INTRODUCTION.
In 2019, 4,777 youth died from a drug overdose in the US.1 Seven-hundred and twenty-seven youth died from overdoses involving benzodiazepines (BZD) and 902 from overdoses involving psychostimulants.2 Opioid-related overdose deaths frequently involve other substances, in youth, stimulants and BZDs are the most commonly involved substances.3 Overdoses can involve prescription drugs accessed through medical prescriptions or through illicit means. Among persons aged 18–25 years, 5.8% report past-year prescription stimulant misuse and 3.8% prescription BZD misuse.4
To inform overdose prevention efforts, we determined how often youth with medically treated overdoses involving BZDs and stimulants had recent BZD or stimulant prescriptions.
METHODS.
We included youth (15–24 years) from the MarketScan commercial claims database with an overdose involving stimulants or BZDs (1/1/2016–12/31/2018). MarketScan covers privately insured individuals and captures diagnoses and procedures from inpatient/outpatient visits and dispensed prescriptions.5 Overdose events treated in an emergency department (ED) or inpatient setting were included, defined as an ICD-10-CM code for an unintentional, intentional, or undetermined poisoning initial encounter (Table). Stimulant overdoses were limited to overdoses involving amphetamine or methylphenidate. We selected the first overdose per person and required ≥6 months of insurance enrollment with prescription coverage prior to the overdose.
Table.
Prior prescriptions in youth (15–24 years) with a medically-treated overdose involving a BZD or stimulant, 2016–2018a,b
| Overdoses involving BZDs | N=2,986 | Intent of overdoses involving BZDsf | ||
|---|---|---|---|---|
| Intentional N=1,664 |
Unintentional N=1,160 |
p-value | ||
| Age at overdose, Median (IQR) | 20 (17–22) | 20 (18–22) | 20 (18–22) | |
| Female | 1,556 (52.1%) | 1,045 (62.8%) | 447 (38.5%) | <0.001 |
| Mental health diagnosis in prior 6 monthsc | 2,232 (74.7) | 1,300 (78.1) | 813 (70.1) | <0.001 |
| Prior BZD prescriptiond | ||||
| 0–1 month | 854 (28.6%) | 590 (35.5%) | 234 (20.2%) | <0.001 |
| 0–6 months | 1,243 (41.6%) | 850 (51.1%) | 348 (30.0%) | <0.001 |
| Days from overdose to most recent prescription, Median (IQR) | 16 (5–39) | 16 (5–37) | 15 (4–40) | |
| Subset with BZD prescription(s) in prior 6 months | N=1,243 | N=850 | N=348 | |
| Number of BZD fills, Median (IQR) | 3 (1–5) | 2 (1–4) | 3 (1–5) | |
| >3 fills dispensed | 470 (37.8%) | 300 (35.3%) | 156 (44.8%) | 0.002 |
| Total BZD days supplied, Median (IQR) | 60 (30–120) | 60 (30–120) | 73 (30–136) | |
| >90 days dispensed | 413 (33.2%) | 267 (31.4%) | 134 (38.5%) | 0.018 |
| Mental health diagnosis in prior 6 monthsc | 1,153 (92.8) | 785 (92.4) | 324 (93.1) | 0.653 |
| Overdoses involving stimulants (amphetamine or methylphenidate) | N=971 | Intent of overdoses involving stimulantsf | ||
| Intentional N=388 |
Unintentional N=524 |
p-value | ||
| Age at overdose, Median (IQR) | 19 (17–22) | 18 (16–20) | 20 (18–22) | |
| Female | 415 (42.7%) | 213 (54.9%) | 179 (34.2%) | <0.001 |
| Mental health diagnosis in prior 6 months | 634 (65.3) | 299 (77.1) | 299 (57.1) | <0.001 |
| Prior stimulant prescriptione | ||||
| 0–1 month | 239 (24.6%) | 137 (35.3%) | 93 (17.7%) | <0.001 |
| 0–6 months | 380 (39.1%)g | 219 (56.4%) | 147 (28.1%) | <0.001 |
