Despite strong scholarly and public health interest in social disparities in pain, information about pain prevalence among sexual minority1 groups is largely absent. This is a critical gap. Sexual-minority adults comprise over 7%, or over 18 million, American adults [38].
More importantly, despite meaningful social and political advances [15; 28] and greater public acceptance [45], sexual-minority adults continue to experience stigma via negative stereotypes, prejudice, discrimination, and violence [1; 53; 70]. Indeed, there is evidence that the stigma and social exclusion not only persist but may be increasing, perhaps partly as a backlash to sociolegal victories and partly due to the increasing political hyperpolarization of the U.S. in recent decades [21; 48; 56]. Correspondingly, sexual-minority adults continue to struggle with worse physical and mental health than straight adults [33; 45; 46; 60; 67] and, worryingly, these disparities appear to be largest in younger cohorts [8; 46; 51]. Although all these factors (stigma, poor physical health, and poor mental health) are known as important correlates of chronic pain [3; 17; 74], there are no population-based national analyses of chronic pain among U.S. sexual-minority adults.
Some studies examined the association between sexual identity and pain among adolescents and young adults [40; 55; 65], older adults [23], or California residents [10]. They found that sexual-minority adults have higher or sometimes comparable prevalence of pain or painful conditions. We are aware of a single study that examined a representative sample of U.S. adults; it focused solely on headache, which was found to be higher among sexual-minority adults [31].
Not only are these studies few in number, but they often merge unique sexual-identity categories into a single group, potentially obscuring important within-group differences [67]. In particular, little is known about pain in bisexual adults [16], the most common sexual-minority identity [56] and the one with the worst health outcomes [24; 38; 46; 67]. Small sample sizes are also common: Studies often include only a few dozen respondents per sexual-minority category, limiting statistical power and reliability of results. Finally, little attention has been paid to the identification of key covariates that could account for observed differences across groups.
Our study overcomes these limitations to provide the first comprehensive overview of chronic pain across sexual-identity categories. We determine the prevalence of two chronic pain outcomes among adults age 18–64 who identify as straight, gay/lesbian, bisexual or “something else,” using the largest nationally-representative up-to-date health survey. We examine the pain disparities net of key covariates known to impact pain levels in the population, including demographic, socioeconomic, health-behavioral, and psychological factors [26; 85]. We present findings in absolute and relative terms, to offer a full picture of the disparities. In the discussion, we articulate steps necessary to better understand the sources of pain disadvantage among sexual-minority adults.
METHODS
Data
Data are from the National Health Interview Survey (NHIS) harmonized by Integrated Public Use Microdata Series, or IPUMS [4], available at https://nhis.ipums.org/nhis/. The NHIS is a large, nationally representative, cross-sectional health survey, conducted by U.S. Census Bureau on behalf of the National Center for Health Statistics (NCHS) [57]. The NHIS is considered a “gold standard” [18] survey for its quality and sample size; it is the primary source of information on the U.S. non-institutionalized civilian population. The survey uses a complex multistage area probability household sample design and oversamples respondents from understudied population groups including Black and Hispanic adults. Census interviewers conduct face-to-face interviews continuously throughout the year and collect data on a wide range of health topics.
We pooled data collected in the 2013–18 waves to maximize sample sizes. 2013 was the first year when NHIS asked about the respondents’ sexual identity; 2018 was the last year before a major redesign that precludes merging later survey years [34].
We defined the analytic sample as adults aged 18–64 who answered the questionnaire themselves (as opposed to having a proxy provide answers, rare in this age range) and who were asked about their sexual identity (about 1% were not asked, typically because the interview was cut short before this question was posed). This definition included 135,962 respondents. Of those, 1,571 (1.1%) did not report their sexual identity and were omitted from the analysis. Questions about site-specific chronic pain were asked of all respondents. Only 125 (<0.1%) responses were missing, yielding an analytic sample size of 134,266. Questions about general chronic pain were asked of a random subsample of respondents, an approach that the NHIS utilizes to reduce respondent burden. Between 2013 and 2018, the question was posed to 95,795 of those in our sample definition, among whom 120 (0.1%) did not provide valid answers, yielding an analytic sample with 95,675 respondents for the general chronic pain analyses.
Variables
Sexual identity.
This key predictor was assessed with the question “Which of the following best represents how you think of yourself?” Respondents were presented with six options: “lesbian or gay,” “straight, that is, not lesbian or gay,” “bisexual,” “something else,” “I don’t know the answer,” and “refused.” We retained the first four and excluded the two latter categories from our analyses based on the following considerations. The NCHS conducted extensive tests of the wording and options for this survey item during its development phase [52] and the first two years of its use [12; 18]; these tests included an analysis of in-depth follow-up questions. For instance, respondents who selected “something else” were asked “by something else, do you mean that…” These probes showed that over 90% of respondents who selected “something else” were in fact members of sexual minority groups, for instance, queer, pansexual, transgender, or “in the process of figuring out their sexuality,” in contrast to only about 20% of those who selected “I don’t know the answer” [18]. Based on these findings, we consider our operationalization to be the optimal approach for delineating sexual minority and straight-identified respondents.
Pain.
We constructed two indicators of pain: chronic pain in 3+ sites and general chronic pain. We analyze both measures of pain based on evidence that disparities may differ across pain definitions [81]; descriptives are shown in Table 1.
Chronic pain in 3+ sites was created from questions about pain in five anatomical sites. The NHIS asked about these five sites because they are the most common and/or disabling types of pain [27; 64]. Respondents were asked: “During the past three months, did you have [low back pain, neck pain, severe headache or migraine, or facial or jaw ache or pain]?” In addition, to measure joint pain, respondents were first asked whether they had “any symptoms of pain, aching, or stiffness in or around a joint during the past 30 days” and those who said yes were then asked whether the onset was at least 3 months prior. For consistent time horizon across all five measures, we used a positive response to this follow-up joint-pain question as an indicator of chronic joint pain. Thus, any respondent could report experiencing chronic pain in 0 to 5 sites (51% had pain in none of the queried sites; 24% had pain in one site; 13% had pain in two sites; 7% had pain in 3 sites; 3% had pain in four sites, and 1% reported pain in all five sites). We dichotomized the number as 0–2 versus 3–5 sites following precedent [81].
General chronic pain was assessed with a single question “In the past […] months, how often did you have pain? Would you say never, some days, most days, or every day?” In 2013, 2014, 2015, and 2018, the question was asked with respect to the “past three months.” In 2016 and 2017, the question was with respect to “past six months.” We combined the information from all six waves following prior findings that population pain prevalence does not differ between these two time horizons [81]. Following established precedent [61], we dichotomized this measure as never or some days versus most or every day.
Table 1.
Pain prevalence levels and differences by sexual identity
| Pain prevalence levels | Pain prevalence differences | Respondent N and % | ||||
|---|---|---|---|---|---|---|
| Prevalence | 95% CI | Percentage-point difference1 | Relative difference1 | Number of respondents2 | Weighted percentage2 | |
| PANEL A. Pain in 3+ sites | ||||||
| Straight | 11.5 | (11.3, 11.7) | -- | -- | 129,426 | 96.65 |
| Gay/lesbian | 16.1 | (14.3, 18.1) | 4.6 | 1.40*** (1.26, 1.56) | 2,743 | 1.86 |
| Bisexual | 20.1 | (17.6, 22.8) | 8.6 | 1.75*** (1.53, 1.99) | 1,595 | 1.14 |
| “Something else” | 22.9 | (18.2, 28.3) | 11.4 | 1.99*** (1.60, 2.46) | 502 | 0.35 |
| PANEL B. Chronic pain | ||||||
| Straight | 17.2 | (16.9, 17.5) | -- | -- | 92,062 | 96.60 |
| Gay/lesbian | 21.7 | (19.3, 24.4) | 4.5 | 1.26*** (1.12, 1.41) | 2,006 | 1.92 |
| Bisexual | 23.7 | (20.8, 26.9) | 6.5 | 1.38*** (1.21, 1.56) | 1,210 | 1.14 |
| “Something else” | 27.0 | (21.8, 32.9) | 9.8 | 1.57*** (1.28, 1.91) | 397 | 0.35 |
p<.001. N = number of respondents, or sample size
NHIS 2013–2018, US adults age 18–64. N=134,266 for pain in 3+ sites and N=95,675 for chronic pain. Overall weighted prevalence was 11.7% (11.5,11.9) for pain in 3+ sites and 17.4% (17.1,17.7) for chronic pain.
“Something else” was the actual verbatim terminology used on the NHIS survey; it captures other non-heterosexual identified adults. More information about the design of the sexual identity question is available elsewhere [52].
Relative to straight respondents. Percentage point difference is just the arithmetic difference in prevalence levels; the relative difference is a prevalence ratio obtained from complex-survey-adjusted (modified/robust) bivariate Poisson model of each outcome as a function of sexual identity.
The number of respondents is the raw count of respondents in the sample with valid information, that is, number used in analyses; the weighted percentage corresponds to the distribution of the groups in the population (target population of the NHIS, which is non-institutionalized US adults).
