Abstract
Background:
Atrial functional mitral regurgitation (AFMR) is associated with increased morbidity and mortality. Left atrial (LA) size and function in AFMR are poorly characterized.
We aimed to assess LA function by reservoir strain (LASr) and estimated reservoir work (LAWr) and their impact on outcome in AFMR.
Methods:
Consecutive patients at our institution between 2001–2019 and with significant (moderate or greater) AFMR were examined. LAWr was estimated as LASr x LA reservoir volume, and patients were grouped by median LASr and LAWr. Outcomes were all-cause death or heart failure hospitalizations.
Results:
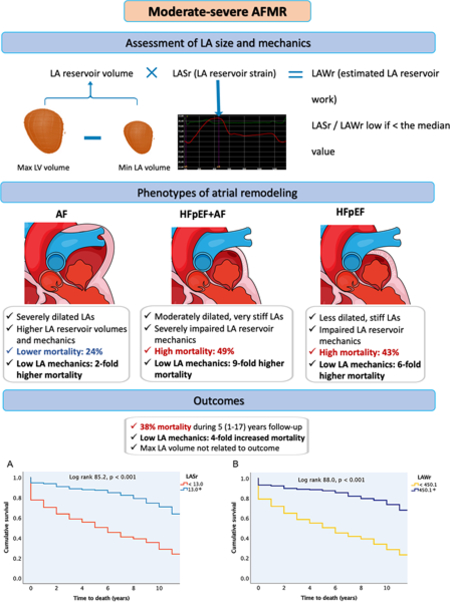
515 AFMR patients were followed up for 5 [1–17] years. Patients had previously documented atrial fibrillation (AF) (37%), heart failure with preserved ejection fraction (HFpEF) without AF (24%), or both (HFpEF+AF, 39%). LA volume was largest in AF, while LA function parameters were most impaired in the combined HFpEF+AF group.
During follow-up, patients with low LASr or LAWr had higher risk of death (p<0.001) and heart failure hospitalization (p<0.05). In Cox regression analyses, low LASr and LAWr, but not LA volume or left ventricular function, were associated with a higher risk of death (LASr: HR 2.3 (95% CI 1.6–3.5), LAWr: HR 3.4 (95% CI 2.4–4.9), both p<0.001) after adjustment for clinical and echocardiographic confounders. Low LASr and LAWr were strongest associated with death in HFpEF and HFpEF+AF.
Conclusions:
LA reservoir function but not LA size is a robust predictor of outcome in significant AFMR. This provides mechanistic insights into the interplay of functional versus geometric LA changes in AFMR.
Journal Subject Terms: Valvular Heart Disease, Remodeling, Echocardiography, Imaging, Mortality/ Survival
Keywords: functional mitral regurgitation, left atrial function, atrial reservoir function, mitral valve, echocardiography
Graphic Abstract:
Introduction
Functional mitral regurgitation (MR) is caused by geometric changes of the mitral apparatus without concomitant structural leaflet pathology. A common type of secondary MR is associated with left ventricular (LV) remodeling in the context of ischemic heart disease or dilated cardiomyopathy. More recently, atrial functional MR (AFMR) has been recognized as a type of secondary MR with distinct mechanisms and clinical features than that due to ischemic or myopathic LV remodeling. AFMR is mostly described in patients with normal LV size and preserved ejection fraction (EF), mitral leaflets with normal echocardiographic appearance and dilated left atrium (LA) 1.
AFMR is common in elderly individuals with atrial arrythmias, but is also associated with heart failure (HF) with preserved ejection fraction (HFpEF) 2. The clinical impact of this secondary MR subtype will escalate due to the ageing of the population worldwide, and the ongoing obesity and atrial fibrillation (AF) epidemic. The mortality risk of AFMR is comparable to that of degenerative MR 3. However, its mechanisms and clinical presentation are poorly defined, and in the recent ESC/EACTS and AHA/ACC valvular heart disease guidelines, AFMR is recognized mainly in the context of AF, and lacks separate recommendations for grading, follow-up, and treatment 4, 5.
Mechanistically, AFMR is commonly attributed to adverse LA remodeling such as increased left atrial and annular size. However, the impact of atrial mechanics has been scarcely described. Atrial mechanical function may be an important contributor to clinical outcome in AFMR 6. We aim to characterize left atrial function and remodeling patterns in a large population of patients with significant AFMR and assess the independent impact of atrial mechanics on the patients′ long-term outcome.
Methods
Study population:
Patients with AFMR examined at the Massachusetts General Hospital in the period 2001–2019 were identified in the institutional echocardiographic database. The definition of AFMR was significant (moderate or greater) MR with normal-sized LV and LV function (LVEF ≥ 50%) (Carpentier type I) 6. Patients with LV wall motion abnormalities or other MR mechanisms were excluded. The echocardiographic evaluation that was the basis for inclusion is referred to as the index examination. Only patients followed up at the Massachusetts General Hospital were included in the study. MR severity was graded using a standardized and integrative method based on combined qualitative, semi-quantitative and quantitative evaluation 7 performed by cardiologists with specialized expertise in echocardiography. Patients with evidence of structural mitral valve pathology, other severe valve disease, hypertrophic or dilated cardiomyopathy, congenital heart disease, pulmonary embolism or constrictive pericarditis were excluded.
Obesity was defined as a body mass index ≥ 30kg/m2. Relevant comorbidities, including HFpEF, daily medication, including HF treatment, and symptoms at presentation were obtained via chart review. History of AF was assessed by manual review of all resting electrocardiograms (available in all patients), 24-hours Holter registrations (available in 11% of the study population) and charts prior to the index examination. Type of heart rhythm during echocardiography was also assessed.
The study was approved by the Institutional Review Board and was conducted in accordance with the revised Declaration of Helsinki. Due to the retrospective nature of the study, informed consent was not required. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Echocardiographic measurements:
Comprehensive transthoracic echocardiograms were performed by experienced sonographers and analyzed on Syngo Dynamics stations (Siemens Medical Solutions Munich, Germany) equipped with 2D speckle tracking software (2D Cardiac Performance Analysis, Tomtec Arena 2.42, Unterschleissheim, Germany).
LA size and function:
LA volume was measured in dedicated apical 4- and 2- chamber views at three different time points: end-diastole (the frame just after mitral valve closure), onset of atrial contraction (identified by the P-wave on ECG) and end-systole (the frame just before mitral valve opening), rendering minimum (LAVmin), pre-A and maximum LA volume (LAVmax), respectively 8. LA appendage and the ostia of pulmonary veins, if visible, were excluded from the volumes. LA’s dilatation was assessed based on LAVmax indexed for body surface area (BSA). The increase in LA volume from minimum to maximum during the reservoir phase defined the LA reservoir volume (also referred to as the total emptying LA volume in the literature) 9. The LA emptying fraction was calculated as the ratio of the LA reservoir volume and LAVmax.
LA strain was measured using specific software (2D Cardiac Performance Analysis, Tomtec Arena, Germany) and end-diastole as the zero-strain reference point 9. LA reservoir function was assessed by the reservoir strain (LASr) and additionally estimated from the product LASr (as a surrogate of LA pressure change 10–12) x LA reservoir volume 13–15, a simplified index of LA’s reservoir work (LAWr).
Additionally, the LA expansion index, a previously proposed marker of reservoir function, was deducted from the ratio of LA reservoir volume to LAVmin 16. In patients in sinus rhythm at the index examination, LA strain during the atrial contraction phase (LASct) was also quantified 9. In patients in AF, both LA size and function were assessed in three consecutive cardiac cycles during reasonably regular rhythm and averaged 9.
Of note, the ratio of mitral peak E-wave velocity and mitral annular e’ velocity is not reported as it is not recommended used in functional analyses in patients with significant MR and preserved LV EF 17, 18.
LV size and function:
LV size was evaluated by the 2D wall and cavity linear dimensions and by triplane volumes following the joint American Society of Echocardiography and European Association of Cardiovascular Imaging guidelines 19. LV hypertrophy was identified as recommended in populations with higher prevalence of obesity as LV mass indexed for height2.7 ≥49.2g/m2.7 in men and ≥46.7 g/m2.7 in women 20–22. The ratio of LV end-diastolic posterior wall thickness/internal diameter (the relative wall thickness) indicated concentric LV geometry when equal or above 0.43 23.
LV systolic function was assessed by both EF and GLS (low if less negative than -16.7% in men and <-17.8% in women) using all three standard apical views 19, 24.
Echocardiographic control group:
To examine the individual impact of AFMR on LA function, we additionally measured LA size and reservoir function in a separate, contemporary cohort (examined between 2017–2022) of patients with an established HFpEF diagnosis, none or trace MR, no history of atrial arrhythmias and sinus rhythm at the index examination, and echocardiographic data suitable for speckle tracking analysis. The exclusion criteria were otherwise similar as for the main study population. A group of 100 controls with a comparable age and gender composition as the main study population was identified and used as a comparison sample in analyses of echocardiographic data.
Outcomes:
We examined the prognostic value of measures of LA reservoir function in relation to all-cause mortality and HF hospitalizations. Patients were followed up beginning with the day of the index examination and up to 2021. All deaths were ascertained from medical records and the social security death index. Hospitalization for HF was ascertained from chart reviews.
