Abstract
Objective
Mitochondrial morphology and function are altered in intestinal epithelia during endotoxemia. However, it is unclear whether mitochondrial abnormalities occur in lung epithelial cells during acute sepsis or whether mitochondrial dysfunction corresponds with altered epithelial barrier function. Thus, we hypothesized that the intestinal epithelium is more susceptible to mitochondrial injury than the lung epithelium during acute sepsis and that mitochondrial dysfunction precedes impaired barrier function.
Methods
Using a resuscitated, feline model of Escherichia coli-induced sepsis, lung and ileal tissues were harvested after 6 hours for histological and mitochondrial ultrastructural analyses in septic (n=6) and time-matched Controls (n=6). HLEC and Caco-2 monolayers (n=5) were exposed to “cytomix” (TNFα: 40 ng/ml, IL-1β: 20 ng/ml, IFNγ: 10 ng/ml) for 24-72 hours, and measurements of transepithelial electrical resistance, epithelial permeability, and mitochondrial membrane potential (ΔΨ) were performed.
Results
Lung epithelial morphology, mitochondrial ultrastructure and pulmonary gas exchange were unaltered in septic animals compared to matching Controls. While histologically intact, ileal epithelia demonstrated marked mitochondrial ultrastructural damage during sepsis. Caco-2 monolayers treated with cytomix showed a significant decrease in mitochondrial ΔΨ within 24 hours, which associated with a progressive reduction in transepithelial electrical resistance and increased epithelial permeability over the subsequent 48 hours. In contrast, mitochondrial ΔΨ and epithelial barrier function were preserved in HLEC following cytomix.
Conclusions
These findings indicate that intestinal epithelium is more susceptible to mitochondrial damage and dysfunction than the lung epithelium in the context of sepsis. Early alterations in mitochondrial function portend subsequent epithelial barrier dysfunction.
Keywords: Acute lung injury, Feline, Mitochondria, Multiple organ failure, Sepsis syndrome
Introduction
Progressive organ dysfunction in the context of critical illness, also know as multiple organ dysfunction syndrome (MODS), most commonly caused by severe infections (sepsis), is the leading cause of mortality in critical care units (45, 48). A growing body of data indicates that altered cell metabolism, particularly mitochondrial, contributes to cell and organ dysfunction. The intestinal epithelium is particularly susceptible to mitochondrial damage (17, 23) and impaired barrier function (19) in the context of severe sepsis; however, little is know about the status of mitochondria in lung epithelium under these conditions. Furthermore, it is unclear whether lung epithelium fundamentally differs from intestinal epithelium in terms of susceptibility to the cytopathic events that characterize severe sepsis, and the functional consequences thereof. In this regard, recent studies indicate that the barrier function of epithelial cells is sensitive to alterations in their bioenergetic status (46, 56).
Based upon human studies showing that intestinal epithelial cells undergo accelerated rates of programmed cell death during sepsis (11), we hypothesized that the intestinal epithelium is more susceptible to mitochondrial damage and dysfunction during severe acute bacterial sepsis than the lung epithelium, and that consequent disruption of epithelial cell metabolism results in altered epithelial barrier function. A large animal model was employed for these investigations as it offers certain advantages over the prototypical rodent sepsis models, especially in the context of acute lung injury. Rodent models of sepsis are limited by the inability to control for potentially confounding physiological variables such as shock, hypoxemia or acidosis, which are typically optimized in the human condition. In this regard, the intestinal epithelium is particularly sensitive to changes in systemic blood pressure and attendant ischemia-reperfusion injury (24). Other advantages of large animal models include the ability to accurately assess lung gas exchange (e.g., during mechanical ventilation) and greater conformity to human anatomy (51). An acute gram-negative bacteremia model was chosen as it induces consistent dose-dependent pathology, such as is found in human sepsis, including alterations of the coagulation cascade (44) and lung and intestinal injury (10, 54). In vitro analyses of lung and intestinal epithelium were performed in concert using a cocktail of pro-inflammatory cytokines (i.e., cytomix), which models the inflammatory milieu of sepsis and is known to alter the function of epithelial cells (9, 50).
The results of these investigations are interesting in that they show the intestinal epithelium to be more sensitive to ultrastructural damage, particularly mitochondrial, than the lung epithelium under conditions modeling acute severe sepsis. Furthermore, in vitro analyses indicate that loss of epithelial barrier function, as reflected by reduced transepithelial electrical resistance (TER) and increased permeability to small molecules, was preceded by a reduction in mitochondrial energy status, suggesting that mitochondrial performance could influence epithelial barrier function during acute inflammatory stress.
Materials and Methods
Animal Preparation
All experiments were approved by The Ohio State University Institutional Laboratory Animal Care and Use Committee, and all care and handling of the animals were in accord with National Institutes of Health guidelines. The experiments used an animal preparation that has been described previously (16, 17). Briefly, fasted, adult male cats were anesthetized with intramuscular ketamine hydrochloride (25 mg/kg) and intravenous sodium pentobarbital (10 mg/kg), intubated for mechanical ventilation and had a femoral artery and vein cannulated to enable continuous recording of systemic arterial pressure and arterial and venous blood sampling. Additional intravenous sodium pentobarbital (~1-5 mg/kg) was provided, as needed, to maintain a proper level of sedation throughout the experimental timecourse. A blood gas analyzer (ABL5; Radiometer America, Westlake, OH) and a cooximeter (OSM3; Radiometer America), specifically for feline blood, were used to assess ongoing blood gas and oxygenation status, enabling corrective measures as needed. Arterial pCO2 and pO2 were maintained within normal limits by adjusting the FIO2 and minute ventilation, as necessary. By administering intravenous bicarbonate, as required, arterial pH was normalized as well. Fluid loss was replenished with buffered isotonic saline (5–10 ml/kg/hr), and rectal temperature was monitored and maintained at 39°C.