Missingness on the individual questions that were used to construct the two pain outcomes was low. For the six site-specific pain items (five sites, but the joint pain comprised two questions), missingness ranged from 36 respondents (0.01%) failing to answer whether their joint pain started more than 3 months ago up to 48 respondents (0.04%) not answering the item about low back pain. Altogether, 134,266 respondents (99.91%) answered all six questions and thus were included in the analysis. The chronic pain question was answered by 95,795 (99.75%) respondents.
Correlations among the five sites range from 0.18 between migraine and joint pain to 0.42 between low back and neck pain (tetrachoric correlations, more appropriate for dichotomous indicators, range from 0.32 to 0.68). This indicates that respondents who report pain at one site are more likely to report pain at other sites, as expected [27], but each of the sites also brings independent information to the analyses. The correlation between the two pain outcomes –chronic pain in 3+ sites and general chronic pain-- was 0.43 (tetrachoric correlation was 0.70). This correlation is high enough to serve as evidence of concurrent validity for each measure; at the same time, it is low enough to justify analyzing each measure separately, as each captures a unique dimension of the respondents’ pain experience.
Covariates.
Table 2 shows the categories for all covariates and their distribution at a glance.
Basic demographics: All regression and decomposition models (see Tables 3 and 4) include basic demographics: age, age squared, sex, year. Age is centered about 45 and specified in decades for regression models. It is scaled to a 0–1 range in decomposition analyses. Age squared captures potential nonlinearities [26; 82] in the age-pain association. NHIS assessed sex dichotomously: Respondents could self-identify as “male” or “female,” with no additional options given or allowed. NHIS asked no questions about gender such as identifying as trans- versus cis-gender. Year of interview is included as continuous to control for secular changes in pain [82; 86], as well as in the social and legal landscape for members of sexual minority groups [13; 73], between 2013 to 2018.
Additional demographic covariates are race/ethnicity, region of residence, immigrant status, language of interview, marital status, and having children at home. Race/ethnicity combines racial and Hispanic-ethnicity self-identifications. Respondents who identified as Hispanic were categorized as such. Respondents who identified as not Hispanic were categorized by NCHS as White (reference), Black, American Indian/Alaskan Native (AIAN), Asian, “multiple race,” and “other.” Region of residence was classified as Northeast (reference), North Central/Midwest, South, and West. Immigrant status was coded as U.S.-born (reference), foreign born and at least 15 years in the U.S., and foreign born and 0–14 years in the U.S. Language of interview was dichotomized as English (reference) or other. Marital status was coded as married (reference), previously married, and never married. Finally, respondents reported whether they had children under 18 at home; we categorized the answer as none (reference), one child, and two or more children.
Socioeconomic characteristics include educational attainment, household income, home ownership as a measure of long-term economic stability [71], and employment status. Education is categorized as less then high school or a General Educational Development (GED) diploma, high school diploma, some college but no postsecondary degree, associate degree, bachelor’s degree (reference), and master’s or higher degree. GED earners were included with the lowest education category based on prior research [80]. Household income was categorized by NCHS as $0–34,999, $35,000–74,999, $75,000–99,999, and $100,000 or more (reference). Home ownership is coded as owning a home (reference), renting, or other arrangement. Finally, employment status is a dichotomous measure of being employed (reference) or not employed.
Health behaviors comprise smoking, BMI as a proxy for diet-related behaviors, alcohol use, physical activity, and sleep duration. Smoking was categorized as never (reference), former, and current. BMI was calculated by the NCHS from self-reported height and weight. We categorized it as <18.5, 18.5–24.9 (reference), 25–29.9, 30–34.9, 35–39.9, and 40 or higher. Alcohol use was classified as never (reference), former, current moderate (reference), and excessive use, which combines binge and heavy drinking [19]. Physical activity was constructed from responses to a set of questions about the frequency and duration of moderate and vigorous exercise and coded as a dichotomous covariate that captured whether a respondent met federal physical-activity guidelines (reference) or not. The threshold to meet the guidelines is 150 minutes per week of moderate activity or 75 minutes of vigorous exercise [72]. Sleep duration was classified as normal (reference, 7–8 hours), short (<7 hours), or long (>8 hours).
Health care experiences are captured with two variables: satisfaction with care, and where the respondent gets medical care when sick. Satisfaction with health care was coded as very satisfied (reference), somewhat satisfied, very or somewhat dissatisfied, and having had no care in the prior 12 months. The place of care included doctor’s office (reference), clinic or health center, hospital, and other or no usual place.
Psychological distress was assessed with the widely-used K6 scale, well-validated in population studies [41]. The measure is based on six items about the frequency of having felt sad, nervous, restless, hopeless, worthless, or like everything was an effort over the past month. We categorized the distress scale that ranged from 0 to 24 points using cutpoints suggested in prior studies [42; 63]: 0–4 for low (reference), 5–12 for moderate, and 13–24 for severe distress.
Table 2.
Characteristics of the target population, by sexual identity.
| Sexual identity | ||||
|---|---|---|---|---|
| Straight | Gay/Lesbian | Bisexual | “Something else” | |
| Age – mean (standard deviation) | 40.9 (13.5) | 39.6 (13.2) | 31.9 (12.2) | 34.7 (14.2) |
| Female | 50.8 | 45.8 | 71.7 | 56.8 |
| Race/ethic identity | ||||
| White | 61.7 | 63.1 | 66.3 | 56.0 |
| Black | 12.1 | 12.8 | 10.7 | 15.5 |
| Hispanic | 17.6 | 16.9 | 15.4 | 16.7 |
| Asian | 6.1 | 3.1 | 3.6 | 3.8 |
| American Indian/Alaska Native | 0.7 | 0.9 | 0.8 | 1.3 |
| Multiracial | 1.6 | 3.1 | 3.1 | 6.1 |
| DK | 0.2 | 0.1 | 0.1 | 0.6 |
| Region of residence | ||||
| Northeast | 17.2 | 18.0 | 15.9 | 19.2 |
| North Central/Midwest | 22.5 | 18.7 | 23.7 | 20.3 |
| South | 36.6 | 36.3 | 32.4 | 30.3 |
| West | 23.7 | 27.0 | 28.0 | 30.2 |
| Immigrant status | ||||
| US-born | 80.1 | 89.0 | 89.0 | 85.7 |
| In US 15+ years | 12.3 | 7.1 | 5.5 | 8.5 |
| In US 0–14 years | 7.3 | 3.8 | 5.5 | 5.1 |
| DK | 0.3 | 0.0 | 0.0 | 0.6 |
| Language of interview | ||||
| English | 93.2 | 97.2 | 96.7 | 95.7 |
| Other | 6.8 | 2.8 | 3.3 | 4.3 |
| Marital Status | ||||
| Married | 53.7 | 23.1 | 21.0 | 18.2 |
| Previously married | 15.1 | 9.8 | 15.1 | 14.2 |
| Never married | 31.0 | 66.8 | 63.4 | 67.5 |
| DK | 0.2 | 0.3 | 0.5 | 0.1 |
| Children at home | ||||
| No children | 54.5 | 86.5 | 73.6 | 82.3 |
| One child | 18.5 | 7.3 | 14.3 | 7.2 |
| Two or more | 27.1 | 6.2 | 12.1 | 10.6 |
| Educational attainment | ||||
| Less than high school | 14.2 | 8.8 | 15.4 | 15.5 |
| High school | 21.1 | 15.7 | 19.5 | 18.2 |
| Some college | 20.1 | 21.3 | 27.5 | 27.3 |
| Associate degree | 11.8 | 11.4 | 9.4 | 12.4 |
