Abstract
Objectives
We investigated whether, over time, baseline obesity is associated with change in depressive symptoms or if baseline symptoms of depression are associated with change in body mass index (BMI) and waist circumference.
Methods
We used latent growth curve modeling to examine data from years 5, 10, 15, and 20 of the Coronary Artery Risk Development in Young Adults study (n = 4643). We assessed depressive symptomatology with the Center for Epidemiological Studies Depression scale.
Results
Respondents who started out with higher levels of depressive symptoms experienced a faster rate of increase in BMI (for Whites only) and waist circumference (for Blacks and Whites) over time than did those who reported fewer symptoms of depression in year 5. Initial BMI and waist circumference did not influence the rate of change in symptoms of depression over time.
Conclusions
Depressive symptomatology likely plays a role in the development of physical health problems, such as cardiovascular disease, through its association with increases in relative weight and abdominal obesity over time.
Nearly two thirds of US adults are overweight or obese,1 andanestimated17%ofAmericans will experience a clinically significant episode of major depression at some point in their lives.2 Evidence suggests some overlap in these populations. Cross-sectional studies show significant correlations between obesity and depression in adolescents and adults,3,4 yet the issue of causal ordering (i.e., whether obesity fosters depression, depression fosters obesity, or both) remains unclear. Although obesity and depression are each recognized as serious public health problems, surprisingly little is known about the relationship between them.3
We extended previous research by examining symptoms of depression and obesity as dynamic, interrelated trajectories and by determining whether the observed associations differ by gender, race/ethnicity, or socioeconomic status (SES). We considered bidirectionality in the association between symptoms of depression and obesity. We used latent growth curve modeling to determine whether trajectories of change in depressive symptom-atology are associated with trajectories of change in body mass index (BMI) and waist circumference and whether sociodemographic characteristics influence the association between these trajectories.
TEMPORAL SEQUENCING
Research suggests that depression is associated with changes in appetite and physical activity that may lead to weight gain. Although depression is sometimes associated with decreased appetite and weight loss, in many cases it is associated with increased appetite and weight gain.3 In addition, depression is associated with reduced physical activity, which may result in weight change.5 Although it is plausible that depressive symptoms lead to weight changes, there is also reason to suspect that obesity leads to change in symptoms of depression. Evidence suggests that obesity is a highly stigmatized condition.6 According to the reflected self-appraisal hypothesis, people who are overweight or obese are likely to internalize negative attitudes from society regarding their condition, which results in self-rejection and increased psychological distress.7,8
Most previous research on the association between obesity and depression used cross-sectional data. Although longitudinal studies have become increasingly common,9–11 only 2 studies have simultaneously examined pathways from depression to obesity and from obesity to depression, and these studies produced conflicting findings. In a nationally representative sample of adolescents in grades 7 through 12, Goodman and Whitaker12 found that symptoms of depression predicted obesity 1 year later, whereas obesity at baseline did not predict symptoms of depression at follow-up. By contrast, a study using data from the Alameda County Study found that, for older adults, obesity at baseline was associated with an increased risk of major depression 5 years later but that baseline depression was not associated with an increased risk of obesity.13 These studies included very different populations. Clearly, research is needed to establish the temporal sequencing of obesity and depression. We examined whether obesity predicts a change in psychological well-being or whether symptoms of depression predict changes in weight in a sample of young adults.
