Abstract
IMPORTANCE
The COVID-19 pandemic has negatively affected adult mental health (MH), with racial and ethnic minoritized groups disproportionately affected.
OBJECTIVE
To examine changes in adult MH-related emergency department (ED) visits into the Delta variant pandemic period and identify changes and inequities in these visits before and during COVID-19 case surges.
DESIGN, SETTING, AND PARTICIPANTS
This epidemiologic cross-sectional study used National Syndromic Surveillance Program data from US adults aged 18 to 64 years from 1970 to 2352 ED facilities from January 1, 2019, to August 14, 2021. All MH-related ED visits and visits related to 10 disorders (ie, anxiety, depressive, bipolar, schizophrenia spectrum, trauma- and stressor-related, attention-deficit/hyperactivity, disruptive behavioral and impulse, obsessive-compulsive, eating, and tic disorders) were identified.
EXPOSURES
The following periods of MH-related ED visits were compared: (1) high Delta variant circulation (July 18-August 14, 2021) with a pre-Delta period (April 18-May 15, 2021), (2) after a COVID-19 case peak (February 14-March 13, 2021) with during a peak (December 27, 2020-January 23, 2021), and (3) the Delta period and the period after a COVID-19 case peak with the respective corresponding weeks during the prepandemic period.
MAIN OUTCOMES AND MEASURES
ED visits for 10 mental disorders and all MH-related visits.
RESULTS
This cross-sectional study included 107 761 319 ED visits among adults aged 18 to 64 years (59 870 475 [56%] women) from January 1, 2019, to August 14, 2021. There was stability in most MH-related ED visit counts between the Delta and pre-Delta periods (percentage change, −1.4% to −7.5%), except for eating disorders (−11.9%) and tic disorders (−19.8%) and after a COVID-19 case peak compared with during a peak (0.6%−7.4%). Most MH-related ED visit counts declined in the Delta period relative to the prepandemic period (−6.4% to −30.7%); there were fluctuations by disorder when comparing after a COVID-19 case peak with the corresponding prepandemic period (−15.4% to 11.3%). Accounting for ED visit volume, MH-related ED visits were a smaller proportion of visits in the Delta period compared with the pre-Delta period (visit ratio, 0.86; 95% CI, 0.85–0.86) and prepandemic period (visit ratio, 0.80; 95% CI, 0.79–0.80). After a COVID-19 case peak, MH-related ED visits were a larger proportion of ED visits compared with during a peak (visit ratio, 1.04; 95% CI, 1.03–1.04) and the corresponding prepandemic period (visit ratio, 1.11; 95% CI, 1.11–1.12). Of the 2 510 744 ED visits included in the race and ethnicity analysis, 24 592 (1%) were American Indian or Alaska Native persons, 33 697 (1%) were Asian persons, 494 198 (20%) were Black persons, 389 740 (16%) were Hispanic persons, 5000 (0.2%) were Native Hawaiian or Other Pacific Islander persons, and 1 172 683 (47%) were White persons. There was between- and within-group variation in ED visits by race and ethnicity and increases in selected disorders after COVID-19 peaks for adults aged 18 to 24 years.
CONCLUSIONS AND RELEVANCE
Results of this cross-sectional study suggest that EDs may have increases in MH-related visits after COVID-19 surges, specifically for young adults and individual racial and ethnic minoritized subpopulations. Public health practitioners should consider subpopulation-specific messaging and programmatic strategies that address differences in MH needs, particularly for those historically marginalized.
The COVID-19 pandemic has resulted in greater self-reported symptoms of anxiety, depression, trauma and stress, tics, and other mental disorders among adults into early 2021.1–9 The pandemic may also have had an effect on mental health (MH)–seeking behavior. In addition to a rise in untreated mental disorders,7 there has been an increase in emergency department (ED) visits for selected aspects of MH in March to October 2020 compared with the prepandemic period.10 There are limited data on contemporary pandemic periods and insufficient information on MH care-seeking behavior and how this is affected by COVID-19 case surges, which is critical for health care planning.
Preexisting health, social, and economic conditions for historically marginalized communities in the US have exacerbated outcomes associated with the pandemic,11–14 including MH.3–5 Racial and ethnic minoritized groups, particularly Black and Hispanic persons, had more symptoms of some mental disorders compared with other groups early in the pandemic.3–5 The cumulative effect of high COVID-19 mortality, economic downturn, and trauma—including racially motivated violence—have MH consequences for racial and ethnic minoritized groups.15–18 EDs serve as a critical entry point for health care services for racial and ethnic minoritized groups owing to lack of primary care and medical home access.19,20 There are limited data on MH care-seeking behavior for these communities during the pandemic.
This analysis examined changes for all MH-related ED visits, and visits for 10 specific mental disorders, for adults aged 18 to 64 years during the pandemic. Data through August 2021 were used to describe MH trends into the Delta variant period on emergency MH care-seeking behavior for US adults, with an emphasis on identifying changes and racial and ethnic inequities in adult MH-related ED visits before and during COVID-19 case surges.
Methods
Participants and Procedures
In this epidemiologic cross-sectional study, we analyzed deidentified electronic medical record data on ED visits for adults aged 18 to 64 years collected via the National Syndromic Surveillance Program (NSSP) from January 1, 2019, to August 14, 2021. More than 3600 facilities from 49 states and District of Columbia contributed data at the time of analysis, constituting approximately 71% of US nonfederal ED facilities.21 Administrative data analyses are considered public health practice by the US Centers for Disease Control and Prevention; therefore, no institutional review board approval or patient consent was required. Race and ethnicity information for all adults was gathered from the database and included American Indian or Alaska Native, Asian, Black, Hispanic, Native Hawaiian or Other Pacific Islander, and White. Persons of Hispanic ethnicity were classified as Hispanic regardless of race; other categories reflect non-Hispanic persons. All MH-related ED visits, and visits related to 10 disorders (ie, anxiety, depressive, bipolar, schizophrenia spectrum, trauma- and stressor-related [TS], attention-deficit/hyperactivity, disruptive behavioral and impulse, obsessive-compulsive, eating, and tic disorders), were identified using chief complaint terms and discharge diagnosis codes (eTable 1 in the Supplement). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Statistical Analysis
As contributing facilities change over time and chief complaint and discharge diagnosis field completeness varies by facility, we limited all analyses to facilities reporting high-quality data (coefficient of variation ≤40; average weekly discharge diagnosis ≥75%) in each period of interest. For race and ethnicity analyses, we also restricted data to include only average weekly data at least 75% or more complete for combined race and ethnicity fields. As of August 2021, NSSP race and ethnicity data were 84.5% complete; completeness and data collection mechanisms vary by facility.
