Abstract
Objective
To determine whether profit status may be associated with differences in hospital days per patient, an outcome that may also be influenced by provider financial goals.
Data Sources
United States Renal Data System and Centers for Medicare and Medicaid Services cost reports.
Design
We compared the number of hospital days per patient per year across for-profit and non-profit dialysis facilities during 2003. To address possible referral bias in the assignment of patients to dialysis facilities, we used an instrumental variable regression method, and adjusted for selected patient-specific factors, facility characteristics such as size and chain affiliation, as well as metrics of market competition.
Data Extraction Methods
All patients who received in-center hemodialysis at any time in 2003 and for whom Medicare was the primary payer were included (N=170,130; roughly two-thirds of the US hemodialysis population). Patients dialyzed at hospital-based facilities and patients with no dialysis facilities within 30 miles of their residence were excluded.
Results
Overall, adjusted hospital days per patient were 17% ± 5% lower in non-profit facilities. The difference between non-profit and for-profit facilities persisted with the correction for referral bias. There was no association between hospital days per patient per year and chain affiliation but larger facilities had inferior outcomes (facilities with 73 or more patients had a 14% ± 1.7% increase in hospital days relative to facilities with 35 or less patients). Differences in outcomes among for-profit and non-profit facilities translated to 1,600 patient-years in hospital that could be averted each year if the hospital utilization rates in for-profit facilities were to decrease to the level of their nonprofit counterparts.
Conclusions
Hospital days per patient-year were statistically and clinically significantly lower among non-profit dialysis providers. These findings suggest that the indirect incentives in Medicare’s current payment system may provide insufficient incentive for for-profit providers to achieve optimal patient outcomes.
Keywords: Dialysis, end-stage renal disease, instrumental variables, for-profit, hospital days
Introduction
Several studies have examined differences in mortality rates among for-profit and non-profit dialysis facilities. These studies have been widely criticized for having insufficiently considered risk adjustment and possible referral bias. A recent comprehensive analysis conducted by [Brooks et al. 2006] utilized an instrumental variable approach and demonstrated no significant difference in mortality rates among for-profit and non-profit dialysis facilities. Since mortality is a terminal event that happens infrequently (at most once for each patient), we are concerned that statistical tests lack sufficient power to detect differences in mortality among for-profits and nonprofits. This paper considers a more frequent event, days in the hospital, to test whether there are significant differences among for-profit and non-profit dialysis.
Selecting a clinical outcome for comparing for-profit and non-profit dialysis providers should be based on a theoretical justification of how the behavior of providers differs based on their profit status and leads to differences in that outcome. The most common justification is based on the assumption of different objectives: for-profits are profit maximizers while non-profits adopt public interest goals [Horwitz 2007]. Therefore, for-profits will be more likely than non-profits to provide profitable services and less likely to provide unprofitable ones. Empirical evidence supporting that theoretical justification in the context of non-profit and for-profit hospitals have been previously reported.
To apply this theoretical justification in the context of dialysis we need to identify a clinical outcome that is inadequately rewarded by the existing reimbursement system: an outcome in which the financial rewards to the provider from interventions that aim to improve it are less than the cost of these interventions. Days in the hospital could provide such a clinical outcome. Preventing infections and other complications in dialysis patients that lead to lengthy hospitalizations is within the realm of activities undertaken by dialysis providers. However, the financial rewards are modest in the form of avoiding missed treatments while the costs can be considerable. If the costs exceed the rewards, then we expect for-profit providers to have higher hospitalization days than non-profit providers. If the costs are less than the rewards, we would expect the opposite. One would expect relatively high costs of hospitalization avoidance strategies, as these would generally require input from professionals (e.g., physicians, pharmacists or registered nurses, functioning to monitor or screen for drug-drug interactions or problems with vascular access) whose services would be more expensive than those conducted for the routine provision of dialysis, which are principally performed by technicians.
We explored these issues by using Medicare data to test for differences in hospital outcomes among patients treated in for-profit versus non-profit facilities.
