Abstract
Objective
To assess the extent to which chronic condition (CC) status and severity affected how soon children had a dental visit after enrolling in Medicaid.
Data Source
Enrollment and claims data (2003–2008) for newly Medicaid-enrolled children ages 3–14 in Iowa.
Study Design
3M Clinical Risk Grouping methods were used to identify CC status (yes/no) and CC severity (less severe/more severe). Survival analysis was used to identify the factors associated with earlier first dental visits after initially enrolling in Medicaid.
Principal Findings
Children with a CC were 17% more likely to have earlier first dental visits after enrolling in Medicaid (P<0.0001). There was no significant difference by CC severity. Children who lived in a dental Health Professional Shortage Area or did not utilize primary medical care had significantly later first Medicaid dental visits whereas these factors failed to reach statistical significance for children with a CC.
Conclusion
While newly Medicaid-enrolled children with a CC were significantly more likely to have earlier first dental visits, we failed to detect a relationship between CC severity and the time to first Medicaid dental visit. The determinants of first Medicaid dental visits were heterogeneous across subgroups of newly Medicaid-enrolled children. Future studies should identify the socio-behavioral factors associated with CCs that are potential barriers to earlier first Medicaid dental visits for newly Medicaid-enrolled children.
Keywords: Medicaid, utilization, dental health services, disabled children, survival analysis
INTRODUCTION
A number of studies have examined dental utilization for Medicaid-enrolled children (Savage et al. 2004; Slayton, Damiano, and Willard 2001; Dubay and Kenney 2001; Macek, Edelstein, and Manski 2001; Lee and Horan 2001). Fewer investigations have evaluated dental utilization for children after they are initially enrolled in Medicaid (Damiano et al. 2008; Chi et al. 2010). Findings from these latter studies suggest that subgroups of newly Medicaid-enrolled children, including those identified with an intellectual and/or developmental disability (IDD), have significantly later first Medicaid dental visits. Children identified with an IDD are part of a larger group of children with chronic conditions (CC), which are defined as conditions lasting ≥ 12 months in 75% of identified cases (Muldoon, Neff, and Gay 1997). While dental care is the most common unmet health care need for children with a CC (Newacheck et al. 2000; Lewis, Robertson, and Phelps 2005), there is limited knowledge on: a) the impact of having a CC on how soon after enrolling in Medicaid children visit a dentist; and b) the impact of CC severity on how soon newly Medicaid-enrolled children visit a dentist. This lack of knowledge is a critical barrier in the development of population-based interventions and policies aimed at improving dental utilization for children who are newly enrolled in Medicaid. The purpose of this study was to identify the determinants of how soon newly Medicaid-enrolled children visited a dentist, with an emphasis on the relationship between CC status and severity, respectively, and the time to first Medicaid dental visit.
In addition to drinking fluoridated water, regular toothbrushing with fluoridated toothpaste, and a diet low in fermentable carbohydrates, first Medicaid dental visits can help to prevent dental caries, the most common childhood disease in the U.S. (USDHHS 2000). Earlier first Medicaid dental visits enable children to benefit from preventive treatments such as topical fluoride and dental sealants (Azarpazhooh and Main 2008a; Azarpazhooh and Main 2008b; Bhuridej et al. 2007). During these visits, dentists are also able to assess a child’s future risk of developing caries; provide caregivers with risk-based anticipatory guidance; and detect incipient disease (Nowak and Casamassimo 1995; Sanchez and Childers 2000; Hale 2003; AAPD 2005–2006). In addition, first Medicaid dental visits are a starting point for subsequent episodes of dental care. While the evidence is anecdotal, these episodes of care typically consist of preventive care and periodic checkups for children with no dental disease or restorative care (e.g., dental fillings, crowns, tooth extractions) and checkups for children with dental disease. There is also a proportion of children with treatment needs who do not return to the dentist after the first Medicaid dental visit. These observations suggest that first Medicaid dental visits are only part of the solution in improving the long-term oral health of Medicaid-enrolled children.
As many as one-in-three children in the U.S. has a CC (Kuhlthau et al. 2002). Children with a CC are at increased risk for poor oral health because of long-term use of prescription medications that contain sugar (Feigal, Jensen, and Mensing 1981) or alter saliva production (Keene, Galasko, and Land 2003); behavioral co-morbidities that make it hard for caregivers to provide regular oral hygiene (Ferguson and Cinotti 2009) or dentists to provide necessary care in an office setting; and reluctance on the part of dentists to treat children with special needs because of inadequate training (Casamassimo, Seale, and Ruehs 2004). Furthermore, over 70% of children with a CC are enrolled in state Medicaid dental programs (Kaiser Commission 2007), which introduces additional program-related barriers to dental utilization (Al Agili et al. 2004; Nainar 2000; Mayer et al. 2000; Al Agili et al. 2007; Lam, Riedy, and Milgrom 1999; Iben, Kanellis, and Warren 2000).
Delayed first Medicaid dental visits may explain, in part, why subgroups of newly Medicaid-enrolled children are at increased risk for oral health disparities. While children with a CC share characteristics that make them less likely to visit a dentist shortly after enrolling in Medicaid, there is currently no empirical support for this hypothesis. In this study, we evaluated the determinants of how soon a child visited a dentist after initially enrolling in Medicaid. Our primary interest was the relationship between CC status (yes/no) and CC severity (less severe/more severe), respectively, and how soon a child saw a dentist for the first time after enrolling in the Iowa Medicaid Program. We used enrollee-level administrative data to test the following hypotheses:
There is no difference in the rates at which children with and without a CC visit a dentist for the first time after enrolling in Medicaid;
Among children with a CC, there is no difference in the rates at which children visit a dentist for the first time after enrolling in Medicaid by CC severity.
This work is a continuation of efforts to identify potential reasons why subgroups of Medicaid-enrolled children tend to have poor oral health. Our findings will be used to develop future research as well as clinical interventions and policies that seek to improve dental utilization for newly Medicaid-enrolled children.