We examined MH-related ED visits before and during the COVID-19 pandemic; periods were selected by examining changes in US COVID-19 case trajectories.22 To examine the association of the Delta pandemic period with MH-related ED visits, we compared visits in a period with high (>90% of US specimens tested) Delta variant circulation (July 18-August 14, 2021) with a period when Delta circulation was low (<15%; April 18-May 15, 2021).23 We compared MH-related ED visits immediately after a COVID-19 case peak (February 14-March 13, 2021) with during a COVID-19 case peak (December 27, 2020-January 23, 2021) to understand trends in MH-related visits after COVID-19 case surges. We compared the Delta period and the period after a COVID-19 case peak with corresponding weeks in 2019 to understand changes in MH-related ED visits before and during the pandemic. Analytic index periods were either the COVID-19 Delta period (July 18-August 14, 2021) or the period after a COVID-19 case peak (February 14-March 13, 2021).
For each index period, raw ED visit counts and MH visits per 100 000 ED visits were calculated overall and by race and ethnicity, sex, and age. The denominator per 100 000 ED visits reflects visits for the subpopulation of interest in stratified results. To examine temporal changes from index to comparison periods, we calculated the percentage change in raw ED visit counts. In line with NSSP data standards, we considered changes in visit volume as follows: high decreases (≥−20%), moderate decreases (>−10% to −<20%), stable (≥−10% to <10%), moderate increases (≥10%–<20%), and high increases (≥20%). These thresholds included rounded percentages. In addition to presenting raw MH-related visit counts, we calculated visit ratios (VRs) and 95% CIs to compare the proportion of MH-related visits of all ED visits in the index with comparison periods. VRs and 95% CIs provided information on whether MH-related visits comprised a larger (VR >1.0) or smaller (VR <1.0) proportion of all ED visits in the index compared with comparison periods. The median (range) number of facilities included in analyses examining all MH-related ED visits and specific disorders overall and by sex and age was 2035 (1970–2041).
Owing to small cell sizes, analyses by race and ethnicity included only the 5 most common disorders and all MH-related visits. Owing to improvements in race and ethnicity data completeness during the pandemic, MH-related visit count percentage change and VRs with 95% CIs for race and ethnicity were only calculated when comparing the Delta with the pre-Delta period and the period after a COVID-19 case peak with during a peak. VRs with 95% CIs were calculated to compare the proportion of MH-related visits between racial and ethnic groups. There were 2352 facilities included in race and ethnicity analyses. All data were analyzed using R software, version 4.1.2 (The R Foundation).
Results
This epidemiologic cross-sectional study included 107 761 319 ED visits among adults aged 18 to 64 years (16 569 474 [15%] aged 18–24 years; 58 682 874 [55%] aged 25–49 years; 32 508 971 [30%] aged 50–64 years; 59 870 475 [56%] women; 47 711 919 [44%] men) from January 1, 2019, to August 14, 2021. There were 2 510 744 ED visits included in the subsample used for the race and ethnicity analysis; sex and age demographic patterns mirrored those for the entire sample. Among these visits, 24 592(1%) were among American Indian or Alaska Native persons, 33 697 (1%) were among Asian persons, 494 198 (20%) were among Black persons, 389 740 (16%) were among Hispanic persons, 5000 (0.2%) were among Native Hawaiian or Other Pacific Islander persons, and 1 172 683 (47%) were among White persons.
MH-related ED visit counts from January 1, 2019, to August 14, 2021, are listed in Figure 1. After a decline in March 2020, MH-related ED visit counts for most disorders rose from the spring to the summer of 2020, with a decline in late fall 2020. MH-related ED visits, overall and for most disorders, were at their highest in the summer to midfall 2020.
Figure 1.

US Mental Health-Related Emergency Department (ED) Visit Counts for Adults Aged 18 to 64 years, Overall and by DisorderThis figure includes data from January 1, 2019, through August 14, 2021. Shaded areas of the graph depict time periods included in the analytic index or comparison periods, which are as follows: the prepandemic comparison periods (February 10-March 9, 2019, and July 14-August 10, 2019), the COVID-19 case peak comparison period (December 27, 2020-January 23, 2021), the period immediately after a COVID-19 case peak index period (February 14-March 13, 2021), a COVID-19 pandemic comparison period with low circulation of the Delta variant, called the pre-Delta period (April 18-May 15, 2021), and a COVID-19 pandemic index period with high circulation of the Delta variant, called the Delta period (July 18-August 14, 2021). To accommodate differences in counts of all mental health-related visits and specific disorders, results for high-prevalence (A), medium-prevalence (B), and low-prevalence (C) disorders are presented.
Delta to Pre-Delta Pandemic Period
Among adults aged 18 to 64 years, there was stability in all MH-related ED visit counts (−3.3%), as well as counts for most specific disorders (range, −1.4% to −7.5%), between the Delta and pre-Delta periods (Table 1). However, there were moderate and high decreases in ED visit counts for eating disorders (−11.9%) and tic disorders (−19.8%), respectively, from the Delta to the pre-Delta periods.
Table 1.
Changes in MH-Related ED Visits for Adults Aged 18 to 64 Years in Selected Periods Before and During the COVID-19 Pandemic, US, February 10, 2019, to August 14, 2021a,b
| After Delta variant onset, index period: July 18-August 14, 2021 | After a COVID-19 case peak, index period: February 14, 2021-March 13, 2021 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Index period compared with MH in the COVID-19 pandemic before the Delta variant period (April 18-May 15, 2021) | Index period compared with prepandemic MH (July 14, 2019-August 10, 2019) | Index period compared with MH during a COVID-19 case peak (December 27, 2020-January 23, 2021) | Index period compared with prepandemic MH (February 10, 2019-March 9, 2019) | |||||||||
| Disorder | Total ED visit counts for MH, No. | ED visits for MH per 100 000 ED visitsc | Change in ED counts for MH, %d | Visit ratio (95% CI)e | Change in ED counts for MH, %d | Visit ratio (95% CI)e | Total ED visit counts forMH, No. | ED visits for MH per 100 000 ED visitsc | Change in ED counts for MH, %d | Visit ratio (95% CI)e | Change in ED counts for MH, %d | Visit ratio (95% CI)e |
| All MH | 249 700 | 6725 | −3.3 | 0.86 (0.85–0.86) | −17.2 | 0.80 (0.79–0.80) | 256 628 | 8728 | 1.5 | 1.04 (1.03–1.04) | −5.4 | 1.11 (1.11–1.12) |
| Anxiety | 122 463 | 3298 | −3.4 | 0.86 (0.85–0.86) | −17.7 | 0.79 (0.78–0.80) | 125 900 | 4282 | 0.6 | 1.03 (1.02–1.03) | −4.2 | 1.13 (1.12–1.14) |
| Depressive | 72 674 | 1957 | −5.7 | 0.84 (0.83–0.84) | −30.7 | 0.67 (0.66–0.67) | 79 463 | 2703 | 1.2 | 1.03 (1.02–1.04) | −15.4 | 1.00 (0.99–1.01) |
| Bipolar | 29 460 | 793 | −6.2 | 0.83 (0.82–0.84) | −25.6 | 0.71 (0.70–0.73) | 32 010 | 1089 | 2.2 | 1.04 (1.03–1.06) | −8.7 | 1.08 (1.06–1.09) |
| Schizophrenia spectrum | 25 309 | 682 | −6.4 | 0.83 (0.82–0.84) | −15.6 | 0.81 (0.80–0.83) | 28 107 | 956 | 1.9 | 1.04 (1.02–1.06) | 5.2 | 1.24 (1.22–1.26) |
| Trauma- and stressor-related | 18 982 | 511 | −6.3 | 0.83 (0.81–0.85) | −24.7 | 0.72 (0.71–0.74) | 20 403 | 694 | 4.9 | 1.07 (1.05–1.09) | −3.9 | 1.13 (1.11–1.15) |
| Attention-deficit/hyperactivity | 6078 | 164 | −7.5 | 0.82 (0.79–0.85) | −30.5 | 0.67 (0.65–0.69) | 6337 | 216 | 3.4 | 1.06 (1.02–1.09) | −14.1 | 1.01 (0.98–1.05) |
| Disruptive behavioral and impulse | 2898 | 78 | −1.4 | 0.87 (0.83–0.92) | −14.2 | 0.82 (0.78–0.87) | 3131 | 106 | 2.1 | 1.04 (0.99–1.10) | 9.5 | 1.29 (1.23–1.36) |
| Obsessive-compulsive | 1276 | 34 | −5.8 | 0.83 (0.77–0.90) | −23.4 | 0.74 (0.68–0.79) | 1373 | 47 | 3.8 | 1.06 (0.98–1.14) | 9.8 | 1.29 (1.20–1.40) |
| Eating | 761 | 21 | −11.9 | 0.78 (0.71–0.86) | −12.1 | 0.84 (0.77–0.93) | 869 | 30 | 6.9 | 1.09 (0.99–1.20) | 11.1 | 1.31 (1.19–1.44) |
| Tic | 263 | 7 | −19.8 | 0.71 (0.60–0.84) | −6.4 | 0.90 (0.76–1.06) | 276 | 9 | 7.4 | 1.10 (0.93–1.30) | 11.3 | 1.31 (1.10–1.56) |
Abbreviations: ED, emergency department; MH, mental health.
