Abstract
Objectives
We evaluated the impact of a mailed, tailored intervention on skin cancer prevention and skin self-examination behaviors of adults at moderate and high risk for skin cancer.
Methods
Adults at moderate and high risk for skin cancer were recruited in primary health care settings in Honolulu, HI, and Long Island, NY. After completing a baseline survey, participants were randomized to 2 groups. The treatment group received tailored materials, including personalized risk feedback, and the control group received general educational materials. Multivariate analyses compared sun protection and skin self-examination between groups, controlling for location, risk level, gender, and age.
Results
A total of 596 adults completed the trial. The tailored materials had a significant effect on overall sun-protection habits, the use of hats, the use of sunglasses, and the recency of skin self-examination. Some effects were moderated by location and risk level.
Conclusions
Tailored communications including personalized risk feedback can improve sun-protection behaviors and skin self-examination among adults at increased risk for skin cancer. These convenient, low-cost interventions can be implemented in a variety of settings and should be tested further to assess their long-term effectiveness.
Skin cancer is the most commonly diagnosed cancer in the United States,1 with more than 1 million Americans diagnosed with skin cancer each year.2 The incidence of skin cancer has increased dramatically worldwide in the last decade.3 Both main types of skin cancer—malignant melanoma and nonmelanoma skin cancer—are now significant and costly public health concerns.2,4 Although skin cancer rates are increasing, it is considered one of the most preventable types of cancer. Prevention guidelines include reducing exposure to ultraviolet radiation (UVR); adopting sun-protection habits including the use of sunscreen, hats, shirts, and sunglasses5,6; performing regular skin self-examination; and seeking professional evaluation of suspicious skin changes. Nevertheless, levels of knowledge, concern, and the practice of prevention and early detection remain relatively low.7,8
Risk factors for skin cancer include age, sunsensitive phenotypes, excess sun exposure, family history, personal history of skin cancer or precancerous lesions, and other medical conditions.9 Most skin cancer prevention interventions reported to date are directed at the general population through school-based curricula and media campaigns,10 and some recent trials have targeted people who experience high sun exposure at work or during outdoor recreation.11–15 Only 2 reported studies have targeted groups at high risk: patients who have been treated for nonmelanoma skin cancer,16 and siblings of melanoma patients.17 There is a need for low-cost, effective interventions to improve skin cancer prevention and early detection behaviors among a broader population of persons at moderate and high risk.
Tailored, mailed communications hold great promise for skin cancer prevention and detection among individuals at increased risk, but these interventions have not been widely tested. Interventions that are tailored to individuals’ characteristics, behaviors, needs, and beliefs are more likely to be seen as personally relevant and thus may be more motivating.18 Tailored interventions have been shown to be effective in the past for other health behaviors, particularly for prevention and screening behaviors.19 The aim of Project SCAPE (Skin Cancer Awareness, Prevention and Education) was to evaluate the impact of tailored interventionson skin cancer prevention and skin self-examination among adults at high and moderate risk for skin cancer in a randomized trial.
METHODS
Project SCAPE was a randomized controlled trial. Adults at high and moderate risk for skin cancer were recruited and randomized to a control group or to receive a tailored intervention. Randomization was stratified by study site (Honolulu, HI, or Long Island, NY) and risk level (moderate or high). The tailored-intervention group received personalized risk feedback, recommendations, and reminders. The control group received brochures containing standard skin cancer prevention and detection information. The study was conducted between spring (April or May) and late summer (September) of 2000 and 2001. Participants completed a baseline survey and sun exposure and protection diary, a telephone interview at midsummer, and a second survey and diary in late summer. Participants were enrolled in the study in 2 cohorts over 2 successive summers. To improve participation and retention, participants were given small incentive gifts for returning surveys and diaries, such as magnets, pens, movie coupons, and video-rental coupons.
The study was conducted in Honolulu, Hawaii, and on Long Island, New York. Both locations have large beach areas where outdoor activities are popular, but they differ greatly in climate and ethnic distribution. Hawaii, the southernmost state in the United States, comprises a heterogeneous mix of ethnic groups, with no group in the majority. Most residents of Honolulu describe themselves as White (28.6%), Asian (40%), or mixed race (19.4%).20 Suffolk County, New York, on Long Island, has a resident population that is 87.1% White.21
Sample Recruitment and Risk Assessment
Participants were recruited in waiting rooms of outpatient primary care practices. Interested individuals were given a brief screening questionnaire, and those meeting inclusion criteria were enrolled in the study. Inclusion criteria were: age 20 to 65 years, resident of Honolulu or Long Island, and moderate or high risk for skin cancer as measured by the Brief Skin Cancer Risk Assessment Tool (BRAT).22 The BRAT asks about family history, previous premalignant lesions, personal history of skin cancer, number of nevi (moles or dark spots) at least .25 inch in diameter, and sun sensitivity. Risk categories were defined by tertile BRAT scores (<27=low risk; 27–35=moderate risk; >35=high risk) determined in a previous study in which the BRAT was found to reliably categorize persons at increased risk for skin cancer and to have good reproducibility.22 Exclusion criteria included currently being treated for melanoma or nonmelanoma skin cancer, not speaking English, and self-reported plans to be out of town for more than 2 weeks during the summer.