METHODS
Conceptual Model
This study adapted an oral health disparities model proposed by Patrick et al. (2006). Our conceptual model classifies the potential determinants of first dental visits after initially enrolled in Medicaid into five domains: ascribed factors (population descriptors), proximal factors (health actions and beliefs), immediate factors (mediating pathways between proximal and intermediate factors), intermediate factors (social environment), and distal factors (health care resource allocation).
Data
Medicaid enrollment and claims files from calendar years (CY) 2005–2008 were obtained under an agreement with the Iowa Department of Human Services. All patient identifiers were removed from the raw data files to ensure confidentiality. The study protocol was approved by the University of Iowa Institutional Review Board.
The enrollment files contained each patient’s program identification number (used to link the Medicaid files), birth date, sex, race/ethnicity, Medicaid eligibility program, zip code and county of residence, and a case number used to link Medicaid enrollees from the same household.
The claims files included all the patient’s inpatient, outpatient, prescription medication, and dental claims from 01/01/2005–12/31/2008 submitted on behalf of the enrollee by a health care professional. When applicable, each inpatient and outpatient claim contained the enrollee’s medical diagnoses (International Classification of Disease, Ninth Revision, Clinical Modification Code) and information on any health services received. The dental claims files contained information on all dental services for which a claim was submitted by a dentist and coded by American Dental Association Current Dental Terminology Codes (ADA 2004).
Study Population
Our study focused on a cohort of children ages 3–14 who were newly enrolled in the Iowa Medicaid program in CY2005. “Newly enrolled” was defined as no evidence of Medicaid enrollment in the 12-month period prior to the child’s first month of enrollment in 2005. In addition, each child had to be enrolled in CY2005 for ≥ 6 months, which is the minimum amount of health service data required by the 3M Clinical Risk Grouping (CRG) methods (3M Health Information Systems 2008). We excluded children under age 3 from our analyses because this group typically exhibits lower rates of dental utilization (Kanellis, Damiano, and Momany 1997). In addition, we excluded children ages 15–17 (to allow for our outcome measure to span up to four years) and children with malignancies because these children have health service utilization patterns that differ from other children (Merrill, Nagamine, and Hambrick 2007). The final dataset contained 10,270 children.
Measures
The outcome variable was how soon after enrolling in Medicaid a child visited a dentist, measured over four years (CY2005–2008). There were two main predictor variables: 1) CC status (yes/no) that was measured for all children; and 2) CC severity (less severe/more severe) that was measured for children with a CC. We used the 3M Health Information Systems CRG Software (Version 6.1) to identify CC status and severity. As described previously by Hughes et al. (2004), the CRG system classifies children in administrative datasets into a mutually exclusive and hierarchical core health status group (CHSG) based on medical diagnoses, health service utilization, and prescription medication use. Based on enrollee claims data from CY2005, we used the CRG software to classify each child into one of the following eight CHSGs:
Healthy
Acute condition
Single minor CC
Minor CC in multiple systems
Single dominant or moderate CC
Significant CC in multiple systems
Dominant CC in three or more organs
Catastrophic CC
For the first set of analyses, which examined the relationship between CC status and how soon a child saw a dentist, children from CHSGs 1–2 were classified as having no CC; children from CHSGs 3–8 were classified as having a CC. The second set of analyses focused on children with a CC to examine the effects of CC severity on how soon a child saw a dentist. We used methods developed by Neff et al. (2009) to restructure CHSGs 3–8 into two mutually exclusive CC severity groups: 1) less severe (children from CHSGs 3–4 and those with a moderate CC from CHSG 5); 2) more severe (children with a single dominant CC from CHSG 5 and those from CHSGs 6–8).
In addition, we evaluated the following variables measured in CY2005 for inclusion in our multiple variable regression models:
Ascribed factors: Age (three levels: 3–7, 8–12, 13–14 years); sex; race/ethnicity; Medicaid eligibility program (Temporary Assistance to Needy Families [TANF], Supplemental Security Income [SSI], Foster Care, Home and Community Based Waiver Program, Other); total length of Medicaid enrollment in months (five levels: 6, 7–12, 13–24, 25–36, ≥ 37); CC status (no/yes); CC severity (less severe/more severe)
Proximal factor: Whether the child utilized primary medical care
Immediate factors: Whether the child had a Medicaid-enrolled sibling under age 18 in the household; whether there was any Medicaid-enrolled adult age 18 or older in the household
Intermediate factor: Rurality of the child’s county of residence based on modified U.S. Department of Agriculture Rural-Urban Continuum Codes (four levels: metropolitan, urban adjacent to metropolitan, urban not adjacent to metropolitan, rural) (USDA ERS 2003)
Distal factor: whether the child lived in a dental Health Professional Shortage Area (HPSA)
Statistical Analyses
Descriptive statistics were generated for the study population and for the comparison groups. We established the α-level at 0.05 for all statistical tests. The chi-square test was used to compare proportions, the t-test and one-way ANOVA to test for differences in means (equal variances assumed), and the log rank test to compare utilization rates across strata (unadjusted for covariates but adjusted for censored data). We tested for a potential interaction between the two immediate factors (additional Medicaid-enrolled child*any Medicaid-enrolled adult) and included this term in the final regression models if it was statistically significant (α=0.05). Survival analytic techniques were used to compare the rates at which children visited a dentist after enrolling in Medicaid. Data were censored when the child: 1) became disenrolled from Medicaid; or 2) failed to have a dental visit by 12/31/08. Kaplan-Meier curves were generated for the main predictor variables. We used time-dependent variables to assess for the proportional hazards assumption and to adjust for any covariates that violated this assumption. Cox proportional hazards regression models (with time-dependent covariates when appropriate) were constructed to identify the factors related to how soon a child had a first dental visit after enrolling in Medicaid. We did not include the number of months of enrollment in Medicaid in the final models because enrollment could extend beyond the date of the dental visit. Including this variable would introduce the potential for temporality violations. All data were analyzed using SAS 9.2 for Windows (PROC LIFETEST and PROC TPHREG statements) (SAS Institute Incorporated 2002–2003).
