Abstract
Serial passage of SIVmac239 allows for greater understanding of the genetic changes necessary for cross-species transmission of primate lentiviruses into humans. Using humanized mice, we show that adaptive mutations continue to accumulate in SIVmac239 during four serial passages, with persistent CD4+ T cell decline and increases in plasma viral loads.
Keywords: SIVmac239 evolution, rhesus macaques, humanized mice, cross-species SIV transmission, SIVmac239 infection of humanized mice, SIVmac239 cross-species transmission, HIV evolution surrogate model
INTRODUCTION
SIVmac and its derivatives are widely used as models for HIV infection due to their ability to mimic AIDS-like pathogenesis in rhesus macaques.1–4 Previously, we showed successful infection and serial passaging of SIVmac239 as well as other SIVs in the humanized mouse model, which harbors a fully functional human immune system.2–15 Here we characterized SIVmac239 following four serial passages in humanized mice and identified the genetic adaptations that arose following in vivo adaptation to the human immune cell environment. Viral pathogenesis was determined by monitoring plasma viral loads weekly using qRT-PCR and CD4+ T cell decline biweekly using flow cytometry. The resulting virus was subjected to Illumina-based deep sequencing to identify mutations that arose at increasing frequencies within the viral population.
MATERIALS AND METHODS
Generation of hu-HSC mice, infection with SIVmac239 and serial passaging
All animal studies have been approved and reviewed by the Colorado State University Institutional Animal Center and Use Committee (Protocol #1202), and animals were maintained by the CSU Painter Animal Center. The preparation of hu-HSC mice was performed according to the previously described procedures.5,10,11,14–17 A total of 8 mice (3 female; 5 male) were used for these experiments.
A human-cell adapted SIVmac239 strain that was serially passaged three times in humanized mice was used to infect hu-HSC mice as previously described.5 Briefly, mice displaying high plasma viral loads 24 weeks post-inoculation were euthanized and cells were collected to propagate and passage the virus for future serial passages of hu-mice.5,10,11
Assessment of Viral Pathogenesis
Pathogenesis of the virus was determined through plasma viral load detection and assessment of CD4+ T cell decline as described previously.5 Briefly, the E.Z.N.A. Viral RNA kit (Omega bio-tek, Norcross, CA) was used to extract viral RNA from plasma isolated weekly from peripheral blood. Quantification of viral loads was performed using qRT-PCR and SYBR Green with the iScript One-Step RT-PCR kit (BioRad, Hercules, CA) based on the manufacturer’s instructions.5
CD4+ T cell levels were assessed as a fraction of CD45+/CD3+ cells following staining of whole blood using mouse anti-human antibodies CD45-APC (eBioscience), CD3-FITC (eBioscience), and CD4-PE (BD Pharmingen, San Jose, CA) and the BD Accuri C6 cytometer as previously described.5,6 CD4+ T cell decline was assessed relative to uninfected controls using a two-tailed Student’s t-test in GraphPad Prism 8.1.0 (p<0.0001). CD4+ T cell decline and Plasma viral loads were displayed as mean ± SD.
Illumina-based deep sequencing
Overlapping amplicon pools were generated from viral RNA collected from two separate infected mice at 3-, 11-, 19- and 25-weeks post-inoculation using Primal Scheme designed primers as described previously.5,18 Amplicons were prepared for sequencing using the TruSeq Nano DNA Library Preparation Kit and run on the MiSeq Illumina desktop sequencer (Invitrogen, Carlsbad, CA).