Methods
Data Sources
Data were obtained from the United States Renal Data System [USRDS]. All patients who received in-center hemodialysis at any time in 2003, had no prior transplants prior to 1/1/2003, and for whom Medicare was the primary payer were included (N=170,130; roughly two-thirds of the US hemodialysis population). These patients received treatment from one of J=3,443 freestanding dialysis facilities in 2003. Patients dialyzed at hospital-based facilities1 and patients with no dialysis facilities within 30 miles2 of their residence were excluded. The following information was available for each patient: age, sex, race, ethnicity, vintage (time since initiation of dialysis), employment status, insurance coverage at the onset of ESRD, height and weight, serum albumin, creatinine, blood urea nitrogen, hemoglobin, estimated glomerular filtration rate, ability to ambulate and/or transfer, tobacco use, alcohol and/or drug dependence, cancer, diabetes, hypertension and four other co morbid conditions. For patient i this biographical information is captured by the vector
| (1) |
A complete history of Medicare institutional claims was available for all patients. Patients who ever switched dialysis facilities during 2003 (<1%) were assumed to have received dialysis from the facility at which they dialyzed for the longest duration during the year. We censored observations at the time of transplantation.
Facility data for the 3,443 freestanding facilities were derived from the dialysis cost report (CMS form “265-94” [2],[4],[9]) and included the following: chain and profit status; location; number of patients; number of registered nurses and licensed practical nurses/nurse aides/technicians; proportion of patients with hematocrit >33% and urea reduction ratio (URR, an index of dialysis efficiency) >65%; average number and duration of treatments per patient per week; average number of times of dialyzer reuse; proportion of patients who have private insurance. Measures of market characteristics for each facility were also computed. The degree of market competition for the zip code of each facility was given by a number that ranged from 0 to 1 with higher values indicating higher level of competition. The market competition metric was obtained by subtracting the Hirschman-Herfindahl index from one. The Hirschman-Herfindahl index is a measure of market concentration defined as the squared sum of market shares of all free-standing facilities located within 30 miles of the given zip code, where higher values indicate higher levels of market concentration (lower competition) [Hirschman 1945], [Herfindahl 1950]. For-profit market share index was defined as the percentage of hemodialysis patients in for-profit clinics within 30 miles of each facility’s zip code. Chain market share was defined similarly. For facility j we will use the vector
| (2) |
to record the facility information that will be used in our analyses: size of the facility3 (1–35 patients; 36–72 patients; >72 patients), chain affiliation, profit status, market competition, for-profit market share, chain market share, and proportion of patients with private insurance.
Outcomes
To test whether profit status is associated with increased hospital days we examined the patient outcome
| (3) |
“Days at risk in 2003” is the number of days in 2003 for which the patient was on a dialysis facility’s regular patient roster, including days of temporary absences due to hospitalizations. “Days in hospital” is the number of days within this period that the patient spent in hospital. Subanalyses were performed for patients who started dialysis, for patients who died, and for patients who received a transplant during the year of study.
Statistical Models
Our framework builds on the ideas used in [McClellan et al. 1994] and [Kessler & McClellan 2000] and directly generalizes the for-profit/non-profit binary choice model in [Brooks et al. 2006] to individual facility choice. Using subscript indices for indexing patients and superscript indices for facilities, for patient i receiving treatment from facility j * we define the vector of patient choice as
| (4) |
First we modeled patient choice as a utility maximization problem whereby a patient chooses the facility that maximizes his/her utility gained from that choice. Thus if denotes the utility gained by patient i from choosing facility j, then
| (5) |
Whenever j is beyond 30 miles of i we impose , so that a patient never chooses a facility further than 30 miles away from their residence4. Otherwise, we allow to depend on the travel distance5 (in miles) from patient i to facility j. also depends on measurable confounders (interactions of known patient-specific factors with facility characteristics) as well as the unobserved confounders . We impose the following functional form on the utilities
| (6) |
Sμ(d) is a decreasing piecewise linear function (parameterized by μ−1, μ0, μ1, μ2, μ3) of travel distances, with {kq}q= 1,2,3 denoting the quartiles of the distribution of . In other words, the appeal of a facility decreases with travel distance. Conditional logistic regression [McFadden 1973] was used to estimate (\6). To account for differences in distance perception across the country, the model was fitted separately for each of the eighteen ESRD Network regions6.
