Abstract
Background:
Older adults have been disproportionately affected by the COVID-19 pandemic. Despite the widespread availability and proved effectiveness of COVID-19 vaccines, the issue of inequity in vaccine uptake in the United States is a potential concern among different populations. This study examined racial and ethnic and income disparities in COVID-19 vaccination rate among Medicare beneficiaries.
Methods:
Data from the Medicare Current Beneficiary Survey (MCBS) COVID-19 Winter 2021 Community Supplement were employed (n=9,606 Medicare beneficiaries, weighted N= 50,512,963). We fitted a logistic regression model to determine the association of vaccination status with beneficiary race and ethnicity and income, after controlled for a set of beneficiary characteristics.
Results:
Compared with non-Hispanic White respondents, Hispanic respondents (OR=0.72, 95% CI: 0.54–0.96, p=0.02) and Black respondents (OR=0.84, 95% CI: 0.67–1.04, p=0.11) were less likely to receive COVID-19 vaccine. In addition, the likelihood of COVID-19 vaccine uptake for beneficiaries who earn less than $25,000 per year was more than 50% lower than that for those whose annual income was $25,000 or more (OR=0.44, 95% CI: 0.37–0.53, p<0.0001).
Conclusions:
Racial and ethnic and income disparities exist in COVID-19 vaccination rate among Medicare beneficiaries nationally. Community-based strategies to boost vaccine uptake may target racial and ethnic minorities and socioeconomically disadvantaged groups to reduce such disparities.
Keywords: COVID-19 Vaccination, Race and Ethnicity, Income Disparities, Older Adults, Medicare Current Beneficiary Survey
INTRODUCTION
Since the onset of the coronavirus disease 2019 (COVID-19) pandemic in early 2020 in the United States, older adults have been disproportionately affected and comprised the majority of severe COVID-19 cases and COVID-related deaths nationally. With several COVID-19 vaccines available after December 2020, older adults are prioritized for early vaccine rollout and have achieved the highest vaccination rate among all age groups.1 As of October 29, 2021, the Center for Disease Control and Prevention (CDC) reported that 96.8% of people of ages 65 or older have gotten at least one dose of a vaccine, 85.1% have been fully vaccinated, and 22% have received the booster dose.1 In addition, a recent study has found that older adults who received both doses of either Pfizer or Moderna vaccines showed a 94% reduced risk of COVID-related hospitalization compared to control patients.2 Despite eventual widespread availability and proved effectiveness of vaccines, the issue of inequity in the United States still poses a risk of stagnation in vaccination rates and results in vaccination disparities among certain populations.3
Previous studies have highlighted that COVID-19 vaccination hesitancy in the United States varies significantly by sociodemographic characteristics, with racial and ethnic minorities and the low-income group reporting higher hesitancy than other groups.4–5 Moreover, there have been evidence that such disparities also exist for other types of vaccines, with vaccination rates being substantially lower for Black, Hispanic, and American Indian/Alaskan Native adults relative to non-Hispanic White adults.6–8 However, by the time of this study being conducted, there were no studies that have examined the issue of disparities in the actual uptake of COVID-19 vaccines among older adults. This study fills this gap and compares the rates of receiving at least one dose of the COVID-19 vaccine by race, ethnicity, and income using data from the most recent Medicare Current Beneficiary Survey (MCBS).
METHODS
Data and Study Sample
The Medicare Current Beneficiary Survey (MCBS), sponsored by the Centers for Medicare & Medicaid Services, is a nationally representative survey of Medicare beneficiaries. For this study, we used publicly available data from the MCBS COVID-19 Winter 2021 Community Supplement, which is a standalone telephone survey collected from March to April 2021.9 The questionnaire is designed to understand the impact of COVID-19 on the lives of Medicare beneficiaries, covering topics such as telemedicine visits, deferred care, COVID-19 testing and vaccination, in addition to routinely collected information on demographic characteristics and health status.9 The original sample includes 11,107 existing MCBS beneficiaries who live in the community at the time of their interview. This study excluded observations with missing values on the outcome variable or covariates, leading to the final sample of 9,606 Medicare beneficiaries (weighted N= 50,512,963).
