An analysis of Centers for Disease Control and Prevention (CDC) mortality data found that firearm-related deaths surpassed motor vehicle collisions as the leading cause of mortality for US children and adolescents aged 1 to 19 years (hereafter “youths”) for the first time in 2020.1 The 2019 to 2020 increase in the crude rate of firearm-related crude rate of firearm-related deaths for youths was more than twice as high as the increase for the general population and was observed across demographic groups.1 We assessed racial and ethnic differences in the overall burden of firearm-related mortality and in the change in firearm-related mortality among youths from 1999 to 2020.
Methods |
Mortality data, race and ethnicity, and population counts for US youths from 1999 to 2020 were taken from the CDC WONDER database.2 Firearm-related mortality was defined broadly to include deaths caused by firearm homicide, firearm suicide, unintentional firearm death, and undetermined intent firearm death (eTable in the Supplement). Four non-Hispanic racial categories were considered—American Indian or Alaska Native, Asian or Pacific Islander, Black or African American, and White—along with the Hispanic ethnicity category (any race) (see eAppendix in the Supplement for details on race and ethnicity). Firearm-related death rates were compared for all groups in 2020 and for Black and White groups from 1999 to 2020. Crude death rates were calculated as the number of deaths per 100 000 population with 95% confidence intervals (eAppendix in the Supplement). Statistical differences in the rate and proportion of firearm-related deaths among groups were computed using the 2-sample t test and 2-proportion z test, respectively. Analysis was done with Microsoft Excel version 1808. A 2-sided P < .05 defined statistical significance. This study used publicly available, deidentified, aggregate participant data and did not require participant informed consent or institutional review board approval per National Institutes of Health guidelines.
Results |
