Abstract
Introduction:
Health care procedures including cancer screening and diagnosis were interrupted due to the COVID-19 pandemic; The extent of this impact on cancer care in the U.S. is not fully understood. We investigated pathology report volume as a reflection of trends in oncology services pre-pandemic and during the pandemic.
Methods:
Electronic pathology reports were obtained from 11 U.S. central cancer registries from NCI’s SEER Program. The reports were sorted by cancer site and document type using a validated algorithm. Joinpoint regression was used to model temporal trends from January 2018-February 2020, project expected counts from March 2020-February 2021 and calculate observed-to-expected ratios. Results were stratified by sex, age, cancer site and report type.
Results:
During the first three months of the pandemic, pathology report volume decreased by 25.5% and 17.4% for biopsy and surgery reports, respectively. The 12-month O/E ratio (Mar 2020-Feb 2021) was lowest for women (O/E 0.90) and patients 65 yrs. and older (O/E 0.91) and lower for cancers with screening (melanoma skin, O/E 0.86; breast, O/E 0.88; lung O/E 0.89, prostate, O/E 0.90; colorectal, O/E 0.91) when compared to all other cancers combined.
Conclusions:
These findings indicate a decrease in cancer diagnosis, likely due to the COVID-19 pandemic. This decrease in the number of pathology reports may result in a stage shift causing a subsequent longer-term impact on survival patterns.
Impact:
Investigation on the longer-term impact of the pandemic on pathology services is vital to understand if cancer care delivery levels continue to be affected.
Keywords: COVID-19, Pandemic, Cancer Surveillance, Pathology Volume, Cancer Care
Introduction
As of November 8th, 2022, almost three years after the first COVID-19 case diagnosed in the U.S., over 97.6 million Americans had been diagnosed with COVID-19 and over 1 million people had died (https://covid.cdc.gov/covid-data-tracker). In March 2020, states began implementing closures and restrictions,1 which likely had a profound, unprecedented impact on healthcare system access and utilization, including cancer care in the U.S.2,3 Individuals with compromised immune systems were at high risk for severe COVID-19 illness and were recommended to shelter in place.4–6 Several professional public health and cancer organizations recommended that non-emergent patient visits, including cancer screenings, be paused.7–9 Surgical interventions were delayed and treatment protocols were adjusted in order to redirect limited healthcare resources, such as personal protective equipment and personnel, from cancer services to pandemic response.3,5,10 As a result, there were interruptions in cancer screenings and treatment, that may have delayed diagnosis and resulted in more advanced stages at diagnosis, worse clinical outcomes, and a downstream impact on survival.11–15 The longer these changes in cancer care delivery persist, the greater the likelihood they could have a substantial negative impact on the decades of progress in decreasing cancer mortality.16
It is well documented that the pandemic led to decreases in cancer screening,9,14,17–19 diagnosis,8,12,15,20–23, treatment,15,24 and patient encounters.25 However, not enough is known about the magnitude and duration of its impact on cancer outcomes and this is reflected in the lack of published data reported by U.S. cancer surveillance systems.26 This study leveraged the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program’s near real time pathology reporting to monitor changes in pathology report volume as a measure of shifts in oncology-related diagnostic procedures (e.g., biopsies) or definitive surgical treatment (e.g., resections). These changes in report volume are a direct reflection of the number of new cancer cases diagnosed. Results are based on SEER pathology report volume across 11 U.S. geographic areas and are stratified by pathology report type and by five major cancer sites (colon/rectum, female breast, lung, melanoma skin [melanoma], and prostate) from January 2018 through December 2021.
Materials and Methods
Selection Criteria
Central cancer registries participating in the SEER Program receive electronic pathology reports in near real-time. Reporting requirements vary by jurisdiction but did not change during the COVID-19 pandemic. Non-reportable tumors or non-cancer diagnosis were filtered out with the remaining reports being automatically matched against the registry database and coded for basic registration elements such as tumor site, laterality, histology and behavior. Electronic pathology reports for 11 population-based cancer registries (CT, GA, HI, IA, KY, LA, NJ, NM, NY, SEA, UT) received between January 2018 and December 2021 were included in this study (N=3,185,808). All pathology reports had complete information on sex, age, cancer site, and report type. Pathology reports were excluded due to inconsistent reporting (N=1,071,212), incomplete, invalid information or male breast cancer report (N=20,833) and/or variability in report volume (N=200,699). Consistent reporting was defined as facilities that reported at least one pathology report per month across the entire study period. Male breast cancer reports were excluded due to its different clinical presentation (e.g., unlikely to be screen-detected) and small number of reports. Variability in report volume was defined as an increase of 95% or greater in report volume from 2018 to 2019 for a given facility. These exclusions were implemented to restrict the analysis to facilities that were consistently reporting and to reduce the impact of factors unrelated to the COVID-19 pandemic, such as facility closures or mergers, on pathology report volume.
Data Processing
Pathology reports were processed via a deep learning Natural Language Processing (NLP) algorithm developed in collaboration with Oak Ridge National Laboratory under the Department of Energy Laboratories National Cancer Institute Collaboration. This algorithm was implemented as an application programming interface (API) that classified reports by the site and histology of primary tumor (female breast, lung, colon/rectum, melanoma, and prostate).27 A second API was developed that classified reports by report type including: biopsy, cytology, molecular & biomarker, surgical resection, and other. The “Other” category includes blood/bone marrow/flow cytometry, autopsy and none previously mentioned. Pathology report types differ based on the type of tissue specimen that was removed, extraction method, and quantity removed. Not all reports include the same amount of information.