Statistical analyses:
All statistical analyses were performed using IBM SPSS Statistics 28.0 (Armonk, NY: IBM Corp.). Between-group differences were assessed by unpaired t-tests, one-way ANOVA with Sidaks′ posthoc test, chi-square or Fisheŕs exact test as appropriate. Due to fundamentally different atrial mechanics, atrial size and function are reported separately for patients in sinus rhythm and atrial fibrillation at the index examination. Findings are reported as mean±standard deviation and median values with error bars for the 95% confidence intervals for continuous variables, and percentages for categorical variables.
The impact of LA function on outcomes was tested in Kaplan-Meier survival analyses with log-rank test for the overall analysis, as well as in univariable and multivariable Cox regression analyses. Additionally, the strength of the relationship between different indexes of LA function and death was assessed in Receiver Operating characteristic (ROC) analysis with comparison between the areas under the curve of the different parameters. For survival analyses, patients were grouped according to the median value of LASr and LAWr, and the association with all-cause death assessed univariably in the whole AFMR population as well as in the three AFMR subgroups: HFpEF, AF, and HFpEF+AF. Multivariable Cox regression models were additionally run in the whole AFMR population, and covariates selected based both on clinical relevance and a p<0.1 level of significance for the association with the dependent variables in univariable analyses. Results are reported as hazard ratios with 95% confidence intervals (CI). A two-tailed p≤0.05 was considered significant both in univariable and multivariable analyses.
Results
Study population:
A total of 515 patients with significant AFMR (97% with moderate and 3% with severe AFMR) were included (Figure 1). Among them, 124 (24%) had previously documented HFpEF but no atrial arrythmias, 193 (38%) had a history of AF, and 198 (38%) had both HFpEF and AF (HFpEF+AF). While the groups had comparable distribution of sexes and equally high prevalence of hypertension, patients with HFpEF+AF were significantly older and had higher prevalence of chronic obstructive pulmonary disease and peripheral vascular disease (Table 1). The AF group had less comorbidities including less diabetes mellitus, chronic kidney disease and clinical vascular disease, slightly higher hemoglobin and lower creatinine than the other two groups. Combined HFpEF+AF was associated with a higher prevalence of symptoms at the index examination, particularly dyspnea and chest pain, and these patients used more often beta-blockers, diuretics and mineralocorticoid receptor antagonists (Table 1).
Figure 1.
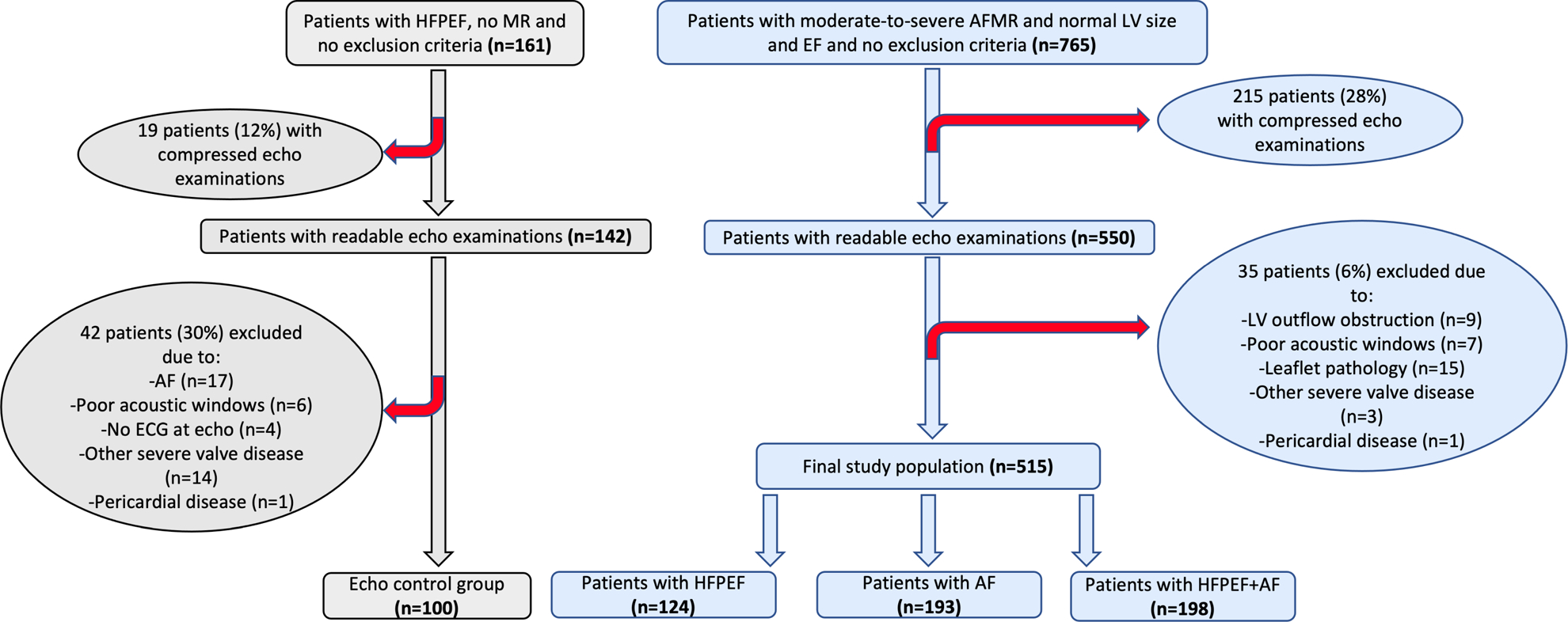
Study enrollment flow chart.
Table 1.
Demographics and clinical characteristics.
| All (n=515) | HFpEF (n=124) | AF (n=193) | HFpEF+AF (n=198) | p value | |
| Age, years | 71 ± 12 | 66 ± 14* | 71 ± 9* | 74 ± 12* | <0.001 |
| Female sex | 56 % | 57 % | 52 % | 58 % | 0.42 |
| Obesity | 26 % | 33 % | 23 % | 25 % | 0.13 |
| Heart rate, bpm | 71 ±18 | 68 ±14 | 72 ± 20 | 73 ± 19 | 0.06 |
| Hypertension | 82 % | 84 % | 79 % | 83 % | 0.44 |
| Hypercholesterolemia | 38 % | 35 % | 35 % | 44 % | 0.09 |
| Diabetes mellitus | 30 % | 35 % | 23 % | 34 % | 0.03 |
| Chronic kidney disease | 20 % | 31 % | 8 % | 25 % | <0.001 |
| COPD | 14 % | 11 % | 6 % | 22 % | <0.001 |
| Previous myocardial infarction | 7 % | 11 % | 3 % | 8% | 0.005 |
| Previous stroke | 7 % | 7 % | 5 % | 10 % | 0.12 |
| Peripheral vascular disease | 12 % | 13 % | 7 % | 16 % | 0.03 |
| Dyspnea | 47 % | 52 % | 36 % | 55 % | <0.001 |
| Chest pain | 55 % | 55 % | 48 % | 63 % | 0.009 |
| Palpitations | 36 % | 23 % | 38 % | 41 % | 0.003 |
| Hemoglobin, g/dl | 11.8 ±2.2 | 11.1 ± 2.2* | 12.5 ± 1.9* | 11.7 ±2.1* | <0.001 |
| Creatinine, mg/dl | 1.3 ± 1.0 | 1.7 ± 1.5* | 1.1 ± 0.5† | 1.3 ± 0.8† | <0.001 |
| Medication | |||||
| Beta-blocker | 65 % | 55 % | 62 % | 75 % | <0.001 |
| ACE inhibitor or ARB | 42 % | 43 % | 40 % | 44 % | 0.71 |
| Diuretic | 52 % | 54 % | 35 % | 67 % | <0.001 |
| MRA | 5 % | 4 % | 2 % | 9 % | 0.007 |
Values are mean ± standard deviation or percentage. The p value in the last table column indicates the statistical significance when testing the overall group differences (by ANOVA for continuous variables and chi-square or Fisheŕs exact test for categorical variables).
p < 0.05 vs. all the other groups by Sidaks′ posthoc test.
p < 0.05 vs. the HFpEF group by Sidaks′ posthoc test.
ACE = angiotensin-converting enzyme; AF = atrial fibrillation; ARB = angiotensin receptor blocker; BMI = body mass index; COPD = chronic obstructive pulmonary disease; HFpEF = heart failure with preserved ejection fraction; MRA = mineralocorticoid receptor antagonist.
Ventricular size and function:
Patients had on average normal LV cavity size, mass, and EF with no between-groups differences (Table 2). Concentric LV remodeling was a frequent finding in this study population, but with an even distribution among the three groups. Of note, LV mass index was similar in HFpEF patients with and without AF, underlining the multifactorial nature of increased LV filling pressure in HFpEF.
Table 2.