RESULTS
Population Characteristics
About 50% of the children in our study population were age 3–7 (Table 1). Over 90% of all children were eligible for Medicaid through TANF. The mean length of enrollment was 29 months.
Table 1.
Description of Population Subgroups and Total Study Population of Newly Medicaid-Enrolled Children Ages 3–14 in Iowa (N=10,270)
| Variable | No Chronic Condition (N=8,915) n (%) | Any Chronic Condition (N=1,355) n (%) | Any Chronic Condition (N=1,355) |
Total Study Population (N=10,270) n (%) | |
|---|---|---|---|---|---|
| Less severe Chronic Condition (N=993) n (%) | More severe Chronic Condition (N=362) n (%) | ||||
| ASCRIBED FACTORS | |||||
| Age (years) | |||||
| Mean ± standard deviation | 7.8 ± 3.5 | 9.0 ± 3.4 | 8.8 ± 3.4 | 9.7 ± 3.2 | 8.0 ± 3.5 |
| 3 to 7 | 4,515 (50.6) | 487 (35.9) | 383 (38.6) | 104 (28.7) | 5,002 (48.7) |
| 8 to 12 | 3,219 (36.1) | 602 (44.4) | 435 (43.8) | 167 (46.1) | 3,821 (37.2) |
| 13 to 14 | 1,181 (13.3) | 266 (19.6) | 175 (17.6) | 91 (25.1) | 1,447 (14.1) |
| Sex | |||||
| Female | 4,523 (50.7) | 502 (37.0) | 380 (38.3) | 122 (33.7) | 5,025 (48.9) |
| Race/ethnicity | |||||
| White | 4,349 (48.8) | 803 (59.3) | 608 (61.2) | 195 (53.9) | 5,152 (50.2) |
| Black | 558 (6.3) | 54 (4.0) | 39 (3.9) | 15 (4.1) | 612 (6.0) |
| Other | 1,285 (14.4) | 95 (7.0) | 73 (7.4) | 22 (6.1) | 1,380 (13.4) |
| Unknown or missing | 2,723 (30.5) | 403 (29.7) | 273 (27.5) | 130 (35.9) | 3,126 (30.4) |
| Medicaid eligibility program | |||||
| Temporary Assistance to Needy Families (TANF) | 8,483 (95.2) | 1,125 (83.1) | 882 (88.9) | 243 (67.1) | 9,608 (93.6) |
| Supplemental Security Income (SSI) | 66 (0.7) | 59 (4.4) | 28 (2.8) | 31 (8.6) | 125 (1.2) |
| Foster care | 317 (3.6) | 131 (9.7) | 71 (7.2) | 60 (16.6) | 448 (4.4) |
| Home and Community Based Waiver | 34 (0.4) | 31 (2.3) | 9 (0.9) | 22 (6.1) | 65 (0.6) |
| Other | 11 (0.1) | 8 (0.6) | 2 (0.2) | 6 (1.7) | 19 (0.2) |
| Total length of Medicaid enrollment (months), 2005–2008 | |||||
| Mean ± standard deviation | 28.8 ± 13.7 | 33.1 ± 13.4 | 31.9 ± 13.6 | 36.3 ± 12.3 | 29.4 ± 13.8 |
| 6 | 163 (1.8) | 15 (1.1) | 11 (1.1) | 4 (1.1) | 178 (1.7) |
| 7 to 12 | 1,682 (18.9) | 158 (11.7) | 133 (13.4) | 25 (6.9) | 1,840 (17.9) |
| 13 to 24 | 1,926 (21.6) | 241 (17.8) | 194 (19.5) | 47 (13.0) | 2,167 (21.1) |
| 25 to 36 | 1,684 (18.9) | 214 (15.8) | 162 (16.3) | 52 (14.4) | 1,898 (18.5) |
| 37 or more | 3,460 (38.8) | 727 (53.7) | 493 (49.6) | 234 (64.6) | 4,187 (40.8) |
| PROXIMAL FACTOR | |||||
| Child used primary medical care in2005 | |||||
| Yes | 6,627 (74.3) | 1,218 (89.9) | 895 (90.1) | 323 (89.2) | 7,845 (76.4) |
| IMMEDIATE FACTORS | |||||
| At least one Medicaid-enrolled sibling in the household | |||||
| Yes | 1,630 (18.3) | 277 (20.4) | 225 (22.7) | 52 (14.4) | 1,907 (18.6) |
| At least one Medicaid-enrolled adult in the household | |||||
| Yes | 1,077 (12.1) | 186 (13.7) | 154 (15.5) | 32 (8.8) | 1,263 (12.3) |
| INTERMEDIATE FACTOR | |||||
| Degree of rurality of child’s county of residence | |||||
| Metropolitan | 4,862 (54.5) | 695 (51.3) | 487 (49.0) | 208 (57.5) | 5,557 (54.1) |
| Urban adjacent to metropolitan | 1,798 (20.2) | 262 (19.3) | 193 (19.4) | 69 (19.1) | 2,060 (20.1) |
| Urban non-adjacent to metropolitan | 1,713 (19.2) | 317 (23.4) | 243 (24.5) | 74 (20.4) | 2,030 (19.8) |
| Rural | 538 (6.0) | 80 (5.9) | 69 (6.9) | 11 (3.0) | 618 (6.0) |
| DISTAL FACTOR | |||||
| Resides in a dental Health Professional Shortage Area | |||||
| Yes | 5,706 (64.0) | 846 (62.4) | 613 (61.7) | 233 (64.4) | 6,552 (63.8) |
Thirteen percent of children had a CC. The mean age of children with a CC was greater than those without a CC (9.0 versus 7.8 years, respectively; P<.0001). A significantly larger proportion of children with a CC were male than those without a CC (63% versus 49.3%, respectively; P<.0001). Children with a CC were enrolled in Medicaid significantly longer than those without a CC (P<.0001).
