Abstract
Objective:
To identify a signature lipid profile from cerebral thrombi in acute ischemic stroke (AIS) patients at the time of ictus.
Methods:
We performed untargeted lipidomics analysis using liquid chromatography-mass spectrometry (LC-MS) on cerebral thrombi taken from a non-probability, convenience sampling of adult subjects (≥ 18 years of age, n = 5) who underwent thrombectomy for acute cerebrovascular occlusion. The data were classified using Random Forest (RF), a machine learning algorithm.
Results:
The top 10 metabolites identified from the RF analysis were of the glycerophospholipid species and fatty acids.
Conclusion:
Preliminary analysis demonstrates feasibility of identification of lipid metabolomic profiling in cerebral thrombi retrieved from AIS patients. Recent advances in omic methodologies enable lipidomic profiling, which may provide insight into the cellular metabolic pathophysiology caused by AIS. Understanding of lipidomic changes in AIS may illuminate specific metabolite and lipid pathways involved and further the potential to develop personalized preventive strategies.
INTRODUCTION
Ischemic stroke is the second leading cause of death and one of the leading causes of disability globally.1 The consequences of AIS are both individual and social, leading to an estimated $34 billion annually in direct and indirect costs, primarily due to lost productivity.1 In AIS, the blockage caused by the cerebral thrombus produces initial hypoxic damage, followed by inflammation and disturbances of lipid metabolism.2,3 There is limited research examining the effects of the physiological lipidomic changes associated with adults following AIS. AIS treatments focus on removing the thrombus and re-establishing cerebral blood flow as quickly as possible, via intravenous lytics (tissue plasminogen activator [tPA] or mechanical thrombectomy [MT]).4–6 MT provides a novel opportunity to study lipid metabolism by allowing researchers to collect the aspirated thrombus and blood from the infarct zone.7,8
There is evidence of interactions between plasma lipoproteins in ruptured atherosclerotic plaques and platelet function.9 Some patient population groups (e.g. hypercholesterolemia), have evidence of abnormal platelet function, which is mediated by the binding of lipoproteins, especially oxidized LDL, to surface receptors.10 In addition, abnormal plasma lipid levels precipitate membrane composition changes by increasing the cholesterol to phospholipid ratio.11 The resulting changes in microviscosity seem to affect transmembrane signaling and may influence receptor binding.11 This not only has important implications with regard to preventive lipid-lowering drug therapy but also with regard to the development of more focused therapeutics in the setting of acute stroke. New science is emerging on the role of the human microbiota in ischemic stroke, and processes resulting from human host-microbial interactions.12,13 Metabolic and other cellular debris within stroke thrombi may provide valuable information as to origin and perhaps inform future treatment.
A limited number of studies have analyzed the histological contents of retrieved cerebral thrombi. These analyses have largely focused on the thrombus morphology and the relative concentration of erythrocytes, leucocytes, platelets, and fibrin within the thrombus.14,15 These human host-derived structural components aid in the selection of devices used in thrombectomy, and have also been correlated with efficacy of tPA.16 Other omic studies have identified 50 unique microRNA signatures in cerebral thrombi from AIS patients (n = 55; 71 years old) that correlate with stroke subtype etiology (large artery atherosclerosis, cardioembolism with atrial fibrillation, and cardioembolism with valvular heart disease).17 Recently, non-human host components of cerebral thrombi have also been described. Patrakka et al. identified bacterial signatures in cerebral thrombi (Steptococcus species, mainly S. mitis, Porphyromonas gingivalis, and Aggregatibacter actinomycetemcomitans) from AIS patients (n = 75; 67 years old).18 Bacterial DNA was detected in 84% of aspirated thrombus samples. The Streptococcus species DNA contained approximately five times more S. mitis DNA in samples from AIS patients compared to controls.18
These studies demonstrate that analysis of thrombus structure is important, but there is a critical knowledge gap related to the functional components within thrombus. Lipidomic profiling is a powerful tool enabling large-scale study of pathways and networks of lipid metabolites in a biological system at a specific point in time.19 Sphingomyelin, ceramide, and cholesterol are involved in structural and functional integrity of neuronal membranes and mediate inflammatory responses.20 Changes in membrane sphingolipids and cholesterol may lead to changes in membrane permeability and result in neurodegeneration. Characterization of the lipid profile from cerebral thrombi in AIS has the potential to elucidate additional pathophysiological mechanisms underlying AIS, offering new avenues of research related to stroke etiology and prevention. The purpose of the study was to identify a signature lipid profile from cerebral thrombi in acute ischemic stroke (AIS) patients at the time of ictus.