Outcome Variable
The outcome variable of interest was the beneficiaries’ COVID-19 vaccination status, which is captured by the question “since the date of COVID-19 vaccine availability, have you had a coronavirus vaccination?” The response options include: yes, no, do not know, and refused. For those who answered yes to having received a COVID-19 vaccine, a follow-up question regarding the number of doses was asked, and the responses are: one, two, or do not know. Based on the two questions, we constructed a dichotomous variable for COVID-19 vaccination status which equaled 1 if the beneficiary has received at least one dose of COVID-19 vaccine or 0 if the respondent is unvaccinated (has not received any COVID-19 vaccine), and excluded “do not know” and “refused” responses.
Independent Variables and Covariates
The key independent variables were race and ethnicity and income level. The MCBS COVID-19 Winter 2021 survey categorized race and ethnicity into four groups: Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other/Unknown; and categorized income as a binary variable: income less than $25,000 per year or income $25,000 or more per year. Sociodemographic covariates included the following variables: sex (male or female), age (younger than 65 years, 65–74 years, and 75 years or older), residence (metro area or non-metro area), region (Northeast, Midwest, South, West), Medicare-Medicaid dual eligibility (yes or no), and language other than English spoken at home (yes or no).
Additionally, we controlled for several health conditions that could potentially affect respondents’ vaccination status, including weak immune system, hypertension, high cholesterol, stroke, cancer, lung disease, diabetes, heart disease, depression, and dementia. For each of the conditions, a binary variable was created which equaled 1 if the respondent reported having the condition and 0 otherwise. Based on findings from previous studies, there is a significant positive association between receiving COVID-19 information from regular news (compared to social media, internet, family/friends, and health care providers) and the intent to receive a COVID-19 vaccine, and thus we included a measure of information sources on COVID-19 in our analysis.5,10,11 Finally, the collected information about beneficiaries’ personal COVID-19 experiences, i.e., whether the survey participant “suspected to have COVID-19”, “was told they have COVID-19”, “tested for COVID-19”, and “have an active COVID-19 infection” were included as dichotomous covariates in the model, where yes was coded as 1 and no as 0. All these variables were selected based on the Andersen’s Behavioral Model (ABM) of Health Services Use and mapped onto the appropriate domain of the ABM (Supplementary Figure S1).12
Statistical Analysis
We first performed descriptive analyses in which we calculated percentages of the two independent variables, and compared beneficiary characteristics across racial and ethnic and income groups separately. In addition, a bar chart was used to illustrate the percentage of receiving at least one dose of COVID-19 vaccine for each racial and ethnic group and for each income group.
In multivariable analysis, we fitted a logistic regression model which has vaccination status as the dependent variable, race and ethnicity and income as key independent variables, and controlled for the covariates described above. To account for the survey sampling approaches, such as disproportionate sampling and survey nonresponse, all analyses were weighted with the sampling weights provided by the MCBS COVID-19 Winter 2021 PUF. Furthermore, we performed the variance inflation factor (VIF) analyses to check if multicollinearity in the multivariable regression existed. As shown in Supplementary Table S1, the VIF of each factor was less than 4, indicating that multicollinearity should not be a concern in this study.13 In addition, reported p-values were two-tailed, with the statistical significance level set at 0.05. STATA version 15.0 was used to conduct all statistical analyses.
RESULTS
Table 1 presents the weighted descriptive statistics for the study sample and by race and ethnicity and by income. In the weighted sample, 76.18% of surveyed beneficiaries are non-Hispanic White, 9.44% are Black, 10.09% are Hispanic, and 6.07% belong to the other or unknown racial and ethnic group; and 29.67% of the weighted sample earn an annual income that is less than $25,000.
Table I.
Sample Characteristics.
