Abstract
Objective:
The Perinatal Neonatal Quality Improvement Network of Massachusetts (PNQIN) sought to adapt the Reduction of Peripartum Racial and Ethnic Disparities Conceptual Framework and Maternal Safety Consensus Bundle by selecting and defining measures to create a bundle to address maternal health inequities in Massachusetts. This study describes the process of developing consensus-based measures to implement the PNQIN Maternal Equity Bundle across MA hospitals participating in AIM (Alliance for Innovation on Maternal Health) Initiative.
Methods:
Our team used a mixed-methods approach to create the PNQIN Maternal Equity Bundle through consensus including a literature review, expert interviews, and a modified Delphi process to compile, define, and select measures to drive maternal equity-focused action. Stakeholders were identified by purposive and snowball sampling and included OB/GYNs, midwives, nurses, epidemiologists, and racial equity scholars. Dedoose 9.0 was used to complete an inductive analysis of interview transcripts. A modified Delphi method was used to reach consensus on recommendations and measures for the PNQIN Maternal Equity Bundle.
Results:
Twenty-five interviews were completed. Seven themes emerged including the need for 1) data stratification by race, ethnicity and language, 2) performance of a readiness assessment, 3) culture shift toward equity, 4) inclusion of anti-racism and bias training, 5) addressing challenges of non-academic hospitals, 6) a life-course approach, and 7) selection of timing of implementation. Twenty initial quality measures (structure, process, and outcome) were identified through expert interviews. Group consensus supported ten measures to be incorporated into the bundle.
Conclusions:
Structure, process, and outcome quality measures were selected and defined for a maternal equity safety bundle that seeks to create an equity-focused infrastructure and equity-specific actions at birthing facilities. Implementation of an equity-focused safety bundle at birthing facilities may close racial gaps in maternal outcomes.
Precis
Establishing structure, process, and outcome measures through expert consensus creates the infrastructure for a maternal safety bundle to reduce inequities in maternal health.
Introduction
Maternal mortality (MM) and severe maternal morbidity (SMM) continue to rise in the US.1,2 Black non-Hispanic (Black) birthing people are more than twice as likely to die in childbirth compared to their White non-Hispanic (White) peers.1-4 In Massachusetts (MA), SMM rates are 2.3 times more common among Black births.5
Many factors contribute to MM, SMM, and inequities including the site of care, timely receipt of care, health insurance type, and pre-existing conditions.6,7 Notably, racism, not race, is an important and independent contributor to worse outcomes.6,8,9 To address systems factors, the Alliance for Innovation on Maternal Health (AIM) publishes maternal safety bundles (MSB) of evidence-based practices and institutional guidelines.10,11 The AIM bundles, implemented through perinatal quality collaboratives (PQCs), include five domains: Readiness, Recognition and Prevention, Response, Reporting and Systems Learning, and most recently, Respectful Care.12,13 While they are evidence-based collections of recommendations, they are intended to be adapted to the needs of each collaborative using quality improvement (QI) methodology.
Maternal Safety Bundles have successfully improved outcomes and reduced racial gaps through structured, actionable steps for implementing evidence-based practices. In California, MM rates decreased and SMM racial disparities reduced after implementing an obstetric hemorrhage MSB while national rates rose.14,15 One health system implemented an equity-focused goal of reducing MM for Black individuals across five hospital sites by forming a data-driven, QI collaborative to address inequities through evidence-based practices.16 Davidson et al. demonstrated a decline in SMM and the SMM racial disparity after data disaggregated by race and ethnicity were presented at department meetings, even before other bundle measures were implemented.17 These findings suggest that calling attention to racial gaps in SMM activates teams toward improvement, may aid in decreasing racial inequities in MM and SMM, and emphasizes the importance of defining measures to target improvements.17
The Perinatal Neonatal Quality Improvement Network of Massachusetts (PNQIN), the MA state PQC, aimed to implement a maternal equity bundle to create an equity-focused infrastructure across birthing facilities in MA. PNQIN sought to adapt the Reduction of Peripartum Racial and Ethnic Disparities Conceptual Framework and Maternal Safety Consensus Bundle and create a maternal safety bundle to equip teams seeking to address discrimination and racism resulting in maternal inequities with action steps and standardized metrics.18 This manuscript describes the methodology of creating the PNQIN Maternal Equity Bundle.