Statistical Analysis and Modeling
To compare pre-pandemic and pandemic pathology report volume, biweekly pathology report volume frequencies were compared for two periods: pre-pandemic and pandemic. The average of the sum of pathology reports during March, April, and May of 2018 and 2019 (pre-pandemic) were compared to the sum of pathology reports during March, April, and May of 2020 (pandemic) for all cancer sites combined by sex, age, and report type. The change in counts for pre-pandemic reports (based on 12 biweekly data points) versus pandemic reports (based on 6 biweekly data points) was tested for significance using t-test with unequal variance.
To calculate the expected number of pathology reports, a Joinpoint regression model (v4.9.1.0) (https://surveillance.cancer.gov/joinpoint/) was used to model temporal trends from January 2018 through February 2020, for a total of 26 months, and the model was then extended to project the pathology report volume. The Joinpoint regression model, developed by the National Cancer Institute, has been widely used to analyze and identify cancer trend changes. The model is composed of piecewise linear segments joined by change points. The pathology report volume was recorded at the middle of the month and on the last day of each month. The Joinpoint model was applied to the 26 months of data, assuming a log-linear model with Poisson count. Because the model is in log-scale, the slope of a segment corresponds to monthly percent change in the pathology report volume in that segment. The slope of the last segment was used to project the expected pathology report volume for the next 12 months (March 2020 to February 2021) during the pandemic. The model was fitted using the default setting of the Joinpoint software. The data was also refitted using the Joinpoint model with first order autocorrelation and results were close to that from the model without incorporating auto-correlation.
We calculated and adjusted the expected counts for the difference in the number of days in each calendar month. We further calculated the observed to expected ratio by month and stratified by sex, age, cancer site, and report type. The standard errors for the ratios were obtained by the delta method,28 which was used to determine the p-value and 95% confidence interval for each O/E ratio.
Data Availability
The raw data for this study is not routinely collected by NCI SEER since pathology reports contain personally identifiable information. The data could be made available upon written request to each participating SEER cancer registry and their approval.
Results
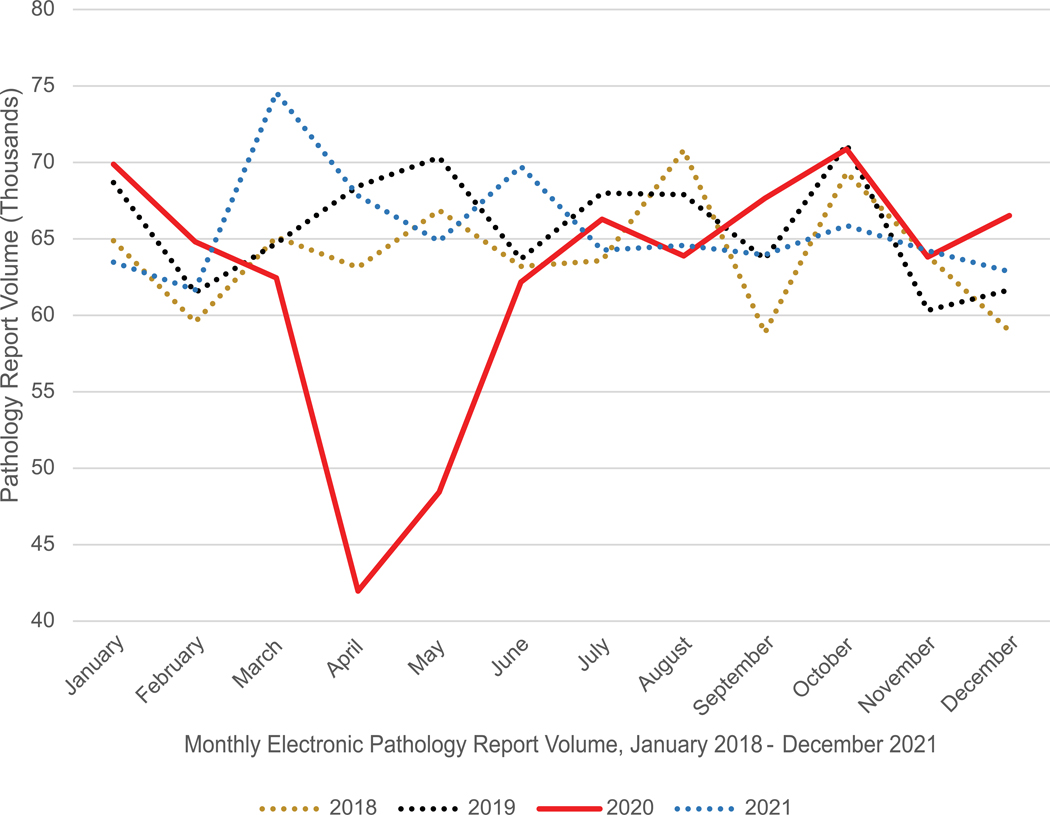
Figure 1 shows the monthly trends for pathology results received from January 2018 through December 2021. Pathology report volume was similar in January and February for all three years (2018 to 2020) representing a pre-pandemic baseline, ranging from 59,570 to 69,833 reports. The lowest report volume occurred in April and May 2020 (41,960 and 48,425, respectively) compared to all other months in the study period. Pathology report volume dropped by 32.8% from March 2020 to April 2020. The largest number of pathology reports (75,000) was in March 2021. Pathology report volume in 2020 was also compared to the volume of COVID-19 cases by geographic region and month. This is provided in Supplementary Figure 1.