| Days from overdose to most recent prescription, Median (IQR) | 20 (8–47) | 21 (9–47) | 14 (5–46) | |
| Subset with stimulant prescription in prior 6 months | N=380 | N=219 | N=147 | |
| Number of stimulant fills, Median (IQR) | 4 (2–5) | 3 (2–5) | 4 (2–6) | |
| >3 fills dispensed | 191 (50.3%) | 102 (46.6%) | 83 (56.5%) | 0.064 |
| Total stimulant days supplied, Median (IQR) | 120 (60–180) | 117 (60–150) | 120 (90–180) | |
| >90 days dispensed | 213 (56.1%) | 112 (51.1%) | 95 (64.6%) | 0.011 |
| Mental health diagnosis in prior 6 months | 335 (88.2) | 199 (90.9) | 123 (83.7) | 0.038 |
BZD: Benzodiazepine; IQR: Interquartile range
ICD-10-CM overdose definitions: Overdose involving BZD: T42.4X1A, T42.4X2A, T42.4X4A; Overdose involving stimulant: amphetamine (T43.621A, T43.622A, T43.624A) and methylphenidate (T43.631A, T43.632A, T43.634A)
Prior prescriptions identified through records of dispensed prescriptions before overdose event. BZDs: alprazolam, chlordiazepoxide, clobazam, clonazepam, clorazepate, diazepam, estazolam, flurazepam, lorazepam, midazolam, oxazepam, quazepam, temazepam, triazolam; Stimulants: Amphetamines (amphetamine, dextroamphetamine, lisdexamfetamine, methamphetamine) and methylphenidates (methylphenidate, dexmethylphenidate)
Mental health diagnoses identified in 6months prior to overdose event (excluding date of overdose event): ICD-9-CM: 290–319; ICD-10-CM: F01-F99; See supplement for specific diagnoses
Prescription anytime in prior 0–12months: Overall: 1,380 (46.2%), intentional: 923 (55.5%), unintentional: 407 (35.1%)
Prescription anytime in prior 0–12months: Overall: 416 (42.8%), intentional: 238 (61.3%), unintentional: 162 (30.9%)
Undetermined overdose events not displayed (BZD: N=162, stimulant: N=59); if multiple overdose codes were recorded with differing intents (intentional, unintentional, undetermined), precedence in classification was given to intentional then unintentional
Overdose by type: Overdose involving amphetamine (n=833), 31.8% have amphetamine prescription in prior 6mo; Overdose involving methylphenidate (n=146), 64.4% have methylphenidate prescription in prior 6mo
In the 6 months prior to the overdose, we identified dispensed BZD and stimulant prescriptions and mental health diagnoses (Table). We summed the number of fills and days supply for prescriptions dispensed in the 6 months prior to the overdose. Results were stratified by intentional self-harm vs. unintentional overdoses. In a secondary analysis, class of prescription stimulant was considered with whether the overdose involved amphetamine or methylphenidate.
RESULTS.
We identified 2,986 youth with an overdose involving BZDs and 971 youth with an overdose involving stimulants (amphetamine/methylphenidate). The majority of youth had a prior mental health diagnosis; 56% of overdoses involving BZDs were intentional compared to 40% of overdoses involving stimulants (Table).
Twenty-nine percent of youth with overdoses involving BZDs had a prescription BZD dispensed in the prior 30 days and 42% in the prior 6 months (Table, Figure). Among youth with a BZD prescription in the prior 6 months, 33% received >90 days supply and 73% had an anxiety disorder diagnosis (eTable). Youth with intentional BZD overdoses were more likely to have a recent BZD prescription (51%) than unintentional overdoses (30%).
Figure.
