Abstract
HCV/HIV co-infected patients who have failed prior HCV treatment with interferon (IFN)/ribavirin (RBV) may require subsequent treatment with new HCV protease inhibitors (PIs). We evaluated HCV NS3 diversity in 26 HIV co-infected patients on stable antiretroviral therapy (ART) who were treated with IFN/RBV. Plasma HCV RNA clonal analysis was performed. There was greater baseline NS3 diversity in nonresponse/relapse patients than in those with sustained virologic response. IFN/RBV did not result in significant changes in HCV protease gene diversity or significant HCV PI resistance mutations. In HIV co-infected patients receiving ART, the effect of prior IFN/RBV treatment on HCV NS3 will likely not impact potential HCV PI efficacy.
Keywords: Antiviral Agents, Genetic Variation, Hepatitis C, chronic, HIV, Serine Endopeptidases, Serine Proteinase Inhibitors
Background
Management of hepatitis C virus (HCV) has become increasingly important in HIV co-infected patients, in order to prevent HCV-related liver disease, hepatocellular carcinoma, and death. To date, HCV treatment has been comprised of pegylated interferon alfa (peg-IFN) and ribavirin-based therapy for at least 24 to 48 weeks. Important factors associated with achieving sustained virologic response (SVR) after HCV therapy are baseline HCV viral load and genotype. In addition, patients with HIV co-infection, particularly those with genotype 1 HCV, have significantly lower rates of treatment response compared to HCV mono-infected patients (40–50% SVR rates in genotype 1 mono-infected, vs. 15–30% in genotype 1 HIV co-infected) [1].
The N-terminal domain of nonstructural protein (NS)-3 encodes a serine protease, which catalyzes post-translational processing of the HCV polyprotein in a step crucial to the assembly and replication of viral particles. Several drugs targeting the HCV protease gene are currently in development. HCV protease inhibitors (PIs) block cleavage of nonstructural proteins, as well as restore innate, interferon-mediated host cellular responses to HCV replication [2], rapidly reducing levels of HCV viremia during PI exposure [3]. Boceprevir and telaprevir are two protease inhibitors that have demonstrated efficacy in treating both treatment-naïve and treatment-experienced genotype 1 HCV-infected patients. When combined with peg-IFN and ribavirin, these PIs resulted in significantly higher SVR rates (60–75%) in treatment-naïve genotype 1 HCV-infected subjects and in genotype 1 patients who previously failed interferon-based therapy [4–6]. Unfortunately, rapid emergence of PI resistance in the NS3 domain was found with PI monotherapy, requiring combination treatment with HCV PIs and peg-IFN/ribavirin.
Due to the error-prone HCV RNA polymerase and high replicative capacity, HCV circulates in individuals as closely-related yet distinct viruses, termed quasispecies. Factors such as immune pressure, viral kinetics, genotype and treatment impact genetic diversity. The NS3 region from genotype 1 mono-infected subjects has demonstrated significant variability at the amino acid (up to 10–11% variability for genotypes 1a/1b) and nucleotide sequence level (up to 26–30% variability) [7]. What impact such NS3 genetic diversity may have on the use of PIs, given emerging data on NS3 PI resistance mutations, is unknown.
Objectives
Further understanding of underlying NS3 diversity among previously treated and HIV co-infected populations is required. We previously evaluated NS3 diversity in co-infected patients initiating HIV antiretroviral therapy (ART) and found no significant effect of ART on HCV protease diversity [8]. Herein we evaluate the effect of interferon/ribavirin therapy on HCV NS3 protease gene sequence diversity and amino acid changes in HIV co-infected patients on ART.
Methods
The National Institute of Allergy and Infectious Diseases and Stanford University institutional review boards approved this study. Subjects were previously enrolled in two prospective studies analyzing HCV virologic responses to: peg-IFN alpha-2b (Peg-Intron; Schering-Plough, Kenilworth, NJ) 1.5μg/kg or peg-IFN alpha-2a (Pegasys; Roche Laboratories, Palo Alto, CA) 180μg subcutaneously weekly with ribavirin (Rebetrol; Schering-Plough) 400mg and 600mg every morning and evening for <75kg, or 600 mg twice per day for >75 kg; or albinterferon alfa-2b (Zalbin; Human Genome Sciences, Rockville, MD) 900 or 1200 μg every 2 weeks with 1000–1200 mg/day ribavirin twice daily, based on body weight. All subjects in our analysis were HCV genotype 1, HIV co-infected subjects receiving ART.
