Abstract
Objectives
The objectives of this study were to examine the type and frequency of symptoms in patients hospitalized with acute heart failure (HF) as well as the relation between symptom patterns and patient characteristics, treatment practices, and hospital outcomes in patients hospitalized with decompensated HF.
Methods
The study sample consisted of 4,537 residents of the Worcester (MA) metropolitan area hospitalized for decompensated HF at 11 greater Worcester medical centers in 1995 and 2000.
Results
The average age of the study sample was 76 years, the majority (57%) were women, and three quarters of our patient population had been previously diagnosed with HF. Dyspnea (93%) was the most frequent complaint reported by patients followed by the presence of peripheral edema (70%), cough (51%), orthopnea (37%), and chest pain/discomfort (30%). Patients reporting few cardiac symptoms were less likely to be treated with effective cardiac therapies during hospitalization than patients with multiple cardiac signs and symptoms, and experienced higher hospital (9.7% vs 7.7%) as well as 30 day (17.1% vs 10.2%) death rates (p<.05).
Conclusions
The results of this study in residents of a large New England community suggest that patients with fewer reported symptoms of decompensated HF were less likely to receive effective cardiac treatments and had worse short-term outcomes. Reasons for these differences in treatment practices and short-term outcomes need to be elucidated and attention directed to these high risk patients.
Keywords: acute heart failure, symptoms, population-based study
Introduction
Despite the increasing prevalence of heart failure (HF) in the U.S., and the considerable morbidity, mortality, and functional disability associated with this clinical syndrome, there is a limited literature describing the symptoms associated with acute HF. The association between patients' symptoms of acute HF, their demographic and clinical characteristics, treatment practices, and short-term outcomes has also been infrequently examined, particularly from the more generalizable perspective of a population-based investigation. Knowledge and awareness of the signs and symptoms of HF by patients, their relatives and close acquaintances, as well as their health care providers is important for enhancing patient's care seeking behavior and institution of early treatment approaches to reduce the exacerbations of, and complications associated with, HF.
The purpose of this study was to describe the type and frequency of various signs and symptoms related to HF in residents of a large New England metropolitan area hospitalized at all area medical centers with decompensated HF [1-3]. Our secondary study objectives were to examine the association between signs and symptoms of acute HF with patients' demographic and clinical characteristics as well as with hospital treatment practices and short-term death rates.
Methods
Residents of the Worcester (MA) metropolitan area (2000 census estimate = 478,000) hospitalized for possible HF at all 11 greater Worcester medical centers during 1995 and 2000 comprised the study sample [1-3]. In brief, the medical records of patients with primary and/or secondary International Classification of Disease (ICD)-9 discharge diagnoses consistent with the possible presence of decompensated HF were reviewed by trained nurse and physician abstractors [1-3]. The primary International Classification of Disease (ICD)-9 code reviewed for the identification of cases of acute HF was ICD code 428. Confirmation of the diagnosis of HF, based on use of the Framingham criteria, required the presence of 2 major criteria or 1 major and 2 minor criteria [4,5] (Appendix). Examples of the major criteria included paroxysmal nocturnal dyspnea, cardiomegaly, and neck vein distention, while examples of the minor criteria included bilateral ankle edema and a night cough.
Information was collected about patients' demographic and clinical characteristics through the review of hospital medical records. Information about prior comorbidities, including a history of HF, was obtained through the review of hospital charts as noted by the attending physicians. Emergency department physicians' and nurses' notes were reviewed to identify patients' presenting signs and symptoms. Information on a total of 14 acute clinical signs and symptoms was collected. These included abdominal pain, angina/chest pain, ascites, cough, dyspnea, edema, fatigue, mental obtundation, nausea/vomiting, nocturnal paroxysms, orthopnea, palpitations, weakness, and weight gain. Classification of these signs and symptoms was based on any mention of its presence as opposed to the documentation of the absence of said finding. Information about hospital treatment practices, lifestyle recommendations by health care providers, and hospital case-fatality rates was also obtained through the retrospective review of hospital records [2]. Patients who developed HF secondary to admission for another illness (e.g., acute myocardial infarction), or after an interventional procedure (e.g., percutaneous coronary intervention), were not included.