Cardiac structure and function.
| All (n=515) | HFpEF (n=124) | AF (n=193) | HFpEF+AF (n=198) | p value | |
| LV EDD, mm | 46 ± 5 | 46 ± 5 | 46 ±5 | 46 ± 5 | 0.59 |
| LV ESD, mm | 30 ± 4 | 30 ± 4 | 31 ± 4 | 31 ± 5 | 0.80 |
| LV mass, g | 177 ± 47 | 178 ± 49 | 177 ± 48 | 177 ± 46 | 0.97 |
| LV mass index, g/h 2.7 | 43 ± 10 | 45 ± 12 | 42 ± 8† | 44 ± 11 | 0.03 |
| LV hypertrophy | 31 % | 40 % | 22 % | 33 % | 0.009 |
| LV relative wall thickness | 0.45 ± 0.09 | 0.45 ± 0.1 | 0.45 ± 0.08 | 0.46 ± 0.09 | 0.23 |
| LV concentric geometry | 57 % | 58 % | 54 % | 59 % | 0.63 |
| LV EDV, ml | 117 ± 35 | 124 ± 34 | 120 ± 36 | 110 ± 33† | 0.001 |
| LV EF, % | 65 ± 7 | 66 ± 7 | 65 ± 7 | 64 ± 8† | 0.03 |
| LV GLS, % | −17.3 ± 4.1 | −19.0 ± 3.9* | −16.7 ± 4.0 | −16.9 ± 4.0 | <0.001 |
| Low GLS | 50 % | 32 % | 55 % | 57 % | <0.001 |
| LV GCS, % | −26.8 ± 5.5 | −28.4 ± 5.0‡ | −25.5 ± 5.3* | −27.0 ± 5.6‡ | <0.001 |
| Dilated right ventricle § | 17 % | 9 % | 15 % | 23 % | 0.04 |
| Right ventricular systolic dysfunction § | 7 % | 6 % | 4 % | 10 % | 0.16 |
| Mild/moderate tricuspid regurgitation | 82 % | 74 % | 83 % | 83 % | <0.001 |
| Estimated SPAP, mmHg | 45 ± 13 | 49 ± 16‡ | 41 ± 9 | 46 ± 13‡ | <0.001 |
Values are mean ± standard deviation or percentage. The p value in the last table column indicates the statistical significance when testing the overall group differences (by ANOVA for continuous variables and chi-square or Fisheŕs exact test for categorical variables).
p < 0.05 vs. all the other groups by Sidaks′ posthoc test.
p < 0.05 vs. the HFpEF group by Sidaks′ posthoc test.
p < 0.05 vs. the AF group by Sidaks′ posthoc test.
Based on qualitative assessment.
AF = atrial fibrillation; EDD = end-diastolic diameter; EDV = end-diastolic volume; EF = ejection fraction; ESD = end-systolic diameter; GCS = global circumferential strain; GLS = global longitudinal strain; HFpEF = heart failure with preserved ejection fraction; LV = left ventricular; SPAP = systolic pulmonary artery pressure.
LV GLS was on average at the lower limit of normal in the whole population (Table 2). In patients in sinus rhythm during the index echocardiography, the mean LV GLS value was normal and comparable between groups: ∕18.9±3.9%/∕19.1±3.5%/∕18.5±3.8% in the HFpEF/ AF/ HFpEF+AF group, respectively. Considering only patients in AF at the index examination, LV GLS was similarly impaired in the AF and HFpEF+AF groups: ∕15.2±3.6% vs ∕15.7±3.7%. Furthermore, patients with combined HFpEF+AF had more frequently a dilated right ventricle with impaired global systolic function (Table 2).
LA function and phenotypes of LA remodeling:
In the whole study population, LAVmax was increased (LAVmax/BSA ≥35ml/m2) in 90% of patients, and severely increased (LAVmax/BSA ≥60ml/m2) in 37%. LASr and LAWr were both severely impaired (Table 3). Patients with LASr and LAWr below the median values were older, had a longer AF history, higher heart rate, used more often a diuretic, had larger LAVmax and LAVmin and more often combined HFpEF+AF.
Table 3.
LA size and function.
| HFpEF controls without MR (n=100) | All patients (n=515) |
HFpEF (n=124) | AF (n=193) | HFpEF+AF (n=198) | p value | |||
| Sinus rhythm at echo | AF at echo | Sinus rhythm at echo | AF at echo | |||||
| LAVmax, ml | 86 ± 28 | 106 ± 36 | 85 ± 24* | 105 ± 27†# | 124 ± 38 | 96 ± 29†# | 118 ± 42 | <0.001 |
| LAVmax/ BSA, ml/m 2 | 46 ± 14 | 56 ± 18 | 45 ± 12* | 55 ± 14†# | 64 ± 17 | 52 ± 14†# | 64 ± 23 | <0.001 |
| LAVmax/BSA ≥35 ml/m2 | 80% | 90% | 78% | 95% | 94% | 94% | 95% | <0.001 |
| LAVmax/BSA ≥60 ml/m2 | 12% | 37% | 11% | 32% | 61% | 24% | 54% | <0.001 |
| LAVmin, ml | 34 ± 18|| | 70 ± 34 | 47 ± 21* | 61 ± 22†# | 96 ± 32 | 58 ± 25†# | 85 ± 36 | <0.001 |
| LAVmin/ BSA, ml/m 2 | 18 ± 9|| | 37 ± 18 | 25 ± 11* | 32 ± 12†# | 50 ± 15 | 31 ± 13†# | 46 ± 21 | <0.001 |
| LA reservoir volume, ml | 52 ± 16|| | 36 ± 15 | 38 ± 14‡ | 44 ± 15†# | 27 ± 11 | 39 ± 15‡# | 33 ± 17 | 0.07 |
| LA emptying fraction, % | 62 ± 11|| | 36 ± 15 | 46 ± 15 | 43 ± 11# | 23 ± 8 | 41 ± 14†# | 29 ± 12 | <0.001 |
| LA expansion index, % | 186 ± 86|| | 66 ± 49 | 102 ± 64* | 80 ± 32# | 31 ± 14 | 79 ± 46# | 45 ± 27 | <0.001 |
| LASr, % | 29.1 ± 8.1|| | 14.8 ± 7.6 | 19.9 ± 8.6§ | 19.4 ± 5.8§# | 9.4 ± 3.5 | 16.5 ± 6.6‡*# | 10.6 ± 5.1 | <0.001 |
| LAWr, %xml | 1550 ± 685|| | 596 ± 482 | 822 ± 507* | 907 ± 522§# | 275 ± 176 | 714 ± 507# | 392 ± 310 | <0.001 |
| LASct, % | −12.3 ± 6.2|| | −3.5 ± 4.5 | −7.2 ± 4.7§ | −6.7 ± 4.2§# | Na | −4.9 ± 3.6*# | na | <0.001 |
Values are mean ± standard deviation or percentage. HFpEF controls without AFMR were compared with the subgroup of patients with HFpEF and AFMR using independent samples t-test.
The p value in the last table column indicates the statistical significance when testing the overall group differences by ANOVA.
p < 0.05 vs. all the other groups by Sidaks′ posthoc test.
p < 0.05 vs. the HFpEF group by Sidaks′ posthoc test.
p < 0.05 vs. the AF group by Sidaks′ posthoc test.
p < 0.05 vs. the HFpEF+AF group by Sidaks′ posthoc test.
p < 0.001 between the HFpEF controls without MR and the HFpEF patient group with AFMR by independent samples t-test.
p < 0.001 between patients in sinus rhythm and patients in AF at the echocardiographic examination in the AF and HFpEF+AF groups, respectively, by independent samples t-test.
AF = atrial fibrillation; BSA = body surface area; HFpEF = heart failure with preserved ejection fraction; LA = left atrial; LASct = left atrial contraction strain; LASr = left atrial reservoir strain; LAVmax = maximum left atrial volume; LAVmin = minimum left atrial volume; LAWr = left atrial reservoir work. Na = not applicable.
The pattern of LA remodeling differed between the 3 AFMR groups. In the AF and HFpEF+AF groups, patients in AF at the index examination (61% and 59% of the AF and HFpEF+AF groups, respectively) had the largest LAVs of the whole population, and concomitantly severely impaired reservoir function by either LASr, LAWr and LA expansion index (Table 3, Figure 2). When comparing only patients in sinus rhythm at echocardiography, the HFpEF and AF groups had significant differences in LAVmax, LAVmin and LA reservoir volume, with the HFpEF patients having the smallest LA volumes and the AF group the largest ones. Moreover, HFpEF patients had comparable LASr, but lower LASr normalized for heart rate and lower LAWr than the AF group. The HFpEF+AF patients had intermediate LA size, but the most severe atrial dysfunction by either LASr or LAWr (Table 3, Figure 2).
Figure 2. Comparison of atrial function and size between HFpEF controls and the three AFMR subgroups: HFpEF, AF and HFpEF+AF.