Subjects were evaluated for HCV quasispecies diversity at baseline (prior to initiation of interferon-based therapy) and at a follow-up time-point no more than 4 weeks after completion of HCV therapy. Outcomes were defined as SVR (undetectable HCV viral load 24 weeks after completion of therapy); virologic nonresponse (NR, detectable viral load throughout treatment, or <2 log10IU/mL reduction in HCV viral load at week 12 of treatment); or virologic relapse (R, viral load decline to undetectable during treatment, but subsequent detectable levels after treatment discontinuation). All patients with SVR attained undetectable HCV viral load at the follow-up time-point, thus were compared to NR/R only at baseline. Within the NR/R group, NS3 quasispecies variability at follow-up was compared to baseline to assess change in genetic diversity with therapy.
Clinical parameters
HCV genotyping was performed using the Versant HCV Genotype 2.0 (LiPA) assay (Siemens Healthcare Diagnostics, Deerfield, IL). Plasma HIV and HCV RNA quantification were performed using VERSANT RNA 3.0 HIV assay (Siemens Healthcare Diagnostics; Deerfield, IL; lower limit of detection (LLOD) 50 copies/mL) and Abbott HCV assay (Abbott; Abbott Park, IL; LLOD 20 copies/mL), respectively. CD4+ T cell counts were measured by flow cytometry.
HCV RNA amplification, cloning, and sequence analysis
HCV NS3 sequences from each patient were generated; approximately 20 clones per sample per time-point were sequenced. The RT-PCR reactions generated amplicons spanning nucleotides 3315–4298 of the HCV genome (NC_004102). Diversity, including differences in synonymous and nonsynonymous nucleotide differences (dS–dN) and normalized Shannon entropy, was analyzed using MEGA (version 4) software as previously described in detail [8].
Statistical analysis
Comparisons within groups (paired comparisons) or between groups (unpaired comparisons) were determined using Wilcoxon Signed-Rank Tests and Mann-Whitney U tests, respectively. Categorical measures between groups were determined using Fisher’s Exact Probability Test. All reported p values were two-tailed, and p <0.05 was considered significant.
Results
Twenty-six co-infected patients were evaluated; baseline demographics are presented in Table 1. The patients were predominantly male (96.2%), 46% were African-Americans and 42% Caucasian, with mean age of 45 years. Eleven patients had SVR and 15 were characterized as NR/R. Average time from baseline to end-of-treatment was 43 (SVR) and 38.3 weeks (NR/R), with median treatment duration of 48 weeks in both groups. Due to adverse events, 2/11 SVR patients received 18–24 weeks, and 7/15 NR/R subjects received 15–36 weeks due to virologic non-response or adverse events. SVR and NR/R groups were similar with respect to age, race, and baseline and follow-up CD4+ cell counts. NR/R patients had higher median baseline HCV viral loads (2.83 × 106 vs. 1.24 × 106 IU/mL, p=0.008) compared to SVR patients. In the NR/R group, there was a nonsignificant decrease in median HCV viral load after treatment (from 2.83 × 106 to 889.2 × 103 IU/mL); in addition, while decreased CD4+ cell counts were seen in both groups between baseline and follow-up, only the decline in the NR/R group was significant (610 vs. 435 cells/mL, p=0.04).
Table 1.
Patient Characteristics
| Characteristica | SVR (n = 11)b | NR/R (n = 15) b | P-valuec |
|---|---|---|---|
| Race (AA/total) | 4/11 | 8/15 | 0.4 |
| Sex (male/total) | 11/11 | 14/15 | 0.2 |
| Median Age, years (range) | 46 (29–62) | 44 (33–69) | 0.9 |
| Median Weeks of Treatment, weeks (range) | 48 (18–48) | 48 (15–48) | 0.3 |
| HIV Viral Load (undetectable/total) | |||
| Baseline | 4/11 | 12/15 | 0.04* |
| Follow-Up | 9/11 | 14/15 | 1.0 |
| P-value | 0.08 | 1.0 | |
| Median HCV Viral Load, IU/mL | |||
| Baseline (range) | 1,243,840 (69,462–2,369,000) | 2,827,770 (981,147–12,190,100) | 0.008* |
| Follow-Up (range) | <20 (n/a) | 889,292 (<20–16,035,500) | -- |
| P-value | -- | 0.05 | |
| Median CD4 Cell Counts, cells/mL | |||
| Baseline (range) | 483 (127–778) | 610 (108–1396) | 0.2 |
| Follow-Up (range) | 311 | 435 (117–640) | 0.2 (120–1123) |
| P-value | 0.07 | 0.04* | |
AA, African American; M, male.