Differences in the characteristics, as well as hospital treatment practices and short-term (hospital and 30 days after admission) death rates, of patients presenting with few (≤2 of the 5 most frequent signs and symptoms reported by patients and ≤3 of the total number of 14 signs and symptoms examined) versus multiple acute HF related symptoms were examined through the use of chi-square tests and t-tests for discrete and continuous variables, respectively.
Logistic regression analyses were utilized to examine the association between number of signs and symptoms of acute HF at the time of hospital presentation with a variety of patient associated characteristics as well as with hospital treatment regimens and short-term death rates. Factors included for consideration in this analysis were included in our regression models based on their associations with prognosis in the setting of HF from prior publications as well as on the basis of their univariate association (p<.20) with hospital and 30 day death rates and differences between patients with few and multiple signs and symptoms of HF (Table 2). For each of the physiologic variables examined, we created quartiles based on commonly utilized cutpoints to make our findings more interpretable. We categorized the individual comorbid conditions into a frequency count of these aggregated comorbidities (e.g., HF, diabetes, coronary heart disease) to make our analytical models more robust and our findings more easily interpretable. Despite the nonrandomized nature of the present study, and potential for confounding by medication indication, we also controlled for the receipt of hospital treatment practices in our regression analyses. Collection of information about 30 day post admission survival status was obtained through the review of hospital medical records and review of state and local death certificates on all study patients.
Table 2. Characteristics of Patients Hospitalized With Acute Heart Failure According to Frequency of Acute Symptoms.
| Characteristic |
Five Most Commonly Reported Symptoms | All Symptoms Examined | ||||
|---|---|---|---|---|---|---|
| Few acute symptoms* (n=1,836) |
Multiple acute symptoms (n=2,701) |
p value |
Few acute symptoms† (n=2,028) |
Multiple acute symptoms (n=2,509) |
p value |
|
| Age (mean, yrs) | 77.4 | 75.1 | <.001 | 76.7 | 75.6 | <.005 |
| Male (%) | 39.7 | 45.5 | <.001 | 41.9 | 44.2 | 0.13 |
| Caucasian (%) | 95.0 | 93.6 | 0.43 | 94.6 | 93.8 | 0.53 |
| Body mass index (%) | ||||||
| 25-29.9 | 27.0 | 27.1 | <.001 | 26.7 | 27.3 | <.001 |
| ≥30 | 20.1 | 32.7 | 24.5 | 30.3 | ||
| Co-morbid condition count (%) | ||||||
| 0-2 | 26.9 | 22.0 | 25.6 | 22.6 | ||
| 3-5 | 57.4 | 58.9 | <.001 | 57.4 | 59.0 | <0.05 |
| ≥6 | 15.7 | 19.1 | 17.0 | 18.4 | ||
| Hospital admission findings (mean) | ||||||
| Systolic blood pressure (mmHg) | 142.8 | 145.9 | <.05 | 144.8 | 144.5 | 0.70 |
| Diastolic blood pressure (mmHg) | 75.7 | 77.5 | <.01 | 76.9 | 76.7 | 0.68 |
| Heart rate (bpm) | 91.0 | 90.5 | 0.48 | 91.1 | 90.4 | 0.34 |
| Laboratory measures (mean, mg/dl) | ||||||
| Blood urea nitrogen | 36.0 | 33.3 | <.005 | 34.2 | 34.6 | 0.62 |
| Creatinine | 1.7 | 1.6 | <.005 | 1.6 | 1.6 | 0.59 |
| Sodium | 137.4 | 137.2 | 0.18 | 137.4 | 137.1 | 0.13 |
≤2 vs. ≥3 of the 5 most commonly reported acute symptoms
≤3 vs ≥4 of the 14 total acute symptoms examined
Results
A total of 4,537 residents of the Worcester metropolitan area were hospitalized with confirmed acute HF at all greater Worcester medical centers during the 2 study years of 1995 and 2000. The average age of study patients was 76 years, more than one-half were women, and the vast majority were Caucasian (Table 1). Approximately three quarters of the study sample had been previously diagnosed with HF.