Figure 1:
Monthly Electronic Pathology Report Volume, January 2018 – December 2021 (11 SEER Registries, >3 million reports).
The average of the sum of pathology reports during March to May of 2018 and 2019 (pre-pandemic period) was compared to the sum of pathology reports during March to May 2020 (pandemic period). For all cancer sites combined, the comparisons showed a significant decrease in report volume among males, females, every age group, and every report type (Table 1). The decrease was slightly larger among females (−24.9%) than males (−21.2%). The decrease was similar across age categories but slightly larger among the oldest age category, ranging from 21.5% among patients 65 to 74 years of age to 25.5% among patients 75 years of age or older. The decrease in pathology report volume varied by report type between the pandemic and pre-pandemic periods, with biopsy and cytology reports for all cancer sites combined decreasing by 25.5% and 25.7%, respectively. In comparison, surgical pathology reports decreased by only 17.4% (Table 1). Additional data by cancer site is provided in Supplementary Table S1.
Table 1.
Pre-pandemic vs. Pandemic Pathology Report Volume in 11 SEER Registries, All Cancer Sites Combined.
| Characteristic | Level | Pre-pandemic Count | Pandemic Count | % Change | 95% CI |
|---|---|---|---|---|---|
| Sex | Male | 84,779 | 66,813 | −21.2 | −20.9: −21.5 |
| Female | 114,483 | 86,019 | −24.9 | −24.6: −25.1 | |
| Age (Yrs.) | < 50 | 34,443 | 26,646 | −22.6 | −22.2: −23.1 |
| 50–64 | 66,174 | 50,405 | −23.8 | −23.5: −24.2 | |
| 65–74 | 57,827 | 45,385 | −21.5 | −21.2: −21.9 | |
| ≥ 75 | 40,818 | 30,396 | −25.5 | −25.1: −25.8 | |
| Report Type | Biopsy | 112,152 | 83,552 | −25.5 | −25.2: −25.8 |
| Surgery | 37,094 | 30,645 | −17.4 | −17.0: −17.8 | |
| Cytology | 21,541 | 16,006 | −25.7 | −25.1: −26.3 | |
| Mol/Bio | 5,873 | 4,400 | −25.1 | −24.0: −26.2 | |
| Othera | 22,604 | 18,229 | −19.4 | −18.8: −19.9 |
– Other report type includes blood/bone marrow/flow cytometry, autopsy, and none of the above
Note: Pre-pandemic is defined as the average of the sum of pathology reports during March, April, and May of 2018 and 2019 (pre-pandemic). Pandemic is defined as the sum of pathology reports during March, April, and May of 2020.
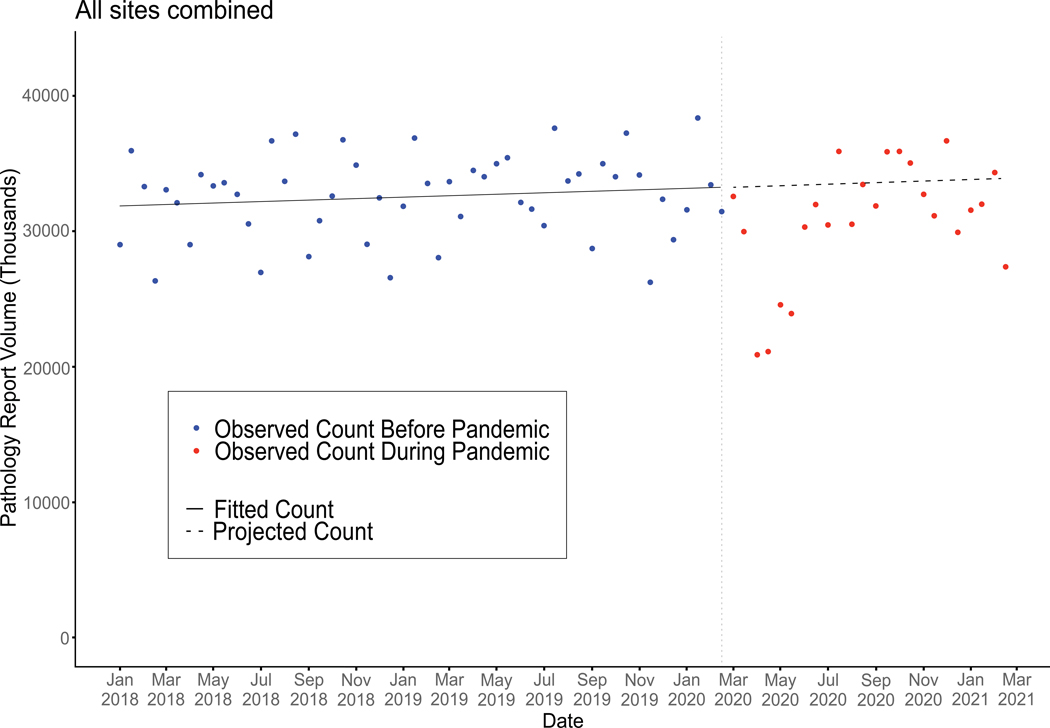
Figure 2 shows results of the Joinpoint model for all cancer sites combined before (January 2018 through February 2020) and during (March 2020 through February 2021) the pandemic. The blue and red data points around the horizontal line indicate the observed biweekly frequency of electronic pathology reports before and during the pandemic, respectively. The solid portion of the horizontal line shows the fitted pathology report counts before the pandemic while the dashed portion to the right of the vertical line shows the expected values of electronic pathology reports in the absence of the pandemic. The expected volume of pathology reports based on the solid and dotted lines shows a consistently increasing trend across the period. However, the observed volumes are inconsistent with the expected trend, especially during the first 3 months of the pandemic (March to May 2020).