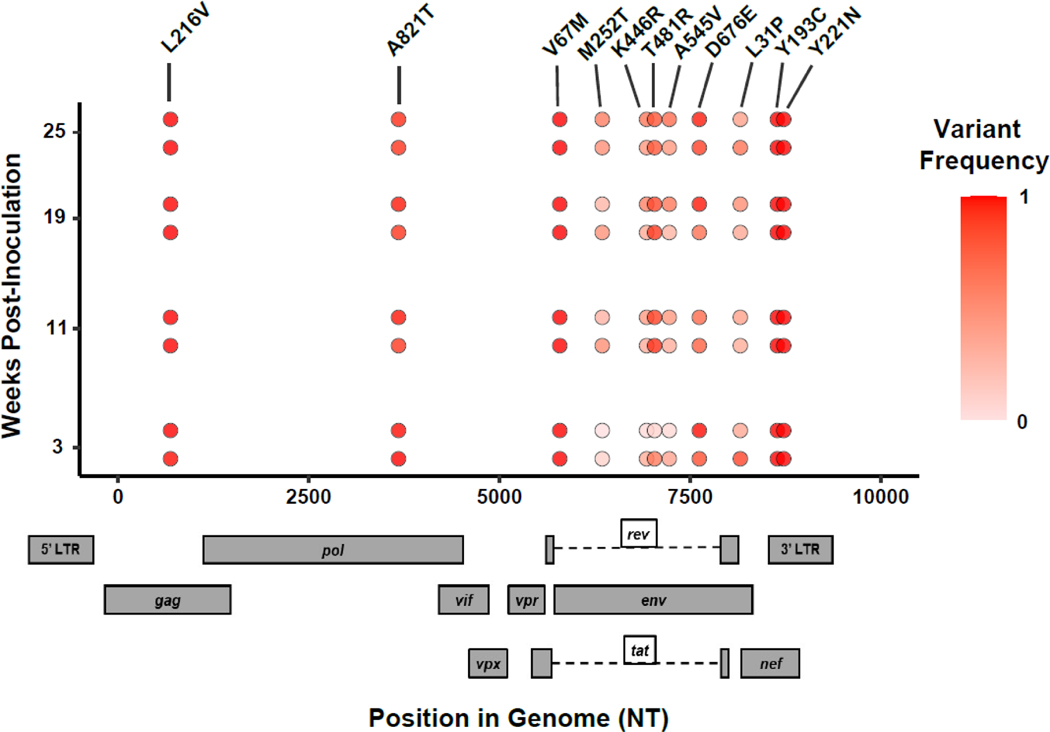
Sequence read processing and variant identification was performed using Geneious Prime v2022.1.1. Paired end reads were merged using BBMerge version 38.84 and read ends were trimmed with a 0.05 error probability rate.19 Reads were mapped against our previously sequenced SIVmac239 reference consensus sequence using Bowtie2 v2.3.0.5,20 SNPs were identified based on a minimum variant frequency of 0.5 and minimum depth of coverage of 100 reads. R and ggplot2 (ISBN: 0387981403) scripts were used to create the genome plot and can be found at https://github.com/stenglein-lab/viral_variant_explorer. Raw sequencing data was deposited to the Sequence Read Archive and are publicly available (Accession Numbers: SRR17194610; SRR20736401-SRR2073606; SRR20736413-SRR2073614)
RESULTS
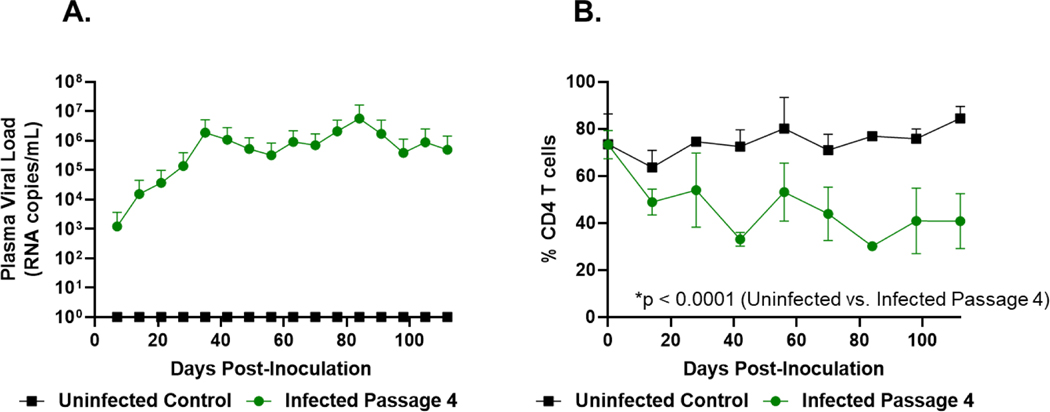
The hu-mouse adapted SIVmac239 fourth passage virus was able to cause viremia with a rapid increase in viral loads reaching a titer of over 1×106 RNA copies/mL within 35 days before peaking around 84 days post-inoculation and gradually declining (Figure 1A). CD4+ T cell decline was observed within two weeks of infection, with a significant, but gradual decline continuing throughout the rest of the viremic phase relative to the uninfected control (*p < 0.0001; Figure 1B). In addition to mutations identified in previous serial passages, we found that the frequency of nonsynonymous SNPs producing M252T, K446R and A545V in env and L31P in nef had increased to >50% of the viral population by the end of the fourth serial passage (Figure 2).5 Additionally, we determined using Geno2pheno that the adapted virus is still primarily a CCR5-tropic virus and has not yet shifted to either an X4 or dual-tropic phenotype by the end of the fourth generation of serial passaging.21
Figure 1. SIVmac239 Plasma Viral Loads and CD4+ T cell decline after four serial passages.