The National Syndromic Surveillance Program collects free-text reason for visit (chief complaint), discharge diagnosis, and patient demographic details. Diagnosis information is collected using International Classification of Diseases, Ninth Revision, Clinical Modification codes; International Classification of Diseases, Tenth Revision, Clinical Modification codes; and Systematized Nomenclature of Medicine codes. ED visits associated with any MH-related visit and specific mental disorders were identified by querying ED visits data from the National Syndromic Surveillance Program using keyword syndromes developed by the US Centers for Disease Control and Prevention in partnership with state and local health departments (eTable 1 in the Supplement).
To reduce artifactual effects from changes in reporting patterns, analyses examining trends in MH-related ED visits overall were restricted to facilities with a coefficient of variation of 40 or less and mean weekly discharge diagnosis of 75% or more from January 2019 to August 2021.
Rate of ED visits for MH outcome equaled the number of ED visits for MH outcome in the period of interest divided by the number of total ED visits in the period of interest multiplied by 100 000.
Percentage change in visits was calculated as the difference in total visits between the index period and the comparison period divided by the total visits during the comparison period multiplied by 100.
Visit ratios equaled the proportion of ED visits for MH outcome during the index period divided by the proportion of ED visits for MH outcome during the comparison period.
Across all MH-related visits and many disorders, White and American Indian or Alaska Native persons had a higher prevalence of ED visits for the disorder of interest per 100 000 ED visits than other groups (eg, all MH-related visits: American Indian or Alaska Native persons, 7428; Asian persons, 6406; Black persons, 6318; Hispanic persons, 6026; Native Hawaiian or Other Pacific Islander persons, 4744; White persons, 9792 per 100 000 ED visits) (Table 2, Figures 2 and 3, eAppendixes 1 and 2 in the Supplement). There were also differences between several other racial and ethnic minoritized groups in MH-related ED visits per 100 000 ED visits in the Delta period, which varied by specific disorders (Figures 2 and 3). For example, Black persons had a lower prevalence of anxiety-related ED visits (2481 per 100 000) than Asian persons (3497 per 100 000) and Hispanic persons (3462 per 100 000) (Figure 2B), but a higher prevalence of schizophrenia spectrum disorder-related ED visits (1244 per 100 000) compared with American Indian or Alaska Native (716 per 100 000), Asian (562 per 100 000), Hispanic (524 per 100 000), and White (757 per 100 000) persons (Figure 3B). MH-related ED visits varied over time within racial and ethnic groups (Table 2). Asian persons had a moderate increase (12.0%), and Native Hawaiian or Pacific Islanders had a moderate decrease (−16.0%) in all MH-related visit counts in the Delta period compared with the pre-Delta period; other groups had stable counts over these periods. Black, Hispanic, and White persons had stable ED visit counts for all specific disorders between the Delta and pre-Delta period. Although visit counts were stable for depressive disorders, American Indian or Alaska Native persons had a high decrease in ED visit counts for bipolar (−30.8%), schizophrenia spectrum (−23.8%), and TS-related (−25.0%) disorders—but a moderate increase in anxiety-related ED visits (9.9%)—in the Delta period compared with the pre-Delta period. Asian persons had moderate to high increases in ED visit counts for anxiety disorders (18.3%), depressive disorders (20.5%), schizophrenia spectrum disorders (18.2%), and TS-related disorders (11.8%); visits for bipolar disorders decreased (−13.6%).
Table 2.
