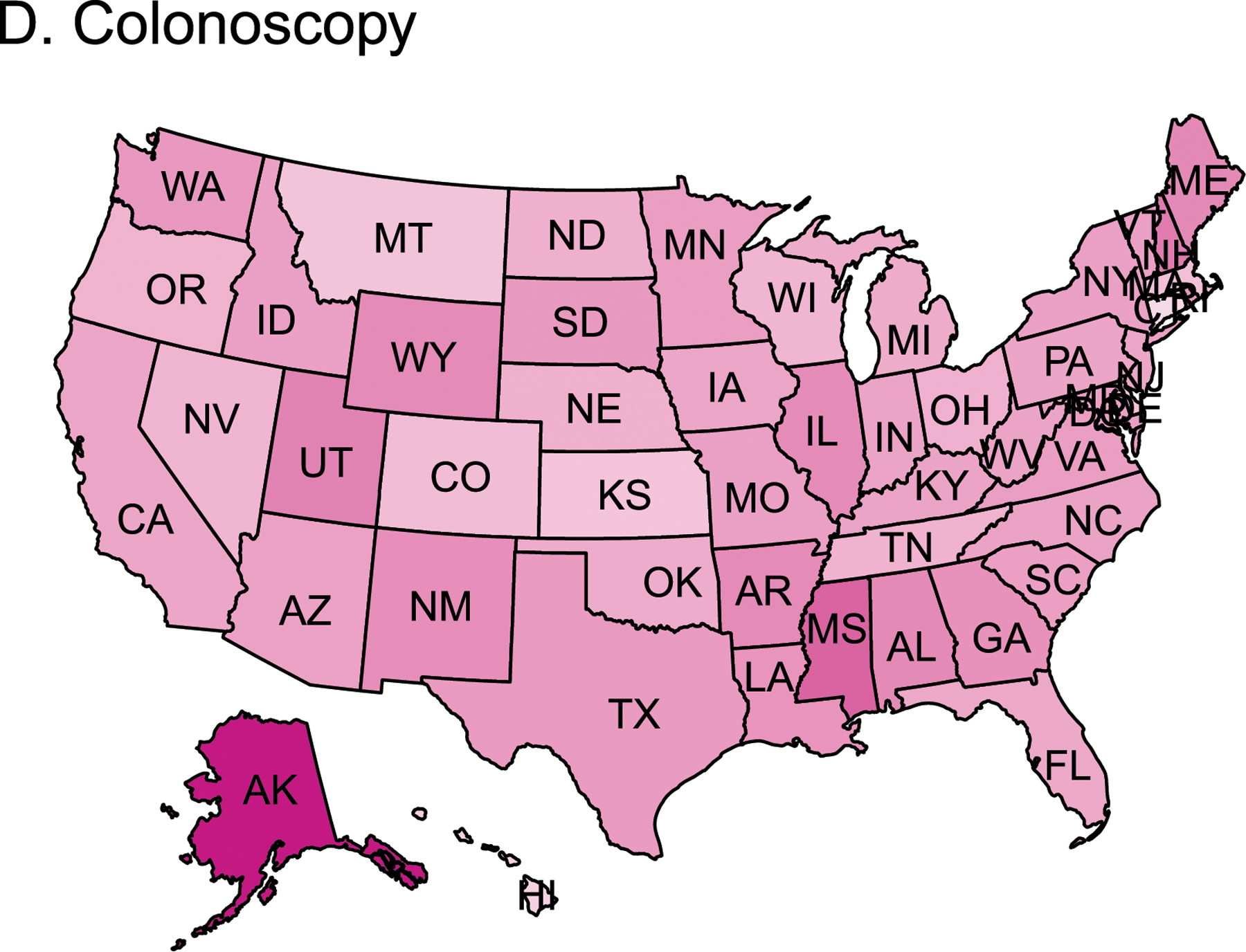

Heatmap of the change in the number of diagnostic and screening procedures performed for cancer in 2020 compared to 2018–2019 baseline in each state for (A) prostate biopsy, (B) chest CT scan, (C) cystoscopy, and (D) colonoscopy. Green states represent a relative increase in procedures performed in 2020, and pink indicates a relative decrease in procedures performed. Grey indicates no data for that state. CT -computed tomography (includes both screening and diagnostic).
Figure 3.




Funnel plot of observed to expected number of diagnostic and screening procedures performed for cancer in 2020 by expected number of procedures (based on 2018–2019 data) per state for (A) prostate biopsy, (B) chest CT scan, (C) cystoscopy, and (D) colonoscopy. CT -computed tomography (includes both screening and diagnostic).
