Abstract
Objective:
To examine associations of school food availability with student intake frequency and BMI, and whether the number of neighborhood food outlets modifies these associations.
Design:
Baseline assessment of a nationally representative cohort study of U.S. 10th graders. Students reported intake frequency of fruits and vegetables (FV), snacks, and soda. BMI was calculated from measured height and weight. Administrators of 72 high schools reported the frequency of school availability of FV, snacks, and soda. The number of food outlets within 1 km and 5 km were linked with geocoded school addresses. Data were analyzed using adjusted linear and logistic mixed models with multiple imputation for missing data.
Setting:
U.S. 2009–2010.
Participants:
2,263 U.S. 10th graders from the Next Generation Health Study (NEXT).
Results:
Greater school FV availability was positively associated with student FV intake. Food outlets within 5 km of schools (but not 1 km) attenuated the association of school FV availability with student intake; this was no longer significant at schools with >58 food outlets within 5 km. School food availability was not associated with student BMI or student snack or soda intake.
Conclusions:
School food availability was associated with student intake of FV, but not with snacks, soda, or BMI. Attenuation of the observed associations by the school neighborhood food environment indicates a need to find ways to support healthy student eating behaviors in neighborhoods with higher food outlet density.
Keywords: School food availability, food environment, food outlets, adolescents, body mass index, food intake
INTRODUCTION
One fifth of U.S. children and adolescents aged 12–19 are obese (1) and few meet national dietary guidelines for a healthy diet (2). Obesity in adolescence is associated with increased risk of adult obesity (3) and related adverse health outcomes including type 2 diabetes, cardiovascular disease, and premature death (4). Strategies targeting behavioral change to prevent obesity in childhood and adolescence often fail in food environments that promote high energy intake and sedentary behavior (5). The internal school food environment (e.g., school lunches and competitive foods available within schools) has frequently been targeted for improving youth diet and weight outcomes. Youths consume over one-third of their daily food in school (6), and students who eat both breakfast and lunch at school consume close to 50% of their total intake at school (7). Additionally, the external school food environment (i.e., foods available in the school’s surrounding neighborhood) becomes increasingly relevant for high schoolers, who have increased autonomy over food decisions and may be less constrained to the internal school food environment than middle schoolers (8).
Policies impacting the provision, restriction, and nutrient content of school lunches and competitive foods and beverages (i.e., foods and beverages offered outside of school meal programs) in middle and high schools are associated with lower intake of restricted foods and beverages (e.g., lower salty snack and soda intake) (9–16), although evidence suggests that students compensate by acquiring restricted foods from alternative sources (17) or consuming greater amounts of unrestricted foods of lower nutritional value while in school (10). Additionally, school policies restricting competitive foods sometimes allow schools to replace restricted foods with similar foods lacking nutritional value (e.g., regular potato chips vs. baked) and fail to require healthier alternatives (e.g., vegetables and whole grains) (13). The effects of these school nutrition policies on body mass index (BMI, kg/m2) have been mixed. Stricter policies have been associated with improved weight status among 10–19 year-olds (9, 18–20); in contrast, associations of stricter nutrition policies with greater odds of overweight and obesity were observed in elementary and middle school students (21, 22), while null associations have been observed in high school students (21, 23) and middle school students (24).
Evidence suggests the internal school food environment may have a smaller impact on diets and weight outcomes of high school students than of those in younger grades (16, 23) due in part to greater influence of the external school food environment (25). High school students have access to neighborhood food outlets (e.g., restaurants, grocery stores, convenience stores and gas stations) before and after school and are often permitted to leave campus during lunch (25). Additionally, data indicate that businesses, including fast food restaurants, are more frequently located within close proximity to high schools than elementary or middle schools (25), and that closer proximity and higher density of food outlets (primarily fast food restaurants and convenience stores) in school and home neighborhoods are associated with less healthy food intake (26–28) and higher BMI (26, 28) in middle and high school students. However, other studies have found null associations of neighborhood food environments with youth diet and weight outcomes (26, 27, 29). Furthermore, few studies have examined associations of the external school food environment with BMI in high school students (28–30), and none have concurrently examined the internal and external food environment. As such, it is unknown whether the external school food environment modifies the relationship of the internal school food environment with student diet and weight outcomes. Thus, the purpose of this study is to investigate whether the neighborhood food environment modifies the association of school food availability with student dietary intake and BMI. We hypothesized that more food outlets in the external school food environment would weaken associations of the internal school food environment with student intake and BMI.
METHODS
Study design
Data come from the baseline assessment of the Next Generation Health Study (NEXT), a nationally representative cohort study of 10th graders enrolled during the 2009–2010 school year and assessed annually for 7 years (n = 2,783). The primary sampling units were school districts stratified across the nine U.S. Census divisions; 81 of 137 schools (public and private) randomly selected agreed to participate, and classrooms from among core subject matter classes within these schools were randomly selected for inclusion. Schools were located in twenty-two states, with at least two states from each census division included. Additional study details are available elsewhere (31). Of the 81 schools included in NEXT, 72 reported on school food availability (n=2,263) and therefore were included in this analysis. Schools with large percentages of African-American students were oversampled to provide reliable estimates for this subgroup; a sufficient number of Hispanic students were obtained to provide reliable subgroup estimates without oversampling. While neighborhood characteristics of schools reporting on food availability were not different from the NEXT full sample, the proportions of white and black students were slightly higher and lower, respectively, in the analytic sample than in the NEXT full sample; there were no other demographic differences (Supplementary Table 1). Students completed self-administered surveys annually and school administrators completed a self-administered survey at baseline (wave 1). All data used in this paper come from wave 1, except for wave 2 intake frequency of sweet and salty snacks (data not available at baseline). Parents provided written informed consent for their child and students provided assent (if <18 years of age) and consent (if ≥ 18 years of age). Study protocol was approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Measures
Anthropometric and Demographic Data.
