Abstract
BACKGROUND:
Children who undergo common outpatient surgeries are routinely prescribed opioids, although available evidence suggests they should be used with discretion for procedures associated with mild to moderate pain. The study assessed trends in postoperative opioid prescribing over time to determine if prescribing declined.
METHODS:
We utilized a private insurance database to study opioid-naïve patients under age 18 who underwent one of 8 surgical procedures 2014–2019. The primary outcome was the likelihood of filling a prescription for opioids within 7 days of surgery and the secondary outcome was the total amount of opioid dispensed. We used Joinpoint regression analysis to identify temporal shifts in trends.
RESULTS:
The study cohort included 124,249 opioid-naïve children. The percentage of children who filled an opioid prescription decreased from 78.2% (95% CI 76.3–80.1%) to 48.0% (95% CI 45.8–50.1%) among adolescents, from 53.9% (95% CI 51.6–56.2%) to 25.5% (95% CI 23.5–27.5%) among school-age children and 30.4% (95% CI 28.6–32.2%) to 11.5% (95% CI 10.1–12.9%) among preschool children. The average morphine milligram equivalent (MME) dispensed declined from 228.9 (95% CI 220.1–237.7) to 110.8 (95% CI 105.6–115.9) among adolescents, 121.3 (95% CI 116.7–125.9) to 65.9 (95% CI 61.1–70.7) among school-age children and 75.3 (95% CI 70.2–80.3) to 33.2 (95% CI 30.1–36.3) among preschool children. Using Joinpoint regression, we identified rapid opioid de-adoption beginning in late 2017, first in adolescents, followed by school-age and then preschool children.
CONCLUSION:
Opioid prescribing after surgery decreased gradually from 2014 to 2017, with a more pronounced decrease seen beginning in late 2017.
INTRODUCTION
Opioids are routinely prescribed for common pediatric surgeries associated with mild to moderate pain; however, evidence suggests recovery is similar with either limited or no opioids.1–8 In children, excessive postoperative opioid exposure has been associated with adverse outcomes such as respiratory depression and new long-term use.6, 9–12
Few data currently exist to characterize opioid prescribing trends for pediatric surgery, and it is unknown to what extent providers have moved away from routine opioid prescribing.2–4, 6, 7, 12, 13 Understanding patterns of opioid prescribing for children after surgery may facilitate policy efforts to address overuse moving forward. For example, opioid prescribing guidelines specific to pediatric surgical patients have recently been published and recommend limiting or avoiding opioid prescriptions for surgeries where pain is anticipated to be minimal.3, 4 These guidelines highlight the risks of opioid prescribing that are unique to pediatric patients.3 However, effective implementation of these evidence-based recommendations is limited by a lack of information on current opioid prescribing patterns and changes in prescribing over time for children undergoing surgery. The present study adds to the information available to policy makers and health systems to develop and target interventions intended to promote evidence-based prescribing.
To address this need, we designed this study to characterize trends in US prescribing practices for opioid-naïve children after surgery, including the percentage filling a prescription, the prescription quantity and refills dispensed. We selected 8 common pediatric surgeries considered to have a low likelihood of significant pain requiring opioids. Since adolescents, school-age and preschool children undergo different types of surgeries, we studied national trends among these three groups.12, 14 We examined if there was a change in study outcomes over time and then utilized Joinpoint regression to characterize changes in slope of identified trends over time. We hypothesized that there would be a decrease in both the likelihood of filling an opioid prescription and prescription quantity consistent with de-adoption of routine opioid prescribing for children undergoing surgery during the study period.
METHODS
Study design and oversight
We conducted a retrospective cohort study using a national insurance database to determine baseline opioid dispensing trends and moments when trends changed between April 1, 2014 and March 31, 2019. Among children that received at least one opioid prescription within 7 days of surgery, we assessed the average amount of opioid dispensed in Morphine Milligram Equivalents (MME), the days supplied and the percentage of children that received more than one prescription (refill) within 30 days of surgery. We performed a visual comparison of trends and used Joinpoint regression analysis to identify points in time when rapid shifts in prescribing trends occurred. The purpose of this descriptive analysis was to characterize specific time points at which prescribing trends changed. As a result, we did not specify time points a priori at which we hypothesized a trend change would occur, and rather allowed the Joinpoint regression program to identify significant points at which change in trend were observed in the data.15 We used patient-level time series segmented regression to validate changes in prescribing likelihood identified by Joinpoint regression and control for potential confounders. This study was determined to be exempt from human subject research review by the University of Pennsylvania Institutional Review Board.