Table 1. Demographic and Clinical Characteristics of the Study Sample.
| Characteristic | n | % |
|---|---|---|
| Age (mean, yrs) | 4,534 | 76.0 |
| Age (yrs) | ||
| <65 | 675 | 14.9 |
| 65-74 | 1,040 | 22.9 |
| 75-84 | 1,731 | 38.2 |
| ≥85 | 1,088 | 24.0 |
| Male | 4,537 | 43.2 |
| Caucasian | 4,537 | 94.2 |
| Body mass index (mean) | 3,722 | 27.7 |
| Comorbidities | ||
| Anemia | 4,537 | 23.5 |
| Chronic lung disease | 4,537 | 34.8 |
| Coronary heart disease | 4,537 | 56.8 |
| Diabetes | 4,537 | 39.9 |
| Heart failure | 4,537 | 74.6 |
| Hyperlipidemia | 4,537 | 20.1 |
| Hypertension | 4,537 | 65.2 |
| Myocardial infarction | 4,537 | 47.9 |
| Renal failure/disease | 4,537 | 23.3 |
| Stroke | 4,537 | 14.6 |
| Physiologic findings (mean) | ||
| Systolic blood pressure (mmHg) | 4,524 | 144.6 |
| Diastolic blood pressure (mmHg) | 4,470 | 76.8 |
| Heart rate (bpm) | 4,532 | 90.7 |
| eGFR | 4,472 | 63.1 |
| Blood urea nitrogen (mg/dl) | 4,482 | 34.4 |
| Serum sodium (mg/dl) | 4,495 | 137.2 |
| Died during hospitalization | 4,537 | 6.8 |
Frequency of Signs and Symptoms of Decompensated HF
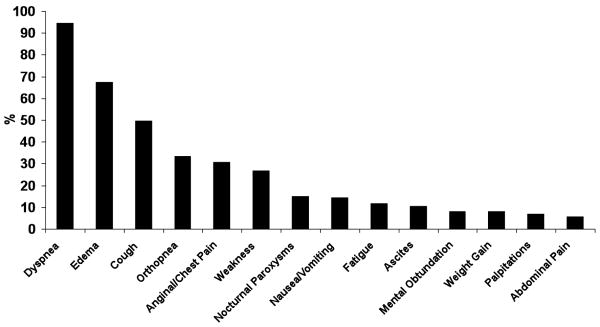
Dyspnea was reported by the vast majority (93%) of study patients as documented in hospital charts (Figure 1). The presence of edema (70%), cough (51%), orthopnea (37%), and chest pain/discomfort (30%) were the next most commonly reported symptoms. The frequency of these symptoms was not appreciably changed when we examined the occurrence of these symptoms in patients with a first episode of HF (Figure 1).
Figure 1.
Distribution of Selected Signs and Symptoms in Patients With Acute Heart Failure
We examined the frequency of multiple signs and symptoms associated with acute HF based on information contained in hospital medical records. Approximately 1 in every 20 patients reported having only 1 acute sign or symptom present, 1 in 4 experienced any 3 acute symptoms, and approximately 1 in 3 reporting experiencing any 5 or more of the 14 signs or symptoms examined; only 15% of hospitalized patients reported experiencing 6 or more of these symptoms. A similar profile of signs and symptoms was observed in patients with a first hospitalized episode of HF.
When we restricted our analysis to the 5 most commonly reported symptoms of decompensated HF, namely shortness of breath, edema, cough, orthopnea, and chest discomfort, 29% of all patients reported the presence of any 2 of these symptoms, 35% reported any 3 of these symptoms, while 24% reported 4 or more of these signs and symptoms.
Characteristics of Patients According to Frequency of Acute Signs and Symptoms
In examining the characteristics of patients experiencing relatively few acute symptoms (≤2 of the 5 most frequent signs and symptoms) as compared to those experiencing multiple (≥3) of the 5 most frequent symptoms reported, patients reporting few acute symptoms were relatively older, more likely to be a woman, but less likely to be overweight or have had selected comorbidities previously diagnosed (Table 2). Patients who reported the presence of 2 or fewer of these symptoms were significantly more likely to have presented with lower blood pressures, and have higher serum levels of blood urea nitrogen and creatinine, than patients with multiple acute signs and symptoms. Relatively similar trends were observed when we examined the distribution of these factors in patients who experienced 3 or fewer of all acute signs and symptoms examined in comparison to those who reported 4 or more of these 14 signs and symptoms (Table 2).
