Abstract
Objectives.
To test the hypothesis that law enforcement efforts to disrupt local drug markets by seizing opioids or stimulants are associated with increased spatiotemporal clustering of overdose events in the surrounding geographic area.
Methods.
We performed a retrospective (January 1, 2020 to December 31, 2021), population-based cohort study using administrative data from Marion County, Indiana. We compared frequency and characteristics of drug (i.e., opioids and stimulants) seizures with changes in fatal overdose, emergency medical services nonfatal overdose calls for service, and naloxone administration in the geographic area and time following the seizures.
Results.
Within 7, 14, and 21 days, opioid-related law enforcement drug seizures were significantly associated with increased spatiotemporal clustering of overdoses within radii of 100, 250, and 500 meters. For example, the observed number of fatal overdoses was two-fold higher than expected under the null distribution within 7 days and 500 meters following opioid-related seizures. To a lesser extent, stimulant-related drug seizures were associated with increased spatiotemporal clustering overdose.
Conclusions.
Supply-side enforcement interventions and drug policies should be further explored to determine whether they exacerbate an ongoing overdose epidemic and negatively affect the nation’s life expectancy.
The overdose epidemic has accounted for nearly 1 million lives lost in the United States in the past 2 decades.1 Although the majority of overdose deaths are opioid related, the type of opioid involved and corresponding mortality rates vary over time, with fentanyl presently driving the fatality count in opioid- and stimulant-involved overdose deaths alike.2,3 Emergency medical services (EMS) are typically deployed in response to overdose and poisoning calls for service, and EMS administer naloxone (an opioid antagonist) when indicated to reverse respiratory depression caused by opioids. Although there are substantial geographic and policy differences in who administers naloxone and under what circumstnaces,4 the number of EMS naloxone administrations per capita are increasingly used for public health surveillance purposes5 and to guide resource allocation.6 However, the search continues to identify factors that reliably precede overdoses to trigger and inform targeted prevention efforts.7–9 We explored law enforcement drug market disruptions as a potential factor.
People can develop a tolerance for opioids, although overdose occurs when dosage exceeds tolerance to the point of respiratory failure. Unknown opioid tolerance at relapse is a documented overdose risk factor among the recently incarcerated10,11 and those discharged from residential treatment and withdrawal management settings.12,13 Reductions in tolerance can occur after any involuntary disruption of an individual’s opioid supply, and accidentally ingesting a dose beyond one’s tolerance can be fatal. This mechanism accounts for the second wave of the overdose epidemic, when consumers shifted from pharmaceutical opioids to heroin. Heroin is a much less consistent and predictable product, increasing the dangers that come of unknown tolerance, especially overdose risk.2,14
This same mechanism has been documented as occurring in the illicit drug market following disruptions from an arrested supplier and consumers contending with new and potentially unfamiliar products.15,16 The impact of these drug market disruptions may be particularly salient for people who use opioids, who can experience painful withdrawal symptoms and diminished biological tolerance even after short periods of abstinence.13 There is also a risk for people who knowingly use stimulants but are opioid naïve and, thus, have lower opioid tolerance; they might seek a new supplier following a drug market disruption and then overdose from fentanyl-contaminated stimulants.3
We tested the hypothesis that law enforcement efforts to disrupt local drug markets through routine supply-side interdictions—as measured by police seizures of opioid- and stimulant-related substances—are associated with increased spatiotemporal clustering of fatal and nonfatal overdoses, as well as increases in EMS naloxone administration, in the area surrounding the seizure. Although the analytical methods we employed cannot establish causality, we hypothesized that the causal mechanism for an association lies in the disruption of a person’s ability to obtain a substance they can accurately dose; this is because that supply has become unavailable, resulting in their transition to an alternate supply with no knowledge of its potency or their ensuing tolerance.11,13,15 Given the potential for withdrawal and overdose because of unknown tolerance among opioid users, we hypothesized an association with EMS naloxone administration following opioid-related seizures. But with the potential for unintentional opioid consumption among stimulant users, we also explored naloxone administration associated with stimulant-related seizures.
METHODS
We performed a retrospective, 2-year, population-based study by using administrative data from Marion County, Indiana. Marion County is the largest county in the state, with a population of nearly 1 million, and is home to Indianapolis, the state capital and 15th largest city in the nation.17 We selected Marion County because it accounts for a quarter of Indiana’s overdose deaths, with a mortality rate higher than the national average, and because of the availability of point-level event information across multiple data sources that are required to test our spatiotemporal hypothesis. The 3 sources of data collected between January 1, 2020, and December 31, 2021, and used in this study included (1) property room drug seizure data from the Indianapolis Metropolitan Police Department, (2) fatal overdose data from the Marion County Coroner’s Office, and (3) nonfatal overdose calls for service and naloxone administration data from the Indianapolis Emergency Medical Services. We conducted our analyses using R version 4.2.0 (RStudio, Boston, MA).
Drug Interdiction
Information on drug seizures included the location (street address), time, date, and physical description of the substance (based largely on law enforcement observation and discernment of the substances). We removed all incidents (which are not mutually exclusive) in which a drug seizure was not disruptive (e.g., a police-controlled purchase as part of an investigation, a found substance); that took place in a geographical area not in the community (e.g., an airport or hospital, police facilities where materials are identified); or that did not meet substance criteria (i.e., seizures of substances other than opioids or stimulants or consisting of only drug paraphernalia). We removed drug seizures with unknown or missing drug incident data and then subclassified seizures as opioid related (e.g., fentanyl, heroin, morphine, prescription opioids) or stimulant related (e.g., amphetamines, cocaine, methamphetamines) based on the reported descriptions.
