Introduction
Acupuncture is recommended as part of comprehensive pain care for low back pain, neck pain, and fibromyalgia by agencies including the Agency for Healthcare Research and Quality.1 There is additional evidence that acupuncture is associated with reductions in total health care spending among patients with low back pain.2
Research suggests that insurance coverage for acupuncture is inconsistent, although there is a lack of published data in most states.3,4 One survey of 45 commercial, Medicaid, and Medicare Advantage plans found that only one-third of plans covered acupuncture, suggesting most patients pay for acupuncture entirely out-of-pocket.5 When insurers covered acupuncture, cost sharing was higher than other nonpharmacological interventions and insurers tended to cover few indications and provider types.4,5
Here, we document trends in insurance coverage for acupuncturist visits using a nationally representative survey. Given Medicare’s 2020 decision to reimburse acupuncture for low back pain, we hypothesize that insurance coverage increased over time.5
Methods
We examined insurance coverage for acupuncturist visits between 2010 and 2019 using the Medical Expenditure Panel Survey (MEPS). We measured the share of respondents aged 18+ with ≥1 acupuncturist visit. Among acupuncture users, we calculated (1) total annual amount paid for acupuncturist visits, (2) annual amount paid out-of-pocket for acupuncturist visits, (3) share of acupuncturist visits with any insurance coverage, and (4) percent paid out-of-pocket for acupuncturist visits. We calculated the outcomes in two-year intervals to improve precision and compared outcomes in 2010–2011 versus 2018–2019 using two-sided pairwise t-tests.
Results
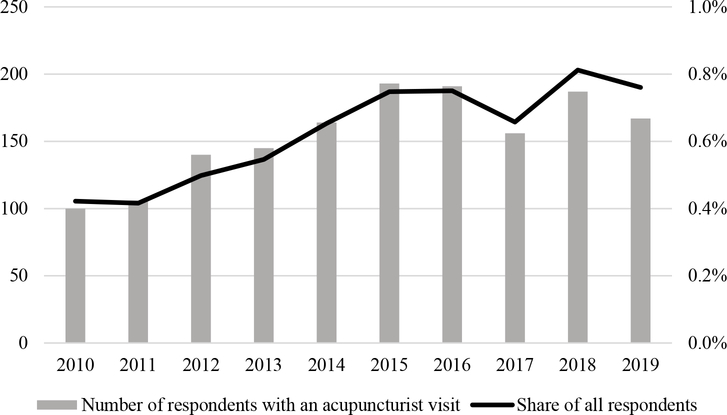
The proportion of respondents with ≥1 acupuncturist visit increased from 0.4% in 2010 to 0.8% in 2019 (Figure 1). The 1,344 acupuncture users were 68.6% female, 18.7% Asian, 6.3% Black, 15.0% Hispanic, 57.1% White, and had an average age of 51.9 years (SD: 15.9).
Figure 1.
Trends in Office Visits with Acupuncturists in the Medical Expenditure Panel Survey, 2010–2019
Notes. Between 2010 and 2019, 1,344 respondents reported at least one visit with an acupuncturist.
Spending on acupuncturist visits increased during the study period (Table 1). On average, the total annual amount paid for acupuncturist visits was $593 (95%CI: $460-$726) in 2010–2011 and $1,022 in 2018–2019 (95%CI: $806-$1,237); the increase was statistically significant (mean difference=$429; 95%CI: $129-$728). While the annual amount paid out-of-pocket increased from $376 (95%CI: $286-$465) in 2010–2011 to $554 (95%CI: $384-$725) in 2018–2019, the change was not statistically significant (mean difference=$179; 95%CI: $−55 to $412). The increase in spending was largely driven by more acupuncturist visits among users, which rose from 5.4 visits in 2010 to 8.2 visits in 2019.
Table 1.