The results of a logistic regression analysis, which included factors associated with the symptoms under study based on their univariate associations and prior findings from the published literature, suggested that relatively older patients, women, those of normal or low body weight, and those with fewer comorbidities present were significantly more likely to report fewer acute symptoms (of the 5 most common symptoms reported) than respective comparison groups (Table 3). Patients with higher levels of systolic blood pressure and those with higher eGFR findings were less likely to report fewer acute symptoms. Relatively similar factors were associated with the reporting of 3 or fewer, compared to 4 or more, of the 14 total symptoms examined, though the statistical significance of several of these factors was attenuated.
Table 3. Factors Associated with Multiple Heart Failure Related Symptoms.
| Characteristic∞ |
Five Most Commonly Reported Symptoms* | All Symptoms Examined† | ||
|---|---|---|---|---|
| Adjusted O.R. |
95% C.I. |
Adjusted O.R. |
95% C.I. |
|
| Age (yrs) | ||||
| 65-74 | 1.25 | 1.01,1.54 | 1.23 | 1.01,1.51 |
| 75-84 | 1.33 | 1.09,1.62 | 1.16 | 0.96,1.39 |
| ≥85 | 1.38 | 1.11,1.71 | 1.20 | 0.98,1.47 |
| Male | 0.76 | 0.67,0.86 | -- | -- |
| Length of hospital stay (≤4 or 5 days) | 0.83 | 0.73,0.94 | -- | -- |
| Body mass index | ||||
| 25-29.9 | 0.79 | 0.68,0.92 | 0.78 | 0.67,0.90 |
| ≥30 | 0.50 | 0.42,0.58 | 0.66 | 0.56,0.77 |
| Co-morbid condition count (%) | ||||
| 3-5 | 0.77 | 0.66,0.89 | 0.86 | 0.74,0.99 |
| ≥6 | 0.64 | 0.51,0.77 | 0.83 | 0.69,1.00 |
| Hospital admission findings | ||||
| Systolic blood pressure (mmHg) | ||||
| 120-139 | 0.96 | 0.80,1.16 | ||
| 140-159 | 0.90 | 0.74,1.09 | ||
| ≥160 | 0.81 | 0.66,0.99 | ||
| Diastolic blood pressure (mmHg) | ||||
| 60-79 | 0.80 | 0.67,0.96 | ||
| 80-99 | 0.86 | 0.71,1.05 | ||
| ≥100 | 0.94 | 0.72,1.22 | ||
| BUN (mg/dl) | ||||
| 30-39 | 0.95 | 0.78,1.15 | ||
| 40-49 | 0.86 | 0.68,1.10 | ||
| ≥50 (ml/min/1.73m2) | 1.04 | 0.84,1.30 | ||
| eGFR | ||||
| 30-59 | 0.80 | 0.65,0.98 | ||
| ≥60 | 0.68 | 0.54,0.85 | ||
2 or fewer of the 5 most commonly reported acute symptoms
3 or fewer of the 14 total acute signs and symptoms examined
reference groups: age <65 years, female, length of hospital stay >5 days, body mass index <25, 0-2 co-morbid conditions, systolic blood pressure <120 mmHg, diastolic blood pressure <60 mmHg, BUN <30 mg/dl, eGFR <30 (ml/min/1.73m2).
O.R. = odds ratio
C.I. = confidence interval
Hospital Treatment Practices and Frequency of HF Signs and Symptoms
Residents of the Worcester metropolitan area who presented to central Massachusetts medical centers with 2 or fewer of the 5 most frequent symptoms examined were less likely to be treated with effective cardiac medications than patients who reported a greater number of acute symptoms (Table 4). These patients were also less likely to have been told by their healthcare providers to carry out various lifestyle changes than patients who presented with multiple HF related symptoms. Relatively similar treatment and lifestyle practice recommendations were observed in patients who reported 3 or fewer of the total number of acute symptoms examined (Table 4).