| (1) | (2) RACE | (3) INCOME | |||||
|---|---|---|---|---|---|---|---|
| Variables | Overall sample (%) | White Non-Hispanic (%) | Black Non-Hispanic (%) | Hispanic (%) | Other Race (%) | Income < 25K (%) | Income ≥ 25K (%) |
| Sex | |||||||
| Male | 45.39 | 45.55 | 42.17 | 46.14 | 47.33 | 37.55 | 48.70 |
| Female | 54.61 | 54.45 | 57.83 | 53.86 | 52.67 | 62.45 | 51.30 |
| Race | |||||||
| White non-Hispanic | 76.18 | 57.90 | 83.90 | ||||
| Black non-Hispanic | 9.45 | 18.22 | 5.74 | ||||
| Hispanic | 8.30 | 15.76 | 5.16 | ||||
| Other race/Unknown | 6.07 | 8.12 | 5.20 | ||||
| Age category | |||||||
| < 65 years | 13.36 | 10.95 | 26.68 | 17.66 | 17.02 | 29.19 | 6.68 |
| 65–74 years | 53.17 | 53.97 | 47.86 | 53.58 | 50.79 | 38.38 | 59.40 |
| ≥ 75 years | 33.47 | 35.09 | 25.45 | 28.76 | 32.19 | 32.43 | 33.92 |
| Income | |||||||
| Less than 25k income | 29.67 | 22.55 | 57.24 | 56.32 | 39.68 | ||
| $25K or more | 70.33 | 77.45 | 42.76 | 43.68 | 60.32 | ||
| Metro | |||||||
| Metro | 80.31 | 78.05 | 86.54 | 92.57 | 82.28 | 75.74 | 82.24 |
| Non-metro | 19.69 | 21.95 | 13.46 | 7.43 | 17.72 | 24.26 | 17.76 |
| Region | |||||||
| Northeast | 17.78 | 18.68 | 12.41 | 16.21 | 16.97 | 17.16 | 18.04 |
| Midwest | 21.81 | 24.87 | 14.44 | 8.66 | 12.83 | 20.09 | 22.53 |
| South | 38.82 | 36.72 | 63.84 | 31.43 | 36.36 | 44.84 | 36.28 |
| West | 21.59 | 19.73 | 9.31 | 43.70 | 33.84 | 17.91 | 23.15 |
| Medicare-Medicaid dual eligibility | |||||||
| Yes | 14.36 | 8.74 | 35.05 | 38.22 | 20.16 | 44.76 | 1.54 |
| No | 85.64 | 91.26 | 64.95 | 61.78 | 79.84 | 55.24 | 98.46 |
| Speak language other than English at home | |||||||
| Yes | 11.05 | 3.06 | 3.40 | 23.69 | 34.00 | 19.27 | 7.59 |
| No | 88.95 | 96.94 | 96.60 | 76.31 | 66.00 | 80.73 | 92.41 |
| Health conditions (Yes) | |||||||
| Weak immune system | 16.87 | 16.83 | 15.15 | 16.72 | 20.19 | 19.48 | 15.77 |
| Hypertension | 62.85 | 60.36 | 77.80 | 63.76 | 69.51 | 66.32 | 61.38 |
| High cholesterol | 63.45 | 62.52 | 66.63 | 69.82 | 61.35 | 63.42 | 63.46 |
| Stroke | 8.88 | 8.46 | 12.44 | 8.02 | 9.75 | 12.23 | 7.46 |
| Cancer | 19.12 | 20.06 | 14.32 | 15.75 | 19.28 | 16.66 | 20.15 |
| Lung disease | 18.74 | 18.53 | 19.38 | 16.68 | 23.16 | 25.20 | 16.02 |
| Diabetes | 31.30 | 26.85 | 44.17 | 46.94 | 45.77 | 36.92 | 28.93 |
| Heart disease | 31.47 | 32.78 | 29.22 | 23.79 | 29.02 | 31.65 | 31.39 |
| Depression | 25.89 | 25.94 | 23.58 | 28.41 | 25.37 | 35.03 | 22.03 |
| Dementia | 2.50 | 2.28 | 2.37 | 4.24 | 3.06 | 3.72 | 1.98 |
| Main information source | |||||||
| Traditional news | 49.81 | 48.33 | 54.65 | 56.64 | 51.48 | 52.89 | 48.51 |
| Social media | 1.25 | 1.12 | 1.21 | 1.94 | 1.98 | 1.73 | 1.05 |
| Government officials | 11.23 | 11.76 | 9.79 | 7.18 | 12.35 | 6.78 | 13.11 |
| Other Internet/webpages | 8.24 | 9.15 | 3.79 | 5.44 | 7.7 | 6.23 | 9.09 |
| Family and friends | 10.07 | 10.21 | 8.50 | 9.87 | 11.06 | 14.46 | 8.22 |
| Health care providers | 19.39 | 19.43 | 22.07 | 18.93 | 15.44 | 17.9 | 20.02 |
| CV19-specific variables (Yes) | |||||||
| Suspected to have CV19 | 8.29 | 8.17 | 6.68 | 11.92 | 7.40 | 9.08 | 7.96 |
| Was told they have CV19 | 4.44 | 4.10 | 4.56 | 8.36 | 3.07 | 4.96 | 4.22 |
| Tested for CV19 | 34.24 | 32.81 | 42.12 | 41.25 | 30.24 | 33.96 | 34.35 |
| Result of active CV19 | 4.05 | 3.64 | 4.88 | 7.61 | 2.97 | 4.31 | 3.94 |
| n (unweighted) | 9,606 | 7,212 | 930 | 969 | 495 | 3,440 | 6,166 |
| N (weighted) | 50,512,963 | 38,482,514 | 4,771,552 | 4,193,335 | 3,065,561 | 14,987,501 | 35,525,463 |
Compared with non-Hispanic White respondents, non-Hispanic Black and Hispanic respondents tended to be slightly younger, make less than $25,000 per year, live in metro areas, be Medicare-Medicaid dual eligible, speak language other than English at home, and have higher rates of hypertension, high cholesterol, diabetes, and dementia. Racial and ethnic minority beneficiaries were also more likely to rely on traditional news or social media as their primary source of COVID-19 information, and to report being told they have COVID-19, having a test for COVID-19, and receiving a positive test result.
