Abstract
Objectives
More than a quarter of human immunodeficiency virus (HIV)-infected persons are undiagnosed and therefore unaware of their HIV+ status. African Americans are disproportionately infected. Although perceived racism influences their attitudes toward HIV prevention, how racism influences their behaviors is unknown. We sought to determine whether perceiving everyday racism and racial segregation influence African American HIV testing behavior.
Methods
This was a clinic-based, multi-level study. Eligibility was limited to African Americans (N=373) seeking sexually transmitted disease diagnoses or screening. We collected survey data, block group characteristics, and lab-confirmed HIV testing behavior. We estimated associations using logistic regression with generalized estimating equations (GEE).
Results
More than 90% of the sample perceived racism, which was associated with higher odds of HIV testing (OR=1.64, 95% CI=1.07, 2.52) controlling for residential segregation and other covariates. Neither patient satisfaction nor mechanisms for coping with stress explained the association.
Conclusions
African Americans are not merely victims of racism but also exercise agency within their social contexts. Those who perceive everyday racism may draw upon health promoting assets relative to their behaviors. How segregation influences testing warrants further research.
Introduction
Despite decreases in mortality due to acquired immune deficiency syndrome (AIDS), the prevalence of human immunodeficiency virus (HIV) infection in the United States remains high overall and diagnoses among African Americans continue to increase.1 Although African Americans represent less than 13% of the US population, they account for 42% of prevalent HIV infections and 54% of annual diagnoses.1 An estimated one-fourth of all HIV-infected US residents have not been diagnosed.2 That HIV positive blacks delay care-seeking more, progress to AIDS faster, and die from AIDS sooner than whites underscores the need to improve HIV screening in this population.3, 4
Sexually transmitted disease (STD) clinics are an important setting for reaching persons at elevated risk of sexual transmission, the primary mode by which HIV transmission occurs.5 These clinics provide testing regardless of an individual's ability to pay. The prevalence of undiagnosed HIV infection is higher in STD clinic populations than in the general population and persons engaging in STD risk behaviors are by definition at risk for HIV transmission. Furthermore, although every exposure to HIV does not result in seropositivity, epidemiologic synergy between HIV and classic STDs such as gonorrhea renders STD-infected persons more susceptible to HIV-infection upon exposure to the virus.6
Population-based surveys suggest that blacks obtain HIV testing at higher rates than do other racial/ethnic groups7; however, self-reports may overestimate actual testing behavior. In one nationally representative study, 25% of blacks reporting prior HIV tests had assumed they were tested during some clinical visit where they had neither requested nor consented to a test.8 Among STD clinic patients, blacks may actually be less likely to test.9
For African Americans, negative attitudes toward HIV prevention are linked to racism.10 Racism has been defined as “an organized system, rooted in an ideology of inferiority that categorizes, ranks, and differentially allocates societal resources to human population groups”.11 (p.76) Racism is a multilevel construct fundamentally influenced by macro-level factors such as residential segregation.12-14 Research suggests that perceiving or experiencing racial discrimination contributes to hypertension15-17, pre-term birth18, mental health outcomes19, 20, and unhealthy coping behaviors (e.g., cigarette smoking and alcohol use)21. Exactly how individuals respond to perceived racism also is important. In the CARDIA study, for instance, persons who perceived and challenged racism on the job had lower systolic blood pressures (i.e., better outcomes) than those whom investigators described as internalizing it.16 For some African Americans, however, overachieving in response to racism may adversely impact health, a phenomenon described as “John Henryism”.22
Racism can be thought of as an element in the social environment; perceived racism is the extent to which individuals are aware of that element. Perceived everyday racism reflects individuals' assessments of potentially negative routine interactions (e.g., being followed while shopping in a store) as resulting from racism rather than as due to other causes (e.g. coincidence).23 In some contexts perceiving racism is detrimental while in others it is self-protective.24
Most racism-related HIV prevention research examines extreme forms of racism rather than everyday racism. These studies indicate that awareness of the US Public Health Services' study of untreated syphilis in African American men and beliefs that “the government is…using AIDS as a way of killing off minority groups”25 are prevalent and associated with negative attitudes about HIV prevention.26-29 Few studies have examined perceived racism's association with HIV preventive behaviors and these primarily assess self-reports of behavior. A national phone survey28 of African Americans (N=500) and a Houston-based survey30 of a multi-racial sample (N=1494) found negative associations between conspiracy beliefs and self-reported condom use for African American men.28, 30 One study31 found perceived everyday racism positively associated with condom use. These studies did not account for residential context.
Perceptions about racism, however, are influenced by interracial interactions. More integrated blacks perceive more racism.32 Outside the workplace, residential areas are the most likely arenas for interactions; often, however, these are racially segregated. The systematic residential isolation of blacks from whites through de facto segregation is a fundamental cause of disparities, differentially influencing access to health care, socioeconomic status, and quality of services.13, 33, 34 Segregation historically has impacted communities in the US South. The most widely assessed dimension of segregation is unevenness. Calculated via the dissimilarity index, D, it indicates an area's relative proportions of minority and majority populations.35
Studies using census geographies such as block groups permit monitoring of area socioeconomic and demographic trends across time and place; census designations are well-defined units of analysis and the socioeconomic data are systematically collected.36 Block groups, which average 1,500 residents, are the smallest geographic units for which the US Census Bureau provides sample data.37 Although many studies operationalize neighborhoods as tracts or zip code regions, block groups may be more appropriate units when studying smaller cities or regions where neighborhood boundaries change rapidly.