In the second stage, we estimated a log-linear model of patient hospital days as follows:
| (7) |
αnetwork(i) is a geographic effect, where the U.S. is divided into one of the eighteen regional ESRD Networks7 [5]. The term βPATi controls for observable patient-specific confounders. The sum gives the characteristics of the facility that patient i received treatment from, so γ represents the effect of facility characteristics such as profit status on patient hospital days. Analogous to the argument in [Brooks et al. 2006], if ζ is correlated with ε then the estimates of γ will be biased. To ameliorate this bias we replace the actual patient facility choice with the predicted choice probabilities from the choice model (6). The only variation in used to estimate γ comes from the travel distances (the instruments), which are assumed to be exogenous.
The use of travel distances as an instrument in the dialysis setting was validated in [Brooks et al. 2006]. To recap, for an instrument to be useful it must be a) related to patient’s choice of dialysis facility and b) unrelated to the unobserved error ε in (7). To verify a) a histogram of the relative8 distance between patients and their chosen facility was produced. A positive skew9 in the histogram would suggest that the patients preferred closer facilities and hence provides support for a). A test of overidentifying restrictions [Stock & Watson 2006] was used to evaluate b).
For comparison with results unadjusted for referral bias, the entire estimation procedure was repeated using the actual patient choice in the second stage in lieu of the predicted choice. Analyses were conducted using SAS (SAS Institute Inc., Cary, NC), Matlab (MathWorks Inc., Natick, MA) and R (The R Foundation for Statistical Computing, www.r-project.org).
Results
Table 1 shows the unadjusted hospital days and facility characteristics by profit and chain status. In general, non-profit facilities were located away from areas with a heavy concentration of for-profit facilities, and independent facilities were outside markets saturated with chain facilities.
Table 1.
Differences in Outcomes and Facility Characteristics by Ownership Status
| Independent | Chain | |||
|---|---|---|---|---|
| Non-Profit | For-Profit | Non-Profit | For-Profit | |
| Proportion of facilities* | 4.4% | 18% | 5.1% | 73% |
| Proportion of patients** | 4.9% | 16% | 4.5% | 75% |
| Days in Hospital per year-at-risk | 18.6 | 19.8 | 16.4 | 19.2 |
| Patients per facility | 73 (4.0) | 64 (1.7) | 60 (2.5) | 67 (1.6) |
| Market Competition*** | 0.25 (0.02) | 0.22 (0.006) | 0.24 (0.01) | 0.22 (0.006) |
| For-Profit market share | 0.56 (0.027) | 0.92 (0.006) | 0.54 (0.023) | 0.92 (0.006) |
| Chain market share | 0.42 (0.026) | 0.49 (0.01) | 0.90 (0.01) | 0.087 (0.007) |
| Private payor mix | 0.26 (0.01) | 0.25 (0.005) | 0.22 (0.008) | 0.25 (0.006) |
Note: Standard errors are reported in the parentheses.
3,443 free-standing dialysis facilities included in study.
170,130 hemodialysis patients in study.
Market competition is measured on a scale from 0 to 1, with higher values indicating higher level of competition. Its precise definition is 1 minus the Hirschman-Herfindahl index, a measure of market competition that also ranges from 0 to 1.
Table 2 presents regression estimates for facility and market characteristics, considering hospital days as the dependent variable (patient characteristics omitted for brevity). Estimates obtained from using actual patient assignment (and therefore unadjusted for referral bias) are also presented. Patients dialyzing at for-profit facilities spent 17% ± 5% more days in hospital than patients dialyzing in non-profit facilities, whereas the effect unadjusted for referral bias was 10% ± 3% (p<0.0001 for both comparisons). Chain affiliation was not associated with the number of hospital days. There was no association between payer mix and hospitalization under the adjusted estimates. However, estimates unadjusted for referral bias showed a significant association between payer mix and hospital days (p<0.0001).
Table 2.