Intervention
The tailored messages tested in Project SCAPE had theoretical foundations in the health belief model23 and social cognitive theory.24 Tailoring variables included risk levels and specific risk factors from the BRAT assessment; reported sun exposure, sun protection, and skin examination practices; readiness to change; barriers to change; and extent of sunscreen application (from the baseline Sun Habits Survey). The key theoretically based constructs of risk perception, barriers and benefits (from the health belief model), behavioral capability (knowledge of skills), and social norms (from social cognitive theory) were hypothesized mediating variables.25
All intervention materials were distributed by mail. The tailored intervention (experimental) group received materials in 3 packages sent at 2-week intervals. Along with personalized risk feedback and recommendations, the experimental group received UV self-monitoring aids, skin self-examination instructions and practice tools, and skin cancer prevention and detection information. (Samples of materials are available by request from K. G.) The control group received a single mailing with a standard sun safety booklet, a tip sheet on sunscreen use, and a bookmark encouraging skin self-examination.
Data Collection
Sun Habits Survey
The baseline Sun Habits Survey asked participants about demographic characteristics, knowledge about skin cancer, habitual sun exposure and sun protection, and whether they had ever and recently (in the past 3 months) conducted a thorough skin self-examination. Sun exposure was measured by asking the respondents to indicate the average number of hours they spent outside between 10 Am and 4 Pm, both for weekdays and weekends. Sun protection habits were assessed by measuring 6 protective behaviors (wearing a shirt with sleeves, wearing sunglasses, staying in the shade, using sunscreen, limiting time in the sun during midday, and wearing a hat) on a 4-point ordinal scale ranging from 1=rarely or never to 4=always. The follow-up Sun Habits Survey asked the same questions. A composite sun protection habits score was calculated by averaging responses to the 6 items (α [internal consistency] = 0.67).26 Test-retest reliability of the composite sun protection habits score was calculated by repeated administrations of the Sun Habits Survey about 4 weeks apart to 62 adults who were not enrolled in the randomized trial (ρ=0.78; P<.001). Reproducibility (ρ) of reported hours of sun exposure was 0.73 for weekdays and 0.63 for weekend days (P<.001).
Sun exposure diary
The sun exposure diary is a 4-day record of sun exposure and protective behaviors. Participants were instructed to complete the diary for 2 weekdays and 2 weekend days, in accordance with previous research indicating that this amount of data is sufficient for estimating weekly behavior.27 The diary was formatted to collect information on activities between 10 Am and 4 Pm each day. Sun protection habits assessed for eachhour during the specified period were: using sunscreen, wearing a hat, staying in the shade, and covering up. Participants were also asked to mark “was indoors” if applicable. The level of sun protection was calculated by dividing the amount of time the individual reported using each type of sun protection by the amount of time spent outside for that day, resulting in a range of 0% to 100%.
The main outcomes for the diary were calculated using 4-day averages combining weekdays and weekends. Outcomes included measures of usual sun protection for each of the 4 habits, average percentage of all methods across the 4 sun protection habits, and an indicator of any sun protection. Reliability was assessed with 62 adults as described above for the Sun Habits Survey. Test-retest reliability of the sun exposure diary measure of average percentage sun protection across the 4 days was 0.69; for any sun protection, 0.73; and for average hours spent outside, 0.72, using the average intraclass correlation method.
Telephone interviews
Telephone interviews were conducted on Monday or Tuesday afternoons or evenings in midsummer. The interviews asked about sun exposure and sun protection habits for the preceding weekend, and receipt of and reactions to the intervention materials.
Reactions to interventions
Questions about participants’ reactions to both the treatment materials and the control materials were included in the follow-up Sun Habits Survey. Participants were asked to rate the materials they received on a scale of 1=not at all to 5=very for 6 features: easy to understand, informative, interesting, personally relevant, attractive, and confusing.