SOCIODEMOGRAPHIC MODERATORS
Several recent reviews have noted that there are likely multiple patterns of association between obesity and depression.3,4,10,14,15 A number of potential moderators have been proposed, including gender, race/ethnicity, and SES,15 as well as severity of depression, severity of obesity, and gene–environment interactions.3 We focus on sociodemographic moderators (i.e., gender, race/ethnicity, and SES). We expect to find that the association between initial symptoms of depression and change in weight will be stronger in population groups that are more likely to experience increased appetite in conjunction with depressed mood. Evidence suggests that increased appetite is more common in depressed womenthanindepressedmen16 andindepressedBlacks thanindepressedWhites.17 Because they tend to have access to fewer stress-buffering resources, members of socially disadvantaged groups, including women, racial/ ethnic minorities, and those with less education, may be more likely to engage in comfort eating behavior to reduce symptoms of distress.18,19 In addition, we expect to find that the association between initial weight and change in depressive symptomatology is stronger in population groups in which obesity is most stigmatized, including women,20 Whites,21 and those of higher SES.22
Previous studies have demonstrated that the association between symptoms of depression and obesity depends on gender, race/ethnicity, and SES, although not all studies have found evidence of moderation.23 In general, studies examining gender differences have found a positive association between relative weight and depression among adolescent girls and adult women24–32 and either no association or an inverse association among boys and men.24–28,33,34 Few studies have examined racial/ethnic or socioeconomic differences in the obesity–depression association. Although most studies report no significant differences between racial/ethnic groups,24,28 one recent study found that overweight or obese Hispanic women were more likely than were overweight or obese White or Black women to have experienced depressedmoodinthepastmonth.29 In another study, no association was found between relative weight and self-esteem among Black women, and it was concluded that overweight may be less distressing for Blacks than for Whites.35 Regarding SES, in one population-based study a positive association was found between degree of overweight and symptoms of depression among better educated women and men but not among those with less education.7 Finally, Moore et al.36 found that the association between obesity and depression did not depend on SES among men but that being obese was associated with higher levels of depression for high SES women and lower levels of depression for low SES women.
Based on our review of the literature, we proposed the following hypotheses: (1) in general, greater depressive symptomatology at baseline would be related to an increase in BMI and waist circumference over time; (2) greater depressive symptomatology at baseline would be more strongly related to increases in BMI and waist circumference over time for women than for men, for Blacks than for Whites (controlling for SES), and for those with lower versus higher SES (controlling for race/ ethnicity); (3) in general, higher BMI and greater waist circumference at baseline would be related to increases in symptoms of depression over time; and (4) higher BMI and greater waist circumference at baseline would be more strongly related to increases in symptoms of depression over time for women than for men, for Whites than for Blacks (controlling for SES), and for those with higher versus lower SES (controlling for race/ethnicity).
METHODS
We used data from the Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a longitudinal study of a biracial (Black and White) cohort of 5115 women and men aged 18 to 30 years at their initial in-person examination, which occurred sometime in either 1985 or 1986. The study was designed to provide approximately equal representation across groups by age, gender, race/ ethnicity, and education. Respondents were recruited from Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. Community-based sampling was performed in Birmingham, Chicago, and Minneapolis. In Oakland, respondents were sampled from the total Kaiser Permanente health plan membership. In-person follow-up examinations were completed 2, 5, 7, 10, 15, and 20 years after the initial examination. Data were from years 5, 10, 15, and 20—the years in which respondents were asked to report symptoms of depression. We excluded 448 respondents who were missing information on 1 or more key study variable (i.e., symptoms of depression, BMI, or waist circumference) at all years examined. The final sample included 4643 respondents.
Measures
We assessed depressive symptomatology in years 5, 10, 15, and 20 with the Center for Epidemiological Studies Depression scale.37 The scale is a widely used and validated measure of depressive symptoms. We asked respondents to report how often they experienced each of 20 symptoms within the past week (0=rarelyornoneofthe time,1=someofthe time, 2=much of the time, and 3=most or all of the time).Highvaluesonthe scale indicate greater psychological distress. The a reliability of thescalewas0.89inyear5and0.90inyears10, 15, and 20.
Weight was measured and recorded to the nearest one half pound; height was measured and recorded to the nearest one half centimeter. BMI was calculated as the ratio of weight to height squared (kg/cm2 × 104). Waist circumference, a measure of central adiposity, was measured and recorded to the nearest one half centimeter.
Moderators included gender (1= woman, 0 = man), race/ethnicity (1= Black, 0 = White), and education at year 5 (1=12 years or fewer, 0 = more than 12 years). When examining the association between depressive symptomatology and obesity, it is important to control for sociodemographic characteristics and behavioral factors that are related to both constructs of interest. Thus, all models included controls for gender, race/ethnicity, education, and age (in years) at year 5 as well as for the number of cigarettes usually smoked per day and the number of alcoholic drinks (beer, wine, or liquor) typically consumed per week at years 5, 10, 15, and 20. Descriptive statistics for all study variables are shown in Table 1.