| Bachelor’s degree | 21.2 | 25.5 | 18.6 | 19.8 |
| Master’s degree or higher | 11.3 | 17.0 | 9.5 | 6.9 |
| DK | 0.3 | 0.2 | 0.0 | 0.0 |
| Household income | ||||
| $0–34,999 | 24.8 | 29.7 | 42.4 | 42.0 |
| $35,000–74,999 | 27.3 | 26.6 | 25.4 | 29.3 |
| $75,000–99,999 | 12.3 | 11.6 | 8.8 | 8.1 |
| $100,000+ | 28.1 | 27.4 | 18.5 | 11.9 |
| DK | 7.5 | 4.6 | 4.8 | 8.7 |
| Home ownership | ||||
| Owns | 62.5 | 52.4 | 38.8 | 41.2 |
| Rents | 35.2 | 45.2 | 56.3 | 53.8 |
| Other | 2.3 | 2.4 | 4.9 | 5.0 |
| Employment status | ||||
| Employed | 73.2 | 75.1 | 67.0 | 64.1 |
| Not employed | 26.7 | 24.9 | 33.0 | 35.9 |
| DK | 0.0 | 0.0 | 0.0 | 0.0 |
| Smoking status | ||||
| Never | 65.0 | 55.9 | 59.0 | 60.6 |
| Former | 18.0 | 21.2 | 18.1 | 15.0 |
| Current | 16.9 | 22.7 | 22.9 | 24.4 |
| DK | 0.1 | 0.3 | 0.0 | 0.0 |
| BMI | ||||
| <18.5 | 1.7 | 2.4 | 2.4 | 2.2 |
| 18.5–24.9 | 33.0 | 35.7 | 34.8 | 41.5 |
| 25–29.9 | 33.0 | 29.6 | 25.1 | 27.0 |
| 30–34.9 | 17.5 | 16.6 | 17.0 | 14.8 |
| 35–39.9 | 7.3 | 7.9 | 9.3 | 5.2 |
| >=40 | 4.9 | 6.5 | 9.8 | 7.3 |
| DK | 2.6 | 1.1 | 1.8 | 2.0 |
| Alcohol use | ||||
| Never | 18.9 | 10.6 | 16.7 | 18.7 |
| Former | 11.2 | 9.7 | 6.1 | 12.4 |
| Moderate | 39.9 | 40.6 | 31.9 | 33.9 |
| Excessive | 29.2 | 38.4 | 45.2 | 34.6 |
| DK | 0.7 | 0.7 | 0.2 | 0.4 |
| Physical activity | ||||
| Adequate activity | 51.4 | 54.1 | 53.9 | 52.6 |
| Low, inadequate activity | 45.4 | 42.7 | 43.6 | 44.0 |
| DK | 3.2 | 3.1 | 2.5 | 3.3 |
| Sleep duration | ||||
| Normal (7–8 hrs) | 59.9 | 58.9 | 51.0 | 46.2 |
| Short (<7 hrs) | 33.4 | 33.7 | 38.8 | 42.4 |
| Long (>8 hrs) | 6.2 | 6.7 | 9.9 | 10.9 |
| DK | 0.5 | 0.7 | 0.2 | 0.5 |
| Satisfaction with health care, past 12 months | ||||
| Very satisfied | 56.8 | 58.6 | 50.7 | 42.8 |
| Somewhat satisfied | 24.6 | 25.1 | 28.9 | 27.4 |
| Very/somewhat dissatisfied | 5.3 | 5.5 | 8.0 | 8.4 |
| Had no care in prior 12 months | 13.2 | 10.8 | 12.1 | 21.1 |
| DK | 0.2 | 0.1 | 0.3 | 0.3 |
| Where usually gets care when sick | ||||
| Doctor’s office | 59.2 | 61.1 | 46.9 | 43.2 |
| Clinic/health center | 20.6 | 18.3 | 24.7 | 26.3 |
| Hospital | 2.2 | 3.0 | 4.1 | 2.7 |
| Other/has no usual place | 17.9 | 17.5 | 24.2 | 27.8 |
| DK | 0.0 | 0.0 | 0.1 | 0.0 |
| Psychological distress | ||||
| Low | 78.3 | 68.7 | 51.1 | 42.3 |
| Moderate | 17.6 | 24.6 | 36.5 | 42.8 |
| Severe | 3.5 | 6.2 | 12.2 | 14.1 |
| DK | 0.6 | 0.5 | 0.2 | 0.8 |
DK=don’t know, refused, or was not ascertained.
NHIS 2013–2018, US adults age 18–64. N=134,347 includes all adults who have at least one non-missing pain outcome.
The numbers are percent of total within each group for all variables except for age where means and standard deviations are shown.
“Something else” was the actual verbatim terminology used on the NHIS survey; it captures other non-heterosexual identified adults. More information about the design of the sexual identity question is available elsewhere [52].
All variables differ significantly across the four groups (p<.001) except low physical activity, which is statistically comparable across the groups.
Table 3.
Pain prevalence ratios for sexual minority adults, different covariate sets
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| PANEL A. Pain in 3+ sites | ||||
| Sexual identity (straight) | ||||
| Gay/lesbian | 1.47*** | (1.32,1.64) | 1.23*** | (1.11,1.36) |
| Bisexual | 2.05*** | (1.80,2.34) | 1.23*** | (1.09,1.39) |
| “Something else” | 2.33*** | (1.88,2.88) | 1.42*** | (1.17,1.73) |
| PANEL B. Chronic pain. | ||||
| Sexual identity (straight) | ||||
| Gay/lesbian | 1.33*** | (1.19,1.49) | 1.17** | (1.06,1.30) |
| Bisexual | 1.88*** | (1.66,2.14) | 1.25*** | (1.11,1.41) |
| “Something else” | 1.89*** | (1.58,2.26) | 1.31** | (1.10,1.54) |
p<.01
p<.001
NHIS 2013–2018, US adults age 18–64. N=134,266 for pain in 3+ sites and N=95,675 for chronic pain, respectively, in both models.
“Something else” was the actual verbatim terminology used on the NHIS survey; it captures other non-heterosexual identified adults. More information about the design of the sexual identity question is available elsewhere [52].
Complex-survey-adjusted (modified/robust) Poisson models of two pain outcomes.
Model 1 adjusts for age, age squared, sex, and year. Model 2 adjusts for all covariates. Complete results with prevalence ratios for all covariates are shown in Supplemental Table S1.
Table 4.
Decomposition of pain difference between straight and sexual minority adults.
| Composition | Unexplained/coefficients | |||||
|---|---|---|---|---|---|---|
| PANEL A. Pain in 3+ sites (total difference 6.20***, 95% CI 5.17, 7.22) | ||||||
| Overall decomposition | 2.52*** | (1.46,3.59) | 40.7% | 3.67*** | (2.25,5.09) | 59.3% |
| Detailed decomposition | ||||||
| Age | −1.16*** | (−1.67,−0.66) | −18.7% | −0.06 | (−1.11,0.98) | −1.0% |
| Demographics | −1.76* | (−3.39,−0.13) | −28.4% | −1.19 | (−3.31,0.92) | −19.3% |
| Socioeconomic status | 0.47 | (−0.17,1.12) | 7.7% | −0.25 | (−1.11,0.61) | −4.0% |
| Health care | 0.27** | (0.10,0.43) | 4.3% | 0.06 | (−0.68,0.82) | 1.0% |
| Health behaviors | 0.60* | (0.10,1.09) | 9.7% | 1.47 | (−1.96,4.90) | 23.4% |
| Psychological distress | 3.83*** | (3.01,4.65) | 61.8% | 0.17 | (−0.73,1.07) | 2.7% |
| PANEL B. Chronic pain (total difference 6.19***, 95% CI 5.00, 7.37) | ||||||
| Overall decomposition | 2.78*** | (1.57,3.99) | 44.9% | 3.41*** | (1.78,5.03) | 55.1% |
| Detailed decomposition | ||||||
| Age | −1.21*** | (−1.72,−0.52) | −18.1% | −0.52 | (−1.75,0.71) | −8.5% |
| Demographics | −1.51 | (−3.34,0.31) | −24.5% | −1.76 | (−1.76,0.71) | −28.5% |
| Socioeconomic status | 0.59 | (−0.18,1.36) | 9.5% | −0.27 | (−4.44,0.91) | −4.4% |
| Health care | 0.21* | (0.14,0.40) | 3.4% | 0.25 | (−1.23,0.69) | 4.1% |
| Health behaviors | 0.43 | (−0.11,0.97) | 6.9% | 0.33 | (−3.34,4.00) | 5.4% |
| Psychological distress | 3.90*** | (2.97,4.83) | 63.05% | 0.18 | (−0.85,1.21) | 2.9% |
p<.05
p<.01
p<.001
NHIS 2013–2018, US adults age 18–64.
N=131,868 for pain in 3+ sites and 94,240 for chronic pain.
Sexual minority adults are all adults who chose a sexual identity category other than straight. It includes gay, lesbian, bisexual, and “something else.” The latter term was the actual terminology used on the NHIS survey; it captures other non-heterosexual identified adults. More information about the design of the sexual identity question is available elsewhere [52].
Approach
We first estimated prevalence of the two pain measures across sexual-identity categories (Table 1). This table shows estimated weighted prevalences with 95% confidence intervals, the number of respondents in each sexual-identity category, and their percent distribution in the population. We also summarized the difference between each sexual-minority group versus straight adults in absolute terms as percentage-point differences, and in relative terms as prevalence ratios (PR) with associated 95% confidence intervals. The prevalence ratios are estimated from bivariate (unadjusted) robust Poisson models. The robust (modified) Poisson models are optimal for dichotomous outcomes. We prefer them over the widely-used logistic model because the latter yields odds ratios, which have somewhat non-intuitive interpretation, whereas the modified Poisson regressions estimate prevalence ratios, which are easy to communicate to experts and non-specialists alike [2; 68].
We then visualized pain prevalence in each sexual-identity group across age (Figure 1). We used semiparametric models of each pain outcome as a function of flexibly-specified age and linearly-specified year and sex. More information on this approach and its implementation in Stata via the plreg function is readily available [47; 76; 84].
Figure 1.