(A) SIVmac239 fourth passage plasma viral loads. Plasma viral loads peaked around 84 days post-inoculation. (B) SIVmac239 fourth passage CD4+ T cell decline. Both data sets are represented as mean ± SD. CD4+ depletion was significant by the end of the serial passage (two-tailed Student’s t-test, p<0.0001).
Figure 2. Nonsynonymous mutations occurring at >50% frequency following four serial passages of SIVmac239.
SNPs identified had a minimum variant frequency of ≥50% and required ≥100 read depth of coverage.
DISCUSSION
The fourth serial passage of SIVmac239 contrasts the earlier passages in both pathogenesis and genetic changes.5 The first three passages showed moderate increases in viral loads, while the fourth passage starting viral loads were greater than 1×103 RNA copies/mL, and continued to rise over 3 logs relatively quickly. This suggests that the fourth serial passage virus is more adapted to human cells than earlier passages.5 Additionally, while CD4+ T cell decline was significant relative to the uninfected controls, there was not as large of a difference between the previous passages and the fourth serial passage relative to the differences in viral loads.5 This indicates that genetic changes that arise in this passage had a greater impact on plasma viral loads than on CD4+ T cell decline.
While the majority of the previously identified mutations were maintained at high frequencies within the viral population, several mutations in env and nef rose above 50% frequency that were not previously seen.5 Furthermore, the retention of previously identified high frequency mutations indicates importance for countering increased fitness for viral replication in the human. Future functional studies on these mutations are likely to shed more light on their specific roles in human host adaptation.
ACKNOWLEDGEMENTS
This research was possible thanks to NIH, USA grant R01 AI123234 to R. A. in addition to the National Center for Research Resources and the Office of Research Infrastructure Programs (ORIP) of the NIH through grant OD011104 at the Tulane National Primate Research Center and NIH grant P51OD011106 at the Wisconsin Primate Research Center. Computational resources were supported by NIH-NCATS Colorado CTSA Grant Number UL1 TR002535. Additional support was provided by the ADEAR Training Program NIH Grant T32AI150547.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors confirm that there are no conflicts of interest involved with these studies.