Among children with a CC (n=1,355), the majority (73.3%) had a less severe CC. Children with a more severe CC were significantly younger than children with a less severe CC (P<.01). In terms of differences across immediate factors, compared to children with a less severe CC, smaller proportions of children with a more severe CC had a Medicaid-enrolled sibling (22.7% and 14.4%, respectively) or adult (15.5% and 8.8%, respectively).
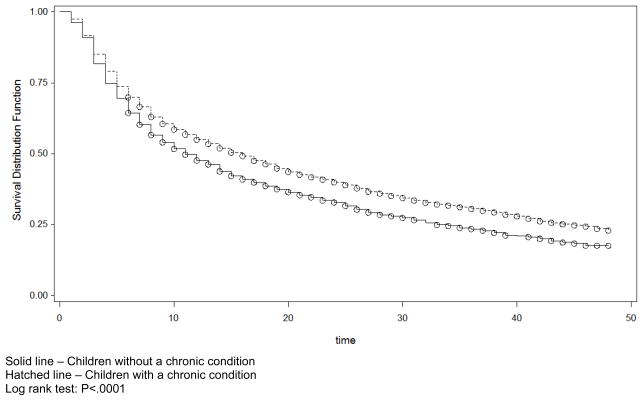
Dental Utilization
Table 2 presents the Kaplan-Meier derived proportions of children with a dental visit after enrolling in Medicaid at specified intervals (adjusted for censoring but not for covariates). About 31% of children had a dental visit within six months of being enrolled in the Medicaid program; the cumulative proportion increased to 46%, 61%, 70%, and 78% by months 12, 24, 36, and 48, respectively. Over the 48-month study period, children with a CC were significantly more likely to have seen a dentist sooner than those without a CC (P<.0001) (Table 2 and Figure 1). While greater proportions of children with a more severe CC had a dental visit at all time intervals than those with a less severe CC, these differences were not statistically significant (P=.25) (Table 2).
Table 2.
Cumulative Proportions of Newly Medicaid-Enrolled Children Ages 3–14 in Iowa with a First Dental Visit at Specified Time Intervals after Enrollment in Medicaid in 2005 (N=10,270)
| Variable/Strata | N | Outcome: Proportion with any dental visit* |
P-value for comparison across strata** | ||||
|---|---|---|---|---|---|---|---|
| 6 months | 12 months | 24 months | 36 months | 48 months | |||
| All children | 10,270 | 0.31 | 0.46 | 0.61 | 0.70 | 0.78 | n/a |
| MAIN INDEPENDENT VARIABLES | |||||||
| Chronic condition status | P<.0001 | ||||||
| Yes | 1,355 | 0.36 | 0.52 | 0.67 | 0.77 | 0.82 | |
| No | 8,915 | 0.30 | 0.45 | 0.60 | 0.69 | 0.77 | |
| Chronic condition severity | P=.25 | ||||||
| Less severe chronic condition | 993 | 0.35 | 0.52 | 0.67 | 0.76 | 0.81 | |
| More severe chronic condition | 362 | 0.37 | 0.53 | 0.69 | 0.78 | 0.85 | |
| ASCRIBED FACTORS | |||||||
| Age (years) | P=.07 | ||||||
| 3 to 7 | 5,002 | 0.30 | 0.46 | 0.61 | 0.71 | 0.78 | |
| 8 to 12 | 3,821 | 0.33 | 0.48 | 0.62 | 0.70 | 0.78 | |
| 13 to 14 | 1,447 | 0.31 | 0.43 | 0.57 | 0.68 | 0.77 | |
| Sex | P<.05 | ||||||
| Female | 5,025 | 0.32 | 0.47 | 0.62 | 0.72 | 0.78 | |
| Male | 5,245 | 0.30 | 0.45 | 0.60 | 0.69 | 0.77 | |
| Race/ethnicity | P<.0001 | ||||||
| White | 5,152 | 0.33 | 0.48 | 0.63 | 0.73 | 0.80 | |
| Black | 612 | 0.24 | 0.38 | 0.49 | 0.62 | 0.70 | |
| Other | 1,380 | 0.30 | 0.46 | 0.60 | 0.67 | 0.75 | |
| Unknown or missing | 3,126 | 0.29 | 0.45 | 0.60 | 0.70 | 0.77 | |
| Medicaid eligibility program | P<.0001 | ||||||
| Temporary Assistance to Needy Families (TANF) | 9,608 | 0.31 | 0.46 | 0.61 | 0.70 | 0.78 | |
| Supplemental Security Income (SSI) | 125 | 0.19 | 0.33 | 0.55 | 0.68 | 0.72 | |
| Foster care | 448 | 0.34 | 0.54 | 0.68 | 0.76 | 0.80 | |
| Home and Community Based Waiver | 65 | 0.23 | 0.29 | 0.36 | 0.49 | 0.58 | |
| Other | 19 | 0.11 | 0.11 | 0.32 | 0.51 | 0.51 | |
| Total length of Medicaid enrollment 2005–2008 (months) | n/a*** | ||||||
| 6 | 178 | 0.26 | - | - | - | - | |
| 7 to 12 | 1,840 | 0.32 | 0.41 | - | - | - | |
| 13 to 24 | 2,167 | 0.28 | 0.42 | 0.53 | - | - | |
| 25 to 36 | 1,898 | 0.30 | 0.46 | 0.59 | 0.69 | - | |
| 37 or more | 4,187 | 0.32 | 0.50 | 0.67 | 0.76 | 0.81 | |
| PROXIMAL FACTOR | |||||||
| Child used primary medical care in 2005 | P<.0001 | ||||||
| Yes | 7,845 | 0.33 | 0.49 | 0.64 | 0.73 | 0.81 | |
| No | 2,425 | 0.24 | 0.37 | 0.52 | 0.61 | 0.68 | |
| IMMEDIATE FACTORS | |||||||
| At least one Medicaid-enrolled sibling in the household | P<.05 | ||||||
| Yes | 1,907 | 0.31 | 0.50 | 0.64 | 0.72 | 0.79 | |
| No | 8,363 | 0.31 | 0.45 | 0.60 | 0.70 | 0.78 | |
| At least one Medicaid-enrolled adult in the household | P=.48 | ||||||
| Yes | 1,263 | 0.29 | 0.49 | 0.63 | 0.70 | 0.78 | |
| No | 9,007 | 0.31 | 0.46 | 0.61 | 0.71 | 0.77 | |
| INTERMEDIATE FACTOR | |||||||
| Degree of rurality of child’s county of residence | P<.05 | ||||||
| Metropolitan | 5,557 | 0.32 | 0.47 | 0.62 | 0.71 | 0.78 | |
| Urban adjacent to metropolitan | 2,060 | 0.29 | 0.45 | 0.60 | 0.70 | 0.77 | |
| Urban non-adjacent to metropolitan | 2,030 | 0.30 | 0.44 | 0.58 | 0.68 | 0.77 | |
| Rural | 618 | 0.32 | 0.50 | 0.64 | 0.74 | 0.93 | |
| DISTAL FACTOR | |||||||
| Resides in a dental Health Professional Shortage Area | P<.05 | ||||||
| Yes | 6,552 | 0.31 | 0.46 | 0.60 | 0.70 | 0.77 | |
| No | 3,718 | 0.31 | 0.47 | 0.63 | 0.72 | 0.79 | |
from Kaplan-Meier curves (adjusted for censored data)
univariate log rank test results for each covariate (unadjusted for other covariates)
significance testing not reported because of temporality-related issues (explained in the Analyses subsection of the Methods section)
Figure 1.