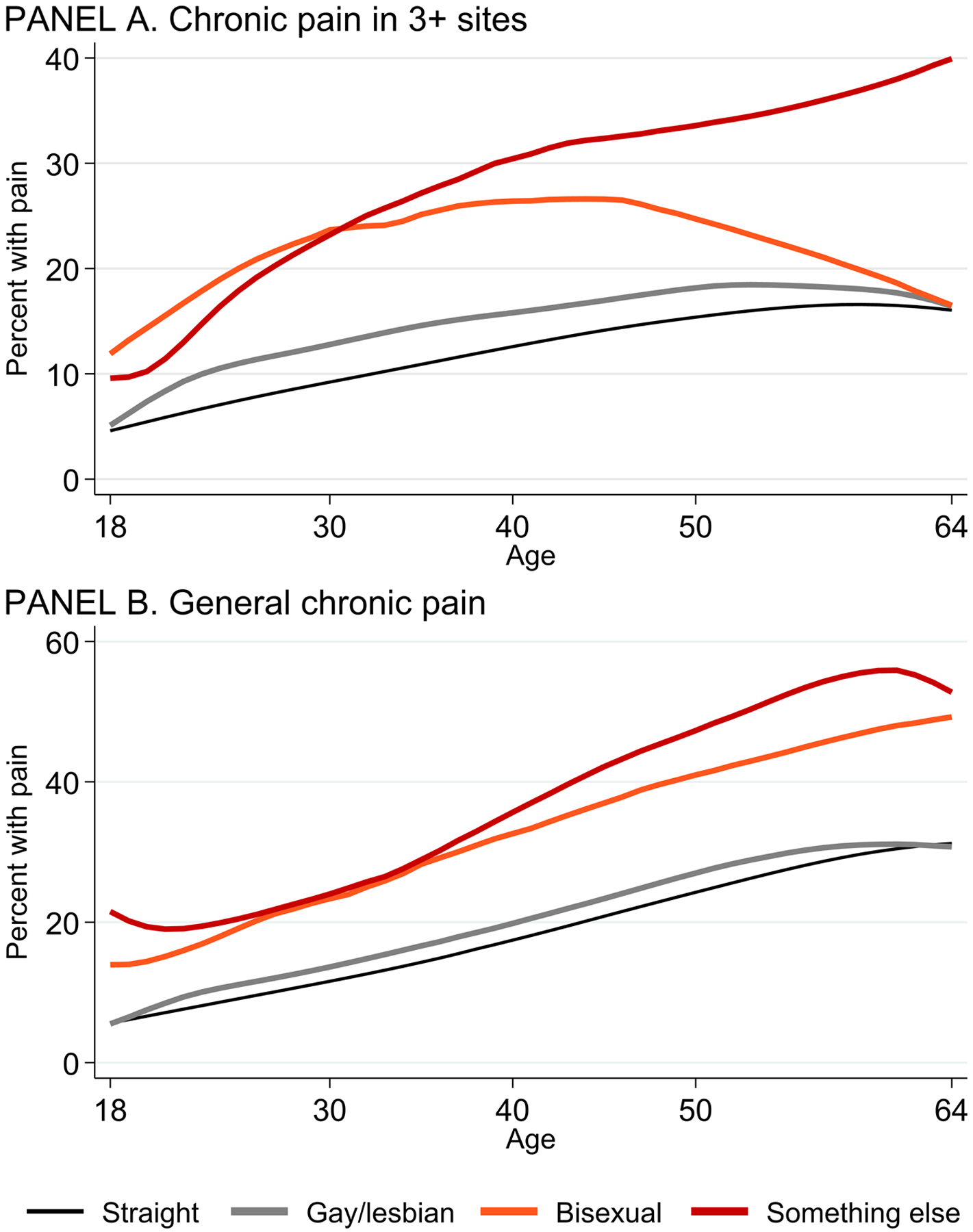
Pain prevalence across age, by sexual identity.
Note
NHIS 2013–2018, US adults age 18–64
Figures visualize findings from semiparametric models of each pain measure (pain in 3+ sites and chronic pain, respectively), with a flexible specification for age, net of sex and year of interview.
Next, we used two approaches to examine the role of covariates (the distribution of which is summarized in Table 2) in the sexual-identity disparities in pain: adjusted Poisson regression model and nonlinear decomposition. First, robust Poisson models were estimated for each pain measure, net of the basic covariate group that comprised age, age squared, sex, and year in Model 1, and a fully adjusted Model 2 (Table 3 shows abbreviated estimates only for the sexual-identity group differences; Supplemental Table S1 shows complete results).
Second, Oaxaca-Blinder-style nonlinear decomposition allowed us to assess the proportion of the observed gap in pain between straight versus sexual-minority adults that is linked to differences in the distribution of covariates or to covariate effects (Table 4). Specifically, the approach quantifies the difference in the outcome (pain) between two groups (straight versus sexual minority) and then decomposes this difference into part linked to population characteristics (compositional changes) and coefficient effects (‘unexplained’) part [5; 59]. We used the mvdcmp extension in Stata for nonlinear decomposition [62], combined with a utility for grouping individual covariates for detailed decomposition, mvdcmpgroup (Powers 2020, personal communication). The effects for categorical variables in this approach are normalized as deviations from a grand mean, which enables calculation of effects for all levels, and yields results that are the same regardless of which level is the omitted reference category [37]. This approach thus yields easily understood results in terms of percent of the observed difference in pain that is linked to compositional differences or effect sizes of included coefficients.
A disadvantage of the Oaxaca-Blinder-style decomposition is that it only allows comparison of two groups at a time. We thus had to combine all sexual-minority groups into one, obscuring potential differences across them. To overcome this weakness, we conducted a supplemental analysis using the Karlson-Holm-Breen (KHB) decomposition method [9; 39]. The KHB decomposition estimates the proportion of observed sexual-identity disparities mediated by each covariate set within a generalized linear modeling framework. The main strength of the KHB is that it allows separate examination of each of the three sexual-poridentity categories; a limitation is that it doesn’t explore the differential effects of covariates (the ‘unexplained’ part in Oaxaca-Blinder). Thus, the KHB supplemental analysis provides a useful complementary perspective on the role of considered covariates in sexual-identity group disparities (Supplemental Table S2).
Finally, we visualized pain prevalence for each pain outcome in each sexual-identity group. We calculated and graphed average predicted probabilities [78] from basic-adjusted and fully-adjusted models using Stata’s margins and coefplot functions (Figure 2). All analyses are conducted in Stata 17 and use appropriate sampling weights.
Figure 2.
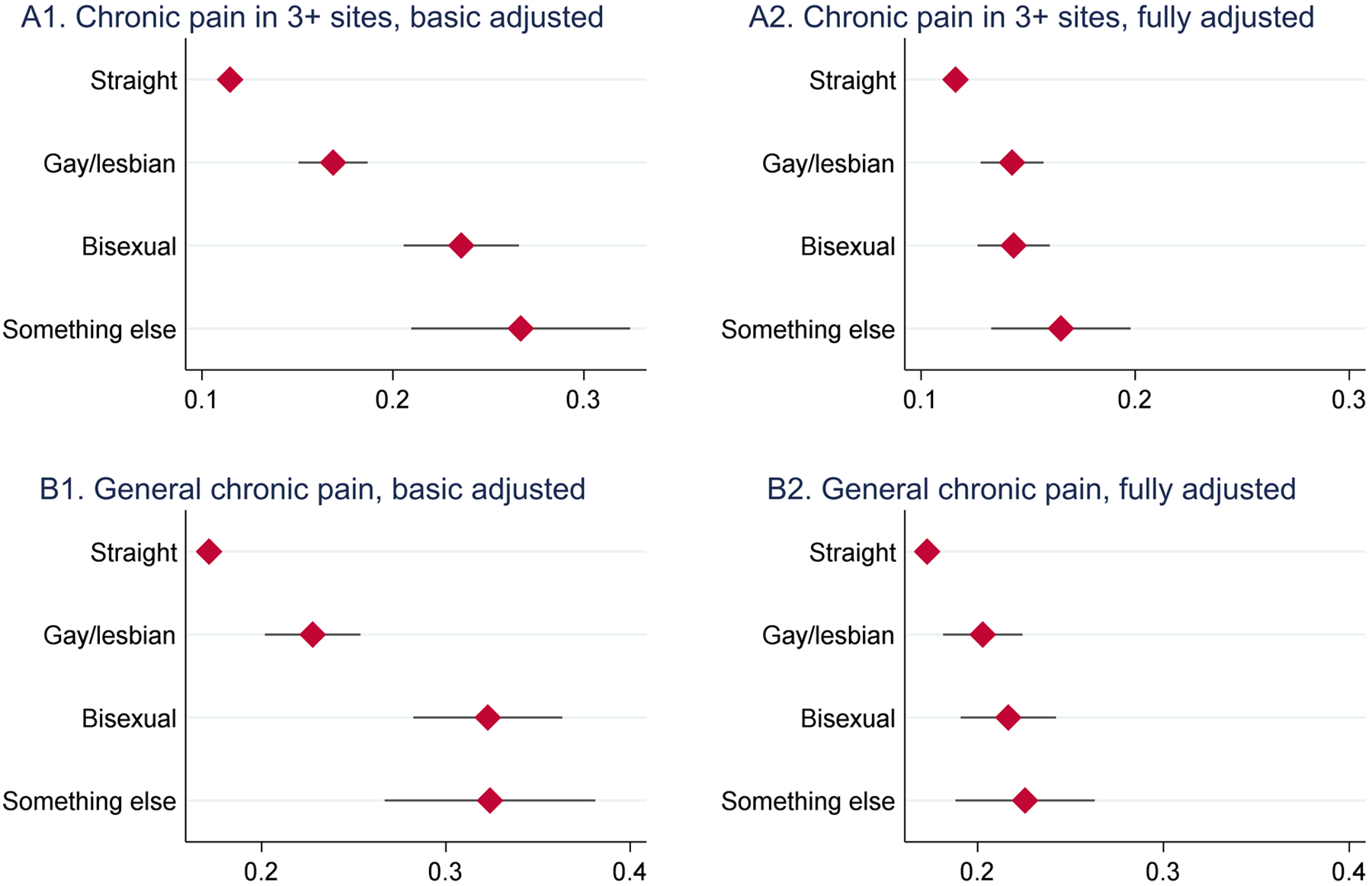
Predicted probability of pain across sexual identity groups
Note
NHIS 2013–2018, US adults age 18–64
Figures show average predicted probabilities of pain (pain in 3+ sites and chronic pain) and their 95% confidence intervals for the population estimates from complex survey-adjusted modified/robust Poisson models.