Figure 2:
Observed and Modeled Volume of Bi-Monthly Electronic Pathology Report for All Cancer Sites Combined, January 2018 – February 2021 from 11 SEER Registries (> 3 million reports).
This figure shows the observed counts based on more than 3 million pathology reports from 11 registries, as well as the projected counts, for all cancer sites combined. The solid-line, representing the fitted model, passes through the observed data with symmetric residuals. The dash-line is the projection count. Each month has two data points.
Results from the Joinpoint model were used to calculate the observed to expected ratios of the pathology report volume during the pandemic from March 2020 through February 2021 (Table 2). An O/E ratio equal to 1 implies that the observed count does not differ from the expected based on data from previous years. An O/E ratio less than 1 implies that there were fewer observed than expected counts. For biopsies and surgical resections, the observed to expected ratios of pathology reports were less than 1 for both sexes, all ages, and each of the five cancer sites (p<0.05). However, the observed to expected ratios were greater than 1 (p<0.05) for: cytology reports for colon/rectum; molecular/biomarker reports for colorectal, lung, melanoma, and prostate cancers; and “other” types of reports for melanoma. Observed to expected ratios of biopsy, surgical, cytology, and molecular/biomarker reports were similar across age groups and sexes. The lowest ratio observed was for “other” pathology reports for lung and prostate cancers (0.72 for each), while the highest ratio (4.44) was for molecular/biomarker reports for prostate cancer.
Table 2.
Observed (March 2020 – February 2021) vs. Expected (March 2020 – February 2021) Pathology Report Volume in 11 SEER Registries.
| Biopsy | Surgical | Cytology | Molecular/Biomarkers | Otherb | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observed | O/E | Observed | O/E | Observed | O/E | Observed | O/E | Observed | O/E | Observed | O/E | ||
| Sex | Male | 173341 | 0.93 * | 52346 | 0.89 * | 37346 | 0.97 * | 6564 | 1.07 * | 46821 | 0.99 | 316418 | 0.94 * |
| Female | 243046 | 0.89 * | 84516 | 0.89 * | 40518 | 0.96 * | 14677 | 1.01 | 39912 | 0.92 * | 422669 | 0.90 * | |
| Age (Yrs.) | < 50 | 62712 | 0.92 * | 26985 | 0.89 * | 11935 | 0.92 * | 4126 | 1.05 * | 17165 | 0.96 * | 122923 | 0.93 * |
| 50–64 | 135240 | 0.91 * | 48469 | 0.89 * | 23294 | 0.99 | 7050 | 1.09 * | 25024 | 0.95 * | 239077 | 0.92 * | |
| 65–74 | 127446 | 0.90 * | 39174 | 0.89 * | 23052 | 0.97 * | 5869 | 0.98 | 25402 | 0.98 | 220943 | 0.91 * | |
| ≥ 75 | 90989 | 0.90 * | 22234 | 0.90 * | 19583 | 0.94 * | 4196 | 0.97 | 19142 | 0.92 * | 156144 | 0.91 * | |
| Primary Site | Colorectal | 28740 | 0.89 * | 22307 | 0.92 * | 1427 | 1.15 * | 1809 | 1.10 * | 414 | 0.86 * | 54697 | 0.91 * |
| Female Breast | 120974 | 0.88 * | 31024 | 0.89 * | 5063 | 0.96 | 8228 | 1.01 | 6484 | 0.82 * | 171773 | 0.88 * | |
| Lung | 38321 | 0.87 * | 9425 | 0.80 * | 23838 | 0.95 * | 2996 | 1.26 * | 634 | 0.72 * | 75214 | 0.89 * | |
| Melanoma | 41327 | 0.85 * | 807 | 0.99 | 885 | 0.94 | 193 | 1.36 * | 286 | 2.38 * | 43498 | 0.86 * | |
| Prostate | 40044 | 0.90 * | 10536 | 0.87 * | 359 | 0.95 | 191 | 4.44 * | 242 | 0.72 * | 51372 | 0.90 * | |
| All Othersa | 146981 | 0.96 * | 62763 | 0.90 * | 46292 | 0.96 * | 7824 | 1.02 | 78673 | 0.98 * | 342533 | 0.95 * | |
(p<0.05)
– All other cancer sites reportable to cancer registries
– Other report type includes blood/bone marrow/flow cytometry, autopsy, and none of the above
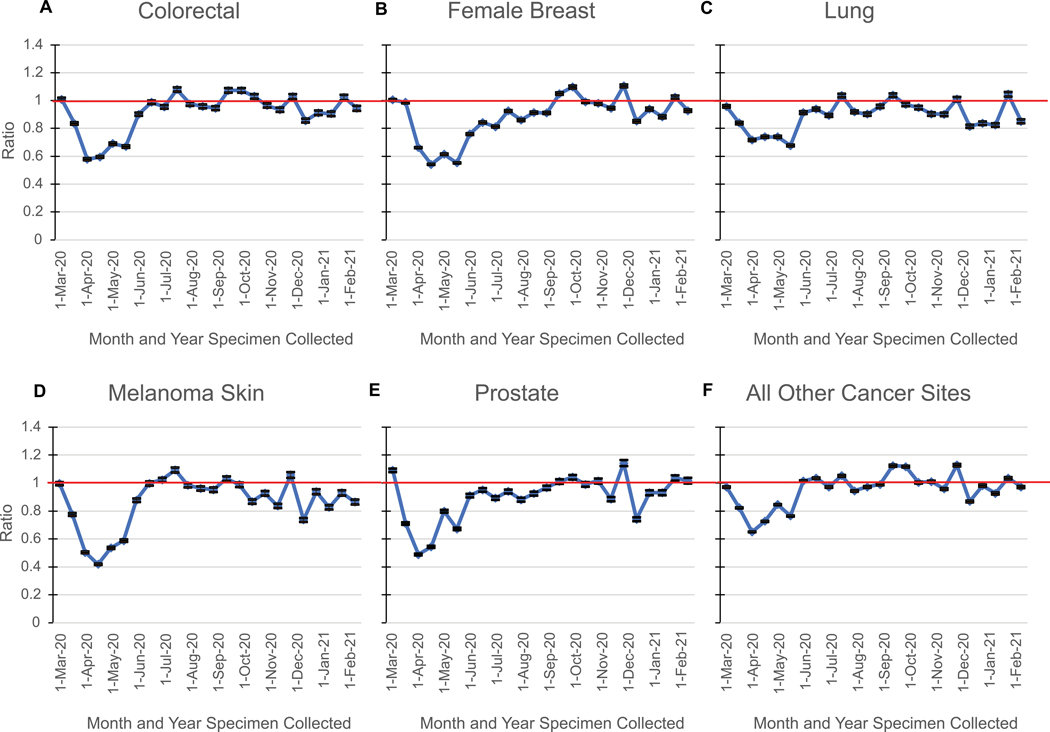