Experimental Protocol
After a 30-minute stabilization period, baseline measurements were obtained, and animals were randomly assigned to receive either intravenous Escherichia coli [5.0 × 108 CFU/kg (in 20 ml), n = 6] or buffered isotonic saline vehicle (Control, n = 6). Bacterial E. coli, serotype O86a:K61, was obtained from the American Type Culture Collection (33985™; Manassas, VA), grown up and prepared as detailed previously (54). The chosen dose proved to be sublethal for the experimental time period involved, yet evidence of acute organ injury typical of severe sepsis was demonstrated in the ileum, liver and heart within 2-4 hours post-treatment consistent with that formerly described (15-17, 28). In keeping with the results of Schlag et al (39), a dose of 1 × 107 CFU/kg E. coli failed to induce acute organ damage (data not shown). Approximately half of the E. coli dose was administered as an intravenous bolus over one minute with the remaining half added to the intravenous drip and dispensed over the succeeding hour. Arterial pCO2 (35-40 mm Hg), pO2 (> 100 mm Hg) and pH (7.35-7.42), paO2 to FIO2 ratio (600 ± 50) and arterial pressure (> 90 mm Hg), along with the relative ileal HbO2 content and blood volume (see below), were kept within normal limits, as detailed elsewhere (16, 17). At 6 hours post-treatment, the experiments were terminated, and tissue samples were harvested for histological and mitochondrial ultrastructural assessment.
Evaluation of Ileal Oxygen Availability
Relative ileal HbO2 content and blood volume were measured at baseline and every 30 minutes thereafter using in vivo reflectance spectrophotometry as reported previously (16, 17). A diode-array UV-visible spectrophotometer (model 8452A; Hewlett Packard, Waldbronn, Germany) equipped with a remote reflectance fiberoptic probe (model RSA-HP-84F; Labsphere, North Sutton, NH) was employed. Relative HbO2 contents were expressed as a percentage of the maximal measurable range in each animal, established by making similar measurements with the animal breathing an FIO2 of 1.0 at baseline (most oxygenated condition) and by excising the complete ileal segment at the end of the experiment (i.e., no further blood flow) and making measurements until tissue oxygen extraction had ended (least oxygenated condition) (17). Relative changes in local tissue blood volume were expressed as a percentage of the same measurements made at baseline. At least 4 determinations of relative HbO2 content and blood volume were made at each time point by making measurements at randomly selected locations along the ileum.
Light and Electron Microscopy and Evaluation of Mitochondrial Injury in the Tissues
At 6 hours post-treatment, lung and ileal tissue samples (~0.5–2.0 mg) were excised and routinely processed for light and electron (Phillips CM-12 transmission electron microscope; Eindhoven, Holland) microscopy evaluation as discussed elsewhere (16, 17). For light microscopy, tissues were formalin-fixed for 72 hours, blocked in paraffin, cut at 4 μm, deparaffinized, and then stained with hematoxylin and eosin. For electron microscopy, tissues were diced and fixed using 4% paraformaldehyde, 2.5% glutaraldehyde, and 0.1 M sucrose in 0.1 M phosphate buffer (pH = 7.4). Specimens were then post-fixed in 1% osmium tetroxide, dehydrated, embedded in Spurr media, cut, mounted on copper grids and stained with 2% uranyl acetate and Reynolds lead citrate.
Feline Tumor Necrosis Factor α (TNFα) Measurement
Serum from Control and E. coli-treated animals was obtained at baseline and then again at 2, 4 and 6 hours post-treatment. TNFα measurements were made by ELISA utilizing a mouse monoclonal capture antibody (Clone Mo199; Boehringer Mannheim, Indianapolis, IN) and a rabbit polyclonal detection antibody to human TNFα. This assay is sensitive to TNFα concentrations ≥ 50 pg/ml and is highly specific for TNFα (1). Given that feline TNFα is known to have 90% homology with human TNFα, the ELISA specificity remains equally high for accurate quantification in feline serum samples as well.
Preparation of Epithelial Cell Cultures
Human lungs were collected with approval from The Ohio State University Institutional Review Board and with patient consent. Normal, healthy adult donor lungs (n = 5) were obtained via open lung biopsy, then primary human lung epithelial cells (HLEC) were isolated after enzymatic dissociation from the trachea, bronchi, and bronchioles, seeded onto collagen-coated, semi-permeable membranes (0.6 cm2, Millicell-HA; Millipore, Billerica, MA) and grown at an air–liquid interface, as formerly described (41, 55). HLEC cells were then cultured in a 50:50 mixture of Dulbecco's Modified Eagle media and Ham's F-12 media (D-MEM/F-12; Invitrogen Corp., Carlsbad, CA), supplemented with 2% Ultroser G (BioSepra; Villeneuve, La Garenne, France) and multiple antibiotics [penicillin (100 U/ml), streptomycin (100 μg/ml), gentamycin (50 μg/ml), fluoconazol (2 μg/ml) and amphotericin B (1.25 μg/ml)]. Similarly, Caco-2 cells were cultured in D-MEM with 20% fetal bovine serum (FBS) supplemented with penicillin (100 U/ml) and streptomycin (100 μg/ml). Forty-eight to 96 hours after seeding, the epithelial cells formed a confluent culture with electrically tight junctions and a transepithelial resistance > 800 Ω. The cells were then incubated with “cytomix” (TNFα: 40 ng/ml, IL-1β: 20 ng/ml and IFNγ: 10 ng/ml) (36) for 24-72 hours at 37°C in a 5% CO2 environment. HLEC cells isolated from individual donors were cultured, treated and examined separately; pooling of cells across donors was never employed.
Determination of Cell Monolayer Resistance and Permeability
HLEC and Caco-2 cell layers, being fed exclusively from the basolateral aspect, were monitored until they excluded medium to the apical side. Cytomix was added to the basolateral side and incubated for the designated time periods. Barrier function, as reflected by the electrical resistance across the epithelial cell layer (Rt), was measured using a portable ohmmeter (Millipore). Epithelial barrier integrity was further evaluated by Lucifer yellow (MW = 457) diffusion. At each time point, Lucifer yellow (Millipore) was added to the donor (apical) chambers (final concentration: 0.1 mg/ml) to monitor membrane integrity. 100 μl aliquots were taken from the acceptor (basolateral) chambers and analyzed in a fluorescent plate reader at excitation and emission wavelengths of 425 nm and 535 nm, respectively (Cytofluor II Fluorescence multi-well plate reader; PerSeptive Biosystems, Inc., Foster City, CA). A threshold value of ≥ 0.25%/hr of Lucifer yellow flux was used to denote barriers that were abnormally permeable.