The purpose of this study was to examine perceived everyday racism's association with routine HIV testing among at-risk African Americans while accounting for racialized residential contexts.
Methods
Population and Setting
Data were collected from March to June 2003 in a public STD clinic located in a North Carolina city with high HIV and STD prevalences. African Americans make up 20% of the county's and 28% of the city's population.37 The city's residential segregation (Dissimilarity Index=0.54) exceeds that of 85% of US cities with comparable population size.38 The African American population resides primarily within two contiguous zip code regions where STD and HIV prevalences were highest. Most persons who obtain care at the clinic reside in these neighborhoods. As established in extensive formative research39, access (e.g., transportation) to the clinic was not a barrier to testing in this population. The clinic is the primary source of HIV tests in the county, providing between 3,000 and 4,000 HIV tests annually.40 Blacks account for more than 60% of the clinic's patients.
Study Design
This was a multilevel, cross-sectional study estimating individual-level associations relative to the behavioral outcome, visit-specific uptake of routine HIV testing, while accounting for population-averaged residential (i.e., “neighborhood”) characteristics and other factors. The conceptual framework guiding the study integrated Critical Race Theory41 concepts and Andersen's Access to Care Model42. As standard practice at the clinic, STD patients seeking non-follow-up care were automatically offered an HIV antibody test during their visit. The University of North Carolina's School of Public Health Institutional Review Board approved all aspects of the study.
Sample
Eligible clinic participants were consecutively enrolled during routine clinic hours. Only outpatients seeking diagnosis or screening for STD and/or HIV infection were eligible for participation; persons seeking follow-up care, information or other services were not eligible. Inclusion criteria were self-reported race as black or African American, age 18 years or older and presenting for diagnosis of or screening for possible STD infection. Of those eligible and invited (N=474), 61 (41 men, 20 women) declined participation, resulting in an 87% response rate; 413 patients consented to and enrolled in the study. Responses from 38 participants (9%) were excluded from the analyses because data on their visit-specific HIV testing behavior, the outcome of interest, were missing. Two additional observations were excluded because of incomplete questionnaires. The final sample size for individual-level analyses was 373, 56% (n=210) women. Block group analyses further excluded 61 observations because participant addresses were unreported (e.g., due to homelessness) or impossible to validate using a geographic information system (GIS). The final sample size for block group analyses was 312 individuals living within 117 block groups.
Data Collection
Participants completed the 101-item questionnaire while seated in the clinic lobby. To enable privacy and to accommodate possible low levels of literacy, participants listened to an audio-taped version of the questionnaire using headsets and marked responses on a corresponding paper form. The audio-taped recording was completed by an African American research assistant native to the region. Each participant's visit-specific HIV testing behavior was ascertained from the clinic's daily log of diagnostic tests and recorded in a manner blinded to questionnaire data collection. All names were then removed from questionnaires.
Outcome Variable
The outcome was visit-specific uptake of HIV testing via blood draw with enzyme-linked immunosorbent assay (ELISA), as recorded in the clinic lab's daily log of administered tests. Test uptake was coded yes=1 or no=0. Each time a study participant was seen, lab technicians summarized patient information (name, chart number, and whether HIV testing was performed) in the daily log relevant to HIV antibody test acceptance.
Explanatory Variables and Covariates
Perceived racism and residential segregation were the key explanatory variables. The questionnaire assessed perceived racism43, 44, coping mechanisms for stress, individuals' demographic characteristics, HIV prevention-related constructs (e.g., perceived risk, HIV knowledge), and clinical encounter factors (e.g., previous clinic use). In the pilot study, internal consistency was high (Cronbach's α≥0.70) for the perceived racism43, 44, patient satisfaction45, HIV knowledge46 and perceived HIV susceptibility47 scales. Reliability and validity of the perceived racism scale had been established previously for in-person 43 and telephone administration44. We used the 10-item sub-scale of the perceived racism scale to assess respondents' perceptions about the extent to which blacks generally encounter several types of white-on-black perceived racist experiences on the job, in social settings and in public settings. For instance, “In general, when blacks shop, they are followed or watched by white security guards or white clerks.” Response options ranged across a four-point Likert-type scale from strongly disagree to strongly agree.
We operationalized residential areas as the Census 2000 block groups in which study respondents resided on the basis of addresses sample members reported in the questionnaires. We obtained data on block group racial composition from the census summary file one and assessed segregation using the dissimilarity index (D). This index reflects the proportion of blacks who must move in order to achieve racially equal population distributions.35 Block group segregation was derived from each block group's constituent blocks' racial composition and compared across the block groups comprising the study area. Index values may range from 0-1, with one indicating complete segregation.