Students self-reported race/ethnicity (categorized as white, black, Hispanic, and other) and gender (male/female); age was calculated based on birthdate reported by parents during the consent process. Family affluence was calculated using the Family Affluence Scale, a validated indicator of family wealth based on participant responses to questions regarding their household car and computer ownership, family vacation, and bedroom sharing (32). A categorical, composite Family Affluence Scale score was used for analysis, with scores 0–2 indicating low, 3–5 middle, and 6–9 high affluence (33). Parent education was reported by the parent completing the consent process and was categorized as high school/GED or less, some college/technical school/associate’s degree, and bachelor’s degree or higher. In two-parent families, the higher parent education was used. Height and weight were measured by trained study staff and were recorded to the nearest 0.1 cm and 0.1 kg, respectively. Measured height and weight were used to calculate BMI. Where BMI was missing at wave 1, BMI at wave 2 was used (from n=118 missing at wave 1, n=29 were available at wave 2). BMI was previously shown to be fairly consistent across waves (34).
School Food Availability.
School administrators completed a survey, including the question, “Can students purchase any of the following items [fruits, vegetables, 100% fruit juice, chocolate candy, other candy, regular salty snacks, low-fat salty snacks, regular sweet snacks, low-fat sweet snacks, soda] from school vending machines or at the school store, cafeteria, or snack bar?” with response options of no, yes-some days, and yes-daily. Responses to availability of fruits, vegetables, and 100% fruit juice were each scored as 0= no days, 1= some days, 2= daily. Overall school fruit and vegetable (FV) availability was calculated by summing the frequency of the availability of each of these items, and ranged from 0 (no fruits, vegetables, or 100% fruit juice offered any day) to 6 (fruits, vegetables, and 100% fruit juice offered daily). Responses to snack items were categorized as chocolate and candy (chocolate + other candy), salty snacks (low-fat + regular salty snacks), and sweet snacks (low-fat + regular sweet snacks), each of which was scored according to the most frequently available snack in each category as 0= no days, 1= some days, 2= daily. Overall school snack availability was calculated by summing the frequency of the availability of each snack category, and ranged from 0 (no snacks offered any day) to 6 (snacks from all categories offered daily). Soda availability was based on the original three response options for this item: 0= no days, 1= some days, 2= daily.
External School Food Environment (Food Outlets).
Food outlet counts within 1 km and 5 km were obtained from business location data provided by Dun & Bradstreet (www.dnb.com) and linked with the school geocoded addresses. These distances correspond to a 10–15 minute walk (1 km) and a 5–10 minute drive (5 km), respectively, representing distances that may be reasonably reached by students before, during, or after school (35, 36). Fast food outlets (chain and independent), full-service restaurants, convenience stores, and grocery stores/supermarkets were summed to calculate the total number of food outlets (hereinafter, all food outlets). Analyses by food outlet category were examined individually for these four outlet types.
Other school neighborhood measures.
Population density and poverty rate by census block were obtained from the 2010 US Census and American Community Survey (37). Census blocks are delineated by the US Census Bureau and are defined as neighborhood areas bounded by visible and non-visible features, such as roads, streams, and county limits and are the basis for all tabulated data (38). Geographic information system data were used to calculate land use mix scores ranging from 0–1 that describe the diversity of land use by ZIP code tabulation area of schools. Scores of 0 and 1 represent the most homogeneous and most diverse land use, respectively (39).
Student food group intake frequency.
Student food group intake frequency was assessed using questions based on the Youth Risk Behavior Surveillance System (40) and the multinational Health Behaviour in School-Aged Children study (41). Participants were asked, “During the past 7 days, how many times did you eat or drink [sweet and salty snacks (assessed at wave 2), soda, and fruits and vegetables]?” Responses ranged from never to 4 or more times per day. FV intake frequency was calculated by summing responses to 100% fruit juices, fruit, green salad, carrots, and other vegetables. Responses for all food groups were converted to number of times per day. Due to low intake frequency of snacks and soda resulting in a right-skewed distribution, variables for intake of these food groups were dichotomized as less than 1 time per day and greater or equal to 1 time per day.
Analysis
Multiple imputation by chained equations was used to impute missing values under the assumption of missing at random. Missing values were present for gender (n=4, 0.2%), age (n=15, 0.7%), BMI (n=89, 3.9%), race/ethnicity (n=8, 0.4%), parental education (n=139, 6.1%), soda intake (n=29, 1.3%), and snack intake (n=309, 13.7%). Using R package “mice”, 50 imputed datasets were generated and imputed values for missing variables were derived from their estimated distribution conditional on other variables. Analyses were repeated per imputed dataset and estimates were combined by Rubin’s rule (42).
School and student characteristics were summarized using frequency and percent, and mean and standard error for categorical and continuous values, respectively. Due to the skewed distribution, the median and interquartile range (IQR) of food outlets were reported. Separate models examined the total number of food outlets within 1 km and 5 km of schools to assess whether the school neighborhood food environment modified the association of school food and drink availability with student BMI and food group intake frequency. For models indicating a statistically significant interaction, regions of significance and interaction plots further examined the interaction, and additional analyses examined food outlet categories separately (fast food outlets, full-service restaurants, convenience stores, and grocery stores/supermarkets). Linear mixed models were used to examine the association of school food and drink availability (FV, snacks, and soda) with student BMI and to examine the association of school FV availability with student FV intake. Logistic mixed models were used to examine associations of school snack and soda availability with student snack and soda intake frequency. All models included sample weight to account for survey design and random intercepts for schools to account for clustering within schools. All models adjusted for student race/ethnicity, family affluence, and highest parent education, as well as school neighborhood land use mix, population density, and poverty rate. Adjustment variables were selected based on literature; bivariate correlations were examined to avoid multicollinearity and bivariate associations were examined for dependent variables and demographic characteristics (Supplementary Table 2). The Johnson-Neyman technique was applied using R package “interactions” to probe significant interactions and determine regions of significance (43), identifying for which values of the moderator (number of food outlets) significance held. However, a limitation of this approach is that statistical significance at higher levels of the moderator may occur as an artifact of the analysis. All analyses were performed in R (Version 4.0.1, R Foundation for Statistical Computing, Vienna, Austria) and interaction plots were generated with SAS (Version 9.4, Enterprise Guide 7.1, SAS Institute Inc., Cary, NC, USA).