Data source
We used de-identified data from Optum’s Clinformatics® Data Mart Database, a US health insurance database with over 15 million annual enrollees from all 50 states.16 The database contained both medical and pharmacy claims data.17 The study sample included all patients under age 18 with a submitted claim for surgery and continuous enrollment for the 90 days prior to the date of surgery during the study period. Demographic variables, such as race and ethnicity, were provided as recorded in the electronic medical record. Eight common pediatric surgeries were selected because severe postoperative pain requiring opioids was anticipated to be uncommon6, 18, 19 3, 4 These procedures were: tonsillectomy (with or without adenoidectomy), adenoidectomy only, laparoscopic appendectomy, cholecystectomy, dental surgery, knee arthroscopy, circumcision, and orchiopexy. Procedures were identified using Current Procedure Terminology (CPT) codes in physician claims (Appendix Table 1). For patients with more than one eligible surgery during the study period, we used the first procedure. Patients with claims for more than one eligible procedure on the same day, patients who required an inpatient stay and those that did not have 90 days of continuous enrollment prior to the procedure and 30 days after were excluded. We also excluded patients with a filled opioid prescription in the 90 days prior to surgery to capture new opioid prescriptions for opioid-naïve children, rather than refills for established chronic pain treatment.
Due to differences in development and anticipated procedure distribution by age, we analyzed data separately in 3 age groups: adolescents (11 through 17 years), school-age children (5 through 10 years) and infants to preschool-age (<5 years). Within a given age group, we limited our analyses to those procedures where we had an average of at least 100 observations per 12 months over the study period. Among adolescents, we studied knee arthroscopy, laparoscopic cholecystectomy, appendectomy, tonsillectomy, adenoidectomy only, dental surgery, orchiopexy and circumcision. Among school-age children, we studied laparoscopic appendectomy, tonsillectomy, adenoidectomy only, dental surgery, orchiopexy and circumcision. Among preschool-age children, we studied tonsillectomy, adenoidectomy only, dental surgery, orchiopexy and circumcision.
We defined baseline comorbidities in the 90 days prior to surgery using International Classification of Diseases (ICD) 9th and 10th revision diagnosis codes (Appendix Table 2) for obstructive sleep apnea (OSA), history of substance abuse, history of overdose, depression, and chronic conditions categorized into ten systems using the Pediatric Complex Chronic Conditions (CCC) classification, Version 2.20
Outcome measures
Our primary outcome was the likelihood of filling an opioid prescription within 7 days of surgery. We included both liquid and tablet formulations, if applicable, of the following medications: codeine, hydrocodone, hydromorphone, morphine, oxycodone and tramadol. The secondary outcome was the total amount of opioid dispensed in the first prescription, measured in MME, which we calculated using standard tables.21 We also examined the average days supplied in the initial prescription and the percentage of patients who received more than one opioid prescription (refill) in the first 30 days after surgery.
Statistical analysis
We compared the distribution of procedures and patient characteristics over the study period and used descriptive statistics and simple hypothesis tests to characterize outcome distribution. By age group and surgery, we plotted the percentage of patients who filled a prescription, the average MME dispensed, days supplied and the percentage who filled more than one prescription to visually examine changes in prescribing outcomes.
We performed a Joinpoint regression analysis for prescription likelihood and MME dispensed to characterize changes over time in outcome trends. Joinpoint regression is a method to describe change in trends over time and to assess if a significant increase or decrease in rate occurred at a discrete moment in time.22, 23 The logistic-linear regression Joinpoint model evaluates a null hypothesis of no change in trend versus a pre-set maximum number of changes and displays the quarterly change that is specific to the trend after versus before a given moment in time where a change in trend is evaluated (i.e., the “Joinpoint”).23 For scenarios where our initial model rejected the null hypothesis of no change (i.e. a change is identified), we assessed if the data were best described with one or two Joinpoints.23
We subsequently performed a linear time series segmented regression analysis for each age group that examined the likelihood of receiving a prescription and included covariates for Joinpoint pre-post time intervals, the interaction between intervals and quarter, gender, surgery type and obstructive sleep apnea diagnosis to verify that differences in trends before vs after identified Joinpoints persisted after controlling for potential confounders. A three-month calendar quarter was selected as the unit of time for these models. Analyses were conducted in SAS (version 9.4, SAS Institute, Cary, NC) and the Joinpoint Trend Analysis Software (Version 4.8.0.1, National Cancer Institute, Bethesda, MD). All tests were two-sided and significance was set at the 5% level.