TABLE 1.
Descriptive Statistics for All Study Variables: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985–2006
| Mean (SD) or % |
|
|---|---|
| Depressive symptomatology | |
| Year 5 | 11.24 (8.14) |
| Year 10 | 10.70 (8.22) |
| Year 15 | 9.16 (7.85) |
| Year 20 | 9.33 (7.87) |
| BMI, kg/m2 | |
| Year 5 | 26.12 (5.90) |
| Year 10 | 27.54 (6.54) |
| Year 15 | 28.72 (6.84) |
| Year 20 | 29.42 (7.24) |
| Waist circumference, cm | |
| Year 5 | 82.01 (12.85) |
| Year 10 | 85.88 (14.65) |
| Year 15 | 89.50 (15.42) |
| Year 20 | 91.93 (15.55) |
| Controls and Moderators | |
| Age, y (year 5) | 29.98 (3.63) |
| Gender | |
| Women | 55 |
| Men | 45 |
| Race/ethnicity | |
| Black | 50 |
| White | 50 |
| Education (year 5) | |
| ≤12 y | 32 |
| >12 y | 68 |
| No. of cigarettes per d | |
| Year 5 | 3.47 (7.40) |
| Year 10 | 2.79 (6.74) |
| Year 15 | 2.16 (6.08) |
| Year 20 | 1.78 (5.50) |
| No. of alcoholic drinks per wk | |
| Year 5 | 4.58 (10.36) |
| Year 10 | 4.47 (8.96) |
| Year 15 | 4.46 (10.12) |
| Year 20 | 4.42 (9.04) |
Note. BMI = body mass index. The total sample was N = 4643.
Plan of Analysis
Latent growth curve analysis is a specific type of random coefficient model that is well suited to the study of individual differences in development and change over time. Based on the structural equation modeling framework, latent growth curve analysis uses repeated measures of a construct to estimate a single underlying growth trajectory. The trajectory is characterized by 2 unobserved latent factors, known as the intercept, or starting point, and the slope, or rate of change over time.38
The first step in this analysis was to describe trajectories of depressive symptoms and obesity. We accomplished this by using measures at 4 time points (years 5, 10, 15, and 20) to estimate unconditional growth models for depressive symptomatology, BMI, and waist circumference. The factor loadings for the 4 time-specific measures of each construct were set to 1 to represent the starting point of each trajectory in year 1. The factor loadings for the slope of each trajectory were set to 0, 1, 2, and 3 to define the rate of change as linear. A quadratic term was also included to test for nonlinearity. The mean of the latent intercept factor provided the group average on the starting point for each trajectory, whereas the mean of the latent slope factor represented the average rate of change. Variances for the 2 latent growth factors described individual variation around the overall means for the intercepts and slopes of depressive symptom-atology, BMI, and waist circumference.38
Our goals were to examine reciprocal influence in the association between trajectories of depression and obesity and to determine whether this association varies according to gender, race/ethnicity, and education. We accomplished this with the use of parallel process growth models. First, we regressed the slope factor for each measure of obesity on the intercept factor for depressive symptomatology. Next, we regressed the slope factor for symptoms of depression on the intercept factors for BMI and waist circumference. This directly addressed the issue of bidirectionality by considering whether earlier levels of 1 construct (e.g., symptoms of depression) predict later developmental trajectories in the other construct (e.g., BMI). First, we performed these analyses for the full sample. Using multiple group analysis, we then performed the analyses separately for women and men; for Blacks and Whites; and for those with 12 or fewer years of education and those with more than 12 years of education.39
To determine whether there was a statistically significant difference between groups in the effect of initial symptoms of depression on the rate of change in BMI, for example, we began by freely estimating the parameters within each group. We then reestimated the model, constraining the effect of the intercept of depression on the slope of BMI to be equal across groups. Next, we calculated the change in χ2 relative to the change in degrees of freedom to determine whether the constraint significantly improved model fit. We conducted all analyses in Mplus version 3 (Muthen and Muthen, Los Angeles, CA). We used an option that allows the analysis of data containing missing values as well as an option that controls for first-order autocorrelated residuals.39
RESULTS
Table 2 presents results from the unconditional growth models for depressive symptom-atology, BMI, and waist circumference. Overall, respondents experienced a decline in symptoms of depression across the transition from young adulthood to middle adulthood (mean of intercept =11.38; P<.001; mean of slope = –1.13; P<.001). By contrast, respondents experienced an increase in both BMI (mean of intercept = 26.14; P<.001; mean of slope =1.59; P<.001) and waist circumference (mean of intercept = 82.06; P<.001; mean of slope = 4.36; P<.001) over time. The signifi-cant positive quadratic term for depressive symptomatology (mean of intercept = 0.16; P<.001) suggests a leveling off of the decline in symptoms of depression over time, whereas the significant negative quadratic terms for BMI (mean of intercept = –0.14; P<.001) and waist circumference (mean of intercept = –0.30; P<.001) suggest a leveling off of the increase in relative weight and abdominal fat over time.