Table 4. Hospital Treatment Practices According to Frequency of Symptoms of Acute Heart Failure.
| Five Most Commonly Reported Symptoms | All Symptoms Examined | |||
|---|---|---|---|---|
| Few acute symptoms* (n=1,836) | Multiple acute symptoms (n=2,701) | Few acute symptoms† (n=2,028) | Multiple acute symptoms (n=2,509) | |
| Medications (%) | ||||
| ACE inhibitors/ARB's | 50.5°° | 55.6 | 51.5° | 55.2 |
| Beta blockers | 39.1° | 42.0 | 40.0 | 41.5 |
| Both therapies | 21.5° | 24.4 | 22.7 | 23.6 |
| Digoxin | 49.3 | 51.3 | 48.9 | 51.8 |
| Diuretics | 96.9°° | 98.3 | 97.1° | 98.3 |
| Lifestyle Recommendations (%) | ||||
| Limit salt intake | 72.2°°° | 85.7 | 74.9°°° | 84.6 |
| Fluid restriction | 17.6°°° | 23.8 | 17.8°°° | 24.2 |
| Smoking cessation | 0.7°° | 1.5 | 0.6°° | 1.6 |
| Increase physical activity | 38.1°°° | 44.0 | 39.7° | 43.1 |
| Limit alcohol consumption | 0.3°° | 1.0 | 0.4° | 1.0 |
P<.05;
P<.01;
P<.001
≤2 vs. ≥3 of the 5 most commonly reported acute symptoms
≤3 vs ≥4 of the 14 total acute symptoms examined
ACE = angiogtensin converting enzyme
ARB = angiotensin receptor blockers
Hospital and Thirty Day Death Rates
Hospital death rates were significantly higher in those who reported few (≤2 of the 5 most common signs and symptoms reported or ≤3 of all signs and symptoms examined) acute symptoms (9.7% and 7.7%, respectively) as compared to those who reported the presence of more of these symptoms (4.8% and 6.1%, respectively). Thirty day death rates after hospital admission were also higher in patients who reported fewer of the most common symptoms reported as compared to those who reported many of the most common symptoms examined (17.1% vs 10.2%) (p<.05).
In addition to the univariate association between the various signs and symptoms of acute HF with hospital and 30 day death rates, we carried out a series of multivariable adjusted regression analyses for purposes of controlling for selected covariates in more systematically examining this association. These variables were controlled for either because they differed between our primary comparison groups (e.g., few vs. more frequent symptoms) or because they had been shown to be of prognostic importance based on findings from the published literature. The results of our regression analyses showed that hospital death rates remained significantly higher in those who reported few, as compared to those who reported the presence of multiple, acute symptoms, with the strongest associations observed when we examined the 5 most commonly reported acute symptoms (Table 5). Similar associations were observed when we examined 30 day death rates, particularly among those who reported ≤2, as compared to 3 or more, of the 5 most commonly reported symptoms. There were no significant differences in the 30 day death rates of those who reported few, as compared to those who reported more, of the 14 total acute symptoms examined (Table 5). Adjustment for hospital treatment practices in each of our regression models resulted in considerable attenuation of our observed findings.
Table 5. Frequency of Symptoms of Acute Heart Failure and Short-Term Mortality.
| Hospital Death Rates | 30 Day Death Rates | |||
|---|---|---|---|---|
| Few acute symptoms* | Few acute symptoms† | Few acute symptoms* | Few acute symptoms† | |
| Controlling variables |
||||
| ▪Age and sex | 2.06 (1.62,2.61) |
1.27 (1.00,1.60) |
1.73 (1.45,2.06) |
1.18 (0.99,1.40) |
| ▪Age, sex, and prior comorbidities1 | 1.82 (1.43,2.33) |
1.16 (0.91,1.47) |
1.55 (1.29,1.86) |
1.08 (0.90,1.29) |
| ▪Age, sex, prior comorbidities, and physiologic findings2 | 1.74 (1.35,2.26) |
1.12 (0.87,1.45) |
1.45 (1.19,1.76) |
1.04 (0.86,1.26) |
| ▪Age, sex, prior comorbidities, physiologic findings, and hospital treatment practices3 | 1.44 (1.80,1.88) |
0.98 (0.75,1.27) |
1.28 (1.05,1.56) |
0.94 (0.77,1.15) |
| ▪All variables univariately related to death | 1.78 (1.40,2.27) |
1.15 (0.90,1.45) |
1.52 (1.27,1.83) |
1.07 (0.89,1.28) |
≤ 2 vs ≥3 of the 5 most commonly reported acute symptoms
≤3 vs ≥4 of the 14 total acute symptoms examined
prior comorbidities = BMI, prior anemia, angina, COPD, CHD, diabetes, HF, hyperlipidemia, MI, renal disease, stroke, and DNR orders
physiologic findings = Factors listed in regression #1 plus admission systolic and diastolic blood pressure, heart rate, eGFR, BUN, serum sodium, and white blood cell count
hospital treatment practices = Factors listed in regression #2 plus use of ACE inhibitors, ARB blockers, beta blockers, digoxin, diuretics, recommendation to reduce salt intake, fluid restriction, smoking cessation, increased physical activity, and alcohol reduction
Hospital death rates controlling variables = age, race, BMI, prior angina, CHD, diabetes, hyperlipidemia, hypertension, MI and DNR orders.