Evaluation of Cellular Mitochondrial Membrane Potential
To assess relative changes in mitochondrial membrane potential (ΔΨ) following cytomix treatment, HLEC and Caco-2 cells were harvested at 24 hours post-treatment and washed with warm PBS. The cells were then re-suspended in 1 ml warm PBS at a concentration of 1 × 106 and incubated with 2 μM JC-1 (34) using the MitoProbe™ JC-1 Assay kit (Invitrogen) at 37°C, 5% CO2 for 20 minutes. Following a single wash with PBS, cells were re-suspended and analyzed by flow cytometry [Becton Dickinson FACS Calibur (BD, Inc.; Franklin Lakes, NJ)] using a 488 nm excitation wavelength with 519 nm (FITC-green) and 578 nm (PE-red) emission filters and photographed during fluorescence microscopy using a standard MF filter [Olympus BX40 (Olympus America, Inc.; Melville, NY)]. 50 μM carbonyl cyanide 3-chlorophenylhydrazone (CCCP), an uncoupler of oxidative phosphorylation, at 37°C for 5 minutes served as a positive control.
Assessment of Apoptotic Epithelial Cell Death
The presence of active caspase-3 was determined by the 7-amido-4-trifluoromethylcoumarin (AFC) assay using specific fluorosubstrates, as detailed previously (13). For all AFC preparations, 3 × 106 cells were pelleted, washed with a magnesium sulfate-containing phosphate buffer, and then lysed by multiple freeze-thaw cycles. Lysates were incubated with either DEVD-AFC [10% glycerol, 50 mM PIPES (pH 7.0), 1 mM EDTA, 1 mM DTT, and 20 μM DEVD-AFC (Enzyme Systems Products, Livermore, CA)] or YVAD-AFC [10% sucrose, 100 mM HEPES (pH 7.5), 0.1% CHAPS, 10 mM DTT, 20 μM YVAD-AFC (Enzyme Systems Products)]. The release of free AFC was determined using a Cytofluor 4000 fluorimeter (PerSeptive Biosystems, Inc., Framingham, MA) employing excitation and emission wavelengths of 400 nm and 505 nm, respectively.
Statistical Analysis
The data was derived from a minimum of 5 independent experiments and was expressed as mean ± SEM, and statistical significance was based upon a value of p ≤ 0.05. SigmaPlot 10.0 and SYSTAT 12.0 software were used to plot the data and carry out the statistical analyses, respectively. Comparisons of feline physiological parameters and TNFα levels were made using one-way analysis of variance (treatment) with repeated measures (time or replicates). Lung wet-to-dry ratios and the flow cytometry-derived red-green fluorescence intensity ratios were compared using the Student's t-test. Relative transepithelial electrical resistance, epithelial permeability and relative caspase-3 activity measurements were analyzed using 2-way ANOVA wherein the p-values of all pair-wise comparisons were obtained using the Tukey multiple comparison method.
Results
Physiological Parameters during the Experimental Protocol
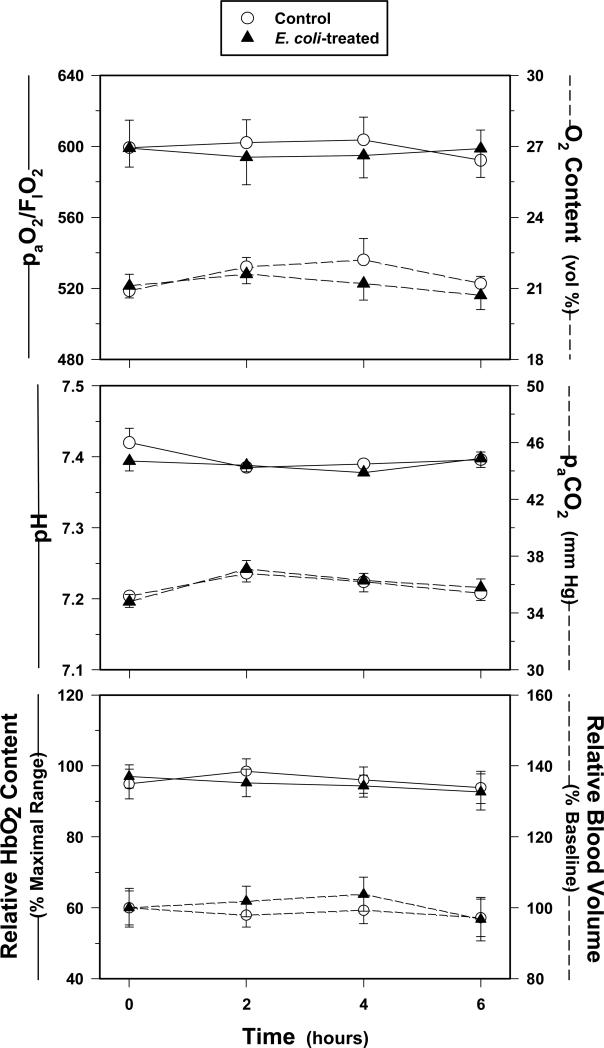
In accordance with the experimental protocol, resuscitation was provided to maintain hemodynamic parameters, temperature and blood gas variables within a pre-determined normal range. All physiological measurements remained relatively unchanged during the 6-hour time period and did not differ significantly between the two groups (Figure 1). Mean arterial pressure, paO2/FIO2 and ileal oxygenation status were relatively constant throughout the experiment and did not vary between E coli-treated and Control groups.
Figure 1.
(Top) paO2 to FIO2 ratio and arterial O2 content, (Middle) pH and paCO2, and (Bottom) relative ileal HbO2 content and blood volume of the E. coli-treated and Control groups as measured over time (values are mean ± SEM). All measurements were comparatively stable over the study period, indicating adequate resuscitation of the E. coli-treated animals and ample O2 availability in the ileal tissues throughout the 6-hour experiment.
Unlike our previously established LPS model (15-17, 28), only minor adjustments in minute ventilation, fluid resuscitation and bicarbonate administration were required through 6 hours post-treatment in this bacteremia model. Positive end-expiratory pressure was never required, and vasoactive agents were never employed. There was no significant difference in the positive inspiratory pressure used, the inspiratory FIO2 and ventilatory frequency required, and the volume of fluid resuscitation needed over time between the groups. However, this did not hold true for longer experimental timecourses. Evaluation much beyond 6 hours was not conducted based upon the increasing mortality rates and enhanced difficulty in maintaining vital function status, resulting primarily from vascular leak-induced systemic hypotension and concomitant bicarbonate loss leading to acidosis, which could not be resolved through the stated resuscitative methods employed.