Methods
Our mixed methods approach to create the Maternal Equity Bundle through consensus included a literature review, expert interviews, and a modified Delphi process with the members of the PNQIN Maternal Equity Bundle workgroup. We searched published literature to identify potential measures for the bundle and themes for implementing equity-focused QI work. We searched MEDLINE, PubMed, Cochrane Library, and Google Scholar from August 2000 to July 2021. Search terms included quality improvement, maternal health, maternal equity, health equity measures, bundle implementation, racial equity projects, perinatal quality, maternal morbidity, maternal mortality, racism, anti-racism, and respectful maternity care. The literature review informed the standardized questions for stakeholder interviews (Appendix 1, available online at http://links.lww.com/xxx), the list of experts we sought to interview, and potential measures for the maternal equity bundle.
Stakeholders were selected using purposive and snowball sampling. In stage one, stakeholders were identified through literature review with relevant publications on the subject matter and reputation as experts in maternal health equity. These included OB/GYN physicians, nurses, midwives, epidemiologists, and scholars in racial equity and maternal-child health. The sample frame was national, but as implementation was explicitly meant for MA, experts who conducted their work in MA were oversampled. In stage two, snowball sampling was used to identify experts as interviewees referred to or suggested other experts. Study participants were contacted by email.
Interviews of expert stakeholders were conducted virtually using Zoom.19 One or two interviewers (AK and KV) were present for each interview. Following participant consent, interviews were conducted using a standardized guide (Appendix 1, http://links.lww.com/xxx) and recorded to Zoom cloud storage, where a transcript was produced using Zoom’s internal transcription program. Transcripts were reviewed, edited for accuracy, and uploaded to Dedoose v9.0.20
Interviews were used to compile measures based on the Donabedian Model for Measuring Healthcare Quality: structures, processes, and outcomes.21 The interviews provided insights on possible bundle measures and measures implementation. After the 15th interview, there were no new themes generated, and it was deemed that data collection reached saturation. The 10 additional interviews confirmed no new emerging themes.
Using traditional inductive qualitative methodology, interview transcripts, and notes were coded using Dedoose v.9.0 software. Codes were generated from the interview transcripts, notes, and interview guide (Appendix 2, available online at http://links.lww.com/xxx). Codes were reviewed and organized by root and sub-codes by AK and AM. Root codes created thematic summaries of key findings. This was presented to the Maternal Equity Bundle workgroup to inform measure selection.
The Delphi phase took place March-June 2022. The Maternal Equity Bundle workgroup, a self-nominated and knowledgeable group of healthcare professionals, scholars, and community members, provided continuous review and feedback on bundle measures and implementation processes. This twenty-two-member group was tasked to select the final structure, process, and outcome measures prior to the bundle launch in September 2022. The modified Delphi rounds were conducted over five 60-minute, virtual meetings with open and anonymous feedback to obtain and synthesize the views of the Maternal Equity Bundle workgroup members. Members received an introduction to the project including goals and context then were presented with twenty-five candidate measures (Table 1) and thematic summaries from the expert stakeholder interviews. To reach a consensus on bundle measures, emphasis was placed on perceived acceptability and feasibility among hospital teams and the appropriateness of measures for addressing maternal equity.22 The table of candidate measures was edited after each Delphi meeting to reflect suggested modifications. Themes uplifted during the Delphi process included creating an infrastructure to address equity on labor units, addressing the leading causes of SMM in MA, and aligning with recent AIM bundles implemented among MA birth facilities. The first three rounds of meetings led to agreement on 10 proposed structure, process, and outcome measures. Over two subsequent Delphi rounds, workgroup members further refined the measures and reached consensus. The senior author (AM) facilitated the discussions of all five Delphi rounds.
Table 1.