Per administrative property room data, each confiscated item is considered a unique event; therefore, 1 incident could have multiple items, and we included each item as an event in this study. Thus, events do not refer to the number of law enforcement interdiction events, but the number of times opioids or stimulants were logged across all interdiction events. Although information on precise quantity is limited because of the lack of confirmatory toxicological results on the seized samples, we normalized information to metric grams and used Indiana criminal codes to determine that 10.4% of all drug seizures were considered large (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Fatal and Nonfatal Overdoses
We looked at 3 overdose outcomes. We identified fatal overdoses using the death certificate and toxicology results for all accidental drug overdose events (code X40-X44 of International Classification of Diseases, 10th Revision [Geneva, Switzerland: World Health Organization; 1992]) from coroner records. Toxicology data provided information about substances detected using thresholds set by the testing agency, and we determined location from the place of injury. However, we examined fatal overdoses without subclassification by underlying substance because most were polydrug overdoses. We defined nonfatal overdoses as any event in which naloxone was administered and a chief complaint or mechanism of injury was recorded as overdose or poisoning, and we looked separately at the naloxone administration event. Although other sources provide nonfatal overdose data (e.g., emergency departments), we chose EMS events based on previous research18 and the ability to measure their spatiotemporal proximity to seizures, removing events that occurred in a hospital setting.
Statistical Analyses
In our primary analysis, we first used the Knox test statistic () to identify excess space–time clustering between police seizures of opioid- and stimulant-related drugs and drug overdose events occurring in the surrounding area over a specific interval of time. To further explore potential time order of associations we then tested for differences in space– time clustering of overdose events before versus after police drug seizures ().
Magnitudes of association.
Informed by earlier studies,19,20 we calculated the 2-sample Knox test statistic () to identify excess space–time clustering between police drug seizures (i.e., opioid related and stimulant related) and overdose (i.e., fatal overdose, nonfatal overdose, and naloxone administration), where consists of the count of overdose events within days and a radius of meters of drug seizures:
| (1) |
In equation 1, is the location (time) of drug seizure , is the location (time) of overdose event , and 1 is the indicator function. To determine excess clustering of overdose events, we compared the Knox statistic with a null hypothesis in which the 2 processes are independent, with the null distribution constructed by randomly shuffling event times of the drug seizures while keeping the locations and event times of the overdoses fixed. We used 200 realizations of reshuffled event times to quantify uncertainty in the null distribution of to disentangle the time ordering of drug seizures and overdose events with the following form, where the count of overdoses within a radius of meters and days before a seizure was subtracted from the count of overdoses within a radius of meters and days after a seizure:
| (2) |
Based on previous research,21 we examined radii of 100, 250, and 500 meters at durations of 7, 14, and 21 days, respectively, and given the total number of seizure events, we report our results in all figures, supplemental tables, and text as per 100 seizure events.
Pre–post differences.
Because overdose events can occur before and after drug seizures, we used a pre–post design to establish time order. First, we estimated a 95% confidence interval (CI) for the expected difference in overdose events under a null distribution (i.e., no association between police seizure and overdose events) of pre–post test differences (i.e., , which can be positive or negative, with a positive value of indicating more overdose events cluster after drug seizures) by resampling. We then calculated observed pre–post test differences in event rates. Observed numbers of drug overdose events per 100 police drug seizures () and pre–post test differences () that lie outside the 95% CIs estimated under the null hypothesis of no association are statistically significant.
RESULTS
Figure 1 describes how we arrived at the final sample of opioid- and stimulant-related drug seizures, and Figure 2 displays their association with overdose events (fatal and combined nonfatal events) in 6-month increments over the 24-month study period (Figure A [available as a supplement to the online version of this article at http://www.ajph.org] animates the daily patterns). There were 2110 opioid-related and 3039 stimulant-related drug seizures during the 24-month study period, representing an average of 7.0 drug seizures per day (range = 0–22). The mean for opioids and stimulants, respectively, was 2.9 and 4.2 drug seizures per day. Death data showed 1171 fatal overdoses, and EMS data showed 12 590 nonfatal overdoses, of which 51.0% (n = 6419) included naloxone administration. These data represent an average of 1.6 fatal overdoses per day (range = 0–7), 17.2 nonfatal overdoses per day (range = 4–35), and 8.8 naloxone administrations per day (range = 0–21).
FIGURE 1— Case Determination of Drug Seizure Events From Property Room Data to Determine Final Sample: Marion County, IN, 2020–2021.