Kaplan-Meier Curves for Newly Medicaid-Enrolled Children Age 3–14 with a Chronic Condition (solid line) and without a Chronic Condition (hatched line) Indicating the Proportions without a First Dental Visit (Y-axis) and the Time to First Dental Visit in Months (X-axis)
Solid line – Children without a chronic condition
Hatched line – Children with a chronic condition
Log rank test: P<.0001
The subgroups with the smallest proportion of children with a first dental visit within six months were those eligible for Medicaid through the Home and Community Based Waiver Program (11%) or SSI (19%). After being in Medicaid for one year, 54% of children eligible for Medicaid through Foster Care had a dental visit – the subgroup with the largest proportion.
Regression Models
We dropped the Medicaid eligibility program variable from our models because of partial collinearity with CC status. In addition, we excluded race/ethnicity because a large proportion of children had unknown or missing data (30.4%). Imputation methods were not used because of the uncertain accuracy of the race/ethnicity variable. All other covariates, including an interaction term between the two immediate factors (having a Medicaid-enrolled sibling and/or adult) were included in our regression models. No covariates violated the proportional hazards assumption. The results are summarized in Table 3.
Table 3.
Multiple Variable Cox Proportional Hazards Regression Models 1 and 2 for Time to First Dental Visit for Newly Medicaid-Enrolled Children Age 3–14 in Iowa
| Model 1: Regression Model For Total Study Population (N=10,270) | Model 2: Regression Model For Children with a Chronic Condition (N=1,355) | |||
|---|---|---|---|---|
| Covariate | Adjusted Hazard Ratio | 95% Confidence Interval | Adjusted Hazard Ratio | 95% Confidence Interval |
| MAIN INDEPENDENT VARIABLES | ||||
| Has a chronic condition | ||||
| Yes | 1.17 | 1.09, 1.25 | n/a | n/a |
| No* | 1.00 | - | n/a | n/a |
| Chronic condition severity | ||||
| Less severe chronic condition* | n/a | n/a | 1.00 | - |
| More severe chronic condition | n/a | n/a | 1.05 | 0.91, 1.20 |
| ASCRIBED FACTORS | ||||
| Age (years) | ||||
| 3 to 7 | 1.05 | 0.97, 1.13 | 0.92 | 0.77, 1.09 |
| 8 to 12 | 1.11 | 1.03, 1.20 | 0.96 | 0.81, 1.14 |
| 13 to 14* | 1.00 | - | 1.00 | - |
| Sex | ||||
| Female | 1.07 | 1.02, 1.13 | 1.04 | 0.91, 1.18 |
| Male* | 1.00 | - | 1.00 | - |
| PROXIMAL FACTOR | ||||
| Child used primary medical care in 2005 | ||||
| Yes | 1.43 | 1.34, 1.52 | 1.20 | 0.97, 1.49 |
| No* | 1.00 | - | 1.00 | - |
| IMMEDIATE FACTORS | ||||
| At least one Medicaid-enrolled sibling in the household | int | - | int | - |
| At least one Medicaid-enrolled adult in the household | int | - | int | - |
| Interaction between having at least one Medicaid- enrolled sibling and adult variables | ||||
| No enrolled sibling/no enrolled adult* | 1.00 | 1.00 | 1.00 | - |
| No enrolled sibling/enrolled adult | 1.03 | 0.92, 1.15 | 0.99 | 0.75, 1.29 |
| Enrolled sibling/no enrolled adult | 1.36 | 1.12, 1.64 | 1.67 | 1.10, 2.55 |
| Enrolled sibling/enrolled adult | 1.86 | 1.43, 2.41 | 2.68 | 1.48, 4.85 |
| INTERMEDIATE FACTOR | ||||
| Degree of rurality of child’s county of residence | ||||
| Metropolitan* | 1.00 | - | 1.00 | - |
| Urban adjacent to metropolitan | 0.90 | 0.84, 0.96 | 0.76 | 0.64, 0.90 |
| Urban non-adjacent to metropolitan | 0.90 | 0.84, 0.96 | 0.83 | 0.71, 0.97 |
| Rural | 1.06 | 0.96, 1.18 | 0.75 | 0.57, 0.99 |
| DISTAL FACTOR | ||||
| Resides in a dental Health Professional Shortage Area | ||||
| Yes | 0.94 | 0.89, 0.99 | 0.94 | 0.82, 1.07 |
| No* | 1.00 | - | 1.00 | - |
reference group
n/a variable not included in the model
int significant interaction; refer to results for each combination of factor levels below
CC Status (Model 1)
After adjusting for model covariates, children with a CC were 17% more likely to have had earlier first dental visits after initially enrolling in Medicaid than those without a CC (P<.0001). Children who lived in a dental HPSA, a distal factor, were 6% less likely whereas those with a primary medical care visit, a proximal factor, were 43% more likely to have had earlier first dental visits after enrolling in Medicaid. Regarding the immediate-level interaction term, there was no difference in the time to first dental visit for children with no enrolled sibling and no enrolled adult (the reference group) and children with no enrolled sibling and an enrolled adult. However, children with an enrolled sibling, regardless of whether they lived with a Medicaid-enrolled adult, were 36%–86% more likely to have had an earlier first dental visit compared to children in the reference group.