New diagnoses of cancer showed a similar temporal trend to that seen for diagnostic and screening procedures, with a dramatic decrease from March-June 2020 (Figure 4A). When examined as percentage of diagnoses normalized by 2018–2019 baseline data, the pattern of decreased diagnoses is consistent across prostate, lung, bladder, and colorectal cancers (Figure 4B). Prostate cancer diagnoses fell >50% by May 2020, resulting in 2,304 fewer cancers diagnosed in May alone (Figure 4C). Similar proportional decreases were seen in new diagnoses of colorectal, lung, and bladder cancer. Although new diagnoses of cancer began to increase in June 2020, they did not reach their pre-pandemic baseline, and no rebound above baseline was seen. As a result, the deficit of new cancer diagnoses continued to accumulate throughout 2020 (Figure 4D). An estimated 11,362 fewer prostate cancers (23% of annual baseline), 2,365 fewer lung cancers (13%), 2,130 fewer bladder cancers (18%), and 1,979 fewer colorectal cancers (20%) were diagnosed in 2020 compared to baseline years 2018–2019.
Figure 4.
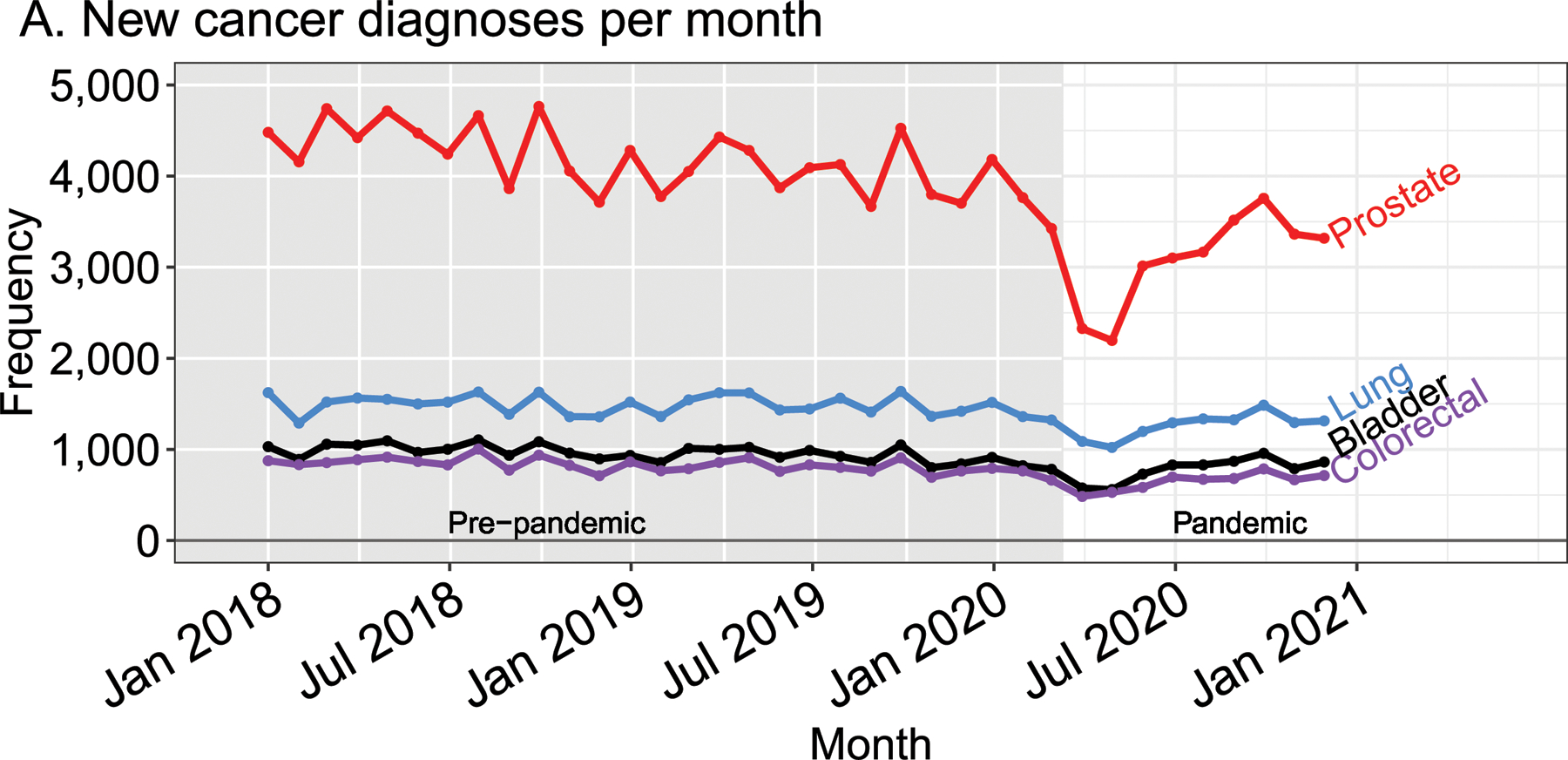
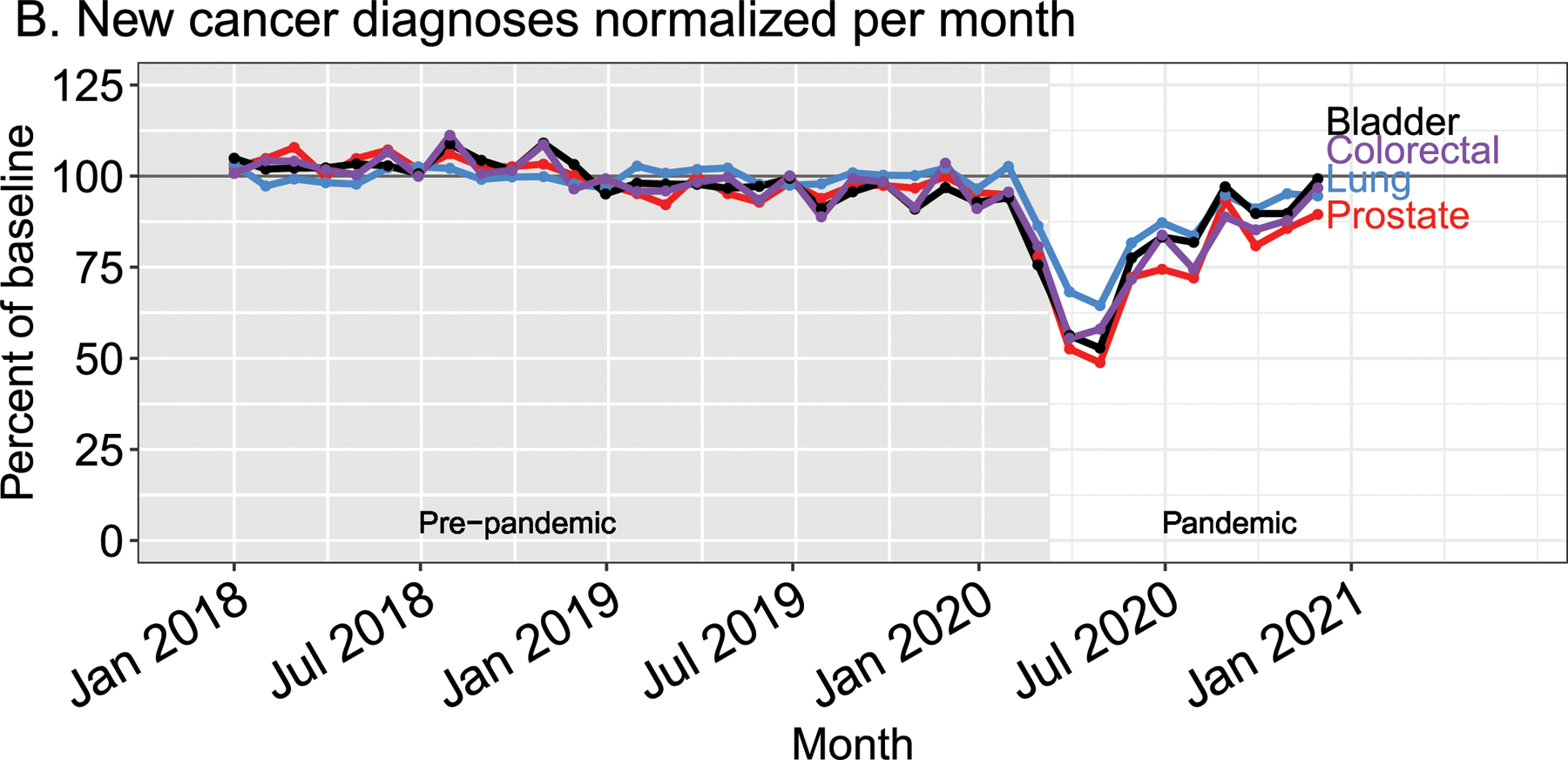
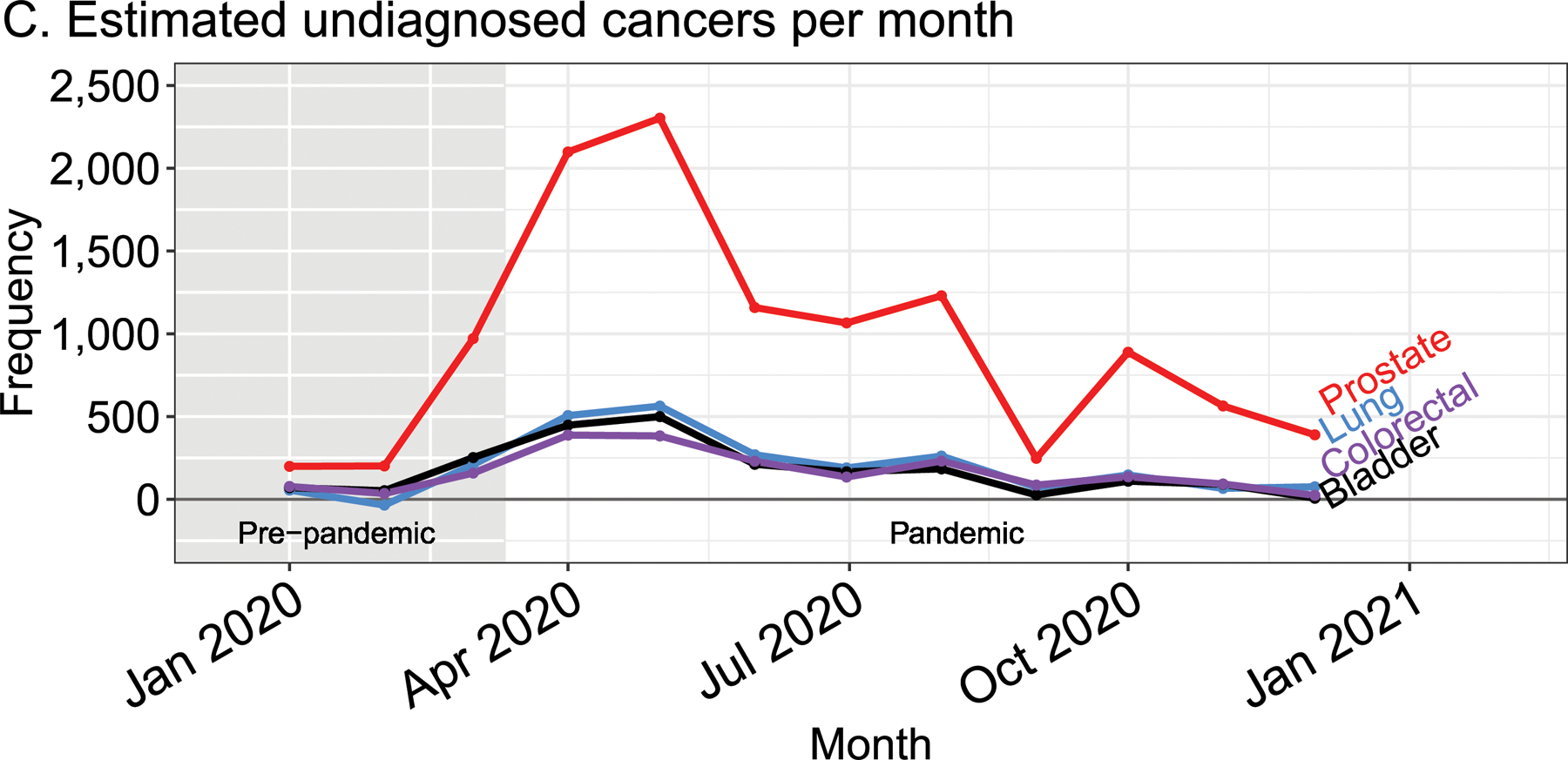
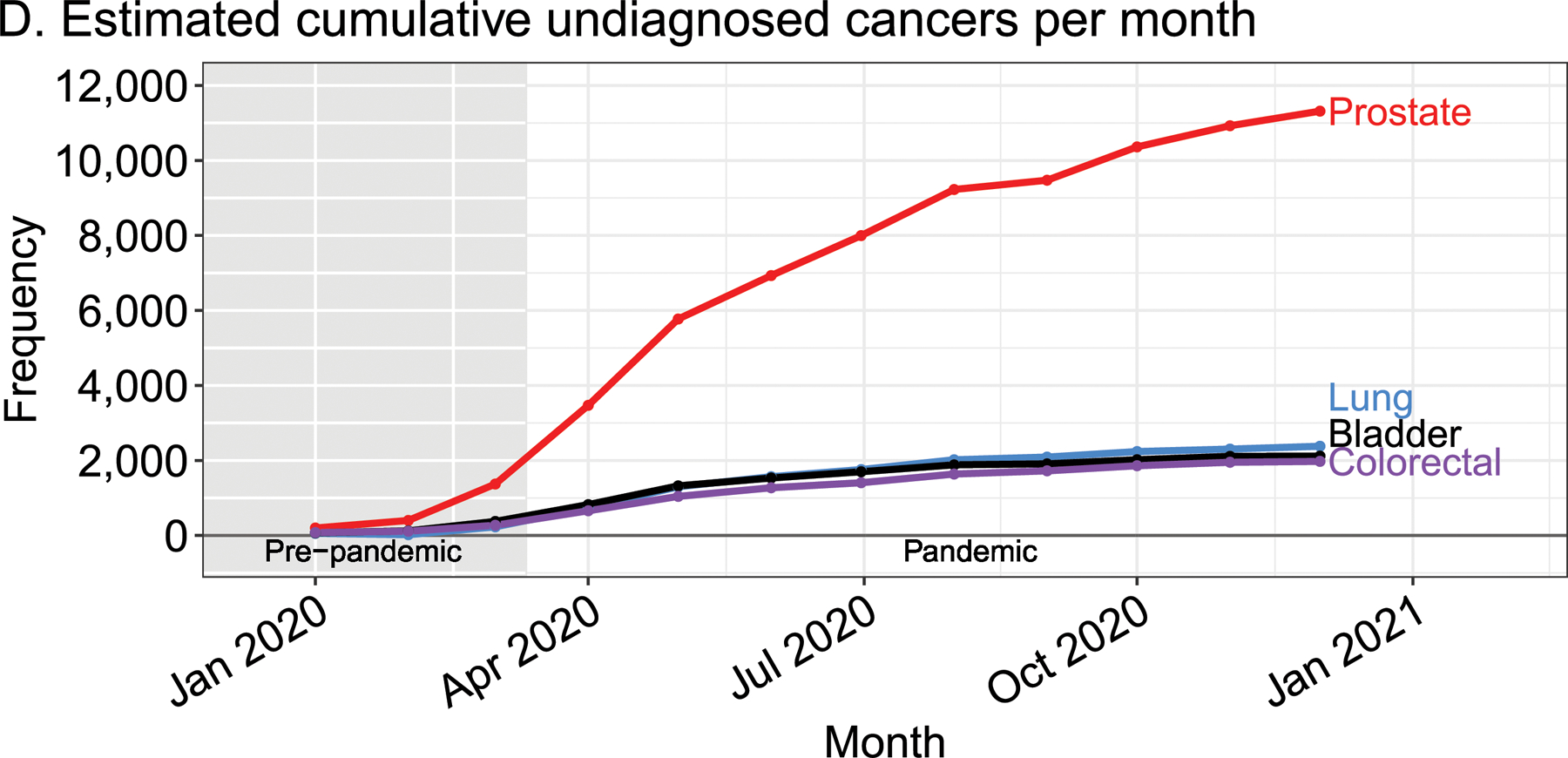
Temporal trends in new cancer diagnoses in the VA health system from 2018 to 2020 are presented as (A) monthly cases and (B) percentage of seasonally adjusted baseline. The estimated (C) monthly and (D) cumulative number of undiagnosed cancers in 2020. The grey, shaded region indicates the pre-pandemic era, defined as prior to March 11, 2020.
To help states (or institutions) plan efforts to clear the backlog of missed procedures, we designed a nomogram displaying the relationship between 3 factors, (1) case deficit as a percent of monthly baseline, (2) percent increase in monthly volume to clear backlog of cases, and (3) number of months needed to clear the backlog (Figure 5). Knowing any two values allows the user to calculate the third value by constructing a straight line passing through the two known inputs. For example, if colonoscopies dropped to 50% of expected volume over a six-month period during the pandemic, a backlog of unperformed colonoscopies equal to 300% of average monthly volume would exist (50% × 6). If resources allow an institution to increase their colonoscopy rates to 25% above their monthly average; then connecting 25 (Percent Increase in Monthly Volume to Clear Cases) and 300 (Case Deficit as Percent of Monthly Baseline) would find that 12 months are required to clear the backlog. Supplemental Figure 1 presents this nomogram using absolute numbers.
Figure 5.
