SUMMARY
Context
Statin use and type has been variably associated with impaired or improved cognitive performance.
Objective
To assess the association of statin use and type (lipophilic vs hydrophilic) and cognitive impairment
Design
Cross-sectional analysis of 24595 (7191 statin users and 17404 non-users) participants (age >45), from a population-based national cohort study (REasons for Geographic And Racial Differences in Stroke) enrolled from January 2003-October 2008 with over-sampling from the southeastern Stroke Belt, and African Americans.
Main Outcomes
Statin use and type were documented in participants’ homes by a trained health professional. Cognitive performance was assessed with a prior validated instrument of global cognitive status (Six-Item Screener). Cognitive impairment was defined as a score of < 4. .
Results
Overall, an association of cognitive impairment and statin use was observed (8.6% of users vs 7.7% or non-users had cognitive impairment p=.014) but, after adjusting for variables known to be associated with cognition (age, gender, race, income, levels of education, and cardiovascular disease) the association was attenuated (OR 0.98, CI; 0.87;1.10). No association was observed between statin type (lipophilic vs hydrophilic) and cognition (OR 1.03, CI; 0.86;1.24), and there were no regional differences in cognitive impairment in statin users (8% in the stroke belt and 7.9% other regions p=0.63).
Conclusions
Statin use and type was marginally associated with cognitive impairment. After adjusting for known variables that affect cognition, no association was observed. No regional differences were observed. This large study found no evidence to support an association between statins and cognitive performance.
Keywords: Statins, Cognition
Cognitive impairment and decrements over time are associated with cardiovascular diseases such as hypertension and diabetes and with cerebrovascular changes such as white matter hyperintensities that are associated with an increased risk for stroke. Research suggests that the prevalence of cognitive impairment is associated with the number and severity of vascular risk factors,[1-4] which include hypercholesterolemia. Individuals with high levels of low density lipoproteins and triglycerides, and/or low levels of high density lipoprotein often receive statins as part of their treatment regimen.
The data are inconsistent as to whether statin use has any association with better or worse cognition. There is also controversy regarding the role of statin type (particularly lipophilic vs non-lipophilic statins, with the hypothesis that lipophilic statins are more likely to cross the blood-brain barrier and thus have more central nervous system effects) in these observations.[5-6] Understanding the relationship between statin use and global cognitive status, and whether this relationship is mediated by statin type, health behaviors, and cardiovascular risk factors, could help delineate the clinical significance of statin use on cognitive function. Questions have been raised regarding the association of cognition and lipid levels, themselves, irrespective of statin use, particularly high density lipoprotein – cholesterol (HDL-C) levels. Specifically, in 3 non-definitive studies, it has been suggested that low HDL-C is associated with cognitive impairment .[7]
It is in the above setting that we evaluated, from the REGARDS data base, the use and type of statin, and HDL-C, and their association with cognition as assessed by the Six-Item Screener of global cognitive status.
METHODS
Study Population
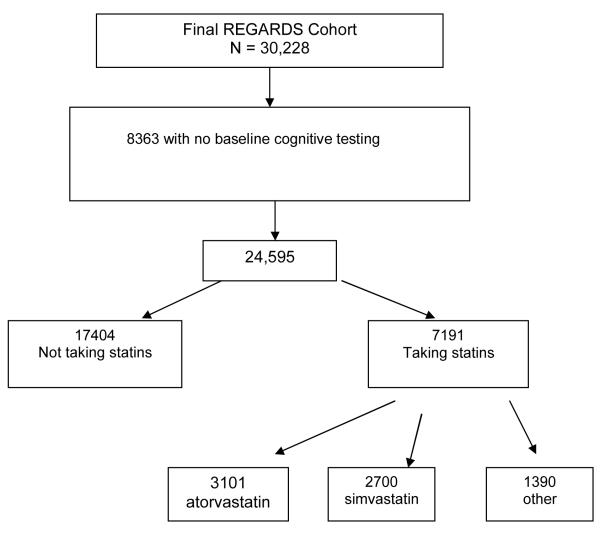
REGARDS is a national cohort of community dwelling individuals over age 45 years recruited with approximately equal representation of whites and blacks, men and women. Twenty percent of the sample was randomly selected from the “buckle” of the Stroke Belt (coastal plain region of North Carolina, South Carolina, and Georgia), 30% from the Stroke Belt states (remainder of North Carolina, South Carolina, and Georgia plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana), and the remaining 50% from the other 40 contiguous states. Individuals were identified from commercially available lists of residents, and recruited using an initial mailing followed by telephone contact. Defined according to standards recommended by Morton et al,[8] 64.6% of eligible individuals who were reached, agreed to participate (Figure 1).