MATERIALS AND METHODS
Study Design.
A prospective observational study design was used to identify a signature lipid profile from cerebral thrombi in acute ischemic stroke patients at the time of ictus. This study was conducted at a large academic comprehensive stroke center in Seattle, Washington. Thrombi not required for clinical studies were collected for this investigation from May 2020 through December 2020. Specimens were retrieved during standard-of-care procedures and preserved utilizing a tissue banking protocol optimized for omic analysis. This study was a non-probability, convenience sampling of adult subjects (≥ 18 years of age) who underwent thrombectomy for large vessel occlusion. All subjects were documented to be COVID negative at the time of thrombectomy. The Institutional Review Board of the University of Washington approved the study.
Study Setting.
Adult patients (≥18 years old) were eligible for inclusion if they underwent mechanical thrombectomy for large vessel occlusion as defined by established guidelines21, and a thrombus was retrieved for analysis.
Data Collection.
A medical record review was conducted to collect admission clinical and demographic variables. These variables included: age, sex, ethnicity, race, body mass index (BMI), chronic comorbid conditions, smoking status, lipid panel on admission, home medication, lytic treatment, National Institutes of Health Stroke Scale (NIHSS) on admission, and time of last known well (LKW) symptom (prior to ischemic stroke). Additionally, endpoint variables were collected, thrombolysis in cerebral infarction (TICI) scores, stroke location, and NIHSS at discharge. Clinical and demographic variables, along with post-thrombectomy endpoints were de-identified and maintained in our institution’s REDCap software.
Thrombus Collection and Storage.
During the thrombectomy, a combined technique was used. In addition to stent retriever, aspiration was applied through an intermediate catheter as well as a large-bore guide catheter positioned in the cervical carotid to help ensure first pass reperfusion. Because the thrombus is frequently adherent to the stent retriever or catheters, it must be washed with sterile saline and gently manipulated in order for transfer into the sterile collection receptable. All thrombi were retrieved after a single pass, to minimize confounding effects from vascular injury and/or blood products that may accumulate after multiple passes are attempted. Thrombus samples were transferred to the −80°C freezer at the conclusion of the procedure, within 4 hours of collection, and stored until lipidomic analysis.
Untargeted Lipidomics Approach.
Materials: Materials: LC–MS grade methanol, dichloromethane, and ammonium acetate were purchased from Fisher Scientific (Pittsburgh, PA) and HPLC grade 1-propanol was purchased from Sigma-Aldrich (Saint Louis, MO). Milli-Q water was obtained from an in-house Ultrapure Water System by EMD Millipore (Billerica, MA). The Lipidyzer isotope labeled internal standards mixture consisting of 54 isotopes from 13 lipid classes was purchased from Sciex (Framingham, MA).
Sample preparation.
Untargeted lipidomic profiling was conducted at the University of Washington’s Northwest Metabolomics Research Center in December 2020. Each thrombus sample was weighed at room temperature (25°C). Since the weights did not match the appearance after homogenization, 10% of the homogenized sample was taken to measure protein by BCA. Based on the protein results, the amount of homogenized sample was scaled to aliquot for lipid extraction so that the sample amounts were similar. Each sample homogenization was transferred to a borosilicate glass culture tube (16 × 100 mm). Next, 250μL of water, 1 mL of methanol, and 450μL of dichloromethane were added to all samples. The mixture was vortexed for 5s and 25μL of the isotope labeled internal standards mixture were added to the tube. Samples were left to incubate at room temperature for 30 min. Next, another 500μL of water and 450μL of dichloromethane were added to the tube, followed by gentle vortexing for 5s, and centrifugation at 2500×g at 15°C for 10 min. The bottom organic layer was transferred to a new tube and 900μL of dichloromethane was added to the original tube for a second extraction. The combined extracts were concentrated under nitrogen and reconstituted in 250μL of the running solution (10mM ammonium acetate in 50:50 methanol: dichloromethane). A pooled quality control (QC) sample was then made by combining small aliquots (~10μl) from each sample. This pooled QC was analyzed twice for the study samples to serve as a replicate throughout the data set to assess process reproducibility and allow for data normalization to account for any instrument drift.
Liquid chromatography-mass spectrometry.