Changes in MH-Related ED Visits for Adults Aged 18 to 64 Years During Selected Periods During the COVID-19 Pandemic, by Race and Ethnicity, US, December 27, 2020, to August 14, 2021a,b
| After Delta variant onset, index period: July 18-August 14,2021 | After a COVID-19 case peak, index period: February 14, 2021-March 13, 2021 | |||||||
|---|---|---|---|---|---|---|---|---|
| Index period compared with MH during the COVID-19 pandemic, prior to Delta variant period (April 18-May 15, 2021) | Index period compared with MH during a COVID-19 case peak (December 27, 2020-January 23, 2021) | |||||||
| Race and ethnicity | Total ED visit counts for MH, No. | ED visits for MH per 100 000ED visitsc | Change in ED counts for MH, %d | Visit ratio (95% CI)e | Total ED visit counts for MH, No. | ED visits for MH per 100 000 ED visitsc | Change in ED counts for MH, %d | Visit ratio (95% CI)d |
| All MH | ||||||||
| American Indian orAlaska Native | 218 | 7428 | −8.3 | 0.84 (0.70–1.00) | 241 | 10 871 | 6.2 | 1.14 (0.96–1.35) |
| Asian | 251 | 6406 | 12.0 | 0.98 (0.82–1.16) | 227 | 7809 | 4.0 | 1.15 (0.96–1.37) |
| Black | 3693 | 6318 | 1.7 | 0.89 (0.85–0.93) | 3489 | 8050 | 3.0 | 1.06 (1.01–1.10) |
| Hispanic | 2792 | 6026 | −0.5 | 0.89 (0.84–0.93) | 2783 | 7946 | −0.3 | 1.05 (1.00–1.11) |
| Native Hawaiian or Other Pacific Islander | 25 | 4744 | −16.0 | 0.78 (0.46–1.31) | 31 | 6798 | 0.0 | 0.98 (0.61–1.58) |
| White | 13 226 | 9792 | 2.2 | 0.87 (0.86–0.90) | 12 388 | 12 301 | 2.0 | 1.05 (1.02–1.07) |
| Anxiety disorders | ||||||||
| American Indian or Alaska Native | 121 | 4123 | 9.9 | 1.01 (0.78–1.30) | 118 | 5323 | 5.1 | 1.12 (0.87–1.45) |
| Asian | 137 | 3497 | 18.3 | 1.05 (0.82–1.34) | 113 | 3887 | 8.0 | 1.20 (0.92–1.56) |
| Black | 1450 | 2481 | 1.3 | 0.89 (0.83–0.96) | 1328 | 3064 | 5.0 | 1.08 (1.00–1.16) |
| Hispanic | 1604 | 3462 | −0.9 | 0.88 (0.83–0.95) | 1518 | 4334 | −5.1 | 1.00 (0.94–1.07) |
| Native Hawaiian or Other Pacific Islander | 12 | 2277 | −33.3 | 0.68 (0.32–1.41) | 13 | 2851 | −38.5 | 0.71 (0.35–1.43) |
| White | 7157 | 5299 | 0.4 | 0.86 (0.83–0.89) | 6655 | 6608 | 0.1 | 1.03 (1.00–1.06) |
| Depressive disorders | ||||||||
| American Indian or Alaska Native | 72 | 2453 | −6.9 | 0.85 (0.62–1.17) | 91 | 4105 | 9.9 | 1.18 (0.88–1.59) |
| Asian | 83 | 2118 | 20.5 | 1.08 (0.79–1.49) | 79 | 2718 | 26.6 | 1.50 (1.08–2.10) |
| Black | 1025 | 1754 | −1.1 | 0.87 (0.80–0.95) | 1001 | 2310 | 3.6 | 1.06 (0.97–1.16) |
| Hispanic | 773 | 1668 | −0.9 | 0.88 (0.80–0.98) | 815 | 2327 | 4.1 | 1.10 (1.00–1.21) |
| Native Hawaiian or Other Pacific Islander | NAf | NAf | NAf | NAf | NAf | NAf | NAf | NAf |
| White | 4273 | 3164 | −2.2 | 0.84 (0.80–0.87) | 4386 | 4355 | 4.3 | 1.07 (1.03–1.12) |
| Bipolar disorders | ||||||||
| American Indian or Alaska Native | 13 | 443 | −30.8 | 0.70 (0.34–1.43) | 15 | 677 | 40.0 | 1.78 (0.78–4.05) |
| Asian | 22 | 562 | −13.6 | 0.76 (0.43–1.34) | 22 | 757 | 4.6 | 1.16 (0.64–2.10) |
| Black | 482 | 825 | −3.1 | 0.85 (0.75–0.96) | 477 | 1101 | 4.2 | 1.07 (0.94–1.21) |
| Hispanic | 218 | 471 | −6.0 | 0.84 (0.70–1.01) | 251 | 717 | 24.3 | 1.39 (1.15–1.68) |
| Native Hawaiian or Other Pacific Islander | NAf | NAf | NAf | NAf | NAf | NAf | NAf | NAf |
| White | 1738 | 1287 | 7.1 | 0.92 (0.86–0.99) | 1547 | 1536 | 0.1 | 1.03 (0.96–1.10) |
| Schizophrenia spectrum disorders | ||||||||
| American Indian or Alaska Native | 21 | 716 | −23.8 | 0.73 (0.41–1.30) | 22 | 992 | 0 | 1.07 (0.59–1.92) |
| Asian | 22 | 562 | 18.2 | 1.05 (0.56–1.96) | 19 | 654 | −31.6 | 0.84 (0.46–1.52) |
| Black | 727 | 1244 | 4.7 | 0.92 (0.83–1.02) | 714 | 1647 | −6.0 | 0.97 (0.87–1.07) |
| Hispanic | 243 | 524 | −2.9 | 0.87 (0.73–1.03) | 296 | 845 | 6.4 | 1.13 (0.96–1.33) |
| Native Hawaiian or Other Pacific Islander | NAf | NAf | NAf | NAf | NAf | NAf | NAf | NAf |
| White | 1022 | 757 | 4.5 | 0.90 (0.82–0.98) | 1011 | 1004 | 11.5 | 1.16 (1.06–1.27) |
| Trauma- and stressor-related disorders | ||||||||
| American Indian orAlaska Native | 24 | 818 | −25.0 | 0.73 (0.43–1.24) | 33 | 1488 | 42.4 | 1.85 (1.06–3.25) |
| Asian | 17 | 434 | 11.8 | 0.97 (0.49–1.95) | 10 | 344 | −10.0 | 1.00 (0.43–2.36) |
| Black | 206 | 352 | −5.8 | 0.83 (0.69–1.00) | 214 | 494 | 14.0 | 1.19 (0.98–1.45) |
| Hispanic | 178 | 384 | −7.9 | 0.83 (0.68–1.01) | 184 | 525 | −6.0 | 0.99 (0.81–1.22) |
| Native Hawaiian or Other Pacific Islander | NAf | NAf | NAf | NAf | NAf | NAf | NAf | NAf |
| White | 796 | 589 | −5.5 | 0.81 (0.74–0.89) | 792 | 786 | 6.2 | 1.10 (0.99–1.21) |
Abbreviations: ED, emergency department; MH, mental health; NA, not available.
The National Syndromic Surveillance Program collects free-text reason for visit (chief complaint), discharge diagnosis, and patient demographic details. Diagnosis information is collected using International Classification of Diseases, Ninth Revision, Clinical Modification codes; International Classification of Diseases, Tenth Revision, Clinical Modification codes; and Systematized Nomenclature of Medicine codes. ED visits associated with any MH-related visit and specific mental disorders were identified by querying ED visits data from the National Syndromic Surveillance Program using keyword syndromes developed by the US Centers for Disease Control and Prevention in partnership with state and local health departments (eTable 1 in the Supplement).
To reduce artifactual effects from changes in reporting patterns, analyses examining trends in MH-related ED visits by race and ethnicity were restricted to facilities with a coefficient of variation of 40 or less and mean weekly discharge diagnosis of 75% or more from January to August 2021 and were further limited to facilities with 75% or more complete data for the combined race and ethnicity fields.
Rate of ED visits for MH outcome equaled the number of ED visits for MH outcome in the period of interest divided by the number of total ED visits in the time period of interest for the subpopulation of interest multiplied by 100 000.
Percentage change in visits was calculated as the difference in total visits between the index period and the comparison period divided by the total visits during the comparison period multiplied by 100.