Compared with respondents whose annual income was $25,000 or more, low-income respondents were more likely to be female, be in the racial and ethnic minority groups, age younger than 65 years, be Medicare-Medicaid dually eligible, have more health problems, and rely primarily on traditional news or family and friends for information on COVID-19. Additionally, respondents who earn less than $25,000 per year were more likely to suspect to have COVID-19, be told they have COVID-19, and test positive for COVID-19, but were less likely to receive a test.
Figure 1 shows the rate of receiving at least one dose of COVID-19 vaccine for each group of interest. Specifically, non-Hispanic White respondents had the highest vaccination rate (68.07%), followed by respondents of other race (62.24%), Hispanic respondents (52.23%), and non-Hispanic Black (51.54%). Vaccination rates by income showed that 73.78% of respondents earning an annual income $25,000 or more have received at least one dose of COVID-19 vaccine, compared with 43.66% for respondents who had income less than $25,000 per year.
Figure 1.
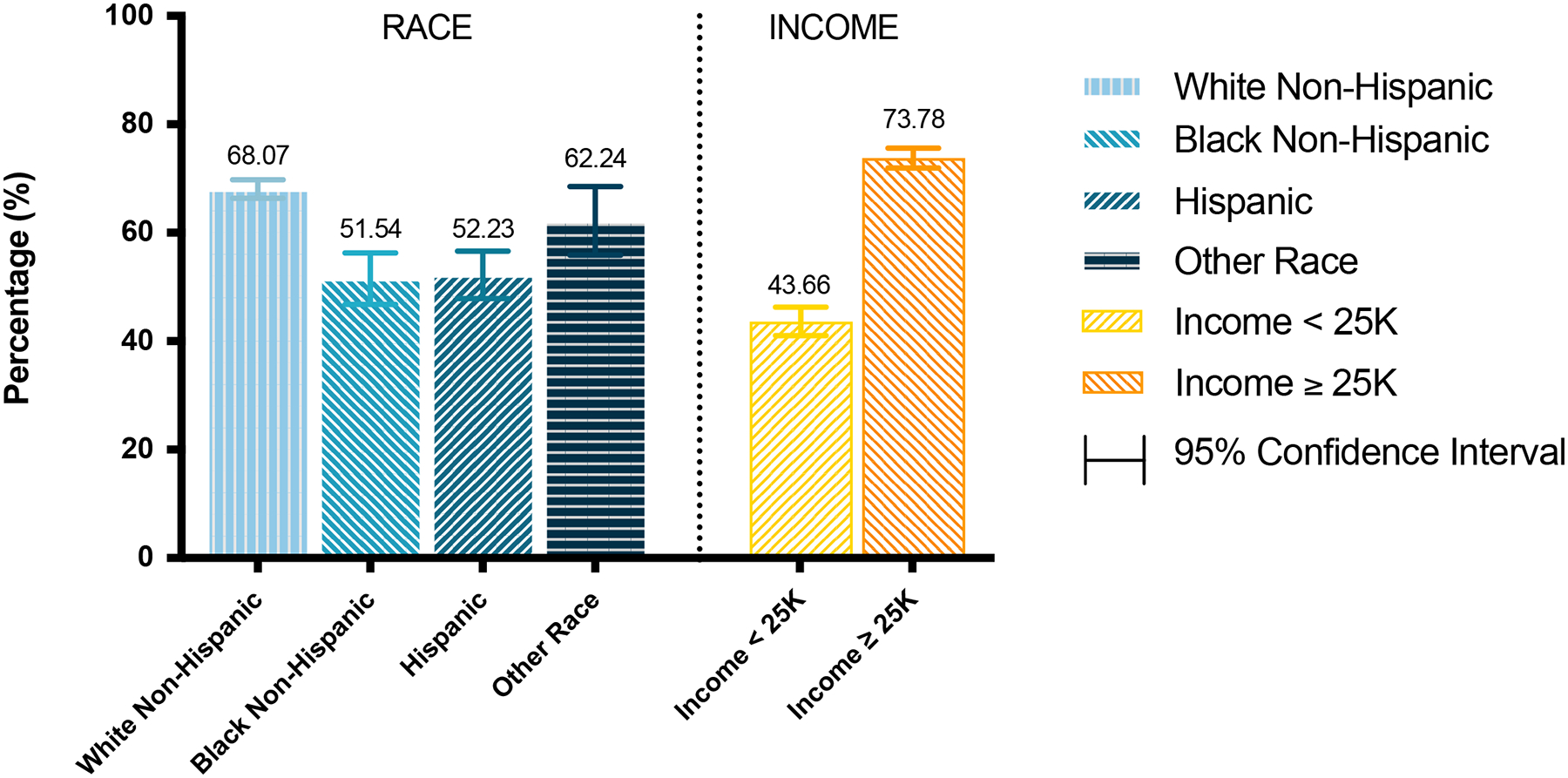
Percentage of Receiving at Least One Dose of COVID-19 Vaccine
