Abstract
Objectives
We conducted a trial to evaluate the effectiveness of a cervical cancer control intervention for Vietnamese women.
Methods
The study group included 234 women who had not received a Pap test in the last three years. Experimental group participants received a lay health worker home visit. Our trial end-point was Pap smear receipt within six months of randomization. Pap testing completion was ascertained through women's self-reports and medical record reviews. We examined intervention effects among women who had ever received a Pap smear (prior to randomization) and women who had never received a Pap smear.
Results
Three-quarters of the experimental group women completed a home visit. Ever screened experimental group women were significantly more likely to report Pap testing (p<0.02) and have records verified Pap testing (p<0.04) than ever screened control group women. There were no significant differences between the trial arms for women who had never been screened.
Conclusions
Our findings indicate that lay health worker interventions for Vietnamese women are feasible to implement and can positively impact levels of Pap testing use among ever screened women (but not never screened women).
Keywords: Asian Americans, Cancer, Screening
INTRODUCTION
Over 10% of Asian Americans are of Vietnamese descent and the Vietnamese American population now exceeds 1,250,000 (1). The majority of Vietnamese Americans came to the United States (US) as refugees or immigrants over the last three decades (2). Cancer registry data show that the cervical cancer incidence rate among Vietnamese women in the US is over twice the cervical cancer incidence rate among non-Latina white women (16.8 versus 8.1 per 100,000) (3). Further, the President's Advisory Commission on Asian Americans recently identified cervical cancer among Vietnamese women as one of the most important health disparities experienced by Asian American populations (4).
According to American Cancer Society guidelines, women should be screened for cervical cancer every one to three years, depending on their risk factors for disease and previous screening history (5). Additionally, national cervical cancer screening goals for the year 2010 specify that at least 97% of women will have received a Pap smear on at least one occasion, and 90% will have received a Pap smear within the previous three years (6). However, California survey data for 2003 indicated that only 70% of Vietnamese women aged 18 years and older had received Pap testing in the previous three years, compared to 84% of white, 87% of black, and 85% of Latina women (7).
Lay health workers are community members who are not certified health care professionals, but have been trained to promote health and/or provide healthcare services within their community. The Cochrane Database for Systematic Reviews recently concluded that lay health worker-based interventions represent a promising approach to disease prevention, and recommended further research on the effectiveness of lay health worker approaches for different health topics and demographic population sub-groups (8). We have previously described our development of a cervical cancer control lay health worker intervention for Vietnamese American women (9). In this report, we provide findings from our randomized controlled trial to evaluate the effectiveness of the lay health worker intervention in improving levels of Pap smear receipt among Vietnamese immigrants to Washington State.
METHODS
Overview of Study Design
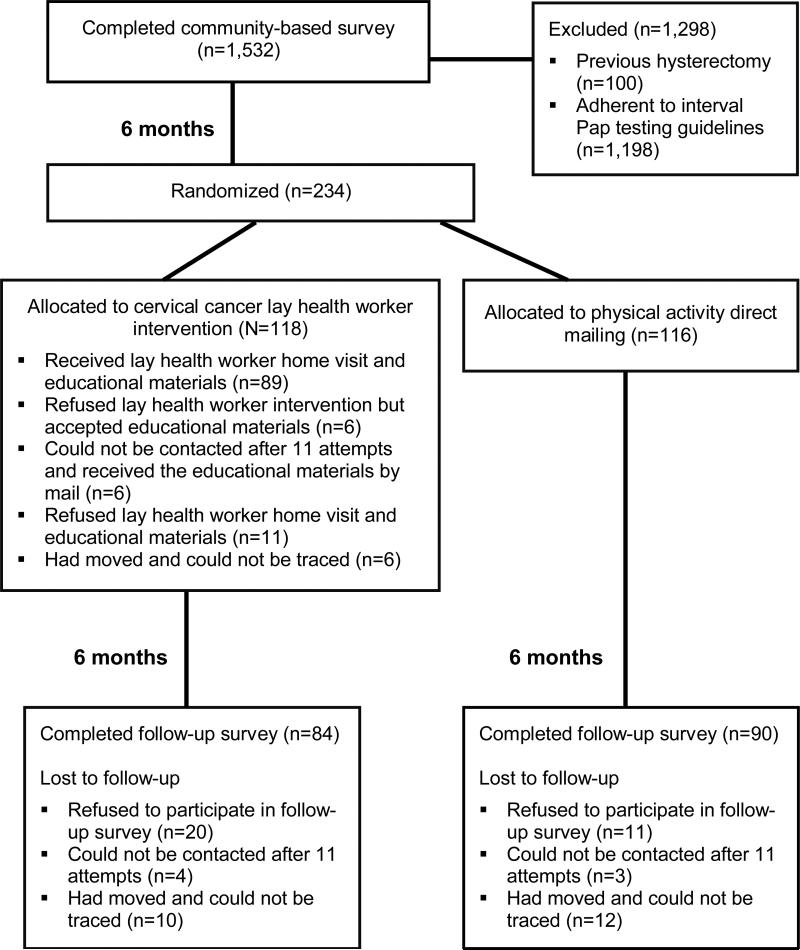