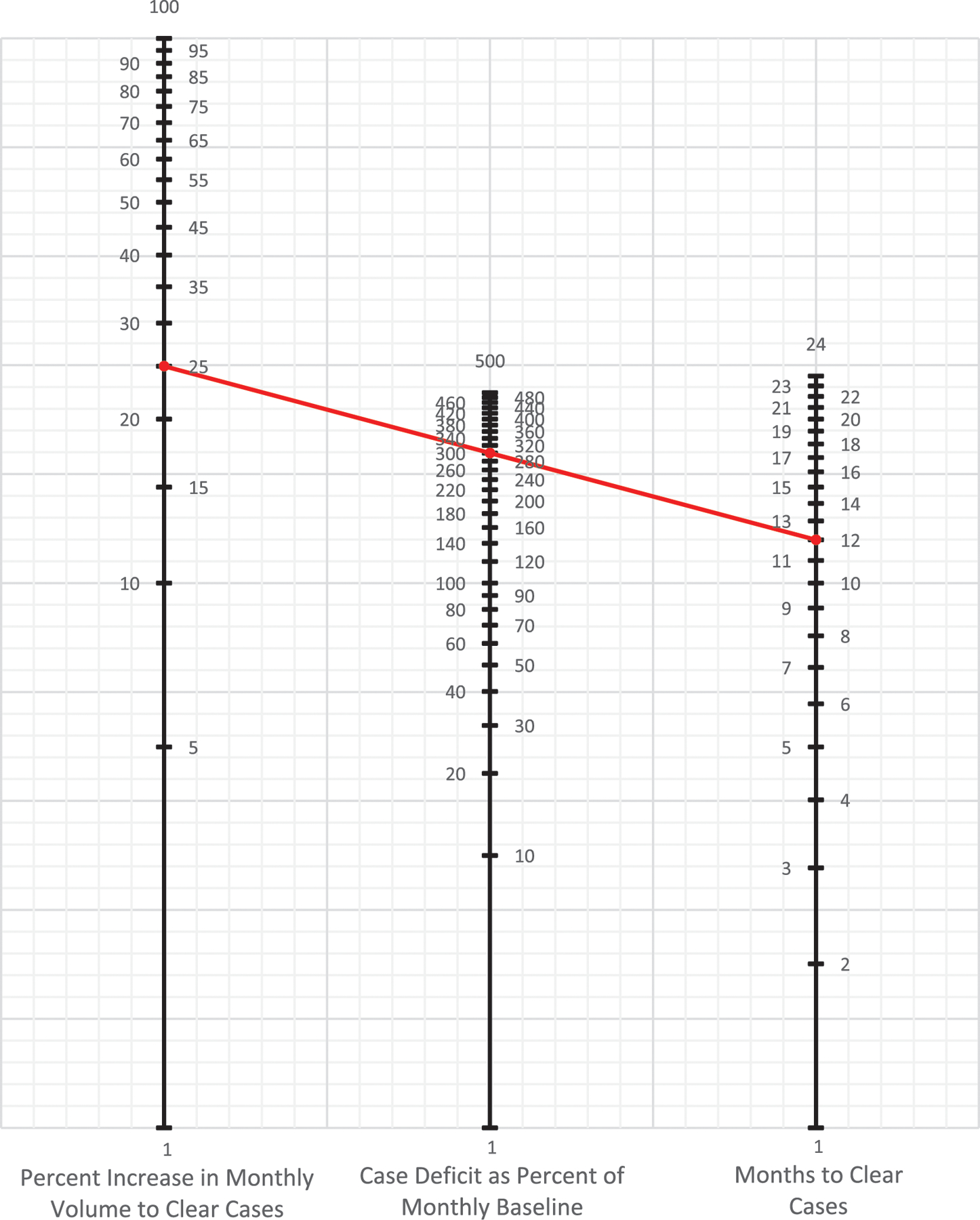
Nomogram to calculate the relationship between unperformed cases, potential monthly capacity above baseline, and months needed to clear all unperformed cases. Formula: Monthly percent increase in volume to clear unperformed cases = Unperformed cases as percent of monthly baseline/months to clear unperformed cases. Example (red line): From 4/1/2020 to 10/1/2020 (6 months), we performed 50% of our expected monthly volume of colonoscopies. We have a backlog of 300% of our monthly volume: 6*50=300%. We can perform up to 125% of our expected monthly volume of colonoscopies, an additional 25%. We connect the 25 on the far-left line with 300 on the middle line using a straight edge to calculate that it will take us 12 months to clear these unperformed cases. Alternatively, we calculate that we have an unperformed case load of 300% of our monthly volume. We want to clear these cases within one year or 12 months. We connect the 12 on the far-right line with 300 on the middle line using a straight edge to calculate that it will take an increased volume of 25% to clear these cases in the desired time period.
Discussion
There was widespread recognition of the disruptions in cancer care during the early period of the COVID-19 pandemic. Patients with known cancers are easily identified, and reductions in treatment activities readily quantified. Accurately identifying the backlog of missed screening or diagnostic procedures and the resulting undiagnosed cancers is challenging. Examining data from the VA health system, we quantified decreases in cancer encounters, diagnostic and screening procedures, and new diagnoses for the four most common cancers in VA patients. We found a dramatic decrease in all three metrics in the early months of the pandemic with no evidence of a subsequent rebound by the end of 2020 that would be sufficient to make-up for lost procedures or diagnoses. Screening chest CT scans were the exception, with a rebound that resulted in no annual deficit for 2020. For other procedures, decreases of up to 45% of typical annual volumes have accumulated and continue to accrue, though at a slower pace. There were large geographic variations in the decreased diagnostic activities for cancers across states and across different cancers, though no specific patterns were identified. Finally, we developed a nomogram for institutions, health systems, or states to estimate the time and resources required to work through the backlog in diagnostic activities accrued during 2020.