Visit ratios equaled the proportion ED visits for MH outcome during the index period divided by the proportion of ED visits for MH outcome during the comparison period.
If index period ED visits counts for a particular race and ethnicity were less than 10, cell volumes were suppressed and are listed as NA.
Figure 2. Mental Health–Related, Anxiety, and Depressive Disorder US Emergency Department (ED) Visits, by Race and Ethnicity, December 27, 2020, to August 14, 2021.
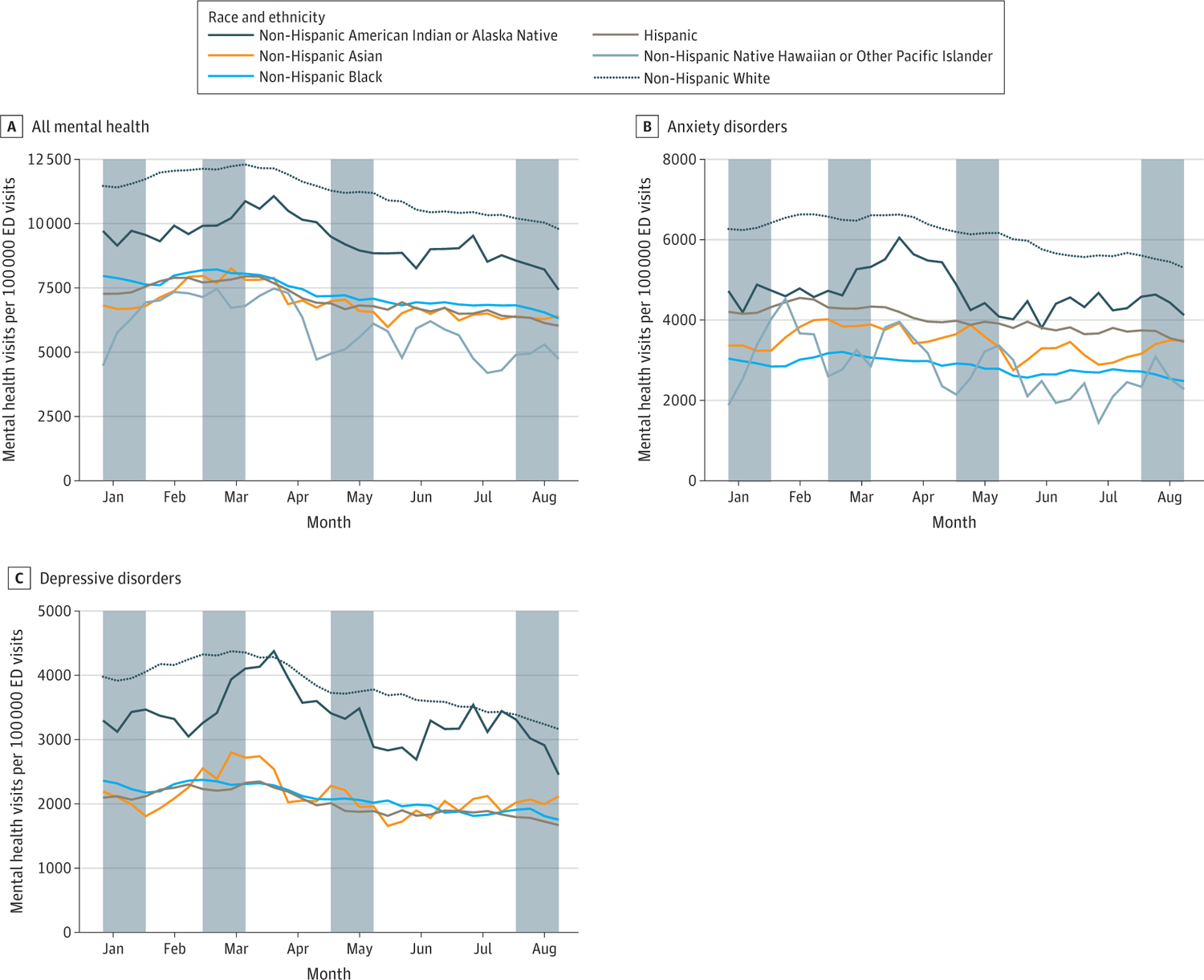
This figure includes data for all mental health (A), anxiety disorders (B), and depressive disorders (C). Shaded areas of the graph depict time periods included in analytic index or comparison periods: a COVID-19 case peak comparison period (December 27, 2020-January 23, 2021), the period immediately after a COVID-19 case peak index period (February 14-March 13, 2021), a COVID-19 pandemic comparison period with low circulation of the Delta variant (the pre-Delta period; April 18-May 15, 2021), and a COVID-19 pandemic index period with high circulation of the Delta variant (the Delta period; July 18-August 14, 2021). These windows were used in the temporal comparisons displayed in Table 2 (eAppendix 1 in the Supplement).
Figure 3. Bipolar, Schizophrenia Spectrum, and Trauma- and Stressor-Related Disorders US Emergency Department (ED) Visits, by Race and Ethnicity, December 27, 2020, to August 14, 2021.