Covariates included patient satisfaction, a potential confounder. Based upon focus groups, we derived a 5-item, ordinal scale from Marshall and Hays' 18-item questionnaire45. Each response was scored on a five-point Likert-type scale (strongly agree to strongly disagree). Stress coping mechanisms were assessed via responses to the statement “How often do you cope with stress by…” Responses were categorized as passive (e.g., sleeping), healthy (e.g., exercising), or negative (e.g., drinking). Standard HIV prevention-related constructs such as perceived HIV risk were assessed using measures borrowed from the CDC's Behavioral Risk Factor Surveillance System (BRFSS)47, 48.
Additional variables reflecting neighborhood deprivation or inequity were derived from census summary files one and three. These included relative income (ratio of block group median income to median income for the region), concentrated poverty (40% or greater poverty within a block group)49, percentage of black residents (proportion of block group population that was black alone or in combination with some other race relative to the block group total population), percentage of vacant households, percentage unemployed, mean educational attainment, and percentage of female-headed households.
Statistical Analyses
We used non-automatic, backward elimination to specify multivariable logistic regression models50 with generalized estimating equations (GEE) to account for variance clustering that occurs when one level of data (i.e., individual) is nested within another (i.e., block group). GEE is preferred to other multilevel approaches (e.g., mixed models) when, as in this study, the group level units are not a random sample of some universe of block groups.51 We specified an exchangeable correlation structure (i.e., any two responses within a cluster have the same correlation) and used robust variance estimators to derive 95% confidence intervals around each estimate. In exploratory analyses we examined variable distributions, collinearity, interaction, and potential statistical confounding. We also compared estimates obtained using the dissimilarity index to those using percentage black. Analyses were conducted using Stata Version 8.52
Results
Table 1 displays sample demographic characteristics. Perceived risk of HIV infection was low across age groups and gender categories. Forty-six percent of sample members were seeking care because they had symptoms of an STD; 10% had been referred by another provider.
TABLE 1. Sample Demographic Characteristics.
| Gender | Testing Behavior | Total | |||
|---|---|---|---|---|---|
| Men | Women | No Test | Test | ||
| N=163 (43.7%) | N=210 (56.3%) | N=165 (44.2) | N=208 (55.8) | N=373 (100.0%) | |
| Perceived Racism* | |||||
| Mean (s.d.) | 28.0 (5.9) | 28.5 (5.8) | 27.4 (5.9) | 28.9 (5.8) | 28.2 (5.9) |
| Range | 10-40 | 10-40 | 10-40 | 10-40 | 10-40 |
| Age (in years) | |||||
| Mean Age (s.d.) | 28.7 (8.9) | 27.7 (8.9) | 27.63 (8.2) | 28.50 (9.4) | 28.1 (8.9) |
| Range | 18-57 | 18-55 | 18-54 | 18-57 | 18-57 |
| Education | |||||
| <HS, n (%) | 13 (8.2) | 22 (10.6) | 15 (9.2) | 20 (9.9) | 35(9.5) |
| HS Diploma, n (%) | 68 (42.8) | 87 (41.8) | 68 (41.5) | 87 (42.9) | 155(42.2) |
| College Deg. or higher, n (%) | 78 (49.1) | 99 (47.6) | 81 (49.4) | 96 (47.3) | 177(48.2) |
| Insurance Status | |||||
| Uninsured, n (%) | 85 (54.5) | 91 (44.2) | 74 (46.0) | 102 (50.8) | 176 (48.6) |
| Medicaid/Medicare, n (%) | 20 (12.8) | 64 (31.1) | 33 (20.5) | 51 (25.4) | 84 (23.2) |
| Privately insured, n (%) | 51 (32.70) | 51 (24.8) | 54 (33.5) | 48 (23.9) | 102 (28.2) |
| Employment Status | |||||
| Unemployed, n (%) | 48 (31.4) | 88 (42.7) | 55 (34.4) | 81 (40.7) | 136 (37.9) |
| Part time, n (%) | 34 (22.2) | 40 (19.4) | 28 (17.5) | 46 (23.1) | 74 (20.6) |
| Full Time, n (%) | 71 (46.4) | 78 (37.9) | 77 (48.1) | 72 (36.2) | 149 (41.5) |
| Income Category (× $1000) | |||||
| <5, n (%) | 37 (23.9) | 72 (35.8) | 47 (29.6) | 62 (31.5) | 109 (30.6) |
| 5-10, n (%) | 20 (12.9) | 43 (21.4) | 24 (15.1) | 39 (19.8) | 63 (17.7) |
| 10-20, n (%) | 45 (29.1) | 37 (18.4) | 40 (25.2) | 42 (21.3) | 82 (23.0) |
| 20-35, n (%) | 35 (22.6) | 38 (18.9) | 34 (21.4) | 39 (19.8) | 73 (20.5) |
| 35+, n (%) | 18 (11.6) | 11 (5.5) | 14 (8.8) | 15 (7.6) | 29 (8.2) |
The 30-unit scale ranges from 10-40 with higher scores indicating higher perceived racism
Perceived racism scores ranged from the absolute minimum, 10, indicating no perceived racism, to the maximum, 40, indicating the highest level of perceived racism assessed on the scale. The observed mean scores revealed, on average, agreement with nearly all of the items on the scale. The range, mean and median scores did not vary by gender.