TABLE 2.
Parameter Estimates of the Unconditional Latent Growth Models of Depressive Symptomatology, BMI, and Waist Circumference: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985–2006
| Intercept, Mean (Variance) |
Slope, Mean (Variance) |
Quadratic, Mean (Variance) |
|
|---|---|---|---|
| Depressive symptomatology | 11.38*** (37.34***) | -1.13*** (12.26***) | 0.16*** (0.55) |
| BMI, kg/m2 | 26.14*** (31.02***) | 1.59*** (5.14***) | -0.14*** (0.59***) |
| Waist circumference, cm | 82.06*** (142.82***) | 4.36*** (3.47) | -0.30*** (-1.12**) |
Note. BMI = body mass index. The total sample was N = 4643.
*P < .05
P < .01
P < .001
Tables 3 and 4 present results from the parallel process models in which the slope factor of each process is regressed on the intercept factor of the other process. To account for nonlinearity in trajectories of depressive symptomatology, BMI, and waist circumference, we allowed some of the factor loadings for the slope of each trajectory to be free in the parallel process models. The first 2 time loadings were set to 0 and 1, and the remaining time loadings were free. Compared with the alternative approach of including a quadratic slope factor in these models, allowing the time loadings to be free has the advantage of using fewer degrees of freedom while still allowing for growth spurts.40
TABLE 3.
Parameter Estimates of Dual Latent Growth Models of Depressive Symptomatology and BMI, by Selected Respondent Characteristics: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985–2006
| Slope of BMI Regressed on Intercept of Depression b (SE) |
Slope of Depression Regressed on the Intercept of BMI b (SE) |
|
|---|---|---|
| Full sample | 0.01 (0.01) | 0.01 (0.01) |
| Gender | ||
| Women | 0.01 (0.01) | 0.00 (0.01) |
| Men | 0.01 (0.01) | 0.01 (0.02) |
| Race/ethnicity | ||
| Black | 0.00x (0.01) | 0.01 (0.01) |
| White | 0.02**y (0.01) | -0.01 (0.02) |
| Education | ||
| ≤12 y | 0.01 (0.01) | 0.01 (0.02) |
| >12 y | 0.01 (0.01) | -0.00 (0.01) |
Note. BMI = body mass index. The total sample was N = 4643. Models controlled for age, gender, race/ethnicity, and education at year 5 and for smoking and alcohol use at years 5, 10, 15, and 20. Superscripts (x,y) that differ significantly across groups indicate significant changes in χ2df (P < .05).
*P < .05
P < .01
***P < .001
TABLE 4.
Parameter Estimates of Dual Latent Growth Models of Depressive Symptomatology and Waist Circumference, by Selected Respondent Characteristics: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985–2006
| Slope of Waist Regressed on Intercept of Depression b (SE) |
Slope of Depression Regressed on Intercept of Waist b (SE) |
|
|---|---|---|
| Full sample | 0.05** (0.02) | 0.00 (0.01) |
| Gender | ||
| Women | 0.03 (0.02) | 0.01 (0.01) |
| Men | 0.06** (0.02) | 0.00 (0.01) |
| Race/ethnicity | ||
| Black | 0.03 (0.02) | 0.01 (0.01) |
| White | 0.07*** (0.02) | -0.01 (0.01) |
| Education | ||
| ≤12 y | 0.03 (0.02) | 0.01 (0.01) |
| >12 y | 0.06*** (0.02) | 0.00 (0.01) |
Note. The total sample was N = 4643. Models controlled for age, gender, race/ethnicity, and education at year 5 and smoking and for alcohol use at years 5, 10, 15, and 20.