As shown in Figure 3, the O/E ratios by cancer site demonstrate pattern variation for both the magnitude of the decline and the subsequent increase to approach expected over time. The O/E ratios for each of the five cancer sites decreased starting in the second half of March 2020, except for female breast cancer reports, whose decrease did not begin until April 2020. During the latter half of March 2020, melanoma had the lowest O/E ratio (0.4) of any of the five cancer sites, while lung cancer maintained the highest O/E ratio (0.7). The return to the expected, or baseline, was delayed for breast and prostate cancers; they did not return to the expected until October 2020. A small “rebound” (O/E>1) was observed in September and October 2020, mainly for colorectal (1.07), breast (1.09) and “All Other” cancers (1.1). A second period of moderate reduction in monthly O/E was observed starting in late December 2020.
Figure 3:
Observed to Expected Ratio, by Cancer Site, Month and Year of Diagnosis
The observed 2020 count was compared to the expected count by ratio (O/E ratio) from March 2020-February 2021. The standard error for the ratio was obtained by the delta method, which was used to determine the p-value and 95% confidence interval for each O/E ratio. Horizontal solid line depicts an O/E ratio of 1.
Discussion
This is the first study to report on changes in the volume of pathology reports on a geographically defined population basis during the first two calendar years of the COVID-19 pandemic (2020–2021) in the U.S. Our investigation provides evidence of disruptions in cancer diagnosis, staging, and surgical oncology services when stay at home orders and changes in clinical guidelines were enacted throughout the U.S. at the start of the pandemic in March 2020. As anticipated with the changes in guidelines from the American Society of Clinical Oncology29 and the American College of Surgeons30, the number of pathology reports decreased overall and by cancer site. While there was some rebound or catch-up, the pathology report volume has yet to achieve the expected volume based on modeled trends.
In examining changes in electronic pathology report volume by month, the lowest observed volume occurred in April 2020 (41,960) while the highest observed volume occurred in March 2021 (74,564) (Figure 1). The increase during this period suggests a potential rebound or “catch up” in cancer-related procedures to compensate for the prior observed deficit early in the pandemic. In addition to the pathology report volume, we examined the ratio of the observed to expected longitudinal trends across the study period (Figure 3). The O/E ratio began to return to pre-pandemic levels (O/E > 1.0) in July 2020, with the exception of breast and prostate cancers, where the increase in ratio was delayed until October. When we compared the volume of pathology reports with COVID-19 case counts for six SEER registries, we observed a sharp decline in pathology reports in the Spring of 2020 but not in the Summer or Fall (SF 1). On the other hand, SF1 showed COVID-19 case surges differ slightly temporally when stratified geographically. The first wave of COVID-19 cases occurred in April of 2020 in the Northeast region and July of 2020 in the Southern region. The largest increase in COVID-19 cases occurred in the Fall of 2020 for both regions while pathology report volume remained relatively consistent during this time. This suggests that the decline in pathology reports in April 2020 are likely due to when recommendations from health organizations and governmental agencies were released.29,30 It was suggested all elective surgeries and non-medical procedures such as cancer screenings be suspended due to the COVID-19 outbreak. Stay at home orders may have also contributed to the decline in pathology reports with patients canceling or rescheduling in-person medical visits.31
During the first three months of the pandemic, the observed reduction in biopsy services was similar to the observed reduction in cytology and molecular testing but larger than the observed reduction in surgical pathology services. This likely reflects continuation of scheduled surgical procedures related to definitive treatment as opposed to diagnostic procedures resulting from cancer screening (Table 1). Detailed percent changes by cancer site are shown in Supplemental Table 1.