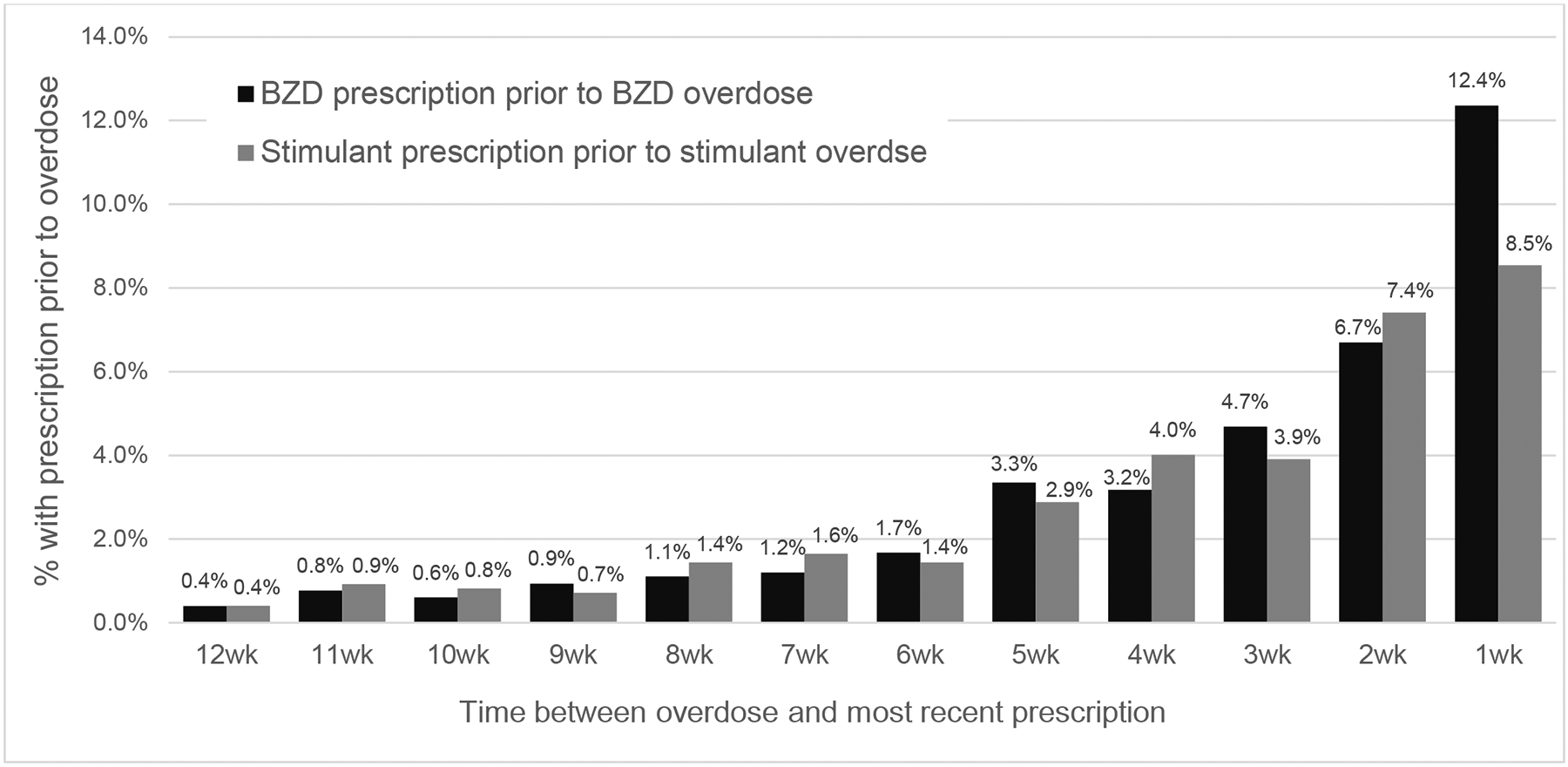
Proportion of youth (15–24 years) with a prescription fill* prior to an overdose involving a benzodiazepine or stimulant by time between prescription and overdose
BZD: Benzodiazepine; wk: week
*Percent with BZD prescription prior to an overdose involving a BZD; Percent with stimulant prescription prior to an overdose involving amphetamine or methylphenidate
A quarter of youth with an overdose involving stimulants (amphetamine/methylphenidate) had a stimulant prescription dispensed in the prior 30 days and 39% in the prior 6 months (Table, Figure). Among youth with a stimulant prescription in the prior 6 months, 56% received >90 days supply and 71% had an ADHD diagnosis (eTable). Youth with intentional stimulant overdoses were more likely to have a recent stimulant prescription (56%) than unintentional overdoses (28%).