With the moratorium on non-emergency clinical encounters throughout much of the US, decreases in treatment and clinical activities that impacted identification of new cancers were seen during the peak of the pandemic.16 The first half of 2020 saw decreased resections for colon and breast cancer, screening, and biopsies in the Medicare population.3, 12, 13 Data also suggest that new diagnoses of cancer decreased during the early stages of the pandemic.10 While these reports were concerning, they reflected activities at the height of the pandemic. Our report examines the entirety of 2020 and estimates the accumulated deficit in new cancer diagnoses and in procedures that could facilitate the diagnosis of new cancers. By computing the cumulative decrease, we identified that through the end of 2020, we have yet to enter a “catching-up” period, where we are clearing the backlog in diagnoses and procedures. Screening chest CT scans represent the exception to this observation, rebounding in the second half of 2020, so that no overall deficit existed by the end of 2020. Rather than focusing only on procedures that were performed specifically as a tool for cancer surveillance, we considered all diagnostic procedures in which a cancer could be diagnosed incidentally, as part of a screening program, or as part of testing based on clinical concerns, to be a “lost opportunity” to diagnose a new cancer.
There may be several reasons why the deficits have persisted even as states and institutions have relaxed COVID-related restrictions. The variations in state-level trends may reflect variations in statewide restrictions, institutional response to local outbreaks, or differences in perceived risk of COVID-19 by patients and institutions.17 Unemployment and the financial hardships from the pandemic may have restricted healthcare access, although not as significant a problem in the VA population as in employer-based insurance. Perceived risks of invasive versus non-invasive procedures may explain why CT scans recovered to near baseline levels by the end of 2020 and accumulated smaller backlogs than colonoscopies. Even if the risks of COVID-19 are minimized through vaccination and herd immunity, patients who have fallen out of the routine of their typical care may encounter barriers to re-entry that are difficult to overcome. For these reasons, health systems will need to identify areas where patients are not following up on their routine cancer care or screening and find ways to reassure and re-engage them.
Data from Brazil suggests that short-term decreases in cancer care lead to increased rates of cancer-related deaths.6 Although increased cancer-specific deaths have not been demonstrated in the US, early reports from New York City found a short-term increase in non-COVID-related mortality during their early pandemic surge.5 Modeling of pre-pandemic data from the United Kingdom suggests that a delay in the identification and care for colorectal cancer could lead to increases in deaths by up to 20%.8 Conversely, extrapolating data from the US based National Cancer Databank, investigators concluded that patients with many cancers, including breast and prostate, could sustain a delay in resection of 3–6 months without significant increase in mortality, particularly if chemotherapy or endocrine therapy was being used.9, 18, 19 We identified a population whose cancer would be undiagnosed and would therefore not be eligible for neoadjuvant therapy. In addition, the pandemic has impacted the ability of centers to deliver neoadjuvant therapy. Our data indicates that backlogs continued to accumulate through the end of 2020, suggesting that the delay in diagnosing new cancer may be longer than 6 months. Some of these cancers may become symptomatic, prompting a work-up and diagnosis; however, others may progress without symptoms, becoming unresectable or metastasizing before detection. Other cancers may be indolent; for example, a majority of prostate cancers are slow growing and will not significantly benefit from early detection. We are unaware of any organized strategy to quantify, identify, and clear the deficit of unperformed procedures and undiagnosed cancers. Our results provide the first steps in this effort.
Given the decrease in diagnostic procedures, we can anticipate healthcare consequences including undiagnosed cancers, upstaging at subsequent diagnosis, increased intensity and complexity of treatment, and increased mortality. Our results indicate that an urgent, informed, and concerted response is needed. Along with providing a blueprint for computing the accumulated deficit within a specific environment, our study provides a tool, a nomogram to guide institutions and health systems to conceptualize the potential increased capacity and time needed to address the unmet needs. Health systems, including the VA, must develop plans to increase capacity to quickly alleviate accumulated demand. Outreach through primary care providers with access to patients that have been lost to follow-up must be instituted. Alternatively, health systems may increase screening intervals, particularly for low-risk individuals, or focus outreach efforts to patients with increased risk factors. Efforts should be deliberate and evidence-based.
Future studies will need to examine the consequences of delayed cancer diagnoses. Increased incidence of unresectable disease, inability to achieve R0 resection, advanced stage at diagnosis, metastatic disease, need for adjuvant therapies, and mortality may indicate that diagnostic delays are impacting patient outcomes. These outcomes may take years to become evident, and our future goals involve identifying these outcomes and developing a surveillance system to monitor for increases. In addition, a more granular examination of state variation will be needed to understand how some states continued providing screening and diagnostic procedures at close to baseline case volumes while others had dramatic decreases of 50% or more.
