Abstract
Background
Globally, respiratory infections are the primary cause of illness in developing countries, specifically among children; however, an etiological agent for many of these illnesses is rarely identified.
Objectives
Our study aimed to estimate the frequency of human bocavirus (HBoV) infection among pediatric populations in Argentina, Nicaragua and Peru.
Methods
We conducted a cross-sectional study using stored samples of an influenza-like illness surveillance program. Irrespective of previous diagnosis, nasopharyngeal or nasal swab specimens were randomly selected and tested using real-time PCR from three sites during 2007 from patients younger than 6 years old.
Results
A total of 568 specimens from Argentina (185), Nicaragua (192) and Peru (191) were tested. The prevalence of HBoV was 10·8% (95% CI: 6·3; 15·3) in Argentina, 33·3% in Nicaragua (95% CI: 26·6; 40·1) and 25·1% in Peru (95% CI: 18·9; 31·3).
Conclusions
These findings demonstrate circulation of HBoV in Argentina, Nicaragua and Peru among children with influenza-like symptoms enrolled in a sentinel surveillance program.
Keywords: Epidemiology, human bocavirus, respiratory illness
Introduction
Globally, respiratory infections are one of the primary causes of illness in developing countries, specifically among children younger than 5 years old. However, the etiology of these acute respiratory infections diagnosed as pneumonia is determined in only 75% of the cases.1 Of these identified respiratory pathogens, typically determined with molecular techniques, viruses account for approximately 15% of the infections.2 Nonetheless, by employing molecular diagnostic techniques in hospital-based studies, one can typically identify up to 90% of the viral agents associated with respiratory tract infections.3
Human bocavirus (HBoV) was originally described by Allander et al.4 among children with respiratory tract infection in Sweden, 2005. Since then, it has been reported in different countries3,5–7 and in patients of differing ages, although the majority of the infections have been detected in young children.5,6
Although our understanding of the epidemiology and genetic characteristics of this novel virus has been enhanced with the increasing information, we are still unable to discern the role of this virus in respiratory infections.8–10 Longtin et al. and Garcia-Garcia et al. have also identified the virus among asymptomatic children.11 The virus has also been identified in fecal samples of Spanish and Brazilian children with diarrheal symptoms.12 Additionally, it is not uncommon to find the virus in co-infection with other known pathogens. Given these inconclusive and confusing findings, the scientific community remains divided as to whether HBoV is a true respiratory pathogen.
Since 2006, the US Naval Medical Research Center Detachment (NMRCD) in Peru has conducted passive influenza-like illness (ILI) surveillance for numerous pathogens in Peru13 and other Central and South American Countries. The ILI sentinel surveillance program enrolls all patients who approach the participating health services with oral temperature of 38°C or higher and sore throat or cough lasting <5 days. Under the regular ILI surveillance program, the specimens are tested for evidence of influenza A and B, adenovirus, parainfluenza 1–3, herpesvirus and respiratory syncytial virus (RSV) infection.
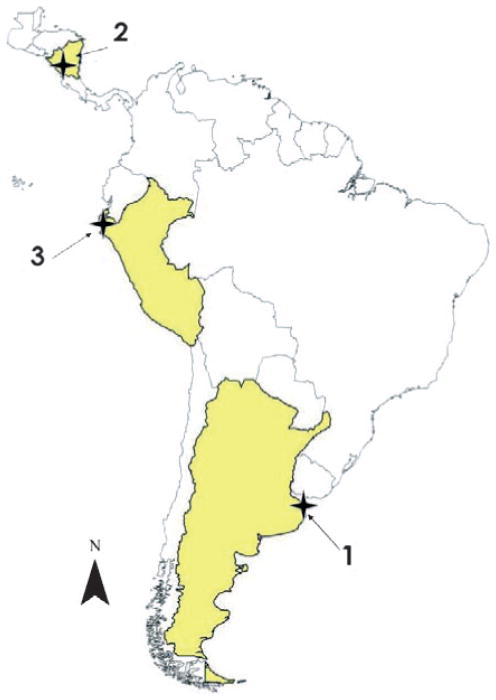
In this framework, our study aimed to identify the frequency of HBoV infection among a pediatric subset of stored samples of the ILI-enrolled population under surveillance from Argentina, Nicaragua and Peru (1, 2, 3, respectively, see Figure 1).