RESULTS
Of the 81 schools included in NEXT, 72 reported on school food availability (n=2,263 students). Participants were on average 16 years old (ranging from 14 to 20; 98% were between 15 and 17), approximately half female, and approximately 40% racial/ethnic minority. Family affluence and parent education were well distributed across the three categories of each variable (Table 1).
TABLE 1:
Individual and school neighborhood characteristics
| Sample and school characteristics | ||
|---|---|---|
| Students (n= 2,263) | ||
| Age (years) | 16.26 ± 0.01 | |
| Gender (% female) | 54.25 (1.66) | |
| BMI (measured) | 24.78 ± 0.13 | |
| Race/Ethnicity (%) | ||
| White | 59.23 (1.62) | |
| Black | 16.07 (1.14) | |
| Hispanic | 19.61 (1.30) | |
| Other | 5.09 (0.77) | |
| Parent Education (%) | ||
| High school, GED, or less | 33.69 (1.58) | |
| Some college/tech school/Associates | 39.48 (1.67) | |
| Bachelor’s degree or higher | 26.83 (1.50) | |
| Family affluence (%) | ||
| Low affluence | 24.04 (1.36) | |
| Moderate affluence | 48.76 (1.66) | |
| High affluence | 27.20 (1.53) | |
| FV intake (times/day) | 3.90 ± 0.08 | |
| Snack intake, times/day (%) | ||
| < 1 | 54.35 (1.73) | |
| ≥ 1 | 45.65 (1.73) | |
| Soda intake, times/day (%) | ||
| < 1 | 61.11 (1.62) | |
| ≥ 1 | 38.89 (1.62) | |
| Schools (n=72) | ||
| Neighborhood land use mix1 | 0.45 ± 0.04 | |
| Neighborhood population density (per square mile) | 7,213.08 ± 2,335.58 | |
| Neighborhood poverty rate2 | 35.07 ± 2.51 | |
| School FV availability score (%) | 4.07 ± 0.24 | |
| 0 (no days) | 6.94 (3.02) | |
| 1–2 | 26.39 (5.23) | |
| 3–5 | 20.84 (4.82) | |
| 6 (all components daily) | 45.83 (5.91) | |
| School snack availability score (%) | 3.61 ± 0.24 | |
| 0 (no days) | 11.11 (3.73) | |
| 1–2 | 20.84 (4.82) | |
| 3–5 | 37.50 (5.75) | |
| 6 (all components daily) | 30.56 (5.47) | |
| School soda availability score (%) | 1.06 ± 0.11 | |
| 0 (no days) | 41.67 (5.85) | |
| 1 (some days) | 11.11 (3.73) | |
| 2 (daily) | 47.22 (5.92) | |
| Neighborhood food outlets within 1 km, median (IQR) and range | ||
| All food outlets | 2 (0 – 12) | 0 – 335 |
| Fast food restaurants | 0 (0 – 2) | 0 – 20 |
| Full-service restaurants | 1 (0 – 4.5) | 0 – 234 |
| Convenience stores | 0 (0 – 1) | 0 – 16 |
| Supermarkets/grocery stores | 1 (0 – 4) | 0 – 92 |
| Neighborhood food outlets within 5 km, median (IQR) and range | ||
| All food outlets | 13.5 (5 – 242.5) | 0 – 2,828 |
| Fast food restaurants | 4.5 (0.5 – 32.5) | 0 – 154 |
| Full-service restaurants | 6.5 (1 – 112) | 0 – 1,831 |
| Convenience stores | 2 (0 – 13.5) | 0 – 129 |
| Supermarkets/grocery stores | 4 (1 – 66.5) | 0 – 974 |
Values are mean or % (SE), or median (IQR) and range.
Weighted means and percentages are reported for all student-level variables.
FV, Fruit and vegetable.
Snack intake measured at wave 2; all others measured at wave 1 (baseline).
A score of 0–1 measured the diversity of land use in schools’ ZIP code tabulation area with 0 representing the most homogeneous land use and 1 representing the most diverse land use.
Percent of the population with income of less than 185% of the Federal Poverty Level.
Approximately half of schools offered fruits, 100% fruit juice, and vegetables daily, nearly one-third offered snacks from each category (chocolate and candy, salty snacks, sweet snacks) daily, and nearly half offered soda daily (Table 1). On average, students reported eating FV approximately 4 times/day, and a majority reported drinking soda or eating snacks < 1 time/day. Schools had a median of 2 (IQR: 0–12) food outlets within 1 km and almost 14 (IQR: 5 – 242.5) within 5 km. Schools with the highest numbers of food outlets within 5 km (>1000 food outlets) were deemed plausible; these schools (n=4) were all in highly urbanized areas of New York, with land use mix scores above the median. Analyses excluding these schools did not change the findings (results not shown).