Quantitative lipidomics was performed with the Sciex Lipidyzer platform consisting of Shimadzu Nexera X2 LC-30AD pumps, a Shimadzu Nexera X2 SIL-30AC autosampler, and a Sciex Q TRAP® 5500 mass spectrometer equipped with SelexION® for differential mobility spectrometry (DMS). 1-propanol was used as the chemical modifier for DMS. Initiation of the samples to the mass spectrometer by flow injection analysis occurred at 8uL/min. Each sample was injected twice, once with the DMS on (PC/PE/ LPC/LPE/SM), and once with the DMS off (CE/CER/DAG/DCER/FFA/HCER/ LCER/TAG). The lipid molecular species were measured using multiple reaction monitoring and positive/ negative polarity switching. Positive ion mode detected lipid classes SM/DAG/CE/CER/ DCER/HCER/DCER/TAG and negative ion mode detected lipid classes LPE/LPC/PC/PE/FFA. A total of approximately 1000 lipids were targeted in the analysis. Overall, 650–700 lipids were detected in the lipid library from the assay.
Statistical Analysis.
Descriptive and frequency statistics (means, standard deviations, frequency distribution, and percentages) were used to characterize AIS subjects. Demographics and baseline characteristics were analyzed using SPSS, version 28 software (IBM, Armonk, NY). Lipid species composition data were analyzed processed using Analyst 1.6.3 and Lipidomics Workflow Manager 1.0.5.0. We determined whether each lipid species had been previously characterized in the Human Metabolome Database (HMDB), LIPIDMAPS, KEGG, and NIST libraries.22,23
Statistical and pathway analyses were carried out using MetaboAnalyst 5.0 (Free Software Foundation), an open-source software for metabolomics/lipidomics.24 MetaboAnalyst 5.0 uses standard hyperparameters including node size, number of trees, and number of features sampled prior to training. MetaboAnalyst supports a wide variety of data input types generated by metabolomic studies including GC/LC-MS raw spectra, MS/NMR peak lists, NMR/MS peak intensity table, NMR/MS spectral bins, and metabolite concentrations.25 The web interface of MetaboAnalyst was implemented based on the JavaServer Faces Technology using the PrimeFaces library (v11.0). The interactive visualization was implemented using JavaScript. The majority of the back-end computations are evaluated by 700+ functions written and built into R (MetaboAnalystR package). Over the past decade, MetaboAnalyst has evolved to become the most widely used platform (> 300,000 users) in the metabolomics community.
Random Forest (RF), a machine learning algorithm, was applied for data analysis. RF is a supervised machine learning classification algorithm used for classification that combines the output of multiple decision trees to reach a single result. RF has been shown to generate accurate and stable predictions for data analysis with relatively small sample sizes. Each forest contained 5,000 trees and each tree was grown from randomly selected 7 features. The importance of each feature was quantified by the mean decrease in accuracy when the feature was excluded from building a forest.26 We removed any metabolite/lipid with > 50% missing values, estimated missing values using K-nearest neighbor, and standardized data by mean and standard deviation. To search for metabolites/lipids from acute ischemic stroke participants, we performed supervised statistical methods for signal selection. The leave-one-person-out cross validation (LOOCV) approach, a k-fold cross validation technique,27 was applied to this data set. LOOCV has been used to validate models where large variations are expected between participants.28 Because of the limitations described above, LOOCV was selected for model validation to reduce bias from standard test/train splits during analysis.29
RESULTS
Sample Characteristics.
Five subjects were included in the present study from the UWCB registry; individual subject characteristics are displayed in Table 1. The average age was 53 ± 26.4 years, and the majority of subjects were male (3 males, 2 females) and white. The most common comorbid conditions were atrial fibrillation (40%) and hypertension (40%). The most common home medications (prior to AIS) were beta-blockers (60%), followed by low dose aspirin (40%) and diuretics (40%). The National Institutes of Health Stroke Scale (NIHSS) was 12 on admission and 6 at discharge (median scores). Cerebral thrombus samples were collected at one of the earliest timepoints (average of 9 hours and 37 minutes from last known well (LKW) to reperfusion time) during an ongoing stroke.
Table 1. Demographic Characteristics of the Sample.
Data are reported as means (SD) unless otherwise noted.