Regression Estimates and Standard Errors for the Associations among Facility and Market Characteristics and Total Number of Hospital Days Per Patient Per Year at Risk.
| Probabilistic patient choice adjusted estimates |
Actual patient choice estimates |
||||
|---|---|---|---|---|---|
| Coefficient (S.E.) | p-value | Coefficient (S.E.) | p-value | ||
| Facility size (# of patients) | 0–35 (lower tier) | 0 | - | 0 | - |
| 35–72 (mid tier) | 0.041 (0.017) | 0.017 | −0.044 (0.013) | 0.001 | |
| 72+ (top tier) | 0.14 (0.017) | <0.001 | −0.021 (0.013) | 0.10 | |
| Profit Status | 0.17 (0.048) | <0.001 | 0.098 (0.030) | <0.001 | |
| Chain Affiliation | 0.058 (0.040) | 0.15 | −0.0034 (0.020) | >0.20 | |
| Market competition - chain interaction | −0.034 (0.050) | >0.20 | 0.00050 (0.079) | >0.20 | |
| Market competition* | 0.23 (0.041) | <0.001 | 0.44 (0.071) | <0.001 | |
| For-Profit Market Share | −0.078 (0.047) | 0.099 | −0.039 (0.032) | >0.20 | |
| Chain Market Share | −0.030 (0.041) | >0.20 | 0.042 (0.027) | 0.13 | |
| Fraction of patients with private insurance | Non-Profit | 0.089 (0.15) | >0.20 | 0.21 (0.11) | 0.042 |
| For-Profit | 0.10 (0.092) | >0.20 | 0.19 (0.055) | <0.001 | |
Market competition is measured on a scale from 0 to 1, with higher values indicating higher level of competition. Its precise definition is 1 minus the Hirschman-Herfindahl index, a measure of market competition that also ranges from 0 to 1.
Neither for-profit nor chain market concentration were associated with hospital days. However, market competition was directly associated with hospital days for both the adjusted and unadjusted estimates. Larger facilities had inferior outcomes (facilities with 73 or more patients had a 14% ± 2% increase in hospital days relative to facilities with 35 or less patients) but the association was not significant under the estimates unadjusted for referral bias.
The association of for-profit status with hospital days for subsets of patients who i) received dialysis for the entire year of 2003; ii) started dialysis during the year; and iii) died during the year were 12% ± 7%, 20% ± 7% and 24% ± 11%, respectively.
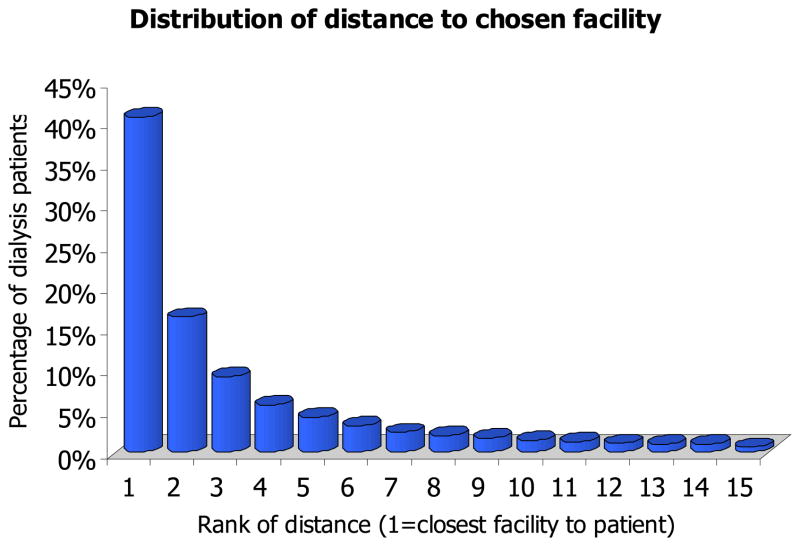
The histogram of Figure 1 shows that patients overwhelmingly prefer dialysis facilities closer to their homes, demonstrating the correlation between facility choice and travel distances. The test of over-identifying restrictions yielded a p-value >0.20, hence we do not reject the null hypothesis that travel distances are uncorrelated with unobserved patient risk factors (and serves as a suitable instrument for reducing referral bias). Hausman’s specification test offered moderate evidence (p=0.10) against random assignment of patients to facilities.
Figure 1.
Histogram of the “relative distance” between patients and their chosen facility. For each patient, we ordered the travel distances in ascending order and used the rank of the chosen facility as the relative distance.
Discussion
Patients treated in for-profit dialysis facilities experienced 17% more instrumental variable risk-adjusted hospital days than in their non-profit counterparts, or about 3 additional days per year. There was no statistically significant difference in hospital days among chain-affiliated and independent facilities. Adjustments for case mix, facility size, payer type, market factors and for referral bias in the choice of dialysis facility were made in order to ensure that these results were not due to either observable risk factors or unobservable referral bias (i.e., sicker patients being referred to for-profit providers and thus artificially increasing hospital days).