Statistical Analysis
Participants who completed Sun Habits Surveys at both baseline and follow-up were considered to have completed the study, although approximately 25% did not complete either or both diaries. Treatment effects were assessed on the basis of reported usual habits (surveys) and daily behavior (diaries). Treatment impact on potential mediating variables was also analyzed. Finally, participants’ reactions to the interventions were compared across treatment groups. Data analyses were conducted using SAS statistical software.28
Descriptive statistics were computed for all survey and diary variables to examine sample responses, distributions, and variability. We performed the χ2 test and the t test on survey baseline responses to check that randomization resulted in comparable groups, to determine whether any characteristics were associated with attrition or missing diary data, and to document differences between the 2 study locations. Covariates (gender, age, location, and risk group) were used throughout all multivariate analyses conducted unless the covariate moderated a treatment effect, in which case the covariate was excluded and a stratified analysis was done.
Three approaches were used to perform multivariate analyses of treatment effects. For survey outcomes—the sun protection habits index, individual habits, sunscreen application index, sun exposure, and number of sunburns—a mixed-model approach (i.e., PROC MIXED) was used with a data set containing 2 records per person and a time variable indicating baseline and follow-up administrations. This approach allows for the test of the (fixed) treatment-by-time interaction effect while accounting for the random effects associated with correlated repeated measurements.29 Some individual measures did not strictly meet the assumption that residuals are normally distributed and were thus subjected to a second analysis using a generalized linear model with Poisson distribution, and using generalized estimating equations that accounted for the covariance structure of the repeated measurements. Both approaches showed excellent agreement with regard to significance level and adjusted means of the treatment-by-time interaction. Therefore, only mixed-model results are presented. For the binomial variable of skin self-examination in the past 3 months, a generalized linear model was used as described above but modeling a binomial distribution.
Mixed models of several of the diary variables also had nonnormal residual distributions and were instead analyzed using a simple change score (i.e., follow-up score minus baseline score). These change score variables had normal distributions and were analyzed with general linear models testing a main effect for treatment group.
Reactions to the intervention and control materials were tested using the Wilcoxon rank-sum test. Mediator analyses were conducted based on the approach described by Baron et al25 and further discussed by MacKinnon et al.30
RESULTS
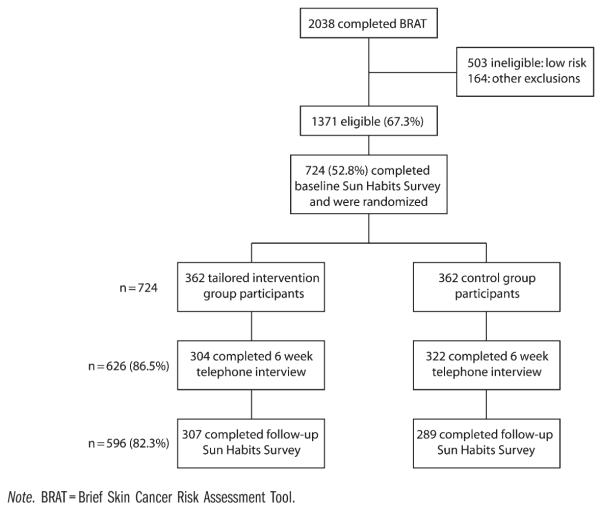
Over 2 summers, 2038 people completed the risk assessment, 1371 (67.3%) were eligible, and 724 completed the baseline survey and were randomized. The study completion rate was 82.3% (n=596). Figure 1 shows participation rates throughout the study.
FIGURE 1.
Number of participants at successive stages of trial: Project SCAPE; Honolulu, HI, and Long Island, NY; 2000 and 2001.
Participants were mostly female and White, and the mean age was 41.7 years (Table 1). Nearly half of participants were college-educated, and more than 60% had household incomes of $40 000 or more per year. More than one third were considered to be at high risk for developing skin cancer, more than two thirds had had a sunburn the previous summer, and less than half had performed a recent skin self-examination. Average sun protection habits were rated between sometimes practiced and usually practiced.
TABLE 1.