| Persons with Acute Ischemic Stroke (n=5) | |
|---|---|
|
| |
| Male Sex (%) | 60% |
|
| |
| Age (years) | 53.0 (26.4) |
|
| |
| Race | |
| Black | 20% |
| White | 60% |
| Declined | 20% |
|
| |
| Comorbidities and Stroke Risks | |
| Smokers (current) | 60% |
| Atrial Fibrillation | 40% |
| Hypertension | 40% |
| Carotid Stenosis | 10% |
|
| |
| BMI | |
| Under/Normal Weight | 20% |
| Overweight | 40% |
| Obese | 20% |
| Morbidly Obese | 20% |
|
| |
| Lipid Panel on Admission | |
| Total Cholesterol (mg/dl) | 134.2 (23.2) |
| HDL (mg/dl) | 28.8 (16.2) |
| LDL (mg/dl) | 74.0 (21.4) |
| Triglycerides (mg/dl) | 233.4 (155.5) |
|
| |
| Medications (Home) | |
| ACE-I | 20% |
| Low dose ASA | 40% |
| Beta-Blockers | 60% |
| Diuretics | 40% |
| Thyroid Medication | 20% |
|
| |
| NIHSS on Admission | *12 (15.6) |
| Moderate Stroke (5–15) | 60% |
| Severe Stroke (≥ 21) | 40% |
|
| |
| NIHSS on Discharge | *6 (15.5) |
| Minor Stroke (1–4) | 40% |
| Moderate Stroke (5–15) | 20% |
| Severe Stroke (≥ 21) | 40% |
|
| |
| tPA administration | 40% |
|
| |
| Stroke Location | |
| Left MCA | 40% |
| Right MCA | 20% |
| Right ICA | 40% |
|
| |
| TICI Score | |
| 3 = Complete Reperfusion | 100% |
|
| |
| LKW to Reperfusion Time (hours) | 9.4 (2.4) |
Key: ACE-I: angiotensin-converting-enzyme inhibitors; ASA: aspirin; BMI: body mass index; HDL: high density lipoprotein; ICA: internal carotid artery; LDL: low density lipoprotein; LKW: last known well; MCA: middle cerebral artery; M1: proximal intracranial MCA segment; NIHSS: National Institutes of Health stroke scale; SD: standard deviation; TICI: thrombolysis in cerebral infarction; tPA: tissue plasminogen activator
Indicates median
Phospholipids of Cerebral Thrombi.
The top 10 metabolites identified from the preliminary RF analysis were mainly of the glycerophospholipid species (phosphatidylethanolamine, phosphoethanolamine, and phosphocholine) and fatty acids, Figure 1. The ten metabolites were phosphatidylethanolamine ((PE(P-18:1/16:0), HMDB0011371; PE(P-18:1/20:3), HMDB0011391; PE(P-16:0/22:6), HMDB0005780; PE(O-16:0/22:4), HMDB0009009; PE(P-16:0/22:4), HMDB11358), phosphoethanolamine (PE(O-16:0/22:4), HMDB0011158), phosphatidylcholine ((PC(18:0/20:0), HMDB0008043), lignoceric acid/tetracosanoic acid (FFA(24:0), HMDB0002003); flufenamic acid (FFA(20:5), HMDB0252331), and hexadienoic acid (FFA(22:4), HMDB0029581).
Figure 1:
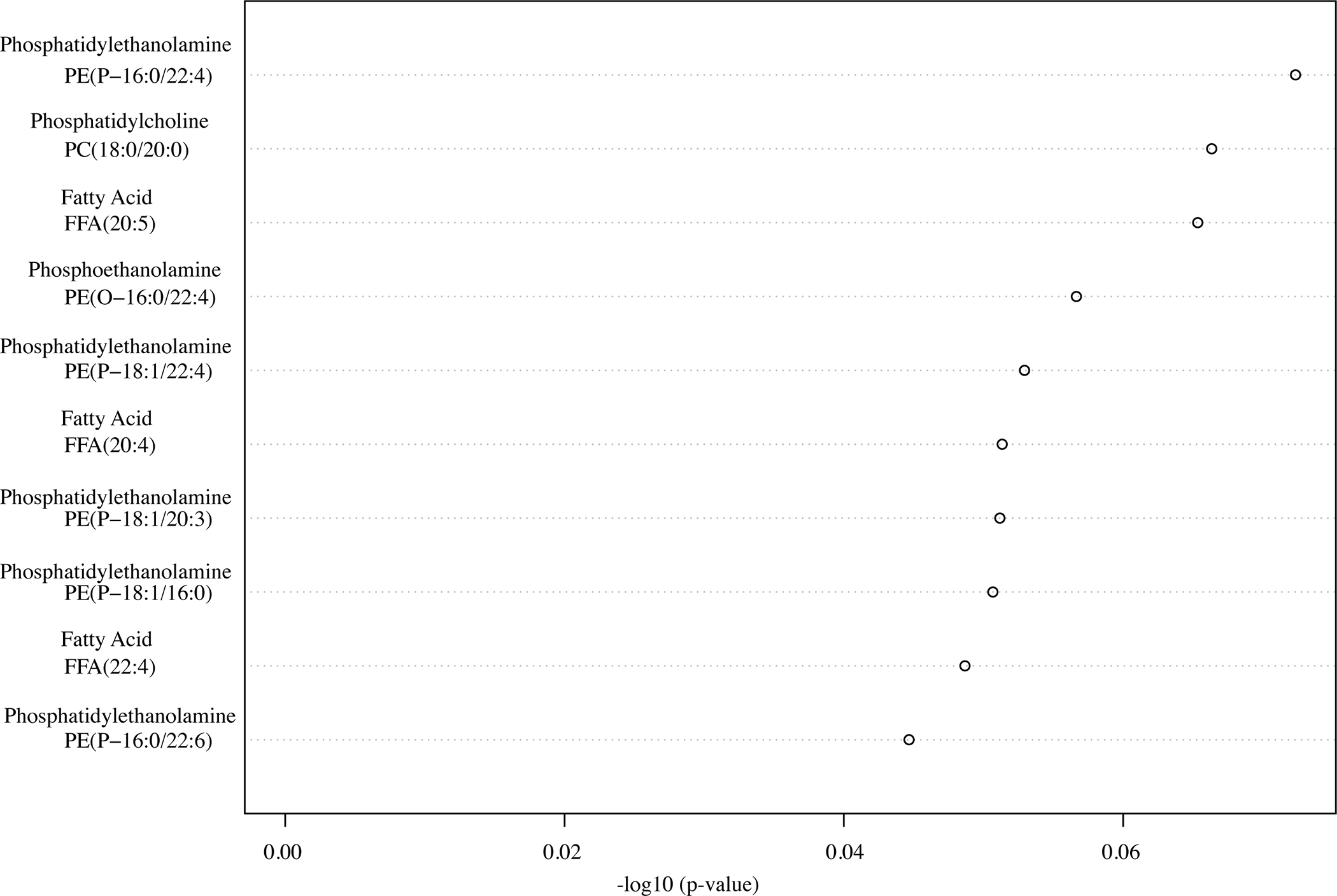
The top 10 lipids of interests from adults with acute ischemic stroke.
DISCUSSION
Our preliminary analysis identified the top 10 lipids of interests from adults with AIS, phosphatidylethanolamine, phospho-ethanolamine, phosphocholine, and fatty acids. The brain is rich is phospholipid content and comprises 75% of lipids in cells. In addition to their role in mediating the host inflammatory response, phospholipids are involved in structural and functional integrity of cellular membranes of both the host, and the human microbiota.30,31 Changes in the structure or function of membrane phospholipids of host or relevant human microbiota may lead to alterations in membrane permeability and contribute to pathology of diverse conditions including AIS, trauma, and neurodegeneration.32 However, with appropriate and timely recognition, the potential exists to reverse metabolic consequences of ‘at risk’ brain tissue.