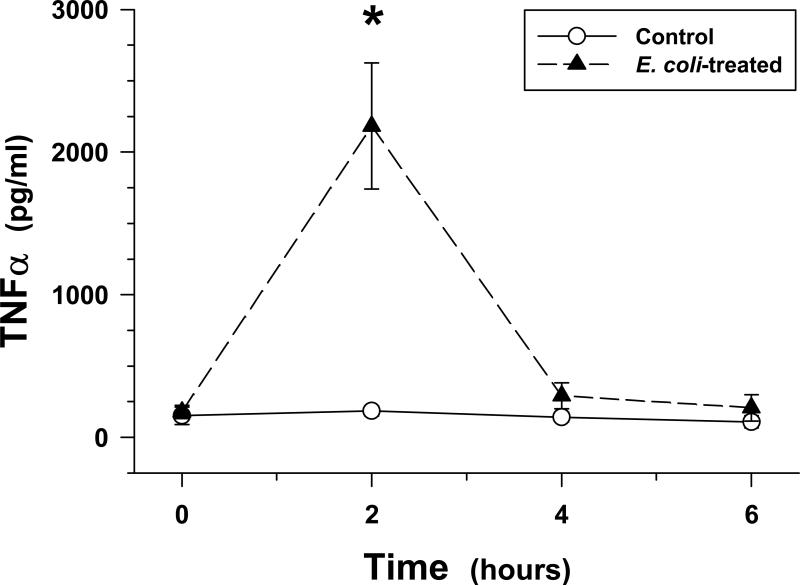
Arterial TNFα Concentrations
Baseline TNFα levels were < 200 pg/ml in the Controls and remained low throughout the 6-hour study period. As expected, TNFα levels increased significantly in the E. coli treatment group and peaked at 2 hours post-treatment before returning to baseline values by 6 hours (Figure 2).
Figure 2.
Arterial plasma TNFα levels as measured over time in the Control and E. coli-treated groups (values are mean ± SEM). E. coli infusion caused a significant increase in TNFα levels that peaked at ~2 hours post-treatment (*p < 0.01, relative to baseline and time-matched Control group).
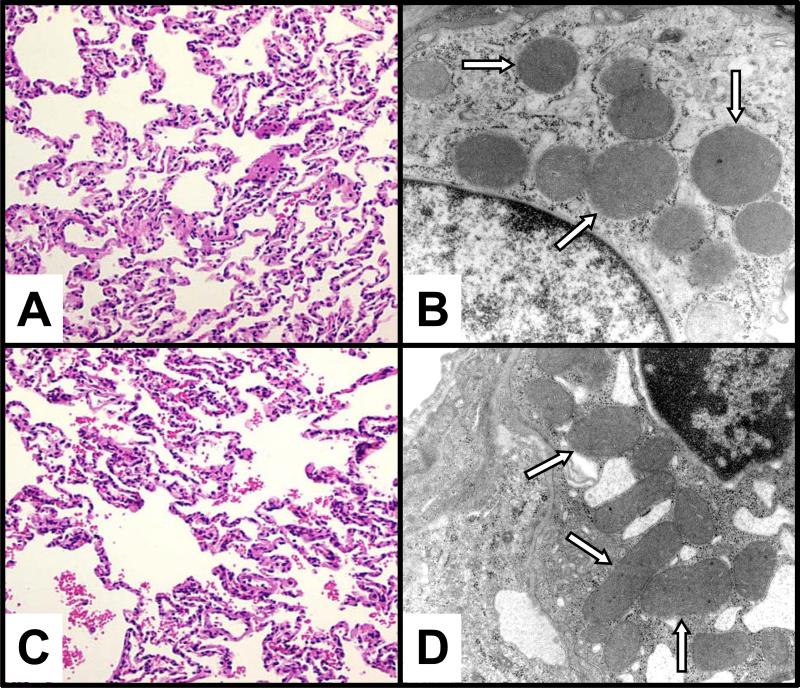
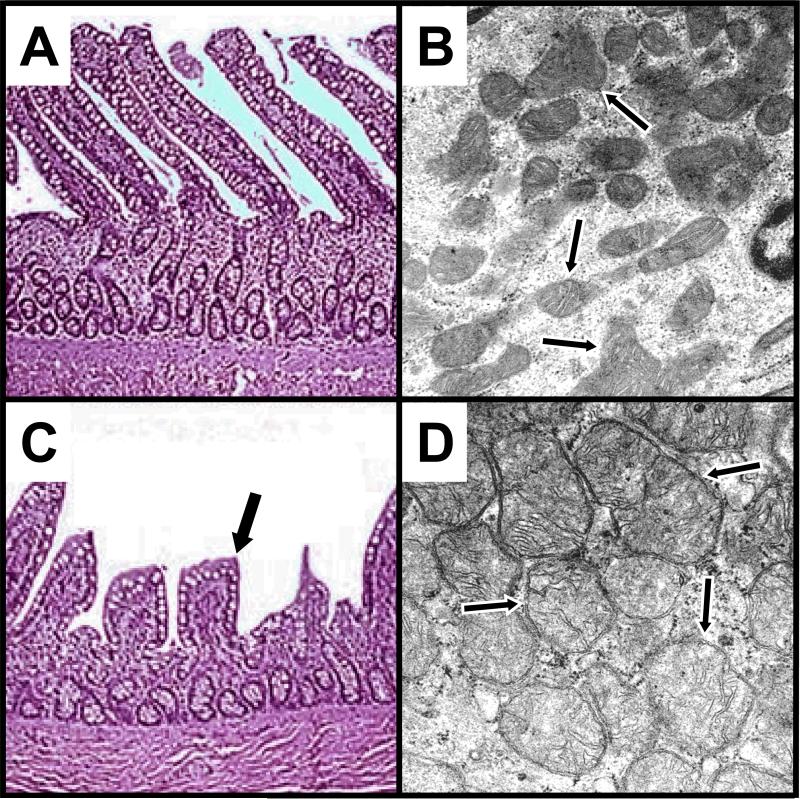
Microscopic Analyses of Feline Lung and Ileal Epithelia during Sepsis
Lung tissue samples harvested 6 hours post-treatment and processed for light microscopic analysis demonstrated an increased presence of septal neutrophilia following E. coli treatment (Figure 3, panels A and C). An average of 50 neutrophils per 100X visual field were observed in the lung tissues of the E. coli-treated group versus < 20 per 100X visual field in corresponding Control tissues. Otherwise, no other differences in the appearance of the lung epithelia were noted between the groups. Lung wet-to-dry ratios were 5.3 ± 0.1 for Controls and 6.2 ± 0.2 in the E. coli treated group (p < 0.05) reflecting mild lung edema. In addition, there were no significant ultrastructural alterations of the lung epithelium, including mitochondria that appeared unchanged following E. coli treatment (Figure 3, panels B and D). Histological analysis of the ileum was notable for retraction of intestinal villi in the E. coli-treated group; however, the mucosal layer remained essentially intact (Figure 4, panels A and C). Furthermore, ultrastructural analyses revealed high-amplitude mitochondrial swelling in the ileal epithelial cells of the E. coli-treated group relative to Controls (Figure 4, panels B and D).