Baseline Characteristics of Participants by Treatment Group and Completion Status: Project SCAPE; Honolulu, HI, and Long Island, NY; 2000 and 2001
| Characteristic | Total (n = 724), % or Mean (SD) |
Intervention Enrolled (n = 362), % or Mean (SD) |
Control Enrolled (n = 362), % or Mean (SD) |
Intervention Completers (n = 307), % or Mean (SD) |
Control Completers (n = 289), % or Mean (SD) |
Pa |
|---|---|---|---|---|---|---|
| Women | 77.5 | 78.7 | 76.2 | 79.8 | 79.9 | .97 |
| Age, y (range = 20–65) | 41.7 (11.0) | 42.1 (10.8) | 41.2 (11.2) | 42.4 (10.6) | 41.3 (11.0) | .22 |
| White | 80.2 | 81.8 | 78.7 | 84.0 | 80.3 | .23 |
| Graduated college | 47.5 | 50.0 | 45.0 | 50.8 | 46.0 | .24 |
| Household income ≥ $40,000 | 63.5 | 64.8 | 62.0 | 66.1 | 62.3 | .35 |
| High risk for skin cancer | 36.6 | 37.0 | 36.2 | 37.5 | 35.0 | .52 |
| Had ≥ 1 sunburns last summer | 69.0 | 69.1 | 69.0 | 67.1 | 69.8 | .48 |
| Skin self-examination in last 3 mo | 46.9 | 46.2 | 47.5 | 43.9 | 47.4 | .40 |
| Sun protection habits indexb | 2.37 (0.54) | 2.39 (0.53) | 2.34 (0.55) | 2.37 (0.52) | 2.37 (0.55) | .87 |
| Sunscreen application indexc | 5.17 (2.73) | 5.26 (2.74) | 5.09 (2.72) | 5.21 (2.76) | 5.12 (2.73) | .70 |
| Risk perceptiond (range = 1–5) | 3.40 (0.95) | 3.38 (0.94) | 3.42 (0.97) | 3.38 (0.95) | 3.43 (0.98) | .54 |
| Perceived benefitse (range = 1–4) | 3.57 (0.46) | 3.59 (0.46) | 3.55 (0.46) | 3.61 (0.44) | 3.55 (0.47) | .13 |
| Perceived barriersf (range = 1–5) | 2.76 (0.73) | 2.75 (0.71) | 2.77 (0.75) | 2.74 (0.71) | 2.75 (0.71) | .80 |
| Social normsg (range = 1–4) | 2.57 (0.66) | 2.56 (0.64) | 2.57 (0.68) | 2.56 (0.64) | 2.57 (0.70) | .79 |
| Knowledgeh (range = 0–7) | 5.19 (1.28) | 5.27 (1.25) | 5.11 (1.31) | 5.27 (1.24) | 5.17 (1.31) | .30 |
Note. Sample sizes were smaller for some items because of some missing data (up to 2%). The χ2 test was used to assess relationships for categorical variables, and the t test was used to assess relationships for continous variables; no significant differences were found.
P value for completers.
Range of values was 1 = rarely or never to 4 = always.
Range of values was 0 = none to 9 = all exposed body parts.
Range of values was 1 = very unlikely to 5 = very likely.
Range of values was 1 = not at all to 4 = a great deal.
Range of values was 1 = strongly agree to 5 = strongly disagree.
Range of values was 1 = none to 4 = most or all.
Range of values was 0–7 (actual number answered correctly).
There were no significant differences between treatment and control groups in gender, education, ethnicity, age, percent high risk, or mean baseline sun habit score for all participants enrolled or for those who completed the study. Attrition was significantly greater among participants who were men, from Honolulu, recruited in year 2, and not White or Asian American. Among those completing baseline and follow-up surveys, 25% did not complete both the baseline and the follow-up diaries. Participants with missing diary data were more often from Long Island and had lower average sun protection habits scores at follow-up but did not differ by treatment arm, gender, education, race, skin cancer risk level, age, or baseline sun protection habits.
Several differences between Honolulu and Long Island participants were noted. Participants from Honolulu included proportionally more men and more persons with lower income (<$40 000 per year), and they were more likely to have had a sunburn in the prior 3 months.
We also conducted risk group and location comparisons of the baseline levels of sun protection on the basis of sun exposure diary data. Participants at higher risk for skin cancer had higher average rates of sun protection across the 4 behaviors (high risk=26.4%; moderate risk=20.2%) and greater use of sunscreen. Honolulu residents reported higher average sun protection behaviors (Honolulu=23.8%; Long Island=20.7%) and significantly more hat use.
Survey Data Main Outcomes
Sun Habits Survey responses were analyzed to determine whether change in usual habits was different for the intervention and control conditions. Table 2 presents the adjusted means for these outcomes and shows the significance of the interaction effect. The sun protection habits index showed a greater increase over time for participants in the intervention arm (effect size=0.13); however, this effect was moderated by location. The intervention arm in both locations showed significant improvement, but the treatment effect was attenuated for Honolulu (effect size=0.04; Long Island effect size=0.23) because the Honolulu comparison-arm participants also significantly increased their practice of sun protection habits. Among the specific habits that contribute to this scale, similarly moderated effects were observed for shade use and limiting exposure during peak hours, with Long Island participants showing treatment effects (shade use P=.056; limiting exposure P=.006). Use of sunglasses was significant but moderated by risk level; only those with moderate risk in the treatment arm showed improved use of sunglasses. Hat use showed a modest unmoderated effect (effect size=0.12). A comparable analysis for skin self-examination within the prior 3 months found a moderated effect, in which recent skin self-examination increased significantly more for the treatment group than for the control group for participants at higher risk for skin cancer (total effect size=0.21; high-risk effect size=0.39). Overall sun exposure and number of sunburns showed improvements across both treatment arms. Weekend and weekday exposure were moderated by location and risk level, respectively, though the results showed similar patterns in the stratified analyses.