RESULTS
Overview
The study cohort included 124,249 patients; 45.0% were female, and the median age was 7.0 years (interquartile ratio (IQR) 4.0–14.0 years) (Table 1). There were 43,487 adolescents (35.1% of the sample), 40,221 (32.5%) school-age children and 40,541 (32.7%) children under age 5. Overall, the most common comorbidities were obstructive sleep apnea (N=18,891; 15.2%, p<0.001), history of congenital defect (N=2,103; 1.7%, p<0.001) and history of cardiovascular diagnosis (N=1,615; 1.3%, p<0.001). 66.4% (N=82,445) of children were White, 9.6% (N=11,989) identified as Hispanic/Latino, 5.7% (N=7,190) were Black or African American and 3.0% (N=3,681) were Asian.
Table 1.
Surgical patient and procedure characteristics, by age group
| Variable/Age group | Infant to preschool-age, 0 to 4 years, N=40,541(32.6%) | School-aged children, 5 to 10 years, N=40,221(32.4%) | Adolescents, 11 to 17 years, N=43,487(35.0%) | Overall (N=124,249) |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age, median (IQR) | 3.0 (1.0–4.0) | 7.0 (5.0–8.0) | 15.0 (13.0–16.0) | 7.0 (4.0–14.0) |
| Female gender, N(%) | 15,345 (38.0%) | 18,191 (45.5%) | 22,124 (50.9%) | 55,880 (45.0%) |
| Surgical procedures | ||||
| Adenoidectomy | 13,515 (33.5%) | 6,048 (15.1%) | 1,604 (3.7%) | 21,167 (17.1%) |
| Appendectomy a | 2,285 (5.7%) | 6,143 (14.1%) | 8,565 (6.9%) | |
| Arthroscopic knee surgery | 11,816 (27.2%) | 12,093 (9.7%) | ||
| Cholecystectomy | 1,165 (2.7%) | 1,239 (1.0%) | ||
| Circumcision | 5,747 (14.2%) | 1,450 (3.6%) | 1,249 (2.9%) | 8,446 (6.8%) |
| Dental surgery | 6,200 (15.4%) | 5,747 (14.4%) | 10,320 (23.7%) | 22,267 (17.9%) |
| Orchiopexy | 1,388 (3.4%) | 1,319 (3.3%) | 1,367 (3.1%) | 4,074 (3.3%) |
| Tonsillectomy +/− Adenoidectomy | 13,540 (33.5%) | 23,098 (57.8%) | 9,823 (22.6%) | 46,461 (37.4%) |
| Common comorbidities | ||||
| Obstructive sleep apnea history, N(%) | 7,575 (18.8%) | 8,974 (22.5%) | 2,339 (5.4%) | 18,891 (15.2%) |
| Congenital defect diagnosis, N(%) | 794 (2.0%) | 590 (1.5%) | 709 (1.6%) | 2,103 (1.7%) |
| Cardiovascular diagnosis, N(%) | 626 (1.5%) | 492 (1.2%) | 490 (1.1%) | 1,615 (1.3%) |
| Neurologic/neuromuscular diagnosis N(%) | 428 (1.1%) | 449 (1.1%) | 385 (0.9%) | 1,262 (1.0%) |
| Race/Ethnicity | ||||
| White, non-Hispanic | 24,950 (61.8%) | 26,872 (67.3%) | 30,348 (69.8%) | 82,445 (66.4%) |
| Black or African American | 2,412 (6.0%) | 2,182 (5.5%) | 2,493 (5.7%) | 7,190 (5.7%) |
| Asian, non-Hispanic | 1,244 (3.1%) | 1,267 (3.2%) | 1,162 (2.7%) | 3,681 (3.0%) |
| Hispanic/Latino | 3,487 (8.6%) | 4,227 (10.6%) | 4,219 (9.7%) | 11,989 (9.6%) |
| Other/Unknown | 8,297 (20.5%) | 5,399 (13.5%) | 5,265 (12.1%) | 19,025 (15.3%) |
Procedures with less than 100 occurrences across 12 calendar months were not included in age brackets
Comorbidities with <1% prevalence were not included.
Among all children, the three most commonly performed surgeries were tonsillectomy with or without adenoidectomy (N=46,461; 37.4%, p<0.001), dental surgery (N=22,267; 17.9%, p<0.001) and adenoidectomy only (N=21,167; 17.1%, p<0.001). Among adolescents, the three most common procedures were knee arthroscopy (N=11,816, 27.2%), dental surgery (N=10,320, 23.7%) and tonsillectomy (N=9,823, 22.6%). School-age children most commonly underwent tonsillectomy (N=23,098, 57.8%) followed by adenoidectomy only (N=6,048, 15.1%) and dental surgery (N=5,747, 14.4%). Among preschool children, tonsillectomy was the most common surgery (N=13,540, 33.5%), followed by adenoidectomy only (N=13,515, 33.5%) and dental surgery (N=6,200, 15.4%).