Preliminary and Selected Measures for PNQIN MA Maternal Equity Bundle from Literature Review, Expert Interviews, and Equity Workgroup Review
| Structure | Process | Outcome | |
|---|---|---|---|
| Candidate Measures |
|
|
|
| Selected Measures | 1 Equity Team 2 Equity Goals 3 REaL Data Collection by Self-Report 4 Data Disaggregation by REaL 5 PREMs |
6 % Staff Trained in Bias and Respectful Care† 7-9 % Perinatal Care Standard Met by REaL: 1)Obstetric Hemorrhage Risk Assessment, 2)QBL use, 3)Timely Treatment for Hypertension |
10 SMM 20/21 Rates by REaL |
PREMs suggested include the Mothers on Autonomy in Decision Making (MADM), Mothers on Respect Index (MORi), Birth Satisfaction Scale, Everyday Discrimination Scale, Discrimination in the Medical Setting Scale, the Press Ganey and Jackson-Hogue-Phillip Scale
Training suggested include the Institute of Perinatal Quality Improvement (PQI) SPEAK UP Against Racism training, National Birth Equity Collaborative training, Harvard Implicit Association Test, Diversity Science, Cultural Maternity Care, March of Dimes and Office of Minority Health training
IRB approval was not obtained as the investigators determined this project was exempt based on published federal exemption categories.23 This investigator determination was based on expert interviews with human subjects not presenting greater than minimal risk to participants, the focus of the interview questions pertaining to their employment expertise and were not questions regarding their private or personal lives, and the project falling under the federal exemption category of benign behavioral intervention.
Results
Twenty-five interviews were completed with 28 participants from across the U.S. between May and August 2021. Thirteen states and Washington, D.C. were represented with nine of 25 participants (36.0%) being from Massachusetts. Other states represented included California, Texas, Oklahoma, Louisiana, Minnesota, Illinois, Georgia, Pennsylvania, Maryland, Rhode Island, and New York.
Seven themes for bundle measures were identified in the expert stakeholder discussion of implementing equity and equity-focused work in maternal health. They included the need for 1) data stratification by race, ethnicity and language, 2) performance of a readiness assessment, 3) culture shift toward equity, 4) inclusion of anti-racism and bias training, 5) addressing challenges of non-academic hospitals, 6) a life-course approach, and 7) selection of timing of implementation. Participants also named facilitators and barriers to conducting equity work during interviews (Box 1). Facilitators included supportive leadership, champions within institutions and departments, political will and support, financial incentives and funding, dedicated time, allies, community consultants, and dedicated students. Barriers included lack of buy-in, lack of funding, lack of allocation of resources and time, interpersonal racism, lack of compensation for this type of work, poor data infrastructure, and unsupportive leadership.
Box 1. Facilitators and Barriers of Maternal Equity Work.
Facilitators
Supportive leadership
Allies; Champions in institutions and departments
Timing around 2020 Racial Uprisings garnering nationwide support and attention
Funding, financial incentives
Political will and support from members of Congress
Dedicated time
Community consultants
Dedicated Students
Barriers
Lack of buy-in, from colleagues and leadership
Lack of funding, lack of compensation for this type of work
Lack of devotion of resources and time from hospital administration
Interpersonal racism
Lack of academic advancement for this type of work
Silos
Lack of data systems
Risk to reputation and litigation
Previous government administration
Data disaggregated by race, ethnicity, and language (REaL) was the most common theme discussed with 23 of 25 (92.0%) of the experts, including 60 comments across 25 interviews. Participants described the need for systems to regularly stratify process and outcome metrics by race, ethnicity, language, and insurance status. Recommendations were to regularly communicate these data to staff through clinical data dashboards. Clinical dashboards allow for rapid reporting of metrics disaggregated by REaL, demonstrate trends over time, and help identify opportunities for improvement by subpopulation. This functionality allows sites to sustain QI work beyond implementing measures for the statewide project. As part of this theme, data infrastructure itself was highlighted as necessary for implementation of the equity bundle. It was suggested that each department create its measures based on root cause analyses and stratify its data by REaL to determine what problems exist in their institution to address them directly.
Participants discussed the value of a readiness assessment conducted on each unit before implementation. Recommendations were to use a tool to assess the unit’s baseline culture of addressing racial inequities, leadership support, available resources and time, data access, and team dedication to bundle implementation. Measurement tools suggested by participants include the Atlas Readiness Assessment Tool and the Organizational Readiness for Implementing Change (ORIC) Survey which determines if organizations are supportive and have the tools necessary to create change.24 One participant suggested a question on clinician attribution to measure the level of clinician ownership of the work required to successfully address health inequities.25
Eight participants (32.0%) noted that by implementing structure measures for an equity bundle, one would change the institution’s culture toward one that emphasizes equity. This begins by having staff understand the historical context of racial inequities. The expected outcome of shifting culture is improvement in patient-reported experience measures. Patients may feel more integrated as contributing members of their healthcare team when included in shared-decision making and patient huddles.26 An additional goal of this bundle is to set a foundation for further equity work within participating institutions.