REFERENCES
- 1.Apetrei C et al. Molecular epidemiology of simian immunodeficiency virus SIVsm in U.S. primate centers unravels the origin of SIVmac and SIVstm. J Virol 79, 8991–9005 (2005). 10.1128/JVI.79.14.8991-9005.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kestler H et al. Induction of AIDS in rhesus monkeys by molecularly cloned simian immunodeficiency virus. Science 248, 1109–1112 (1990). 10.1126/science.2160735 [DOI] [PubMed] [Google Scholar]
- 3.Naidu YM et al. Characterization of infectious molecular clones of simian immunodeficiency virus (SIVmac) and human immunodeficiency virus type 2: persistent infection of rhesus monkeys with molecularly cloned SIVmac. J Virol 62, 4691–4696 (1988). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daniel MD et al. Isolation of T-cell tropic HTLV-III-like retrovirus from macaques. Science 228, 1201–1204 (1985). 10.1126/science.3159089 [DOI] [PubMed] [Google Scholar]
- 5.Curlin JZ et al. In vivo Infection Dynamics and Human Adaptive Changes of SIVsm-Derived Viral Siblings SIVmac239, SIVB670, and SIVhu in Humanized Mice as a Paralog of HIV-2 Genesis. Frontiers in Virology 1 (2021). 10.3389/fviro.2021.813606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curlin J et al. Evolution of SIVsm in humanized mice towards HIV-2. J Med Primatol (2020). 10.1111/jmp.12486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curlin J et al. SIVcpz cross-species transmission and viral evolution toward HIV-1 in a humanized mouse model. J Med Primatol 49, 40–43 (2020). 10.1111/jmp.12440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmitt K et al. SIV progenitor evolution toward HIV: A humanized mouse surrogate model for SIVsm adaptation toward HIV-2. J Med Primatol 47, 298–301 (2018). 10.1111/jmp.12380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmitt K et al. Mimicking SIV chimpanzee viral evolution toward HIV-1 during cross-species transmission. J Med Primatol 49, 284–287 (2020). 10.1111/jmp.12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmitt K et al. Cross-Species Transmission and Evolution of SIV Chimpanzee Progenitor Viruses Toward HIV-1 in Humanized Mice. Frontiers in Microbiology 11 (2020). 10.3389/fmicb.2020.01889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmitt K et al. Modeling the evolution of SIV sooty mangabey progenitor virus towards HIV-2 using humanized mice. Virology 510, 175–184 (2017). 10.1016/j.virol.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphey-Corb M et al. Isolation of an HTLV-III-related retrovirus from macaques with simian AIDS and its possible origin in asymptomatic mangabeys. Nature 321, 435–437 (1986). 10.1038/321435a0 [DOI] [PubMed] [Google Scholar]
- 13.Akkina R. New generation humanized mice for virus research: comparative aspects and future prospects. Virology 435, 14–28 (2013). 10.1016/j.virol.2012.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akkina RK, Rosenblatt JD, Campbell AG, Chen IS & Zack JA. Modeling human lymphoid precursor cell gene therapy in the SCID-hu mouse. Blood 84, 1393–1398 (1994). [PubMed] [Google Scholar]
- 15.Bai J et al. Characterization of anti-CCR5 ribozyme-transduced CD34+ hematopoietic progenitor cells in vitro and in a SCID-hu mouse model in vivo. Mol Ther 1, 244–254 (2000). 10.1006/mthe.2000.0038 [DOI] [PubMed] [Google Scholar]
- 16.Berges BK, Akkina SR, Folkvord JM, Connick E & Akkina R. Mucosal transmission of R5 and X4 tropic HIV-1 via vaginal and rectal routes in humanized Rag2−/− gammac −/− (RAG-hu) mice. Virology 373, 342–351 (2008). 10.1016/j.virol.2007.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veselinovic M, Charlins P & Akkina R. Modeling HIV-1 Mucosal Transmission and Prevention in Humanized Mice. Methods Mol Biol 1354, 203–220 (2016). 10.1007/978-1-4939-3046-3_14 [DOI] [PubMed] [Google Scholar]
- 18.Quick J et al. Multiplex PCR method for MinION and Illumina sequencing of Zika and other virus genomes directly from clinical samples. Nat Protoc 12, 1261–1276 (2017). 10.1038/nprot.2017.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bushnell B, Rood J & Singer E. BBMerge - Accurate paired shotgun read merging via overlap. PLoS One 12, e0185056 (2017). 10.1371/journal.pone.0185056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Langmead B & Salzberg SL. Fast gapped-read alignment with Bowtie 2. Nat Methods 9, 357–359 (2012). 10.1038/nmeth.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doring M et al. geno2pheno[ngs-freq]: a genotypic interpretation system for identifying viral drug resistance using next-generation sequencing data. Nucleic Acids Res 46, W271–W277 (2018). 10.1093/nar/gky349 [DOI] [PMC free article] [PubMed] [Google Scholar]