Figure 1.
Study sites.
Materials and methods
We randomly selected a total of 568 stored nasopharyngeal swabs or nasal washes collected in 2007 from children younger than 6 years old who suffered fever and cough or sore throat in three study sites from the program. The facilities included in the study were three city hospitals in Buenos Aires, Argentina, in Managua and Masaya, Nicaragua; and one primary healthcare center in Managua, Nicaragua and four in Piura, Peru: 1) Hospital Infantil from Buenos Aires, Argentina; 2) Hospital Departamental Humberto Alvarado from Masaya, Hospital Infantil Manuel Jesus Rivera “La Mascota” and Centro de Salud Villa Venezuela from Managua, Nicaragua; and 3) Centro de Salud Chiclayito, Bellavista, Pachitea and Centro Medico Militar, Piura, Peru (Figure 1).
All samples tested for HBoV were assessed using real-time PCR as described by Lu et al.14 The DNA was extracted and eluted from 200 μl of transport media using QIAmp DNA blood Mini kit (Qiagen, Valencia, CA, USA). The samples were tested for NS1 and NP1 genes (Table 1) by real-time PCR using the TaqMan® Universal PCR Master Mix Reagent kit (Applied Biosystems, Foster City, CA, USA). The PCR was carried out in a volume of 20 μl of master mix and 5 μl of sample. The thermocycling conditions were as follows: 95°C for 3 minutes, followed by 45 cycles of 95°C for 15 seconds and 60°C for 1 minute. Amplification was performed on an ABI 7500 real-time PCR system (Applied Biosystems). Sequencing was conducted on any positive real-time PCR samples.
Table 1.
Primers and probes used to detect human bocavirus
| Primer / probe | Sequence (5′–3′) | Gene |
|---|---|---|
| NS1-F | TGC AGA CAA CGC YTA GTT GTT T | NS-1 |
| NS1-R | CTG TCC CGC CCA AGA TAC A | NS-1 |
| NS1 | P 6FAM-CCA GGA TTG GGT GGA ACC TGC AAA-BHQ | NS-1 |
| NP1-F | AGA GGC TCG GGC TCA TAT CA | NP-1 |
| NP1-R | CAC TTG GTC TGA GGT CTT CGA A | NP-1 |
| NP1 | P VIC-AGG AAC ACC CAA TCA RCC ACC TAT CGT CT-BHQ | NP-1 |
HBoV infection was determined from stored samples from each site, and 95% confidence intervals were estimated with the binomial exact test. An exploratory analysis was performed to determine the differences in distribution of HBoV infection, by country and within country, by age or gender, using a t-test for equal variance and a chi-square test. The presence of co-infections was assessed with cross-tabulations. All analyses were performed with Stata / SE 10.1, StataCorp LP, College Station, TX, USA.
Results
Study population
A total of 568 nasopharyngeal swabs were tested. Of these, 185, 192 and 191 individuals from Argentina, Nicaragua and Peru, respectively, met the inclusion criteria. All individuals were children with a median age of 1 year (range: 0–5 years). All sites had the same median age; however, mean ages were 1·21 years in Nicaragua (SD: 1·40), 1·75 years in Argentina (SD: 1·45) and 1·79 years in Peru (SD: 1·50). Forty-five percent of all participants were girls. A slight predominance in male participants was observed in each of the sites: 52·4% Argentina, 58·8% Nicaragua and 53·4% Peru, although this finding was not statistically significant.
HBoV prevalence
The prevalence of HBoV for the entire study population was 23·2% (95% CI: 19·7; 26·7) (n = 132). The site in Argentina showed a lower prevalence of HBoV infection when compared to Peru or Nicaragua (both P < 0·001, using Fisher’s exact test). The estimated prevalence for each site and binomial exact confidence intervals are presented in Table 2. HBoV was detected in 132 / 568 (23·2%) specimens, 34% (45 / 132) of which were co-infected with another respiratory virus.