School food availability and student intake: all school neighborhood food outlets
In models investigating all school neighborhood food outlets within a 1 km radius, school FV availability was positively associated with student FV intake (β: 0.15; 95% CI: 0.002, 0.29) meaning that for every one unit increase in school FV availability students ate fruits and vegetables 0.15 more times per day. The number of food outlets within 1 km was not associated with student FV intake, and there was no interaction of food outlets with school FV availability (Table 2). In models investigating food outlets within a 5 km radius, school FV availability and food outlets were both positively associated with student FV intake (β: 0.17; 95% CI: 0.02, 0.31), and food outlets attenuated the positive association of school FV availability with student FV intake (Figure 1A). Regions of significance showed that the positive association of school FV availability with student FV intake occurred at schools with less than 59 and with over 1990 food outlets within 5 km (Figure 1B). In schools with 59–1990 food outlets within 5 km, school FV availability was not associated with intake. School availability of snacks and soda was not associated with intake.
TABLE 2:
Model estimates of the associations of school food and drink availability (frequency), the school neighborhood food environment (count of total food outlets within 1 km and 5 km), and their interaction with corresponding student intake frequency (times/day) of fruits and vegetables (FV), snacks, and soda
| FV intake (times/day) | Snacks intake (≥1 time/day)1 | Soda intake (≥1 time/day) | |
|---|---|---|---|
| Independent variables | β (95% Cl) | OR (95% CI) | OR (95% CI) |
| Model 1: 1 km school food environment | |||
| School availability2 | 0.15 (0.002, 0.29) * | 1.01 (0.94, 1.08) | 1.03 (0.87, 1.22) |
| All food outlets | 0.02 (−0.02, 0.07) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| School availability*All food outlets | −0.004 (−0.01, 0.002) | 1.00 (1.00, 1.01) | 1.00 (0.99, 1.01) |
| Model 2: 5 km school food environment | |||
| School availability | 0.17 (0.02, 0.31) * | 1.02 (0.95, 1.09) | 1.04 (0.88, 1.23) |
| All food outlets | 0.002 (0.0002, 0.004) * | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| School availability*All food outlets | −0.0004 (−0.001, −0.0001) * | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.01) |
Snack intake measured at wave 2; all others measured at wave 1 (baseline).
School availability of the food group corresponding to the outcome variable (e.g., school fruit and vegetable availability with student fruit and vegetable intake frequency). FV availability score ranges from 0 (no fruits, vegetables or 100% fruit juice offered any day) to 6 (fruits, vegetables and 100% fruit juice offered every day); snacks availability score ranges from 0 (no chocolate and candy, salty snacks or sweet snacks offered any day) to 6 (chocolate and candy, salty snacks and sweet snacks offered every day); soda availability score ranges from 0 (no soda offered any day) to 2 (soda offered every day).
Linear (FV intake) and logistic (snack and soda intake) mixed models were used to calculate estimates.
Models adjusted for race/ethnicity (ref=white), parent education (ref=high school or less), family affluence (ref=low affluence), neighborhood land use mix, neighborhood population density, and neighborhood poverty rate.
p < 0.05
FIGURE 1A:

Interaction plot showing simple slopes of the regression of school FV availability on student FV intake at different levels of all food outlets within a 5 km radius of schools. Solid lines indicate that the slopes are within the regions of significance (p < 0.05) presented in Figure 1B, while dashed lines indicate the slopes are outside of the regions of significance (p ≥ 0.05) presented in Figure 1B.
FIGURE 1B:
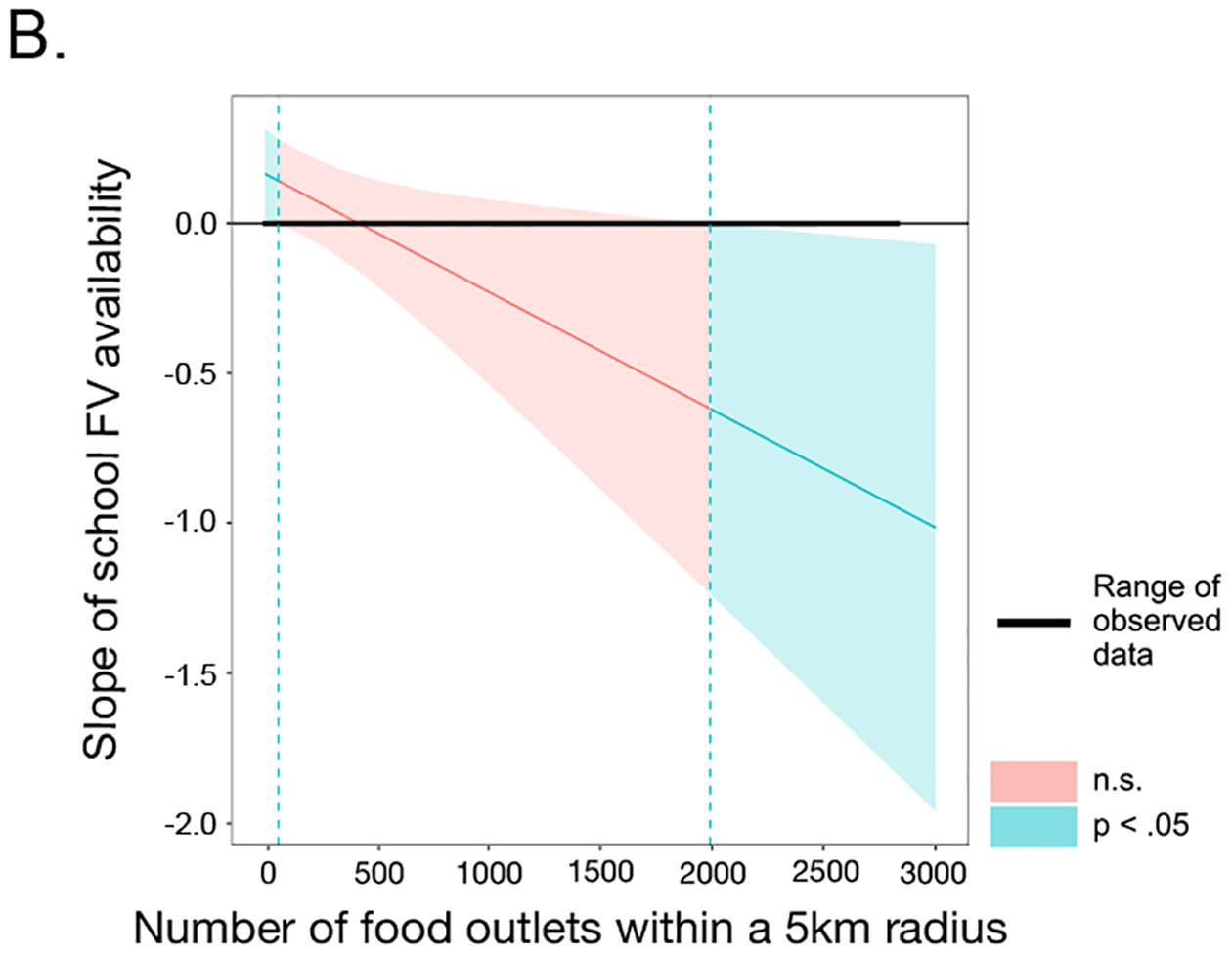
Johnson-Neyman regions of significance and confidence bands (95% CI) for the conditional relation between school FV availability and student FV intake as a function of all food outlets within 5 km of schools. Blue shaded areas reflect regions of significance ([0,58.9] and [>1990.2]) and the bold horizontal line indicates the range of observed food outlets in the sample data [0,2828]. When the number of food outlets is between 0 and 58 and 1991 and higher, the slope of school FV availability is p < 0.05.