Table 2 presents odds ratios (ORs) for receiving at least one dose of COVID-19 vaccine in the logistic regression. Compared with non-Hispanic White respondents, Hispanic respondents were significantly less likely to receive vaccine (ORunadjusted=0.51, 95% CIunadjusted=0.43–0.61, punadjusted<0.0001; ORadjusted=0.72, 95% CIadjusted: 0.54–0.96, padjusted=0.02). Although non-Hispanic Black respondents also had a lower odds of receiving vaccine, this association was no longer statistically significant after adjusting for the covariates (ORunadjusted=0.50, 95% CIunadjusted=0.42–0.60, punadjusted<0.0001; ORadjusted=0.84, 95% CIadjusted: 0.67–1.04, padjusted=0.11). Compared with beneficiaries earning an annual income $25,000 or more, those who earn less than $25,000 were substantially less likely to be vaccinated (ORunadjusted=0.28, 95% CIunadjusted=0.24–0.31, punadjusted<0.0001; ORadjusted =0.44, 95% CIadjusted: 0.37–0.53, padjusted<0.0001). Being dually eligible, having a stroke, relying on social media, family and friends, or internet as a primary source of COVID-19 information, and having suspected to have COVID-19 were all associated with a reduced likelihood of COVID-19 vaccine uptake; while being in older age groups, having high cholesterol, relying on governmental officials as a primary source of COVID-19 information, and having tested for COVID-19 were associated with greater odds of receiving at least one dose of vaccine.
Table 2.