TABLE 2.
Effects of Tailored Messages on Sun Protection Habits and Skin Self-Examination: Survey Results: Project SCAPE; Honolulu, HI, and Long Island, NY; 2000 and 2001
| Treatment Group (n = 307) |
Control Group (n = 289) |
||||
|---|---|---|---|---|---|
| Baseline, Adjusted Meana (SE) | Follow-Up, Adjusted Meana (SE) | Baseline, Adjusted Meana (SE) | Follow-Up, Adjusted Meana (SE) | P | |
| Sun protection habits indexb,c | 2.34 (0.03) | 2.57 (0.03) | 2.34 (0.03) | 2.46 (0.03) | .001 |
| Use sunscreenc | 2.54 (0.06) | 2.78 (0.06) | 2.63 (0.06) | 2.84 (0.06) | .57 |
| Wear a shirtc | 1.95 (0.06) | 2.08 (0.06) | 1.94 (0.06) | 1.94 (0.07) | .08 |
| Wear a hatc | 1.91 (0.06) | 2.21 (0.06) | 2.00 (0.06) | 2.11 (0.06) | .003 |
| Stay in shadeb,c | 2.25 (0.05) | 2.49 (0.05) | 2.20 (0.05) | 2.40 (0.05) | .43 |
| Wear sunglassesc,d | 2.79 (0.07) | 3.03 (0.07) | 2.79 (0.07) | 2.85 (0.07) | .004 |
| Limit exposure in peak hoursb,c | 2.55 (0.05) | 2.78 (0.05) | 2.47 (0.06) | 2.59 (0.06) | .10 |
| Sunscreen application indexe | 5.05 (0.18) | 5.51 (0.18) | 4.93 (0.18) | 5.10 (0.18) | .14 |
| Sun exposure between 10 Am and 4 Pmf | 2.55 (0.07) | 2.22 (0.07) | 2.60 (0.08) | 2.34 (0.08) | .35 |
| Weekday sun exposure | 2.05 (0.08) | 1.80 (0.08) | 2.12 (0.08) | 2.04 (0.08) | .11 |
| Weekend sun exposure | 3.01 (0.09) | 2.58 (0.09) | 3.02 (0.09) | 2.60 (0.09) | .97 |
| Sunburnsg | 1.44 (0.07) | 0.89 (0.07) | 1.37 (0.07) | 0.96 (0.07) | .14 |
| Skin self-examinationd,h | 0.39 (0.03) | 0.71 (0.03) | 0.43 (0.03) | 0.61 (0.03) | .004 |
Note. Sample sizes for separate analyses were lower because of missing data (up to 3%).
Means calculated with adjustment for covariates (location, risk level, age, gender) unless otherwise stated. Mixed models were used (except for skin self-examination), with P value indicating the significance of the time × intervention term.
Location covariate was excluded because of interaction with treatment effect.
Range of values was 1 = rarely or never to 4 = always.
Risk level covariate was excluded because of interaction with treatment effect.
Range of values was 0 = none to 9 = all exposed body parts.
Range of values was 1 = 1 hour or fewer to 6 = 6 hours per day.
Range of values was 0 = none to 3 = 3 or more sunburns.
Proportion adjusted for covariates. Model was a generalized linear model with binomial distribution using generalized estimating equations.
Diary Data Main Outcomes
Baseline mean scores showed that, on average, 67% of the time participants used 1 or more of sunscreen, shade, a hat, or covering up when outside. Average sunscreen and shade use were both about 31%, hat use was 15%, and covering up was 12%. The average use across the 4 behaviors was 22.3%. Average hours spent outside were 2.4 on weekdays and 3.2 on weekends.
Diary data were analyzed as simple change scores from baseline to follow-up. Compared with the control group, the treatment group showed significant improvement on the sun protection habits composite (effect size=0.39), sunscreen use, and hat wearing (Table 3). The sun protection habits composite was moderated by age and showed greater improvement for intervention participants older than age 40 years. Use of any protection and sunscreen differed by location, with the Long Island treatment group showing significant effects not found among Honolulu participants. Hat use increased among higher-risk persons in the treatment group. Most other diary measures were in the expected direction, with the treatment group showing more sun protection improvements than the control group.
TABLE 3.