This study leveraged statistical models to generate expected pathology report volumes in the absence of the pandemic. These expected volumes provide the longitudinal perspective of cancer care services (Figure 3; Table 2), allowing us to examine the O/E ratios across the 12-month periods. We found that overall, among males, the reduction in surgical pathology reports was greater than the reduction in biopsy reports, and there was no difference among females (Table 2). This observation may be attributable to a decrease in the number of biopsies, resulting in fewer diagnosed cases and therefore fewer cases recommended for surgical oncology services. Alternatively, this finding could be explained by delays in surgery scheduling or by changes in treatment modalities from surgery to radiation and/or systemic therapy.
During the pandemic period, we observed more molecular reports than expected on a 12-month basis (Table 2). This may have been driven by the increase in utilization of prognostic scores for prostate, lung, and melanoma cancers. The penetrance of molecular testing appeared to slow for a short period in early 2022 but to rebound forcefully in late 2022.32,33
The indirect impact of the pandemic is extensive and is observed from March 2020 to February 2021, through a lower-than-expected pathology report volume. With O/E ratios below 1 across sex and age groups, there is evidence that all demographic groups were impacted by the pandemic and experienced fewer than expected cancer diagnostic and definitive surgical procedures for all cancer sites examined. A previous study similarly found a 10% decline in pathology report volume in Georgia and Louisiana in 2020, indicating a decrease in cancer diagnoses and surgical treatment as a result of the pandemic.26 There was a higher impact among women which is clearly shown when the absolute number of pathology reports are compared three months before versus three-months post-pandemic (−21.2% female, −24.9% male). The analysis of O/E ratios shows the differential impact by sex was more severe in relation to biopsy procedures (0.89 female, 0.93 male) and was not observed for surgical procedures (0.89 female; 0.89 male). There is no strong evidence for gender-related differences in the rate of initial colorectal screening between males and females.34 However, based on pre-pandemic data more women are eligible and undergo cancer screening for breast, cervical and/or colorectal cancer than eligible men for colorectal cancer.35 Thus, recommendations to temporarily suspend screening coupled with the population proportion eligible for screening could explain the gender-related differential impact we report in this analysis of biopsy pathology reports.
Figure 3 illustrates that the observed to expected ratios between March 2020 and May or June 2020 decreased across all cancer sites at the start of the pandemic and were lowest in April 2020. O/E ratios were the lowest for melanoma and prostate cancer in April 2020, demonstrating a differential impact of the pandemic according to cancer site. Similarly, Chen et al. reported a cancer screening deficit for breast, colorectal, and prostate cancer in the US between March and May 2020 based on their analysis of administrative claims data and enrollment information covering approximately 60 million people.17
The correlation between when stay at home orders and changes in clinical guidelines were put in place and when a decrease in pathology report volume was observed, particularly among screen-detected cancers, suggests that this disruption had a larger effect in cancers with screening. Using modeling validated by the Cancer Intervention and Surveillance Modeling Network, Alagoz et al. predicted that COVID-19-related disruptions in cancer care will have a long-term cumulative impact on cancer mortality.36 However, some authors reported that changes in cancer care experienced in the first two months of the pandemic did not persist, and this might attenuate the effect of screening deficits on survival and mortality.37 However, we found that the decrease in the number of pathology reports persisted when we consider the first 12 months of the pandemic. If this deficit is indeed associated with a stage shift, it could result in a subsequent longer-term impact on survival patterns.
Results similar to ours have been reported using other national pathology databases and cancer registries. Van Velthuysen et al. used data reported to the Netherlands nationwide database of pathology reports to study the impact of the COVID-19 pandemic on diagnostic pathology.38 The investigators reported that the number of skin histologic examinations dropped more than examinations of any other organ during the governmental-ordered lockdowns against the coronavirus. Other authors hypothesized that shifting available resources toward managing COVID patients led to a significant diagnostic delay in melanoma patients.39 Likewise, among the five cancer sites we examined, we found the largest drop among skin melanomas. In addition, van Velthuysen et al. reported that for cancers in general, biopsies dropped more severely than surgical resections.38 Our data support these findings only partially: indeed, we observed a larger drop for two cancer sites with screening recommendations (breast and colorectal) and for skin melanoma, but not for cancers with cytologic diagnosis (lung) or for cancers with equally effective alternative treatments to surgery (i.e., prostate cancer). Additional evidence that screen detected cancers, in particular breast cancer, were affected more severely than non-screen detected cancer has been provided by Eijkelboom et al. using data from the Netherlands Cancer Registry.40 Our results come to support these findings, given that the drop of pathology reports in the “All Other” category was smaller than in any other demographic or cancer-sited based group.
This study has several strengths and builds upon a study by Yabroff et al.26 Our paper expands on the Yabroff et al. study by covering a larger proportion (20.6% versus 4.6%) of the U.S. population, by representing more diverse populations (both rural and urban), over a longer observation period and by analyzing over 3 million electronic pathology reports (versus less than 560,000 in Yabroff et al.). This study also assessed pathology report volume changes by report type rather than overall total report volume. This assessment by report type and cancer site enabled us to evaluate cancers likely to be diagnosed by screening (breast, colorectal, and prostate) versus those diagnosed more typically through symptoms (lung and melanoma). The patterns noted for breast, colorectal, and prostate cancers were different from those observed for lung cancer and melanoma, with the latter showing smaller O/E ratios for biopsies and a more rapid return to the expected baseline.