Prescription likelihood, average MME, days supplied and refill trends over time
Comparing the first quarter of the five-year study period to the last quarter, the percentage filling an opioid prescription after surgery decreased from 78.2% (95% CI 76.3–80.1%) to 48.0% (95% CI 45.8–50.1%) among adolescents, from 53.9% (95% CI 51.6–56.2%) to 25.5% (95% CI 23.5–27.5%) among school-age children and from 30.4% (95% CI 28.6–32.2%) to 11.5% (95% CI 10.1–12.9%) among preschool children (p<0.001 for all groups; Figure 1). The likelihood of receiving a prescription varied across procedures; among adolescents, opioids were most common after knee arthroscopy, tonsillectomy, orchiopexy and laparoscopic cholecystectomy, while in preschool and school-age children, opioids were most commonly prescribed after orchiopexy, tonsillectomy and circumcision.
Figure 1. Percentage of Children Who Received a Prescription for Opioids After Surgery, Overall and by Procedure, 2014–2019.
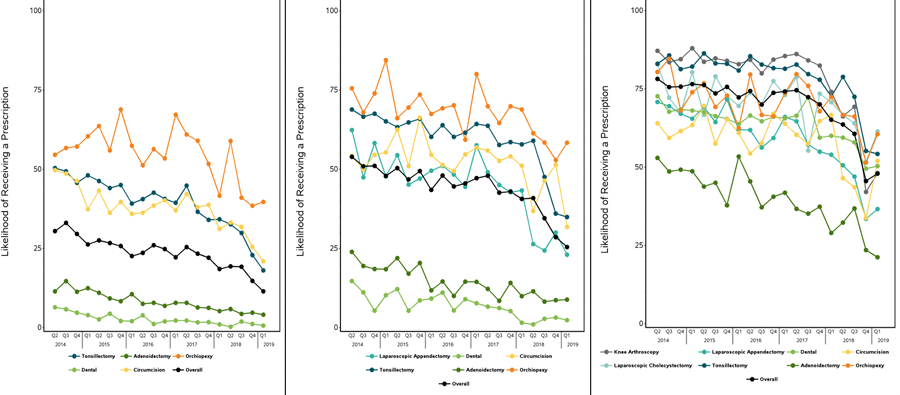
Each figure displays, by year, the percentage of children undergoing a given surgery who did not receive a prescription for opioids when an equivalent recovery without opioids was considered possible. Panels show data for the relevant procedures specific to the three age groups: (A) Infant to 4 years (B) 5 to 10 years (C) 11 to 17 years
The average MME dispensed in the first prescription declined over the study period from 228.9 (95% CI 220.1–237.7) to 110.8 (95% CI 105.6–115.9) among adolescents, from 121.3 (95% CI 116.7–125.9) to 65.9 (95% CI 61.1–70.7) among school-age children and from 75.3 (95% CI 70.2–80.3) to 33.2 (95% CI 30.1–36.3) among preschool children. (p<0.001 for all groups; Figure 2). The average days’ supply in the first prescription declined over the study period from 5.2 days (95% CI 5.1–5.4) to 3.0 days (95% CI 2.9–3.1) among adolescents, 7.7 days (95% CI 7.4–7.9) to 3.4 days (95% CI 3.2–3.6) among school-age children and 8.0 days (95% CI 7.6–8.3) to 3.3 days (95% CI 3.1–3.6) among preschool children (Appendix Figure 2). The likelihood of receiving an opioid refill decreased from 12.7% (95% CI 11.1–14.3%) to 5.4% (95% CI 4.4–6.3%) among adolescents, 5.1% (95% CI 4.1–6.1%) to 3.1% (95% CI 2.3–3.8%) among school-age children and 1.6% (95% CI 1.1–2.1%) to 0.51% (95% CI 0.21–0.81%) among preschool-age children (p<0.001 for all comparisons; Appendix Figure 1). Hydrocodone was the most commonly prescribed opioid among all three groups over the study period, followed by oxycodone; while the likelihood of filling a hydrocodone prescription reflected overall trends, oxycodone prescribing remained static overall in the two younger age groups until a modest decline was noted beginning in 2018 (Appendix Figure 3).
Figure 2. Postoperative Opioid Prescription Quantity, Among Children Who Received an Opioid Prescription, Overall and by Procedure, 2014–2019.