*P < .05
P < .01
P < .001
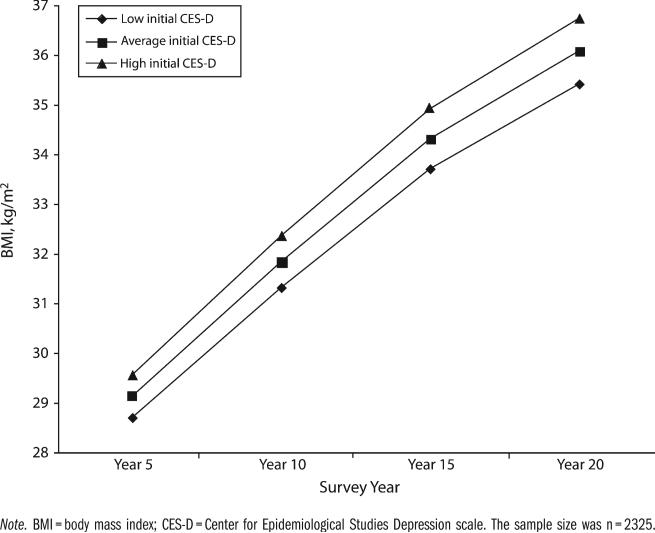
Table 3 presents results of models in which the slope of BMI was regressed on the intercept of depressive symptomatology. These results demonstrate the circumstances under which baseline symptoms of depression were related to change in relative weight over time. For most groups examined, there was no association between initial level of depressive symptoms and the rate of change in BMI. As shown in Figure 1, however, Whites who started out with higher levels of depressive symptoms experienced a faster rate of increase in BMI over time than did those who reported fewer symptoms of depression in year 5. There was no association between initial depressive symptoms and the rate of change in BMI among Blacks, and the difference between Blacks and Whites was statistically significant.
FIGURE 1.
Predicted trajectories of BMI for Whites, by initial depressive symptomatology: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985– 2006.
Table 3 presents results of models in which the slope of depressive symptomatology was regressed on the intercept of BMI. These results demonstrate the circumstances under which relative weight at baseline was related to change in symptoms of depression over time. There are no groups for whom initial BMI was associated with change in depressive symptomatology.
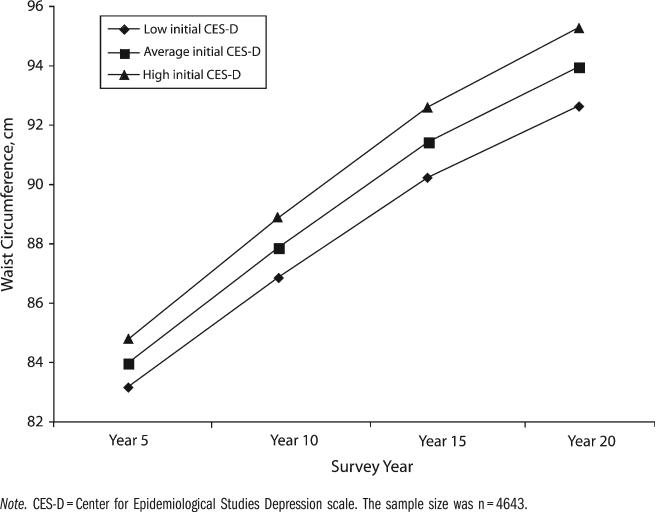
Table 4 presents the results of parallel process models for depressive symptomatology and waist circumference. In the full sample, those who initially reported more symptoms of depression experienced a faster rate of increase in waist circumference over time than did those who report fewer symptoms of depression in year 5 (Figure 2). Among men, Whites, and those with more education, initial depressive symptomatology was associated with a faster rate of increase in waist circumference over time. Among women, Blacks, and those with less education, initial symptoms of depression were not associated with change in waist circumference over time. Chi-squared difference tests indicated that the observed differences between women and men, Blacks and Whites, and those with high and low education were not statistically significant.