SVR, sustained virologic response; NR, nonresponse; R, relapse.
Asterisk (*) denotes a P-value with significance of <0.05.
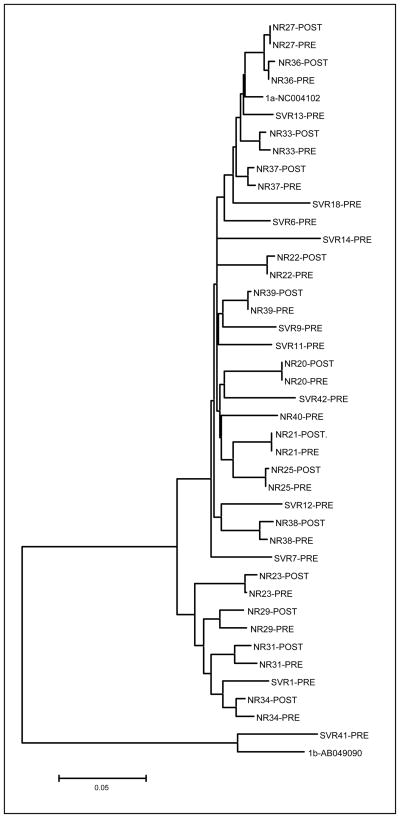
Genetic diversity and complexity measures were calculated from nucleotide sequences of 903 NS3 gene clones (median 23 clones per patient time-point; range 13–30 clones). There was no difference in the number of clones analyzed per patient per time-point between the two groups or between time-points within the NR/R group. All clones phylogenetically clustered appropriately by patient, and all patients’ sequences segregated appropriately by genotype (data not shown).
Differences in the genetic variability and complexity between patients at the nucleotide and amino acid level are shown in Table 2. At the nucleotide level, there was no significant difference in NS3 gene genetic distances between baseline and follow-up (0.012 at baseline, vs. 0.007 at follow-up, p=0.21) in the NR/R group. Similarly, there was no significant change in dS/dN between baseline and post-HCV treatment time-points.
Table 2.
Comparison of HCV NS3 gene quasispecies parameters in HIV/HCV co-infected patients
| Parametera | Non-response/Relapse (NR/R) |
Sustained Virologic Response (SVR) |
|||
|---|---|---|---|---|---|
| Pre-Treatment (n = 15) | Follow-Up (n = 14) | P-valueb | Pre-Treatment (n = 11) | P-valuec | |
| Genetic Diversity (na) (range) | 0.012 (0.003–0.028) | 0.007 (0.001–0.029) | 0.21 | 0.003 (0.001–0.036) | 0.004 |
| dS/dN (na) (range) | 0.038 (0.007–0.100) | 0.023 (−0.001–0.098) | 0.67 | 0.005 (−0.006–0.046) | 0.008 |
| p-distance (aa) (range) | 0.006 (0.002–0.0017) | 0.003 (0.000–0.003) | 0.30 | 0.004 (0.000–0.005) | 0.009 |
na, nucleic acid; aa, amino acid.
Wilcoxon Signed Rank Test.
Compared to NR/R pre-treatment, Mann-Whitney U-test.
While no change in diversity was noted over time among the NR/R group, significant differences between the two outcome groups were seen with respect to baseline NS3 diversity. Greater baseline NS3 diversity was seen in patients who subsequently had NR/R responses, compared to those who had SVR outcomes (genetic distance 0.012 in NR/R vs. 0.003 in SVR, p=0.004; dS/dN 0.038 vs. 0.005, p=0.008).
At the amino acid level, diversity was evaluated by examining the p-distance between clones of each patient. Again, in NR/R patients there was no significant change in p-distance between the two time-points. However, the NR/R group p-distance was significantly higher at baseline compared to the SVR group (0.006 vs. 0.004, p=0.009).
NS3 amino acid changes were then examined for known resistance mutations and functional enzyme residues. No active site positions (H57, D81, S139) or metal-binding residues (C97, C99, C145, H149) had amino acid substitutions in any of the clones examined. In the NR/R group, two patients at baseline and 2 different patients at follow-up each had a single clone with the R155G substitution. Those with baseline R155G each had a different single, additional clone at baseline with a significant NS3 mutation (P88L and A156V). None of these persisted at both time-points. In the SVR group, all of the clones from one patient had a V36M mutation at baseline.