Lipidomic results demonstrated elevated concentration levels of phosphatidylcholines (PC) and phosphatidylethanolamines (PE), and fatty acids among adults with AIS within the first 24 hours of hospitalization. An explanation for the increased concentration levels in phospholipids could be attributed to repair of compromised phospholipid membranes and an early response to AIS. Phospholipid levels have been reported in the brains, serum, and plasma of patients with AIS and/or in animal models of AIS (transient middle cerebral artery occlusion [tMCAO]). PE and PC have been shown to be significantly higher in individuals with chronic comorbidities who experienced AIS compared to those without AIS.33 Further, serum metabolic profiling has identified higher levels of lipid metabolites, including PE, lyso-PE, PC, lyso-PC, and phosphatidylserine (PS) in AIS patients compared to healthy controls.34 The presence of altered lipid metabolism in AIS has also been confirmed in animal studies. A tMCAO mouse model using mass spectrometry imaging demonstrated a significant increase of phosphatidylinositol 4-phosphate in the penumbra 24 hours post-tMCAO and PC and lyso-PC isoforms in the infarction region compared to uninjured healthy brain tissue.35
Lipids identified in thrombi may relate to etiology subtypes, systemic thrombosis or pathology at the site of origin, or local tissue responses and continued interaction with blood products at the site of occlusion. In hypercholesterolemia patients there is evidence of abnormal platelet function mediated by the binding of lipoproteins. In subjects with diffuse intracranial atherosclerosis, arterial wall cholesterol content is a predictor of development and severity of arterial thrombosis and may contribute to additional thrombogenesis.36 These findings suggest there may be opportunities to exploit a novel metabolic regulatory pathway in platelets that influences thrombus formation by modulating the content of specific lipids/phospholipids, which generate key mediators of platelet activation. Additionally, abnormal plasma lipid levels precipitate membrane composition changes by increasing the cholesterol to phospholipid ratio. The resulting changes in microviscosity may contribute to thrombus structure and elevated ratios identified in thrombi may reinforce or present new opportunities for secondary prevention. Further, the propensity of atherosclerotic plaques to rupture may be influenced by their lipid distribution and content. After plaque disruption and mobilization, additional thrombus formation may occur once exposed to blood from the arterial lumen because plaque debris has been shown to contain potent thrombogenic agents such as tissue factor, collagen, and lipids.37 Differences in thrombus lipid composition, species, and distribution between stable and unstable plaques may reflect differences in lipid pools and the degree of macrophage involvement.38 The role of lipidomic molecules in AIS is complex requiring additional studies to determine how and whether plaque lipids influence the stability of plaques, or if these are causal risk factors related to stroke subtypes, metabolic comorbid conditions, or reflect anticoagulation, antiplatelet, and lipid-lowering therapies.