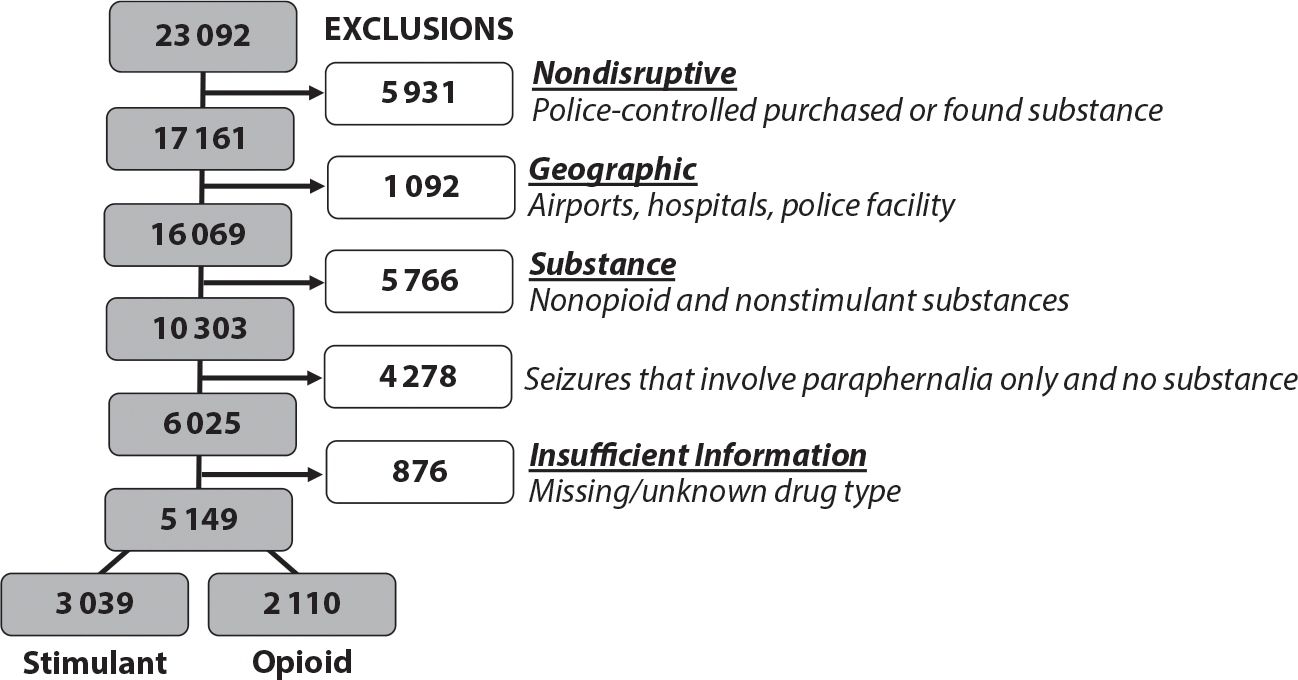
Note. Records ranged from January 1, 2020, to December 31, 2021, and included 23 092 seizure events. Nondisruptive seizures included those coded as found, stolen, or nonevidentiary, whereas geographic removals included 98 events at an airport or hospital and 944 events with the police district coded as the location. For substance exclusions, 84.1% of the 5766 substances that were not coded as opioids or stimulants were cannabis related. After these exclusion criteria, there were 14.5% (n 5 876) events without complete information on the substance or location, resulting in a final sample of 5149. Seizure events were not mutually exclusive because 244 cases were both opioid and stimulant related.
FIGURE 2— Drug Seizures (Opioid-Related and Stimulant-Related) and Overdose (Fatal Overdose, Nonfatal Overdose, and Naloxone Administration) Events Over 6-Month Increments (a) Jan 1–Jun 30, 2020, (b) Jul 1–Dec 31, 2020, (c) Jan 1–Jun 30, 2021, and (d) Jul 1–Dec 31, 2021: Indianapolis, IN.
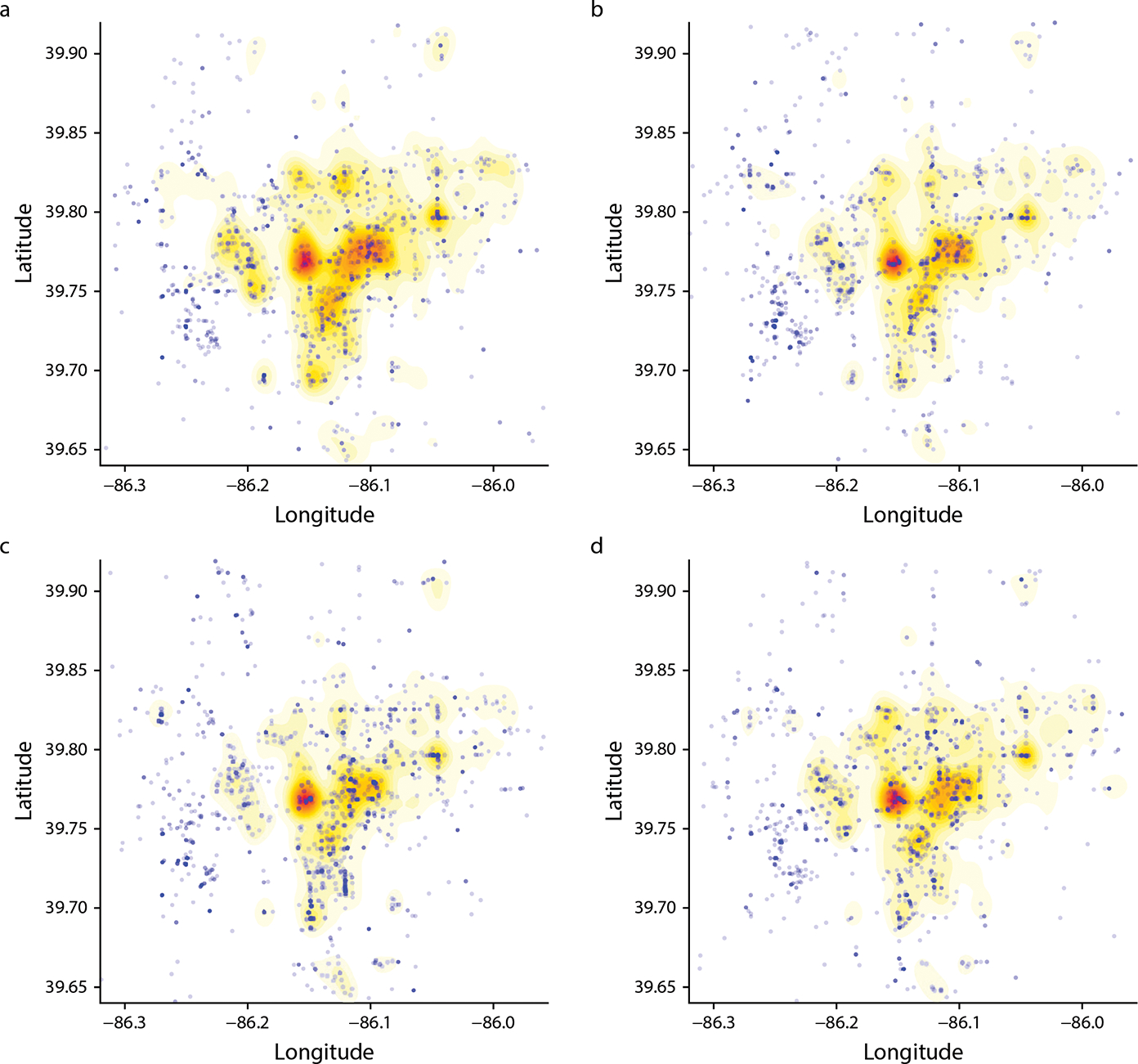
Note. Drug seizures include both opioid- and stimulant-related events; overdose events include both fatal and nonfatal, which include naloxone administrations.