Fifty-five percent of participants obtained HIV tests during their clinical visits. Proportionally fewer men than women (χ2=6.25, DF=1, p=0.01) tested. Relative to younger participants (i.e., age<30 years), greater proportions of participants aged 45 years old or older tested (54% versus 68%), but this difference was not statistically significant. HIV knowledge and perceived HIV risk were unrelated to testing behavior.
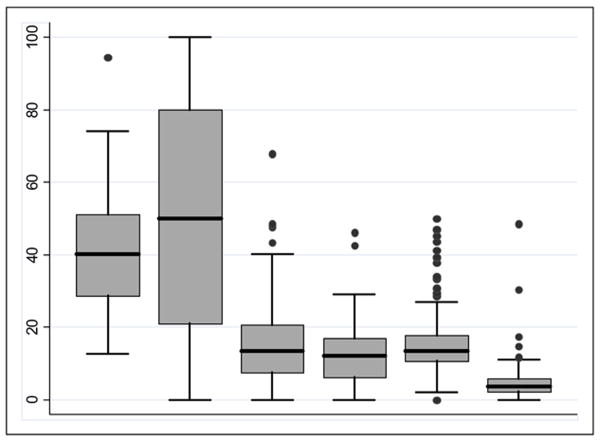
Figure 1 displays summary data on residential characteristics. Spatially, residences clustered around the clinic and loosely followed major roads (data not shown). Between one and 14 participants resided in each block group. Block group dissimilarity index scores ranged from D=0.13 to 0.94; however, they were heavily centered around the median, 0.40. Testers resided in more integrated areas and non-testers resided in more segregated areas (data not shown).
Figure 1. Distribution of Selected Residential Characteristics (N=117 block groups).
Box Labels (left to right in figure) Dissimilarity Index score (×100); % Black; % Vacant Households; % Poverty; % of Female Headed Households; % Unemployed
Note. Horizontal lines within each box indicate medians; each box's lower and upper bounds indicate the 25th and 75th percentiles, respectively; the lower and upper whiskers indicate the range of values within 1.5 times the interquartile range; and, darkened circles indicate outliers.
The final statistical model is shown in Table 2. The full model included perceived racism, individual demographic characteristics, patient satisfaction, symptoms, ever previously obtaining an HIV test, perceived HIV risk, coping mechanisms, HIV knowledge and block group characteristics. Perceived racism was associated with higher odds of obtaining routine HIV testing during the clinic visit in crude analyses; this association persisted in the final model (OR=1.64, 1.07, 2.52). Each 10-unit increase (e.g. from “medium” to “high”) on the 30-unit Perceived Racism Scale corresponded with approximately 60% higher odds of testing. The point estimate for the dissimilarity index (OR=0.32, 0.05, 2.18) in the final model suggested higher levels of segregation were associated with not testing; however, the 95% CI included the null value. In models replacing the dissimilarity index with percentage black, the percentage of blacks in block groups was unassociated with HIV testing (OR=0.99, 0.99, 1.00).
Table 2. Logistic Regression GEE Model Assessing Perceived Racism, Block Group Characteristics and Testing (N=301)†‡.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Perceived racism | 1.68 (1.17, 2.40) | 1.67 (1.14, 2.44) | 1.59 (1.07, 2.38) | 1.72 (1.14, 2.60) | 1.64 (1.07, 2.52) |
| Patient satisfaction | … | … | 1.00 (0.94, 1.06) | 0.99 (0.93, 1.05) | 0.99 (0.93, 1.05) |
| Healthy coping | … | … | … | … | 1.08 (0.91, 1.27) |
| Negative coping | … | … | … | … | 0.96 (0.89, 1.05) |
| Passive coping | … | … | … | 0.88 (0.78, 1.00) | 0.89 (0.78, 1.01) |
| Symptoms (y/n) | … | … | 0.56 (0.34, 0.93) | 0.58 (0.35, 0.97) | 0.57 (0.34, 0.96) |
| Previous Test (y/n) | … | … | 1.88 (0.97, 3.63) | 1.77 (0.91, 3.45) | 1.78 (0.91, 3.49) |
| Gender (ref=woman) | … | … | 0.46 (0.26, 0.81) | 0.39 (0.22, 0.71) | 0.37 (0.20, 0.69) |
| BG segregation | … | 0.26 (0.05, 1.28) | 0.34 (0.06, 1.91) | 0.32 (0.05, 1.96) | 0.32 (0.05, 2.18) |
Excludes observations missing data on any variable included in the model
Note: Model 1 is crude; Model 2 includes perceived racism and block group residential segregation; Model excludes stress coping mechanisms; Model 4 includes passive coping mechanisms; Model 5 includes passive, healthy and negative coping
Discussion
Nearly all participants in this study perceived everyday racism; the more racism perceived the higher the odds of being tested for HIV during an STD clinic visit. Neither patient satisfaction nor stress coping mechanisms explained this association. Previous research linking perceived racism to attitudes has suggested it may negatively influence behaviors.53 Our findings did not support that hypothesis. One reason may be that while this study examined everyday racism, most previous research has focused on extreme forms of racism (e.g., HIV conspiracy beliefs). In racially stratified societies individuals are constantly exposed to everyday racism43; so, it is conceivable that there may be contexts in which perceiving it is health protective.