CC Severity (Model 2)
Among children with a CC, there was no significant difference in the time to first dental visit after enrolling in Medicaid by CC severity (P=.53). The only two factors for which there were significant differences in the hazard ratios were the interaction term between the two immediate factors (Medicaid-enrolled sibling and/or adult) and the intermediate factor (rurality). Similar to findings from Model 1, children with an enrolled sibling, regardless of whether there was a Medicaid-enrolled adult in the household, were 1.67–2.68 times as likely to have an earlier first dental visit after enrolling in Medicaid, compared to children in the reference group (no enrolled sibling and no enrolled adult). Children who lived in non-metropolitan areas were significantly less likely to have an earlier first visit than those living in metropolitan areas.
DISCUSSION
Main Findings
This is the first published study to date that examined the factors related to the rates at which newly Medicaid-enrolled children had a first dental visit with an emphasis on the impact of CC status and severity. There are three main findings.
First, after adjusting for covariates, children with a CC were 17% more likely than those without a CC to have had earlier first dental visits after initially enrolling in Medicaid. This finding suggests that compared to newly Medicaid-enrolled children without a CC, children with a CC in Iowa are: a) able to overcome the barriers to dental care at higher rates; and b) more likely to utilize all types of care including dental care. These explanations are not mutually exclusive, as Medicaid-enrolled children with a CC may be more successful at obtaining dental care as a result of the effort involved in obtaining medical care.
Second, among children with a CC, there was no statistically significant difference by CC severity. There are two potential explanations. Because of sparse data, especially in the most severe CHSGs, we dichotomized the CC severity variable. This approach could have eliminated any potential differences that existed across CC subgroups. However, a competing problem associated with the alternative approach – comparing the time to first dental visit for unbalanced CC severity subgroups – is low statistical power. Another explanation for these results is that CC severity may be a less important determinant of the time to first dental visit for newly Medicaid-enrolled children than other factors, such as behavioral or medical co-morbidities, that make it difficult for dentists to treat such patients or for caregivers to take their child to a dentist.
Third, there were similarities and differences across the two models in terms of the combination of factors related to the timing of first dental visits. For instance, primary medical care visits and not living in a dental HPSA were associated with earlier visits in Model 1 and were statistically insignificant in Model 2 whereas the interaction between the two proximal factors was significant in both models. These results suggest that the determinants of earlier first dental visits for newly Medicaid-enrolled children are heterogeneous across subgroups. To ensure optimal effectiveness, future clinical interventions may need to consider this heterogeneity to address the needs of child subgroups within the Medicaid population.
Previous Work
Compared to previous findings reported by Damiano et al. (2008), the proportion of children in our study with a first dental visit by 36 months (70%) was lower than for Medicaid-enrolled children ages 0–18 (75%), which is surprising given that we excluded children <3 years. The proportion of children with a CC with a visit within 36 months in our study (77%) was greater than for children in the Medicaid program (73%) but less than the rates for children enrolled in the Separate State Children’s Health Insurance Program (S-SCHIP) I or III (80% and 82%, respectively). This latter finding suggests that Medicaid-enrolled children with a CC are more similar to children from higher-income households and may explain why children with a CC were more likely to have earlier first dental visits after initially enrolling in Medicaid than those without a CC.
Other Determinants of Earlier First Medicaid Dental Visits
Regarding the other factors from our models, children living in non-metropolitan areas (an intermediate factor) were generally less likely to have earlier first dental visits after initially enrolling in Medicaid, which is consisted with findings reported by Damiano et al. (2008). This may be related to variations in the distribution of dentists in metropolitan versus non-metropolitan areas such as distance to the nearest dentist who accepts Medicaid insurance. In addition, from both models, the interaction term between the two proximal factors – having a Medicaid-enrolled sibling or adult in the household – was significant. Compared to children with no enrolled sibling and no enrolled adult, children with an enrolled sibling were more likely to have an earlier first visit after enrolling in Medicaid. There are limitations to these findings given that we lacked other household-level measures such as employment status of the caregiver. Even so, these findings provide preliminary support for policies and interventions that enroll all children from the same household into Medicaid as a way to ensure timely first dental visits after initial enrollment in the Medicaid program.
Contributions, Limitations, and Future Research
Strengths and Weaknesses
This study had a number of strengths. We assessed dental utilization over multiple years, adopted analytic techniques that enabled us to maximize the use of our data through censoring, and used validated methods of identifying children with a CC. However, there are two main limitations. Because we lacked clinical data, we were not able to measure the level of unmet need or the appropriateness of care received by children who had a dental visit. In addition, our study design precluded us from including in our models the behavioral determinants of utilization as reported by caregivers and dentists, which may be even more important than CC status or severity as implied by the model proposed by Patrick and colleagues. We expect these limitations to be addressed in the future through clinical research efforts that incorporate survey and clinical data. These primary data elements can then be combined with administrative data to further expand our conceptual and empirical understanding of the determinants of the time to first dental visit after initial enrollment in Medicaid.