Logistic Regression Results Showing Odds Ratios for Receiving at Least One Dose of Vaccine (n=9,606; N=50, 512,963)
| Variables | Unadjusted Odds Ratio for Race (95% CI) | P-value | Unadjusted Odds Ratio for Income (95% CI) | P-value | Adjusted Odds Ratio (95% CI) | P-value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female | 1.00 (0.89, 1.12) | 0.95 | ||||
| Race | ||||||
| Black non-Hispanic | 0.50 (0.42, 0.60) | 0.00 | 0.83 (0.67, 1.04) | 0.11 | ||
| Hispanic | 0.51 (0.43, 0.61) | 0.00 | 0.72 (0.54, 0.96) | 0.02 | ||
| Other race/Unknown | 0.77 (0.59, 1.02) | 0.07 | 0.98 (0.74, 1.30) | 0.88 | ||
| Age category | ||||||
| 65–74 years | 4.33 (3.49, 5.38) | 0.00 | ||||
| ≥ 75 years | 6.35 (5.05, 8.00) | 0.00 | ||||
| Income | ||||||
| Less than 25k income | 0.28 (0.24, 0.31) | 0.00 | 0.44 (0.37, 0.53) | 0.00 | ||
| Metro | ||||||
| Metro | 1.11 (0.92, 1.35) | 0.28 | ||||
| Region | ||||||
| Midwest | 1.07 (0.84, 1.36) | 0.59 | ||||
| South | 1.05 (0.83, 1.34) | 0.67 | ||||
| West | 1.24 (0.90, 1.71) | 0.18 | ||||
| Medicare-Medicaid dual eligibility | ||||||
| Yes | 0.74 (0.61, 0.90) | 0.00 | ||||
| Speak language other than English at home | ||||||
| Yes | 1.04 (0.78,1.39) | 0.78 | ||||
| Health conditions (Yes) | ||||||
| Weak immune system | 0.89 (0.76, 1.39) | 0.18 | ||||
| Hypertension | 0.94 (0.83, 1.06) | 0.29 | ||||
| High cholesterol | 1.19 (1.04, 1.37) | 0.01 | ||||
| Stroke | 0.74 (0.63, 0.87) | 0.00 | ||||
| Cancer | 1.20 (1.05, 1.37) | 0.00 | ||||
| Lung disease | 0.95 (0.84, 1.08) | 0.44 | ||||
| Diabetes | 1.00 (0.89, 1.15) | 0.88 | ||||
| Heart disease | 1.12 (0.99, 1.28) | 0.08 | ||||
| Depression | 0.96 (0.84, 1.09) | 0.49 | ||||
| Dementia | 1.03 (0.75, 1.41) | 0.87 | ||||
| Main information source | ||||||
| Social media | 0.54 (0.31, 0.92) | 0.03 | ||||
| Government officials | 1.78 (1.42, 2.24) | 0.00 | ||||
| Other Internet/webpages | 0.79 (0.65, 0.95) | 0.01 | ||||
| Family and friends | 0.65 (0.54, 0.77) | 0.00 | ||||
| Health care providers | 0.91 (0.77, 1.06) | 0.21 | ||||
| CV19-specific variables (Yes) | ||||||
| Suspected to have CV19 | 0.58 (0.44, 0.76) | 0.00 | ||||
| Was told they have CV19 | 0.80 (0.44, 1.48) | 0.48 | ||||
| Tested for CV19 | 1.49 (1.31, 1.70) | 0.00 | ||||
| Result of active CV19 | 0.62 (0.38, 1.04) | 0.07 |
DISCUSSION
According to recent guidelines of the Centers for Disease Control and Prevention, widespread vaccination of COVID-19 is the most efficacious and safest approach to protect everyone, especially those at high risk, from severe COVID-19 complications and death, and to end the pandemic.14 Although older adults have a higher average COVID-19 vaccination rate than people of other age groups, previous studies have revealed that vaccine hesitancy among older adults is common and varies substantially over subgroups: Women, non-Hispanic Black persons, Hispanic persons, smokers, and those with lower income were more likely to report negative vaccine intent.5,15 Moreover, recent research demonstrated that the vaccine hesitant tended to have persistently low vaccination rate even under financial and non-financial incentives.16 Unlike most previous studies examining vaccine hesitancy, our study focused on racial and ethnic and income disparities in the actual COVID-19 vaccine uptake among Medicare beneficiaries and found that Hispanic and low-income older adults were less likely to receive the vaccine as of April 2021 (when the survey was completed). Specifically, although the overall vaccination rate for at least one dose was 63.9%, the rate for Hispanic beneficiaries was 16% lower than the rate for non-Hispanic White beneficiaries (52% vs 68%), and the rate for respondents who earn less than $25,000 per year was 30% lower than those who earn $25,000 and more (74% vs 44%). Although the non-Hispanic Black persons had higher (with statistical significance) COVID-19 vaccine hesitancy than the non-Hispanic Whites in prior studies,5,15 such significant difference was not observed in actual vaccine uptake. In this study, the absence of a significant difference in vaccination rates between non-Hispanic White and non-Hispanic Black respondents may have been a result of the relatively small sample size of Black beneficiaries (nblack=930 vs. nwhite=7,212) and the converging trend between the Black and White populations. As suggested by a 2021 NPR/PBS NewsHour/Marist poll, the differences in vaccine hesitancy between the Black and White populations had started to converge but remained high for the Hispanics (Black: 25%, White: 28%, and Hispanic: 37%).17 Furthermore, we found that beneficiaries who relied on social media or internet as their primary COVID-related information source were less likely to receive the first dose of COVID-19 vaccine compared with those relying on regular news or government officials, which aligns with precious studies demonstrating the effect of information sources on vaccine hesitancy.5, 11 Overall, our findings suggested that racial and ethnic and income disparities in actual vaccine uptake among the older persons persist even after the CDC recommendations. Thus, there is a clear urgency for addressing the issue of vaccine disparity and improving current vaccination strategies among under-vaccinated populations.