Our main finding is consistent with our original hypothesis that patients treated in for-profit dialysis providers will have higher hospital days per year because the cost of any interventions that would prevent lengthy hospital admissions are greater than the financial rewards from avoiding missed treatment. In that context, prevention of lengthy hospital admissions is an example of an unprofitable activity and thus less likely to be adopted by for-profit providers.
A recent study has also provided results that are consistent with the same basic hypothesis that for-profit dialysis providers are more likely than their non-profit counterparts to take profitable actions and shirk on unprofitable ones. Large for-profit dialysis chains were found to use higher epoetin dose adjustments and target higher hemoglobin levels, probably because the cost of achieving higher hemoglobin concentrations is less than the additional reimbursement for higher epoetin dose [Thamer et al. 2007]. However, alternative explanations exist. Even though the unit for comparing differences in outcomes was the dialysis provider, the frequency and duration of hospital admissions are also influenced by the nephrologists and other admitting physicians and by the admitting hospital. One could not rule out the hypothesis that the difference is due to the behavior of these other parties: for instance, revenue maximizing physicians would be more likely to admit patients and keep patients in hospital longer, because payments for hospital care of ESRD patients are derived on a fee-for-service basis, whereas routine maintenance dialysis care is capitated. This perverse incentive might be tempered if physicians’ financial interests were more closely linked to the dialysis facility but may be exaggerated if physicians only see a small number of patients (because of increased competition). We were unable to directly adjust for hospital and physician-specific effects (admitting hospital and physician identifiers are not included in the USRDS data). However, we partially corrected for such effects by controlling for observable facility and market characteristics that are expected to be correlated with physician incentives: chain affiliation (physicians are more likely to have a financial stake in independent facilities) and market competition (physician revenue from capitated outpatient treatments drop when competition for patients increase, raising the importance of revenue from services derived from hospital stays).
It is also possible that the differences identified here could be explained by relationships for-profit and non-profit dialysis providers form with hospitals and physicians in their area. Specifically, our data have revealed that only patients treated in chain-affiliated non-profit clinics had a lower number of hospital days. There were no significant differences across patients treated in independent clinics or for-profit chains (results not shown). In the time period considered here, there were four for-profit chains and one non-profit chain. The non-profit chain’s business model, unlike its for-profit counterparts, relied on close relationships with academic centers and nephrologists in geographic proximity with its clinics. This relationship may affect the incentives of admitting physicians to admit and discharge patients from a hospital, and can influence the difference in the number of hospital days in patients across the four for-profit and the one non-profit chain.
Generally, our results suggest that financial incentives in the current reimbursement system inadequately reward efforts to reduce lengthy hospital stays, leading to potentially preventable differences in the number of hospital days between for-profit and non-profit providers. A pay-for-performance system in which payments to providers depend on downstream outcomes could strengthen the providers’ incentives to improve care or adopt business models that lower the number of hospital days per patient per year. For example, a facility’s composite payment rate could be supplemented by a bonus payment when it outperforms its expected hospitalization rates. The monthly capitation rate paid to physicians could also be similarly modified.
Certainly, any modification to the current payment system would require adequate case mix adjustment to prevent cherry picking by dialysis providers. The current formula for case mix adjustment depends only on age and body size. A more comprehensive adjustment might include selected co-morbid conditions with reasonably objective diagnostic criteria (e.g., diabetes). Audits may be needed as part of such a system in order to avoid “classification creep” [Pitches et al. 2003].
Previous studies have examined the relation between profit status and mortality in dialysis facilities [Garg et al. 1999], [Irvin 2000], [Port et al. 2000], [Devereaux et al. 2002], [Brooks et al. 2006], and among profit status, facility size and intermediate outcomes such as dialysis adequacy and control of anemia [Frankenfield 2000]. While some (Garg et al., Port et al. and Devereaux et al.) reported 8–20% higher mortality in for-profit facilities, Irvin found no differences. These studies were criticized on the basis that their findings could be explained by referral bias: sicker patients referred to facilities of higher perceived quality. [Brooks et al. 2006] provided the most comprehensive examination to date: using a more complete set of risk adjustors and an instrumental variable approach to adjust for selection bias, these authors identified no statistically significant differences in mortality across for-profit and non-profit providers. However, this could be due to the fact that instrumental variable methods may not have enough power to detect differences in mortality across groups [Greene 2002].