Electronic pathology reports are submitted to cancer registries in near real time and thus the reports can serve as a strong proxy for cancer diagnosis and surgical treatment. They are also a timelier proxy than hospital cancer abstracts, which are typically delayed. These real time data specifically enabled us to evaluate whether the pandemic’s impact differed by demographic characteristics and cancer site as the COVID-19 pandemic evolved. Due to the delays in cancer incidence reporting, a long-term analysis using cancer diagnosis reports only would have not been possible.
This study also has limitations. Our investigation included only 11 cancer registration jurisdictions in the U.S, that covers approximately 20% of the US population in 2020. The epidemic has consisted of several waves and not all regions of the country have experienced high rates of COVID-19 infections simultaneously. Furthermore, recommendations to delay screening and elective surgery have not been implemented consistently in all U.S. jurisdictions. Therefore, our findings might not apply for every jurisdiction.
Moreover, the number of pathology reports per case has historically varied by primary cancer site, for example more reports are typically available per breast cancer case than for a prostate cancer case. Thus, the patterns we report might be more representative of cancers with multiple biopsies and surgical treatments, procedures that are, in turn, more likely to generate pathology reports. While this study demonstrates the ability to use existing tools and methods to provide near real time assessment of the impact of the pandemic on cancer diagnosis, a limitation related to that real time assessment is the inability to evaluate long term outcomes that may be a result of the decrease in cancer diagnoses.
This study highlights the ability of surveillance systems such as the NCI’s SEER Program to quickly adapt and leverage routine data collection from real-world data sources, such as electronic pathology reports, to assess the potential impact of acute public health emergencies. Moreover, this study highlights how population-based cancer surveillance systems provide the framework for data collection and analysis to investigate how changes in oncology care guidelines may affect quality of care and long-term cancer outcomes.
While the SEER Program focuses on tracking population-level cancer trends across the U.S., this study demonstrates its broader capabilities. It will be important to continue investigating the longer-term impact of the pandemic on oncology services at a time when professionals might expect to see a return to pre-pandemic cancer care delivery levels. Additionally, it will be important to understand which populations and cancer sites might be experiencing more severe long-term impacts in oncology services as a result of the pandemic.
Supplementary Material
Acknowledgments:
We gratefully acknowledge the contributions of the state and regional cancer registry staff and health department personnel for their work in collecting the data used in this report. In addition, we thank Information Management Services, Inc., for assistance in compiling the data used in this report.
Financial support, including the source and number of grants, for each author:
This project has been funded in whole or in part with Federal funds from the National Cancer Institute, National Institutes of Health, Department of Health and Human Services, under
S.M.S. Contract No. HHSN261201800004I
X.W. Contract No. HHSN261201800007I
B.Y.H. Contract No. HHSN261201800011I
J.N.H. Contract No. HHSN261201800005I
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Cancer Institute.
Footnotes
Conflict of interest disclosure statement: The authors declare no potential conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. CDC Museum COVID-19 Timeline. 2022. [cited 2022 Nov 7]. Available from: https://www.cdc.gov/museum/timeline/covid19.html.
- 2.Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):e045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richards M, Anderson M, Carter P, Ebert BL, Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nat Cancer. 2020;1(6):565–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chavez-MacGregor M, Lei X, Zhao H, Scheet P, Giordano SH. Evaluation of COVID-19 mortality and adverse outcomes in US patients with or without cancer. JAMA Oncol. 2022;8(1):69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer care in the time of COVID-19. Ann Intern Med. 2020;172(11):756–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. People with Certain Medical Conditions. 2022. [cited 2022 Nov 8]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- 7.Centers for Medicare and Medicaid. CMS adult elective surgery and procedures recommendations. 2020. [cited 2022 Nov 8]. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf.
- 8.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3(8):e2017267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhahri A, Tegene T. The impact of COVID-19 on breast cancer care: delays in screening. Journal of Clinical Oncology. 2021;39(28_suppl):130–130. [Google Scholar]
- 10.Ueda M, Martins R, Hendrie PC, McDonnell T, Crews JR, Wong TL, et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020;18(4):366–369. [DOI] [PubMed] [Google Scholar]
- 11.Sharpless NE. COVID-19 and cancer. Science. 2020;368(6497):1290. [DOI] [PubMed] [Google Scholar]
- 12.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riera R, Bagattini ÂM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Glob Oncol. 2021;(7):311–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh Q. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7(3):458–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patt D, Gordan L, Diaz M, Okan T, Grady L, Harmison M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;(4):1059–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. An Update on Cancer Deaths in the United States. 2022. [cited 2022 Nov 8]. Available from: https://www.cdc.gov/cancer/dcpc/research/update-on-cancer-deaths/index.htm.