Although the positive association between perceived racism and HIV testing may seem counterintuitive, support for it exists in previous research. Others have found that perceiving racism is not inherently detrimental and that African Americans who notice it in their social environments and challenge it may have healthier outcomes than do those who deny its existence or blame themselves or other minorities for observed disparities.16 The findings also concur with those of the one other study found that examined perceived everyday racism and HIV preventive behaviors.31 Investigators using the 38-item Racism and Life Experiences Scale (SP Harrell, PhD, unpublished data, 1997) observed that perceived racism was prevalent and positively associated with condom-related HIV preventive behaviors among African American women.
We controlled for coping mechanisms because how individuals deal with racism they perceive has implications for their well-being.23 Resiliency, which we did not directly measure, may explain positive associations between perceived racism and health protective behaviors such as HIV testing. According to the resiliency hypothesis, blacks who perceive racism and develop ways to function day-to-day in spite of it have higher resiliency levels and cope better with racism-related stressors. An alternative explanation is that social support, also unmeasured in this study, could have confounded the association between perceived racism and testing if persons with greater perceived support felt more comfortable both reporting perceived racism and obtaining HIV tests.
Fewer residents of more segregated block groups got tested. This finding is consistent both with the hypothesis that more segregated blacks perceive racism less54 and with the observed association in this study between lower perceived racism and not getting tested. While segregation often signals blacks' poor access to care, extensive formative research preceding this study indicated access to the STD clinic was not a barrier.39 Rather, segregation was included because of its conceptual relevance to perceived racism. The small geographic area studied, and its predominately black composition, however, biased any associations around segregation toward the null. The findings contrast with a Los Angeles study in which, regardless of race/ethnicity, persons living in “predominately black” areas were more likely to obtain HIV tests.55 That study operationalized neighborhoods using ZIP codes rather than the census designations recommended for monitoring population health.56 It also used percentage black as a proxy measure of segregation, rather than a segregation index as used in this study. Percentage black may measure unspecified socioeconomic or racial/ethnic factors. Then, too, this research was conducted in the US South where distinctive racial relations persist and racial groups are less heterogeneous. The complex relationships between segregation, network characteristics such as network-specific HIV prevalences, and behaviors require further research.57-59
That perceived HIV risk was low corroborates other research60, 61. Denial and fear of becoming HIV infected may explain this common finding.62 Primary prevention to promote accurate risk assessments will remain important in the increasingly screening-oriented prevention climate.63
Greater conceptual and empirical clarification of ‘racism’ constructs is also needed. This study assessed two related concepts: perceived racism, an individual level factor, and residential segregation, a macro level factor. Most research emphasizes interpersonal discrimination rather than structural factors, which may underlie persistent disparities.64
Limitations and Strengths
The study had several limitations. Thirty eight observations were excluded because the participants' testing behaviors were not recorded in the clinic's log. This only occurred if individuals reported a false name to the study and/or clinic, suggesting distrust and/or stigma in this population. Sensitivity analyses using single unit contrasts on the 30-unit perceived racism scale indicated that these missing cases did not substantially distort the findings. Although slightly lower mean perceived racism scores biased the results slightly away from the null, similar point estimates and substantially overlapping confidence intervals were obtained whether these 38 observations were excluded (OR=1.04; 95% CI=1.01, 1.09), recoded to “no test” (OR=1.05; 95% CI=1.02,1.09), or recoded to “test” (OR=1.03; 95% CI=1.00, 1.06). The study did not control for risk behaviors such as injection drug use, which could influence testing behavior. Although the dissimilarity index is the most widely-used measure of residential segregation, it is insensitive to extremely high or low minority populations, may underestimate overall levels of segregation and does not address geographic considerations captured by other measures (e.g., local area spatial autocorrelations).35, 65 The geographic region studied here was small and limited in its racial heterogeneity. Block group estimates, therefore, were biased toward the null. Lastly, data were sparse (n≤5) in most block groups. One strength of GEE is that it accommodates sparse or missing data66; nonetheless, we confirmed the main association by conducting logistic regression analyses that excluded block group level variables and found basically the same results (OR=1.64; 95% CI: 1.06, 2.55).