Our findings suggest that one universal vaccination policy may not be adequate to close the gap in vaccination coverage and reduce inequalities. To promote equitable vaccination coverage as well as overall uptake rate, it is important to identify communities with low vaccination rates and build community partnerships between vaccine providers and trusted messengers to increase awareness about COVID-19 vaccine and booster, and develop tailored approaches to accommodate community’s needs and ensure adequate access to vaccines. Additional efforts at state and national levels are also required to provide financial support and implement new policies to redress systemic racial and ethnic and socioeconomic inequalities.
There are several limitations of this study. First, given the observational nature of the cross-sectional study, we were only able to evaluate associations but not causality. Second, our analysis was based on self-reported data, which could be subject to recall bias and measurement error. Third, the publicly available MCBS data have released somewhat limited information, which prevented us from conducting more detailed analyses. For example, the other/unknown race and ethnicity group was treated as a homogenous group, but there were likely differences in vaccination rates within the group; the only available geographical variable is on region level, thus state-level or county-level analysis was not possible; and this study did not examine the reasons underlying vaccination disparities due to lack of data. However, prior literature suggested that such disparities result from factors both within and outside of health care, such as concerns on the safety and the effectiveness of COVID-19 vaccines, lack of insurance, financial restrictions, and distrust of health care systems.18,19 Finally, as the outcome of interest of this study is receipt of at least on dose of COVID-19, the findings may not entirely reflect the full vaccination status.
In conclusion, our study found that Hispanic and low-income Medicare beneficiaries were less likely to receive COVID-19 vaccines, which confirmed our hypothesis that racial and ethnic and income-related vaccination disparities exist among older adults. Efforts at the local, state, and federal levels are needed to ameliorate these disparities and to ensure equitable distribution and access to COVID-19 vaccines for racial and ethnic minorities and other socioeconomically disadvantaged groups.
Supplementary Material
Supplementary Table S1 – The variance inflation factor (VIF) values of the independent variables and covariates in the logistic regression model
Supplementary Figure S1 – The conceptual framework based on Anderson’s Behavioral Model of Healthcare Utilization and the corresponding components
Key Points.
Among Medicare beneficiaries, White respondents had the highest rate of receiving at least one dose of COVID-19 vaccine (68%), followed by respondents of other race (62%), Hispanic respondents (52%), and non-Hispanic Black respondents (52%).
74% of respondents earning an annual income $25,000 or more have received at least one dose of COVID-19 vaccine, compared with 44% for respondents who had income less than $25,000 per year
Racial and ethnic and income disparities exist in COVID-19 vaccination rate among Medicare beneficiaries nationally.
Why Does this Paper Matter?
This study reveals the existence of racial and ethnic and income disparities in COVID-19 vaccination rates among older adults and highlights the importance of community-based strategies to boost vaccine uptake in hard-to-reach groups and ensuring equitable distribution and access to the vaccines.
ACKNOWLEDGEDMENTS
Sponsor’s Role:
This research was funded by the National Institute of Health (NIH) under grant R01AG069733. The views expressed in this article are those of the authors and do not necessarily represent the view of the NIH. The NIH has no role in study design, data collection, analyses, or interpretation of results.
Footnotes
Conflicts of Interest: The authors have declared no conflicts of interest for this article.
REFERENCES
- 1.Centers for Disease Control and Prevention. CDC COVID Data Tracker (online). Available at: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total. Accessed November 25, 2021.