Policy Implications
Regardless of CC status, 22% of children in our study did not have a dental visit within four years of being enrolled in the Medicaid program. Comparable estimates for privately-insured children are not available. In our study, 54% of children did not utilize dental care within one year, compared to 64.2% of poor children ages 2–17 in the U.S. who did not have a dental visit in 2003 (Brown 2006). This comparison suggests that our four-year non-use rate of 22% may be lower than the national average. Furthermore, while the numbers of children eligible for Medicaid through the Home and Community Based Waiver Program was small (n=65), 42% did not have a dental visit. The latter finding is worrisome given that most of these children were long-term enrollees (≥37 months) and young (ages 3–7) – a subgroup for whom timely first dental visits and preventive care are critical in minimizing oral health-related morbidities and the high costs associated with providing treatment under general anesthesia. In light of previous findings that Medicaid-enrolled children are at increased risk for caries (Brickhouse, Rozier, and Slade 2008), Medicaid policies need to ensure that all enrolled children see a dentist shortly after joining the program.
Conclusions
Our findings suggest that newly Medicaid-enrolled children with a CC did not have later first dental visits than children without a CC. And while children with more severe CCs may encounter greater barriers to care, we found that CC severity was not significantly associated with the time to first dental visit after initially enrolling in Medicaid. Future studies should identify the socio-behavioral factors associated with CC severity that may be more important determinants of first dental visits for newly Medicaid-enrolled children. We also found that the determinants of the time to first dental visit after enrolling in Medicaid vary for all Medicaid-enrolled children versus Medicaid-enrolled children with a CC. These findings play an important role in the development of future clinical interventions and policies aimed at improving dental utilization for specific subgroups of children in the Medicaid program that exhibit the greatest disparities in utilization and oral health.
Acknowledgments
This study was supported by NIH/NIDCR Grant T32-DE014678-06, HRSA Dental Public Health Specialty Training Grant D13-HP30026, a Delta Dental Foundation of Iowa Dissertation Research Grant, and a NIH/NIDCR Career Developmental Award 1K08-DE020856-01. The manuscript represents original work that has not been published elsewhere. Parts of the manuscript were presented at the 88th International Association of Dental Research Conference in Barcelona, Spain (July 2010). All the authors take full responsibility for this work and have no conflicts of interest. The study received approval from the University of Iowa Institutional Review Board.
Contributor Information
Donald L. Chi, Email: dchi@uw.edu.
Elizabeth T. Momany, Email: elizabeth-momany@uiowa.edu.
John Neff, Email: john.neff@seattlechildrens.org.
Michael P. Jones, Email: michael-p-jones@uiowa.edu.
John J. Warren, Email: john-warren@uiowa.edu.
Rebecca L. Slayton, Email: rebecca-slayton@uiowa.edu.
Karin Weber-Gasparoni, Email: karin-weber@uiowa.edu.
Peter C. Damiano, Email: peter-damiano@uiowa.edu.
References
- 3M Health Information Systems. 3M Clinical Risk Grouping Software Version 6.1 for Windows. Wallingford, CT: 2008. [Google Scholar]
- Al Agili D, Roseman J, Pass M, Thornton J, Chavers L. Access to dental care in Alabama for children with special needs: parents’ perspectives. J Am Dent Assoc. 2004;135(4):490–5. doi: 10.14219/jada.archive.2004.0216. [DOI] [PubMed] [Google Scholar]
- Al Agili D, Pass M, Bronstein J, Lockwood S. Medicaid participation by private dentists in Alabama. Pediatr Dent. 2007;29(4):293–302. [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry Council on Clinical Affairs (AAPD CCA) Policy on use of a caries-risk assessment tool (CAT) for infants, children, and adolescents. Pediatr Dent. 2005–2006;27(7 Suppl):25–27. [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry Clinical Affairs Committee, American Academy of Pediatric Dentistry Council on Clinical Affairs (AAPD CAC and AAPD CCA) Guideline on periodicity of examination, preventive dental services, anticipatory guidance, and oral treatment for children. Pediatr Dent. 2005–2006;27(7 Suppl):84–86. [PubMed] [Google Scholar]
- American Dental Association (ADA) Current dental terminology 2005, CDT-2005. Chicago, IL: American Dental Association; 2004. [Google Scholar]
- Azarpazhooh A, Main PA. Fluoride varnish in the prevention of dental caries in children and adolescents: a systematic review. J Can Dent Assoc. 2008a;74(1):73–79. [PubMed] [Google Scholar]
- Azarpazhooh A, Main PA. Pit and fissure sealants in the prevention of dental caries in children and adolescents: a systematic review. J Can Dent Assoc. 2008b;74(2):171–177. [PubMed] [Google Scholar]
- Bhuridej P, Kuthy RA, Flach SD, Heller KE, Dawson DV, Kanellis MJ, Damiano PC. Four-year cost-utility analyses of sealed and nonsealed first permanent molars in Iowa Medicaid-enrolled children. J Public Health Dent. 2007;67(4):191–8. doi: 10.1111/j.1752-7325.2007.00025.x. [DOI] [PubMed] [Google Scholar]
- Brickhouse TH, Rozier RG, Slade GD. Effects of enrollment in medicaid versus the state children’s health insurance program on kindergarten children’s untreated dental caries. Am J Public Health. 2008 May;98(5):876–81. doi: 10.2105/AJPH.2007.111468. Epub 2008 Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E. Statistical Brief #117 March 2006. Agency for Healthcare Research and Quality; Rockville, MD: 2006. [Accessed on July 23, 2010]. Children’s dental visits and expenses, United States, 2003. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st117/stat117.shtml. [Google Scholar]
- Casamassimo P, Seale NS, Ruehs K. General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dent Educ. 2004;68(1):23–8. [PubMed] [Google Scholar]
- Chi D, Momany E, Jones M, Damiano P. Newly Medicaid-enrolled children with an intellectual and/or developmental disability in Iowa have later first dental visits. Am J Public Health. 2010 doi: 10.2105/AJPH.2010.191940. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiano PC, Momany ET, Carter KD, Jones MP, Askelson NM. Time to first dental visit after initially enrolling in Medicaid and S-SCHIP. Med Care. 2008;46(12):1234–9. doi: 10.1097/MLR.0b013e31817d92cd. [DOI] [PubMed] [Google Scholar]
- Dubay L, Kenney GM. Health care access and use among low-income children: who fares best? Health Aff (Millwood) 2001;20(1):112–21. doi: 10.1377/hlthaff.20.1.112. [DOI] [PubMed] [Google Scholar]
- Feigal RJ, Jensen ME, Mensing CA. Dental caries potential of liquid medications. Pediatrics. 1981;68(3):416–9. [PubMed] [Google Scholar]
- Ferguson F, Cinotti D. Home oral health practice: the foundation for desensitization and dental care for special needs. Dent Clin North Am. 2009;53(2):375–87. xi. doi: 10.1016/j.cden.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Hale KJ American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 Pt 1):1113–1116. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- Hughes JS, Averill RF, Eisenhandler J, Goldfield NI, Muldoon J, Neff JM, Gay JC. Clinical Risk Groups (CRGs): a classification system for risk-adjusted capitation-based payment and health care management. Med Care. 2004;42(1):81–90. doi: 10.1097/01.mlr.0000102367.93252.70. [DOI] [PubMed] [Google Scholar]
- Iben P, Kanellis MJ, Warren J. Appointment-keeping behavior of Medicaid-enrolled pediatric dental patients in eastern Iowa. Pediatr Dent. 2000;22(4):325–329. [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Aging out of EPSDT: issues for young adults with disabilities. [Accessed on 07/01/2010];Issue Paper #7491. 2007 Available at: http://www.kff.org/medicaid/upload/7491.pdf.