Table 2.
Prevalence of human bocavirus in study population by country
| Country | Sample size | Positive samples | Prevalence | 95% CI |
|---|---|---|---|---|
| Argentina | 185 | 20 | 10·8 | 6·3; 15·3 |
| Nicaragua | 192 | 64 | 33·3 | 26·6; 40·1 |
| Peru | 191 | 48 | 25·1 | 18·9; 31·3 |
| Total | 568 | 132 |
The t-test for equal variance to assess the age distribution between children positive or negative for HBoV infection (variance ratio test: P = 0·517) showed no age effect (P = 0·056), and we obtained the same outcome when examining the age distribution within each of the countries.
Sixty-one percent of the children who tested positive for HBoV were boys, but the gender distribution across sites was not significantly different (P = 0·110).
Discussion
This study, performed in a population of participants in a respiratory surveillance program in three different geographical sites in Latin America, presents evidence of the circulation of HBoV in Argentina, Nicaragua and Peru. The virus had previously been reported to circulate in Brazilian children.5,14,15 The prevalence reported in the original study from Allander et al. was 3·5% in hospitalized patients in Sweden. Additional studies, mostly among hospitalized children and infants with respiratory infections, have identified prevalence proportions ranging from 1·5% to 19% in different regions.11,16,17 The different values reported from these studies may be because of sampling techniques, study populations and the sensitivity of the diagnostic assay.18 The prevalence of infection detected in our study in Argentina is consistent with these findings. However, the prevalence rates that we identified in Nicaragua and Peru are higher than have been previously reported for this virus. The reason why these two sites have higher prevalence rates may be related to the circulation of the virus in these areas caused by appropriate environmental conditions (susceptible population, climate, geography, migration, etc.) that may also favor persistent infection as has been reported in other studies.19 Despite the difference in prevalence rates among the three sites, the age and gender distribution of our samples are similar and comparable to other studies with a peak in HBoV infection in children 1 year of age and a slight increase in detection among boys. In our study, as in previous studies, HBoV has been identified as a co-infecting agent in a high proportion (ranging from 9·5% to 83·0%) of respiratory illnesses.4,6,20–23
The role of HBoV as a pathogen remains unclear.8,9 In our study, we detected HBoV as the most common viral agent, i.e. 23·2% of the total samples tested. However, we were unable to detect an agent in 49·0% of the samples, and we did not test for some known respiratory viruses, such as human rhinovirus, coronavirus or for bacterial agents. Previous studies have shown that upper respiratory infections among children may be caused by a variety of viral agents and very frequently occur as co-infections24,25, and this may be the case for these HBoV-positive samples. Furthermore, additional studies have detected HBoV in fecal samples of patients with both respiratory and gastrointestinal symptoms12,26,27, and in Brazil, there was evidence of infection in children with only symptoms of gastrointestinal distress, no respiratory symptoms.14 This may suggest an alternative transmission route for the virus and its pathogenic role in the gastrointestinal tract. However, a recent study by Garcia-Garcia et al.28 demonstrated that HBoV infection among hospitalized children with respiratory symptoms was more frequent than in healthy ones.
Future studies should include testing for evidence of HBoV within populations from additional surveillance sites from a variety of locations globally, evaluating the severity of HBoV cases, and assessment of non-respiratory patients (healthy individuals) to help better define this virus as a potential pathogen.