Figure 1.
Exclusionary Cascade For Analysis of the Subpopulation
Demographic information, medical history, and cognitive assessment were obtained by trained interviewers using a computer-assisted telephone interview (CATI). Consent was obtained verbally by telephone and subsequently in writing during a follow-up in-home visit by a healthcare professional. A brief physical exam including anthropometric and blood pressure measurements, blood samples, and an electrocardiogram was conducted in-person, 3-4 weeks after the telephone interview. For the in-home visit, participants were asked to provide bottles of all medications (including over-the-counter ones) taken during the prior two weeks; medication names were recorded by the health professionals and later confirmed for the specific drug name. These were then coded into classes. Participants were followed by telephone at six-month intervals for surveillance of medical events including potential stroke events. The study methods were reviewed and approved by all involved Institutional Review Boards. Additional methodological details are provided elsewhere.[9] As of October 11, 2008, we had data on 24,595 participants. The primary predictor variables were the use of statins (yes, no) and type of statin (lipophilic, non-lipophilic. We considered lovastatin and simvastatin to be lipophilic and atorvastatin, pravastatin, fluvastatin, and rosuvastatin to be hydrophilic.
Cognitive Assessment
Cognitive assessment was conducted during the baseline telephone interview useing The Six-item Screener (SIS) which is designed for either in-person or telephone administration, and is a test of global cognitive function derived from the widely used Mini-Mental State examination.[10] The SIS has been validated against the Mini-1 Mental State examination, other cognitive measures, and diagnoses of dementia and non-dementia cognitive impairment in two populations: in a community-based survey of 344 black adults with a second-stage formal diagnostic evaluation and a clinical sample of 651 adults (16.1% black) with the same diagnostic evaluation.11 Items from the SIS assess recall and temporal orientation. Scores range from 0 to 6; a score of 4 or fewer correct answers indicates cognitive impairment.[5] A cutpoint of 4 or fewer correct had 74.2% sensitivity and 80.2 % specificity to clinically diagnosed CIND (Cognitive Impairment Not Demented). The same cutpoint was 96.8% sensitive and 68.6 specific to a diagnosis of dementia (a cutpoint of 3 or fewer correct had better specificity for dementia diagnosis). The SIS operates about as well as the widely used MMSE for identifying gross (but not subtle) cognitive deficits worthy of further evaluation. The SIS has since been used as an index of cognitive impairment in the context of depression treatment over a two-year period in a sample of 1,684 IMPACT study participants, and it has been validated against the MMSE and the Mini-Cog in two studies of older emergency department patients. [12]
The Six-item Screener used to assess cognitive status likely lacks sensitivity to subtle cognitive changes. Even so, previous findings from REGARDS attest to its utility in detecting broad patterns of association with conditions affecting cognition, such as traditional cardiovascular risk factors[13], chronic kidney disease[14], and congestive heart failure[15]. In addition, the rate of incident cognitive impairment we found using the SIS (approximately 4% annually) is comparable to annual incidence rates reported by studies that used detailed clinical diagnostic assessments for dementia (3.2%)[16,17] and mild cognitive impairment (5.1%)18]. Furthermore, associations of SIS performance with well-established risk factors for cognitive decline, such as age and education, were in the expected direction, lending support to the validity of the SIS. Between January 2003 and October 2008, 30,228 participants were enrolled. We included participants who completed the REGARDS Medications Inventory, including the Morisky Scale* a measure of medication adherence[19] (audited and recorded by Examination Management Services Inc –EMSI - examiners). The cognitive assessment was not added until January 2004, reducing the sample size to 24, 595 (figure 1).
*In the mid-1980s, Morisky and colleagues developed a brief questionnaire to aid practitioners in prospectively predicting adherence with antihypertensive medications. Subsequently, the instrument was validated in a number of studies and demonstrated to have good psychometric properties. To score the 4 point Morisky Scale, each question that is answered with a NO receives a score of 1. The possible scoring range is herefore 0 to 4. Patients with higher scores are predicted to be more dherent to prescribed medication therapies. Patients with lower scores are at greater risk for nonadherent behavior.