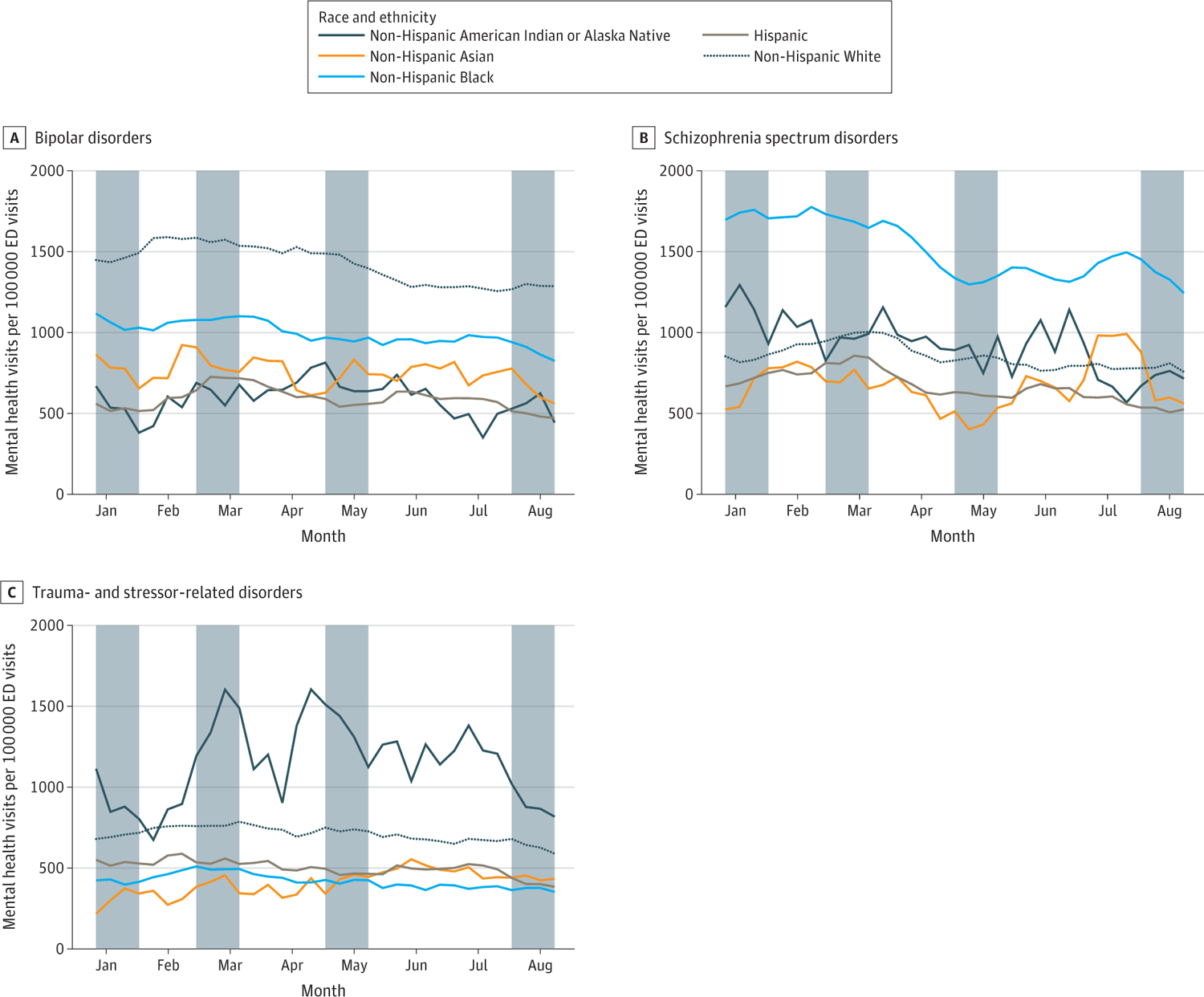
This figure includes data for bipolar disorders (A), schizophrenia spectrum disorders (B), and trauma- and stressor-related disorders (C). Shaded areas of the graph depict time periods included in analytic index or comparison periods: a COVID-19 case peak comparison period (December 27, 2020-January 23, 2021), the period immediately after a COVID-19 case peak index period (February 14-March 13, 2021), a COVID-19 pandemic comparison period with low circulation of the Delta variant (the pre-Delta period; April 18-May 15, 2021), and a COVID-19 pandemic index period with high circulation of the Delta variant (the Delta period; July 18-August 14, 2021). These windows were used in the temporal comparisons displayed in Table 2 (eAppendix 2 in the Supplement).
VRs with 95% CIs, including for some racial and ethnic groups, were mostly less than 1.0 (Tables 1 and 2), indicating MH-related ED visits composed a smaller proportion of all ED visits in the Delta period compared with the pre-Delta period. For American Indian or Alaska Native and Asian persons, VRs and 95% CIs mostly spanned 1.0, indicating no difference in the proportion of MH-related ED visits in the Delta period compared with the pre-Delta period. Findings by sex and for those aged 25 to 49 years and 50 to 64 years mostly reflected nonstratified findings (eTable 2 in the Supplement). For adults aged 18 to 24 years, many disorders had moderate to high decreases in ED visit counts in the Delta period compared with the pre-Delta period.
Changes Immediately After a COVID-19 Case Peak
Among adults aged 18 to 64 years, there was stability in adult MH-related ED visit counts overall (1.5%), including for specific disorders (range, 0.6%–7.4%) after a COVID-19 case peak compared with during a peak (Table 1). Similar to the Delta period findings, there were between-group racial and ethnic differences in ED visit prevalence for all MH-related visits and specific disorders (Figures 2 and 3).
For within-group differences, there was stability in all MH-related ED visit counts during and immediately after a COVID-19 case peak for all specific racial and ethnic subpopulations (range, −0.3% to 6.2%) (Table 2). For Black, Hispanic, and White persons, there was limited variability in ED visit counts for most disorders during this period. However, each of these groups had increases in the percentage change in visit counts for 1 disorder in the period after a COVID-19 case peak compared with during a peak (Black persons, 14.0% increase in TS-related disorder visits; Hispanic persons, 24.3% increase in bipolar disorder visits; White persons, 11.5% increase in schizophrenia spectrum disorder visits) in the period after a COVID-19 case peak. For Asian persons, there was stability in ED visit counts for several disorders, but high increases in depressive disorders (26.6%) and decreases in schizophrenia spectrum disorders (−31.6%) in the period after a COVID-19 case peak. Among American Indian or Alaska Native persons, anxiety and schizophrenia spectrum–related ED visit counts were stable after a COVID-19 case peak, but there were moderate to high increases in ED visit counts for other disorders (depressive disorders, 9.9%; bipolar disorders, 40.0%; TS-related disorders, 42.4%).
For MH-related visits overall and specific disorders, VRs were mostly greater than 1.0 with 95% CIs excluding 1.0 (Tables 1 and 2). This predominantly indicates that MH-related ED visits composed a larger proportion of all ED visits in the period immediately after a COVID-19 case peak compared with during a peak. For some racial and ethnic groups, VR point estimates were similar but with wider CIs that often spanned 1.0, which could be due to small sample size. Findings by age and sex reflected overall patterns, with several exceptions (eTable 2 in the Supplement): there was a moderate increase (10.9%) in eating disorder–related ED visit counts for men; high increases (25.8%) in tic disorder–related ED visit counts for women; and moderate to high increases in visit counts for 3 disorders (disruptive behavioral and impulse disorders, 11.8%; eating disorders, 12.5%, tic disorders, 25.8%) among adults aged 18 to 24 years after a COVID-19 case peak compared with during a peak.
MH-Related ED Visits Compared With Prepandemic
Among adults aged 18 to 64 years, there were decreases for all MH-related ED visit counts (−17.2%) and for most disorders (range, −12.1% to −30.7%) when comparing the Delta period with the corresponding period in 2019, except for tic disorders, which was stable (−6.4%) (Table 1). Across most disorders and all MH-related visits, VRs were mostly less than 1.0 with 95% CIs that excluded 1.0 (Table 1), indicating that MH-related ED visits were a smaller proportion of ED visits in the Delta period compared with the corresponding prepandemic period in 2019. Findings by sex and age mostly reflected nonstratified results (eTable 2 in the Supplement).