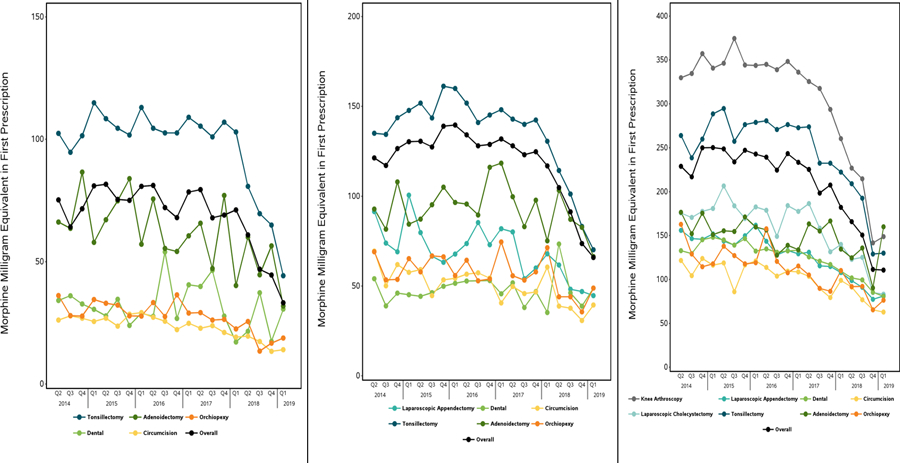
Panels show total amount of opioid in Morphine Milligram Equivalents (MME) dispensed in the first opioid prescription filled within 7 days after surgeries specific to the three age groups: (A) Infant to 4 years (B) 5 to 10 years (C) 11 to 17 years
Joinpoint regression
Our Joinpoint analysis of temporal trends in the likelihood of filling an opioid prescription revealed an initial period of gradual change, followed by a period of more rapid decline (Figure 3; Table 2). While this pattern occurred in all age groups, the timing of the trend change differed by age. Adolescents were the first to demonstrate a sharp change in the likelihood of filling a prescription. The quarterly decrease in prescribing was 0.47%/quarter (p=0.04 for trend) until Quarter 4 of 2017, when it decreased to 8.3%/quarter (p<0.001) between Quarter 4 of 2017 and Quarter 1 of 2019. School-age children followed a similar trajectory with a decrease of 1.4%/quarter (p<0.001) from the beginning of the study period until Quarter 2 of 2018; after this point, prescribing decreased by 17.6%/quarter (p<0.001) until the end of the study period. Among preschool children, prescribing decreased slightly until Quarter 3 of 2018 (2.6%/quarter, p<0.001) when it began to decline rapidly (27.5%/quarter, p=0.09). Similar patterns were observed in Joinpoint regressions examining trends in average MME dispensed over time. We also confirmed the changes in trends identified by Joinpoint regression for odds of receiving a prescription in a segmented regression analysis that controlled for potential confounders (Appendix Table 3).
Figure 3. Joinpoint Regression Models, by Age Group, 2014–2019.
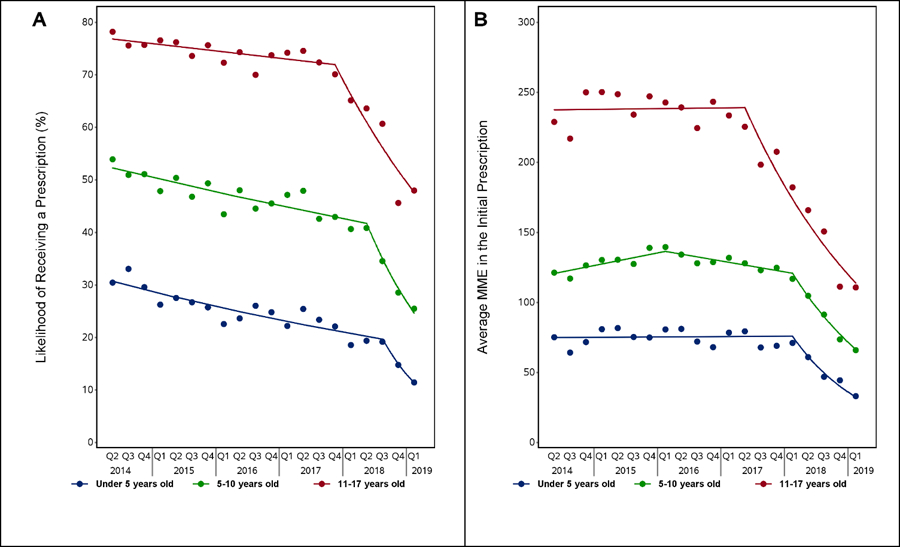
Panels show (A) the likelihood of receiving an opioid prescription after surgery and (B) the total amount of opioid in Morphine Milligram Equivalents (MME) dispensed in the first opioid prescription filled within 7 days after surgery, specific to the three age groups
Table 2.