30 day death rates controlling variables = age, race, BMI, prior anemia, angina, CHD, diabetes, CHF, hyperlipidemia, hypertension, MI, stroke and DNR orders.
Discussion
The results of our study in residents of a large central New England metropolitan area provide insights to the clinical symptoms associated with decompensated HF and the relation of these signs and symptoms to patients' demographic and clinical characteristics, treatment practices, and short-term outcomes. Our results suggest that many patients with HF present with multiple acute signs and symptoms, and the vast majority present with breathlessness and signs of congestion, and not those indicative of low cardiac output. That said, approximately 40% of patients reported 2 or fewer common symptoms of HF. Patients reporting fewer HF related symptoms were older and more likely to be female, less likely to have serious accompanying comorbidities, and were less likely to be treated with effective cardiac therapies. Symptom presentation was similar for patients with an initial or previously documented episode of HF and whether we examined the 5 most common symptoms reported by patients or all 14 of the acute signs and symptoms examined.
The profile of different symptoms, extent of delay in seeking medical care, and relation of acute symptoms to medical treatment and hospital outcomes in hospitalized patients with decompensated HF has not been examined in detail in the published literature. In prior studies based on the review of information contained in hospital medical records, which was similar to the approach utilized in the present investigation, the frequency and type of symptoms reported by patients with acute HF were similar to those observed in our population-based investigation [6-10]. For example, in a study based on the review of the medical records of 753 patients with HF who were hospitalized at a Veteran's Administration hospital, the most common symptoms reported by patients at the time of hospital admission were dyspnea, edema, and fatigue [7].
Heart failure is typically associated with multiple clinical signs and symptoms that can interact thereby affecting a patients' perception of some or all of these acute symptoms. The intensity, timing, level of distress, and quality of symptoms, as well as mismatch between the symptoms expected and those actually experienced, may each affect a patient's perception of, and responses to, their acute symptomatology [11]. Psychologic as well as situational factors may also influence the acute symptom experience and its interpretation. In our study, we found that patients' reporting of symptoms may also impact how they are treated once they seek medical attention.
Patients who reported fewer symptoms of acute HF were less likely to be treated with effective treatment regimens and use of different nonpharmacologic regimens. In addition, in both crude and multivariable adjusted analyses, our findings suggest that patients with fewer signs and symptoms of decompensated HF, particularly those related to the 5 most commonly reported symptoms, are at greater risk for dying during their acute hospitalization as well as during the first month of their hospital admission. It needs to be noted, however, and despite the nonrandomized nature of the present study which places appropriate caveats on the interpretation of our findings, that after adjustment for the receipt of various hospital treatment practices, the association between hospital and 30 day death rates became increasingly attenuated (especially for the 5 most commonly reported acute symptoms). These findings suggest that the failure to treat these patients with effective cardiac medications may lead to increased short-term death rates in this relatively under-recognized (e.g., fewer acute symptoms) patient population.
Numerous hypotheses can be offered for our observed findings. It is possible that patients reporting fewer acute symptoms may have experienced longer delays to hospital presentation, more atypical presentation, and more diagnostic uncertainty leading to possible delays in appropriate treatment and higher death rates. The observed differences in hospital treatment practices based on the number of symptoms reported by patients suggest that healthcare providers respond differently based on patients' symptom profile. It is also possible that the reporting of fewer symptoms is a marker for patients with more severe comorbidities, or even impaired cognition, that may impact subsequent survival. Further studies need to be carried out to understand the reasons for these observed associations including a more detailed assessment of the frequency, intensity, and duration of patient's symptoms and actions taken to seek acute medical care.