The majority of the experts (76.0%) discussed the importance of anti-racism and bias training as a measure for the equity bundle. Participants noted a need for increased awareness of bias on individual levels, both in the contemporary and historical context. Participants discussed various training options (see Table 1). Several named Respectful Maternity Care as a specific bias training that should be required in implementing this bundle. Some suggested specific respectful care policies guided by community input at each institution, such that patients give input on what respectful care means. Although many participants advocated for anti-bias training, 12.0% expressed concern for the efficacy of bias training.
Non-academic hospitals need to be involved in toolkit development and buy-in given they are a large proportion of birthing facilities in MA. These hospitals have different resources, trainee availability, and may serve different communities than academic hospitals. Engaging only with hospitals that have resource-rich settings would skew results and decrease the generalizability of the efficacy of the bundle.
Five participants (20.0%) noted the disconnect between data ascertained during birth hospitalization and peripartum data from the ambulatory setting. They noted that data ascertained during the birth hospitalization was more extensive than in the prenatal period, identifying an opportunity for improvement. They noted there is a need for better data collection throughout the life course beyond the reproductive periods. Participants also suggested including data on the social context of the birthing person. Suggested scales included the Index of Concentration at the Extremes and the Social Vulnerability Index.27,28
The racial justice movements against police violence in 2020 and the health inequities highlighted by COVID-19 have brought attention to improving health equity across fields of medicine. Participants reported that this work is more readily accepted now. One participant discussed that enhanced awareness occurred when people were incited by George Floyd’s murder, and many organizations donated time and funding to equity work that previously had not. Participants suggested community partnerships should be at the core of the work and included in each site equity team.
Twenty-six structure, process, and outcome measures were derived from literature review and interviews. The modified Delphi consensus process determined the ten measures selected for the Maternal Equity Bundle (Table 1). Structure measures, systems needed to implement the QI work to improve inequities, included (1) a formal and diverse equity team with community engagement, (2) equity goals developed and communicated (such as an anti-racism statement), (3) collection and availability of self-reported REaL data, and (4) implementation of a patient-reported experience measure (PREM). PREM Scales, the Mothers on Autonomy in Decision Making (MADM) and Mothers on Respect Index (MORi), were discussed and recommended by 10 of 25 experts (40.0%).29,30 Participants additionally suggested a qualitative option for the PREM, to yield greater context of the patient experiences.
Selected process measures are the process measures of the two previously implemented PNQIN bundles (severe hypertension and OB hemorrhage) with rates disaggregated by race and ethnicity. These include reporting percent of individual medical records with obstetric hemorrhage risk assessment score, percent of births utilizing a quantitative measurement of blood loss (QBL), and percent of patients receiving timely treatment for severe hypertension within 60 minutes of a sustained severe-range blood pressure measurement. In addition, a process measure was selected to report the percentage of staff trained in bias and respectful care. For full detail of the process measures, see Appendix 3, available online at http://links.lww.com/xxx. Comments for selecting these measures highlighted the feasibility of implementing familiar bundle measures with the addition of metrics for sub-populations reported.
The selected outcome measure was SMM (both SMM 20 and SMM 21 which included blood transfusion).31 Considerations for outcome measures included patient health outcomes and subjective experiences with the healthcare system during the perinatal period. The final measures suggested for implementing the Maternal Equity Bundle are included in Table 1.