- Kanellis MJ, Damiano PC, Momany ET. Utilization of dental services by Iowa Medicaid-enrolled children younger than 6 years old. Pediatr Dent. 1997;19(5):310–4. [PubMed] [Google Scholar]
- Keene J, Jr, Galasko G, Land M. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71–9. doi: 10.14219/jada.archive.2003.0019. [DOI] [PubMed] [Google Scholar]
- Kuhlthau KA, Beal AC, Ferris TG, Perrin JM. Comparing a diagnosis list with a survey method to identify children with chronic conditions in an urban health center. Ambul Pediatr. 2002;2(1):58–62. doi: 10.1367/1539-4409(2002)002<0058:cadlwa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Lam M, Riedy C, Milgrom P. Improving access for Medicaid-insured children: focus on front-office personnel. J Am Dent Assoc. 1999;130(3):365–373. doi: 10.14219/jada.archive.1999.0206. [DOI] [PubMed] [Google Scholar]
- Lee MA, Horan SA. Children’s access to dental care in Connecticut’s Medicaid managed care program. Matern Child Health J. 2001;5(1):43–51. doi: 10.1023/a:1011397818512. [DOI] [PubMed] [Google Scholar]
- Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005;116(3):e426–31. doi: 10.1542/peds.2005-0390. [DOI] [PubMed] [Google Scholar]
- Macek MD, Edelstein BL, Manski RJ. An analysis of dental visits in U.S. children, by category of service and sociodemographic factors, 1996. Pediatr Dent. 2001;23(5):383–9. [PubMed] [Google Scholar]
- Mayer ML, Stearns SC, Norton EC, Rozier RG. The effects of Medicaid expansions and reimbursement increases on dentists’ participation. Inquiry. 2000;37(1):33–44. [PubMed] [Google Scholar]
- Merrill CT, Nagamine M, Hambrick MM Pediatric Hospital Stays for Cancer. HCUP Statistical Brief #37 September 2007. Agency for Healthcare Research and Quality; Rockville, MD: 2005. [Accessed on September 25, 2009]. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb37.pdf. [PubMed] [Google Scholar]
- Muldoon J, Neff J, Gay J. Profiling the health service needs of populations using diagnosis-based classification systems. J Ambul Care Manage. 1997;20(3):1–18. doi: 10.1097/00004479-199707000-00002. [DOI] [PubMed] [Google Scholar]
- Nainar S. Dentists’ ranking of Medicaid reimbursement rates as a measure of their pediatric Medicaid participation. ASDC J Dent Child. 2000;67(6):422–4. [PubMed] [Google Scholar]
- Neff J, Clifton H, Goldenberg C, Park K, Danielson B, Popalisky J. Selecting children with long lasting chronic conditions for care coordination in a hospital affiliated community clinic. Platform presentation at the Pediatric Academic Society Meeting; Baltimore, Maryland. 2009. Unpublished data. [Google Scholar]
- Newacheck P, McManus M, Fox H, Hung Y, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105(4):760–6. doi: 10.1542/peds.105.4.760. [DOI] [PubMed] [Google Scholar]
- Nowak AJ, Casamassimo PS. Using anticipatory guidance to provide early dental intervention. J Am Dent Assoc. 1995;126(8):1156–1163. doi: 10.14219/jada.archive.1995.0337. [DOI] [PubMed] [Google Scholar]
- Patrick D, Lee R, Nucci M, Grembowski D, Jolles C, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;15;6(Suppl 1):S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez OM, Childers NK. Anticipatory guidance in infant oral health: rationale and recommendations. Am Fam Physician. 2000;61(1):115–20. 123–4. [PubMed] [Google Scholar]
- SAS Institute Incorporated. SAS Release 9.2 for Windows. Cary, NC: 2002–2003. [Google Scholar]
- Savage MF, Lee JY, Kotch JB, Vann WF., Jr Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418–23. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- Slayton RL, Damiano PC, Willard JC. Perceived dental needs of children enrolled in Iowa’s Medicaid Supplemental Security Income (SSI) health plan. ASDC J Dent Child. 2001;68(3):206–10. 152. [PubMed] [Google Scholar]
- U. S. Department of Agriculture Economic Research Service (USDA ERS) [Accessed on 09/19/2009];Measuring Rurality: Rural-Urban Continuum Codes. 2003 Available at: http://www.ers.usda.gov/Data/RuralUrbanContinuumCodes.
- U.S. Department of Health and Human Services (USDHHS) [Accessed on 09/20/2009];Oral Health in America: A Report of the Surgeon General. 2000 Available at: http://www2.nidcr.nih.gov/sgr/sgrohweb/home.htm.