Joinpoint regression analysis for likelihood of receiving an opioid prescription and average MME, if issued, by age group
| Likelihood of receiving a prescription | Average MME dispensed in initial prescription | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trend 1 | Trend 2 | Trend 1 | Trend 2 | Trend 3 | ||||||
| Quarter percentage change (SE) | p-value | Quarter percentage change (SE) | p-value | Quarter percentage change (SE) | p-value | Quarter percentage change (SE) | p-value | Quarter percentage change (SE) | p-value | |
| 0–4 years | −2.6% (0.003) | <0.001 | −27.5% (0.15) | 0.09 | 0.09% (0.005) | 0.85 | −21.2% (0.04) | <0.001 | ||
| 5–10 years | −1.4% (0.002) | <0.001 | −17.6% (0.04) | <0.001 | 1.8% (0.004) | 0.002 | −1.5% (0.005) | 0.007 | −14.9% (0.02) | <0.001 |
| 11–17 years | −0.4% (0.002) | 0.04 | −8.3% (0.02) | <0.001 | 0.06% (0.006) | 0.92 | −10.6% (0.01) | <0.001 | ||
DISCUSSION
Among 124,249 opioid-naïve children undergoing 8 common pediatric surgeries between 2014 to 2019, opioid prescribing declined substantially over time; prescribing first decreased gradually from 2014 through late 2017, followed by a more rapid period of decline from 2017 through 2019. Both the onset and the magnitude of decrease in the likelihood of filling an opioid prescription differed for adolescents, school-age and preschool children. Overall, prescribing was more common as age increased. We noted that the rate of decline in prescribing likelihood was steeper among younger children and that they received an increased days’ supply compared to adolescents. With regard to the average MME dispensed, we noted similar trends in the rate of decline that began first among adolescents. As an example of change in prescribing trends, the average preschool-age child who filled an opioid prescription at the beginning of the study period received 75.3 MME, approximately 15 5mg hydrocodone tablets, and 33.2 MME, approximately 6.5 5mg tablets, at the end of the study period. The latter amount is equivalent to a 7-day supply for an average 4-year-old.
Our Joinpoint analyses characterized specific moments in time when rapid de-escalation of routine opioid prescribing began. The drop in prescribing occurred first among adolescents in Quarter 4 of 2017. School-age children followed a similar pattern in Quarter 2 of 2018. Preschool-age children were noted to begin to exhibit this decrease three months later in Quarter 3 of 2018. The results do not identify the specific events that caused these declines, however, there are several possible explanations. First, the declines in prescribing may have been a delayed response to the Food and Drug Administration (FDA) April 2017 restriction on use of tramadol and codeine in children and to increased attention placed on risks of opioid prescribing after pediatric surgery when they were not needed.24 However, these recommendations focused on children under age 12, while changes were first seen among adolescents. Second, a series of studies that discussed the risks of opioid prescribing after pediatric surgery, including potential risks of new chronic use with excessive prescribing,9, 10 were published in early 2018. It is possible that increasing general awareness of these risks prior to study publication may have contributed to prescribing decline when it was not indicated. Third, in a previous study, our group identified decreases in opioid prescribing after surgery associated with release of a guideline on opioid prescribing for chronic pain by the US Centers for Disease Control and Prevention in March 2016.25 It is possible that decreases observed in children could reflect a ‘spillover effect’ of these guidelines from adult to pediatric prescribers. Of note, Renny et al. utilized pharmacy claims data to identify an overall downtrend in all-cause pediatric opioid prescriptions between 2006–2018, suggesting that the declines observed here may be reflective of broader trends away from opioids for pain management in children that were not limited to the context of surgery.13 It is also possible that local or state policy changes, health system initiatives, or insurer policies for coverage of pain treatments may have contributed to changes over time in opioid dispensing trends after surgery in children
Our findings have helped to fill significant gaps in knowledge with regard to opioid dispensing and pain management in pediatrics. The trend towards de-adoption identified by our group is supported by a growing body of evidence suggesting that opioids can be discretionary after common pediatric surgeries associated with mild to moderate pain.12, 26 27 For example, society guidelines for the most common surgery studied, tonsillectomy, first recommended non-opioid analgesics as first line therapy in February 2019 after data demonstrated equivalent pain control for most children.28 Increasing knowledge prompted publication of Michigan OPEN’s first national pediatric opioid prescribing range recommendations in May 2020 and the first comprehensive expert consensus guidelines specific to pediatric surgery for discretionary opioid use in January 2021.3, 28 With increasing awareness of multi-modal pain management and new knowledge of prescribing trends specific to each age group and surgery, we recommend use of our results to inform targeted guideline implementation efforts.