School availability and student intake of FV: food outlet categories
Fast food outlets.
Fast food outlets within 1 km were positively associated with student FV intake (β: 0.33; 95% CI: 0.03, 0.63) (Table 3), but attenuated the positive association between school availability and student intake (Supplementary Figure 1A). Regions of significance showed that the positive association of school FV availability with student FV intake was observed at schools with 0 and with over 10 fast food outlets (but not 1–10 outlets) within 1 km (Supplementary Figure 1B). Similarly, fast food outlets within a 5 km radius were positively associated with student FV intake (β: 0.05; 95% CI: 0.02, 0.08) (Table 3) and attenuated the positive association of school FV availability with student FV intake (Supplementary Figure 1C). Regions of significance showed that this relationship was observed at schools with less than 12 and with over 52 fast food outlets within 5 km, but not at schools with 12–52 fast food outlets within 5 km (Supplementary Figure 1D).
TABLE 3:
Model estimates of the associations of school FV availability (frequency), the school neighborhood food environment (count of food outlets within 1 km and 5 km) by food outlet categories, and their interaction with student FV intake frequency (times/day)
| Food outlet category | ||||
|---|---|---|---|---|
| Fast food outlets | Full-service restaurants | Convenience stores | Grocery stores/Supermarkets | |
| FV intake (times/day) | ||||
| Independent variables | β (95% Cl) | β (95% Cl) | β (95% Cl) | β (95% Cl) |
| Model 1: 1 km school food environment | ||||
| School FV availability1 | 0.16 (0.01, 0.31) * | 0.15 (0.003, 0.29) * | 0.14 (−0.002, 0.29) | 0.15 (−0.002, 0.29) |
| Food outlets | 0.33 (0.03, 0.63) * | 0.06 (−0.05, 0.18) | −0.12 (−0.42, 0.19) | 0.04 (−0.03, 0.11) |
| School FV availability *Food outlets | −0.07 (−0.13, −0.01) * | −0.01 (−0.03, 0.01) | −0.02 (−0.05, 0.02) | −0.01 (−0.02, 0.002) |
| Model 2: 5 km school food environment | ||||
| School FV availability | 0.24 (0.08, 0.40) * | 0.16 (0.02, 0.31) * | 0.16 (0.01, 0.31) * | 0.15 (0.002, 0.30) * |
| Food outlets | 0.05 (0.02, 0.08) * | 0.01 (0.001, 0.01) * | 0.03 (−0.01, 0.06) | 0.004 (−0.001, 0.01) |
| School FV availability *Food outlets | −0.01 (−0.01, −0.004) * | −0.001 (−0.002, −0.0002) * | −0.005 (−0.01, −0.00001) * | −0.001 (−0.001, 0.0001) |
School availability of the food group corresponding to the outcome variable (e.g., school fruit and vegetable availability with student fruit and vegetable intake frequency). FV availability score ranges from 0 (no fruits, vegetables or 100% fruit juice offered any day) to 6 (fruits, vegetables and 100% fruit juice offered every day); snacks availability score ranges from 0 (no chocolate and candy, salty snacks or sweet snacks offered any day) to 6 (chocolate and candy, salty snacks and sweet snacks offered every day); soda availability score ranges from 0 (no soda offered any day) to 2 (soda offered every day).
Linear mixed models were used to calculate estimates.
Models adjusted for race/ethnicity (ref=white), parent education (ref=high school or less), family affluence (ref=low affluence), neighborhood land use mix, neighborhood population density, and neighborhood poverty rate.
p < 0.05
Full-service restaurants.
The number of full-service restaurants within 1 km was not associated with student FV intake and there was no statistically significant interaction between the number of full-service restaurants and school FV availability (Table 3). Full-service restaurants within a 5 km radius were positively associated with student FV intake (β: 0.01; 95% CI: 0.001, 0.01) (Table 3), but attenuated the positive association between school FV availability and student FV intake (Supplementary Figure 2A). Regions of significance showed that this relationship was observed at schools with less than 26 and with over 737 full-service restaurants within 5 km, but not at schools with 27–737 full-service restaurants within 5 km (Supplementary Figure 2B).