Model 1 adjusts for age, age squared, sex, and year.
Model 2 adjusts for all covariates.
We conducted numerous auxiliary checks to assess the robustness of our findings to different analytic decisions. Overall, we found the results to be stable across variable, model, and sample specifications, such as defining the age as 18+ or 25+ or estimating the models using logistic regression models. Of particular interest, we estimated models of 14 additional pain measures. The findings are in Supplemental Table S3. Models 1 and 2 focus on alternative operationalizations of site-specific pain (number of pain sites and pain in any site); models 3–7 focus on the five individual pain sites (facial/jaw pain, migraine/headache, joint pain, low back pain, and neck pain). Models 8 and 9 use data from 2013, 2014, 2015, and 2018, when general chronic pain was assessed using the 3-month horizon (not combining it with the 6-month horizon that was asked in 2016 and 2017); additionally, respondents in these waves were askec about pain severity, where severe pain is defined as having “a lot of pain” as opposed to “little” or “in between.” Models 10 and 11 use data from 2016 and 2017, from which two different measures were defined: chronic pain with only the 6-month horizon and high-impact pain, defined as pain that limited life or work activities on most days or every day as opposed to never or some days. Finally, models 12–14 were estimated using data collected in 2019 and 2020. Because of significant changes in sampling design and data collection procedures [35], combining 2019+ with prior waves is not recommended. We estimated models of general chronic pain, severe pain, and high-impact pain using pooled 2019 and 2020 waves. These supplemental models corroborate our main findings but there are some exceptions, which we comment on in the discussion section.
RESULTS
Prevalence of pain among sexual-minority and straight adults
Table 1 shows pain prevalence by sexual identity for both pain measures, using absolute and relative measures. The table also lists the number of respondents in each sexual-identity category and the population proportion they represent (weighted proportions). We highlight three findings. First, pain prevalence is higher for sexual-minority, compared with straight, adults. The differences are substantively large in absolute and relative terms. Pain prevalence is 4.5–11.4 percentage points higher for sexual-minority adults across the three sexual-identity groups and two pain outcomes. For instance, 11.5% of straight adults report pain in 3+ sites, in contrast to over 20% of bisexual adults and those who identified as “something else.” In relative terms, the unadjusted bivariate pain prevalence ratios range from PR=1.26 (95% CI 1.12, 1.41) for gay/lesbian, relative to straight adults, in chronic pain, up to PR=1.99 (95% CI 1.60, 2.46) for adults who identified as “something else,” relative to straight, for pain in 3+ sites. Second, the three sexual minority groups differ in pain prevalence from one another: adults who identified as “something else” have the highest pain prevalence, followed closely by bisexual adults; gay/lesbian adults have the lowest prevalence among the three. And finally, we note that the sample sizes are adequate for all sexual-minority groups and both pain outcomes, with the smallest N=397 for adults who identified as “something else” in analyses of general chronic pain, up to N=2,743 for gay/lesbian adults in analyses of chronic pain in 3+ sites.
Figure 1 visualizes pain prevalence differences among the four sexual-identity groups across age. It was important to check for crossovers or irregularities that would preclude analyzing the full age range together. The figure shows that the patterns across the four groups largely persist across 18–64 age range, except for bisexual adults when analyzing pain in 3+ sites: at mid- and older adulthood their pain converges to that of straight and gay/lesbian adults, although this could possibly be a function of sparse data as there are few older bisexual adults. Overall, the figure highlights the high pain prevalence in sexual-minority groups, especially bisexual adults and those identifying as “something else,” compared with their straight counterparts.
Characteristics of sexual minority and straight groups
We next examined whether the observed pain disparities could be due to differences in key covariates across the four sexual-identity groups. Table 2 shows that, indeed, the four groups differ with respect to all characteristics (at p<.001) except physical activity, where inadequate physical activity level is similar across all four groups. Sexual-minority adults are less likely to be married, have children, or own a home, and more likely to smoke and drink excessively, compared with their straight counterparts. There are differences across the three sexual-minority groups, however. For some variables, only bisexual respondents or those who identify as “something else” differ substantially from straight adults. For instance, bisexual adults are particularly young and have a high prevalence of obesity. Gay/lesbian adults have the highest education of any group, which could be protective against pain [85]. Bisexual adults and those who identify as “something else” are likely to live in low-income households; they also have particularly high levels of psychological distress: 12.2% and 14.1%, respectively, have severe psychological distress compared with 3.5% among straight and 6.2% among gay/lesbian adults.
Poisson regression models
The next question is how these differences might correlate with the pain disparities. Table 3 shows the pain prevalence differences controlling for key covariates (in contrast to unadjusted estimates shown in Table 1). Net of age, age squared, sex, and year of interview (Model 1), gay/lesbian adults have 47% higher prevalence of chronic pain in 3+ sites and 33% higher prevalence of general chronic pain, compared with straight adults. Bisexual adults have 105% and 88% higher prevalence, and adults who identified as “something else” have 133% and 89% higher prevalence of the two pain outcomes, respectively, compared with straight respondents. Net of all covariates (Model 2), the differences between sexual minority and straight adults are smaller but all six estimates remain statistically significant and substantively large. They range from 17% higher prevalence of general chronic pain among gay/lesbian vs. straight adults, up to 42% higher prevalence of pain in 3+ sites among adults who identify as “something else,” compared with their straight counterparts. Supplemental Table S1 shows the full results with point estimates and 95% confidence intervals for all covariates from these four models. The table shows a significant association of many characterristics with pain, even independent of other covariates: non-Hispanic whites, females, adults residing in the Western Census region, the U.S.-born, less educated, lower-income, not employed, current or former smokers, those with former or excessive alcohol use, obese, not physically active, not sleeping an optimal duration, and those less satisfied with their health care have a higher prevalence of pain than their peers. The prevalence ratios for psychological distress are particularly large: adults with severe distress scores have over 200% higher prevalence of pain in 3+ sites (PR=3.16, 95% CI 2.99,3.33) and over 100% higher prevalence of chronic pain (PR=2.13, 95% CI 2.02,2.25), compared with adults who reported low psychological distress, net of all other covariates.
Decomposition Analyses
The findings from the nonlinear Oaxaca-Blinder approach decompose the observed difference in pain prevalence between two groups –straight versus sexual minority -- into a part linked to compositional differences, that is, differences in covariates’ distributions, and a part linked to differences in the associations between the covariates and pain. For pain in 3+ sites, summarized in the top part of Table 4, sexual-minority adults had 6.20 percentage-point higher prevalence than straight adults (95% CI 5.17,7.22). About 41% of this difference could be attributed to the different distribution of characteristics of straight versus sexual-minority adults, while 59% of the pain difference was ‘unexplained’ or due to differential effects of the covariates. The most salient characteristic was psychological distress, which accounted for 62% of the compositional difference. Age (−19%) and other demographic characteristics (−28%) were also notable contributors. The negative sign means that the lower age of sexual minority adults and the racial/ethnic, geographic, and immigrant status composition differences between straight and sexual-minority adults acted as a suppressor of the disparities. Socioeconomic status (8%) and health care covariates (4%) played only a modest, and statistically not significant, role. Findings for general chronic pain were similar: Sexual minority adults had 6.19 percentage point higher pain prevalence than straight adults (95% CI 5.00, 7.37), and 45% of this disparity was due to differential distribution of covariates. Psychological distress (63%) again was the most impactful covariate; age (18%) and other demographics (24%) were salient as well, while socioeconomic status (9%) and health care (3%) were not statistically significant contributors.