The study design is summarized in Figure 1. Trial participants were women who participated in a community-based survey, conducted in metropolitan Seattle, over a 12-month period during 2006 and 2007. Women were eligible for participation in our community-based survey if they were of Vietnamese descent, aged 20-79 years, and able to speak Vietnamese or English. The survey was conducted face-to-face in women's homes. Respondents provided information about their Pap testing history and demographic characteristics. A total of 1,532 women completed surveys and the survey response rate was 72%. Our sampling and survey methods have been described in detail elsewhere (10,11).
FIGURE 1.
TRIAL OVERVIEW
Community-based survey respondents were eligible for the trial if they were with uteri and non-adherent to guidelines for interval Pap testing. Because regular Pap testing is no longer recommended for women aged 70-79 years who have a history of previous testing, survey respondents in this age-group were only eligible if they had never been screened. Women aged 20-69 years were eligible if they had not been screened for cervical cancer in the previous three years (5).
Trial-eligible women were randomized six months after they participated in the community-based survey. Immediately after randomization, individuals in the experimental group received a cervical cancer lay health worker intervention (that included the use of audio-visual and print educational materials); and control group participants received a mailing of physical activity print materials (pamphlet and fact sheet), as well as a pedometer with instructions for use.
Our primary trial outcome was Pap testing completion within six months of randomization. Outcome ascertainment was based on responses to a follow-up survey. We also attempted to verify self-reports of Pap testing in the interval between randomization and follow-up survey completion with medical records.
All study materials were translated into Vietnamese using standard methods (12). Project personnel with direct participant contact (survey interviewers and lay health workers) were all bicultural, bilingual Vietnamese American women.
Consent Procedures
The Fred Hutchinson Cancer Research Center Institutional Review Board approved our study protocols. Participants provided written consent for the community-based survey, trial follow-up survey, and release of medical records; and verbal consent for the lay health worker intervention. During the community-based survey consent process, women were explicitly told that they might be offered health education in the future (if they participated in the community-based survey).
Randomization
We randomized 234 women into the trial. Our random assignment was performed separately for the women who had never received a Pap smear (n=106) and the women who had received at least one Pap smear but had not been screened recently (n=126). A project coordinator assigned women to the experimental or control group using computer generated randomization lists. The randomization order was based on date of community-based survey completion.
Pap Testing Educational Materials
We used findings from an earlier qualitative study to develop culturally and linguistically appropriate materials for use in the cervical cancer control lay health worker intervention. Our material development has been described in detail elsewhere (9). Project materials included a Vietnamese language DVD (with English sub-titles) and a pamphlet (with both Vietnamese and English text). These materials provide basic information about cervical cancer and the Pap test (within the context of Vietnamese traditional beliefs about women's health), and emphasize the importance of Pap testing for all women (including those who are asymptomatic, not currently sexually active, and post-menopausal). Several visual aids were also developed by the project: a graph showing cervical cancer incidence rates by race/ethnicity, a gynecologic anatomy diagram, and a figure showing how cervical cancer progresses.