Use of actual, not self-reported, HIV testing reassures us of the validity of this measure of stigmatized behavior. Similarly, our operationalization of residential areas as block groups may better approximate neighborhood patterns in small cities, where neighborhood boundaries may be small or may shift quickly. The public health literature on racism, which primarily targets mental health, chronic disease and birth-related outcomes, is advanced by this research on an infectious disease-related outcome. Although social context was not empirically confirmed as a risk factor for testing or failure to test, the field is advanced conceptually by the inclusion of context in the study's design.67
Implications for Practice and Policy
African Americans are not merely victims of racism but also exercise agency within and regarding their social contexts. Those who perceive everyday racism may draw upon health promoting assets relative to their behaviors. We recommend that practitioners work closely with this population to identify transferable, health protective skills to promote preventive behaviors among other blacks and that future research help to clarify the settings, outcomes and subpopulations in which perceived racism is detrimental versus constructive.
Fullilove suggests that racism is the “elephant in the room” when providers and educators deliver counseling, testing and education in this population.68 By showing that perceived racism was not a barrier to HIV prevention, our findings like Fullilove's argument challenge assumptions that awareness of racism necessarily inhibits HIV prevention among blacks. Intervention research is needed to explore whether discussing racism during counseling, testing or education can reduce distrust and improve communication between African Americans and prevention professionals. For residents of more segregated areas who may be less likely to obtain clinic-based HIV testing, outreach may prove to be effective for reaching this population.
Policies attentive to assets-based interventions, cultural competence and equity are needed to guide the development and implementation of any prevention strategies (i.e., targeted outreach) that aim to integrate racism-related concerns and prevention efforts.69
Acknowledgments
This research was supported by the National Institute of Allergy and Infectious Diseases (Fellowship #: 1 F31 AI058914-01), the Agency for Healthcare Research and Quality (Grant #'s: T32-HS00032, T32-HS00031) and the W. K. Kellogg Foundation Kellogg Health Scholars Program (Grant # P0117943) administered via the Center for the Advancement of Health. The following units at the University of North Carolina also provided support: Office of the Vice-Chancellor for Research and Development, Department of Social Medicine, Cecil G. Sheps Center for Health Services Research, Center for AIDS Research, North Carolina Rural Health Research Program, and Center for the Study of the American South. The authors acknowledge Anissa Vines, Lori Carter-Edwards and Dionne Godette whose feedback strengthened the manuscript.
Footnotes
Contributors: Chandra Ford conceived of the study, led in conducting the analyses and led in writing the manuscript. Mark Daniel assisted with study design, analyses and manuscript revisions. Jo Anne Earp assisted with study design, interpretation of findings and manuscript revisions. Jay Kaufman assisted with analyses, interpretations of findings and manuscript revisions. Carol Golin and William Miller assisted with study design and manuscript revisions.
Human Participant Protection: The study was approved by the Institutional Review Board of the University of North Carolina's School of Public Health.
References
- 1.Kaiser Family Foundation. The HIV/AIDS Epidemic in the United States. Menlo Park, CA: Kaiser Family Foundation; 2004. [Google Scholar]
- 2.MacKellar DA, Valleroy LA, Secura GM, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr. 2005 Apr 15;38(5):603–614. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham WE, Markson LE, Andersen RM, et al. Prevalence and predictors of highly active antiretroviral therapy use in patients with HIV infection in the United States. HCSUS Consortium. HIV Cost and Services Utilization. J Acquir Immune Defic Syndr. 2000 Oct 1;25(2):115–123. doi: 10.1097/00042560-200010010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Turner BJ, Cunningham WE, Duan N, et al. Delayed medical care after diagnosis in a US national probability sample of persons infected with human immunodeficiency virus. Arch Intern Med. 2000 Sep 25;160(17):2614–2622. doi: 10.1001/archinte.160.17.2614. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report: Cases of HIV infection and AIDS in the United States and Dependent Areas, 2005. Vol. 17. Atlanta, GA: US Department of Health and Human Services, Center for Disease Control and Prevention; 2006. [Google Scholar]
- 6.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(3):3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebrahim SH, Anderson JE, Weidle P, Purcell DW. Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS. 2004 Jan;18(1):27–33. doi: 10.1089/108729104322740893. [DOI] [PubMed] [Google Scholar]