- 2.Tenforde MW, Olson SM, Self WH, et al. Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Among Hospitalized Adults Aged ≥65 Years - United States, January-March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(18):674–679. Published 2021 May 7. doi: 10.15585/mmwr.mm7018e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaiser Family Foundation (KFF). Latest Data on COVID-19 Vaccinations by Race/Ethnicity (online). Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/. Accessed December 21, 2021
- 4.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhagianadh D, Arora K. COVID-19 Vaccine Hesitancy Among Community-Dwelling Older Adults: The Role of Information Sources [published online ahead of print, 2021 Aug 7]. J Appl Gerontol. 2021;7334648211037507. doi: 10.1177/073346482110375074 [DOI] [PubMed] [Google Scholar]
- 6.Grohskopf LA, Liburd LC, Redfield RR. Addressing Influenza Vaccination Disparities During the COVID-19 Pandemic. JAMA. 2020;324(11):1029–1030. doi: 10.1001/jama.2020.15845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen AK, Warnock R, Selna W, Chu S, Kelman JA. Patient characteristics of Medicare beneficiaries who report not getting influenza and pneumococcal vaccinations, 2001–2013. Hum Vaccin Immunother. 2020;16(5):1086–1092. doi: 10.1080/21645515.2019.1688033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spencer JC, Calo WA, Brewer NT. Disparities and reverse disparities in HPV vaccination: A systematic review and meta-analysis. Prev Med. 2019;123:197–203. doi: 10.1016/j.ypmed.2019.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medicare Current Beneficiary Survey. 2021. Data User’s Guide: COVID-19 Winter Supplement Public Use File. Available at: https://www.cms.gov/files/document/2021mcbscovidpufdugwinter.pdf. Accessed November 25, 2021.
- 10.Piltch-Loeb R, Savoia E, Goldberg B, et al. Examining the effect of information channel on COVID-19 vaccine acceptance. PLoS One. 2021;16(5):e0251095. Published 2021 May 12. doi: 10.1371/journal.pone.0251095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim J, Kim Y, Li Y. Source of information on COVID-19 vaccine and vaccine hesitancy among U.S. Medicare beneficiaries [published online ahead of print, 2021 Dec 11]. J Am Geriatr Soc. 2021;10.1111/jgs.17619. doi: 10.1111/jgs.17619 [DOI] [PubMed] [Google Scholar]
- 12.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995. Mar;36(1):1–10. [PubMed] [Google Scholar]
- 13.Hair JF Jr., Anderson RE, Tatham RL & Black WC Multivariate Data Analysis (3rd ed). New York: Macmillan. 1995. [Google Scholar]
- 14.Centers for Disease Control and Prevention. How CDC is Making COVID-19 Vaccine Recommendations (online). Available at: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations-process.html. Accessed November 25, 2021
- 15.Kim D Associations of Race/Ethnicity and Other Demographic and Socioeconomic Factors with Vaccine Initiation and Intention During the COVID-19 Pandemic in the United States. medRxiv.2020. Available at: https://www.medrxiv.org/content/10.1101/2021.02.16.21251769v2.full.pdf. Accessed April 5, 2022 [Google Scholar]
- 16.Chang T, Jacobson M, Shah M, Pramanik R, & Shah SB (2021). Financial incentives and other nudges do not increase covid-19 vaccinations among the vaccine hesitant(No. w29403) National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NPR/PBS NewsHour/Marist Poll. Americans weigh in on COVID-19 relief package…Biden approval rating at 49% http://maristpoll.marist.edu/npr-pbs-newshour-marist-poll-results-analysis-21/. Published 2021. Accessed 4 April, 2022.
- 18.Callaghan T, Moghtaderi A, Lueck JA, Hotez PJ, Strych U, Dor A, … & Motta M Correlates and disparities of COVID-19 vaccine hesitancy. 2020; Available at SSRN 3667971. [DOI] [PMC free article] [PubMed]
- 19.Restrepo N, & Krouse HJ COVID-19 Disparities and Vaccine Hesitancy in Black Americans: What Ethical Lessons Can Be Learned?. Otolaryngology–Head and Neck Surgery.2021;01945998211065410. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1 – The variance inflation factor (VIF) values of the independent variables and covariates in the logistic regression model
Supplementary Figure S1 – The conceptual framework based on Anderson’s Behavioral Model of Healthcare Utilization and the corresponding components