Statistical Analysis
Geographic and ethnic differences in statin use and statin type and their cross-sectional associations with measures of cognition were determined. We excluded individuals who lacked cognitive function measures. We examined frequency distributions of each variable and then examined bivariate relationships between the outcome and each covariate of interest using Pearson’s chi-square. Significance was set at p<0.05.
Logistic regression (PROC LOGISTIC in SAS 9.1 Cary, NC) was used to calculate odds ratios (ORs) and 95% confidence intervals (CI) for our multivariable models. Examining the potential for interaction by race, a p value of 0.34 was observed so stratified analyses were not performed. it should be noted that although race is a significant predictor of cognitive function, and the analysis has been adjusted for race, estimated racial differences in cognition are not provided as they do not affect the conclusions drawn in the paper. Variables were considered in a series of incremental models, first adjusting for demographic factors and then the other concomitant variables and diseases potentially associated with the outcome variable. Both a summary variable reflecting any use of a statin as well as a variable stratified by statin type was analyzed. Covariates included ethnicity, age, geographic location, race, urban/rural location, income, level of education, sex, Framingham Coronary Disease Risk (REF), or history of heart disease (MI, vascular disease, or vascular intervention; and EKG evidence of MI), and prior history of stroke (self-reported stroke or TIA). In addition we included systolic blood pressure, pulse pressure, total cholesterol, LDL-C and HDL-C as both continuous and discreet quartiles as covariates.
We prespecified a logistic model based on previous analyses examining cognitive decline in REGARDS. We conducted the Cox proportional Hazards model and mixed linear model. After the final logistic model was determined (n=21317), we performed a series of sensitivity analyses to examine model robustness. We first stratified the results by Morisky score considering perfect adherers (n=4590, 64%). Morisky score was not a statistically significant effect modifier or confounder. We also examined the association between statin use and cognition in those who did not report income and did not find a difference compared with the models presented.
Results
As shown in Tables 1 and 2, there were 7191 participants who were receiving statins, and 17,404 participants who were not The proportion of participants receiving statins was similar by region (29% in the stroke belt vs 30% in other regions (p=011). Overall, cognitive impairment was observed in 8.6% of users vs 7.7% of non-users, (p=0.014), but there were no regional differences (8% in the stroke belt and 7.9% in other regions demonstrated cognitive impairment p=0.63). However, cognitive impairment was also a function of type of statin use, male sex, age, urban dwelling, lower income, lower educational status, presence of heart disease or stroke, elevated systolic blood pressure (SBP) and pulse pressure (PP), diabetes mellitus, and higher Framingham Coronary Risk.
Table 1.
Demographic characteristics of sample population
| Sample Size |
Cognitive Performance Impaired |
p value | Statin Use Taking Statin |
p value | |||
|---|---|---|---|---|---|---|---|
| No | % | No | % | ||||
| All | 24595 | 1958 | 8.0% | 7191 | 29% | ||
| Statin Use | |||||||
| No | 17404 | 1338 | 7.7% | 0 | 0% | ||
| Yes | 7191 | 620 | 8.6% | 0.014 | 7191 | 100% | |
| Type of Statin | |||||||
| atorvastatin | 3101 | 255 | 8.2% | 0.560 | 3101 | 100% | |
| simvastatin | 2700 | 251 | 9.3% | 0.007 | 2700 | 100% | |
| Lipophilica | 3415 | 316 | 9.3% | 0.003 | 3415 | 100% | |
| Region (missing 9) | |||||||
| Other regions | 10663 | 839 | 7.9% | 3174 | 30% | ||