- 8.Aragon R, Kates J, Greene L. African Americans' views of the HIV/AIDS epidemic at 20 years. Menlo, CA: Kaiser Family Foundation; 2001. [Google Scholar]
- 9.Schwarcz SK, Spitters C, Ginsberg MM, Anderson L, Kellogg T, Katz MH. Predictors of human immunodeficiency virus counseling and testing among sexually transmitted disease clinic patients. Sex Transm Dis. 1997 Jul;24(6):347–352. doi: 10.1097/00007435-199707000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Dalton HL. AIDS in blackface. Daedalus. 1989 Summer;118(3):205–227. [PubMed] [Google Scholar]
- 11.Williams DR, Rucker TD. Health Care Financ Rev Summer. 2000;21(4):75–90. [PMC free article] [PubMed] [Google Scholar]
- 12.Jones CP. Levels of racism: a theoretic framework and a gardener's tale. Am J Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001 Sep-Oct;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92(4):615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams DR, Neighbors HW. Racism, discrimination and hypertension: evidence and needed research. Ethn Dis. 2001 Fall;11(4):800–816. [PubMed] [Google Scholar]
- 16.Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA Study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clark R. Self-reported racism and social support predict blood pressure reactivity in Blacks. Ann Behav Med. 2003 Spring;25(2):127–136. doi: 10.1207/S15324796ABM2502_09. [DOI] [PubMed] [Google Scholar]
- 18.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003 Jan 1;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 19.Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health status of African Americans: a thirteen year national panel study. Ethn Dis. 1996;6:132–147. [PubMed] [Google Scholar]
- 20.Neighbors HW, Jackson JS, Broman CL, Thompson E. Racism and the mental health of African Americans: the role of self and system blame. Ethn Dis. 1996;6:167–175. [PubMed] [Google Scholar]
- 21.Kwate NO, Valdimarsdottir HB, Guevarra JS, Bovbjerg DH. Experiences of racist events are associated with negative health consequences for African American women. J Natl Med Assoc. 2003 Jun;95(6):450–460. [PMC free article] [PubMed] [Google Scholar]
- 22.James SA, Hartnett SA, Kalsbeek WD. John Henryism and blood pressure differences among black men. J Behav Med. 1983 Sep;6(3):259–278. doi: 10.1007/BF01315113. [DOI] [PubMed] [Google Scholar]
- 23.McNeilly MD, Anderson NB, Armstead CA, et al. The Perceived Racism Scale: a multidimensional assessment of the experience of white racism among African Americans. Ethn Dis. 1996;6:154–166. [PubMed] [Google Scholar]
- 24.Mays VM, Cochran SD, Barnes NW. Race, Race-Based Discrimination, and Health Outcomes Among African Americans. Annu Rev Psychol. 2006 Sep 5; doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herek GM, Capitanio JP. Conspiracies, contagion, and compassion: trust and public reactions to AIDS. AIDS Educ Prev. 1994;6(4):365–375. [PubMed] [Google Scholar]
- 26.Thomas SB, Quinn SC. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the Black community. Am J Public Health. 1991;81(11):1498–1504. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klonoff EA, Landrine H. Do Blacks believe that HIV/AIDS is a government conspiracy against them? Prev Med. 1999;28:451–457. doi: 10.1006/pmed.1999.0463. [DOI] [PubMed] [Google Scholar]
- 28.Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005 Feb 1;38(2):213–218. doi: 10.1097/00126334-200502010-00014. [DOI] [PubMed] [Google Scholar]
- 29.Green B, Maisiak R, Wang M, Britt M, Ebeling N. Participation in health education, health promotion, and health research by African Americans: effects of the Tuskegee Syphilis Experiment. J Health Educ. 1997 Jul-Aug;28(4):196–204. [Google Scholar]
- 30.Ross MW, Essien EJ, Torres I. Conspiracy beliefs about the origin of HIV/AIDS in four racial/ethnic groups. J Acquir Immune Defic Syndr. 2006 Mar;41(3):342–344. doi: 10.1097/01.qai.0000209897.59384.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jipguep MC, Sanders-Phillips K, Cotton L. Another look at HIV in African American women: The impact of psychosocial and contextual factors. J Black Psychol. 2004 August;30(3):366–385. [Google Scholar]
- 32.Jackson PB. Health inequalities among minority populations. J Gerontol B Psychol Sci Soc Sci. 2005 Oct;60(Spec No 2):63–67. doi: 10.1093/geronb/60.special_issue_2.s63. [DOI] [PubMed] [Google Scholar]
- 33.Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Soc Sci Med. 2000;51(8):1143–1161. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- 34.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 35.Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces. 1988;67(2):281–315. [Google Scholar]
- 36.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 37.US Census Bureau GD, Cartographic Operations Branch. Census Block Groups: Cartographic Boundary Files Descriptions and Metadata. 2002 [Google Scholar]
- 38.U.S. Census. Profile of General Demographic Characteristics: 2000. [November 15, 2004]; [Website] http://factfinder.census.gov.