Conclusions
These findings demonstrate circulation of HBoV in Argentina, Nicaragua and Peru. The age and gender distribution is similar to what has been reported previously. HBoV was found in 23% of the samples collected from children with respiratory symptoms, which is somewhat higher to what has been reported previously. As in previous studies, HBoV was found mainly as a co-infecting agent in our samples, making it difficult to determine whether it is a pathogenic virus, exacerbates the symptoms of other viral infections22, or is merely a persistent non-pathogenic (commensal) virus.19 Routine testing for HBoV among patients with respiratory symptoms should be included in the testing strategy among any respiratory illness surveillance system, as has been previously suggested.3
Addendum
G Salmon-Mulanovich, JM Montgomery, Blazes DL Blazes, AG Lescano contributed to the concept and design of the study. G Salmon-Mulanovich, M Sovero analyzed and interpreted the data. VA Laguna-Torres, TJ Kochel, G Chauca, JM Montgomery, Blazes DL Blazes, AG Lescano revised the intellectual content of the manuscript. JF Sanchez, F Rodriguez, E Parrales, V Ocaña, M Barrantes revised and approved the version to be published.
Acknowledgments
This work was funded by DoD-GEIS and supported by work unit number 847705 82000 25GB B0016. The authors thank Dean Erdman and Melissa Wilby from the Gastroenteritis and Respiratory Virus Lab Branch, Centers for Disease Control and Prevention, Atlanta, GA, for providing the positive controls for these assays, and the students and faculty of the Maestría en Epidemiología Clínica con Mención en Métodos Cuantitativos from Universidad Peruana Cayetano Heredia (NIH / FIC TW007393-01) for their guidance and suggestions on the study design.
Footnotes
Disclaimer
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the US Government.
IRB statement
The Naval Medical Research Center Detachment Institutional Review Board determined the investigation (PJT.NMRCD.028) did not meet the definition of human subject research.
Copyright statement
The authors are military service members and employees of the US Government. This work was prepared as part of their official duties. Title 17 USC §105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 USC §101 defines US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Meetings
The majority these findings were presented as a poster at the 25th Annual Clinical Virology Symposium, in Daytona Beach, Florida 19–22nd April, 2009.
Conflict of interest
The authors declare no conflict of interest or significant financial interest TO DISCLOSE related to the entity funding the project or any other institution involved with the investigation.
References
- 1.Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86:408–416. doi: 10.2471/BLT.07.048769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott JA, Brooks WA, Peiris JS, Holtzman D, Mulhollan EK. Pneumonia research to reduce childhood mortality in the developing world. J Clin Invest. 2008;118:1291–1300. doi: 10.1172/JCI33947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arden KE, McErlean P, Nissen MD, Sloots TP, Mackay IM. Frequent detection of human rhinoviruses, paramyxoviruses, coronaviruses, and bocavirus during acute respiratory tract infections. J Med Virol. 2006;78:1232–1240. doi: 10.1002/jmv.20689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allander T, Tammi MT, Eriksson M, Bjerkner A, Tiveljung-Lindell A, Andersson B. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc Natl Acad Sci U S A. 2005;102:12891–12896. doi: 10.1073/pnas.0504666102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albuquerque MC, Pena GP, Varella RB, Gallucci G, Erdman D, Santos N. Novel respiratory virus infections in children, Brazil. Emerg Infect Dis. 2009;15:806–808. doi: 10.3201/eid1505.081603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi EH, Lee HJ, Kim SJ, et al. The association of newly identified respiratory viruses with lower respiratory tract infections in Korean children, 2000–2005. Clin Infect Dis. 2006;43:585–592. doi: 10.1086/506350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sloots TP, McErlean P, Speicher DJ, Arden KE, Nissen MD, Mackay IM. Evidence of human coronavirus HKU1 and human bocavirus in Australian children. J Clin Virol. 2006;35:99–102. doi: 10.1016/j.jcv.2005.