For adults aged 18 to 64 years, ED visit counts for all MH-related visits (−5.4%) and for anxiety (−4.2%), bipolar (−8.7%), schizophrenia (5.2%), and TS (−3.9%) disorders were stable when comparing the period after a COVID-19 case peak with the corresponding prepandemic period (Table 1). There were moderate increases in ED visit counts for disruptive behavioral and impulse disorders (9.5%), obsessive-compulsive disorders (9.8%), eating disorders (11.1%), and tic disorders (11.3%), and moderate decreases for 2 disorders (attention-deficit/hyperactivity and depressive disorders), when comparing the period after a COVID-19 case peak with the corresponding prepandemic period. When stratified by sex and age, findings were similar for the most common disorders. However, increases in ED visit counts for obsessive-compulsive disorder were greater for men (18.8%) and particularly for those aged 50 to 64 years (19.2%). For eating and tic disorders, women (eating, 12.7%; tic, 34.1%) and people aged 18 to 24 years (eating, 22.8%; tic, 73.3%) had the greatest increases (eTable 2 in the Supplement). VRs were mostly greater than 1.0 with 95% CIs that excluded 1.0 (Table 1), indicating that MH-related ED visits composed a larger proportion of all ED visits after a COVID-19 case peak compared with the corresponding prepandemic period.
Discussion
The COVID-19 pandemic has had collateral effects on MH1–9; to our knowledge, this epidemiologic cross-sectional study was the first analysis to examine differences in MH-related ED visits in the Delta period and to investigate the association of COVID-19 case surges with MH-related ED visits. Study findings suggest that all MH-related ED visit counts were mostly stable into the Delta period (except among Asian persons who had visit increases and people of Native Hawaiian or Other Pacific Islander race and ethnicity who had visit decreases) compared with a pre-Delta period but had declined since the corresponding prepandemic period. MH-related ED visits compose a smaller proportion of all ED visits in this period compared with earlier in the pandemic and prepandemic period. Given that self-reported MH concerns have increased during the pandemic,1–9 poor MH may be untreated or undertreated. Although it is possible that increases in primary care telemedicine use24–26 or other services may be offsetting some decreases in MH-related ED visits during these periods, these resources may be less available to disproportionately affected subpopulations27—such as racial and ethnic minoritized groups—who have historically been more likely to use EDs as first-line health care.19,20 Given the effect poor MH can have on life-long health,28 access to flexible MH services tailored to individual needs and accounting for differences in service access and availability are critical.
Study findings suggest that MH-related ED visit counts were mostly stable when comparing the period after a COVID-19 case peak with during a peak; some exceptions included adults aged 18 to 24 years. Compared with the prepandemic period, there were increases in ED visit counts for 4 disorders, decreases for 2 disorders, and stability for the remaining disorders and all MH-related visits. When accounting for ED visit volume,29,30 our results indicated that MH-related visits composed a larger proportion of ED visits after COVID-19 peaks compared with the corresponding prepandemic period. This aligns with previous work examining MH-related ED visits in 2020, which indicated that MH-related visits accounted for a higher proportion of visits than during the prepandemic period.10 Increases in MH-related ED visit counts after a COVID-19 case peak were notable for several racial and ethnic minoritized groups, including American Indian or Alaska Native persons. The increases observed after a COVID-19 case peak may suggest that individuals are experiencing stress and increases in poor MH in the periods after a COVID-19 case surge, as witnessed after a public health crisis.31–33 Alternatively, individuals may be delaying MH care during COVID-19 peaks owing to limited accessibility or perceived safety of services,34 or care may be unavailable given reduced capacity. After a COVID-19 case peak, hospitals may need to prepare for a potential increase in MH care in emergency health care settings.
Study results showed variation in patterns for MH care-seeking, which change based on the time of the pandemic, both in ED visits within and across racial and ethnic groups. This highlights the need to support persons who have used EDs as a safety net during the prepandemic period.19,20 The variation in MH-related ED visits, including across specific disorders, by racial and ethnic group subpopulation suggests that communication and advocacy interventions may need to be tailored for groups who are experiencing increases in poor MH during the pandemic. Within-group variability of MH-related ED visits during the pandemic suggests the need for attention from clinicians related to continuity of care for those with preexisting MH problems. Focus on proactive and preventive care for racial and ethnic groups more likely to experience new MH needs during the pandemic may be warranted. Race and ethnicity are related to inequities in hospital care and mortality, and stigmatizing experiences and other factors that lead to mistrust.35,36 Primary prevention efforts are needed to maintain mental and physical health, sustain community resilience, and overcome additive stress owing to the COVID-19 pandemic.
Limitations
This study had some limitations. Although NSSP data represent approximately 71% of US ED facilities, these data are not nationally representative. After limiting our study to facilities that reported high-quality data, results may not be generalizable to all NSSP-contributing facilities. ED visit counts should be considered an underestimate of MH-related disorders that are identified in ED visit records, given that these data do not include all US EDs. There were substantial changes in ED health care–seeking behavior during the pandemic,29,30 which may have affected results as the characteristics of persons seeking care before and during the pandemic may have changed. Although all examined MH definitions were validated on NSSP data from multiple US jurisdictions, there may have been misclassification owing to challenges with identifying and reporting MH-related visits. We could not distinguish between acute and chronic presentation of MH-related visits, or visits where MH was a comorbidity but not the primary reason for the visit. Estimates provided do not capture all health care–seeking needs for persons experiencing MH challenges given that many people receive MH care outside of EDs. Moreover, this analysis focused on MH and did not include suicide or other behavioral health–related outcomes, which are critical and should be examined in future research. Finally, there may have been misclassification in race and ethnicity, which could influence estimates of inequities in MH-related ED visit burden.
Conclusions
This epidemiologic cross-sectional study described changes in MH-related ED visits into the Delta variant pandemic period and during and after peaks in US COVID-19 cases. The findings suggest that there were fluctuations in patterns of MH-related ED visits relative to COVID-19 case surges, which differed by race and ethnicity. Emergency health care professionals may experience increases in MH-related visits during COVID-19 case surges (such as during the Delta period) among Asian persons and after COVID-19 case surges, particularly for adults aged 18 to 24 years and for American Indian or Alaska Native persons. There may also be increases in visits for specific disorders for individual racial and ethnic groups. Public health practitioners should consider subpopulation-specific messaging and programmatic strategies that address differences in MH prevention and intervention needs across subpopulations, particularly those who have been marginalized in the US.
Supplementary Material
Key Points.
Question
How have adult mental health (MH)–related emergency department (ED) visits changed during the COVID-19 pandemic?
Findings
In this cross-sectional study of 107 761 319 eligible ED visits, MH-related visit count findings depended on the COVID-19 pandemic period examined, whether this was compared with other periods in the pandemic or prepandemic period, and which mental disorder was examined. There was between- and within-group variation in ED visits by race and ethnicity, which varied by pandemic period examined, and there were increases in some disorders after COVID-19 case peaks for adults aged 18 to 24 years.
Meaning
Results of this study suggest that EDs may have increases in MH-related visits after COVID-19 surges, especially for young adults and some racial and ethnic minoritized subpopulations.
Footnotes
Conflict of Interest Disclosures: None reported.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Contributor Information
Kayla N. Anderson, National Center for Injury Prevention and Control, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Lakshmi Radhakrishnan, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Rashon I. Lane, National Center for Chronic Disease Prevention and Health Promotion, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Michael Sheppard, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Jourdan DeVies, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia; Oak Ridge Institute for Science and Education, Oak Ridge, Tennessee.