- 17.Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Haren RM, Delman AM, Turner KM, Waits B, Hemingway M, Shah SA, et al. Impact of the COVID-19 pandemic on lung cancer screening program and subsequent lung cancer. J Am Coll Surg. 2021;232(4):600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller MJ, Xu L, Qin J, Hahn EE, Ngo-Metzger Q, Mittman B, et al. Impact of COVID-19 on cervical cancer screening rates among women aged 21–65 years in a large integrated health care system — Southern California, January 1–September 30, 2019, and January 1–September 30, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):109–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tang A, Neeman E, Vuong B, Arasu VA, Liu R, Kuehner GE, et al. Care in the time of COVID-19: impact on the diagnosis and treatment of breast cancer in a large, integrated health care system. Breast Cancer Res Treat. 2022;191(3):665–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman HW, Chen Z, Niles JK, Fesko YA. Changes in newly identified cancer among US patients from before COVID-19 through the first full year of the pandemic. JAMA Netw Open. 2021;4(8):e2125681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaufman HW, Chen Z, Niles JK, Fesko YA. New cancer diagnoses still lagging in the United States in second full year of COVID-19 pandemic. JCO Clin Cancer Inform. 2022;(6):e2200102. [DOI] [PubMed] [Google Scholar]
- 23.Englum BR, Prasad NK, Lake RE, Mayorga-Carlin M, Turner DJ, Siddiqui T, et al. Impact of the COVID-19 pandemic on diagnosis of new cancers: a national multicenter study of the Veterans Affairs Healthcare System. Cancer. 2022;128(5):1048–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powis M, Milley-Daigle C, Hack S, Alibhai S, Singh S, Krzyzanowska MK. Impact of the early phase of the COVID pandemic on cancer treatment delivery and the quality of cancer care: a scoping review and conceptual model. Int J Qual in Health Care. 2021;33(2):mzab088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;(4):657–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yabroff KR, Wu XC, Negoita S, Stevens J, Coyle L, Zhao J, et al. Association of the COVID-19 pandemic with patterns of statewide cancer services. J Natl Cancer Inst. 2022;114(6):907–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alawad M, Gao S, Qiu JX, Yoon HJ, Blair Christian J, Penberthy L, et al. Automatic extraction of cancer registry reportable information from free-text pathology reports using multitask convolutional neural networks. J Am Med Inform Assoc. 2020;27(1):89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lehmann EL. Theory of Point Estimation. John Wiley and Sons Inc.; 1983. [Google Scholar]
- 29.American Society of Clinical Oncology. COVID-19 Clinical Oncology Frequently Asked Questions (FAQs). 2020. [cited 2023 January 3]. Available from: https://old-prod.asco.org/sites/new-www.asco.org/files/content-files/blog-release/pdf/COVID-19-Clinical%20Oncology-FAQs-3–12-2020.pdf.
- 30.American College of Surgeons. COVID-19: Elective Case Triage Guidelines for Surgical Care - Cancer Surgery. 2020. [cited 2023 Jan 3]. Available from: https://www.facs.org/media/btthhitp/guidance_for_triage_of_nonemergent_surgical_procedures_cancer_surgery.pdf.
- 31.American Society of Clinical Oncology, Harris Insights & Analytics LLC ASC. ASCO 2020 Cancer Opinions Survey. 2020 [cited 2023 Jan 4]. Available from: https://old-prod.asco.org/sites/new-www.asco.org/files/content-files/2020-ASCO-National-Cancer-Opinions-Survey-New-Findings.pdf.
- 32.Russo J, Giri VN. Germline testing and genetic counselling in prostate cancer. Nat Rev Urol. 2022;19(6):331–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hill MV, Vidri RJ, Deng M, Handorf E, Olszanski AJ, Farma JM. Real-world frequency of BRAF testing and utilization of therapies in patients with advanced melanoma. Melanoma Res. 2022;32(2):79–87. [DOI] [PubMed] [Google Scholar]
- 34.Valery JR, Applewhite A, Manaois A, Dimuna J, Sher T, Heckman MG, et al. A retrospective analysis of gender-based difference in adherence to initial colon cancer screening recommendations. J Prim Care Community Health. 2020;11:215013272093132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hall IJ, Tangka FKL, Sabatino SA, Thompson TD, Graubard BI, Breen N. Patterns and trends in cancer screening in the United States. Prev Chronic Dis. 2018;15:E97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alagoz O, Lowry KP, Kurian AW, Mandelblatt JS, Ergun MA, Huang H, et al. Impact of the COVID-19 pandemic on breast cancer mortality in the US: estimates from collaborative simulation modeling. J Natl Cancer Inst. 2021;113(11):1484–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caswell-Jin JL, Shafaee MN, Xiao L, Liu M, John EM, Bondy ML, et al. Breast cancer diagnosis and treatment during the COVID-19 pandemic in a nationwide, insured population. Breast Cancer Res Treat. 2022;194(2):475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Velthuysen MLF, van Eeden S, le Cessie S, de Boer M, van Boven H, Koomen BM, et al. Impact of COVID-19 pandemic on diagnostic pathology in the Netherlands. BMC Health Serv Res. 2022;22(1):166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jeremić J, Suđecki B, Radenović K, Mihaljević J, Radosavljević I, Jovanović M, et al. Impact of the COVID-19 pandemic on melanoma diagnosis: Increased Breslow thickness in primary melanomas—A single center experience. Int J Environ Res Public Health. 2022;19(24):16806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eijkelboom AH, de Munck L, Lobbes MBI, van Gils CH, Wesseling J, Westenend PJ, et al. Impact of the suspension and restart of the Dutch breast cancer screening program on breast cancer incidence and stage during the COVID-19 pandemic. Prev Med. 2021;151:106602. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data for this study is not routinely collected by NCI SEER since pathology reports contain personally identifiable information. The data could be made available upon written request to each participating SEER cancer registry and their approval.