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson LJ. Human bocavirus: a new viral pathogen. Clin Infect Dis. 2007;44:911–912. doi: 10.1086/512438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackay IM. Human bocavirus: multisystem detection raises questions about infection. J Infect Dis. 2007;196:968–970. doi: 10.1086/521311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sloots TP, Whiley DM, Lambert SB, Nissen MD. Emerging respiratory agents: New viruses for old diseases? J Clin Virol. 2008;42:233– 243. doi: 10.1016/j.jcv.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longtin J, Bastien M, Gilca R, et al. Human bocavirus infections in hospitalized children and adults. Emerg Infect Dis. 2008;14:217– 221. doi: 10.3201/eid1402.070851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vicente D, Cilla G, Montes M, Pérez-Yarza EG, Pérez-Trallero E. Human bocavirus, a respiratory and enteric virus. Emerg Infect Dis. 2007;13:636–637. doi: 10.3201/eid1304.061501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laguna-Torres VA, Gómez J, Ocaña V, et al. Influenza-Like Illness Sentinel Surveillance in Peru. PLoS ONE. 2009;4:e6118. doi: 10.1371/journal.pone.0006118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu X, Chittaganpitch M, Olsen SJ, et al. Real-time PCR assays for detection of bocavirus in human specimens. J Clin Microbiol. 2006;44:3231–1. doi: 10.1128/JCM.00889-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Souza EL, Ramos JG, Proenca-Modena JL, et al. Human bocavirus in very young infants hospitalized with acute respiratory infection in northeast Brazil. J Trop Pediatr. 2009;56:125–127. doi: 10.1093/tropej/fmp026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bastien N, Brandt K, Dust K, Ward D, Li Y. Human bocavirus infection, Canada. Emerg Infect Dis. 2006;12:848. doi: 10.3201/eid1205.051424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bastien N, Chui N, Robinson JL, et al. Detection of human bocavirus in Canadian children in a 1-year study. J Clin Microbiol. 2007;45:610–613. doi: 10.1128/JCM.01044-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allander T. Human bocavirus. J Clin Virol. 2008;41:29–33. doi: 10.1016/j.jcv.2007.10.026. [DOI] [PubMed] [Google Scholar]
- 19.Blessing KMD, Neske FDB, Herre UMD, Kreth H-WMD, Weissbrich BMD. Prolonged detection of human bocavirus DNA in nasopharyngeal aspirates of children with respiratory tract disease. Pediatr Infect Dis J. 2009;28:1018–1019. doi: 10.1097/INF.0b013e3181a854ae. [DOI] [PubMed] [Google Scholar]
- 20.Qu X, Duan ZJ, Qi ZY, et al. Human bocavirus infection, People’s Republic of China. Emerg Infect Dis. 2007;13:165. doi: 10.3201/eid1301.060824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monteny M, Niesters HG, Moll HA, Berger MY. Human bocavirus in febrile children, The Netherlands. Emerg Infect Dis. 2007;13:180– 182. doi: 10.3201/eid1301.060819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allander T, Jartti T, Gupta S, et al. Human bocavirus and acute wheezing in children. Clin Infect Dis. 2007;44:904–910. doi: 10.1086/512196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fry AM, Lu X, Chittaganpitch M, et al. Human bocavirus: a novel parvovirus epidemiologically associated with pneumonia requiring hospitalization in Thailand. J Infect Dis. 2007;195:1038–1045. doi: 10.1086/512163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruohola A, Waris M, Allander T, Ziegler T, Heikkinen T, Ruuskanen O. Viral etiology of common cold in children, Finland. Emerg Infect Dis. 2009;15:344. doi: 10.3201/eid1502.081468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jartti T, Lee WM, Pappas T, Evans M, Lemanske RF, Jr, Gern JE. Serial viral infections in infants with recurrent respiratory illnesses. Eur Respir J. 2008;32:314–320. doi: 10.1183/09031936.00161907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lau SKP, Yip CCY, Que T, et al. Clinical and molecular epidemiology of human bocavirus in respiratory and fecal samples from children in Hong Kong. J Infect Dis. 2007;196:986–993. doi: 10.1086/521310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JI, Chung JY, Han TH, Song MO, Hwang ES. Detection of human bocavirus in children hospitalized because of acute gastroenteritis. J Infect Dis. 2007;196:994–997. doi: 10.1086/521366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.García-García ML, Calvo C, Pozo F, et al. Human bocavirus detection in nasopharyngeal aspirates of children without clinical symptoms of respiratory infection. Pediatr Infect Dis J. 2008;27:358. doi: 10.1097/INF.0b013e3181626d2a. [DOI] [PubMed] [Google Scholar]