Lay Health Workers
Two lay health workers were selected. They were both fluently bilingual ethnic Vietnamese women who grew up in Vietnam and were conversant with Vietnamese culture. These women were married with children so that traditional Vietnamese participants would have comfort and confidence in discussing reproductive concerns with them. Neither of the lay health workers was a certified health professional. The lay health workers were trained to act as role models, give social support, and provide tailored responses to each woman's individual barriers to Pap testing (e.g., believing that Pap testing is unnecessary for asymptomatic women) (9).
Lay Health Worker Intervention
Lay health workers made up to 11 attempts to complete a home visit with each experimental group participant. Women who refused a home visit were offered the educational materials (DVD and pamphlet). If a lay health worker was unable to contact a participant, the educational materials were mailed to her home. During home visits, lay health workers systematically asked participants if they could watch the DVD together, offered participants a copy of the DVD and pamphlet, and showed participants the visual aids. Finally, the lay health workers attempted to complete follow-up telephone calls with participants one month after completed home visits to offer further assistance, as necessary.
Follow-up Survey
To trace individuals who had recently moved, we used contact information for friends/relatives (provided at the time of the baseline survey), and the national change of address system. Interviewers made up to 11 follow-up contact attempts (including weekday, weekend, and evening attempts). All follow-up interviews were conducted face-to-face in participants’ homes. Respondents received a small financial incentive for follow-up survey completion. Each follow-up survey respondent was asked whether she had ever had a Pap test and, if so, when she was last screened. Other questions assessed exposure to the Pap testing educational materials. Follow-up survey interviewers were unaware of each participant's trial randomization assignment.
Medical Record Reviews
Follow-up survey respondents who reported they had received Pap testing in the six-month interval since their random assignment were asked to provide information about the date of testing, as well as the name and location of the clinic or doctor's office where testing was performed. Each of these participants was also asked to sign a medical release form giving project staff permission to request medical record verification of her self-reported Pap test. A copy of the Pap test result was then requested (from the relevant clinic or doctor's office) using a form that provided the participant's name, age, and self-reported date of testing. The project contacted each health care facility up to three times (twice by mail and once by telephone).
Process Evaluation
Process data were collected to document the implementation and content of our cervical cancer control intervention. Specifically, lay health workers routinely completed forms addressing the outcome of home visit attempts (e.g., agreed to participate in a home visit, refused a home visit but accepted the educational materials, or refused a home visit and the health education materials). They also documented use of the project DVD, pamphlet, and visual aids, as well as follow-up telephone calls. A home visit was considered complete if the lay health worker was able to complete a discussion about Pap testing at a woman's home.
Statistical Analysis
Our primary outcome analysis included all randomized individuals and assumed that participants without follow-up data were not screened after randomization. We also conducted a secondary outcome analysis that only included randomly assigned women with follow-up data. Experimental group women who did not receive the cervical cancer screening intervention were included in study analyses. Our outcome evaluation was conducted using follow-up survey data and then repeated using medical records data. We conducted stratified analyses and examined intervention effects among women who had ever received a Pap smear (prior to randomization) and women who had never received a Pap smear (as well as the study group as a whole). Fisher's exact tests were used to evaluate statistical significance with respect to differences in proportions between the arms. Unconditional logistic regression was also performed to adjust the intervention effect for demographic variables..
RESULTS
Follow-up Survey Response
Our follow-up survey response is detailed in Figure 1. Eight-four (71%) of the 118 women who were randomized to the experimental arm and 90 (78%) of the 116 women who were randomized to the control arm completed follow-up surveys. The proportions of experimental and control group with follow-up data were not significantly different.
Study Group Characteristics
Only one of the trial participants who completed a follow-up survey (randomized to the experimental arm) was born in the US. The baseline characteristics of all women assigned to the experimental and control arms are given in Table 1. Our two trial groups were equivalent with respect to demographic characteristics.
TABLE 1.