Convenience stores.
In models investigating convenience stores within a 5 km radius, the association of convenience stores with student FV intake did not reach statistical significance (Table 3), but the number of convenience stores within a 5 km radius attenuated the positive association between school FV availability and student FV intake (Supplementary Figure 3A). Regions of significance showed that this relationship was observed at schools with up to 3 convenience stores within 5 km, but not at schools with over 3 convenience stores within 5 km (Supplementary Figure 3B). Although results were consistent in the 1 km and 5 km models, the associations did not reach statistical significance in the model investigating convenience stores within a 1 km radius.
Grocery stores/Supermarkets.
The number of grocery stores/supermarkets within 1 km and 5 km was not associated with student FV intake, and there was no interaction of grocery stores/supermarkets with school FV availability (Table 3).
School food availability and student BMI: all school neighborhood food outlets
Neither school FV availability, school snack and soda availability, nor the total number of school neighborhood food outlets was associated with student BMI (Table 4).
TABLE 4:
Model estimates of the associations of school food and drink availability (frequency), the school neighborhood food environment (count of total food outlets within 1 km and 5 km), and their interaction with student BMI (kg/m2)
| School food and drink availability1 | |||
|---|---|---|---|
| FV | Snacks | Soda | |
| Student BMI (kg/m2) | |||
| Independent variables | β (95% Cl) | β (95% Cl) | β (95% Cl) |
| Model 1: 1 km school food environment | |||
| School availability | 0.14 (−0.12, 0.41) | −0.08 (−0.34, 0.19) | 0.10 (−0.43, 0.63) |
| All food outlets | 0.01(−0.07, 0.10) | −0.001 (−0.03, 0.03) | −0.002 (−0.03, 0.02) |
| School availability *All food outlets | −0.002 (−0.01, 0.01) | −0.00001 (−0.02, 0.02) | −0.01 (−0.03, 0.02) |
| Model 2: 5 km school food environment | |||
| School availability | 0.17 (0.10, 0.44) | −0.06 (−0.32, 0.21) | 0.14 (−0.39, 0.68) |
| All food outlets | 0.002 (−0.23, 0.53) | 0.0002 (−0.002, 0.002) | −0.0001 (−0.002, 0.002) |
| School availability *All food outlets | −0.0003 (−0.09, 0.03) | −0.0002 (−0.001, 0.001) | −0.001 (−0.003, 0.001) |
School availability of the food group corresponding to the outcome variable (e.g., school fruit and vegetable availability with student fruit and vegetable intake frequency). FV availability score ranges from 0 (no fruits, vegetables or 100% fruit juice offered any day) to 6 (fruits, vegetables and 100% fruit juice offered every day); snacks availability score ranges from 0 (no chocolate and candy, salty snacks or sweet snacks offered any day) to 6 (chocolate and candy, salty snacks and sweet snacks offered every day); soda availability score ranges from 0 (no soda offered any day) to 2 (soda offered every day). Snack intake measured at wave 2; all others measured at wave 1 (baseline).
Linear mixed models were used to calculate estimates.
Models adjusted for race/ethnicity (ref=white), parent education (ref=high school or less), family affluence (ref=low affluence), neighborhood land use mix, neighborhood population density, and neighborhood poverty rate.
p < 0.05
DISCUSSION
In this nationally representative sample of U.S. adolescents, greater school FV availability was positively associated with student FV intake. The number of total food outlets (including full-service restaurants, fast food outlets, convenience stores, and supermarkets and grocery stores) within a 5 km radius of schools attenuated the association of school FV availability with student intake. The positive association of school FV availability with student FV intake was non-significant when there were more than 58 neighborhood food outlets within 5 km. Because different foods are available from different food outlets, we further examined this association by food outlet type, and found that fast food outlets (within 1 and 5 km of schools) and full-service restaurants and convenience stores (within 5 km of schools), but not grocery stores/supermarkets attenuated the association of school FV availability with student FV intake. Neither the number of school neighborhood food outlets nor school availability of snacks and soda was associated with student snack and soda intake, and neither school food availability nor neighborhood food outlets were associated with student BMI.
No previous studies have assessed whether the external school food environment (i.e., food outlets in school neighborhoods) moderates the association of the internal school food environment (i.e. availability of foods and beverages within schools) with student dietary intake. Our findings suggest that the school’s external food environment may limit the potential impact of the internal school food environment on student outcomes; this was the case for food outlets within 5 km but not 1 km of schools, which could be due to limited observations with a substantial number of food outlets within 1 km (50% of schools had 2 or fewer food outlets within 1 km). Furthermore, the significant interactions observed at the upper range of food outlets may be due to constraints of a linear model (i.e., an interaction will eventually lead to a predictor slope of 0 and cross over to a reversed association), limiting interpretability. Evidence regarding the association of proximity of food outlets to schools with student FV intake has been mixed (27, 28, 44); our finding of a positive association raises the question of whether the external school food environment could be leveraged to promote healthful choices targeted to students. A possible explanation for the finding that grocery stores/supermarkets did not modify the association of school FV availability with student FV intake may be better access to small stores around schools than to larger grocery stores (44). The finding that school FV availability was positively associated with student FV intake at schools with fewer than 59 food outlets within 5 km is consistent with previous studies that found school policies targeting the provision of healthy foods were associated with greater intake of those foods (14, 16). In the present study, neither the internal nor external school food environment was associated with student snack or soda intake. Although this contradicts findings from previous studies reporting significant associations of policies limiting the sale of unhealthy foods and drinks in schools with lower intake of those items (10–12, 14, 15), many of these studies focused on in-school consumption (10, 14, 15). This suggests that consumption of these foods outside school may counteract the impact of in-school restrictions on students’ overall diet (10, 14, 17). Similarly, we did not find associations of the internal or external school food environment with student BMI. Although stricter school nutrition policies have been associated with improved weight outcomes (9, 18–20), our results are consistent with studies reporting null associations (21, 23). However, the positive association of school FV availability with student FV intake only in the presence of low numbers of surrounding food outlets is a novel finding that suggests that the external school food environment modifies the relationship of the internal school food environment with adolescent food intake in some contexts. Targeted strategies may be needed to increase student FV intake in schools with higher neighborhood food outlet density.