- 39.Ford CL, Tilson EC, Smurzynski M, Leone PA, Miller WC. Confidentiality concerns, perceived staff rudeness and other HIV testing barriers. J Equity Health. 2008 In press. [Google Scholar]
- 40.Anonymous. HIV Counseling and Testing Sites. Raleigh, NC: Wake County Human Services; 1999. [Google Scholar]
- 41.Delgado R, Stefancic J. Critical Race Theory: An Introduction. First. New York, New York: New York University Press; 2001. [Google Scholar]
- 42.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995 March;36:1–10. [PubMed] [Google Scholar]
- 43.McNeilly MD, Anderson NB, Robinson EL, et al. Convergent, discriminant, and concurrent validity of the Perceived Racism Scale: a multidimensional assessment of the experience of racism among African Americans. Handbook of Tests and Measurements for Black Populations. 1996:359–373. [Google Scholar]
- 44.Vines AI, McNeilly MD, Stevens J, Hertz-Picciotto I, Baird M, Baird DD. Development and reliability of a Telephone-Administered Perceived Racism Scale (TPRS): a tool for epidemiological use. Ethn Dis. 2001;11(2):251–262. [PMC free article] [PubMed] [Google Scholar]
- 45.Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short-form (PSQ-18) Santa Monica, CA: RAND; 1994. [Google Scholar]
- 46.Rietmeijer CA, Lansky A, Anderson JE, Fichtner RR. Developing standards in behavioral surveillance for HIV/STD prevention. AIDS Educ Prev. 2001;13(3):268–278. doi: 10.1521/aeap.13.3.268.19740. [DOI] [PubMed] [Google Scholar]
- 47.Longshore D, Stein JA, Anglin MD. Psychosocial antecedents of needle/syringe disinfection by drug users: a theory-based prospective analysis. AIDS Educ Prev. 1997;9(5):442–459. [PubMed] [Google Scholar]
- 48.Holtzman D, Bland SD, Lansky A, Mack KA. HIV-related behaviors and perceptions among adults in 25 states: 1997 Behavioral Risk Factor Surveillance System. Am J Public Health. 2001;91(11):1882–1888. doi: 10.2105/ajph.91.11.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Massey DS. The age of extremes: concentrated affluence and poverty in the twenty-first century. Demography. 1996 Nov;33(4):395–412. discussion 413-396. [PubMed] [Google Scholar]
- 50.Kleinbaum DG. Logistic Regression: A Self-Learning Text. First. New York, NY: Springer-Verlag; 1994. [Google Scholar]
- 51.Liang KY, Zeger SL. Regression analysis for correlated data. Annual Review of Public Health. 1993;14:43–68. doi: 10.1146/annurev.pu.14.050193.000355. [DOI] [PubMed] [Google Scholar]
- 52.Stata for Windows [computer program] Version 8/SE. College Station, TX: 2003. [Google Scholar]
- 53.Quinn SC. Belief in AIDS as a form of genocide: implications for HIV prevention programs for African Americans. J Health Educ. 1997 November/December;28 6:S6–S11. [Google Scholar]
- 54.Cole ER, O SR. Race, Class and the Dilemmas of Upward Mobility for African Americans. J Soc Issues. 2003;59(4):785–802. [Google Scholar]
- 55.Taylor SL, Leibowitz A, Simon PA, Grusky O. ZIP code correlates of HIV-testing: a multi-level analysis in Los Angeles. AIDS Behav. 2006 Sep;10(5):579–586. doi: 10.1007/s10461-005-9064-4. [DOI] [PubMed] [Google Scholar]
- 56.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures--the public health disparities geocoding project (US) Public Health Rep. 2003 May-Jun;118(3):240–260. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Laumann EO, Youm Y. Racial/Ethnic Group Differences in the Prevalence of Sexually Transmitted Diseases in the United States: A Network Explanation. Sex Transm Dis. 1999;26(5):250–261. doi: 10.1097/00007435-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 58.Wallace R, Wallace D. U.S. apartheid and the spread of AIDS to the suburbs: a multi-city analysis of the political economy of spatial epidemic threshold. Soc Sci Med. 1995 Aug;41(3):333–345. doi: 10.1016/0277-9536(94)00349-x. [DOI] [PubMed] [Google Scholar]
- 59.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005 Feb 1;191(Suppl 1):S115–122. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- 60.Ford CL, Daniel M, Miller WC. High rates of HIV testing despite low perceived HIV risk among African-American sexually transmitted disease patients. J Natl Med Assoc. 2006 Jun;98(6):841–844. [PMC free article] [PubMed] [Google Scholar]
- 61.Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health. 2007 Oct;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kowalewski MR, Henson KD, Longshore D. Rethinking perceived risk and health behavior: a critical review of HIV prevention research. Health Educ Behav. 1997;24(3):313–325. doi: 10.1177/109019819702400305. [DOI] [PubMed] [Google Scholar]
- 63.Thrasher AD, Ford CL, Nearing KA. Cost-effectiveness of screening for HIV. N Engl J Med. 2005 May 19;352(20):2137–2139. author reply 2137-2139. [PubMed] [Google Scholar]
- 64.Griffith DM, Mason M, Yonas M, et al. Dismantling institutional racism: Theory and action. Am J Community Psychol. 2007;39(3-4):381–392. doi: 10.1007/s10464-007-9117-0. [DOI] [PubMed] [Google Scholar]
- 65.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003 Feb;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS® system. Cary, NC: SAS Institute; 2000. Generalized Estimating Equations; p. 254. [Google Scholar]
- 67.Bond L, Lauby J, Batson H. HIV testing and the role of individual- and structural-level barriers and facilitators. AIDS Care. 2005 Feb;17(2):125–140. doi: 10.1080/09541020512331325653. [DOI] [PubMed] [Google Scholar]
- 68.Fullilove RE. HIV prevention in the African-American community: Why isn't anybody talking about the elephant in the room? AIDScience. 2001;1(7):1–7. [Google Scholar]
- 69.Airhihenbuwa CO. Eliminating health disparities in the African American population: The interface of culture, gender and power. Health Educ Behav. 2006;33(4):488–501. doi: 10.1177/1090198106287731. [DOI] [PubMed] [Google Scholar]