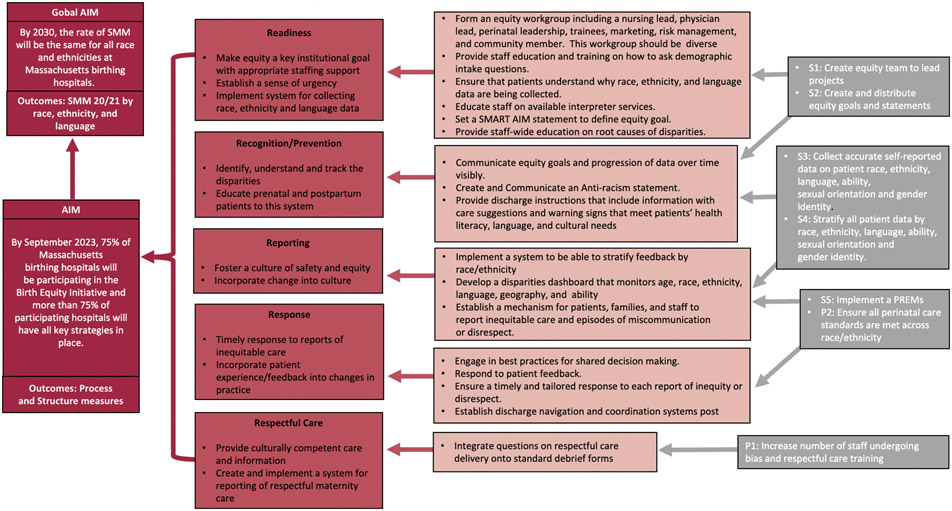
Themes from the stakeholder interviews are reflected in selected bundle measures: 1) equity-focused governance with community partnership, 2) antiracism and bias training, 3) demographic data collection by self-report and processes and outcomes stratified by REaL, and 4) a focus on patient experiences and optimal outcomes for all populations. These findings are presented in the resulting driver diagram depicted in Figure 1. A driver diagram is a visual display that organizes the project goals, proposed activities, and measures clearly outlining the relationship between the aim of the improvement project and the changes to be tested, implemented, and measured.32
Figure 1.
Driver diagram for the Massachusetts Maternal Equity Bundle. SMM, severe maternal morbidity; SMART, specific, measurable, applicable, realistic, and timely; PREM, patient-reported experience measure.
Discussion
We created a Maternal Equity Safety Bundle through a rigorous process of qualitative interviews and through utilization of the Delphi method to establish measures from an existing Conceptual Framework and Maternal Safety Consensus Bundle.18 Several themes, facilitators, barriers, and suggested measures emerged from our process to select and define measures for the PNQIN Maternal Equity Bundle, The most suggested activity for hospital teams to implement was data disaggregation by race and ethnicity highlighting broad interest among experts for teams to assess outcomes by subpopulations to target interventions. Reported facilitators and barriers informed the measures implemented, namely the unique barrier of interpersonal racism. The selected measures reflect an expert-recommended intention to shift practice and culture to achieve equity.
In response to a national call to action to address MM and SMM racial inequities, PNQIN began work to shift practice and culture to achieve equity. In 2019, PNQIN launched the MA AIM Initiative to build a culture of equity in obstetric care delivery and eliminate racism’s influence on birth experiences and outcomes. Our Maternal Equity Bundle development process sought to provide hospital teams with an infrastructure to improve equity based on tools to build awareness, provide training, and support measurement of outcomes to assess efficacy. These tools are designed to support teams engaging in informed discussions around racism in medical practice and dismantle the policies, procedures, and behaviors within their organizations that generate and perpetuate racial inequities.
From our process, we propose the following foundational components equity work: 1) prioritization from leadership, 2) antiracism and bias training, 3) data disaggregation by REaL, and 4) patient voice and community engagement. First, leadership support of equity as a core principle for the department and an overarching goal for the institution is a necessary step when implementing QI projects aimed at reducing racial inequities. Next, advancing bias awareness and training is a step toward changing the culture of the institution to acknowledge implicit bias and the role of structural inequities in the care they provide. As such, California has mandated Implicit Bias training for all perinatal care clinicians practicing in the state.33 In a study of Society for Maternal-Fetal Medicine members, 83% surveyed agreed that disparities affect their practice but only 29% believed that personal biases affect how they care for their patients.34 The importance of training discussed in the interviews was translated into creating a process measure of the percentage of nurses and physicians trained in antiracism and implicit bias. Third, self-report of demographic data collected by health systems is recommended to accurately document and identify outcomes and experiences by patient REaL.35,36 The MA Department of Public Health created a Racial Equity Data Road Map as a tool to inform hospitals on best practices for data collection, community engagement, and actionable solutions to improve racial equity.37 Lastly, a focus on patient experiences and outcomes stratified by race and ethnicity allows for teams to ensure respectful care is provided to all populations.38 Patient voice and community engagement are crucial to affecting change.