These findings should be interpreted in consideration of the strengths and limitations of the study design. Strengths include the nationally representative sample, which supports the generalizability of the findings. Additionally, the large sample size, use of directly measured BMI, and assessment and control for multiple neighborhood covariates strengthen the internal validity of the findings. However, limitations to internal validity include the lack of detailed information on food outlet data (i.e., criteria used to define food outlets as fast food outlets, full-service restaurants, convenience stores, and supermarket and grocery stores) and the observational study design and cross-sectional analysis, precluding determination of directionality and therefore inferences regarding causality. Despite the longitudinal design of the study, data on the internal and external school food environment were only available at baseline. Although student demand may influence the internal and external school food environment, it is unlikely there would be sufficient change in school policies or the external environment to implement longitudinal analyses using the current study design. Finally, our cross-sectional analyses included some data from wave 2, which may have slightly attenuated the associations.
In conclusion, these findings based on a national sample of U.S. 10th graders indicate that the school neighborhood food environment may modify the relationship of the school food environment with student eating behaviors. Additional research is needed to understand how the internal school food environment can help support optimal diet quality in adolescents in the context of varying external food environments.
Supplementary Material
FUNDING:
This project (contract number HHSN275201200001I) was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Heart, Lung and Blood Institute (NHLBI), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA), and the National Institute on Drug Abuse (NIDA).
ABBREVIATIONS:
- BMI
body mass index
- FV
fruits and vegetables
- IQR
interquartile range
Footnotes
CONFLICT OF INTEREST: GMB, CS, LML, DLH, and TRN report no conflicts of interest.
TRIAL REGISTRATION: NEXT Generation Health Study is a registered study with number NCT01031160 in Clinicaltrials.gov.
ETHICAL STANDARDS DISCLOSURE
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Written informed consent was obtained from all participants (if <18 years of age, parents provided consent for their child and students provided assent).
DATA SHARING STATEMENT
Data from the Next Generation Health Study are available through the Data and Specimen Sharing Hub (DASH), a centralized data resource for researchers to access data from research studies funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development for use in secondary research. For further information, please visit: https://dash.nichd.nih.gov/
REFERENCES
- 1.Hales CM, Carroll MD, Fryar CD et al. (2017) Prevalence of Obesity Among Adults and Youth: United States, 2015–2016, pp. 8 [USDoHaH Services, editor]: Centers for Disease Control National Center for Health Statistics. [Google Scholar]
- 2.Kimmons J, Gillespie C, Seymour J et al. (2009) Fruit and vegetable intake among adolescents and adults in the United States: percentage meeting individualized recommendations. Medscape J Med 11, 26. [PMC free article] [PubMed] [Google Scholar]
- 3.Simmonds M, Llewellyn A, Owen CG et al. (2016) Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev 17, 95–107. [DOI] [PubMed] [Google Scholar]
- 4.Ebbeling CB, Pawlak DB Ludwig DS (2002) Childhood obesity: public-health crisis, common sense cure. The Lancet 360, 473–482. [DOI] [PubMed] [Google Scholar]
- 5.Osei-Assibey G, Dick S, Macdiarmid J et al. (2012) The influence of the food environment on overweight and obesity in young children: a systematic review. BMJ Open 2, e001538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.USDA (2001) School Nutrition Dietary Assessment Study-II: Summary of Findings. Nutrition Assistance Program Report Series. vol. CN-01-SNDAIIFR. Alexandria, VA: USDA. [Google Scholar]
- 7.Briefel RR, Wilson A Gleason PM (2009) Consumption of low-nutrient, energy-dense foods and beverages at school, home, and other locations among school lunch participants and nonparticipants. J Am Diet Assoc 109, S79–90. [DOI] [PubMed] [Google Scholar]
- 8.Green EM, Spivak C Dollahite JS (2021) Early adolescent food routines: A photo-elicitation study. Appetite 158, 105012. [DOI] [PubMed] [Google Scholar]
- 9.Datar A & Nicosia N (2017) The Effect of State Competitive Food and Beverage Regulations on Childhood Overweight and Obesity. J Adolesc Health 60, 520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cullen KW, Watson K, Zakeri I et al. (2006) Exploring changes in middle-school student lunch consumption after local school food service policy modifications. Public Health Nutr 9, 814–820. [DOI] [PubMed] [Google Scholar]
- 11.Woodward-Lopez G, Gosliner W, Samuels SE et al. (2010) Lessons learned from evaluations of California’s statewide school nutrition standards. Am J Public Health 100, 2137–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cradock AL, McHugh A, Mont-Ferguson H et al. (2011) Effect of school district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004–2006. Prev Chronic Dis 8, A74. [PMC free article] [PubMed] [Google Scholar]
- 13.Taber DR, Chriqui JF Chaloupka FJ (2012) Differences in nutrient intake associated with state laws regarding fat, sugar, and caloric content of competitive foods. Arch Pediatr Adolesc Med 166, 452–458. [DOI] [PubMed] [Google Scholar]
- 14.Cullen KW, Watson K Zakeri I (2008) Improvements in middle school student dietary intake after implementation of the Texas Public School Nutrition Policy. Am J Public Health 98, 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson DB, Bruemmer B, Lund AE et al. (2009) Impact of school district sugar-sweetened beverage policies on student beverage exposure and consumption in middle schools. J Adolesc Health 45, S30–37. [DOI] [PubMed] [Google Scholar]