Supplemental decomposition using the Karlson-Holm-Breen (KHB) approach, which allowed the examination of the three sexual-minority groups separately, provided a helpful complementary perspective (see Supplemental Table S2). Adults in all three sexual-identity categories had significantly more pain in 3+ and general chronic pain, compared with straight adults, across all models. Jointly, the considered covariates mediated about 44% of the pain disparities between gay/lesbian and straight adults net of age, sex, and year of interview (or more precisely, as Model 7 shows, 44.2% for pain in 3+ sites and 44.7% for general chronic pain) and 60–70% of the disparities between adults who self-identified as bisexual or “something else” versus their straight counterparts (see Model 7’s “% mediated” section). Psychological distress included in Model 5 was the most salient covariate, mediating the majority of the pain disparities for both pain outcomes and all three sexual-identity groups. For gay/lesbian adults, distress explained 36.3% of the differences in pain in 3+ sites and 46.4% for general chronic pain. The percent mediated by distress is greater than the total percent (46.4% versus 44.7%) because socioeconomic status is a suppressor, as gay/lesbian adults have higher SES but greater pain than straight adults. Among adults who self-identified as bisexual or “something else,” psychological distress accounted for roughly 52–57% of the pain disparities. Socioeconomic status and health care included in Models 3 and 6, respectively, were of lesser importance. SES was actually a suppressor of the disparities for gay/lesbian adults as noted above; for adults who identified as bisexual or “something else,” SES explained only 9.1–17.7% of the disparities. Health care was of modest importance as well, explaining between 2.8% and 8.7% of the disparities across the three sexual identity groups and two pain measures.
Predicted Probabilities
Finally, Figure 2 visualizes the pain disparities in absolute terms, adjusted for covariates. The figure shows average predicted probabilities of pain for each sexual-identity group, controlling for basic demographics (Plots A1 and B1 on the left) and for all covariates (Plots A2 and B2 on the right). Three patterns stand out. First, the figures highlight the substantively large pain disparity for the sexual-minority groups, especially in the basic-adjusted models. Second, the figures show large differences across the three sexual-identity categories, as already noted, with particularly high levels of pain for bisexual adults and those who identified as “something else.” And third, the covariates explain a large part of the pain excess, although not all: even plots B1 and B2, from fully-adjusted models, show a significantly higher pain prevalence among sexual-minority adults compared with their straight peers.
DISCUSSION
This study presented the first comprehensive analysis of chronic pain prevalence among sexual-minority U.S. adults who identify as gay or lesbian, bisexual, or “something else.” We highlight three key findings.
First, sexual-minority adults experience significantly and substantially more pain than straight adults. As a group, they have more than 6 percentage points higher pain prevalence, whether measured as chronic pain in 3+ sites or general chronic pain. This translates to over a million more LGBTQ adults experiencing pain over what would be expected if they had pain on par with straight adults. This result is consistent with the rapidly developing literature on LGBTQ health, which has documented disparities in other aspects of mental and physical health [8; 23; 29; 33; 45; 46; 49; 51; 56]. Our study extends the findings to pain, which has been described as a sensitive holistic measure of population health [83].
At the same time, our second key finding shows that pain varies across sexual-minority groups. Bisexual adults and those who identify as “something else” have dramatically more pain than gay/lesbian adults. For instance, gay/lesbian adults have 47% higher age- and sex-adjusted prevalence of pain in 3+ sites than straight adults, but respondents who identify as bisexual or “something else” have over twice the prevalence of straight adults. This finding mirrors results for physical health [33; 46] and mental health [66]. It is likely a function of “double discrimination,” which bisexual and other sexual-minority adults experience from straight as well as gay/lesbian communities, resulting in invisibility [67], identity invalidation [14], and lack of community support [66].
Parenthetically, in supplemental analyses with 2019–20 data (which had to be analyzed separately due to changes in the NHIS data collection procedures [58]), the gap between adults identifying as bisexual or “something else” versus straight was as large or larger than in the prior years, while gay/lesbian adults had pain prevalence on par with their straight counterparts. This finding, which needs to be corroborated in future analyses, suggests increasing disparities within the sexual-minority community, potentially reflecting lessened stigma for gay/lesbian Americans, but continued or worsening social exclusion, discrimination, and violence [70] among adults with bisexual or other sexual-minority identities.
The third key finding pertains to correlates of the disparities. Demographic, socioeconomic, health-behavioral, health-care factor, and psychological distress variables together explain about 41% of the excess pain among sexual-minority adults for pain in 3+ sites, and 45% for chronic pain. Psychological distress is by far the most salient correlate, accounting for the largest part of disparities for both pain outcomes and all three sexual identity groups. Socioeconomic status (SES) and health care covariates, in contrast, played only a modest role in the pain disparities. Although this finding may be unexpected given the importance of SES for pain in general [26; 36; 43; 85], it corroborates results from a recent major study that also found only a modest role of SES in LGBTQ health disparities [67]. We posit that this pattern is consistent with conceptual frameworks of LGBTQ health disparities, which focus on the role of stigma-related psychosocial factors rather than socioeconomic inputs.
Conceptually, LGBTQ pain disparities can be understood with the help of three complementary and interrelated theories: stigma as a fundamental cause of health, minority stress theory, and the social ecological framework. Stigma, a devaluation of sexual-minority identities, relationships, behaviors, and communities, occurs at interpersonal, institutional, and structural/systemic levels [44; 53]. Interpersonally it may cause rejection and violence; at institutional and systemic levels it results in discrimination and exclusion in economic, educational, and political arenas [20; 48; 77]. Across all levels, stigma thus causes stress, harming the health of the stigmatized groups [67]. Stigma as a fundamental cause of health thus underscores the harmful negative stereotyping, prejudice, and discrimination that harms health via persistent chronic stress due to social exclusion [29; 30]. Meanwhile, minority stress theory, the most widely examined model of minority health, focuses on the stress pathway by positing that LGBTQ adults have worse health due to the unique stressors they face as members of a stigmatized minority [22; 49; 51].
The social ecological framework highlights that these social stressors do not inhere within, or originate from, LGBTQ individuals, but from the interpersonal, community, institutional, and structural factors affecting them. Thus, ongoing stress resulting from social exclusion and threats due to stigma originating across micro-, meso-, and macro-level contexts may be the key upstream driver of the pain disparities for sexual minority adults [55]. It may explain why SES did not have strong observable direct effects on the disparities if the harmful effects of stigma flow primarily via psychosocial mechanisms by undermining social relationships [30], increasing negative health behaviors [23; 51], and restricting resources [53; 75] necessary to successfully cope with the excess stress.
The main limitations of our analysis inhere in not having the scope or data to address these and other underlying explanations necessary to better understand the pain patterns for sexual-minority adults and the sources of the disparities. In that sense, the following paragraphs not only delineate the limitations but also serve as a roadmap for future data-collection efforts and empirical studies.
First, sexual identity intersects with gender, as well as racialized, socioeconomic, and other identities and statuses [8; 16; 25]. These intersectional identities result in unique minority stressors and may thus influence pain beyond their arithmetic sum [11; 56]. Moreover, with respect to gender specifically, since stigma is driven by social categories rather than biological sex assigned at birth, the lack of questions about gender identity in NHIS poses an additional limitation. If gender were available in the NHIS data, analysis of intersectionality between sexual and gender identities would be possible with the existing sample sizes. Other intersectional identities may require larger samples than even NHIS currently provides but may become feasible within a few years as additional data accumulate, or from new targeted data collections.
Second, while our analysis explored more detailed sexual-identity categories than prior work, our data still included a residual category for respondents who reported sexual orientation other than heterosexual, gay, lesbian, or bisexual. This “something else” category includes adults who self-identify as pansexual, asexual, queer, or who prefer not to use a specific identity, and the aggregation may obscure relevant pain differences. It is unlikely that NHIS or other federally-funded health surveys will be able to disaggregate this category. We therefore urge LGBTQ-focused data collection efforts, which include sufficient sexual-identity detail, to add pain measures, as powerful barometers of population health and wellbeing [83].
Third, dimensions of sexual orientation comprise not only sexual identity, but also sexual attraction and behavior [7; 60]. These dimensions do not overlap perfectly and, in fact, may have different correlations with pain, as limited prior studies have found for physical [60] and mental health [7]. Federally-funded studies like the NHIS should consider adding items capturing multiple dimensions of sexuality, to better understand the excess pain of LGBTQ adults.
Fourth, chronic pain is a dynamic, multidimensional phenomenon with complicated disease trajectories [79]. Our analyses used static measure that adequately captures population pain burden at a given time, but not individual pain trajectories. Future analyses should use longitudinal panels to explore whether the “disease course” of pain differs across sexual identity because we need to understand the dynamics of pain onset, duration, change, and especially recovery over the life course.
And finally, this last point also highlights limitations with respect to the causality of the associations we described. Because our data were cross-sectional, we caution that the causal arrows among many covariates, although especially psychological distress and pain, are bidirectional [6]. Longitudinal data and causal analytic approaches will thus be needed to disentangle the complex inter-relationships among sexual identity, covariates including mental health, and pain. Additionally, it will be important to directly measure and include upstream structural factors to test the conceptual frameworks we discussed above. These should include measures of structural discrimination and stigma [32; 54], but also protective factors that may buffer negative experiences. The protective factors must comprise experienced social support [56], including from the LGBTQ community [51], as well as individual and community resilience [50]. This research can provide evidence for macro-level policy changes, such as protective policies including non-discrimination laws and hate-crime statutes [29].