| Stroke Belt | 13923 | 1119 | 8.0% | 0.63 | 4014 | 29% | 0.11 |
| Race (missing 3) | |||||||
| White | 14349 | 753 | 5.2% | 4379 | 30.5% | ||
| Black | 10246 | 1205 | 11.8% | <0.001 | 2812 | 27.4% | <0.001 |
| Gender | |||||||
| Male | 9862 | 899 | 9.1% | 3289 | 33.4% | ||
| Female | 14733 | 1059 | 7.2% | <0.001 | 3902 | 26.5% | <0.001 |
| Age group | |||||||
| 40–54 | 3753 | 160 | 4.3% | 570 | 15.2% | ||
| 55–64 | 9057 | 505 | 5.6% | 2452 | 27.1% | ||
| 65–74 | 7690 | 694 | 9.0% | 2728 | 35.5% | ||
| 75–84 | 3620 | 493 | 13.6% | 1301 | 35.9% | ||
| 85+ | 475 | 106 | 22.3% | <0.001 | 140 | 29.5% | <0.001 |
| Rural/urban (missing 9) | |||||||
| Non-urban* | 7302 | 511 | 7.0% | 2158 | 29.6% | ||
| Urban | 17284 | 1447 | 8.4% | <0.001 | 5030 | 29.1% | 0.47 |
| Income (missing 3228) | |||||||
| $20K | 4362 | 565 | 13.0% | 1303 | 29.9% | ||
| $20K–$34K | 5792 | 543 | 9.4% | 1741 | 30.1% | ||
| $35K–74K | 7244 | 394 | 5.4% | 2151 | 29.7% | ||
| $75+ | 3969 | 121 | 3.0% | 0.001 | 1060 | 26.7% | 0.001 |
| Years of education (missing 22) |
|||||||
| <High school | 2915 | 505 | 17.3% | 960 | 32.9% | ||
| High school | 6443 | 590 | 9.2% | 1970 | 30.6% | ||
| Some college | 6669 | 444 | 6.7% | 1879 | 28.2% | ||
| College+ | 8546 | 412 | 4.8% | <0.001 | 2373 | 27.8% | <0.001 |
Includes lovastatin and simvastatin
Table 2.
Concurrent health conditions
| Sample Size | Cognitive Performance Impaired |
p value | Statin Use Taking Statin |
p value | |||
|---|---|---|---|---|---|---|---|
| No | % | No | % | ||||
| All | 24595 | 1958 | 8.0% | 7191 | 29% | ||
| History of heart disease (missing 592) | |||||||
| No | 18607 | 1347 | 7.2% | 4489 | 24.1% | ||
| Yes | 5396 | 538 | 10.0% | <0.001 | 2520 | 46.7% | <0.001 |
| History of stroke (missing 39) | |||||||
| No | 22165 | 1640 | 7.4% | 6132 | 27.7% | ||
| Yes | 2391 | 315 | 13.2% | <0.001 | 1040 | 43.5% | <0.001 |
| History of hypertension (missing 356) | |||||||
| No | 9795 | 631 | 6.4% | 1977 | 20.2% | ||
| Yes | 14444 | 1299 | 9.0% | <0.001 | 5141 | 35.6% | <0.001 |
| History of diabetes (missing 1338) | |||||||
| No | 18128 | 1299 | 7.2% | 4515 | 24.9% | ||
| Yes | 5129 | 556 | 10.8% | <0.001 | 2341 | 45.6% | <0.001 |
| Framingham cardiac risk score (missing 6663) | |||||||
| Q1 | 4490 | 193 | 4.3% | 876 | 19.5% | ||
| Q1–Median | 4491 | 278 | 6.2% | 1155 | 25.7% | ||
| Median–Q3 | 4491 | 359 | 8.0% | 1235 | 27.5% | ||
| Q3 or higher | 4490 | 494 | 11.0% | <0.001 | 1118 | 24.9% | <0.001 |
| Systolic blood pressure (missing 659) | |||||||
| Q1 (70.0-117.0 mmHg) | 6116 | 369 | 6.0% | 1616 | 26.4% | ||
| Q2 (117.5-125.0 mmHg) | 6006 | 423 | 7.0% | 1726 | 28.7% | ||
| Q3 (125.5-137.0 mmHg) | 5970 | 523 | 8.8% | 1918 | 32.1% | ||
| Q4 (137.5-245.0 mmHg) | 5844 | 598 | 10.2% | <0.001 | 1744 | 29.8% | <0.001 |
| Pulse pressure (missing 661) | |||||||
| Q1(14.5-40.5 mmHg) | 5150 | 322 | 6.3% | 1221 | 23.7% | ||
| Q2 (41.0-48.5 mmHg) | 6065 | 378 | 6.2% | 1703 | 28.1% | ||
| Q3 (49.0-57.5 mmHg) | 6397 | 538 | 8.4% | 1987 | 31.1% | ||
| Q4 (58.0-143.0 mmHg) | 6322 | 675 | 10.7% | <0.001 | 2092 | 33.1% | <0.001 |
| HDL (missing 1127) | |||||||
| Q1 (7.0-40.0 mg/dL) | 5656 | 461 | 8.2% | 1875 | 33.2% | ||
| Q2 (41.0-50.0 mg/dL) | 6359 | 502 | 7.9% | 2089 | 32.9% | ||
| Q3 (51.0-61.0 mg/dL) | 5475 | 395 | 7.2% | 1579 | 28.8% | ||
| Q4 (62.0-199.0 mg/dL) | 5978 | 480 | 8.0% | 0.26 | 1310 | 21.9% | <0.001 |
As seen in Table 3, when the above variables were entered into the multivariable model, cognitive impairment was not associated with statin use. We also found no association between cognitive impairment and HDL-C levels. Imputation of the income status and sensitivity analysis using the Morisky score of medication adherence (among only the 64% of the cohort that reported perfect adherence) did not change the lack of association between cognitive impairment and either statin use or HDL-C level.