Discussion
Our study is the first to evaluate HCV NS3 sequence diversity in HIV co-infected patients and the relationship to interferon-based treatment. Our results indicate there is no significant effect of interferon/ribavirin therapy on NS3 quasispecies diversity in NR/R co-infected subjects. Major NS3 PI resistance or active site NS3 mutations were found rarely. These results suggest that prior HCV treatment with IFN/RBV would not appear to markedly impact the potential efficacy of subsequent HCV PI treatment in co-infected patients.
A significant association was seen between treatment failure and higher baseline NS3 diversity in this cohort of genotype 1 patients. Prior studies have demonstrated correlations between increased quasispecies variability in the HCV hypervariable region 1 (HVR1) at baseline and nonresponse to antiviral therapy in genotype 1 mono-infected patients [9]. Some studies demonstrate low baseline HVR1 genetic complexity, in addition to other factors such as baseline viral load, predict interferon response [10]; whereas other studies have found a quasispecies complexity correlates with early, but not sustained, virologic response [11–12]. Similar observations have been made with other genotypes and interferon-treated HIV co-infected subjects [13]. These studies suggest that HVR1 complexity and diversity, via host selection pressure or other factors, influences interferon responsiveness. In contrast, fewer studies have evaluated associations between NS3 quasispecies diversity and interferon response, and none have been described in a co-infected population. Among mono-infected patients, Donlin et al. evaluated full HCV open-reading frame consensus sequences from genotype 1a/1b patients and found - in contrast to our results–that marked, versus poor, virologic response at day 28 of HCV therapy was associated with lower NS3 diversity [14]. Of note, significantly lower baseline HCV viral loads were seen among responders and correlated with interferon response.
PI mutations seen in our study included V36M, P88L, R155G, and A156V. V36M confers low-moderate resistance to telaprevir, and higher level resistance in conjunction with R155K or A156T; it has also been noted at low frequencies (<1%) in PI treatment-naïve patients. A156V is associated with resistance to multiple PIs, including telaprevir; whereas a different substitution at this site, A156T, confers high-level resistance to boceprevir and telaprevir. R155G is a minor variant of unclear significance that emerges after PI use and may confer low-level telaprevir resistance. R155K/T, however, is a common resistance mutation for multiple PIs, particularly telaprevir [15]. P88L has been noted after exposure to the now-discontinued BILN-2061, and has unclear significance for current PIs. Thus, NS3 resistance mutations are occasionally found in PI-naïve patients; however, IFN/RBV treatment does not appear to select for these mutations or increase their prevalence.
Our results are potentially limited by the small sample size in each group. Thus, we were unable to evaluate NS3 diversity differences between genotype 1a and 1b. Significantly more NR/R patients had baseline undetectable HIV viral load; however, HIV RNA has not been found to correlate with HCV diversity. While NS3 diversity was higher among NR/R subjects, HCV viral load was also higher in this group. In accordance with prior studies, lower HCV viral load was independently associated with response. However, our primary analysis was not affected, as no significant NS3 diversity changes were noted in the NR/R group with treatment. Of note, we acknowledge that recent use of ultra-deep sequencing suggests prevalence of minor variants in even treatment-naïve HCV patients; however, the impact of such low-frequency resistance mutations on PI treatment efficacy is unstudied and comparisons between clonal analysis and deep sequencing have not yet been made.
In summary, we found no significant effect of HCV interferon-based therapy on NS3 protease sequence diversity or sequence mutations in our cohort of genotype 1 HIV co-infected patients. As HCV PIs are introduced in clinical practice, further understanding of HCV NS3 diversity in this therapeutically challenging co-infected population is needed. However, our results indicate that the potential efficacy of HCV PIs will be unaffected by previous HCV treatment in co-infected patients.
Figure 1.
Phylogenetic tree of NS3 gene consensus sequences of HIV/HCV co-infected patients
Acknowledgments
Financial support: This study was supported in part by a grant from the Department of Veterans Affairs and by the Intramural Research Program of the NIH [National Institute of Allergy and Infectious Diseases and NIH Clinical Center].
Footnotes
Potential conflicts of interest: All authors: No conflicts.
Disclaimer: The content of this publication does not necessarily reflect the views of policies of the Department of Health and Human Services or the Department of Veterans Affairs, nor does mention of trade names, commercial products or organizations imply endorsement by the U.S. Government.