BASELINE CHARACTERISTICS OF RANDOMIZED WOMEN
| Characteristic | Experimental n = 118 N (%) | Control n = 116 N (%) | p-value |
|---|---|---|---|
| Age (years) | |||
| < 50 | 56 (47) | 49 (43) | 0.51 |
| ≥ 50 | 62 (53) | 65 (57) | |
| Education (years) | |||
| < 12 | 64 (54) | 59 (51) | 0.69 |
| ≥ 12 | 54 (46) | 57 (49) | |
| Marital status | |||
| Currently married | 77 (65) | 81 (70) | 0.49 |
| Not currently married | 41 (32) | 35 (30) | |
| Years in US | |||
| < 15 | 83 (70) | 70 (61) | 0.13 |
| ≥ 15 | 35 (30) | 45 (39) | |
| English proficiency | |||
| Does not speak well or at all | 50 (42) | 54 (47) | 0.60 |
| Speaks well or fluently | 68 (58) | 62 (53) | |
| Pap testing history | |||
| Ever screened | 64 (54) | 64 (55) | 0.90 |
| Never screened | 54 (46) | 52 (45) |
Medical Records Verification
Twenty-eight of the experimental group and 16 of the control group reported they had received a Pap test in the six-month interval between randomization and follow-up. We were able to request medical records for 25 of these experimental group participants and all of these control group participants. (The three other participants refused to sign a medical records release or provided insufficient information about the clinic where Pap testing was performed.) All the health care facilities responded to our requests for information about cervical cancer screening. Medical records verified self-reported Pap testing for 18 (64%) of the 28 experimental group women and 8 (50%) of the 16 control group women who self-reported Pap testing.
Outcome Analyses
Table 2 provides findings from our primary outcome analyses (all randomized women), as well as our secondary outcome analyses (all women with follow-up data). Among all randomized women, 24% of the experimental group reported Pap testing after randomization, compared to 14% of the control group (p=0.07). Medical records verified Pap smear receipt for 15% of the 118 experimental group participants and 7% of the 116 control group participants (p=0.06). Our stratified analyses documented an intervention effect for women who had received at least one Pap smear during their lifetime (but had not received a Pap smear in the three years prior to randomization). There were no significant differences in experimental and control group Pap testing completion rates among women who had never been screened for cervical cancer at baseline. Findings from the unadjusted analyses were unchanged in logistic regression analyses (adjusting for demographic characteristics).
TABLE 2.
OUTCOME EVALUATION
| Outcome | Group | Experimental N (%) | Control N (%) | p-value | OR (95% CI)* |
|---|---|---|---|---|---|
| Primary analysis – All randomized women (experimental group N=118, control group N=116) | |||||
| Self-reported Pap testing | All women | 28 (24) | 16 (14) | 0.07 | 1.78 (0.88–3.60) |
| Ever screened women | 20 (31) | 8 (13) | 0.02 | 3.15 (1.20–8.27) | |
| Never screened women | 8 (15) | 8 (15) | 1.00 | 0.85 (0.28–2.58) | |
| Medical records verified Pap testing | All women | 18 (15) | 8 (7) | 0.06 | 2.37 (0.94–5.97) |
| Ever screened women | 13 (20) | 4 (6) | 0.03 | 3.63 (1.06–12.45) | |
| Never screened women | 5 (9) | 4 (8) | 1.00 | 1.00 (0.24–4.19) | |
| Secondary analysis – Women with follow-up data (experimental group N=84, control group N=90) | |||||
| Self-reported Pap testing | All women | 28 (33) | 16 (18) | 0.02 | 2.17 (1.03–4.56) |
| Ever screened women | 20 (43) | 8 (16) | 0.004 | 4.25 (1.50–12.01) | |
| Never screened women | 8 (22) | 8 (21) | 1.00 | 0.80 (0.25–2.60) | |
| Medical records verified Pap testing | All women | 18 (21) | 8 (9) | 0.03 | 2.84 (1.09–7.39) |
| Ever screened women | 13 (28) | 4 (8) | 0.01 | 4.59 (1.28–16.48) | |
| Never screened women | 5 (14) | 4 (10) | 0.73 | 1.17 (0.26-5.30) | |
Adjusted for age, education, marital status, years in US, and English proficiency
Process Measures
Lay health workers were able to complete home visits with 75% of the women randomized to our experimental arm (Figure 1). The remaining women either refused a home visit but accepted the educational materials (5%), could not be contacted after 11 attempts and received the educational materials by mail (5%), refused a home visit and the educational materials (9%), or had moved and could not be traced (5%). Twenty-five of the 28 experimental group women who reported a Pap test at follow-up had completed a lay health worker home visit (one woman had received the educational materials by mail, and two had refused the home visit and educational materials).