Experts offered lessons learned from implementation of equity work. Those who have implemented maternal equity projects in their institutions have reported experiences of defensiveness from colleagues and suggested an Appreciative Inquiry Approach that focuses on what the team was doing well, inquires how the problem has come to exist, and explores data collectively.39,40 The equity team leading this group must have staff representation of the populations served by the institution, including leadership in nursing and physician teams, on-the-ground nurses, residents, students, anesthesiologists, and pediatric teams. Members of site implementation teams need support to devote, discuss, and process this work, which requires dedicated time and staffing. The expert stakeholders interviewed suggested a stepwise approach to implementing the bundle, starting with recognition and structure measures.
The strengths of our process include the mixed method approach and reach of expertise among the stakeholders interviewed, resulting in a wide range of proposed measures and the ability to discuss what existing measures lack. We also incorporated direct feedback from stakeholders regarding the bundle, which made it more feasible to implement.
Limitations of this qualitative approach include the subjective nature of interviewee comments and the consensus process among workgroup members. Further, the stakeholder interviews did not include representatives of patient advocacy groups and demographic statistics of the experts interviewed were not collected. While the Maternal Equity Bundle Workgroup includes patient representatives and stakeholders from urban and rural hospitals and academic and community settings, it is difficult to account for the wide variety of experiences in MA and may not adequately address geographic variations across the state. The Maternal Equity Bundle created is best suited for implementation in MA but could be adapted for other states in the U.S. However, hospitals and PQCs should consider the contextual similarities to determine how generalizable the findings will be to their setting.
The PNQIN Maternal Equity Bundle was implemented across MA in September 2022. Next steps include the evaluation of efficacy, feasibility, and acceptability of the bundle implementation process, and initial evaluation results will be incorporated for future versions of the equity bundle.
Supplementary Material
Acknowledgements
The authors thank the Massachusetts Department of Public Health Bureau of Family Health and Nutrition, National Institutes of Health National Institute on Minority Health and Health Disparities (NIHMD), members of the Reducing Racial Disparities in Maternal Morbidity post COVID19: Assessing the Integration of Maternal Safety Bundles and Community-Based Doulas to Improve Outcomes for Black Women (Be A Mom Study), the members of the Perinatal Neonatal Quality Improvement Network of Massachusetts (PNQIN) Equity Bundle Workgroup and those interviewed for their contribution in the development of the PNQIN Maternal Equity Bundle. The content is solely the responsibility of the authors and does not necessarily represent the official views of the acknowledged agencies. Funders had no role in the preparation of this manuscript.
Funding
This work was supported by the Miller Family Fund Award for Research in Reproductive Health and Family Planning at Tufts University School of Medicine for AK and the National Institutes of Health (NIMHD) Award Number 1R01MD016026-01 1 for HD, AM, EL and NAO.
Footnotes
Financial Disclosure
Chloe Zera reports money was paid to her institution from Ariadne Labs/Harvard School of Public Health and the CVS Health Foundation. Julianne Lauring reports receiving payment from GSK Pharmaceutical. Andrew Healy reports Baystate Medical Center has received money for his participation in the state quality collarborative (PNQIN) (approximately $10,000/ year). Audra R. Meadows reports receiving payment from the Institute for Healthcare Improvement, Institute for Perinatal Quality Improvement, and the March of Dimes. She has received consulting support to the CMQCC or California Maternal Quality Care Collaborative. The other authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
The authors’ Positionality Statement is available online at http://links.lww.com/xxx.