Figure 3.
Representative light (LM) and electron (EM) photomicrographs, respectively, of Control (A and B) and E. coli-treated (C and D) feline lung tissue. No significant difference was observed in the histological appearance of the alveolar epithelium or the epithelial mitochondrial ultrastructure between the Control and E. coli-treated animals after 6 hours. In addition, the mitochondria (white arrows) appeared intact and did not show the typical features of cytopathic injury, namely swelling and loss of cristae. (LM - staining: hematoxylin and eosin; original magnification: 20X, EM - staining: uranyl acetate and lead citrate; original magnification: 20,000X).
Figure 4.
Representative light (LM) and electron (EM) photomicrographs, respectively, of Control (A and B) and E. coli-treated (C and D) feline ileal tissue. E. coli-treated specimens (C) demonstrated retraction (black arrow) and occasional loss of villi compared to matching Controls (A). In contrast to observations in the lungs, dramatic changes in mitochondrial morphology were evident in the ileum following E. coli treatment (D), evidenced by mitochondrial swelling with a loss of well-defined cristae (black arrows). (LM - staining: hematoxylin and eosin; original magnification: 20X, EM - staining: uranyl acetate and lead citrate; original magnification: 55,000X).
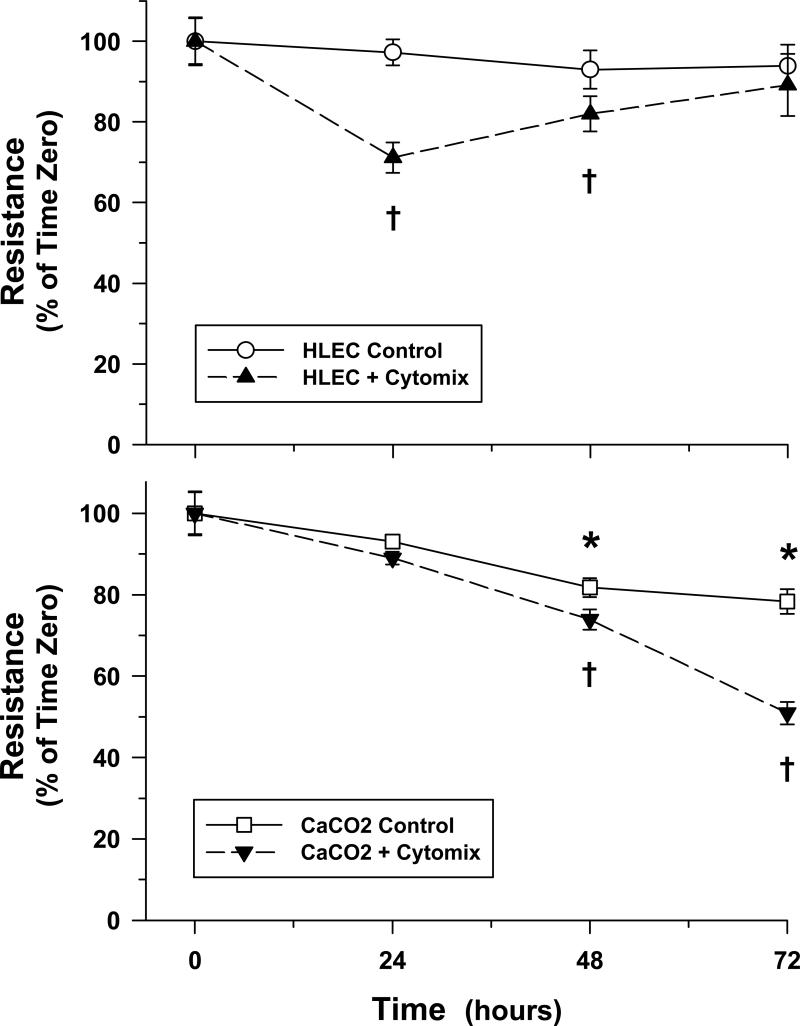
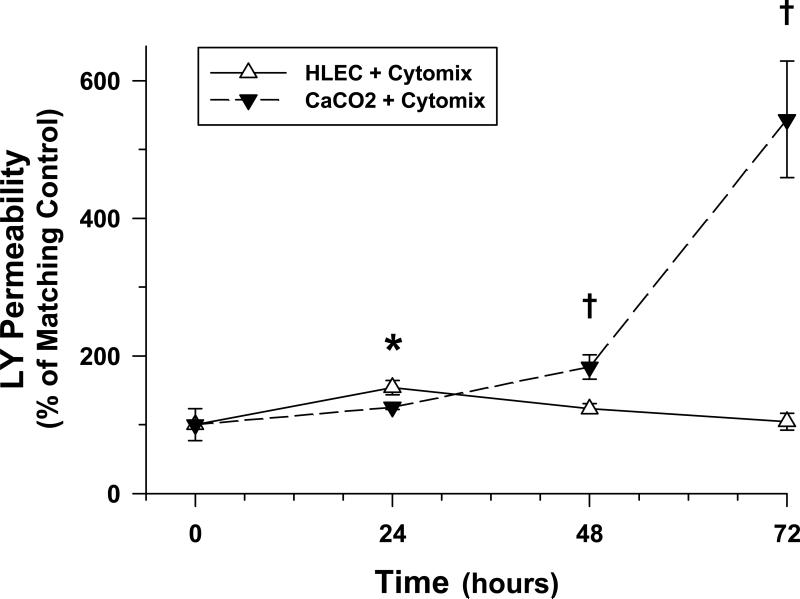
Transepithelial Electrical Resistance (TER) and Permeability Changes in Response to Putative Sepsis Mediators (Cytomix)
In vitro analyses were performed to detect changes in TER in both lung (HLEC) and intestinal (Caco-2) epithelial monolayers over time in response to cytomix. TER was significantly reduced in HLEC monolayers at 24 hours post-treatment relative to matched untreated Controls but gradually returned toward baseline conditions becoming fully restored after 72 hours (Figure 5). In contrast, Caco-2 monolayers demonstrated a progressive decline in TER over time becoming significant 48 hours after cytomix exposure (Figure 5), corresponding with an ever-increasing permeability to small molecules (Figure 6).