Roseric Azondekon, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Amanda R. Smith, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia; Epidemic Intelligence Service, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Rebecca H. Bitsko, National Center on Birth Defects and Developmental Disabilities, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Kathleen P. Hartnett, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Barbara Lopes-Cardozo, Center for Global Health, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Rebecca T. Leeb, National Center on Birth Defects and Developmental Disabilities, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Katharina L. van Santen, ICF International, Atlanta, Georgia.
Kelly Carey, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Sophia Crossen, InductiveHealth Informatics, Ottawa, Kansas.
Taylor P. Dias, Deloitte, Atlanta, Georgia.
Sam Wotiz, Deloitte, Atlanta, Georgia.
Jennifer Adjemian, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Loren Rodgers, Center for Surveillance, Epidemiology, and Laboratory Services, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Rashid Njai, Office of Minority Health and Health Equity, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Craig Thomas, National Center for Chronic Disease Prevention and Health Promotion, US Centers for Disease Control and Prevention, Atlanta, Georgia.
REFERENCES
- 1.Aknin LB, De Neve J-E, Dunn EW, et al. Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspect Psychol Science. Published online January 19, 2022. doi: 10.1177/17456916211029964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201–211. doi: 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Czeisler ME, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czeisler ME, Lane RI, Wiley JF, Czeisler CA, Howard ME, Rajaratnam SMW. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Netw Open. 2021;4(2):e2037665. doi: 10.1001/jamanetworkopen.2020.37665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKnight-Eily LR, Okoro CA, Strine TW, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70(5): 162–166. doi: 10.15585/mmwr.mm7005a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mataix-Cols D, Ringberg H, Fernández de la Cruz L. Perceived worsening of tics in adult patients with Tourette syndrome after the COVID-19 outbreak. Mov Disord Clin Pract. 2020;7(6):725–726. doi: 10.1002/mdc3.13004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020-February 2021. MMWR Morb Mortal Wkly Rep. 2021;70(13):490–494. doi: 10.15585/mmwr.mm7013e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henssler J, Stock F, van Bohemen J, Walter H, Heinz A, Brandt L. Mental health effects of infection containment strategies: quarantine and isolation–a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2021;271(2):223–234. doi: 10.1007/s00406-020-01196-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith AR, DeVies J, Caruso E, et al. Emergency department visits for COVID-19 by race and ethnicity—13 states, October–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(15):566–569. doi: 10.15585/mmwr.mm7015e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gold JAW, Rossen LM, Ahmad FB, et al. Race, ethnicity, and age trends in persons who died from COVID-19—United States, May-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1517–1521. doi: 10.15585/mmwr.mm6942e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with COVID-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Dyke ME, Mendoza MCB, Li W, et al. Racial and ethnic disparities in COVID-19 incidence by age, sex, and period among persons aged <25 years—16 US jurisdictions, January 1-December 31, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(11):382–388. doi: 10.15585/mmwr.mm7011e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bailey ZD, Moon JR. Racism and the political economy of COVID-19: will we continue to resurrect the past? J Health Polit Policy Law. 2020;45(6): 937–950. doi: 10.1215/03616878-8641481 [DOI] [PubMed] [Google Scholar]
- 16.Cheah CSL, Wang C, Ren H, Zong X, Cho HS, Xue X. COVID-19 racism and mental health in Chinese American families. Pediatrics. 2020;146(5): e2020021816. doi: 10.1542/peds.2020-021816 [DOI] [PubMed] [Google Scholar]
- 17.Wu C, Qian Y, Wilkes R. Anti-Asian discrimination and the Asian-White mental health gap during COVID-19. Ethn Racial Stud. 2021;44(5): 819–835. doi: 10.1080/01419870.2020.1851739 [DOI] [Google Scholar]
- 18.Curtis DS, Washburn T, Lee H, et al. Highly public anti-Black violence is associated with poor mental health days for Black Americans. Proc Natl Acad Sci U S A. 2021;118(17):e2019624118. doi: 10.1073/pnas.2019624118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown LE, Burton R, Hixon B, et al. Factors influencing emergency department preference for access to health care. West J Emerg Med. 2012;13 (5):410–415. doi: 10.5811/westjem.2011.11.6820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parast L, Mathews M, Martino S, Lehrman WG, Stark D, Elliott MN. Racial/ethnic differences in emergency department utilization and experience. J Gen Intern Med. 2022;37(1):49–56. doi: 10.1007/s11606-021-06738-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Centers for Disease Control and Prevention. NSSP facility participation by US county. Accessed September 9, 2021. https://www.cdc.gov/nssp/participation-coverage-map.html
- 22.US Centers for Disease Control and Prevention. COVID data tracker. Accessed September 9, 2021. https://covid.cdc.gov/covid-data-tracker/#cases_casesper100k
- 23.US Centers for Disease Control and Prevention. Variant proportions. Accessed September 9, 2021. https://covid.cdc.gov/covid-data-tracker/#variant-proportions
- 24.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181(3):388–391. doi: 10.1001/jamainternmed.2020.5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mansour O, Tajanlangit M, Heyward J, Mojtabai R, Alexander GC. Telemedicine and office-based care for behavioral and psychiatric conditions during the COVID-19 pandemic in the United States. Ann Intern Med. 2021;174(3):428–430. doi: 10.7326/M20-6243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhai Y A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom. 2021; 90(1):64–66. doi: 10.1159/000509000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Mental health action plan, 2013–2020. Accessed September 9, 2021. https://www.who.int/publications/i/item/9789241506021
- 29.Hartnett KP, Kite-Powell A, DeVies J, et al. ; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adjemian J, Hartnett KP, Kite-Powell A, et al. Update: COVID-19 pandemic-associated changes in emergency department visits—United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(15):552–556. doi: 10.15585/mmwr.mm7015a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jalloh MF, Li W, Bunnell RE, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018;3(2):e000471. doi: 10.1136/bmjgh-2017-000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Aida J, Hikichi H, Kondo K, Kawachi I. Association of postdisaster depression and posttraumatic stress disorder with mortality among older disaster survivors of the 2011 great East Japan earthquake and tsunami. JAMA Netw Open. 2019;2 (12):e1917550. doi: 10.1001/jamanetworkopen.2019.17550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shear MK, McLaughlin KA, Ghesquiere A, Gruber MJ, Sampson NA, Kessler RC. Complicated grief associated with Hurricane Katrina. Depress Anxiety. 2011;28(8):648–657. doi: 10.1002/da.20865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36): 1250–1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang X, Carabello M, Hill T, Bell SA, Stephenson R, Mahajan P. Trends of racial/ethnic differences in emergency department care outcomes among adults in the United States from 2005 to 2016. Front Med (Lausanne). 2020;7:300. doi: 10.3389/fmed.2020.00300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang X, Carabello M, Hill T, He K, Friese CR, Mahajan P. Racial and ethnic disparities in emergency department care and health outcomes among children in the United States. Front Pediatr. 2019;7:525. doi: 10.3389/fped.2019.00525 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