Our study has several limitations. The VA population is older and predominantly male, making assessment of diseases like breast cancer difficult, though we found no evidence in the published literature to suggest that the pandemic affected healthcare for women differently than men. The patient population dictated our selection of the four target cancers, and it is possible that other cancers may offer different results. While the results are from an administrative database, it is reasonable to anticipate that there was no selection bias with respect to clinical encounters for different cancers. The VA’s Care in the Community (CITC) program allows Veterans to seek care outside of the VA system, and these data would not be included in our analysis. Given evidence that clinical encounters and diagnostic procedures decreased across all healthcare in the US,3, 10 it seems unlikely that the decrease in cancer care at VA institutions was being made up by outside centers. VA centers do not have the same financial pressures as other institutions, and these results may not be generalizable to all populations. CPT codes could not reliably differentiate screening and diagnostic colonoscopies, although all colonoscopies represent an opportunity to identify a cancer. The VINCI data involves administrative data, where miscoding of procedural data is low but exists.20
Conclusion
Health systems across the US have suffered a major disruption in cancer care from COVID-19. While the extent and impact of the pandemic on immediate treatment of known cancers is predictable and has been reported on, we found a major reduction in diagnostic procedures that are used to identify new cancers and a consequent reduction in diagnosis of new cancers. The deficits vary by geographic location and by cancer type. We also provide the means to facilitate a recovery plan to resolve these unmet healthcare needs and avoid the potential for worse long-term cancer outcomes.
Supplementary Material
The authors have the following funding sources:
Veterans Affairs awards HSRD C19-20-407, RRD RX000995 and CSRD CX001621, and NIH awards NS080168, NS097876 and AG000513 (BKL); National Institutes of Health awards AG028747, DK072488, and Baltimore VA Medical Centre GRECC (JDS); National Institutes of Health T32 AG00262 (NKP)
Footnotes
Conflict of Interest:
The authors have no conflicts of interest to disclose.
References
- 1.Centers for Medicare & Medicaid Services. Non-Emergent, Elective Medical Services, and Treatment Recommendations. Available from URL: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf [accessed 9/17/2020].
- 2.American College of Surgeons. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. Available from URL: https://www.facs.org/COVID-19/clinical-guidance/triage [accessed 10/8/2020].
- 3.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clin Cancer Inform. 2020;4: 1059–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richards M, Anderson M, Carter P, Ebert BL, Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nat Cancer. 2020;1: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID Response Team, New York City Department of Health and Mental Hygiene. Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak - New York City, March 11-May 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69: 603–605. [DOI] [PubMed] [Google Scholar]
- 6.Fonseca GA, Normando PG, Loureiro LVM, et al. Reduction in the Number of Procedures and Hospitalizations and Increase in Cancer Mortality During the COVID-19 Pandemic in Brazil. JCO Glob Oncol. 2021;7: 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu SJ, George EL, Maggio PM, Hawn M, Nazerali R. The Consequences of Delaying Elective Surgery: Surgical Perspective. Ann Surg. 2020;272: e79–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21: 1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turaga KK, Girotra S. Are We Harming Cancer Patients by Delaying Their Cancer Surgery During the COVID-19 Pandemic? Ann Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the Number of US Patients With Newly Identified Cancer Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Netw Open. 2020;3: e2017267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller MJ, Xu L, Qin J, et al. Impact of COVID-19 on Cervical Cancer Screening Rates Among Women Aged 21–65 Years in a Large Integrated Health Care System - Southern California, January 1-September 30, 2019, and January 1-September 30, 2020. MMWR. Morbidity and Mortality Weekly Report. 2021;70: 109–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filipe MD, van Deukeren D, Kip M, et al. Effect of the COVID-19 Pandemic on Surgical Breast Cancer Care in the Netherlands: A Multicenter Retrospective Cohort Study. Clin Breast Cancer. 2020;20: 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Haren RM, Delman AM, Turner KM, et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg. 2021;232: 600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasad NK, Englum BR, Turner DJ, et al. A Nation-wide Review of Elective Surgery and COVID-Surge Capacity. J Surg Res. 2021;267: 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zullig LL, Jackson GL, Dorn RA, et al. Cancer incidence among patients of the U.S. Veterans Affairs Health Care System. Military medicine. 2012;177: 693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Surgeons. COVID-19: Executive Orders by State on Dental, Medical, and Surgical Procedures Available from URL: https://www.facs.org/covid-19/legislative-regulatory/executive-orders [accessed 10/8/2020.
- 17.Hoehn RS, Zureikat AH. Cancer disparities in the COVID-19 era. J Surg Oncol. 2020;122: 371–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dee EC, Mahal BA, Arega MA, et al. Relative Timing of Radiotherapy and Androgen Deprivation for Prostate Cancer and Implications for Treatment During the COVID-19 Pandemic. JAMA Oncol. 2020;6: 1630–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Minami CA, Kantor O, Weiss A, Nakhlis F, King TA, Mittendorf EA. Association Between Time to Operation and Pathologic Stage in Ductal Carcinoma in Situ and Early-Stage Hormone Receptor-Positive Breast Cancer. J Am Coll Surg. 2020;231: 434–447 e432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee DS, Stitt A, Wang X, et al. Administrative hospitalization database validation of cardiac procedure codes. Med Care. 2013;51: e22–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