Our approach is similar to that in [Brooks et al. 2006], uses more recent data, and is based on a two stage regression method validated in [McClellan et al. 1994]. In contrast, we considered an alternative outcome – hospital days – that occurs more frequently than death and may be more modifiable. Using hospital days, the instrumental variable approach may be sensitive enough to detect significant differences across providers, whereas no difference was shown in mortality. A statistical test provided evidence that this approach could have partially corrected for referral bias, although the method is not fool proof: if unobservable risk factors are correlated with the instrument (i.e., travel distance to a dialysis facility) used to create the random patient cohorts, then the estimated effects may still be biased.
This study has several other important limitations. Claims data do not capture information on hospitalization for patients who have non-Medicare insurance, so the results we have observed may not be generalizable to patients with employer group health insurance or those below 65 years of age during the first three years of ESRD. Moreover, these results may not apply to hospital-affiliated dialysis facilities which were excluded from the analysis. Furthermore, as discussed earlier, hospital admissions and discharges are not only influenced by dialysis providers and referring nephrologists but also by other physicians – generalists and specialist – and by hospital processes. For example, if dialysis facilities were more likely to be located closer to for-profit hospitals, then the difference in hospital outcomes between for-profit and non-profit facilities could be due to the processes in for-profit hospitals. We were unable to adjust for differences in hospital characteristics (or other physician behavior) because claims data could not be linked to specific hospitals and physicians.
The results presented add to an established literature [Himmelstein et al. 1999], [Tu & Reschovsky 2002], [Rosenau & Linder 2003], [Schlesinger & Gray 2006] comparing outcomes among for-profit and non-profit health care organizations, including dialysis providers, hospitals, and HMOs. Unlike some previously published reports, we are disinclined to interpret our results as proof that for-profits are inherently inferior. Rather, we view it as evidence that for-profit dialysis organizations may be more responsive to market forces and may be more likely than their non-profit counterparts to take actions to improve outcomes where adequately rewarded for the cost of these actions.
Footnotes
Hospital based facilities cater mainly to in-patients, and hence deal with a much sicker population. The inclusion of hospital-based facilities (the majority of which are non-profit) would likely negatively bias the outcomes of non-profit facilities.
Hemodialysis patients need to travel to a dialysis facility for treatment three times a week. For patients with no facilities within 30 miles of their residence, the choice between a provider that is 33 miles away vs. another that is 36 miles away is not going to be driven by travel time considerations, unlike choosing between 1 mile and 4 miles. As such, travel distances would not be a good instrument for this group.
the 33rd and 66th percentiles of facility patient sizes were 35 and 72 respectively.
Since a patient has to travel to the clinic for treatment thrice weekly, it is reasonable to assume that he would only consider nearby facilities. This assumption speeds up computations.
A patient’s distance to a facility was calculated as the geodesic distance from the center of the patient’s residential zipcode to the center of the zipcode where the facility resides.
Networks 2 (New York) and 3 (New Jersey, Puerto Rico and Virgin Islands) were combined and Network 6 was split into two subregions: Georgia and the Carolinas.
Networks 2 (New York) and 3 (New Jersey, Puerto Rico and Virgin Islands) were combined and Network 6 was split into two subregions: Georgia and the Carolinas.
For each patient, we ordered the travel distances in ascending order and used the rank of the chosen facility as the “relative” distance.
Recall that positive skew = mass of the distribution concentrated at lower values.
References
- 1.Brooks JM, Irwin CP, Hunsicker LG, Flanigan MJ, Chrischilles EA, Pendergast JF. Effect of Dialysis Center Profit-Status on Patient Survival: A Comparison of Risk-Adjustment and Instrumental Variable Approaches. Health Services Research. 2006;41(6):2267–2289. doi: 10.1111/j.1475-6773.2006.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CMS ESRD Provider Public Use File:cms.hhs.gov/ESRDGeneralInformation/02_data.asp?#TopOfPage
- 3.Devereaux PJ, Schünemann HJ, Ravindran N, et al. Comparison of mortality between private for profit and private not-for profit hemodialysis centers: a systematic review and meta-analysis. JAMA. 2002;288:2449–57. doi: 10.1001/jama.288.19.2449. [DOI] [PubMed] [Google Scholar]
- 4.Dialysis Facility Compare: medicare.gov/Dialysis/Static/AboutQualityMeasures.asp
- 5.End Stage Renal Disease Networks. www.esrdnetworks.org.