Study Strengths and Limitations
The strengths of the present study are the inclusion of all hospitalized patients with decompensated HF from a large New England metropolitan area, use of standardized criteria for confirmation of the diagnosis of HF, and inclusion of a wide variety of possible symptoms of HF. The limitations of this study include the reliance of information contained in hospital medical records and inability to separate the chief symptom complaint from more ancillary symptoms. Our study also does not necessarily confirm the absence of selected symptoms of acute HF, but merely the absence of documentation of the various symptoms examined. Due to the large amount of missing data on ejection fraction, we were unable to further classify patients into those with systolic from those with diastolic HF. Factors such as socioeconomic status, noncardiac disabilities, usual activity levels, prior treatment history, cognitive function, and a history of depression were unable to be examined in the present study. Our study sample was primarily Caucasian and the present findings may not apply to patients of other race/ethnicities.
Conclusions
The results of the present population-based study suggest that patients with acute HF present with many signs and symptoms of decompensation. Patients who report fewer symptoms tend to be older, female, have fewer comorbidities present, have lower prescription rates of HF therapy, and have worse short-term outcomes in comparison to patients who report the presence of multiple acute symptoms. These findings suggest that health care providers should pay particular attention to patients with acute HF who present with fewer symptoms of decompensated HF and increase their efforts of surveillance and targeted therapeutic approaches in these high risk patients.
Acknowledgments
Grant support for this project was provided by the National Heart, Lung, and Blood Institute (R37 HL69874).
Appendix
Framingham Heart Study Criteria
| Major | Minor |
|---|---|
|
|
Major or Minor
|
References
- 1.Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. Am J Med. 2005;118:728–734. doi: 10.1016/j.amjmed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg RJ, Spencer FA, Farmer C, Lessard D, Pezzella SM, Meyer T. Use of disease-modifying therapies in patients hospitalized with heart failure: a population-based perspective. Am J Med. 2007;120:98.e1–8. doi: 10.1016/j.amjmed.2006.05.051. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Ciampa J, Lessard D, Meyer TE, Spencer FA. Long-term survival after heart failure: a contemporary population-based perspective. Arch Intern Med. 2007;167:490–496. doi: 10.1001/archinte.167.5.490. [DOI] [PubMed] [Google Scholar]
- 4.Ho KKL, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: The Framingham Study. J Am Coll Cardiol. 1993;22(Suppl A):6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 5.Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol. 1999;33:1948–1955. doi: 10.1016/s0735-1097(99)00118-7. [DOI] [PubMed] [Google Scholar]
- 6.Friedman M. Older adults' symptoms and their duration before hospitalization for heart failure. Heart Lung. 1997;26:169–176. doi: 10.1016/s0147-9563(97)90053-4. [DOI] [PubMed] [Google Scholar]
- 7.Evangelista L, Dracup K, Doering L. Treatment-seeking delays in heart failure patients. J Heart Lung Transplant. 2000;19:932–938. doi: 10.1016/s1053-2498(00)00186-8. [DOI] [PubMed] [Google Scholar]
- 8.Schift GD, Fung S, Speroff T, McNutt RA. Decompensated heart failure: symptoms, patterns of onset, and contributing factors. Am J Med. 2003;114:625–630. doi: 10.1016/s0002-9343(03)00132-3. [DOI] [PubMed] [Google Scholar]
- 9.Parshall MB, Welsh JD, Brockopp DY, Heiser RM, Schooler MP, Cassidy KB. Dyspnea duration, distress and intensity in emergency department visits for heart failure. Heart, Lung. 2001;30:47–56. doi: 10.1067/mhl.2001.112492. [DOI] [PubMed] [Google Scholar]
- 10.Bekelman DB, Havranek EP, Becker DM, Kutner JS, Peterson PN, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007;13:643–648. doi: 10.1016/j.cardfail.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Horne R, James D, Petrie K, Weinman J, Vincent R. Patients' interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart. 2000;83:388–393. doi: 10.1136/heart.83.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]