References
- 1.Thoma ME, Declercq ER. Changes in Pregnancy-Related Mortality Associated With the Coronavirus Disease 2019 (COVID-19) Pandemic in the United States. Obstet Gynecol. 2023;Publish Ahead of Print. doi: 10.1097/AOG.0000000000005182 [DOI] [PubMed] [Google Scholar]
- 2.Health, United States, Annual Perspective, 2020-2021. National Center for Health Statistics (U.S.); 2022. doi: 10.15620/cdc:122044 [DOI] [PubMed] [Google Scholar]
- 3.Chinn JJ, Eisenberg E, Artis Dickerson S, et al. Maternal mortality in the United States: research gaps, opportunities, and priorities. Am J Obstet Gynecol. 2020;223(4):486–492.e6. doi: 10.1016/j.ajog.2020.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–1036. doi: 10.1097/aog.0b013e31826d60c5 [DOI] [PubMed] [Google Scholar]
- 5.Diop H, Declercq ER, Liu CL, et al. Trends and inequities in severe maternal morbidity in Massachusetts: A closer look at the last two decades. PLOS ONE. 2022;17(12):e0279161. doi: 10.1371/journal.pone.0279161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howell EA. Reducing Disparities in Severe Maternal Morbidity and Mortality: Clin Obstet Gynecol. Published online January 2018:1. doi: 10.1097/GRF.0000000000000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell EA, Ahmed ZN. Eight steps for narrowing the maternal health disparity gap: Step-by-step plan to reduce racial and ethnic disparities in care. Contemp ObGyn. 2019;64(1):30–36. [PMC free article] [PubMed] [Google Scholar]
- 8.Greenberg MB, Gandhi M, Davidson C, Carter EB. Society for Maternal-Fetal Medicine Consult Series #62: Best practices in equitable care delivery–Addressing systemic racism and other social determinants of health as causes of obstetrical disparities. Am J Obstet Gynecol. 2022;227(2):B44–B59. doi: 10.1016/j.ajog.2022.04.001 [DOI] [PubMed] [Google Scholar]
- 9.Deyrup A, Graves JL. Racial Biology and Medical Misconceptions. N Engl J Med. 2022;386(6):501–503. doi: 10.1056/NEJMp2116224 [DOI] [PubMed] [Google Scholar]
- 10.Henderson ZT, Ernst K, Simpson KR, et al. The National Network of State Perinatal Quality Collaboratives: A Growing Movement to Improve Maternal and Infant Health. J Womens Health. 2018;27(3):221–226. doi: 10.1089/jwh.2018.6941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Main EK. Reducing Maternal Mortality and Severe Maternal Morbidity Through State-based Quality Improvement Initiatives. Clin Obstet Gynecol. 2018;61(2):319–331. doi: 10.1097/GRF.0000000000000361 [DOI] [PubMed] [Google Scholar]
- 12.Mahoney J. The Alliance for Innovation in Maternal Health Care: A Way Forward. Clin Obstet Gynecol. 2018;61(2):400–410. doi: 10.1097/GRF.0000000000000363 [DOI] [PubMed] [Google Scholar]
- 13.Alliance for Innovation on Maternal Health. Measurement of Respectful Care in AIM Statement. Published online October 21, 2021. https://saferbirth.org/wp-content/uploads/2021_10_21-Statement-on-Measurement-of-Resepctful-Care-in-AIM_.pdf
- 14.Main EK, Markow C, Gould J. Addressing Maternal Mortality And Morbidity In California Through Public-Private Partnerships. Health Aff (Millwood). 2018;37(9):1484–1493. doi: 10.1377/hlthaff.2018.0463 [DOI] [PubMed] [Google Scholar]
- 15.Main EK, Chang SC, Dhurjati R, Cape V, Profit J, Gould JB. Reduction in racial disparities in severe maternal morbidity from hemorrhage in a large-scale quality improvement collaborative. Am J Obstet Gynecol. 2020;223(1):123.e1–123.e14. doi: 10.1016/j.ajog.2020.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamm RF, Howell E, James A, et al. Implementation and outcomes of a system-wide women’s health ‘team goal’ to reduce maternal morbidity for black women: a prospective quality improvement study. BMJ Open Qual. 2022;11(4):e002061. doi: 10.1136/bmjoq-2022-002061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davidson C, Denning S, Thorp K, et al. Examining the effect of quality improvement initiatives on decreasing racial disparities in maternal morbidity. BMJ Qual Saf. Published online April 15, 2022:bmjqs-2021-014225. doi: 10.1136/bmjqs-2021-014225 [DOI] [PubMed] [Google Scholar]
- 18.Howell EA, Brown H, Brumley J, et al. Reduction of Peripartum Racial and Ethnic Disparities: A Conceptual Framework and Maternal Safety Consensus Bundle. Obstet Gynecol. 2018;131(5):770–782. doi: 10.1097/AOG.0000000000002475 [DOI] [PubMed] [Google Scholar]
- 19.Zoom. Accessed December 4, 2022. https://zoom.us/
- 20.Dedoose. Accessed December 4, 2022. https://www.dedoose.com/