FIGURE 2.
Predicted trajectories of waist circumference, by initial depressive symptomatology: CARDIA Study; Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA; 1985–2006.
Table 4 presents results of models in which the slope of depressive symptomatology was regressed on the intercept of waist circumference. There are no groups for whom initial waist circumference was related to change in symptoms of depression over time.
DISCUSSION
Our first goal was to determine whether obesity is associated with changes in psychological well-being or whether symptoms of depression are associated with changes in BMI and waist circumference. The findings suggest that baseline depressive symptomatology influences the rate of change in BMI among Whites and waist circumference among Blacks and Whites over time. Contrary to the reflected self-appraisal hypothesis,7,8 however, initial BMI and waist circumference do not influence the rate of change in symptoms of depression over time. These findings are consistent with previous research on adolescents12 but are inconsistent with previous research on older adults.13 These inconsistencies in the literature highlight the need formoreresearchonthe issue oftemporal sequencing in the association between obesity and depression.
Our second goal was to examine potential sociodemographic moderators of the association between symptoms of depression and obesity. For the sample as a whole, those who started out with higher levels of depressive symptomatology experienced a faster rate of increase in waist circumference over time. We hypothesized that members of socially disadvantaged groups—including women, racial/ ethnic minorities, and those with less education—would experience larger increases in waist circumference than would those with greater social status. Contrary to expectations, however, we found that the association between initial symptoms of depression and change in waist circumference did not significantly differ by gender, race/ethnicity, or education.
Although we did not find an association between initial depressive symptoms and change in BMI over time for the sample as a whole, we did find this association for 1 subgroup. Given the evidence that increased appetite is more common among depressed Blacks than it is among depressed Whites,17 we expected to find that initial symptoms of depression would be more strongly related to increases in BMI over time for Blacks than it would be for Whites. Contrary to expectations, we found that, among Whites only, those who reported more symptoms of depression at baseline experienced a faster rate of increase in BMI over time than did those who initially reported fewer symptoms of depression. The discrepancy between the results of the current study and results of previous research may be owing to differences in the measurement of depression (a continuous measure of symptoms of depression vs a dichotomous measure of clinical depression). Future research should explore this possibility.
Measurement of Obesity
We found that trajectories of depressive symptomatology were related to trajectories of relative weight (as indicated by BMI) for Whites only. By contrast, we found that trajectories of depressive symptomatology were related to trajectories of waist circumference for the sample as a whole. Although we were not able to examine mechanisms underlying the observed association between depressive symptoms and waist circumference, chronic stress arousal, which is common in depression, is linked to endocrine and metabolic imbalances that promote abdominal fat storage.41,42 This may explain why there is more evidence for an association between initial depressive symptoms and changes in waist circumference, a measure of central adiposity, versus changes in BMI, a measure of relative weight.
Limitations and Directions for Future Research
This study has 2 main limitations. First, even though we use prospective longitudinal data, which help establish temporal order in the association between obesity and depression, we were unable to answer the question of true causality. Although it appears that poor psychological well-being leads to increases in BMI among Whites and waist circumference for Blacks and Whites over time, we cannot eliminate the possibility that the observed association is spurious (i.e., owing to some unobserved third variable).
Another limitation of this study is that it does not examine any potential mechanisms, or mediators, underlying the association between depressive symptoms and weight gain, which may help us understand why people who experience more symptoms of depression gain body mass and abdominal fat at a faster rate than do those who experience less psychological distress. Potential mediators include the use of antidepressants, which are known to cause weight gain,43 as well as chronic stress arousal and changes in exercise and diet. The identification of mechanisms linking distress to weight gain would strengthen the claim of a causal relationship between these 2 serious public health problems and would aid in the development of intervention strategies to reduce weight gain in persons experiencing symptoms of depression.