Table 3.
Univariate and multivariate logistic models for predicting cognitive impairment
| Univariate Associations |
Model 2a | Model 3 a | Model 4a | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Statin Use | ||||||||
| Yes vs No | 1.13 | (1.03, 1.25) | 1.03 | (0.93, 1.14) | 0.99 | (0.89, 1.12) | 0.98 | (0.87, 1.10) |
| Gender | ||||||||
| Male vs Female | 1.30 | (1.18, 1.42) | 1.38 | (1.25, 1.52) | 1.57 | (1.41, 1.75) | 1.56 | (1.39, 1.74) |
| Age group | ||||||||
| 55–64 vs 40–54 | 1.33 | (1.11, 1.59) | 1.36 | (1.13, 1.63) | 1.34 | (1.10, 1.64) | 1.34 | (1.09, 1.64) |
| 65–74 vs 40–54 | 2.23 | (1.87, 2.66) | 2.37 | (1.98, 2.84) | 1.95 | (1.60, 2.39) | 1.94 | (1.59, 2.37) |
| 75–84 vs 40–54 | 3.54 | (2.94, 4.26) | 3.99 | (3.31, 4.82) | 2.94 | (2.38, 3.64) | 2.91 | (2.35, 3.61) |
| 85+ vs 40–54 | 6.45 | (4.94, 8.43) | 7.59 | (5.77, 9.98) | 5.06 | (3.67, 6.98) | 4.98 | (3.61, 6.88) |
| Income | ||||||||
| <$20K vs >$75K | 4.73 | (3.87, 5.79) | 2.48 | (1.97, 3.13) | 2.47 | (1.96, 3.12) | ||
| $20K–$34K vs >$75K | 3.29 | (2.69, 4.02) | 2.02 | (1.62, 2.52) | 2.02 | (1.62, 2.52) | ||
| $35K–74K vs >$75K | 1.83 | (1.49, 2.25) | 1.46 | (1.18, 1.81) | 1.46 | (1.17, 1.81) | ||
| Years of education | ||||||||
| <High school vs college+ | 4.14 | (3.60, 4.75) | 1.80 | (1.51, 2.15) | 1.79 | (1.50, 2.14) | ||
| High school vs college+ | 1.99 | (1.75, 2.27) | 1.35 | (1.16, 1.58) | 1.35 | (1.15, 1.57) | ||
| Some college vs college+ | 1.41 | (1.23, 1.62) | 1.12 | (0.96, 1.31) | 1.12 | (0.95, 1.31) | ||
| History of heart disease | ||||||||
| Yes vs No | 1.42 | (1.28, 1.58) | 1.09 | (0.96, 1.23) | ||||
| History of stroke | ||||||||
| Yes vs No | 1.90 | (1.67, 2.16) | 1.41 | (1.21, 1.64) | 1.40 | (1.20, 1.63) | ||
All models control for race in addition to other covariates Model 3 is the final model.
Hypertension, diabetes, systolic blood pressure, pulse pressure, HDL, and Framingham cardiac risk score were considered as covariates, but were not significant predictors in the fully adjusted model. The results were similar to those presented in Model 4.
Lipophilic vs Non-lipophilic Statins: (Table 4)
Table 4.