- 21.Donabedian A. Evaluating the Quality of Medical Care. Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niederberger M, Spranger J. Delphi Technique in Health Sciences: A Map. Front Public Health. 2020;8. Accessed January 23, 2023. https://www.frontiersin.org/articles/10.3389/fpubh.2020.00457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Exemptions (2018 Requirements). 46.104 Code of federal Regulations. Department of Health and Human Services. 2018. Accessed April 24, 2023. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/common-rule-subpart-a-46104/index.html [Google Scholar]
- 24.Shea CM, Jacobs SR, Esserman DA, Bruce K, Weiner BJ. Organizational readiness for implementing change: a psychometric assessment of a new measure. Implement Sci. 2014;9(1):7. doi: 10.1186/1748-5908-9-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arrington LA, Edie AH, Sewell CA, Carter BM. Launching the Reduction of Peripartum Racial/Ethnic Disparities Bundle: A Quality Improvement Project. J Midwifery Womens Health. 2021;66(4):526–533. doi: 10.1111/jmwh.13235 [DOI] [PubMed] [Google Scholar]
- 26.Weiseth A, Plough A, Aggarwal R, et al. Improving communication and teamwork during labor: A feasibility, acceptability, and safety study. Birth. 2022;49(4):637–647. doi: 10.1111/birt.12630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cutter SL, Boruff BJ, Shirley WL. Social Vulnerability to Environmental Hazards*. Soc Sci Q. 2003;84(2):242–261. doi: 10.1111/1540-6237.8402002 [DOI] [Google Scholar]
- 28.Massey D. Residential segregation and neighborhood conditions in US metropolitan areas. In: America Becoming: Racial Trends and Their Consequences. Vol 1. 1. ; 2001:391–434. [Google Scholar]
- 29.Vedam S, Stoll K, Martin K, et al. The Mother’s Autonomy in Decision Making (MADM) scale: Patient-led development and psychometric testing of a new instrument to evaluate experience of maternity care. PloS One. 2017;12(2):e0171804. doi: 10.1371/journal.pone.0171804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vedam S, Stoll K, Rubashkin N, et al. The Mothers on Respect (MOR) index: measuring quality, safety, and human rights in childbirth. SSM - Popul Health. 2017;3:201–210. doi: 10.1016/j.ssmph.2017.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Severe Maternal Morbidity in the United States. Reproductive Health, Centers for Disease Control and Prevention (CDC). Published February 2, 2021. Accessed April 20, 2023. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
- 32.Driver Diagram. Tools, Institute for Healthcare Improvement. Accessed April 20, 2023. https://www.ihi.org/resources/Pages/Tools/Driver-Diagram.aspx
- 33.SB-464 California Dignity in Pregnancy and Childbirth Act.; 2019. Accessed April 3, 2023. https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201920200SB464
- 34.Moroz L, Riley LE, D’Alton M, et al. SMFM Special Report: Putting the “M” back in MFM: Addressing education about disparities in maternal outcomes and care. Am J Obstet Gynecol. 2018;218(2):B2–B8. doi: 10.1016/j.ajog.2017.11.592 [DOI] [PubMed] [Google Scholar]
- 35.Magaña López M, Bevans M, Wehrlen L, Yang L, Wallen GR. Discrepancies in Race and Ethnicity Documentation: a Potential Barrier in Identifying Racial and Ethnic Disparities. J Racial Ethn Health Disparities. 2017;4(5):812–818. doi: 10.1007/s40615-016-0283-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boehmer U, Kressin NR, Berlowitz DR, Christiansen CL, Kazis LE, Jones JA. Self-Reported vs Administrative Race/Ethnicity Data and Study Results. Am J Public Health. 2002;92(9):1471–1472. doi: 10.2105/AJPH.92.9.1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manning SE, Blinn AM, Selk SC, et al. The Massachusetts Racial Equity Data Road Map: Data as a Tool Toward Ending Structural Racism. J Public Health Manag Pract. 2022;28(Supplement 1):S58–S65. doi: 10.1097/PHH.0000000000001428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shakibazadeh E, Namadian M, Bohren M, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG Int J Obstet Gynaecol. 2018;125(8):932–942. doi: 10.1111/1471-0528.15015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barrett FJ, Fry RE. Appreciative Inquiry: A Positive Approach to Building Cooperative Capacity. 1st ed. Taos Institute Publications; 2005. [Google Scholar]
- 40.Arrington LA. The 5D Cycle for Health Equity: Combining Black Feminism, Radical Imagination, and Appreciative Inquiry to Transform Perinatal Quality Improvement. J Midwifery Womens Health. 2022;67(6):720–727. doi: 10.1111/jmwh.13418 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.