Figure 5.
Transepithelial electrical resistance (TER) of HLEC (Top) and Caco-2 (Bottom) monolayers exposed to control or cytomix-treated media as measured over time (values are mean ± SEM). Although a transitory drop in TER was observed in HLEC monolayers 24 hours after cytomix treatment, resistance returned towards control levels thereafter. Conversely, TER fell progressively over time in Caco-2 monolayers, particularly following cytomix treatment (*p < 0.05, compared to baseline; †p < 0.05, relative to baseline and corresponding time-matched Controls).
Figure 6.
Epithelial permeability to Lucifer yellow of cytomix-treated HLEC and Caco-2 monolayers over time (values are mean ± SEM). Following cytomix treatment, epithelial permeability was transiently elevated at 24 hours post-treatment in HLEC monolayers compared to matching Controls but normalized thereafter. By contrast, Caco-2 monolayers demonstrated a progressive increase in permeability beginning 48 hours after cytomix treatment relative to matching Controls (*p < 0.05, compared to baseline; †p < 0.05, relative to baseline and corresponding time-matched Caco-2 monolayers).
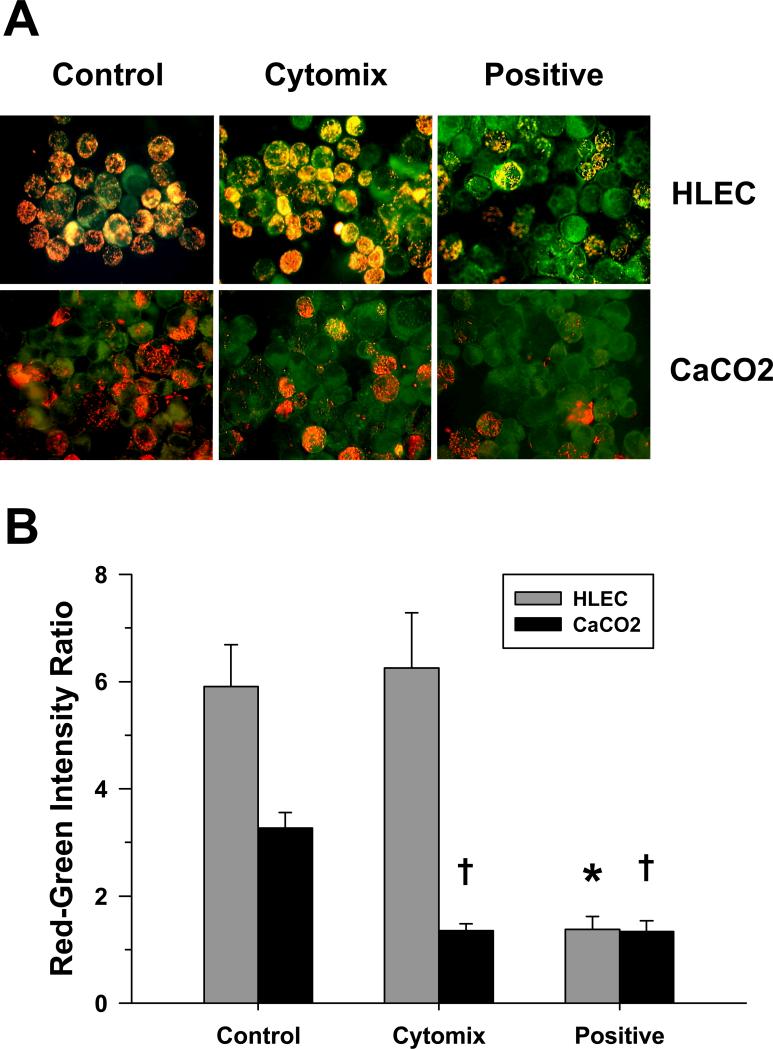
Mitochondrial Membrane Potential (ΔΨ) in HLEC and Caco-2 Epithelial Cells following Cytomix
Relative changes in mitochondrial ΔΨ, as reflected by the alterations in the red-green fluorescence intensity ratio following exposure to the membrane potential-sensitive dye, JC-1, were determined in HLEC and Caco-2 epithelial cells 24 hours after cytomix. No significant change in mitochondrial ΔΨ was observed in the lung epithelial cells. However, intestinal epithelial cell mitochondrial ΔΨ was dramatically diminished, consistent with a decreased red-green intensity ratio comparable to that induced by the positive control, CCCP (Figure 7).
Figure 7.
(A) Representative fluorescence photomicrographs of HLEC and Caco-2 cells exposed to the membrane potential-sensitive dye, JC-1, 24 hours after cytomix treatment or in time-matched Controls. Orange-red fluorescence is indicative of cells having a normal elevated mitochondrial membrane potential (ΔΨ). HLEC cells appeared unchanged following cytomix; whereas, Caco-2 cells fluoresced predominantly green, indicative of de-energization, and were comparable to CCCP-treated (positive) cells. (B) Red-green fluorescence intensity ratio following flow cytometry of HLEC and Caco-2 cells exposed to JC-1 24 hours post-treatment with cytomix or in time-matched Controls (values are mean ± SEM). Unlike the HLEC cells, Caco-2 cells demonstrated a significant decrease in the red-green ratio related to the loss of ΔΨ similar to that observed following CCCP treatment (*†p < 0.01, compared to matching Controls).