- 6.Frankenfield DL, et al. Impact of facility size and profit status on intermediate outcomes in chronic dialysis patients. Am J Kidney Diseases. 2000;36:318–26. doi: 10.1053/ajkd.2000.8981. [DOI] [PubMed] [Google Scholar]
- 7.Garg PP, Frick KD, Diener-West M, Powe NR. Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med. 1999;341:1653–60. doi: 10.1056/NEJM199911253412205. [DOI] [PubMed] [Google Scholar]
- 8.Greene WH. Econometric Analysis. Prentice Hall; 2002. [Google Scholar]
- 9.HCRIS Renal Facility Cost Report:cms.hhs.gov/costreports/04_renalfacility.asp
- 10.Herfindahl O. PhD dissertation. Columbia University; New York: 1950. Concentration in the US Steel Industry. [Google Scholar]
- 11.Himmelstein DU, et al. Quality of Care in Investor-Owned vs Not-for-Profit HMOs. JAMA. 1999;281:159–163. doi: 10.1001/jama.282.2.159. [DOI] [PubMed] [Google Scholar]
- 12.Hirschman A. National Power and the Structure of Foreign Trade. University of California Press; Berkeley: 1945. [Google Scholar]
- 13.Horwitz JR. Does Nonprofit Ownership Matter? Yale Journal on Regulation. 2007;24:139–204. [Google Scholar]
- 14.Irvin RA. Quality of care differences by ownership in United States renal dialysis facilities. ASAIO J. 2000;46:775–778. doi: 10.1097/00002480-200011000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Kessler DP, McClellan MB. Is hospital competition socially wasteful? Q J Econ. 2000;115:577–615. [Google Scholar]
- 16.McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994;272:859–66. [PubMed] [Google Scholar]
- 17.McFadden D. Conditional Logit Analysis of Qualitative Choice Behavior. In: Zarembka P, editor. Frontiers in Econometrics. New York: Academic; 1973. [Google Scholar]
- 18.Pitches D, Burl A, Fry-Smith A. How to make a silk purse from a sow’s ear – a comprehensive review of strategies to optimize data for corrupt managers and incompetent clinicians. British Medical Journal. 2003;327:1436–9. doi: 10.1136/bmj.327.7429.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Port FK, Wolfe RA, Held PJ. Ownership of dialysis facilities and patients’ survival. N Engl J Med. 2000;342:1053–6. doi: 10.1056/NEJM200004063421415. [DOI] [PubMed] [Google Scholar]
- 20.Rosenau PV, Linder SH. Two Decades of Research Comparing For-Profit and Nonprofit Health Provider Performance in the United States. Social Science Quarterly. 2003;84:219–241. [Google Scholar]
- 21.Schlesinger M, Gray BH. How Nonprofits Matter In American Medicine, And What To Do About It. Health Affairs. 2006;25(4):W287–W303. doi: 10.1377/hlthaff.25.w287. [DOI] [PubMed] [Google Scholar]
- 22.Stock JH, Watson MW. Introduction to Econometrics. Addison Wesley; 2006. [Google Scholar]
- 23.Thamer M, Zhang Y, Kaufman J, et al. Dialysis Facility Ownership and Epoetin Dosing in Patients Receiving Hemodialysis. JAMA. 2007;297:1667–74. doi: 10.1001/jama.297.15.1667. [DOI] [PubMed] [Google Scholar]
- 24.Tu HT, Reschovsky JD. Assessments of Medical Care by Enrollees in For-Profit and Nonprofit Health Maintenance Organizations. N Engl J Med. 2002;346:1288–93. doi: 10.1056/NEJMsa011250. [DOI] [PubMed] [Google Scholar]
- 25. [Accessed online December 29, 2008.];United States Renal Data System. www.usrds.org.