Magnitudes of Association
Police seizures described as opioids were significantly associated with spatiotemporal clustering of fatal overdoses, nonfatal overdoses, and naloxone administrations at all selected time and distance parameters used in the analysis (100 m at 7 days, 250 m at 14 days, 500 m at 21 days; Figure 3; Figure B [available as a supplement to the online version of this article at http://www.ajph.org] provides the full set of comparisons). For example, the expected number of fatal overdoses within 500 meters and 21 days of opioid-related drug seizures ranged from 18.0 to 22.7 per 100 drug seizures, so the observed rate of 23.6 was higher than expected under the estimated null distribution. Stimulant-related drug seizures were also significantly associated with increased spatiotemporal clustering of overdose events but only at a distance of 100 meters within 7 days; the pattern of association was stronger for nonfatal overdoses.
FIGURE 3— Spatiotemporal Associations Between Opioid-Related and Stimulant-Related Drug Seizures and Fatal Overdose, Nonfatal Overdose, and Naloxone Administration Events: Marion County, IN, 2020–2021.
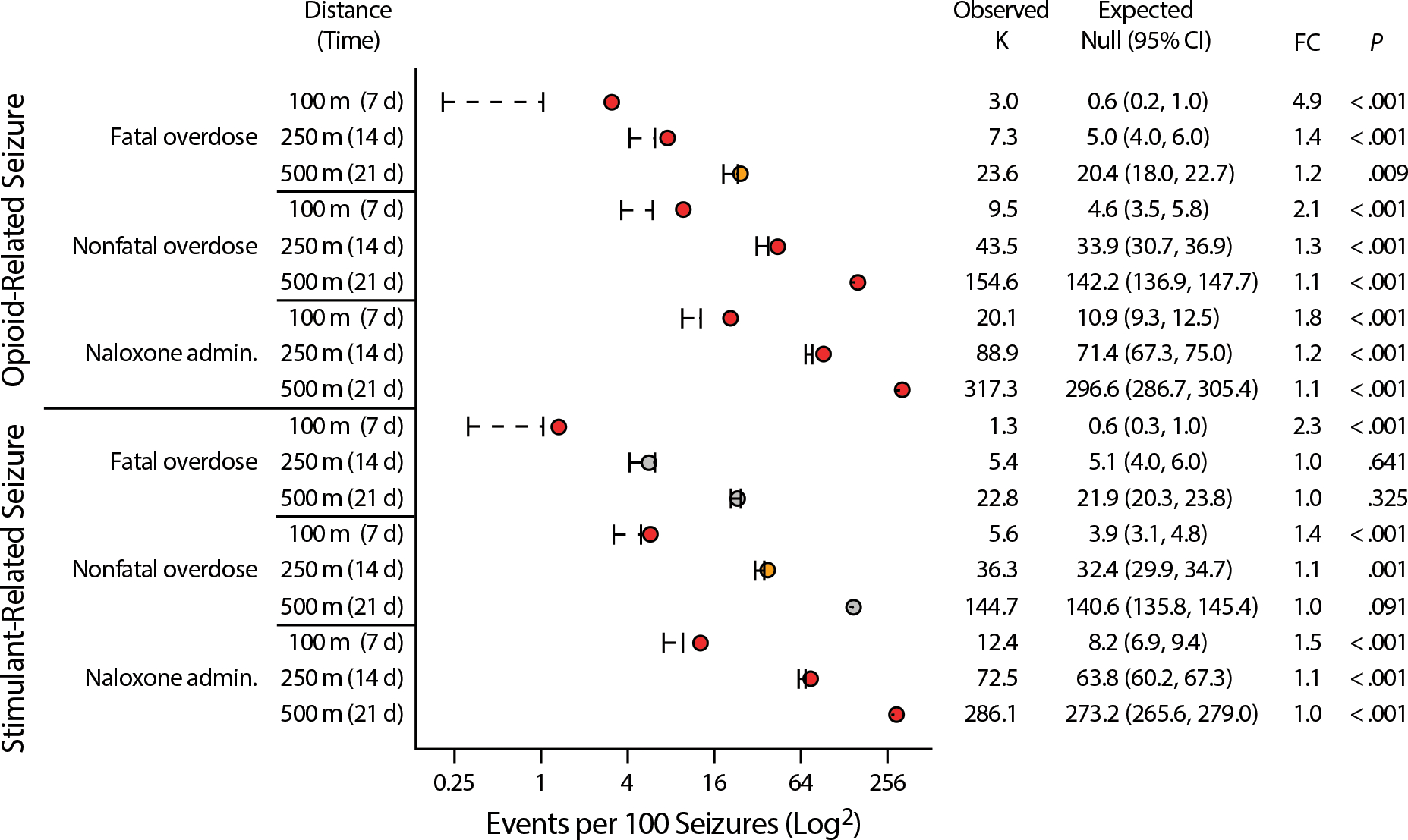
Note. admin 5 administration; CI 5 confidence interval; FC 5 fold change observed vs expected.