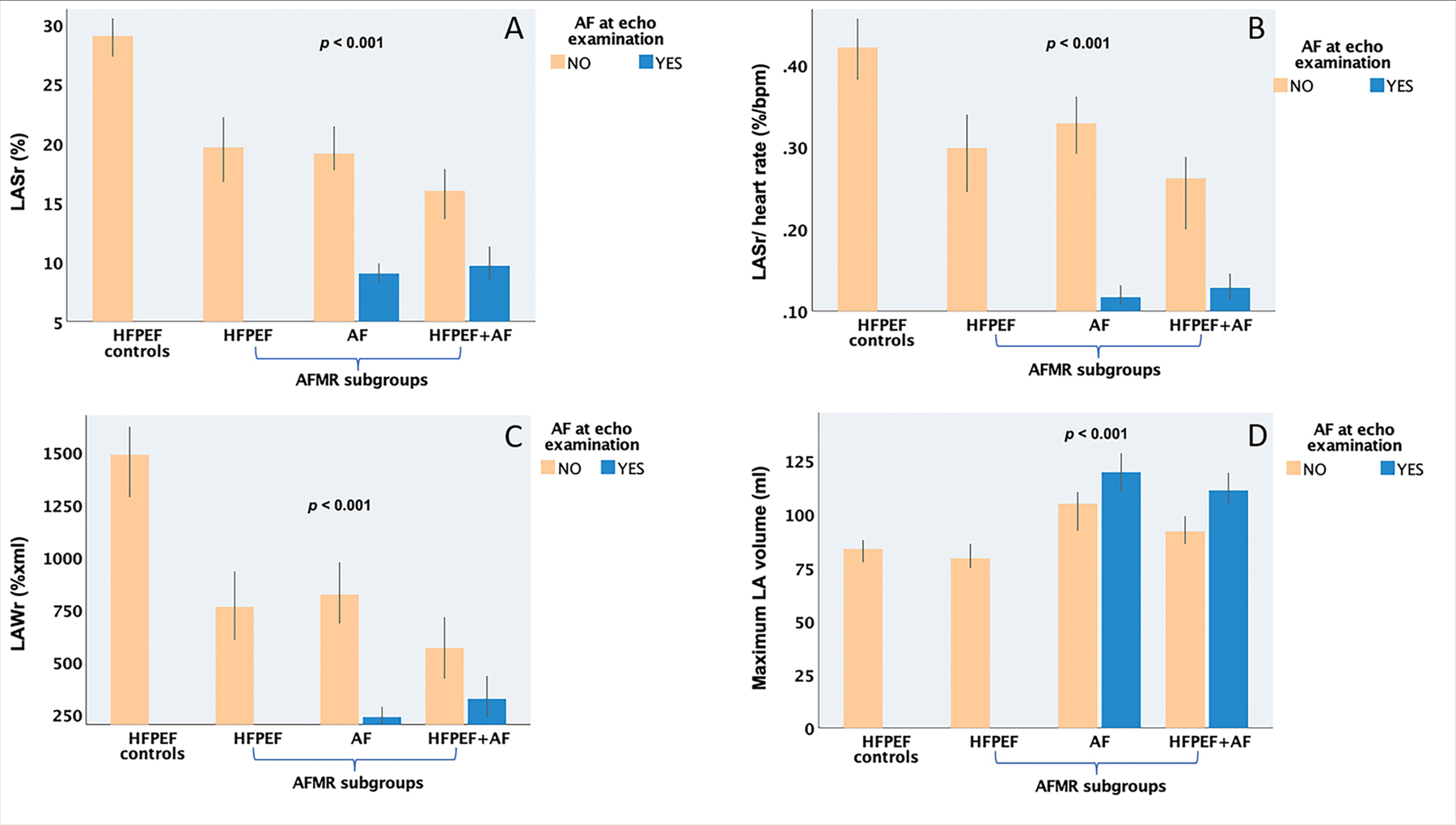
Panel A) LASr. Panel B) LASr normalized for heart rate. Panel C) LAWr. Panel D) LAVmax. P value for comparison between groups by one-way ANOVA with Sidaks′ posthoc test.
AF = atrial fibrillation; HFpEF = heart failure with preserved ejection fraction; LASr = left atrial reservoir strain; LAVmax = maximum left atrial volume; LAWr = left atrial reservoir work.
To assess the contribution of AFMR to atrial remodeling, the AFMR patients were compared to a contemporary cohort of HFpEF subjects with similar sex and age distribution, but with no or only trace MR. LAVmax was comparable between patients with HFpEF with and without MR, but subjects with HFpEF and no MR had smaller LAVmin, larger reservoir volume, and significantly higher LA function by either LASr, LAWr, LA emptying fraction and expansion index (Table 3, Figure 2).
Impact of atrial function on outcomes:
During the median follow-up of 5 [1–17] years, the AFMR patients experienced a high number of adverse events, including 197 (38%) deaths and 153 (30%) first time HF hospitalizations. Only 14 patients (2.7%) underwent mitral valve surgery. The AF group has lower mortality (24%) and hospitalizations for HF symptoms (20%), while adverse events were most common in the HFpEF+AF group with 49% mortality and 33% first-time HF hospitalizations during the study period (p<0.001).
Of all the atrial functional indexes, LAWr followed by LASr had the strongest association with all-cause death (Figure 3). When the whole patient population was grouped according to the median value of either LASr or LAWr, low atrial function by either parameter was strongly associated with higher risk of death over time (Figure 4) and with a higher probability of HF hospitalization (Figure 5).
Figure 3. Receiver Operating characteristic (ROC) analysis showing the strength of the univariable relationship between different indexes of LA reservoir function (LAWr, LASr, LA emptying fraction and LA expansion index) and all-cause death.
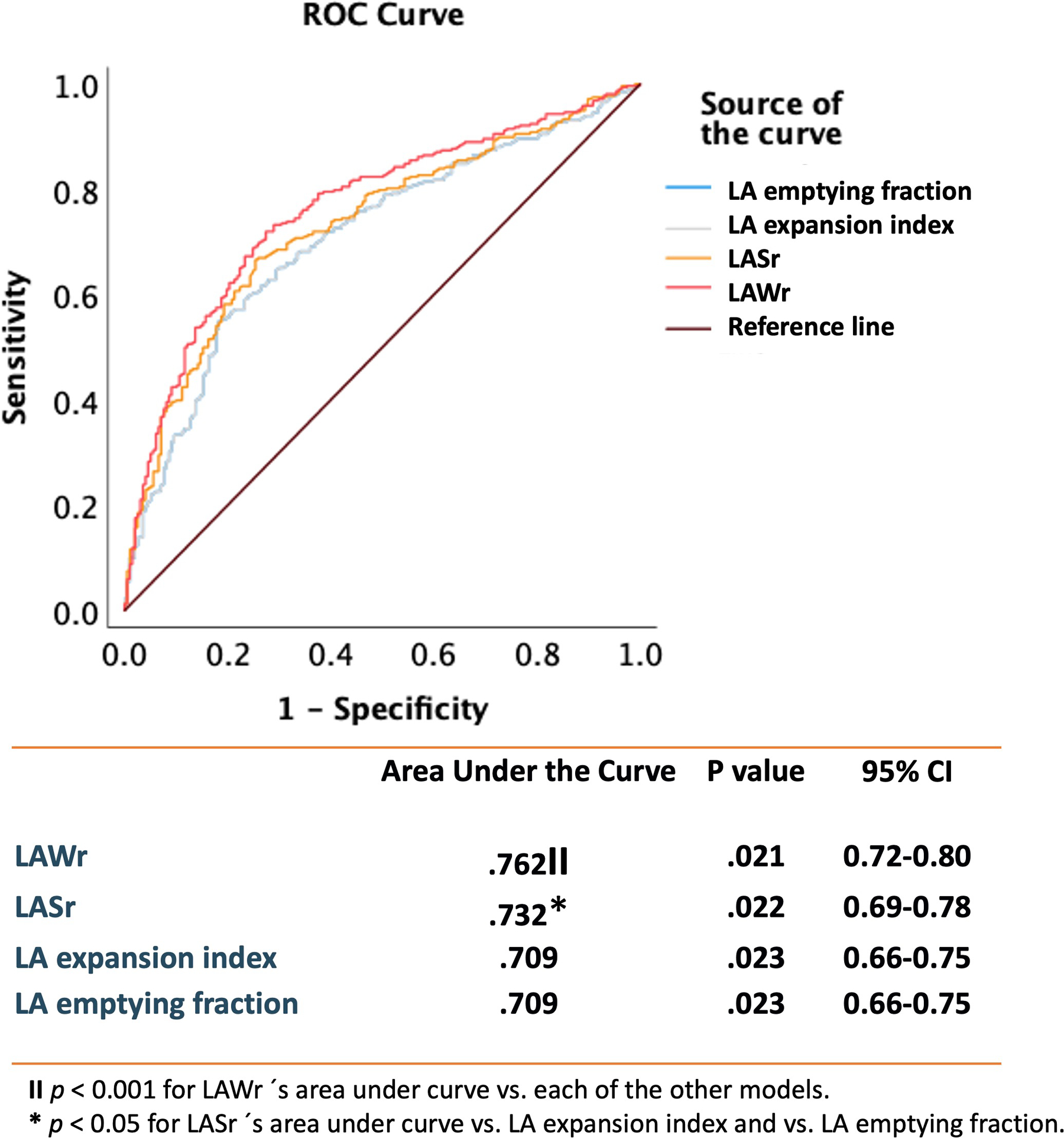
The table shows the areas under the curve (column 2) with the p value for the association between each index of LA reservoir function and all-cause death (column 3) and the 95% Confidence Intervals (column 4). Additionally, the p values for the comparison between the areas under the curve of the four indexes of LA reservoir function are indicated by the symbols || and *.
|| p < 0.001 for LAWr s′ area under curve vs. each of the other models.