Project personnel reported watching the DVD with 80% of the 89 home visit participants. Our three visual aids were shown during 94% of home visits, and the DVD and pamphlet were both provided at the end of all lay health worker visits. Follow-up telephone calls were successfully completed with 84% of the home visit participants. Three-quarters (75%) of the 84 experimental arm women with follow-up data self-reported they had watched the DVD and 55% self-reported they had read the pamphlet.
DISCUSSION
Our findings indicate that lay health worker interventions for Vietnamese women are acceptable to the community, feasible to implement, and can positively impact levels of Pap testing use among women who have previously been screened for cervical cancer (but are non-adherent with guidelines for interval screening). Specifically, 84% of the 106 women that our lay health workers were able to contact completed a home visit. Additionally, we demonstrated an intervention effect among previously screened women using a conservative approach which assumed that all women without follow-up data were unscreened, as well as that failure to retrieve a Pap testing medical record always meant that the woman was truly unscreened.
A previous California study randomized Vietnamese women to lay health worker group education plus media-based education (combined intervention) or media-based education alone (media only intervention). Women provided information about their Pap testing history four months after randomization. The combined intervention was more effective than the media only intervention in increasing the rate of previous Pap testing receipt (66% to 82% versus 70% to 76%, p<0.001). Among those who had never been screened, significantly more women in the combined intervention group (46%) than in the media only group (27%) obtained Pap tests (p<0.001) (13). It is possible that the California intervention was more effective for previously unscreened women than our intervention because of differences in the intervention intensity and/or components. Specifically, the California intervention included two face-to-face educational sessions with lay health workers (rather than one face-to-face educational session) and use of a flipchart (rather than a DVD).
In our study, 33% of experimental group women with follow-up data and 18% of control group women with follow-up data reported Pap testing (p=0.02). Previous studies have evaluated lay health worker interventions for women who are non-adherent to Pap testing guidelines among other racial/ethnic minority groups with similar results. Another Washington State study focused on Chinese American women. Six months after randomization, 37% of the experimental group and 22% of the control group reported Pap testing (p=0.07) (14). A Texas study focused on low-income Hispanic women. Pap testing completion was significantly higher in the experimental group (40%) than the control group (24%) when women were interviewed after an interval of six months (15).
Our study strengths include a randomized controlled design, as well as use of both self-report and medical records data for end-point ascertainment. Several studies have found that the accuracy of screening test self-reports among Asian American women is relatively low, compared to the accuracy among non-Latina white women (16,17). For example, one study was able to verify Pap smear self-report for 85% of non-Latina white women, but only 68% of Chinese women and 67% of Filipina women (16). We were able to request medical records for 41 (93%) of the 44 women who reported Pap testing following randomization, and were able to verify Pap testing for 24 (63%) of these 41 women. Asian naming systems may result in misfiling of test results and difficulty finding medical records. It is possible, therefore, that at least some of the women whose self-reported recent Pap testing could not be verified had, in fact, received a recent Pap smear.
Our study has several limitations that should be recognized. First, we recruited individuals living in one geographic area of the US, and the results may not be applicable to all Vietnamese American women. Second, only individuals who agreed to complete a baseline survey were eligible for participation in the trial, and survey responders may be more receptive to health education programs than survey non-responders. Third, although we requested the medical records of all individuals who reported Pap testing since randomization, we made no attempt to verify the accuracy of self-reports among women who reported they had not been tested. It is possible that some of these individuals received a Pap test, without their knowledge, during a gynecologic exam for a health problem. Finally, our follow-up interval was only six months and some trial participants may have received Pap testing after their follow-up survey.