Pre–Post Differences
Figure 4 shows the observed pre–post drug seizure differences in overdose events versus what was expected under the null distribution (Figure C [available as a supplement to the online version of this article at http://www.ajph.org] shows the same for all time and distance parameters used in the analysis). The difference in fatal overdoses and naloxone administrations before and after opioid-related seizures was significantly greater than expected under the null distribution. By contrast, only at a distance of 100 meters over 7 days were the observed pre–post test differences in nonfatal overdoses higher than expected under the null distribution.
FIGURE 4— Observed vs Expected Pre–Post Differences in Spatiotemporal Associations Between Opioid-Related and Stimulant-Related Drug Seizures and Fatal Overdose, Nonfatal Overdose, and Naloxone Administration Events: Marion County, IN, 2020–2021.
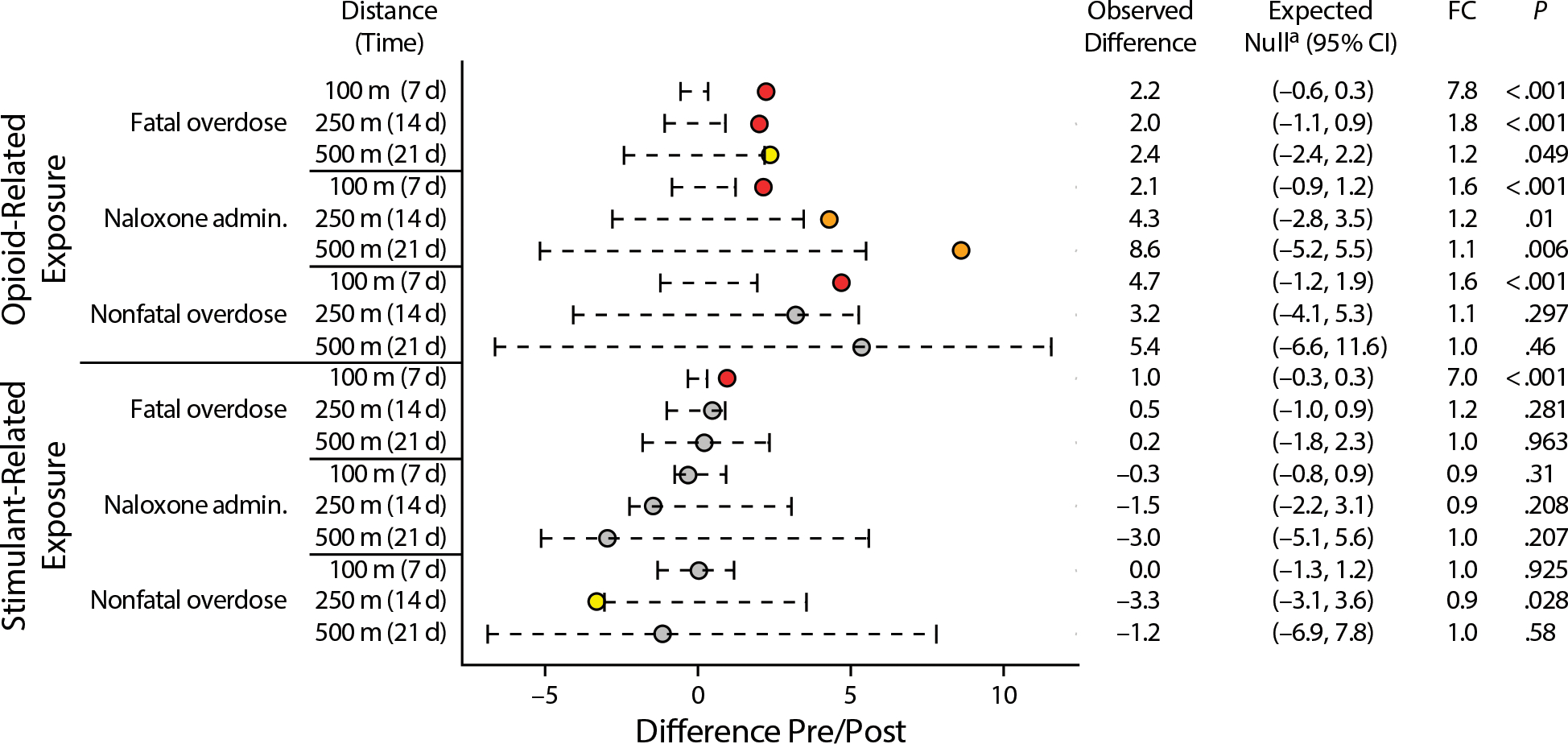
Note. admin 5 administration; CI 5 confidence interval; FC 5 fold change observed vs expected.
aThe observed pre–post difference is compared to the 95% CI for the expected difference estimated under the null distribution.
There were fewer statistically different changes from the estimated null distribution following stimulant-related seizures. Only at 100 meters within 7 days was the observed pre–post test difference in fatal overdoses following stimulant-related seizures higher than expected under the estimated null distribution. Moreover, the observed pre–post test difference in nonfatal overdoses with stimulant-related drug seizures was lower than expected compared with the estimated null distribution only at 250 meters within 14 days.