* p < 0.05 for LASr s′ area under curve vs. LA expansion index and vs. LA emptying fraction.
LA = left atrial; LASr = left atrial reservoir strain; LAWr = left atrial reservoir work; ROC = Receiver Operating characteristic.
Figure 4. Kaplan-Meier curves for time to all-cause death.
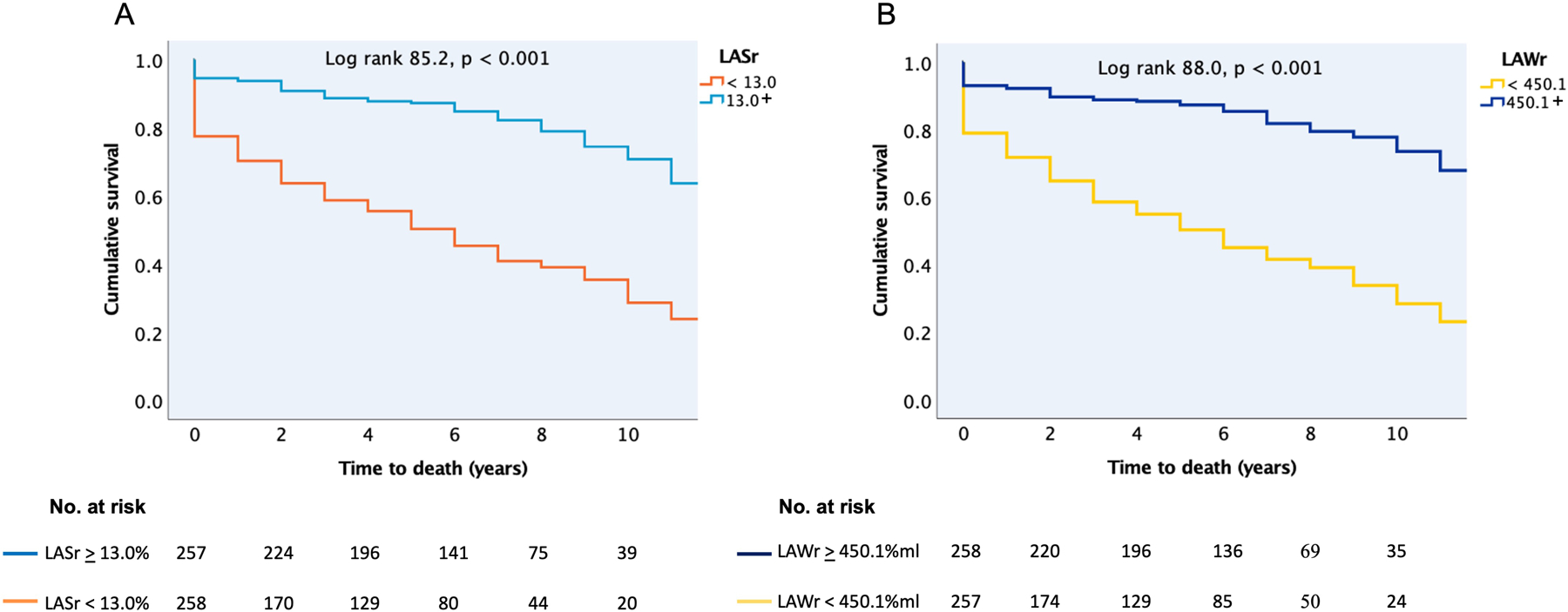
Panel A) In patients with LASr < or ≥ the median value of 13.0%. Panel B) In patients with LAWr < or ≥ the median value of 450.1 %xml. The value of the log rank test is given for the overall analysis with the respective p value.
ASr = left atrial reservoir strain; LAWr = left atrial reservoir work.
Figure 5. Kaplan-Meier curves for time to first HF hospitalization after inclusion in the study.
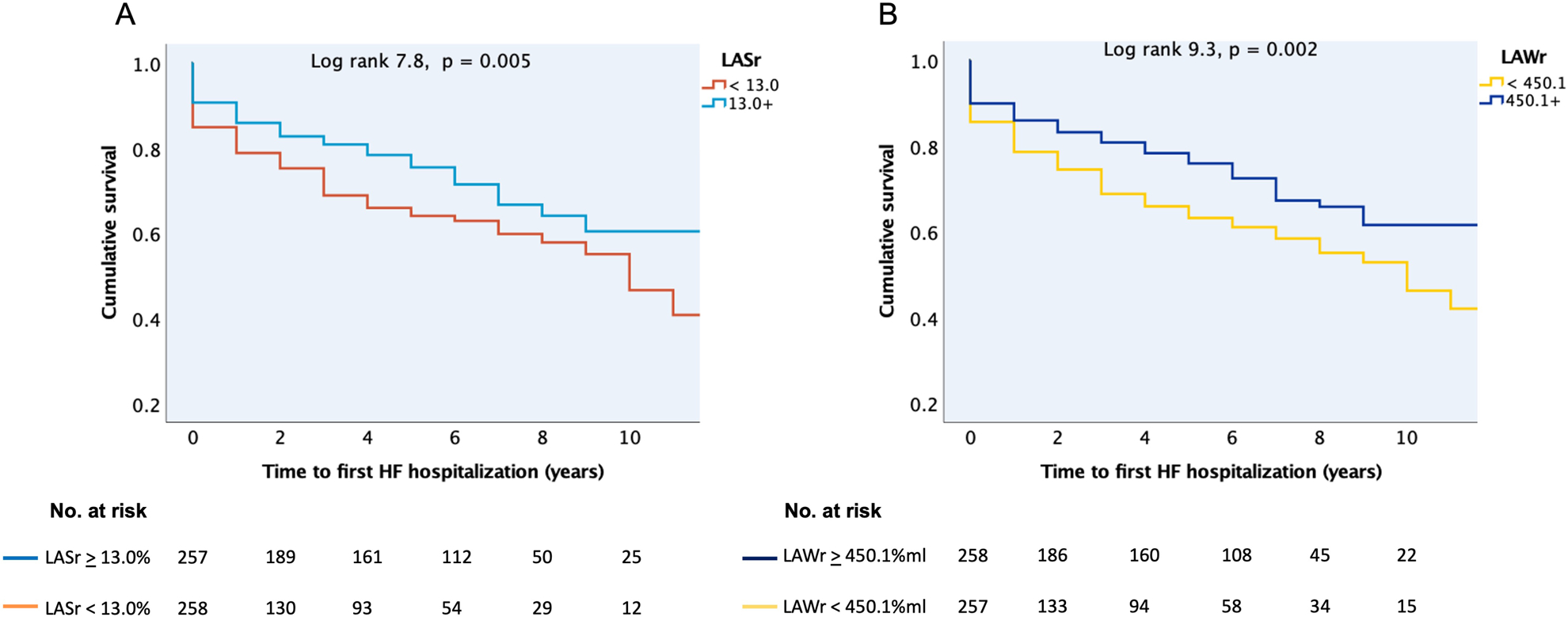
Panel A) In patients with LASr < or ≥ the median value of 13.0%. Panel B) In patients with LAWr < or ≥ the median value of 450.1 %xml. The value of the log rank test is given for the overall analysis with the respective p value.
HF = heart failure; LASr = left atrial reservoir strain; LAWr = left atrial reservoir work.
In univariable Cox regression analyses, low LAWr and low LASr predicted a 4.1- and 3.9-fold higher risk of all-cause death (Table 4). In subgroup analyses, low LAWr and low LASr were strongest associated with death in the HFpEF+AF group (Table 5). Concentric LV geometry and lower LA reservoir volume, as well as higher age, chronic obstructive pulmonary disease, chronic kidney disease, peripheral vascular disease, HF treatment, or being in the HFpEF+AF subgroup predicted also higher risk of death. Importantly, neither LV function nor LAVmax were associated with outcome in patients with significant AFMR. Having AF at index examination did not predict outcome. After adjustment for these confounders in multivariable models, LAWr below the median value of 450.1%xml remained the strongest independent predictor caring a 3.4-fold higher risk of death. LARs under the median value of 13% translated into an independent 2.3-fold higher risk of all-cause death (Table 4). When LAVmax was forced into the multivariable models, the results remained unchanged.
Table 4.