DISCUSSION.
A considerable fraction of youth with overdoses involving BZDs and stimulants had recent prescriptions for these drugs. Prior BZD and stimulant prescriptions were more common in youth with intentional overdoses. This underscores the importance of incorporating self-injury assessment into clinical practice for youth prescribed BZDs and stimulants and highlights the need for differing prevention efforts for intentional and unintentional youth overdoses.
The majority of youth with a BZD or stimulant prescription prior to overdose had a mental health diagnosis. These medications are prescribed for mental health problems common in youth6,7 and can be effective treatments. However, as these drugs are commonly misused4 and involved in overdoses, weighing risks and benefits at prescribing remains imperative.
Primary considerations of this research include that we cannot distinguish amphetamine overdoses related to prescription amphetamine vs. an illicit substance. We miss overdoses that did not present to the ED or hospital, including fatal overdoses occurring outside these settings, and events in which BZD or stimulant involvement was not recorded. Without comparator groups, we are unable to assess comparative overdose liability by prescription characteristics.
Given that a fourth of youth with overdoses involving these drugs have prescriptions for them in the prior month, results suggest an avenue of prevention and motivate future work examining overdose risk following prescription. Because the potential for harm with BZD and stimulants increases with selected combinations of prescription medications, alcohol, and illicit drugs, especially concurrent BZD and opioid use;8,9 these concerns warrant attention and discussion at prescription initiation.
Supplementary Material
Funding/Support.
Research reported in this publication was supported by the National Institute on Drug Abuse (Bethesda, MD) under Award Number 1K01DA050769-01A1.
Abbreviations.
- BZD
benzodiazepine
- ED
emergency department
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10-CM
International Classification of Diseases, Tenth Revision, Clinical Modification
Footnotes
Conflict of Interest Disclosures. Drs. Bushnell, Calello, Gerhard, and Olfson have no disclosures to report related to this work. Dr. Samples has received consulting fees from the American Society of Addiction Medicine.
Article Summary. Within a commercial claims database, this study identified how frequently youth with an overdose involving BZDs or stimulants had a recent BZD or stimulant prescription.
REFERENCES
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. WISQARS - Web-based Injury Statistics Query and Reporting System. https://www.cdc.gov/injury/wisqars/index.html
- 2.CDC, National Center for Health Statistics. Wide-ranging online data for epidemiologic research (WONDER). Accessed 10/18/2021, 2021. http://wonder.cdc.gov [Google Scholar]
- 3.Lim JK, Earlywine JJ, Bagley SM, Marshall BDL, Hadland SE. Polysubstance Involvement in Opioid Overdose Deaths in Adolescents and Young Adults, 1999–2018. JAMA Pediatr. Feb 1 2021;175(2):194–196. doi: 10.1001/jamapediatrics.2020.5035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). 2020.
- 5.IBM Watson Health™. IBM MarketScan Research Databases for Health Services Researchers. IBM Corporation. https://www.ibm.com/downloads/cas/6KNYVVQ2 [Google Scholar]
- 6.Centers for Disease Control and Prevention. Data and Statistics on Children’s Mental Health. Accessed 10/15/2021, https://www.cdc.gov/childrensmentalhealth/data.html
- 7.Kessler RC, Avenevoli S, McLaughlin KA, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Psychol Med. Sep 2012;42(9):1997–2010. doi: 10.1017/S0033291712000025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma V, Simpson SH, Samanani S, Jess E, Eurich DT. Concurrent use of opioids and benzodiazepines/Z-drugs in Alberta, Canada and the risk of hospitalisation and death: a case cross-over study. BMJ Open. Nov 20 2020;10(11):e038692. doi: 10.1136/bmjopen-2020-038692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu KY, Hartz SM, Borodovsky JT, Bierut LJ, Grucza RA. Association Between Benzodiazepine Use With or Without Opioid Use and All-Cause Mortality in the United States, 1999–2015. JAMA Netw Open. Dec 1 2020;3(12):e2028557. doi: 10.1001/jamanetworkopen.2020.28557 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