- 16.Rovner AJ, Nansel TR, Wang J et al. (2011) Food Sold in School Vending Machines Is Associated With Overall Student Dietary Intake. J Adolesc Health 48, 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taber DR, Chriqui JF, Powell LM et al. (2012) Banning all sugar-sweetened beverages in middle schools: reduction of in-school access and purchasing but not overall consumption. Arch Pediatr Adolesc Med 166, 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coffield JE, Metos JM, Utz RL et al. (2011) A multivariate analysis of federally mandated school wellness policies on adolescent obesity. J Adolesc Health 49, 363–370. [DOI] [PubMed] [Google Scholar]
- 19.Taber DR, Chriqui JF, Perna FM et al. (2012) Weight status among adolescents in States that govern competitive food nutrition content. Pediatrics 130, 437–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanchez-Vaznaugh EV, Sanchez BN, Baek J et al. (2010) ‘Competitive’ food and beverage policies: are they influencing childhood overweight trends? Health Aff (Millwood) 29, 436–446. [DOI] [PubMed] [Google Scholar]
- 21.Riis J, Grason H, Strobino D et al. (2012) State school policies and youth obesity. Matern Child Health J 16 Suppl 1, S111–118. [DOI] [PubMed] [Google Scholar]
- 22.Hennessy E, Oh A, Agurs-Collins T et al. (2014) State-level school competitive food and beverage laws are associated with children’s weight status. J Sch Health 84, 609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox MK, Dodd AH, Wilson A et al. (2009) Association between School Food Environment and Practices and Body Mass Index of US Public School Children. J Am Diet Assoc 109, S108–S117. [DOI] [PubMed] [Google Scholar]
- 24.Jensen CD, Sato AF, McMurtry CM et al. (2012) School Nutrition Policy: An Evaluation of the Rhode Island Healthier Beverages Policy in Schools. ICAN: Infant, Child, & Adolescent Nutrition 4, 276–282. [Google Scholar]
- 25.Sturm R (2008) Disparities in the food environment surrounding US middle and high schools. Public Health 122, 681–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laska MN, Hearst MO, Forsyth A et al. (2010) Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr 13, 1757–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith D, Cummins S, Clark C et al. (2013) Does the local food environment around schools affect diet? Longitudinal associations in adolescents attending secondary schools in East London. BMC Public Health 13, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davis B & Carpenter C (2009) Proximity of fast-food restaurants to schools and adolescent obesity. Am J Public Health 99, 505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green MA, Radley D, Lomax N et al. (2018) Is adolescent body mass index and waist circumference associated with the food environments surrounding schools and homes? A longitudinal analysis. Bmc Public Health 18, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang X, Ohri-Vachaspati P, Abbott JK et al. (2014) Associations between food environment around schools and professionally measured weight status for middle and high school students. Child Obes 10, 511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li K, Simons-Morton BG, Brooks-Russell A et al. (2014) Drinking and parenting practices as predictors of impaired driving behaviors among U.S. adolescents. J Stud Alcohol Drugs 75, 5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Currie C, Molcho M, Boyce W et al. (2008) Researching health inequalities in adolescents: The development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Social Science & Medicine 66, 1429–1436. [DOI] [PubMed] [Google Scholar]
- 33.Boyce W, Torsheim T, Currie C et al. (2006) The Family Affluence Scale as a Measure of National Wealth: Validation of an Adolescent Self-Report Measure. Social Indicators Research 78, 473–487. [Google Scholar]
- 34.Lipsky LM, Haynie DL, Liu D et al. (2015) Trajectories of eating behaviors in a nationally representative cohort of U.S. adolescents during the transition to young adulthood. International Journal of Behavioral Nutrition and Physical Activity 12, 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Austin SB, Melly SJ, Sanchez BN et al. (2005) Clustering of Fast-Food Restaurants Around Schools: A Novel Application of Spatial Statistics to the Study of Food Environments. American Journal of Public Health 95, 1575–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vilme H, Paul CJ, Duke NN et al. (2020) Using geographic information systems to characterize food environments around historically black colleges and universities: Implications for nutrition interventions. Journal of American College Health, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Esri Demographics American Community Survey (ACS). https://doc.arcgis.com/en/esri-demographics/data/acs.htm (accessed October 26 2020
- 38.United States Census Bureau What are census blocks? https://www.census.gov/newsroom/blogs/random-samplings/2011/07/what-are-census-blocks.html (accessed October 26 2020
- 39.Frank LD, Andresen MA Schmid TL (2004) Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med 27, 87–96. [DOI] [PubMed] [Google Scholar]
- 40.Brener ND, Eaton DK, Flint KH et al. (2013) Methodology of the Youth Risk Behavior Surveillance System - 2013.
- 41.Roberts C, Freeman J, Samdal O et al. (2009) The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. International Journal of Public Health 54, 140–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rubin DB (1987) Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons Inc. [Google Scholar]
- 43.Bauer DJ & Curran PJ (2005) Probing Interactions in Fixed and Multilevel Regression: nferential and Graphical Techniques. Multivariate Behavioral Research 40, 373–400. [DOI] [PubMed] [Google Scholar]
- 44.Jago R, Baranowski T, Baranowski JC et al. (2007) Distance to food stores & adolescent male fruit and vegetable consumption: mediation effects. International Journal of Behavioral Nutrition and Physical Activity 4, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from the Next Generation Health Study are available through the Data and Specimen Sharing Hub (DASH), a centralized data resource for researchers to access data from research studies funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development for use in secondary research. For further information, please visit: https://dash.nichd.nih.gov/