There were 4357 reported firearm-related deaths for US youths in 2020, a crude rate of 5.62 (95% CI, 5.45–5.79) deaths per 100 000 population. The crude rate per 100 000 population of firearm-related mortality for Black youths in 2020 (17.40 [95% CI, 16.65–18.15]) was statistically significantly higher than for any other group (American Indian or Alaska Native, 9.05 [95% CI, 7.03–11.48]; Asian or Pacific Islander, 1.32 [95% CI, 1.01–1.68]; Hispanic, 4.01 [95% CI, 3.73–4.29]; and White, 3.40 [95% CI, 3.22–3.58]) (all comparisons with Black youths, P < .001) (Figure 1). Black youths accounted for 47.1% (n = 2053) of firearm-related deaths in 2020, a mean of 5 to 6 deaths per day, despite making up 15.2% of the population of 1-to 19-year-olds. White youths accounted for a smaller proportion of firearm-related deaths in 2020 (31.6%) relative to their proportion of the population (52.2%) (P < .001 comparing proportions of Black vs White youths).
Figure 1.
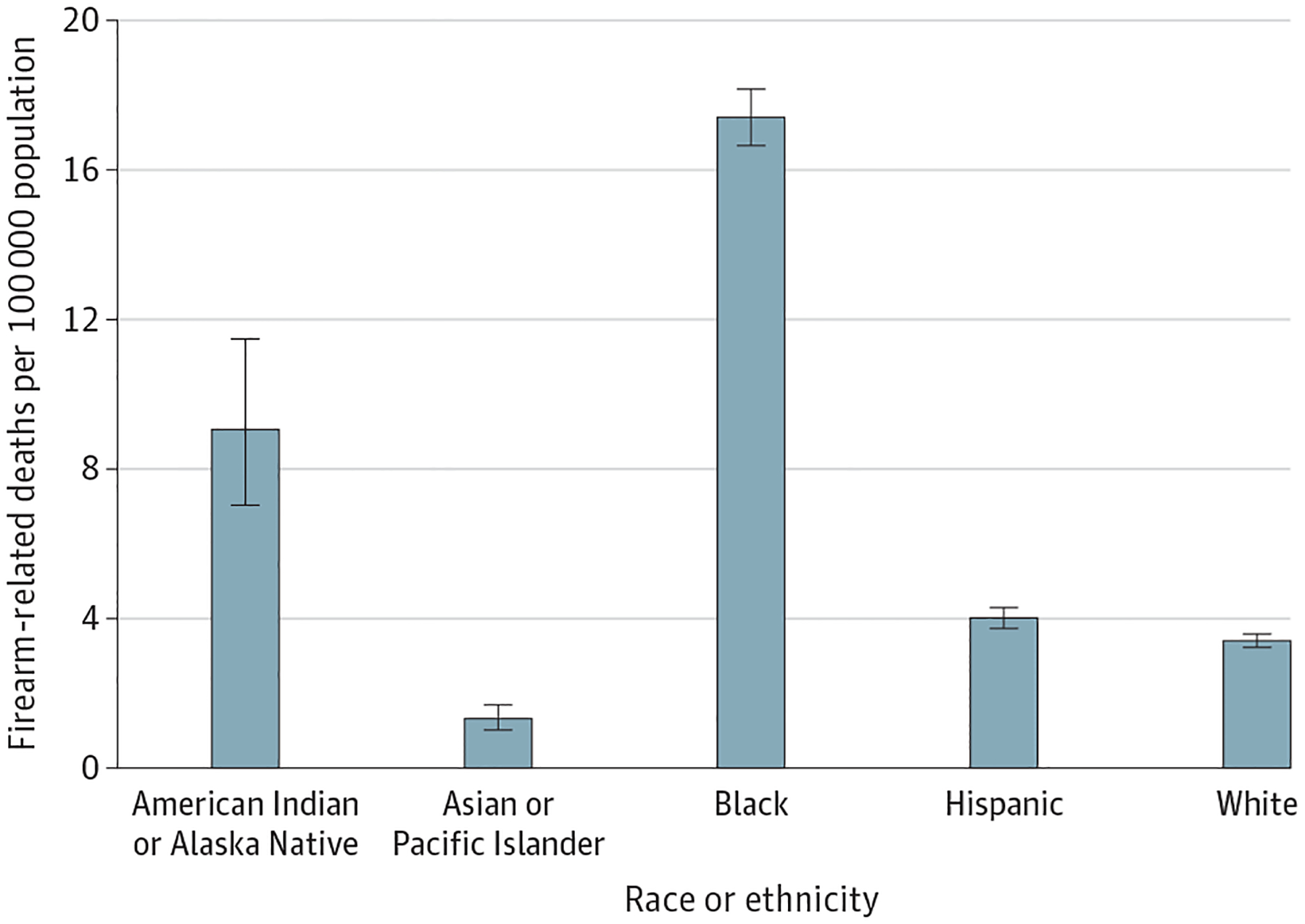
Firearm-Related Deaths Among US Youths in 2020
Crude firearm-related death rate per 100 000 population (whiskers indicate 95% CIs) for US racial and ethnic groups. Numbers of deaths: American Indian and Alaskan Native, 68; Asian or Pacific Islander, 64; Black, 2053; Hispanic, 789; White, 1376.
The rate of firearm-related deaths per 100 000 among US youths fluctuated over time (Figure 2), from 4.42 (95% CI, 4.28–4.58) in 1999, decreasing to 4.34 (95% CI, 4.19–4.49) in 2019 and increasing to 5.62 (95% CI, 5.45–5.79) in 2020 (29.5% increase between 2019 and 2020). The 2019 to 2020 increase in firearm-related deaths per 100 000 for Black youths was 39.2% (2019: 12.50 [95% CI, 11.87–13.14]; 2020: 17.40 [95% CI, 16.65–18.15]) vs 16.4% for White youths (2019: 2.92 [95% CI, 2.75–3.08]; 2020: 3.40 [95% CI, 3.22–3.58]). The rate of firearm-related deaths per 100 000 for Black youths increased every year since 2013 (8.35 [95% CI, 7.83–8.87]), with a 108.3% increase from 2013 to 2020 for Black youths compared with a 47.8% increase for White youths over the same time (2013: 2.30 [95% CI, 2.15–2.44]).
Figure 2.