Acknowledgments
The authors thank the Robert Wood Johnson Foundation Health and Society Scholars program for its financial support. Work on this article was supported (or partially supported) by contracts from the National Heart, Lung, and Blood Institute: University of Alabama at Birmingham, Coordinating Center (grant N01-HC-95095); University of Alabama at Birmingham, Field Center (grant N01-HC-48047); University of Minnesota, Field Center and Diet Reading Center (year 20 examination; grant N01-HC-48048); Northwestern University, Field Center (grant N01-HC-48049); Kaiser Foundation Research Institute (grant N01-HC-48050); University of California, Irvine, Echocardiography Reading Center (years 5 and 10 examinations; grant N01-HC-45134); Harbor-UCLA Research Education Institute, Computed Tomography Reading Center (year 15 examination; grant N01-HC-05187); Wake Forest University (year 20 examination; grant N01-HC-45205); New England Medical Center (year 20 examination; grant N01-HC-45204).
Footnotes
Contributors
B. L. Needham originated the study, conducted the analysis, and led the writing. E. S. Epel, N. E. Adler, and C. Kiefe helped to conceptualize ideas, interpret findings, and review drafts of the article.
Human Participant Protection
The institutional review board of the University of Alabama at Birmingham approved this study. The CARDIA steering committee approved this article.
Contributor Information
Belinda L. Needham, Department of Sociology, University of Alabama, Birmingham..
Elissa S. Epel, Department of Psychiatry, University of California, San Francisco..
Nancy E. Adler, Department of Medical Psychology and the Department of Psychiatry, University of California, San Francisco..
Catarina Kiefe, Department of Quantitative Health Sciences, University of Massachusetts Medical School..
References
- 1.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults. JAMA. 2002;288(14):1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 2.Blazer DG, Kessler RC, McGonagle KA, et al. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151(7):979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 3.Stunkard AJ, Myles SF, Allison KC. Depression and obesity. Biol Psychiatry. 2003;54(3):330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 4.Faith MS, Matz PE, Jorge MA. Obesity-depression associations in the population. J Psychosom Res. 2002;53(4):935–942. doi: 10.1016/s0022-3999(02)00308-2. [DOI] [PubMed] [Google Scholar]
- 5.Paluska SA, Schwenk T. Physical activity and mental health: current concepts. Sports Med. 2000;29(3):167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- 6.Puhl R, Borwnell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 7.Ross CE. Overweight and depression. J Health Soc Behav. 1994;35(1):63–79. [PubMed] [Google Scholar]
- 8.Cooley CH. Human Nature and the Social Order. Schocken Books; New York: 1964. [Google Scholar]
- 9.Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes. 2008;32(6):881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- 10.Fabricatore AN, Wadden TA. Psychological aspects of obesity. Clin Dermatol. 2004;22:332–337. doi: 10.1016/j.clindermatol.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Blaine B. Does depression cause obesity? J Health Psychol. 2008;13(8):1190–1197. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 12.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 13.Roberts RE, Deleger S, Strawbridge WJ, et al. Prospective association between obesity and depression: evidence from the Alameda County Study. Int J Obes Relat Metab Disord. 2003;27(4):514–521. doi: 10.1038/sj.ijo.0802204. [DOI] [PubMed] [Google Scholar]
- 14.McElroy SL, Kotwal R, Malhotra S, et al. Are mood disorders and obesity related? A review for the mental health professional. J Clin Psychiatry. 2004;65(5):634–651. doi: 10.4088/jcp.v65n0507. [DOI] [PubMed] [Google Scholar]
- 15.Friedman MA, Brownell KD. Psychological correlates of obesity: moving to the next research generation. Psychol Bull. 1995;117(1):3–20. doi: 10.1037/0033-2909.117.1.3. [DOI] [PubMed] [Google Scholar]
- 16.Angst J, Gamma A, Sellaro R, et al. Toward validation of atypical depression in the community: results of the Zurich cohort study. J Affect Disord. 2002;72(2):125–138. doi: 10.1016/s0165-0327(02)00169-6. [DOI] [PubMed] [Google Scholar]
- 17.O'Neil O, Dong Y, Lawson WB, et al. Differential Expression of Atypical Depression in African Americans and Its Association with Cardiovascular Risk Factors and Diseases. American Psychiatric Association; Arlington, VA: 2009. [Google Scholar]