Trends in Spending and Insurance Coverage for Acupuncturist Visits in the Medical Expenditure Panel Survey, 2010–2019
| Total annual amount paid for acupuncturist visits (mean, 95%CI) | Annual amount paid out-of-pocket for acupuncturist visits (mean, 95%CI) | Share of acupuncturist visits with any insurance coverage (mean, 95%CI) | Percent paid out-of-pocket for acupuncturist visits (mean, 95%CI) | Number of unique visits with an acupuncturist | |
|---|---|---|---|---|---|
| 2010–2011 | $593.00 | $375.51 | 41.1% | 66.9% | 1,052 |
| ($460.29–725.70) | ($286.12–464.90) | (38.1–44.0%) | (64.4–69.3%) | ||
| 2012–2013 | $588.45 | $286.54 | 43.9% | 58.2% | 1,665 |
| ($454.96–721.95) | ($228.34–344.74) | (41.5–46.3%) | (55.9–60.4%) | ||
| 2014–2015 | $583.58 | $314.27 | 43.4% | 61.0% | 2,090 |
| ($494.66–672.50) | ($254.86–373.69) | (41.3–45.5%) | (59.2–62.9%) | ||
| 2016–2017 | $728.31 | $358.58 | 47.8% | 57.6% | 2,205 |
| ($593.47–863.16) | ($276.28–440.89) | (45.7–49.9%) | (55.7–59.4%) | ||
| 2018–2019 | $1,021.57 | $554.26 | 50.2% | 57.5% | 2,656 |
| ($806.32–1,236.82) | ($383.54–724.99) | (48.3%-52.1%) | (55.8–59.1%) |
Notes. Dollar amounts were adjusted for inflation to 2019 dollars using the health care consumer price index. Visits with negative spending amounts were excluded.
Sources: Blewett LA, Rivera Drew JA, Griffin R, King ML, Williams KCW. IPUMS Health Surveys: Medical Expenditure Panel Survey, Version 1.1 [dataset]. 2019; https://meps.ipums.org/meps/.
U.S. Bureau of Labor Statistics, Consumer Price Index for All Urban Consumers: Medical Care in U.S. City Average [CPIMEDSL], retrieved from FRED, Federal Reserve Bank of St. Louis; https://fred.stlouisfed.org/series/CPIMEDSL.
The share of acupuncturist visits with any insurance coverage increased from an average of 41.1% (38.1%−44.0%) in 2010–2011 to 50.2% (48.3%−52.1%) in 2018–2019 (mean difference=9.1 percentage points (pp); 95%CI: 5.6pp-12.7pp), while the percent paid out-of-pocket declined from 66.9% (95%CI: 64.4%−69.3%) in 2010–2011 to 57.5% (95% CI: 55.8%−59.1%) in 2018–2019 (mean difference=−9.4pp; 95%CI: −12.5pp to −6.3pp).
Discussion
Between 2010 and 2019, the share of MEPS respondents with ≥1 acupuncturist visit doubled, and the rate of insurance coverage increased by nearly 10 percentage points. This finding aligns with a recent study from Oregon Medicaid, which found both expanded coverage for acupuncture and more acupuncture utilization.6
Nevertheless, half of respondents reported no insurance coverage for acupuncturist visits in 2019, and most spending occurred out-of-pocket. Insurers have cited an inconsistent evidence base as one driver of coverage decisions, yet acupuncture has been demonstrated effective for various pain conditions that aren’t always covered.1,5 For example, Medicare reimburses acupuncture for low back pain, excluding other conditions for which acupuncture is recommended.1,5
The study had notable limitations. The MEPS is nationally representative, but its size resulted in fewer than 1,400 respondents with an acupuncturist visit. Measures were self-reported. We cannot assess whether respondents were referred to acupuncturists nor do we examine indications associated with acupuncture therapy.
Acknowledgements
Dr. Candon had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the statistical analysis. Dr. Dusek and Dr. Nielsen report partial support from the National Center for Complementary and Integrative Health (U01 AT010598 - Acupuncture in the Emergency Department for Pain).
References
- 1.Skelly AC, Chou R, Dettori JR, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Comparative Effectiveness Review No. 227. AHRQ Publication No. 20-EHC009. 2020; https://effectivehealthcare.ahrq.gov/products/noninvasive-nonpharm-pain-update/research. Accessed April 17, 2020. [PubMed] [Google Scholar]
- 2.Olaisen RH. Associations Between Complementary and Alternative Medicine and Health Care Expenditures Among Adults With Chronic Back Pain. Med Care. 2020;58(8):689–695. [DOI] [PubMed] [Google Scholar]
- 3.Nahin RL, Barnes PM, Stussman BJ. Insurance coverage for complementary health approaches among adult users: United States, 2002 and 2012. NCHS Data Brief. 2016(235):1–8. [PubMed] [Google Scholar]
- 4.Bleck R, Marquez E, Gold MA, Westhoff CL. A scoping review of acupuncture insurance coverage in the United States. Acupunct Med. 2020:964528420964214. [DOI] [PubMed] [Google Scholar]
- 5.Heyward J, Jones CM, Compton WM, et al. Coverage of nonpharmacologic treatments for low back pain among U.S. public and private insurers. JAMA Network Open 2018;1(6):e183044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choo EK, Charlesworth CJ, Gu Y, Livingston CJ, McConnell KJ. Increased use of complementary and alternative therapies for back pain following statewide medicaid coverage changes in Oregon. J Gen Intern Med. 2021;36(3):676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]