Distinguishing between stroke subtypes and knowing the time of stroke onset are critical in clinical and nursing practice. Classification of stroke subtype could aid in early treatment and prevention of long-term recurrence in patients. A complementary approach for blood biomarkers in acute stroke diagnosis may be to identify thrombus biomarkers which reflect the body’s response to the damage at the site of origin caused by the different types of stroke. This could assist in clarifying the pathophysiological mechanism of AIS and promoting the secondary prevention and management of patients who experienced AIS.
The pilot nature of this study, including a small sample size (n = 5) and lack of controls are limitations to this study. Utilizing an untargeted lipidomics approach provides several thousands of known and unknown metabolites and lipids, thus limiting much of our focus to the known associations and causing difficulty in identifying unknown but potentially relevant lipids. Additional studies using a targeted lipidomic approach will be necessary to verify lipids associated with AIS, including an assessment of the human host response, environmental controls, and any microbial-derived contributions. Identified lipids in this study may also be influenced by the gut microbiome. We did not control for diet and due to the emergent nature of AIS, subjects may not have fasted before thrombus collection. Lipid-altering medications may also affect lipidomic investigations, but it is not known if the lipid metabolites identified in the thrombi are acute or chronic contributors to pathology and at what stage of AIS they are generated. AIS subjects received propofol infusion for sedation during thrombectomy and this may have affected lipid levels.
Nurses play a key role in the prevention and management of AIS. Recent advances in omics-based science may inform tailored approaches to nursing practice.39 Biomarker signatures offer a vital resource for predicting stroke severity and identifying those who would benefit from early intervention to promote optimal recovery. Analysis of thrombi samples using approaches such as lipidomics may provide knowledge of early pathophysiological changes after AIS onset, the interplay of different pathways of injury, and responsiveness to reperfusion treatment. Future studies will focus on specific lipids and related metabolites compared between plasma and thrombi samples, and associations to symptoms and outcomes. Should pathophysiological mechanisms related to lipid metabolism underlie development of symptoms and outcomes in AIS, relevant treatments to address changes could be tested for efficacy in AIS survivors in a future clinical trial. Interventions (e.g., dietary, physical activity) that reduce or enhance lipid metabolism could be used to improve symptoms and outcomes in AIS survivors. The presence of increased lipid levels and association to clinical outcomes may indicate those with an increased risk for disability and poorer health post-AIS, enabling development of personalized interventions in order to improve symptoms and functional outcomes.
CONCLUSION
High throughput techniques were applied to cerebral thrombi from AIS subjects for the purpose of testing feasibility of lipidomic analysis on this novel biospecimen. Multiple substances were identified including phosphatidylethanolamine, phosphoethanolamine, phosphocholine, and fatty acids. Thrombi from cerebral arteries of AIS patients are an untapped resource that enable direct evaluation of lipid biological markers. Understanding of lipidomic changes in AIS may illuminate specific metabolite and lipid pathways involved and further the potential to develop personalized preventive strategies.
ACKNOWLEDGEMENT
This work was supported by Dr. Hilaire Thompson’s Joanne Montgomery Endowed Professorship. Dr. Sarah Martha was supported by NIH/NINR T32NR016913 and is currently supported by NIH/NINR K23NR019864. The authors would like to acknowledge the University of Washington’s Northwest Metabolomics Research Center for their analytical support.
Footnotes
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. ML has received educational grants from Stryker and Medtronic. ML has equity interest in Synchron, Cerebrotech, Proprio, Hyperion Surgical, and Fluid Biomed. ML is an adviser for Metis Innovative. ML is a consultant for Medtronic and Aeaean Advisers. MW has received research support from Cerenovus and was previously an educational consultant to Medtronic.
DATA AVAILABILITY STATEMENT
The datasets generated for this study are available on request to the corresponding author (SM).