DISCUSSION
Our population-based study provides evidence that police seizures of substances identified as opioids or stimulants are significantly associated with increased spatiotemporal clustering of overdose events in the immediate surrounding geographic area (radii of 100 m, 250 m, and 500 m) over 1-, 2-, and 3-week periods. Importantly, the difference in spatiotemporal clustering of all 3 overdose event rates before and after opioid-related seizures was higher than expected under the estimated null distribution across all radii and time intervals although this pattern of association was less consistent among stimulant-related seizures. This is consistent with our hypothesized mechanism because persons with opioid use disorder who lose their supply will experience both diminishing tolerance and withdrawal, whereby even the anticipation of painful symptoms may lead them to seek a new supply while discounting risks that stem from the differences in potency inherent in an illicit opioid market; this results in unknown tolerance, uncertainty about a safe dose, and increased overdose risk.
We were unable to assert a causal relationship between law enforcement drug market disruptions and overdose, and our study was not designed to, but our results are consistent with other evidence of this association.18,19,22–24 Moreover, federal agencies already recognize the harms that emerge from these disruptions; for example, the Centers for Disease Control and Prevention developed the Opioid Rapid Response Program, an interagency effort designed to reduce overdose by rapidly increasing access to treatment of chronic pain and substance use disorder in the wake of enforcement actions against pain clinics and opioid prescribers.25,26 Routine supply-side interdictions among police may merit similar efforts to prevent resulting overdose in the surrounding community—but with more frequent need, given the prevailing volume of seizures.
Officers might also use the considerable discretion at their disposal when interacting with persons who use drugs, particularly in enforcing misdemeanors or nonviolent felonies that regulate drugs to reduce harms that might come from disrupting an individual’s drug supply.27 Additionally, our study suggests that information on drug seizures may provide a touchpoint that is further upstream than other postoverdose events, providing greater potential to mitigate harms. For example, although the role of law enforcement in overdose remains a topic of debate,28 public safety partnerships could entail timely notice of interdiction events to agencies that provide overdose prevention services, outreach, and referral to care.25
Efforts to disrupt the illicit drug supply have historically incentivized potency to minimize volume (and therefore transportation risk) and maximize profit, bringing the United States from an overdose epidemic fueled by prescription medications to illicitly manufactured fentanyl.29 As drug markets become less predictable and morbidity and mortality among people who use drugs increases, it is critical that communities not only create low barrier access to evidence-based treatment but also implement harm reduction strategies that directly address supply-side drivers of accidental overdose. Naloxone distribution, drug-checking, and overdose prevention sites are strategies first developed and implemented by people who use drugs that can be facilitated or enhanced by law enforcement cooperation through exceptions or “carve-outs” of drug criminalization to protect public health.30,31 These practices provide people who use drugs with shelter from the harms of drug policy but fall short of reassessing and revising policies that might prevent these harms in the first place.32,33
Moreover, to explore whether policies or practices affect the association between seizures and overdose observed in this study, it is critically important to replicate our analysis in other jurisdictions that are more or less punitive to determine whether seizures are associated with overdose in jurisdictions where people have access to a wider range of overdose prevention practices. For example, Indiana’s Good Samaritan Law (Indiana Code Title 16. Health § 16–42-27–2(g)-(h)) provides immunity from prosecution for drug possession provided the person administered naloxone and remained on the scene to cooperate with first responders. However, this law offers no protections for the overdose victim, which is uncommon for such laws and may contribute to decreased overdose calls for service in Indianapolis.34 Additionally, although a legal framework for syringe service programs is in place, the unauthorized possession of syringes remains a felony crime in Indiana (Indiana Code Title 16. Health § 16–42-19–18) and may contribute to arrest following overdose calls for service,35 likewise creating hesitancy to summon help.
Limitations
As with all observational studies, we cannot infer causality from the statistical associations. Although our use of the Knox test was novel and well suited to test our spatiotemporal hypothesis, it did not allow us to consider the influence of community-level factors that might affect results. Additionally, the setting of this study was 1 urban catchment area, yielding findings that may not be generalizable to rural settings or urban areas with different population characteristics or policy environments. We also do not know whether police actively targeted areas at greater overdose risk with an incidental frequency that enhanced the appearance of a pattern.
We relied on administrative data that are inherently subject to measurement error. Lack of information about the precise substance and quantity of each seizure or the characteristics of people subject to related enforcement, including association with the drug market as a supplier or consumer, inhibited our ability to explore these factors as potential sources of variation. We do not know whether these results would generalize to an illicit opioid market consisting mainly of analgesics or heroin when estimating dosage under uncertain circumstances. Both substances are much less potent than fentanyl and provide a larger margin of error. We also have no information to inform us of whether there should be a lagged time between seizures based on time to loss of supply, considering that people do not run out of their supply the moment a nearby seizure occurs.
Our measure of nonfatal overdose is also limited because fear of arrest is a well-established deterrent to calling 911 to report an overdose and because community naloxone administration often goes unreported. Certain populations are more likely to administer naloxone themselves or less likely to call 911, especially if previous incidents resulted in incarceration. It is also conceivable that EMS responses vary by neighborhood, that community-level naloxone distribution is affecting results, or that high-profile law enforcement interdiction events may result in a temporarily reduced willingness to call EMS for overdose emergencies. However, these factors would bias our findings toward the null hypothesis, rather than away from it.