References
- 1.Ghany M, Strader D, Thomas D, Seeff L. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49(4):1335–74. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foy E, Li K, Sumpter R, Jr, et al. Control of antiviral defenses through hepatitis C virus disruption of retinoic acid-inducible gene-I signaling. Proc Natl Acad Sci U S A. 2005;102(8):2986–91. doi: 10.1073/pnas.0408707102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamarre D, Anderson P, Bailey M, et al. An NS3 protease inhibitor with antiviral effects in humans infected with hepatitis C virus. Nature. 2003;426(6963):186–9. doi: 10.1038/nature02099. [DOI] [PubMed] [Google Scholar]
- 4.Kwo P, Lawitz EJ, McCone J, et al. HCV SPRINT-1: Final results SVR 24 boceprevir plus peginterferon alfa-2B/ribavirin HCV 1 treatment naive patients [abstract 4]. Programs and abstracts of the 44th Annual Meeting of the European Association For The Study Of The Liver; Copenhagen, Denmark. 2009. [Google Scholar]
- 5.McHutchison JG, Everson GT, Gordon SC, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360(18):1827–38. doi: 10.1056/NEJMoa0806104. [DOI] [PubMed] [Google Scholar]
- 6.McHutchison J, Manns M, Muir A, et al. PROVE 3 Final results and 1-Year durability of SVR with telaprevir-based regimen in hepatitis C genotype 1-infected patients with prior non-response, viral breakthrough or relapse to peginterferon-alfa-2a/b and ribavirin therapy [abstract 66]. Programs and abstracts of the 60th Annual Meeting of the American Association for the Study of Liver Diseases; Boston, MA. 2009. [Google Scholar]
- 7.Holland-Staley CA, Kovari LC, Golenberg EM, Pobursky KJ, Mayers DL. Genetic diversity and response to IFN of the NS3 protease gene from clinical strains of the hepatitis C virus. Arch Virol. 2002;147(7):1385–406. doi: 10.1007/s00705-002-0807-5. [DOI] [PubMed] [Google Scholar]
- 8.Winters MA, Chary A, Eison R, Asmuth D, Holodniy M. Impact of highly active antiretroviral therapy on hepatitis C virus protease quasispecies diversity in HIV co-infected patients. Journal of Medical Virology. 2010;82:791–798. doi: 10.1002/jmv.21679. [DOI] [PubMed] [Google Scholar]
- 9.Morishima C, Polyak S, Ray R, et al. Hepatitis C virus-specific immune responses and quasi-species variability at baseline are associated with nonresponse to antiviral therapy during advanced hepatitis C. J Infect Dis. 2006;193(7):931–40. doi: 10.1086/500952. [DOI] [PubMed] [Google Scholar]
- 10.Salmeron J, Casado J, de Rueda P, et al. Quasispecies as predictive factor of rapid, early and sustained virological responses in chronic hepatitis C, genotype 1, treated with peginterferon-ribavirin. Journal of Clinical Virology. 2008;41(4):264–9. doi: 10.1016/j.jcv.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 11.Abbate I, Lo Iacono O, Di Stefano R, et al. HVR-1 quasispecies modifications occur early and are correlated to initial but not sustained response in HCV-infected patients treated with pegylated- or standard-interferon and ribavirin. J Hepatol. 2004;40(5):831–6. doi: 10.1016/j.jhep.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Chambers TJ, Fan X, Droll DA, et al. Quasispecies heterogeneity within the E1/E2 region as a pretreatment variable during pegylated interferon therapy of chronic hepatitis C virus infection. J Virol. 2005;79(5):3071–83. doi: 10.1128/JVI.79.5.3071-3083.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shire N, Horn P, Rouster S, Stanford S, Eyster ME, Sherman K. HCV kinetics, quasispecies, and clearance in treated HCV-infected and HCV/HIV-1-coinfected patients with hemophilia. Hepatology. 2006;44(5):1146–57. doi: 10.1002/hep.21374. [DOI] [PubMed] [Google Scholar]
- 14.Donlin MJ, Cannon NA, Yao E, et al. Pretreatment sequence diversity differences in the full-length hepatitis C virus open reading frame correlate with early response to therapy. J Virol. 2007;81(15):8211–24. doi: 10.1128/JVI.00487-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson AJ, McHutchison JG. Antiviral resistance and specifically targeted therapy for HCV (STAT-C) J Viral Hepat. 2009;16(6):377–87. doi: 10.1111/j.1365-2893.2009.01124.x. [DOI] [PubMed] [Google Scholar]