Subanalyses comparing specific statins (n=7191)
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Use of lipophyllic vs hydrophyllic statin (multivariate n= 6237) Yes vs No |
1.17 | (0.99, 1.37) | 1.03 | (0.86, 1.24) |
| Use of simvastatin vs other statins (multivariate n= 6237) Yes vs No |
1.15 | (0.97, 1.35) | 1.05 | (0.87, 1.27) |
| Use of atorvastatin vs other statins (multivariate n= 6237) Yes vs No |
0.91 | (0.77, 1.08) | 1.01 | (0.83, 1.22) |
| Use of simvastatin vs atorvastatin (multivariate n= 5018) Yes vs No |
1.14 | (0.95, 1.37) | 1.03 | (0.84, 1.26) |
All models control for race, age, gender, income, education, and history of stroke
The majority of statin use was simvastatin (n=2700) and atorvastatin (n=3102), accounting for 81% of all statin use. Thus, any comparison of lipophilic vs non-lipophilic statin use was primarily driven by these two statins. As a result, we did not feel that stratification by the degree of lipophilicity was appropriate and just compared atorvostatin to simvastin. With univariate analysis there was at best a trend toward more cognitive impairment with lipophilic vs hydrophilic statins (simvastatin vs atorvastatin), but upon adjustment there was no apparent difference.
Discussion
Our aim was to determine associations of cognitive impairment and statin use and type, as well as HDL-C levels. These aims were a result of the inconsistent literature which has reported an association of statin use with impaired or improved cognitive performance along with studies that have reported a neutral effect. The REasons for Geographic And Racial Differences in Stroke (REGARDS) study allowed us to perform a cross-sectional analysis in a large population-based cohort (n=24595) to address this question. Overall, without adjustment for potential confounders, a small but significantly higher rate of cognitive impairment was found in statin users with a trend toward lipophilic statins being more likely to be associated with cognitive impairment than hydrophilic statins. When adjusted for factors that would likely affect cognitive performance, no association with statin use or type, nor with HDL-C was demonstrated. As expected, there were associations of cognitive impairment with age, lower level of education and income, sex, urban dwelling, CVD, diabetes mellitus, FRS, SBP, and PP.
Many of the studies exploring the relationship between statins and cognition have been conducted on either clinical populations[8,20] or on populations that were relatively homogenous with respect to age (mostly ages 60 years and above)[21] and race (predominantly non-African American)[22]. It has been suggested that statin use is associated with improved cognition although some studies have suggested that statins have no effect or may even be detrimental. A review of PubMed by one of the coauthors (Dr. Kana) using the search terms “statins and cognitive assessment”, “statins and cognitive function”, “statins and cognition” and the references sited within the resulting papers, found 79 review papers and 120 studies examining the association between statins and cognition. These studies ranged from case studies[5-8] to randomized controlled studies[23]. We excluded from consideration studies without human subjects, studies of children, studies in a language other than English, studies without a focus on statins and cognitive function. We also excluded ongoing studies without published results with respect to impact on cognition, conceptual and design papers, opinion papers and studies of special populations (for example of airline crews, traumatic brain injury patients) resulting in 63 total reviews and studies. These studies yielded varying results with respect to the effect of statins on cognition, with some studies showing no effect[9, 23 , a few showing worsening of cognitive function[5-7] some demonstrating small benefits[24) and the rest inconclusive[25,26]
It was hypothesized that there were a number of variables that could affect the association between stains use and cognitive impairment, including increasing age, SES, geographic location, vascular disease etc. (See Table 2). What is clearly evident from our analysis is that age “drove” the univariate association of statin use and cognitive function; and, when any other model with age adjustment was used, no association was observed between statin use or HDL-C level and cognitive impairment.
Limitations
The REGARDS study relied on in home evaluation of statin use. During the in-home visit participants were asked to show the bottles of all prescribed and over the counter medications they were taking in order to be certain that participants were actually complying with that therapy, although it is still possible that some participants may not have taken their statins as prescribed. However, a sensitivity analysis of those who indicated perfect adherence (as assessed by the Morisky scale) did not change the results. While we did not have long-term adherence data, the Morisky score has been shown to be a valid measure of medication adherence.[19] This cross-sectional study did not have information on duration of statin exposure, nor baseline cognitive status prior to statin use. Nevertheless, our study can be compared with the findings of other cross-sectional studies. The Six Item Screener we used to evaluate cognitive impairment, has been validated, but the use of a more formal and complete evaluation of cognitive performance might be more sensitive to subtle differences in cognitive function. Finally, specific dosage information is not available.