- 18.Jackson JS, Knight KM. Race and self-regulatory behaviors: the role of the stress response and the HPA axis in physical and mental health disparities. In: Schaie KW, Carstensen LL, editors. Social Structure, Aging, and Self-Regulation in the Elderly. Springer; New York: 2006. pp. 189–208. [Google Scholar]
- 19.Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30(3):241–256. [PubMed] [Google Scholar]
- 20.Sarlio-Lahteenkorva S, Lahelma E. The association of body mass index with social and economic disadvantage in women and men. Int J Epidemiol. 1999;28(3):445–449. doi: 10.1093/ije/28.3.445. [DOI] [PubMed] [Google Scholar]
- 21.Hebl MR, Heatherton TF. The stigma of obesity in women: the difference is Black and White. Pers Soc Psychol Bull. 1998;24(4):417–426. [Google Scholar]
- 22.Wardle J, Griffith J. Socioeconomic status and weight control practices in British adults. J Epidemiol Community Health. 2001;55(3):185–190. doi: 10.1136/jech.55.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wardle J, Williamson S, Johnson F, et al. Depression in adolescent obesity: cultural moderators of the association between obesity and depressive symptoms. Int J Obes. 2006;30(4):634–643. doi: 10.1038/sj.ijo.0803142. [DOI] [PubMed] [Google Scholar]
- 24.Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health. 2005;36(1):48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 25.Anderson SE, Cohen P, Naumova EN, et al. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med. 2006;160(3):285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 26.Richardson LP, Davis R, Poulton R, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157(8):739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 27.Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. Int J Obes. 1992;16(12):999–1003. [PubMed] [Google Scholar]
- 28.Carpenter KM, Hasin DS, Allison DB, et al. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90(2):251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heo M, Pietrobelli A, Fontaine KR, et al. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes. 2006;30(3):513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 30.Herva A, Laitinen J, Miettunen J, et al. Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int J Obes. 2006;30(3):520–527. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 31.Pinhey TK, Rubinstein DH, Colfax RS. Overweight and happiness: the reflected self-appraisal hypothesis reconsidered. Soc Sci Q. 1997;78(3):747–755. [Google Scholar]
- 32.Noppa H, Hallstrom T. Weight gain in adulthood in relation to socioeconomic factors, mental illness and personality traits: a prospective study of middle-aged women. J Psychosom Res. 1981;25(2):83–89. doi: 10.1016/0022-3999(81)90094-5. [DOI] [PubMed] [Google Scholar]
- 33.Dragan A, Akhtar-Danesh N. Relation between body mass index and depression: a structural equation modeling approach. BMC Med Res Methodol. 2007;7:14–24. doi: 10.1186/1471-2288-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pine DS, Cohen P, Brook J, et al. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87(8):1303–1310. doi: 10.2105/ajph.87.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faith MS, Mannibay E, Kravitz M, et al. Relative body weight and self-esteem among African Americans in four nationally representative samples. Obes Res. 1998;6(6):430–437. doi: 10.1002/j.1550-8528.1998.tb00375.x. [DOI] [PubMed] [Google Scholar]
- 36.Moore ME, Stunkard A, Srole L. Obesity, social class, and mental illness. JAMA. 1962;181:962–966. doi: 10.1001/jama.1962.03050370030007. [DOI] [PubMed] [Google Scholar]
- 37.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 38.Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson C, et al., editors. Multivariate Applications in Substance Use Research: New Methods for New Questions. Erlbaum; Mahwah, NJ: 2000. pp. 1–42. [Google Scholar]
- 39.Muthen LK, Muthen BO. Mplus User's Guide. 3rd ed. Muthen and Muthen; Los Angeles: 1998–2004. [Google Scholar]
- 40.Acock AC. Growth curves and extensions using Mplus. [February 11, 2010];Lecture Notes for Presentation at Academic Sinica. Available at: http://people.oregonstate.edu/~acock/growth-curves. Published 2005.
- 41.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2(2):73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 43.Fava M. Weight gain and antidepressants. J Clin Psychiatry. 2000;61:37–41. [PubMed] [Google Scholar]