LIMITATIONS
This study has limitations. Our patient population was from a private insurance claims database, and it is possible that findings may not be broadly applicable to patients covered by public insurance programs or patients without insurance. We cannot rule out that disparities in pain management did not increase during the study period, and further research is indicated to characterize these disparities. In addition, although we were able to document prescribing trends after surgery, we were unable to characterize the opioid quantity consumed by individual children and their family’s unique perception of post-operative pain management, and additional research is indicated. While we noted that opioid refills decreased over the study period, we were not able to definitively measure pain experience, including pain scores and patient satisfaction. Finally, at the societal level, patient-level variables may have changed over the study period with possible implications for influence on prescribing, but it is reassuring that our study cohort remained demographically similar over time.
CONCLUSIONS
We identified that de-adoption of routine opioid prescribing after common pediatric surgeries occurred during the study period. This trend was first noted in adolescents in late 2017, and it was then identified among school-age and preschool-age children over time. Additional research is indicated to better understand the reasons underlying changes in patterns of opioid prescribing for children of different ages after surgery.
Supplementary Material
Table of Contents Summary
Using Joinpoint regression, our study identified substantial decreases in postoperative opioid dispensing after outpatient pediatric surgeries beginning in 2017.
What’s Known on This Subject
Children who undergo common outpatient surgeries are routinely prescribed opioids, although available evidence suggests they should be used with discretion for procedures associated with mild to moderate pain.
What This Study Adds
Between 2014–2019, study results identified a substantial decrease in both the percentage of children filling an opioid prescription and the opioid quantity dispensed that began in 2017. The onset of this decline differed by age group and surgery.
Funding/Support:
This work is funded R01DA042299 (MDN and HW) from the National Institute on Drug Abuse (North Bethesda, Maryland) and the University of Pennsylvania’s McCabe Foundation (TNS; Philadelphia, Pennsylvania)
Role of Funder:
Neither funding source had any role in the design or conduct of the study.
Abbreviations:
- MME
Morphine Milligram Equivalents
- CPT
Current Procedure Terminology
- ICD
International Classification of Diseases
- OSA
obstructive sleep apnea
Footnotes
Conflict of Interest Disclosures: No authors reported disclosures.
REFERENCES
- 1.Wunsch H, Wijeysundera DN, Passarella MA, Neuman MD. Opioids Prescribed After Low-Risk Surgical Procedures in the United States, 2004–2012. JAMA Apr 19 2016;315(15):1654–7. doi: 10.1001/jama.2016.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franz AM, Martin LD, Liston DE, Latham GJ, Richards MJ, Low DK. In Pursuit of an Opioid-Free Pediatric Ambulatory Surgery Center: A Quality Improvement Initiative. Anesth Analg Mar 1 2021;132(3):788–797. doi: 10.1213/ANE.0000000000004774 [DOI] [PubMed] [Google Scholar]
- 3.Kelley-Quon LI, Kirkpatrick MG, Ricca RL, et al. Guidelines for Opioid Prescribing in Children and Adolescents After Surgery: An Expert Panel Opinion. JAMA Surg Jan 1 2021;156(1):76–90. doi: 10.1001/jamasurg.2020.5045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michigan Opioid Prescribing Engagement Network (OPEN). Prescribing Recommendations URL: https://michigan-open.org/prescribing-recommendations/. Accessed on 25 May 2021.