Predictors of all-cause death in patients with moderate and greater AFMR. In the multivariable model, either LASr<13.0% and LA reservoir volume (model 1) or LAWr<450.1 % x ml (model 2), in combination with the other variables, were used.
| Univariable analyses | Multivariable analyses | |||||
| Model 1 | Model 2 | |||||
| Variable | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | P |
| Low LASr (<13%) | 3.88 (2.81–5.35) | <0.001 | 2.32 (1.55–3.46) | <0.001 | - | - |
| Low LAWr (<450.1 %xml) | 4.06 (2.92–5.66) | <0.001 | 3.42 (2.41–4.85) | <0.001 | ||
| Age, years | 1.04 (1.03–1.05) | <0.001 | 1.02 (1.00–1.03) | 0.04 | 1.02 (1.00–1.03) | 0.02 |
| Female sex | 1.24 (0.94–1.64) | 0.14 | ||||
| Heart rate, bpm | 1.01 (1.00–1.01) | 0.11 | ||||
| Obesity | 0.91 (0.66–1.26) | 0.59 | ||||
| COPD | 2.20 (1.57–3.07) | <0.001 | 1.36 (0.95–1.93) | 0.09 | 1.50 (1.06–2.13) | 0.02 |
| AF at examination | 1.22 (0.92–1.62) | 0.16 | ||||
| HFpEF+AF subgroup | 1.81 (1.37–2.40) | <0.001 | 1.42 (1.04–1.93) | 0.03 | 1.33 (0.99–1.81) | 0.06 |
| Hypertension | 1.36 (0.90–2.06) | 0.14 | ||||
| Hypercholesterolemia | 0.83 (0.62–1.11) | 0.22 | ||||
| Diabetes mellitus | 1.21 (0.90–1.63) | 0.20 | ||||
| Chronic kidney disease | 2.32 (1.71–3.15) | <0.001 | 2.20 (1.59–3.03) | <0.001 | 2.20 (1.60–3.03) | <0.001 |
| Peripheral vascular disease | 1.65 (1.14–2.39) | 0.008 | 1.08 (0.73–1.58) | 0.71 | 1.09 (0.74–1.59) | 0.67 |
| Diuretic | 3.22 (2.36–4.39) | <0.001 | 2.76 (1.91–3.99) | <0.001 | 2.59 (1.80–3.73) | <0.001 |
| ACE inhibitor or ARB | 1.51 (1.14–2.02) | 0.005 | 0.80 (0.58–1.10) | 0.17 | 0.81 (0.59–1.11) | 0.19 |
| Beta-blocker | 1.88 (1.36–2.59) | <0.001 | 1.16 (0.81–1.67) | 0.41 | 1.18 (0.83–1.69) | 0.36 |
| LV concentric geometry | 1.36 (1.02–1.82) | 0.04 | 1.03 (0.76–1.38) | 0.87 | 1.04 (0.77–1.40) | 0.82 |
| LV EF, % | 0.99 (0.98–1.02) | 0.95 | ||||
| LV GLS, % | 1.02 (0.99–1.06) | 0.26 | ||||
| LAVmax, ml | 1.00 (0.99–1.00) | 0.20 | ||||
| LA reservoir volume, ml | 0.96 (0.95–0.97) | <0.001 | 0.98 (0.96–0.99) | <0.001 | - | - |
ACE = angiotensin-converting enzyme; AF = atrial fibrillation; ARB = angiotensin receptor blocker; COPD = chronic obstructive pulmonary disease; EF = ejection fraction; GLS = global longitudinal strain; HFpEF = heart failure with preserved ejection fraction; HR = hazard ratio; LA = left atrial; LASr = left atrial reservoir strain; LAVmax = maximum left atrial volume; LAWr = left atrial reservoir work; LV = left ventricular.
Table 5.
Univariable Cox analyses of the association between low LASr and low LAWr and all-cause death in subgroups of patients with significant AFMR. Low LASr and low LAWr are defined as values below the median of 13.0% and 450.1 % x ml, respectively.
| HFpEF (n=124) | AF (n=193) | HFpEF+AF (n=198) | ||||
| Variable | HR (95% CI) | P | HR (95% CI) | P | HR (95% CI) | P |
| Low LASr (<13%) | 6.63 (3.77–11.66) | <0.001 | 1.65 (0.89–3.07) | 0.11 | 9.39 (5.19–16.98) | <0.001 |
| Low LAWr (<450.1 %xml) | 5.46 (3.17–9.42) | <0.001 | 1.98 (1.04–3.77) | 0.04 | 9.74 (5.18–18.30) | <0.001 |
AF = atrial fibrillation; HFpEF = heart failure with preserved ejection fraction; HR = hazard ratio; LASr = left atrial reservoir strain; LAWr = left atrial reservoir work.
Discussion
In a large cohort of patients with moderate and greater AFMR, we found that AFMR is associated with either AF alone, or HFpEF with or without AF. We demonstrate that these commonly AFMR-linked pathologies are associated with partially different patterns of LA remodeling, with more severely dilated atria with higher storage capacity in AFMR patients with AF alone, and smaller, stiffer atria in HFpEF. LA function assessed by LASr or LAWr -a simplified index of the passive LA work in the reservoir phase- had a strong impact on patients′ mortality risk after correction for multiple confounders and was a particularly powerful predictor of death in the HFpEF groups. On the contrary, LAVmax, a guideline recommended criterion for grading and considering intervention in chronic MR, had no impact on outcome in patients with significant AFMR. Finally, LAVmax did not distinguish between HFpEF subjects with or without AFMR, in contrast to atrial function which was significantly lower in the presence of AFMR.
AFMR clinical presentation:
Functional MR in patients with normal LV size and EF but dilated LA has received increased clinical attention during the last years due to its escalating prevalence and recognition. AFMR commonly occurs in patients with a history of AF 1, 25. Recent AHA/ACC and ESC/EACTS guidelines for the management of valvular heart disease describe AFMR as a MR subtype associated with longstanding AF and attribute its etiology to atrial annular dilatation 4, 5. However, AFMR has also been described previously in HFpEF patients albeit in a limited number of studies and mostly in patients with mild MR 6, 26. In the present cohort, we show that HFpEF is highly associated with AFMR being present in 63% of our patients. Interestingly, LA was rarely severely dilated in the AFMR patients with HFpEF but no history of AF (11% of this group), implying that annular dilation is not the sole mechanisms behind significant MR in this clinical setting.
Phenotypes of atrial remodeling in AFMR:
AF and HFpEF increase in prevalence with age, have similar risk factors and clinical features, and are physiopathologically linked in complex and still incompletely understood ways 27. In 285 HFpEF patients, Reddy et al described a continuum of disease with increasing AF burden, from none to paroxysmal and then permanent, in parallel with increasing LA myopathy assessed by LASr or LA compliance 28. In contrast, in AFMR, we did not see a continuum pattern with development of AF signaling an end stage process, but rather distinct phenotypes with important mechanistic insights about the interplay between atrial function and atrial structural remodeling. The AF alone patients had larger LA reservoir volumes suggesting more compliant atria with higher storage reserves and hence greater accommodation of the AFMR-related LA volume overload. In contrast, the HFpEF alone patients had lower LA reservoir volumes suggesting smaller, stiffer atria 29. This was associated with higher estimated pulmonary pressures as well as worse outcomes, denoting the adverse prognostic impact of a noncompliant LA. By cardiac MRI, myocardial fibrosis has previously been shown to be common in HFpEF patients 30, but its distribution in the cardiac chambers has been less characterized. Our findings suggest that HFpEF patients that develop significant AFMR might be a HFpEF subgroup with excessive fibrosis of the LA 29. This requires however further elucidation by histopathological and imaging studies.
Atrial mechanical function was significantly lower in our AFMR patients than in previously published healthy individuals of similar age 31. Additionally, in HFpEF patients without AF, atrial function was lower in those with AFMR than in those without MR from our control group, consistent with previously described cohorts 2.
Of note, assessment of both LA and LV strain was significantly influenced by presence of AF, with impaired LV GLS in patients in AF compared to normal values in those in sinus rhythm at the index examination, and concomitantly severely impaired LASr and LAWr. AF causes both loss of atrial contraction and atrial relaxation, and LA function should ideally be assessed in sinus rhythm in patients with still paroxysmal AF, and otherwise reported separately for patients in different types of cardiac rhythms at echocardiography.
Atrial dysfunction and outcome in AFMR:
Reduced atrial deformation in the reservoir phase has recently been identified as a predictor of worse outcome in HF patients 32, including patients with HFpEF 2, as well as in patients with primary MR referred to mitral valve repair 33, 34 and patients with secondary MR of ventricular cause 35.
Atrial function has not been previously characterized in relation to outcome in AFMR of more than mild degree. This study examined a large AFMR cohort with a high number of adverse events during long-term follow-up, including a 38% mortality. This confirms previous findings of comparable excess mortality in patients with primary MR and AFMR 3. We additionally found that reduced LASr was a predictor of both all-cause death and higher risk of HF hospitalization in patients with AFMR. Moreover, combining LASr and LA reservoir volume in LAWr improved both prediction of death, and the distinction between the AFMR phenotypes. As such, low LAWr in AFMR was strongly related to worse survival in patients with HFpEF, highlighting the important negative prognostic impact of LA noncompliance.
Of note, LASr and LAWr performed better in risk prediction analyses than other previously proposed markers of LA function, including the LA expansion index 16.
Neither maximum LA size nor LV function as assessed by LVEF and GLS had an impact on prognosis in our study population. This challenges the common belief that LA enlargement is both the cause and the determinant of outcome in AFMR patients 4, 36, 37.
Clinical implications:
AFMR has been etiologically attributed to atrial and annular dilation, with later studies also demonstrating an additional role of incomplete leaflet remodelling and atriogenic posterior leaflet tethering 25, 38–40. The role of abnormal atrial mechanical function has not been previously examined. Our study included patients with established moderate or greater AFMR so we could not address the initial cause of the regurgitation. However, in significant AFMR, it is noteworthy that LA dilation, assessed as maximum LA volume at end-systole, had no impact on prognosis, and that only 37% of the whole cohort had severely dilated LA by standard criteria. Moreover, LAVmax was comparable between HFpEF patients with AFMR and HFpEF controls without MR. So, even if LA and annular dilation might be the kick-off of AFMR, its progression and prognosis are more closely related to atrial dysfunction.