Sun Protection Diary Results of Behavior Change From Baseline to Follow-Up: Project SCAPE; Honolulu, HI, and Long Island, NY; 2000 and 2001
| Treatment Group, Adjusted Mean (SE) of Change Scorea |
Control Group, Adjusted Mean (SE) of Change Scorea |
Pb | |
|---|---|---|---|
| Average sun protection habitsc | 8.60 (1.31) | 1.85 (1.36) | <.001 |
| Any sun protectiond | 11.10 (2.88) | 5.19 (2.98) | .10 |
| Use sunscreend | 8.78 (2.80) | 0.93 (2.90) | .03 |
| Wear a shirt | 10.01 (2.21) | 3.69 (2.34) | .05 |
| Wear a hate | 6.31 (1.99) | 0.04 (2.07) | .02 |
| Stay in shade | 7.71 (2.53) | 1.90 (2.67) | .12 |
| Sun exposure totalf | −0.34 (0.11) | −0.21 (0.11) | .41 |
| Sun exposure weekdaysf | −0.17 (0.14) | −0.30 (0.14) | .53 |
| Sun exposure weekendsf | −0.45 (0.14) | −0.11 (0.15) | .10 |
Note. Sample sizes for separate analyses were lower because of missing data (up to 4%). Sample size for treatment group was n = 234; for the control group n = 211.
% used at follow-up minus % used at baseline.
F test result for intervention effect from generalized linear model.
Means calculated with adjustment for location, gender, and risk group covariates.
Means calculated with adjustment for age, gender, and risk group covariates.
Means calculated with adjustment for location, gender, and risk group covariates.
Follow-up hours minus baseline hours.
Reactions to Interventions
At the midsummer telephone interviews, nearly all respondents reported receiving materials from Project SCAPE, about half had read all the materials, and 80% still had the materials. Treatment group respondents’ ratings were significantly higher on all responses, with differences ranging from 3% to 15% (P<.01). At follow-up, respondents’ reactions to the mailed materials were compared for the intervention and control arms. Whereas both groups had positive reactions to the mailings, with most ratings at 4 or higher on a 5-point scale, the intervention participants rated their materials significantly higher than the control group on all items.
Mediators Analysis Findings
Hypothesized mediators (risk perception, perceived benefits, perceived barriers, social norms, knowledge, and intention to increase sun protection) were assessed for differences by treatment arm. Although risk perception and intention to increase sun protection differed significantly by treatment arm, their mediation of the sun protection habits index (in individual models) was either not significant when treatment was in the model (risk perception), or the mediation effect was not statistically significant (intention to increase sun protection).
DISCUSSION
This study showed that using mailed, tailored communications had a modest positive impact on skin cancer prevention practices. Based on survey data, the intervention yielded significant reported increases in overall sun protection habits, use of hats and sunglasses, and performance of skin self-examinations. Data from 4-day diaries showed similar patterns but also showed that use of sunscreen was significantly improved for the treatment group.
Some effects were moderated by location and risk level. Less intervention impact was seen for participants from Honolulu because the control group also increased their sun protection habits, possibly because of environmental context or racial/ethnic differences.31 The higher-risk group showed more increase in skin self-exams than the moderate risk group.
The increase in recent skin self-examination in the Project SCAPE treatment group is note-worthy, given the difficulty of achieving sustained changes in habitual sun protection behaviors. Although neither professional nor self-administered examinations of the skin have been shown to reduce mortality in a randomized controlled trial, monthly thorough skin self-examination has been associated with reduced melanoma mortality.32,33 Early detection is an increasingly important tool in skin cancer control34 and is most likely to be beneficial for early detection in high-risk individuals.
A recent study of preventive interventions for adults at increased risk for skin cancer used 4 telephone counseling calls, tailored print materials, and links to free skin screening programs.17 The interventions were effective in increasing both professional and skin self-examinations, but they did not lead to greater sunscreen use in the treatment group. By comparison, Project SCAPE was relatively low-intensity and inexpensive, but it focused more on preventive behaviors and achieved modest impact on sun safety habits, including increases in sunscreen use, as measured by diary assessments. Small effect sizes were achieved with a low-cost intervention.
Findings from survey data revealed no relative increase in habitual sunscreen use among those who received the tailored materials. However, the diary data revealed a significantly greater increase in sunscreen use in the treatment group. In another study of the validity of self-reports of sunscreen use among 564 adults and children, we found that diary assessments were better correlated with an objective measure of sunscreen use (skin swabbing) than survey measures.35 This suggests that using 2 different types of assessment tools may provide a better overall picture of intervention effects, though few skin cancer studies report the use of such methods.36
Strengths of this study include its relatively large size, 2 geographic locations, assessment of both habitual (survey) and daily (diary) prevention and exposure behaviors, and more diverse ethnicity of participants than most other skin cancer prevention trials. However, participants were mostly female, relatively well-educated, and affluent, and it is possible that print materials would not work as well in less-educated groups. Other limitations include different amounts of attention to treatment and control groups, lack of long-term follow-up, and reliance on self-report. We note that the use of self-report is appropriate in population-based skin cancer prevention research37 and that good validity of self-reports of sunscreen35 has now been established.