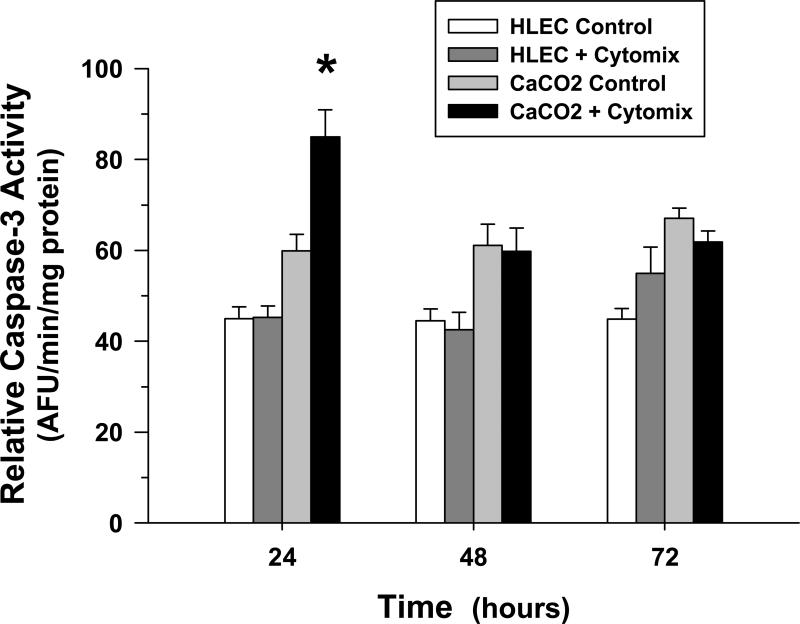
Apoptosis following Cytomix Treatment
Increased programmed cell death, as reflected by an elevated caspase-3 activity, was evaluated over time in the HLEC and Caco-2 epithelial cells following cytomix treatment. No significant change in relative caspase-3 activity following cytomix was observed in the lung epithelial cells within 72 hours post-treatment. However, enhanced apoptosis, indicated by an increased relative caspase-3 activity, was demonstrated in the intestinal epithelial cells 24 hours after cytomix treatment but was unchanged from matching untreated Controls thereafter (Figure 8).
Figure 8.
Relative caspase-3 activity in Control and cytomix-treated HLEC and Caco-2 cells over time (values are mean ± SEM). Although no change in activity was observed in the HLEC cells over time, a significant increase in activity was verified in the Caco-2 cells 24 hours after cytomix treatment (*p < 0.05, relative to matching Controls) but not at later timepoints.
Discussion
These investigations show for the first time that lung epithelium, compared to intestinal epithelium, is resistant to mitochondrial injury in the context of acute severe sepsis. The in vivo studies showed that intestinal epithelial injury, characterized by altered mitochondrial morphology, is an early occurrence during severe bacteremic sepsis; whereas, the lung epithelium is preserved (Figures 3 and 4). In keeping with preserved lung morphology, pulmonary gas exchange was unchanged during the acute phase of sepsis (Figure 1). However, it was unclear from the in vivo investigations whether the relative resistance of the lung epithelium to sepsis relates to intrinsic cellular properties or is dependent upon other variables, such as differences in regional blood flow, inflammatory cell activation or the absence of bacteria (which is present in the intestinal lumen).
The in vitro model provided for a more sustained exposure to putative sepsis mediators while controlling for potentially confounding environmental variables, such as ambient oxygen tension, cytokine concentrations, or regional bacterial populations. Under identical experimental conditions, cultured lung epithelial cells were shown to be more resistant to pro-inflammatory cytokine-mediated mitochondrial dysfunction compared to intestinal epithelial cells. Although mitochondrial damage can trigger cell death, changes in mitochondrial function (Figure 7) were not associated with significant cell death under our experimental conditions, as reflected in the relative caspase-3 activity (Figure 8), but did precede changes in barrier function, as indicated by the decreased TER (Figure 5) and increased permeability (Figure 6) to small molecules.
Certain organs are known to be highly susceptible to injury during critical illness. It has long been recognized that the intestinal epithelium is prone to damage during conditions modeling sepsis, even when controlling for blood flow (i.e., tissue oxygenation) (16, 17), and intestinal epithelial injury is believed to participate in the propagation of systemic inflammation by promoting the invasion of microorganisms or the translocation of bacterial products (19). Likewise, lung epithelial integrity is thought to influence susceptibility to infection (i.e., barrier function) (47) and alveolar fluid accumulation in the context of acute lung injury (5). In keeping with previous investigations performed in humans who had died from sepsis (24), this study demonstrated the ileum to be prone to acute damage; whereas, the lung was relatively resistant at least during the initial stage of sepsis. Moreover, the mitochondrial ultrastructural changes in the liver (not shown) and ileum (Figure 4), including high amplitude swelling and loss of mitochondrial cristae integrity, conform to those described previously in these tissues in humans (14, 52) and animals (15-17, 28) during severe sepsis or acute endotoxemia.
Although sepsis is a significant cause of acute lung injury, the lung epithelial barrier was shown to resist injury, at least in the acute phase of severe bacteremic sepsis. Our findings are consistent with previous studies which found lung epithelial cells to be resistant to pro-inflammatory mediators (e.g., TNFα, IFNγ), unless the cells are rendered susceptible to injury by other factors, such as zinc depletion (3) or alcohol exposure (8). This would explain why a minority of patients presenting with sepsis develop severe acute lung injury (ALI) (18, 33, 49); whereas, the risk of ALI increases when a second risk factor is present, such as alcoholism (31), zinc depletion (29) or ventilator-induced lung injury (2, 20). Presumably, there are a number of comorbid conditions contributing to sepsis-induced ALI in humans that are yet to be identified.
The incidence of intestinal epithelial damage and related changes in function during sepsis is difficult to determine since sensitive clinical diagnostic clinical tools are lacking. However, early post-mortem examination of septic humans demonstrated that the intestinal mucosa is particularly prone to cytopathic changes (5, 24). This conforms to the common association of sepsis with altered gut motility and absorption (27, 32, 35), and supports the notion that the gut is the “motor” of MODS, relating to epithelial damage, translocation of bacteria and bacterial products, and the perpetuation of innate immune responses (26, 43). Moreover, intestinal epithelial damage alters the capacity to provide nutrient support, thereby contributing to nutritional deficiencies in the setting of sepsis (27, 35). Thus, further investigations into the mechanisms of intestinal epithelial injury are warranted.
Changes in intestinal barrier function are preceded by changes in the mitochondrial energy state (electrochemical gradient) in vitro. JC-1 is a fluorescent cationic dye that is rapidly sequestered within energized mitochondria, forming red-fluorescing aggregates. In contrast, when the mitochondria become de-energized, JC-1 remains in the cytoplasm in a monomeric form which fluoresces green. Hence, the ratio of red to green fluorescence reflects the mitochondrial energization status (25). Using this sensitive approach, we observed that cytomix-treated gut epithelial cells exhibited mitochondrial de-energization within 24 hours; whereas, lung epithelial cells did not. Mitochondrial damage and dysfunction are well-documented in various tissues, including the intestinal epithelium, in various models of sepsis (5, 14, 17, 23, 52, 53). Mitochondrial mechanisms are believed to explain the high rate of intestinal epithelial apoptosis observed during sepsis (12) and are expected to result in reduced ATP-dependent functions, including the maintenance of tight junctions and ion transport (38). Mitochondrial de-energization corresponded with subsequent alterations in intestinal epithelial barrier function, as reflected by reduced TER and increased permeability, such as is observed when epithelial cells are exposed to metabolic toxins (38). The dramatic increase in permeability to small molecules and reduction in TER observed in the Caco-2 cells 72 hours after cytomix in the absence of significant ongoing cell death could be explained by the disruption of intercellular tight junctions.