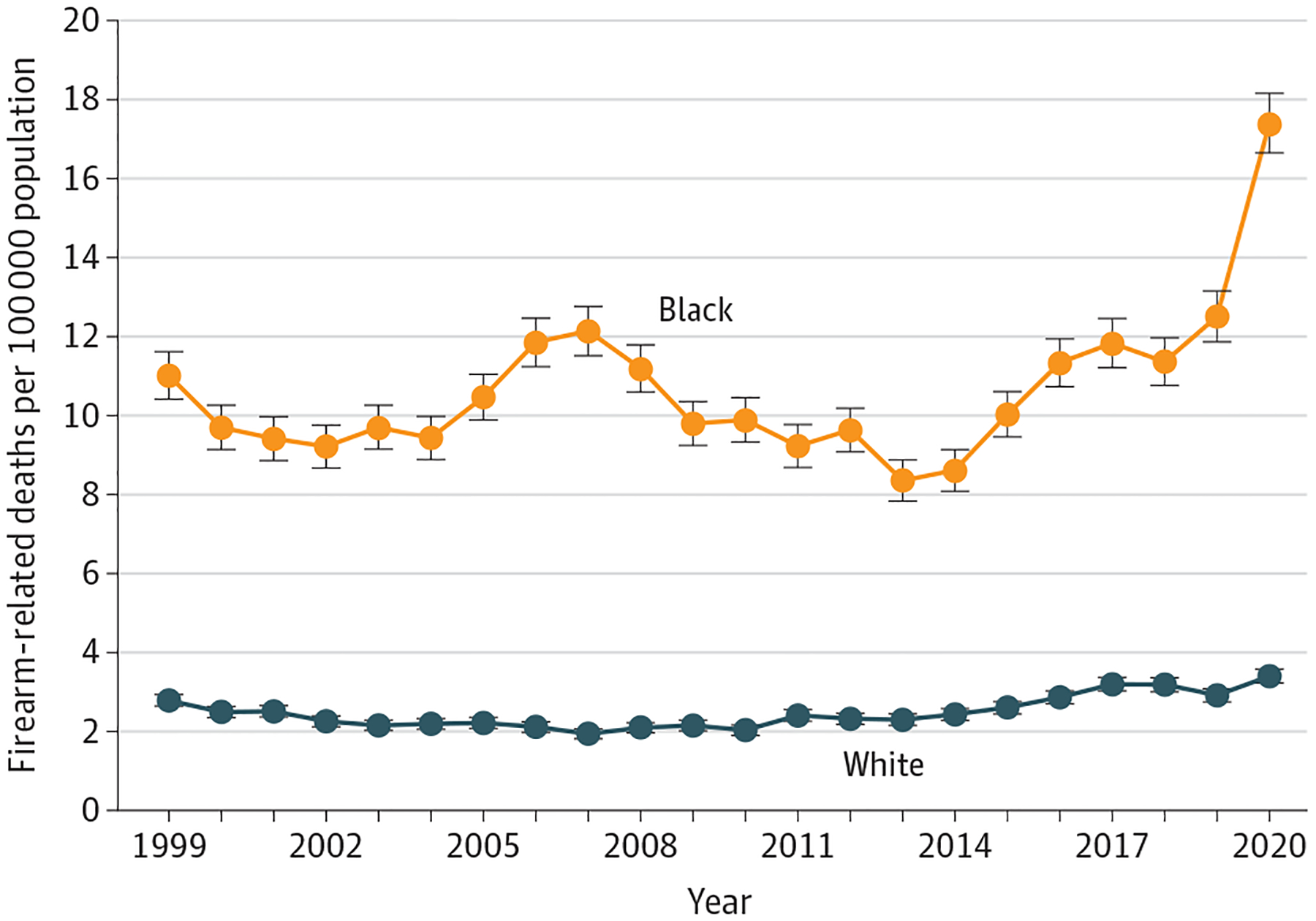
Firearm-Related Deaths Among US Youths From 1999 to 2020
Crude firearm-related death rate per 100 000 population (whiskers indicate 95% CIs) for Black and White youths.
Discussion |
This study found racial and ethnic differences in firearm-related deaths of US youths, with the highest overall burden and recent increase among Black youths. The large increase in firearm-related mortality between 2019 and 2020 may be related to the COVID-19 pandemic and social unrest; further follow-up is needed to see if this trend continues. This study is limited by its reliance on mortality data from the CDC, which may lack precise cause-of-death specification by physicians and involve biases based on coding protocols3; mortality rates may be underreported for the American Indian or Alaska Native group.4 Strategic and effective public health interventions to curtail gun violence and prevent firearm-related deaths among US youths are warranted, especially among Black youths.5
Supplementary Material
Funding/Support:
This work was supported by the National Institutes of Health (NIH) Distinguished Scholars Program (Dr Mariño-Ramírez) and the Division of Intramural Research of the National Institute on Minority Health and Health Disparities at the NIH.
Role of the Funder/Sponsor:
The study supporters had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
References
- 1.Goldstick JE, Cunningham RM, Carter PM. Current causes of death in children and adolescents in the United States. N Engl J Med. 2022;386(20):1955–1956. doi: 10.1056/NEJMc2201761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC WONDER database. Accessed June 7, 2022. https://wonder.cdc.gov/
- 3.Zemach R. What the vital statistics system can and cannot do. Am J Public Health. 1984;74(8):756–758. doi: 10.2105/AJPH.74.8.756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espey DK, Jim MA, Richards TB, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butts JA, Roman CG, Bostwick L, Porter JR. Cure violence: a public health model to reduce gun violence. Annu Rev Public Health. 2015;36:39–53. doi: 10.1146/annurev-publhealth-031914-122509 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