Our results add to the evidence concerning the effectiveness of lay health worker approaches to cervical cancer control in Vietnamese and other Asian immigrant communities (13,14,18). Future research should evaluate the effectiveness of lay health education for other racial/ethnic minority and limited English proficient groups, as well as other screening modalities (e.g., fecal occult blood testing and colonoscopy). It will also be important for researchers to conduct dissemination studies focusing on the adaptation and implementation of cervical cancer control lay health worker interventions in community health center and other community-based organization settings (15).
ACKNOWLEDGEMENTS
This publication was supported, in part, by grant R01-CA-115564 from the National Cancer Institute, cooperative agreement U01-CA-114640 from the National Cancer Institute, and cooperative agreement U48-DP-000050 from the Centers for Disease Control and Prevention. The contents of the article are solely the responsibility of the authors and do not necessarily represent the views of the National Cancer Institute nor the Centers for Disease Control and Prevention. We thank the Vietnamese survey interviewers and lay health workers for their outstanding work.
REFERENCES
- 1.US Census Bureau . The American Community–Asians: 2004. US Department of Commerce; Washington DC: 2007. [Google Scholar]
- 2.Chan S, Lee E. Families with Asian Roots. In: Lynch EW, Hanson MJ, editors. Developing Cross-cultural Competence. Paul Brookes Publishing; Baltimore: 2004. pp. 241–245. [Google Scholar]
- 3.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations. Cancer Causes Control. 2008;19(3):227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asian Americans and Pacific Islanders–Addressing Health Disparities: Opportunities for Building a Healthier America. Department of Health and Human Services; Washington DC: 2003. President's Advisory Commission on Asian Americans and Pacific Islanders. pp. 21–23. [Google Scholar]
- 5.Saslow D, Runowicz CD, Solomon D, et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52(6):342–362. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services . Healthy People 2010–Understanding and Improving Health. US Government Printing Office; Washington DC: 2000. pp. 3–23. [Google Scholar]
- 7.Holtby S, Zahnd E, Lordi N, McCain C, Chia YJ, Kurata J. Health of California's Adults, Adolescents, and Children. California Department of Health Services; Sacramento: 2006. p. 23. [Google Scholar]
- 8.Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care. The Cochrane Library. 2005;(1):2. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Burke NJ, Jackson JC, Lam DH, Acorda E, Chan NL, Taylor VM. Good health for New Years: development of a cervical cancer control outreach program for Vietnamese immigrants. J Cancer Educ. 2004;19(4):244–250. doi: 10.1207/s15430154jce1904_13. [DOI] [PubMed] [Google Scholar]
- 10.Taylor VM, Yasui Y, Nguyen T, et al. Pap smear receipt among Vietnamese immigrants: the importance of health care factors. Ethnic Health. 2009;14(6):575–589. doi: 10.1080/13557850903111589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor VM, Nguyen TT, Do HH, Li L, Yasui Y. Lessons learned from the application of a Vietnamese surname list for survey research. J Immigr Minor Health. 2009 doi: 10.1007/s10903-009-9296-x. Epub Oct 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eremenco SL, Cella D, Arnold BJ, et al. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28(2):212–232. doi: 10.1177/0163278705275342. [DOI] [PubMed] [Google Scholar]
- 13.Mock J, McPhee SJ, Nguyen T, et al. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97(9):1693–1700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor VM, Hislop TG, Jackson JC, et al. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. J Natl Cancer Inst. 2002;94(9):670–677. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernandez ME, Gonzales A, Tortolero-Luna G, Saavedra-Embesi M, Chan W, Vernon SW. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am J Public Health. 2009;99(5):936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McPhee SJ, Nguyen TT, Shema SJ, et al. Validation of recall of breast and cervical cancer screening by women in an ethnically diverse population. Prev Med. 2002;35(5):463–473. doi: 10.1006/pmed.2002.1096. [DOI] [PubMed] [Google Scholar]
- 17.Pasick R, Stewart S, Bird J, O'Nofrio C. Quality of data in multiethnic health surveys. Public Health Rep. 2001;116(1):223–243. doi: 10.1093/phr/116.S1.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CNH. Opening pathways to cancer screening for Vietnamese-American women: Lay health workers hold a key. Prev Med. 1998;27:821–829. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]