While our data points to the important prognostic impact of low LA function in AFMR, it does not exclude that treating AFMR per se might improve outcomes. Strategies addressing both AFMR, rhythm control and LA dysfunction such as an atrial shunt device can be considered 41. In our study, common medications which are recommended for HF with reduced EF such as angiotensin receptor blockers, angiotensin-converting enzyme inhibitors and beta-blockers, did not have independent prognostic value in AFMR, while use of diuretics more than doubled the risk of death, perhaps reflecting, at least partially, their use in more advanced HF stages. This might suggest that optimal medical treatment for patients with HF with reduced EF, with demonstrated value in secondary MR of ventricular cause 42, 43, does not have the same advantages in AFMR. Catheter AF ablation has previously been shown to reduce LA size and AFMR severity in selected AF patients 37. However, ablations can increase LA stiffness through scar formation 44, and one should probably be particularly careful in using this therapeutic strategy in patients with concomitant AF and HFpEF that have, as our data show, limited atrial expansibility and severe LA dysfunction.
Studies on the relative contribution of atrial dysfunction versus increasing MR volume to symptoms during exercise are lacking in AFMR patients. Exercise testing may unmask stiff LAs or worsening MR in symptomatic AFMR patients.
Study limitations:
The present study is a retrospective follow-up of patients with significant AFMR and has the limitations inherent to this study design. However, it is the largest AFMR cohort characterized clinically and echocardiographically up to this date, and our findings contribute to better understanding of an increasingly prevalent MR subtype. Data on AFMRs effective regurgitant orifice area and regurgitation volume were not available for the present analyses; however, the vast majority of the patients (97%) had moderate AFMR based on a comprehensive evaluation done by experienced echo-cardiologists. History of AF was based on review of all previous electrocardiograms and clinical charts, so one cannot exclude that some HFpEF patients might have had an undocumented AF episode. However, this would only reduce the observed differences between the AFMR phenotypes (bias toward the null). Similarly, even if none of our AF patients had previous HF hospitalizations and this subgroup had significantly less dyspnea and use of diuretics, some of the AF patients might have had earlier stages of HFpEF 27. However, this would again only bias our results towards the null. Contemporary controls with AFMR and no MR were not followed-up for the same duration of time as AFMR patients. The control group was though only selected for comparison of atrial remodeling between HFpEF with and without AFMR, as LA function in relation to outcome has been previously reported in HFpEF patients with no significant MR 2, 28. Finally, LAWr requires further validation in both experimental and clinical settings.
Conclusions:
AFMR develops in patients with AF and/or HFpEF in whom it is associated with partially different LA remodeling patterns. LA mechanics does not parallel changes in LA size and is severely impaired in significant AFMR, and particularly in patients with a history of HFpEF in whom it is a strong predictor of death. Neither maximum LA size nor LV function are significant prognosticators in AFMR. The outcome of patients with AFMR is related to the degree of LA reservoir dysfunction independent of comorbidities and medical treatment.
Clinical Perspective.
In a large cohort of patients with moderate and greater atrial functional mitral regurgitation (AFMR), we found that AFMR is commonly associated with heart failure with preserved ejection fraction and/or atrial fibrillation. Depending on the linked pathology, we identified distinct patterns of left atrial remodeling in AFMR, with more severely dilated atria with higher storage capacity in patients with atrial fibrillation, and smaller, noncompliant atria in heart failure with preserved ejection fraction. Patients with significant AFMR experienced a high number of adverse events, including a 38% mortality and 30% first time heart failure hospitalizations during a 5-year follow-up. Impaired left atrial function assessed by either the reservoir strain or the product of reservoir strain x left atrial reservoir volume (a simplified index of left atrial reservoir work) was a strong predictor of death in AFMR, particularly in the setting of heart failure with preserved ejection fraction. The maximum left atrial volume, a guideline recommended criterion for grading and considering intervention in chronic mitral regurgitation, was not related to outcome in significant AFMR. The current findings support future investigations to evaluate different treatment strategies addressing both the mitral regurgitation and the left atrial dysfunction in AFMR.
Funding:
Dana Cramariuc received open project support from Helse Vest (project number F-12615) during the conduct of this study. Antonia van Kampen has been awarded the American Heart Association Postdoctoral Fellowship Award. Judy Hung was supported in part by NIH/NHLBI 2 RO1HL103723-05. Judy Hung is also the PI of an Institutional Research grant for core lab adjudication from Edwards Lifesciences.
Abbreviations:
- AF
atrial fibrillation
- AFMR
atrial functional mitral regurgitation
- BSA
body surface area
- EF
ejection fraction
- GLS
global left ventricular longitudinal strain
- HF
heart failure
- HFpEF
heart failure with preserved ejection fraction
- LA
left atrium
- LASr
left atrial reservoir strain
- LAWr
left atrial reservoir work
- LAVmax
maximum left atrial volume
- LAVmin
minimum left atrial volume
- LV
left ventricle
- MR
mitral regurgitation
Footnotes
Disclosures: The authors have no disclosures related to the present study.
Reference list
- 1.Muraru D, Guta AC, Ochoa-Jimenez RC, Bartos D, Aruta P, Mihaila S, Popescu BA, Iliceto S, Basso C and Badano LP. Functional Regurgitation of Atrioventricular Valves and Atrial Fibrillation: An Elusive Pathophysiological Link Deserving Further Attention. J Am Soc Echocardiogr 2020;33:42–53. [DOI] [PubMed] [Google Scholar]
- 2.Tamargo M, Obokata M, Reddy YNV, Pislaru SV, Lin G, Egbe AC, Nishimura RA and Borlaug BA. Functional mitral regurgitation and left atrial myopathy in heart failure with preserved ejection fraction. Eur J Heart Fail 2020;22:489–498. [DOI] [PubMed] [Google Scholar]
- 3.Dziadzko V, Dziadzko M, Medina-Inojosa JR, Benfari G, Michelena HI, Crestanello JA, Maalouf J, Thapa P and Enriquez-Sarano M. Causes and mechanisms of isolated mitral regurgitation in the community: clinical context and outcome. Eur Heart J 2019;40:2194–2202. [DOI] [PubMed] [Google Scholar]
- 4.Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2022;43:561–632. [DOI] [PubMed] [Google Scholar]
- 5.Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021;143:e72–e227. [DOI] [PubMed] [Google Scholar]
- 6.Deferm S, Bertrand PB, Verbrugge FH, Verhaert D, Rega F, Thomas JD and Vandervoort PM. Atrial Functional Mitral Regurgitation: JACC Review Topic of the Week. J Am Coll Cardiol 2019;73:2465–2476. [DOI] [PubMed] [Google Scholar]
- 7.Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, Han Y, Hung J, Lang RM, et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 2017;30:303–371. [DOI] [PubMed] [Google Scholar]
- 8.Thomas L, Muraru D, Popescu BA, Sitges M, Rosca M, Pedrizzetti G, Henein MY, Donal E and Badano LP. Evaluation of Left Atrial Size and Function: Relevance for Clinical Practice. J Am Soc Echocardiogr 2020;33:934–952. [DOI] [PubMed] [Google Scholar]
- 9.Badano LP, Kolias TJ, Muraru D, Abraham TP, Aurigemma G, Edvardsen T, D'Hooge J, Donal E, Fraser AG, Marwick T, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 2018;19:591–600. [DOI] [PubMed] [Google Scholar]
- 10.Cameli M, Sparla S, Losito M, Righini FM, Menci D, Lisi M, D'Ascenzi F, Focardi M, Favilli R, Pierli C, et al. Correlation of Left Atrial Strain and Doppler Measurements with Invasive Measurement of Left Ventricular End-Diastolic Pressure in Patients Stratified for Different Values of Ejection Fraction. Echocardiography 2016;33:398–405. [DOI] [PubMed] [Google Scholar]
- 11.Inoue K, Khan FH, Remme EW, Ohte N, Garcia-Izquierdo E, Chetrit M, Monivas-Palomero V, Mingo-Santos S, Andersen OS, Gude E, et al. Determinants of left atrial reservoir and pump strain and use of atrial strain for evaluation of left ventricular filling pressure. Eur Heart J Cardiovasc Imaging 2021;23:61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Popescu BA, Beladan CC, Nagueh SF and Smiseth OA. How to assess left ventricular filling pressures by echocardiography in clinical practice. Eur Heart J Cardiovasc Imaging 2022;23:1127–1129. [DOI] [PubMed] [Google Scholar]