Public Health Implications
Our study adds to a growing body of literature that suggests drug criminalization and supply-side interdiction might produce more public harm than public good. This casts doubt on the core assumption of state and federal drug policy and suggests that police officers intending to protect the public’s health and safety may be inadvertently exacerbating harms such as fatal overdose. Policymakers need to revisit the role drug policies play in perpetuating an overdose epidemic that is negatively affecting the nation’s life expectancy. This should include careful consideration of the population-level consequences from decades of interdiction efforts that have not resulted in any meaningful reduction in the price or availability of drugs in the community over any substantial period and may contribute to increased risk of overdose and its sequelae, including death.
Supplementary Material
ACKNOWLEDGMENTS
This study was funded by the Centers for Disease Control and Prevention (grant 1R01CE003362-01).
We would like to thank Dan O’Donnell and Tom Arkins for identifying the hypothesized mechanism for this study, Meredith Canada for assisting with data acquisition, and Jes Cochran for project consultation. Additionally, we thank the Indianapolis Emergency Medical Services, Marion County Coroner’s Office, and the Indianapolis Metropolitan Police Department for providing administrative data sources.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study, including waiver of the Health Insurance Portability and Accountability Act authorization and analysis of limited data sets, was approved by the Wayne State University institutional review board (#21–09-3996).
Reprints can be ordered at http://www.ajph.org by clicking the “Reprints” link.
Contributor Information
Bradley Ray, RTI International, Research Triangle Park, NC..
Steven J. Korzeniewski, School of Medicine, Wayne State University, Detroit, MI.
George Mohler, Computer Science Department, Boston College, Chestnut Hill, MA.
Jennifer J. Carroll, Department of Sociology and Anthropology, North Carolina State University, Raleigh.
Brandon del Pozo, Warren Alpert School of Medicine, Brown University, Providence, RI.
Grant Victor, School of Social Work, Rutgers University, New Brunswick, NJ.
Philip Huynh, Center for Behavioral Health and Justice, Wayne State University.
Bethany J. Hedden, Center for Behavioral Health and Justice, Wayne State University.
REFERENCES
- 1.Ahmad FB, Cisewski JA, Rossen LM, Sutton P. Provisional drug overdose death counts. 2023. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed February 21, 2023.
- 2.Ciccarone D The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344–350. 10.1097/YCO.0000000000000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park JN, Rashidi E, Foti K, Zoorob M, Sherman S, Alexander GC. Fentanyl and fentanyl analogs in the illicit stimulant supply: results from US drug seizure data, 2011–2016. Drug Alcohol Depend. 2020;218:108416. 10.1016/j.drugalcdep.2020.108416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmes LM, Rishworth A, King BH. Disparities in opioid overdose survival and naloxone administration in Pennsylvania. Drug Alcohol Depend. 2022;238:109555. 10.1016/j.drugalcdep.2022.109555 [DOI] [PubMed] [Google Scholar]
- 5.Lindstrom HA, Clemency BM, Snyder R, Consiglio JD, May PR, Moscati RM. Prehospital naloxone administration as a public health surveillance tool: a retrospective validation study. Prehosp Disaster Med. 2015;30(4):385–389. 10.1017/S1049023X15004793 [DOI] [PubMed] [Google Scholar]
- 6.Ising A, Proescholdbell S, Harmon KJ, Sachdeva N, Marshall SW, Waller AE. Use of syndromic surveillance data to monitor poisonings and drug overdoses in state and local public health agencies. Inj Prev. 2016;22(suppl 1):i43–i49. 10.1136/injuryprev-2015-041821 [DOI] [PubMed] [Google Scholar]
- 7.Schell RC, Allen B, Goedel WC, et al. Identifying predictors of opioid overdose death at a neighborhood level with machine learning. Am J Epidemiol. 2022;191(3):526–533. 10.1093/aje/kwab279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marks C, Abramovitz D, Donnelly CA, et al. Identifying counties at risk of high overdose mortality burden during the emerging fentanyl epidemic in the USA: a predictive statistical modeling study. Lancet Public Health. 2021;6(10):e720–e728. 10.1016/S2468-2667(21)00080-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bozorgi P, Porter DE, Eberth JM, Eidson JP, Karami A. The leading neighborhood-level predictors of drug overdose: a mixed machine learning and spatial approach. Drug Alcohol Depend. 2021;229(pt B):109143. 10.1016/j.drugalcdep.2021.109143 [DOI] [PubMed] [Google Scholar]
- 10.Mital S, Wolff J, Carroll JJ. The relationship between incarceration history and overdose in North America: a scoping review of the evidence. Drug Alcohol Depend. 2020;213:108088. 10.1016/j.drugalcdep.2020.108088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joudrey PJ, Khan MR, Wang EA, et al. A conceptual model for understanding post-release opioid-related overdose risk. Addict Sci Clin Pract. 2019;14(1):17. 10.1186/s13722-019-0145-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faggiano F, Mathis F, Diecidue R, et al. Opioid overdose risk during and after drug treatment for heroin dependence: an incidence density case–control study nested in the VEdeTTE cohort. Drug Alcohol Rev. 2021;40(2):281–286. 10.1111/dar.13173 [DOI] [PubMed] [Google Scholar]
- 13.Strang J, McCambridge J, Best D, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326(7396):959–960. 10.1136/bmj.326.7396.959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mark TL, Parish W. Opioid medication discontinuation and risk of adverse opioid-related health care events. J Subst Abuse Treat. 2019;103:58–63. 10.1016/j.jsat.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 15.Carroll JJ, Rich JD, Green TC. The protective effect of trusted dealers against opioid overdose in the US. Int J Drug Policy. 2020;78:102695. 10.1016/j.drugpo.2020.102695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Victor GA, Strickland J, Kheibari A, Flaherty C. A mixed-methods approach to understanding overdose risk-management strategies among a nationwide convenience sample. Int J Drug Policy. 2020;86:102973. 10.1016/j.drugpo.2020.102973 [DOI] [PubMed] [Google Scholar]
- 17.US Census Bureau. Fastest-growing cities are still in the West and South. May 26, 2022. Available at: https://www.census.gov/newsroom/press-releases/2022/fastest-growing-cities-population-estimates.html. Accessed June 20, 2022.