Project SCAPE adds to the body of evidence supporting the promise of tailored communications,19,38 especially for increased-risk adults. Tailored messages have the potential to focus prevention efforts on those who can most benefit from them, thereby increasing the efficiency and effectiveness of health promotion and cancer prevention interventions. Given the magnitude of the public health problem of skin cancer and the lack of proven therapeutic interventions for high-risk groups,39 it is important to further test inexpensive, convenient interventions such as tailored communications. Future studies should include longer follow-up periods and tests of the dissemination of tailored materials through community and health care organizations.
Acknowledgments
The authors wish to acknowledge the contributions of Martin Weinstock, Gabriela Layi, Jeanne Kidd, Diana Evensen, and Jennifer Chee to the development and conduct of this trial. This work was supported by National Cancer Institute (grant CA 76419). K. Glanz’s work was supported in part by a Distinguished Scholar Award from the Georgia Cancer Coalition.
Footnotes
Reprints can be ordered at http://www.ajph.org by clicking the “Reprints/Eprints” link.
Human Participant Protection This study was approved by the institutional review boards of the University of Hawaii and Stony Brook University.
Contributor Information
Karen Glanz, School of Medicine and the School of Nursing, University of Pennsylvania, Philadelphia..
Elinor R. Schoenfeld, Department of Preventive Medicine, Stony Brook University, Stony Brook, NY..
Alana Steffen, Cancer Research Center of Hawaii, University of Hawaii, Honolulu..
References
- 1.Jemal A, Devesa S, Hartge P, Tucker M. Recent trends in cutaneous malignant melanoma incidence among Whites in the United States. J Natl Cancer Inst. 2001;93(9):678–683. doi: 10.1093/jnci/93.9.678. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society . Cancer Facts and Figures 2008. American Cancer Society; Atlanta, GA: 2008. [Google Scholar]
- 3.Ries LAG, Melbert D, Krapcho M, et al. Surveillance Epidemiology and End Results Web site. National Cancer Institute; Bethesda, MD: [Accessed September 5, 2006]. 2008. Previous version: SEER cancer statistics review, 1975– 2005. Available at: http://seer.cancer.gov/csr/1975_2005. [Google Scholar]
- 4.Housman TS, Feldman SR, Williford PM, et al. Skin cancer is among the most costly of all cancers to treat for the Medicare population. J Am Acad Dermatol. 2003;48(3):425–429. doi: 10.1067/mjd.2003.186. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong BK. How sun exposure causes skin cancer: An epidemiological perspective. In: Hill D, Elwood JM, English DR, editors. Prevention of Skin Cancer. Kluwer Academic Publishers; Dordrecht, the Netherlands: 2004. pp. 89–116. [Google Scholar]
- 6.US Dept of Health and Human Services Dept of Health and Human Services; Washington, DC: Healthy People 2010: Understanding and Improving Health. (2nd ed) 2000
- 7.Hall HI, Saraiya M, Thompson T, Hartman A, Glanz K, Rimer B. Correlates of sunburn experiences among US adults: results of the 2000 National Health Interview Survey. Public Health Rep. 2003;118(6):540–549. doi: 10.1016/S0033-3549(04)50290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the US population. Am J Prev Med. 2008;34(2):87–93. doi: 10.1016/j.amepre.2007.09.032. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63(1–3):8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 10.Saraiya M, Glanz K, Briss P, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med. 2004;27(5):422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Buller DB, Andersen PA, Walkosz BJ, et al. Randomized trial testing a worksite sun protection program in an outdoor recreation industry. Health Educ Behav. 2005;32(4):514–535. doi: 10.1177/1090198105276211. [DOI] [PubMed] [Google Scholar]
- 12.Weinstock MA, Rozzi JS, Redding CA, Maddock JE. Randomized controlled community trial of the efficacy of a multicomponent stage-matched intervention to increase sun protection among beachgoers. Prev Med. 2002;35(6):584–592. doi: 10.1006/pmed.2002.1114. [DOI] [PubMed] [Google Scholar]
- 13.Glanz K, Lew RA, Song V, Murakami-Akatsuka L. Skin cancer prevention in outdoor recreation settings: effects of the Hawaii SunSmart Program. Eff Clin Pract. 2000;3(2):53–61. [PubMed] [Google Scholar]
- 14.Geller AC, Glanz K, Shigaki D, Isnec MR, Sun T, Maddock J. Impact of skin cancer prevention on outdoor aquatics staff: the Pool Cool program in Hawaii and Massachusetts. Prev Med. 2001;33(3):155–161. doi: 10.1006/pmed.2001.0870. [DOI] [PubMed] [Google Scholar]
- 15.Glanz K, Geller AC, Shigaki D, Maddock JE. A randomized trial of skin cancer prevention in aquatics settings: the POOL COOL program. Health Psychol. 2002;21(6):579–587. [PubMed] [Google Scholar]
- 16.Robinson JK. Compensation strategies in sun protection behaviors by a population with nonmelanoma skin cancer. Prev Med. 1992;21(6):754–765. doi: 10.1016/0091-7435(92)90082-s. [DOI] [PubMed] [Google Scholar]
- 17.Geller AC, Emmons KM, Brooks DR, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107(4):806–814. doi: 10.1002/cncr.22050. [DOI] [PubMed] [Google Scholar]
- 18.Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring Health Messages: Customizing Communication with Computer Technology. Erlbaum; Mahwah, NJ: 2000. [Google Scholar]
- 19.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau [Accessed July 12, 2008];State & County QuickFacts: Hawaii. Available at: http://quickfacts.census.gov/qfd/states/15000.html.