In conclusion, this analysis provides for a greater understanding of the relationship and frequency of statin use to global cognitive status, and whether this relationship is mediated by statin type, health behaviors, and cardiovascular risk factors. When adjusted for variables that have been related to cognitive impairment, we found no association between statin use and cognitive impairment.
CONDENSED ABSTRACT.
In this cross-sectional analysis of 24595 (7191 statin users) participants from a population-based national cohort study we assessed the association of statin use and type, and cognitive impairment. Overall, an association of cognitive impairment and statin use was observed but, after adjusting for variables known to be associated with cognition the association was attenuated. No association was observed between statin type and cognition, and there were no regional differences in cognitive impairment in statin users. This large study found no evidence to support an association between statins and cognitive performance.
Acknowledgments
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors acknowledge the participating investigators and institutions for their valuable contributions: The University of Alabama at Birmingham, Birmingham, Alabama (Study PI, Statistical and Data Coordinating Center, Survey Research Unit): George Howard DrPH, Leslie McClure PhD, Virginia Howard PhD, Libby Wagner MA, Virginia Wadley PhD, Rodney Go PhD, Monika Safford MD, Ella Temple PhD, Margaret Stewart MSPH, J. David Rhodes BSN; University of Vermont (Central Laboratory): Mary Cushman MD; Wake Forest University (ECG Reading Center): Ron Prineas MD, PhD; Alabama Neurological Institute (Stroke Validation Center, Medical Monitoring): Camilo Gomez MD, Susana Bowling MD; University of Arkansas for Medical Sciences (Survey Methodology): LeaVonne Pulley PhD; University of Cincinnati (Clinical Neuroepidemiology): Brett Kissela MD, Dawn Kleindorfer MD; Examination Management Services, Incorporated (In-Person Visits): Andra Graham; Medical University of South Carolina (Migration Analysis Center): Daniel Lackland DrPH; Indiana University School of Medicine (Neuropsychology Center): Frederick Unverzagt PhD; National Institute of Neurological Disorders and Stroke, National Institutes of Health (funding agency): Claudia Moy PhD.
Footnotes
Conflict of Interest Statement: No conflicts to disclose for any authors
Contributor Information
Stephen P Glasser, University of Alabama at Birmingham, Division of Preventive Medicine.
Virginia Wadley, University of Alabama at Birmingham.
Suzanne Judd, Department of Biostatistics.
Bhumika Kana, University of Alabama at Birmingham.
Valerie Prince, Samford University McWhorter School of Pharmacy, Birmingham, AL.
Nancy Swords Jenny, University of Vermont College of Medicine, Burlington VT.
Brett Kissela, Department of Neurology University of Cincinnati, Cincinnati, OH.
Monika Safford, University of Alabama at Birmingham, Division of Preventive Medicine.
Ronald Prineas, Department of Epidemiology and Prevention, Wake Forest University School of Medicine, Winston-Salem, NC.
George Howard, Department of Biostatistics, School of Public Health, University of Alabama at Birmingham.