- 18.Rhodes B, Costenbader B, Wilson L, et al. Urban, individuals of color are impacted by fentanyl-contaminated heroin. Int J Drug Policy. 2019;73:1–6. 10.1016/j.drugpo.2019.07.008 [DOI] [PubMed] [Google Scholar]
- 19.Mohler G, Mishra S, Ray B, et al. A modified two-process Knox test for investigating the relationship between law enforcement opioid seizures and overdoses. Proc R Soc Math Phys Eng Sci. 2021;477(2250):20210195. 10.1098/rspa.2021.0195 [DOI] [Google Scholar]
- 20.Klauber MR. Two-sample randomization tests for space–time clustering. Biometrics. 1971;27(1):129–142. 10.2307/2528932 [DOI] [Google Scholar]
- 21.Carter JG, Mohler G, Ray B. Spatial concentration of opioid overdose deaths in Indianapolis: an application of the law of crime concentration at place to a public health epidemic. J Contemp Crim Justice. 2019;35(2):161–185. 10.1177/1043986218803527 [DOI] [Google Scholar]
- 22.Zibbell JE, Clarke SD, Kral AH, Richardson NJ, Cauchon D, Aldridge A. Association between law enforcement seizures of illicit drugs and drug overdose deaths involving cocaine and methamphetamine, Ohio, 2014–2019. Drug Alcohol Depend. 2022;232:109341. 10.1016/j.drugalcdep.2022.109341 [DOI] [PubMed] [Google Scholar]
- 23.Zibbell JE, Aldridge AP, Cauchon D, DeFiore-Hyrmer J, Conway KP. Association of law enforcement seizures of heroin, fentanyl, and carfentanil with opioid overdose deaths in Ohio, 2014–2017. JAMA Netw Open. 2019;2(11):e1914666. 10.1001/jamanetworkopen.2019.14666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lowder EM, Zhou W, Peppard L, Bates R, Carr T. Supply-side predictors of fatal drug overdose in the Washington/Baltimore HIDTA region: 2016–2020. Int J Drug Policy. 2022;110:103902. 10.1016/j.drugpo.2022.103902 [DOI] [PubMed] [Google Scholar]
- 25.Rubel SK, Neubert P, Navarretta N, Logan S. Facilitating overdose risk mitigation among patients following a clinician office closure: a Connecticut case study of the opioid rapid response program. J Public Health Manag Pract. 2022;28(1, suppl 6):S381–S387. 10.1097/PHH.0000000000001555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Acharya JC, Lyons BC, Murthy V, et al. An emergency preparedness response to opioid-prescribing enforcement actions in Maryland, 2018–2019. Public Health Rep. 2021;136(1 suppl):9S–17S. 10.1177/00333549211046110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.del Pozo B, Beletsky L, Goulka J, Kleinig J. Beyond decriminalization: ending the war on drugs requires recasting police discretion through the lens of a public health ethic. Am J Bioeth. 2021;21(4):41–44. 10.1080/15265161.2021.1891339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doe-Simkins M, El-Sabawi T, Carroll JJ. Whose concerns? It’s time to adjust the lens of research on police-involved overdose response. Am J Public Health. 2022;112(9):1239–1241. 10.2105/AJPH.2022.306988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beletsky L, Davis CS. Today’s fentanyl crisis: prohibition’s iron law, revisited. Int J Drug Policy. 2017;46:156–159. 10.1016/j.drugpo.2017.05.050 [DOI] [PubMed] [Google Scholar]
- 30.Lambdin BH, Davidson PJ, Browne EN, Suen LW, Wenger LD, Kral AH. Reduced emergency department visits and hospitalisation with use of an unsanctioned safe consumption site for injection drug use in the United States. J Gen Intern Med. 2022;37(15):3853–3860. 10.1007/s11606-021-07312-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Betsos A, Valleriani J, Boyd J, Bardwell G, Kerr T, McNeil R. “I couldn’t live with killing one of my friends or anybody”: a rapid ethnographic study of drug sellers’ use of drug checking. Int J Drug Policy. 2021;87:102845. 10.1016/j.drugpo.2020.102845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Netherland J, Kral AH, Ompad DC, et al. Principles and metrics for evaluating Oregon’s innovative drug decriminalization measure. J Urban Health. 2022;99(2):328–331. 10.1007/s11524-022-00606-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pamplin JR II, Rouhani S, Davis CS, King C, Townsend TN. Persistent criminalization and structural racism in US drug policy: the case of overdose good Samaritan laws. Am J Public Health. 2023;113(S1):S43–S48. 10.2105/AJPH.2022.307037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Network for Public Health Law. 50-State survey. Legal interventions to reduce overdose mortality: overdose good Samaritan laws. Available at: https://www.networkforphl.org/wp-content/uploads/2021/08/2021-50-State-Survey-Legal-Interventions-to-Reduce-Overdose-Mortality-Overdose-Good-Samaritan-Laws-8-18.pdf. Accessed April 9, 2023. [Google Scholar]
- 35.Wagner KD, Koch B, Bowles JM, Verdugo SR, Harding RW, Davidson PJ. Factors associated with calling 911 for an overdose: an ethnographic decision tree modeling approach. Am J Public Health. 2021;111(7):1281–1283. 10.2105/AJPH.2021.306261 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