- 21.US Census Bureau [Accessed July 12, 2008];State & County QuickFacts: Suffolk County, New York. Available at: http://quickfacts.census.gov/qfd/states/36/36103.html.
- 22.Glanz K, Schoenfeld E, Weinstock M, Layi G, Kidd J, Shigaki D. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detect Prev. 2003;27(4):311–315. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- 23.Janz NK, Champion VL, Strecher VJ. The Health Belief Model. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research and Practice. 3rd ed Jossey-Bass; San Francisco, CA: 2002. pp. 45–66. [Google Scholar]
- 24.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.Glanz K, Lew R, Song V, Ah Cook V. Factors associated with skin cancer prevention practices in a multiethnic population. Health Educ Behav. 1999;26(3):344–359. doi: 10.1177/109019819902600305. [DOI] [PubMed] [Google Scholar]
- 27.Glanz K, Silverio R, Farmer A. Diary reveals sun protective practices. Skin Cancer Found J. 1996;14:27–28. 86. [Google Scholar]
- 28.SAS [computer program] Version 9.1 SAS Institute; Cary, NC: 2003. [Google Scholar]
- 29.Littell RC, Pendergast J, Natarajan R. Modelling covariance structure in the analysis of repeated measures data. Stat Med. 2000;19(13):1793–1819. doi: 10.1002/1097-0258(20000715)19:13<1793::aid-sim482>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 30.MacKinnon DP, Taborga MP, Morgan-Lopez AA. Mediation designs for tobacco prevention research. Drug Alcohol Depend. 2002;68(suppl 1):S69–S83. doi: 10.1016/s0376-8716(02)00216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pichon LC, Mayer JA, Slymen DJ, Elder JP, Lewis EC, Galindo GR. Ethnoracial differences among outdoor workers in key sun-safety behaviors. Am J Prev Med. 2005;28(4):374–378. doi: 10.1016/j.amepre.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Berwick M, Begg CB, Fine JA, Rouseh GC, Barnhill RL. Screening for cutaneous melanoma by skin self-examination. J Natl Cancer Inst. 1996;88(1):17–23. doi: 10.1093/jnci/88.1.17. [DOI] [PubMed] [Google Scholar]
- 33.Weinstock MA. Early detection of melanoma. JAMA. 2000;284(7):886–889. doi: 10.1001/jama.284.7.886. [DOI] [PubMed] [Google Scholar]
- 34.Weinstock MA. Cutaneous melanoma: public health approach to early detection. Dermatol Ther. 2006;19(1):26–31. doi: 10.1111/j.1529-8019.2005.00053.x. [DOI] [PubMed] [Google Scholar]
- 35.Glanz K, McCarty F, Nehl EJ, et al. Validity of self-reported sunscreen use by parents, children and life-guards. Am J Prev Med. 2009;36(1):63–69. doi: 10.1016/j.amepre.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glanz K, Mayer JA. Reducing ultraviolet radiation exposure to prevent skin cancer: methodology and measurement. Am J Prev Med. 2005;29(2):131–142. doi: 10.1016/j.amepre.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Glanz K, Yaroch AL, Dancel M, et al. Measures of sun exposure and sun protection practices for behavioral and epidemiologic research. Arch Dermatol. 2008;144(2):217–222. doi: 10.1001/archdermatol.2007.46. [DOI] [PubMed] [Google Scholar]
- 38.Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Ann Behav Med. 2006;31(3):205–233. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- 39.Bath-Hextall F, Leonardi-Bee J, Somchand N, Webster A, Delitt J, Perkins W. Interventions for preventing non-melanoma skin cancers in high-risk groups. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD005414.pub2. CD005414. [DOI] [PMC free article] [PubMed] [Google Scholar]