References
- 1.Elias MF, Sullivan LM, D’Agostino RB, et al. Framingham stroke risk profile and lowered cognitive performance. Stroke. 2004;35(2):404–9. doi: 10.1161/01.STR.0000103141.82869.77. [DOI] [PubMed] [Google Scholar]
- 2.Pavlik VN, Hyman DJ, Doody R. Cardiovascular risk factors and cognitive function in adults 30-59 years of age (NHANES III) Neuroepidemiology. 2005;24(1-2):42–50. doi: 10.1159/000081049. [DOI] [PubMed] [Google Scholar]
- 3.Prencipe M, Santini M, Casini AR, et al. Prevalence of non-dementing cognitive disturbances and their association with vascular risk factors in an elderly population. J Neurol. 2003;250(8):907–12. doi: 10.1007/s00415-003-1094-0. [DOI] [PubMed] [Google Scholar]
- 4.Saxby BK, Harrington F, McKeith IG, et al. Effects of hypertension on attention, memory, and executive function in older adults. Health Psychol. 2003;22(6):587–91. doi: 10.1037/0278-6133.22.6.587. [DOI] [PubMed] [Google Scholar]
- 5.King DS, Wilburn AJ, Wofford MR, et al. Cognitive impairment associated with atorvastatin and simvastatin. Pharmacotherapy. 2003;23(12):1663–7. doi: 10.1592/phco.23.15.1663.31953. [DOI] [PubMed] [Google Scholar]
- 6.Orsi A, Sherman O, Woldeselassie Z. Simvastatin-associated memory loss. Pharmacotherapy. 2001;21(6):767–9. doi: 10.1592/phco.21.7.767.34577. [DOI] [PubMed] [Google Scholar]
- 7.Harrison RW, Ashton CH. Do cholesterol-lowering agents affect brain activity? A comparison of simvastatin, pravastatin, and placebo in healthy volunteers. Br J Clin Pharmacol. 1994;37(3):231–6. doi: 10.1111/j.1365-2125.1994.tb04268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. 2006;163(3):197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 9.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 10.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 11.Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–81. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Wilber ST, Carpenter CR, Hustey FM. The Six-Item Screener to detect cognitive impairment in older emergency department patients. Acad Emerg Med. 2008;15(7):613–6. doi: 10.1111/j.1553-2712.2008.00158.x. [DOI] [PubMed] [Google Scholar]
- 13.Howard G, Wadley VG, Unverzagt FW, et al. Stroke risk factors are predictive of cognitive decline in the absence of clinically diagnosed incident stroke. (abstract) Stroke. 2008:39. [Google Scholar]
- 14.Kurella Tamura M, Wadley V, Yaffe K, et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2008;52(2):227–34. doi: 10.1053/j.ajkd.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pullicino PM, Wadley VG, McClure LA, et al. Factors contributing to global cognitive impairment in heart failure: results from a population-based cohort. J Card Fail. 2008;14(4):290–5. doi: 10.1016/j.cardfail.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wadley VG, Unverzagt FW, McGuire LC, et al. Incidence of impaired cognitive screening status is higher than average in the Stroke Belt: The Reasons for Geographic and Racial Differences in Stroke Study. Under review.
- 17.Hendrie HC, Ogunniyi A, Hall KS, et al. Incidence of dementia and Alzheimer disease in 2 communities: Yoruba residing in Ibadan, Nigeria, and African Americans residing in Indianapolis, Indiana. JAMA. 2001;285(6):739–47. doi: 10.1001/jama.285.6.739. [DOI] [PubMed] [Google Scholar]
- 18.Manly JJ, Tang MX, Schupf N, et al. Frequency and course of mild cognitive impairment in a multiethnic community. Ann Neurol. 2008;63(4):494–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Gengo F, Cwudzinski D, Kinkel P, et al. Effects of treatment with lovastatin and pravastatin on daytime cognitive performance. Clin Cardiol. 1995;18(4):209–14. doi: 10.1002/clc.4960180406. [DOI] [PubMed] [Google Scholar]
- 21.Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 22.Szwast SJ, Hendrie HC, Lane KA, et al. Association of statin use with cognitive decline in elderly African Americans. Neurology. 2007;69(19):1873–80. doi: 10.1212/01.wnl.0000279333.77404.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peters JT, Garwood CL, Lepczyk M. Behavioral changes with paranoia in an elderly woman taking atorvastatin. Am J Geriatr Pharmacother. 2008;6(1):28–32. doi: 10.1016/j.amjopharm.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Carlsson CM, Gleason CE, Hess TM, et al. Effects of simvastatin on cerebrospinal fluid biomarkers and cognition in middle-aged adults at risk for Alzheimer’s disease. J Alzheimers Dis. 2008;13(2):187–97. doi: 10.3233/jad-2008-13209. [DOI] [PubMed] [Google Scholar]
- 25.Caballero J, Nahata M. Do statins slow down Alzheimer’s disease? A review. J Clin Pharm Ther. 2004;29(3):209–13. doi: 10.1111/j.1365-2710.2004.00560.x. [DOI] [PubMed] [Google Scholar]
- 26.Kuller LH. Statins and dementia. Curr Atheroscler Rep. 2007;9(2):154–61. doi: 10.1007/s11883-007-0012-9. [DOI] [PubMed] [Google Scholar]