REFERENCES
- 1.Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics—2021 Update. Circulation. 2021;143(8):e254–e743. doi:doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 2.Doyle KP, Simon RP, Stenzel-Poore MP. Mechanisms of ischemic brain damage. Neuropharmacology. Sep 2008;55(3):310–8. doi: 10.1016/j.neuropharm.2008.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tobin MK, Bonds JA, Minshall RD, Pelligrino DA, Testai FD, Lazarov O. Neurogenesis and inflammation after ischemic stroke: what is known and where we go from here. J Cereb Blood Flow Metab. Oct 2014;34(10):1573–84. doi: 10.1038/jcbfm.2014.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. Dec 14 1995;333(24):1581–7. doi: 10.1056/nejm199512143332401 [DOI] [PubMed] [Google Scholar]
- 5.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. Apr 23 2016;387(10029):1723–31. doi: 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 6.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. The New England journal of medicine. Jan 1 2015;372(1):11–20. doi: 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 7.Fraser JF, Collier LA, Gorman AA, et al. The Blood And Clot Thrombectomy Registry And Collaboration (BACTRAC) protocol: novel method for evaluating human stroke. J Neurointerv Surg. Mar 2019;11(3):265–270. doi: 10.1136/neurintsurg-2018-014118 [DOI] [PubMed] [Google Scholar]
- 8.Maekawa K, Shibata M, Nakajima H, et al. Erythrocyte-Rich Thrombus Is Associated with Reduced Number of Maneuvers and Procedure Time in Patients with Acute Ischemic Stroke Undergoing Mechanical Thrombectomy. Cerebrovascular diseases extra. 2018;8(1):39–49. doi: 10.1159/000486042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of Plaque Formation and Rupture. Circulation Research. 2014;114(12):1852–1866. doi:doi: 10.1161/CIRCRESAHA.114.302721 [DOI] [PubMed] [Google Scholar]
- 10.Wang N, Tall AR. Cholesterol in platelet biogenesis and activation. Blood. 2016;127(16):1949–1953. doi: 10.1182/blood-2016-01-631259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gasser JA, Betteridge DJ. Lipids and thrombosis. Baillieres Clin Endocrinol Metab Dec 1990;4(4):923–38. doi: 10.1016/s0950-351x(05)80085-0 [DOI] [PubMed] [Google Scholar]
- 12.Battaglini D, Pimentel-Coelho PM, Robba C, et al. Gut Microbiota in Acute Ischemic Stroke: From Pathophysiology to Therapeutic Implications. Review. Frontiers in Neurology. 2020-June-25 2020;11doi: 10.3389/fneur.2020.00598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pluta R, Januszewski S, Czuczwar SJ. The Role of Gut Microbiota in an Ischemic Stroke. International journal of molecular sciences. 2021;22(2):915. doi: 10.3390/ijms22020915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niesten JM, van der Schaaf IC, van Dam L, et al. Histopathologic composition of cerebral thrombi of acute stroke patients is correlated with stroke subtype and thrombus attenuation. PLoS One. 2014;9(2):e88882. doi: 10.1371/journal.pone.0088882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bacigaluppi M, Semerano A, Gullotta GS, Strambo D. Insights from thrombi retrieved in stroke due to large vessel occlusion. J Cereb Blood Flow Metab. Aug 2019;39(8):1433–1451. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niessen F, Hilger T, Hoehn M, Hossmann KA. Differences in clot preparation determine outcome of recombinant tissue plasminogen activator treatment in experimental thromboembolic stroke. Stroke. Aug 2003;34(8):2019–24. doi: 10.1161/01.str.0000080941.73934.30 [DOI] [PubMed] [Google Scholar]
- 17.Kim JM, Byun JS, Kim J, et al. Analysis of microRNA signatures in ischemic stroke thrombus. Journal of neurointerventional surgery. Jul 8 2021;doi: 10.1136/neurintsurg-2021-017597 [DOI] [PubMed] [Google Scholar]
- 18.Patrakka O, Pienimäki JP, Tuomisto S, et al. Oral Bacterial Signatures in Cerebral Thrombi of Patients With Acute Ischemic Stroke Treated With Thrombectomy. J Am Heart Assoc. Jun 4 2019;8(11):e012330. doi: 10.1161/jaha.119.012330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh A Tools for metabolomics. Nature Methods. 2020/January/01 2020;17(1):24–24. doi: 10.1038/s41592-019-0710-6 [DOI] [PubMed] [Google Scholar]