Conclusion
We uncovered high levels of pain among sexual-minority adults, especially among those who identified as bisexual or “something else,” and found psychological distress to be a highly salient factor implicated in these pain disparities. Despite encouraging social and legal progress, numerous studies show overwhelmingly that sexual-minority status remains a source of stigma and discrimination [29; 44; 69; 75], which, through psychosocial or material mechanisms, may increase the risk of pain. We hope that future research, as well as new data collection to fill current data gaps, will contribute to a fuller understanding of pain disparities by sexual identity, with the ultimate goal of reducing pain in this integral segment of the population, eliminating health disparities, and achieving full health and wellbeing for all.
Supplementary Material
ACKNOWLEDGEMENTS
Research reported in this analysis was supported by a Canadian Social Science and Humanities Research Council (SSHRC) Insight Grant, and by the National Institute on Aging of the National Institutes of Health under Award Number R01AG065351. The content is solely the responsibility of the authors and does not necessarily represent the official views of SSHRC or the National Institutes of Health.
We thank Harry Alorgbey Sardina, Zoe Huang, Merita Limani, Feinuo Sun, Jason Winders, and Zachary Zimmer for their helpful comments on the manuscript during its development and revisions.
Footnotes
All authors declare no conflicts of interest.
This analysis was not previously presented at any meetings or conferences.
We use the term “sexual minority” rather than “sexual minoritized” to follow precedent in up-to-date scholarship. However, it is important to note that minorities—whether sexual or other, such as racial/ethnic—are minorities because they are “minoritized,” that is, marginalized and disenfranchised by social forces.
Contributor Information
Anna Zajacova, University of Western Ontario.
Hanna Grol-Prokopczyk, University at Buffalo, State University of New York.
Hui Liu, Michigan State University.
Rin Reczek, Ohio State University.
Richard L. Nahin, National Center for Complementary and Integrative Health, National Institutes of Health
REFERENCES
- [1].Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A Systematic Review of the Discrimination Against Sexual and Gender Minority in Health Care Settings. International Journal of Health Services 2020;50(1):44–61. [DOI] [PubMed] [Google Scholar]
- [2].Barros AJ, Hirakata VN. Alternatives for Logistic Regression in Cross-Sectional Studies: An Empirical Comparison of Models that Directly Estimate the Prevalence Ratio. Medical Research Methodology 2003;3(21):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Blanchflower DG, Bryson A. Further decoding the mystery of American pain: The importance of work. PLOS ONE 2022;17(1):e0261891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Blewett LA, Drew JAR, Griffin R, King ML, Williams KCW. IPUMS Health Surveys: National Health Interview Survey, Version 6.4 [dataset]. In: IPUMS editor. Minneapolis, MN, 2019. [Google Scholar]
- [5].Blinder AS. Wage Discrimination: Reduced Form and Structural Estimates. The Journal of Human Resources 1973;8(4):436–455. [Google Scholar]
- [6].Bondesson E, Larrosa Pardo F, Stigmar K, Ringqvist Å, Petersson IF, Jöud A, Schelin MEC. Comorbidity between pain and mental illness – Evidence of a bidirectional relationship. European Journal of Pain 2018;22(7):1304–1311. [DOI] [PubMed] [Google Scholar]
- [7].Bostwick WB, Boyd CJ, Hughes TL, McCabe SE. Dimensions of Sexual Orientation and the Prevalence of Mood and Anxiety Disorders in the United States. American Journal of Public Health 2010;100(3):468–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bränström R, Hatzenbuehler ML, Pachankis JE. Sexual orientation disparities in physical health: age and gender effects in a population-based study. Social psychiatry and psychiatric epidemiology 2016;51(2):289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Breen R, Karlson KB, Holm A. Total, Direct, and Indirect Effects in Logit and Probit Models. Sociological Methods & Research 2013;42(2):164–191. [Google Scholar]
- [10].Cochran SD, Mays VM. Physical Health Complaints Among Lesbians, Gay Men, and Bisexual and Homosexually Experienced Heterosexual Individuals: Results From the California Quality of Life Survey. American Journal of Public Health 2007;97(11):2048–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Crenshaw K Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. The University of Chicago Legal Forum 1989:139. [Google Scholar]
- [12].Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Sexual orientation in the 2013 National Health Interview Survey : A quality assessment. Vital and Health Statistics, Vol. 2. Hyattsville, MD: National Center for Health Statistics; 2014. pp. 1–32. [PubMed] [Google Scholar]
- [13].Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Barriers to Health Care Among Adults Identifying as Sexual Minorities: A US National Study. American Journal of Public Health 2016;106(6):1116–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Doan Van EE, Mereish EH, Woulfe JM, Katz-Wise SL. Perceived Discrimination, Coping Mechanisms, and Effects on Health in Bisexual and Other Non-Monosexual Adults. Arch Sex Behav 2019;48(1):159–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Drabble LA, Wootton AR, Veldhuis CB, Riggle EDB, Rostosky SS, Lannutti PJ, Balsam KF, Hughes TL. Perceived psychosocial impacts of legalized same-sex marriage: A scoping review of sexual minority adults’ experiences. PLOS ONE 2021;16(5):e0249125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dyar C, Taggart TC, Rodriguez-Seijas C, Thompson RG, Elliott JC, Hasin DS, Eaton NR. Physical Health Disparities Across Dimensions of Sexual Orientation, Race/Ethnicity, and Sex: Evidence for Increased Risk Among Bisexual Adults. Archives of Sexual Behavior 2019;48(1):225–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. The Journal of Pain 2016;17(9, Supplement):T70–T92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Elliott MN, Dahlhamer JM, MacCarthy S, Beckett MK, Orr N, Guerino P, Agniel D, Saunders CL, Schuster MA, Ng JH, Martino SC. Using Ancillary Sociodemographic Data to Identify Sexual Minority Adults Among Those Responding “Something Else” or “Don’t Know” to Sexual Orientation Questions. Medical Care 2019;57(12):e87–e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS. Prevalence of Alcohol Dependence Among US Adult Drinkers, 2009–2011. Preventing Chronic Disease 2014;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Everett BG, Limburg A, Homan P, Philbin MM. Structural Heteropatriarchy and Birth Outcomes in the United States. Demography 2022;59(1):89–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Feinberg A, Branton R, Martinez-Ebers V. The Trump Effect: How 2016 Campaign Rallies Explain Spikes in Hate. PS: Political Science & Politics 2022;55(2):257–265. [Google Scholar]
- [22].Flentje A, Heck NC, Brennan JM, Meyer IH. The relationship between minority stress and biological outcomes: A systematic review. Journal of Behavioral Medicine 2020;43(5):673–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fredriksen-Goldsen KI, Kim H-J, Shui C, Bryan AEB. Chronic Health Conditions and Key Health Indicators Among Lesbian, Gay, and Bisexual Older US Adults, 2013–2014. American Journal of Public Health 2017;107(8):1332–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gates GJ. How many people are lesbian, gay, bisexual, and transgender? Los Angeles, CA: The Williams Institute, UCLA, 2011. [Google Scholar]
- [25].Gorman BK, Denney JT, Dowdy H, Medeiros RA. A New Piece of the Puzzle: Sexual Orientation, Gender, and Physical Health Status. Demography 2015;52(4):1357–1382. [DOI] [PubMed] [Google Scholar]
- [26].Grol-Prokopczyk H Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain 2017;158(2):313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Gureje O, Von Korff M, Simon GE, Gater R. Persistent Pain and Well-beingA World Health Organization Study in Primary Care. JAMA 1998;280(2):147–151. [DOI] [PubMed] [Google Scholar]
- [28].H.R. 8404 – 117th Congress (2021–2022). The Respect for Marriage Act, 2022. [Google Scholar]
- [29].Hatzenbuehler ML. Structural Stigma and the Health of Lesbian, Gay, and Bisexual Populations. Current Directions in Psychological Science 2014;23(2):127–132. [Google Scholar]
- [30].Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a Fundamental Cause of Population Health Inequalities. American Journal of Public Health 2013;103(5):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Heslin KC. Explaining Disparities in Severe Headache and Migraine Among Sexual Minority Adults in the United States, 2013–2018. The Journal of Nervous and Mental Disease 2020;208(11):876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Homan P, Brown TH, King B. Structural Intersectionality as a New Direction for Health Disparities Research. Journal of Health and Social Behavior 2021:00221465211032947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hsieh N, Shuster SM. Health and Health Care of Sexual and Gender Minorities. Journal of Health and Social Behavior 2021;62(3):318–333. [DOI] [PubMed] [Google Scholar]
- [34].IPUMS. 2019. NHIS Redesign. Minneapolis, MN: National Center for Health Statistics, n.d. [Google Scholar]
- [35].IPUMS. 2019. NHIS Redesign. Minneapolis, MN: Minnesota Population Center, University of Minnesota, n.d. [Google Scholar]