- 5.Ceelie I, de Wildt SN, van Dijk M, et al. Effect of intravenous paracetamol on postoperative morphine requirements in neonates and infants undergoing major noncardiac surgery: a randomized controlled trial. JAMA Jan 9 2013;309(2):149–54. doi: 10.1001/jama.2012.148050 [DOI] [PubMed] [Google Scholar]
- 6.Kelly LE, Sommer DD, Ramakrishna J, et al. Morphine or Ibuprofen for post-tonsillectomy analgesia: a randomized trial. Pediatrics Feb 2015;135(2):307–13. doi: 10.1542/peds.2014-1906 [DOI] [PubMed] [Google Scholar]
- 7.Moore RA, Derry S, Aldington D, Wiffen PJ. Single dose oral analgesics for acute postoperative pain in adults - an overview of Cochrane reviews. Cochrane Database Syst Rev Sep 28 2015;(9):CD008659. doi: 10.1002/14651858.CD008659.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horton JD, Munawar S, Corrigan C, White D, Cina RA. Inconsistent and excessive opioid prescribing after common pediatric surgical operations. J Pediatr Surg Jul 2019;54(7):1427–1431. doi: 10.1016/j.jpedsurg.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 9.Harbaugh CM, Lee JS, Hu HM, et al. Persistent Opioid Use Among Pediatric Patients After Surgery. Pediatrics Jan 2018;141(1)doi: 10.1542/peds.2017-2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harbaugh CM, Nalliah RP, Hu HM, Englesbe MJ, Waljee JF, Brummett CM. Persistent Opioid Use After Wisdom Tooth Extraction. JAMA Aug 7 2018;320(5):504–506. doi: 10.1001/jama.2018.9023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuman MD, Bateman BT, Wunsch H. Inappropriate opioid prescription after surgery. Lancet Apr 13 2019;393(10180):1547–1557. doi: 10.1016/S0140-6736(19)30428-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Cleve WC, Grigg EB. Variability in opioid prescribing for children undergoing ambulatory surgery in the United States. J Clin Anesth Sep 2017;41:16–20. doi: 10.1016/j.jclinane.2017.05.014 [DOI] [PubMed] [Google Scholar]
- 13.Renny MH, Yin HS, Jent V, Hadland SE, Cerda M. Temporal Trends in Opioid Prescribing Practices in Children, Adolescents, and Younger Adults in the US From 2006 to 2018. JAMA Pediatr Jun 28 2021;doi: 10.1001/jamapediatrics.2021.1832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardin AP, Hackell JM, Committee On P, Ambulatory M. Age Limit of Pediatrics. Pediatrics Sep 2017;140(3)doi: 10.1542/peds.2017-2151 [DOI] [PubMed] [Google Scholar]
- 15.Wiener RS, Welch HG. Trends in the use of the pulmonary artery catheter in the United States, 1993–2004. JAMA Jul 25 2007;298(4):423–9. doi: 10.1001/jama.298.4.423 [DOI] [PubMed] [Google Scholar]
- 16.Optum Research Data Assets: Product Sheets OPTUM. https://www.optum.com/content/dam/optum/resources/productSheets/5302_Data_Assets_Chart_Sheet_ISPOR.pdf. Accessed on December 1 2020.
- 17.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in Opioid Prescribing Through Evidence-Based Prescribing Guidelines. JAMA Surg Mar 1 2018;153(3):285–287. doi: 10.1001/jamasurg.2017.4436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamdar PM, Liddy N, Antonacci C, et al. Opioid Consumption After Knee Arthroscopy. Arthroscopy Mar 2021;37(3):919–923 e10. doi: 10.1016/j.arthro.2020.10.019 [DOI] [PubMed] [Google Scholar]
- 19.Barazanchi AWH, MacFater WS, Rahiri JL, et al. Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth Oct 2018;121(4):787–803. doi: 10.1016/j.bja.2018.06.023 [DOI] [PubMed] [Google Scholar]
- 20.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr Aug 8 2014;14:199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Centers for Medicare and Medicaid Services. Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors. US Centers for Medicare and Medicaid Services,. Accessed April 14, 2019, https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-April-2017.pdf
- 22.Gillis D, Edwards BPM. The utility of joinpoint regression for estimating population parameters given changes in population structure. Heliyon Nov 2019;5(11):e02515. doi: 10.1016/j.heliyon.2019.e02515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med Feb 15 2000;19(3):335–51. doi: [DOI] [PubMed] [Google Scholar]
- 24.US Food and Drug Administration (FDA). FDA Drug Safety Communication: FDA restricts use of prescription codeine pain and cough medicines and tramadol pain medicines in children. Accessed on 1 July 2021 at url: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-restricts-use-prescription-codeine-pain-and-cough-medicines-and.
- 25.Sutherland TN, Wunsch H, Pinto R, et al. Association of the 2016 US Centers for Disease Control and Prevention Opioid Prescribing Guideline With Changes in Opioid Dispensing After Surgery. JAMA Netw Open Jun 1 2021;4(6):e2111826. doi: 10.1001/jamanetworkopen.2021.11826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Monitto CL, Hsu A, Gao S, et al. Opioid Prescribing for the Treatment of Acute Pain in Children on Hospital Discharge. Anesth Analg Dec 2017;125(6):2113–2122. doi: 10.1213/ANE.0000000000002586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stokes SC, Theodorou CM, Brown EG, Saadai P. Variations in Perceptions of Postoperative Opioid Need for Pediatric Surgical Patients. JAMA Surg Jun 23 2021;doi: 10.1001/jamasurg.2021.2076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell RB, Archer SM, Ishman SL, et al. Clinical Practice Guideline: Tonsillectomy in Children (Update)-Executive Summary. Otolaryngol Head Neck Surg Feb 2019;160(2):187–205. doi: 10.1177/0194599818807917 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