- 13.Dermlim A, Osuga T, Nakamura K, Morita T, Nisa K, Sasaoka K, Leela-Arporn R, Nagata N, Tamura M, Sasaki N, et al. Effect of acute volume loading on left atrial strain values derived from two-dimensional speckle tracking echocardiography in dogs. J Vet Med Sci 2019;81:949–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inoue K, Kawakami H, Akazawa Y, Higashi H, Higaki T and Yamaguchi O. Echocardiographic Assessment of Atrial Function: From Basic Mechanics to Specific Cardiac Diseases. J Cardiovasc Dev Dis 2022;9:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sonnenblick EH. Force-velocity relations in mammalian heart muscle. Am J Physiol 1962;202:931–9. [DOI] [PubMed] [Google Scholar]
- 16.Genovese D, Muraru D, Marra MP, Carrer A, Previtero M, Palermo C, Tarantini G, Parati G, Iliceto S and Badano LP. Left Atrial Expansion Index for Noninvasive Estimation of Pulmonary Capillary Wedge Pressure: A Cardiac Catheterization Validation Study. J Am Soc Echocardiogr 2021;34:1242–1252. [DOI] [PubMed] [Google Scholar]
- 17.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277–314. [DOI] [PubMed] [Google Scholar]
- 18.Smiseth OA, Morris DA, Cardim N, Cikes M, Delgado V, Donal E, Flachskampf FA, Galderisi M, Gerber BL, Gimelli A, et al. Multimodality imaging in patients with heart failure and preserved ejection fraction: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2022;23:e34–e61. [DOI] [PubMed] [Google Scholar]
- 19.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1–39 e14. [DOI] [PubMed] [Google Scholar]
- 20.de Simone G, Izzo R, Chinali M, De Marco M, Casalnuovo G, Rozza F, Girfoglio D, Iovino GL, Trimarco B and De Luca N. Does information on systolic and diastolic function improve prediction of a cardiovascular event by left ventricular hypertrophy in arterial hypertension? Hypertension 2010;56:99–104. [DOI] [PubMed] [Google Scholar]
- 21.Grymyr LMD, Nadirpour S, Gerdts E, Nedrebo BG, Hjertaas JJ, Matre K and Cramariuc D. Left ventricular myocardial oxygen demand and subclinical dysfunction in patients with severe obesity referred for bariatric surgery. Nutr Metab Cardiovasc Dis 2021;31:666–674. [DOI] [PubMed] [Google Scholar]
- 22.Grymyr LMD, Nadirpour S, Gerdts E, Nedrebo BG, Hjertaas JJ, Matre K and Cramariuc D. One-year impact of bariatric surgery on left ventricular mechanics: results from the prospective FatWest study. Eur Heart J Open 2021;1:oeab024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015;16:233–70. [DOI] [PubMed] [Google Scholar]
- 24.Sugimoto T, Dulgheru R, Bernard A, Ilardi F, Contu L, Addetia K, Caballero L, Akhaladze N, Athanassopoulos GD, Barone D, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging 2017;18:833–840. [DOI] [PubMed] [Google Scholar]
- 25.Kagiyama N, Mondillo S, Yoshida K, Mandoli GE and Cameli M. Subtypes of Atrial Functional Mitral Regurgitation: Imaging Insights Into Their Mechanisms and Therapeutic Implications. JACC Cardiovasc Imaging 2020;13:820–835. [DOI] [PubMed] [Google Scholar]
- 26.Ennezat PV, Marechaux S, Pibarot P and Le Jemtel TH. Secondary mitral regurgitation in heart failure with reduced or preserved left ventricular ejection fraction. Cardiology 2013;125:110–7. [DOI] [PubMed] [Google Scholar]
- 27.Kotecha D, Lam CS, Van Veldhuisen DJ, Van Gelder IC, Voors AA and Rienstra M. Heart Failure With Preserved Ejection Fraction and Atrial Fibrillation: Vicious Twins. J Am Coll Cardiol 2016;68:2217–2228. [DOI] [PubMed] [Google Scholar]
- 28.Reddy YNV, Obokata M, Verbrugge FH, Lin G and Borlaug BA. Atrial Dysfunction in Patients With Heart Failure With Preserved Ejection Fraction and Atrial Fibrillation. J Am Coll Cardiol 2020;76:1051–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cameli M, Lisi M, Righini FM, Massoni A, Natali BM, Focardi M, Tacchini D, Geyer A, Curci V, Di Tommaso C, et al. Usefulness of atrial deformation analysis to predict left atrial fibrosis and endocardial thickness in patients undergoing mitral valve operations for severe mitral regurgitation secondary to mitral valve prolapse. Am J Cardiol 2013;111:595–601. [DOI] [PubMed] [Google Scholar]
- 30.Sweeney M, Corden B and Cook SA. Targeting cardiac fibrosis in heart failure with preserved ejection fraction: mirage or miracle? EMBO Mol Med 2020;12:e10865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nielsen AB, Skaarup KG, Hauser R, Johansen ND, Lassen MCH, Jensen GB, Schnohr P, Mogelvang R and Biering-Sorensen T. Normal values and reference ranges for left atrial strain by speckle-tracking echocardiography: the Copenhagen City Heart Study. Eur Heart J Cardiovasc Imaging 2021;23:42–51. [DOI] [PubMed] [Google Scholar]
- 32.Bouwmeester S, van der Stam JA, van Loon SLM, van Riel NAW, Boer AK, Dekker LR, Scharnhorst V and Houthuizen P. Left atrial reservoir strain as a predictor of cardiac outcome in patients with heart failure: the HaFaC cohort study. BMC Cardiovasc Disord 2022;22:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stassen J, van Wijngaarden AL, Butcher SC, Palmen M, Herbots L, Bax JJ, Delgado V and Ajmone Marsan N. Prognostic value of left atrial reservoir function in patients with severe primary mitral regurgitation undergoing mitral valve repair. Eur Heart J Cardiovasc Imaging 2022;19;24:142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Debonnaire P, Leong DP, Witkowski TG, Al Amri I, Joyce E, Katsanos S, Schalij MJ, Bax JJ, Delgado V and Marsan NA. Left atrial function by two-dimensional speckle-tracking echocardiography in patients with severe organic mitral regurgitation: association with guidelines-based surgical indication and postoperative (long-term) survival. J Am Soc Echocardiogr 2013;26:1053–62. [DOI] [PubMed] [Google Scholar]
- 35.Stassen J, Namazi F, van der Bijl P, van Wijngaarden SE, Kamperidis V, Marsan NA, Delgado V and Bax JJ. Left Atrial Reservoir Function and Outcomes in Secondary Mitral Regurgitation. J Am Soc Echocardiogr 2022;35:477–485 e3. [DOI] [PubMed] [Google Scholar]
- 36.Gertz ZM, Raina A, Mountantonakis SE, Zado ES, Callans DJ, Marchlinski FE, Keane MG and Silvestry FE. The impact of mitral regurgitation on patients undergoing catheter ablation of atrial fibrillation. Europace 2011;13:1127–32. [DOI] [PubMed] [Google Scholar]
- 37.Gertz ZM, Raina A, Saghy L, Zado ES, Callans DJ, Marchlinski FE, Keane MG and Silvestry FE. Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control. J Am Coll Cardiol 2011;58:1474–81. [DOI] [PubMed] [Google Scholar]
- 38.Dal-Bianco JP, Aikawa E, Bischoff J, Guerrero JL, Handschumacher MD, Sullivan S, Johnson B, Titus JS, Iwamoto Y, Wylie-Sears J, et al. Active adaptation of the tethered mitral valve: insights into a compensatory mechanism for functional mitral regurgitation. Circulation 2009;120:334–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silbiger JJ. Does left atrial enlargement contribute to mitral leaflet tethering in patients with functional mitral regurgitation? Proposed role of atriogenic leaflet tethering. Echocardiography 2014;31:1310–1. [DOI] [PubMed] [Google Scholar]
- 40.Mesi O, Gad MM, Crane AD, Ramchand J, Puri R, Layoun H, Miyasaka R, Gillinov MA, Wierup P, Griffin BP, et al. Severe Atrial Functional Mitral Regurgitation: Clinical and Echocardiographic Characteristics, Management and Outcomes. JACC Cardiovasc Imaging 2021;14:797–808. [DOI] [PubMed] [Google Scholar]
- 41.Shah SJ, Borlaug BA, Chung ES, Cutlip DE, Debonnaire P, Fail PS, Gao Q, Hasenfuss G, Kahwash R, Kaye DM, et al. Atrial shunt device for heart failure with preserved and mildly reduced ejection fraction (REDUCE LAP-HF II): a randomised, multicentre, blinded, sham-controlled trial. Lancet 2022;399:1130–1140. [DOI] [PubMed] [Google Scholar]
- 42.Solomon SD, Skali H, Anavekar NS, Bourgoun M, Barvik S, Ghali JK, Warnica JW, Khrakovskaya M, Arnold JM, Schwartz Y, et al. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation 2005;111:3411–9. [DOI] [PubMed] [Google Scholar]
- 43.Kang DH, Park SJ, Shin SH, Hong GR, Lee S, Kim MS, Yun SC, Song JM, Park SW and Kim JJ. Angiotensin Receptor Neprilysin Inhibitor for Functional Mitral Regurgitation. Circulation 2019;139:1354–1365. [DOI] [PubMed] [Google Scholar]
- 44.Packer M Effect of catheter ablation on pre-existing abnormalities of left atrial systolic, diastolic, and neurohormonal functions in patients with chronic heart failure and atrial fibrillation. Eur Heart J 2019;40:1873–1879. [DOI] [PMC free article] [PubMed] [Google Scholar]