- [36].Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and Socioeconomic Disparities in Disabling Chronic Pain: Findings From the Health and Retirement Study. The Journal of Pain 2017;18(12):1459–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Jann B The Blinder-Oaxaca decomposition for linear regression models. Stata Journal 2008;8(4):453–479. [Google Scholar]
- [38].Jones JM. LGBT Identification in U.S. Ticks Up to 7.1%. Washington, DC: Gallup, 2022. [Google Scholar]
- [39].Karlson KB, Holm A, Breen R. Comparing Regression Coefficients Between Same-sample Nested Models Using Logit and Probit: A New Method. Sociological Methodology 2012;42:286–313. [Google Scholar]
- [40].Katz-Wise SL, Everett B, Scherer EA, Gooding H, Milliren CE, Austin SB. Factors associated with sexual orientation and gender disparities in chronic pain among U.S. adolescents and young adults. Preventive Medicine Reports 2015;2:765–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kessler RC, Andrews G, Colpe LJ, al. E. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 2002;32(06):959–976. [DOI] [PubMed] [Google Scholar]
- [42].Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE. Screening for serious mental illness in the general population. Archives of general psychiatry 2003;60(2):184–189. [DOI] [PubMed] [Google Scholar]
- [43].Khalatbari-Soltani S, Blyth FM. Socioeconomic position and pain: a topical review. PAIN 2022;163(10). [DOI] [PubMed] [Google Scholar]
- [44].Link BG, Phelan JC. Conceptualizing Stigma. Annual Review of Sociology 2001;27:363–385. [Google Scholar]
- [45].Liu H, Reczek C, Wilkinson L. Introduction: The Health and Well-Being of Sexual Minority Couples. In: Liu H, Reczek C, Wilkinson L, editors. Marriage and Health: The Well-Being of Same-Sex Couples. New Brunswick, NJ: Rutgers University Press, 2020. pp. 1–12. [Google Scholar]
- [46].Liu H, Reczek R. Birth Cohort Trends in Health Disparities by Sexual Orientation. Demography 2021;58(4):1445–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Lokshin M Semi-Parametric Difference-Based Estimation of Partial Linear Regression Models. Stata Journal 2006;6(3):377–383. [Google Scholar]
- [48].Matsick JL, Wardecker BM, Oswald F. Treat sexual stigma to heal health disparities: Improving sexual minorities’ health outcomes. Policy Insights from the Behavioral and Brain Sciences 2020;7(2):205–213. [Google Scholar]
- [49].Meyer IH. Minority Stress and Mental Health in Gay Men. Journal of Health and Social Behavior 1995;36(1):38–56. [PubMed] [Google Scholar]
- [50].Meyer IH. Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity 2015;2(3):209–213. [Google Scholar]
- [51].Meyer IH, Russell ST, Hammack PL, Frost DM, Wilson BD. Minority stress, distress, and suicide attempts in three cohorts of sexual minority adults: A US probability sample. PLoS One 2021;16(3):e0246827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Miller K, Ryan JM. Design, Development and Testing of the NHIS Sexual Identity Question. Hyattsville, MD: National Center for Health Statistics, 2011. [Google Scholar]
- [53].Mize TD. Sexual Orientation in the Labor Market. American Sociological Review 2016;81(6):1132–1160. [Google Scholar]
- [54].Montez JK, Hayward MD, Zajacova A. Trends in U.S. Population Health: The Central Role of Policies, Politics, and Profits. Journal of Health and Social Behavior 2021;62(3):286–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Nagata JM, Ganson KT, Tabler J, Blashill AJ, Murray SB. Disparities Across Sexual Orientation in Migraine Among US Adults. JAMA Neurology 2021;78(1):117–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].National Academies of Sciences E, and Medicine,. Understanding the Well-Being of LGBTQI+ Populations. Washington, DC: National Academies Press, 2020. [PubMed] [Google Scholar]
- [57].National Center for Health Statistics. National Health Interview Survey, Vol. 2016, 2016. [Google Scholar]
- [58].National Center for Health Statistics. Preliminary evaluation of the impact of the 2019 National Health Interview Survey questionnaire redesign and weighting adjustments on Early Release Program estimates. Hyattsville, Maryland, 2020. [Google Scholar]
- [59].Oaxaca R Male-Female Wage Differentials in Urban Labor Markets. International Economic Review 1973;14(3):693–709. [Google Scholar]
- [60].Patterson JG, Jabson JM. Sexual orientation measurement and chronic disease disparities: National Health and Nutrition Examination Survey, 2009–2014. Annals of Epidemiology 2018;28(2):72–85. [DOI] [PubMed] [Google Scholar]
- [61].Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and Profile of High-Impact Chronic Pain in the United States. The Journal of Pain 2019;20(2):146–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Powers DA, Yoshioka H, Yun M-S. Mvdcmp: Multivariate Decomposition for Nonlinear Response Models. The Stata journal 2011;11(4):556–576. [Google Scholar]
- [63].Prochaska JJ, Sung H-Y, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research 2012;21(2):88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Rice ASC, Smith BH, Blyth FM. Pain and the global burden of disease. Pain 2016;157(4):791–796. [DOI] [PubMed] [Google Scholar]
- [65].Roberts AL, Rosario M, Corliss HL, Wypij D, Lightdale JR, Austin SB. Sexual orientation and functional pain in U.S. young adults: the mediating role of childhood abuse. PLoS One 2013;8(1):e54702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Ross LE, Salway T, Tarasoff LA, MacKay JM, Hawkins BW, Fehr CP. Prevalence of Depression and Anxiety Among Bisexual People Compared to Gay, Lesbian, and Heterosexual Individuals:A Systematic Review and Meta-Analysis. The Journal of Sex Research 2018;55(4–5):435–456. [DOI] [PubMed] [Google Scholar]
- [67].Stacey L, Reczek R, Spiker R. Toward a Holistic Demographic Profile of Sexual and Gender Minority Well-being. Demography 2022;59(4):1403–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: Choice comes with consequences. Statistics in Medicine 2016;35(30):5730–5735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Taylor P A survey of LGBT Americans : attitudes, experiences and values in changing times. Washington, DC: Pew Research Center, 2013. [Google Scholar]
- [70].Truman JL, Morgan RE. Violent Victimization by Sexual Orientation and Gender Identity, 2017–2020: U.S. Department of Justice, 2022.
- [71].Turner TM, Luea H. Homeownership, wealth accumulation and income status. Journal of Housing Economics 2009;18(2):104–114. [Google Scholar]
- [72].U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. In: CfDCaP Department of Health and Human Services editor. Washington DC: Department of Health and Human Services, Centers for Disease Control and Prevention, 2018. [Google Scholar]
- [73].U.S. Supreme Court. Obergefell v. Hodges. 135 SCt 2584, 2015.
- [74].Vang ZM, Chau S, Kobayashi KM, Owen MJ, McKenzie-Sampson S, Mayrand-Thibert J, Brass GM. Pain and Functional Limitations Among Midlife and Older Canadians: The Role of Discrimination, Race, and Sense of Belonging. The Journals of Gerontology: Series B 2021:gbab137. [DOI] [PubMed] [Google Scholar]
- [75].VanKim NA. Sexual minority status: An overlooked stigma that affects food insecurity. American Journal of Clinical Nutrition 2021;114(6):1890–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Veradi V Semiparametric regression in Stata. RePEc:boc:usug13:14, 2013. [Google Scholar]
- [77].Wickham RE, Gutierrez R, Giordano BL, Rostosky SS, Riggle EDB. Gender and Generational Differences in the Internalized Homophobia Questionnaire: An Alignment IRT Analysis. Assessment 2021;28(4):1159–1172. [DOI] [PubMed] [Google Scholar]
- [78].Williams R Using the Margins Command to Estimate and Interpret Adjusted Predictions and Marginal Effects. The Stata journal 2012;12(2):308–331. [Google Scholar]
- [79].Yang Y, Grol-Prokopczyk H. Chronic Pain and Friendship among Middle-Aged and Older U.S. Adults. Journal of Gerontology: Series B Social Sciences 2020;Published 29 October 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Zajacova A Health in Working-Age Americans: Adults with a High School Equivalency (GED) Diploma Are Similar to Dropouts, Not High School Graduates. American Journal of Public Health 2012;102(S2):S284–S290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Zajacova A, Grol-Prokopczyk H, Fillingim R. Beyond Black vs White: Racial/Ethnic Disparities in Chronic Pain including Hispanic, Asian, Native American, and Multiracial U.S. Adults. PAIN® 2022;163(9): 1688–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Zajacova A, Grol-Prokopczyk H, Zimmer Z. Pain Trends Among American Adults, 2002–2018: Patterns, Disparities, and Correlates Demography 2021;58(2):711–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Zajacova A, Grol-Prokopczyk H, Zimmer Z. Sociology of Chronic Pain. Journal of Health and Social Behavior 2021;62(3):302–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Zajacova A, Montez JK. Explaining the increasing disability prevalence among mid-life US adults, 2002 to 2016. Social Science & Medicine 2018;211:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Zajacova A, Rogers RG, Grodsky E, Grol-Prokopczyk H. The Relationship between Education and Pain among Adults Aged 30–49 in the United States. Journal of Pain 2020;21(11–12):1270–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Zimmer Z, Zajacova A. Persistent, Consistent and Extensive: The Trend of Increasing Pain Prevalence in Older Americans. J Gerontol 2020;75(2):436–447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