- 20.Adibhatla RM, Hatcher JF. Altered lipid metabolism in brain injury and disorders. Subcell Biochem. 2008;49:241–68. doi: 10.1007/978-1-4020-8831-5_9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. Dec 2019;50(12):e344–e418. doi: 10.1161/str.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 22.Kanehisa M Toward understanding the origin and evolution of cellular organisms. Protein Sci. 2019;28(11):1947–1951. doi: 10.1002/pro.3715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institute of Standards and Technology (NIST) Standard Reference Database. https://www.nist.gov/srd/nist-standard-reference-database-1a-v17
- 24.Chong J, Wishart DS, Xia J. Using MetaboAnalyst 4.0 for Comprehensive and Integrative Metabolomics Data Analysis. Current Protocols in Bioinformatics. 2019;68(1):e86. doi: 10.1002/cpbi.86 [DOI] [PubMed] [Google Scholar]
- 25.Xia J, Psychogios N, Young N, Wishart DS. MetaboAnalyst: a web server for metabolomic data analysis and interpretation. Nucleic Acids Research. 2009;37(suppl_2):W652–W660. doi: 10.1093/nar/gkp356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen X, Ishwaran H. Random forests for genomic data analysis. Genomics. Jun 2012;99(6):323–9. doi: 10.1016/j.ygeno.2012.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu T, Sun Y, Jia W, Li D, Zou M, Zhang M. Study on the Estimation of Forest Volume Based on Multi-Source Data. Sensors. 2021;21(23):7796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kearns M, Ron D. Algorithmic Stability and Sanity-Check Bounds for Leave-One-Out Cross-Validation. Neural Computation. 1999;11(6):1427–1453. doi: 10.1162/089976699300016304 [DOI] [PubMed] [Google Scholar]
- 29.Ko AHR, Cavalin PR, Sabourin R, Britto AdS. Leave-One-Out-Training and Leave-One-Out-Testing Hidden Markov Models for a Handwritten Numeral Recognizer: The Implications of a Single Classifier and Multiple Classifications. IEEE Transactions on Pattern Analysis and Machine Intelligence. 2009;31(12):2168–2178. doi: 10.1109/TPAMI.2008.254 [DOI] [PubMed] [Google Scholar]
- 30.Adibhatla RM, Hatcher JF. Role of Lipids in Brain Injury and Diseases. Future Lipidol Aug 2007;2(4):403–422. doi: 10.2217/17460875.2.4.403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cho G, Lee E, Kim J. Structural insights into phosphatidylethanolamine formation in bacterial membrane biogenesis. Scientific reports. 2021;11(1):5785–5785. doi: 10.1038/s41598-021-85195-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muralikrishna Adibhatla R, Hatcher JF. Phospholipase A2, reactive oxygen species, and lipid peroxidation in cerebral ischemia. Free Radic Biol Med. Feb 1 2006;40(3):376–87. doi: 10.1016/j.freeradbiomed.2005.08.044 [DOI] [PubMed] [Google Scholar]
- 33.Afshinnia F, Jadoon A, Rajendiran TM, et al. Plasma lipidomic profiling identifies a novel complex lipid signature associated with ischemic stroke in chronic kidney disease. J Transl Sci. 2020;6(6):419. [PMC free article] [PubMed] [Google Scholar]
- 34.Sun H, Zhao J, Zhong D, Li G. Potential serum biomarkers and metabonomic profiling of serum in ischemic stroke patients using UPLC/Q-TOF MS/MS. PloS one. 2017;12(12):e0189009. doi: 10.1371/journal.pone.0189009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mulder IA, Ogrinc Potočnik N, Broos LAM, et al. Distinguishing core from penumbra by lipid profiles using Mass Spectrometry Imaging in a transgenic mouse model of ischemic stroke. Scientific Reports. 2019/January/31 2019;9(1):1090. doi: 10.1038/s41598-018-37612-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lepropre S, Kautbally S, Octave M, et al. AMPK-ACC signaling modulates platelet phospholipids and potentiates thrombus formation. Blood. 2018/September// 2018;132(11):1180–1192. doi: 10.1182/blood-2018-02-831503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilcox JN. Analysis of local gene expression in human atherosclerotic plaques by in situ hybridization. Trends in Cardiovascular Medicine. 1991/January/01/ 1991;1(1):17–24. doi: 10.1016/1050-1738(91)90054-I [DOI] [PubMed] [Google Scholar]
- 38.Rezkalla SH, Holmes DR Jr. Lipid-rich plaque masquerading as a coronary thrombus. Clin Med Res. 2006;4(2):119–122. doi: 10.3121/cmr.4.2.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martha SR, Auld JP, Hash JB, Hong H. Precision Health in Aging and Nursing Practice. J Gerontol Nurs Mar 1 2020;46(3):3–6. doi: 10.3928/00989134-20200129-03 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author (SM).