Recent studies indicate that cellular bioenergetics strongly influences epithelial barrier functions, particularly with respect to tight junctions. Conditions favoring moderate levels of ATP depletion, such as sustained hypoxia or inhibition of glycolysis, are sufficient to promote altered intestinal epithelial permeability and disruption of tight junctions (46). Mechanistically, Zheng et al recently demonstrated that epithelial tight junction assembly and disassembly is tightly regulated by AMP-activated protein kinase (AMPK). More specifically, the activity of AMPK is modulated by the cellular ATP:AMP ratio with lower ratios favoring disassembly of tight junctions (56). Other possible mechanisms linking loss of epithelial barrier function to mitochondrial dysfunction includes impaired ATP-dependent pump functions (42) or increased mitochondrial oxidant production. With respect to the latter, oxidant stress is known to elicit remodeling of actin filaments leading to loss of barrier function (6), and epithelial mitochondria are shown to produce higher levels of oxidants in response to putative sepsis mediators (8). Although altered ATP flux was not specifically addressed in these studies, the observed alterations in ultrastructure (in vivo) and function (in vitro) of intestinal mitochondria, the primary and most efficient source of ATP (compared to glycolysis), would predispose to ATP depletion such as is documented in other tissues during sepsis (7).
Additional investigations are needed to determine why the intestinal epithelium is more prone to damage and dysfunction than the lung epithelium during sepsis/acute inflammation. Based upon the in vitro investigations wherein the concentrations of cytokines, oxygen tension and other variables were carefully controlled, it is evident that intestinal epithelial injury is not merely explained by regional differences in oxygen tension (e.g., blood flow), inflammatory cell infiltration or the proximity to bacteria, which are variables that must be considered in vivo. Possible explanations for the greater sensitivity of the intestinal epithelium to sepsis and putative sepsis mediators (e.g., cytomix) include differences in oxidant/anti-oxidant balance or enhanced sensitivity to the effects of pro-inflammatory mediators such as IFNγ (42) or TNFα (21).
There are several notable study limitations to be recognized. The large animal model, which requires continuous monitoring and resuscitation to normalize physiological variables, does not allow us to model subacute lung injury; however, this was not the goal of the in vivo investigations. We were primarily interested in determining whether the intestinal mucosa was more susceptible to injury than the lung epithelium in the context of “resuscitated” sepsis, wherein variables such as blood gases and pH, blood pressure, oxygenation and body temperature were optimized, as is the standard in clinical practice. The in vitro model (i.e., cytomix) does not exactly model conditions of sepsis but provides for reproducible exposure to the putative pro-inflammatory mediators of sepsis, which are known to contribute to cytopathic events. In particular, cytomix has been used extensively to model epithelial responses during acute inflammation (4, 22, 50). Another potential limitation relates to the comparison of primary lung epithelial cell (HLEC) responses to those of an immortalized human intestinal epithelium cell line (Caco-2). Cultured primary human lung epithelial cells optimally represent the intact human lung epithelium. In lieu of primary gut epithelial cells, Caco-2 cells are considered to most closely approximate primary intestinal epithelium in terms of in vitro modeling (37, 40), including pre-clinical pharmaceutical and toxicological testing (30). Furthermore, when comparing the cytomix-induced responses of HLEC and Caco-2 cells to the epithelial pathology during gram-negative sepsis, the results are comparable in that both models show the intestinal epithelium to be more susceptible to injury, with evidence of early mitochondrial alterations.
In summary, this study confirmed that the intestinal epithelium is prone to injury during gram-negative bacteremia and that mitochondrial damage is an early manifestation. Under conditions modeling acute inflammation in vitro (i.e., cytomix), reduced mitochondrial transmembrane electrochemical gradient (de-energization) corresponded with subsequent impairment of intestinal epithelial barrier function. In contrast, the lung epithelium was resistant to both mitochondrial and barrier dysfunction under these conditions. We speculate that mitochondrial dysfunction (e.g., impaired ATP production and/or increased ROS formation) may contribute to altered intestinal epithelial barrier function in the setting of sepsis. To the extent that changes in intestinal epithelial function equate with adverse clinical outcomes (e.g., bacterial translocation, impaired absorption of nutrients), it follows that cytoprotective strategies would hold promise for improving outcomes in sepsis. Indeed, recent studies suggest that interventions designed to protect intestinal epithelial mitochondria are beneficial in the context of sepsis (12, 16). Future studies designed to determine why lung epithelium is relatively resistant to injury in the context of acute inflammation may lead to the discovery of novel therapeutic targets.
Acknowledgements
The authors wish to thank Edward P. Calomeni, Kathleen S. Wolken and the university's Campus Microscopy and Imaging Facility for their technical expertise and assistance in preparing the tissue and cell samples for light and electron microscopy analyses. In addition, the authors express appreciation to the Lifeline of Ohio for the lung donation procurements.
Financial Support: National Institutes of Health (AI083912-01: EDC, HL086981-01: DLK and HL69899: RJF) and the OSU Medical Center Davis Developmental Grant (EDC).
References
- 1.Allen JN, Herzyk DJ, Allen ED, Wewers MD. Human whole blood interleukin-1-b production: kinetics, cell source, and comparison with TNF-a. J Lab Clin Med. 1992;119:538–546. [PubMed] [Google Scholar]
- 2.ARDSnetwork Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 3.Bao S, Knoell DL. Zinc modulates cytokine-induced lung epithelial cell barrier permeability. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1132–L1141. doi: 10.1152/ajplung.00207.2006. [DOI] [PubMed] [Google Scholar]
- 4.Bastarache JA, Wang L, Geiser T, Wang Z, Albertine KH, Matthay MA, Ware LB. The alveolar epithelium can initiate the extrinsic coagulation cascade through expression of tissue factor. Thorax. 2007;62:608–616. doi: 10.1136/thx.2006.063305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berthiaume Y, Matthay MA. Alveolar edema fluid clearance and acute lung injury. Respir Physiol Neurobiol. 2007;159:350–359. doi: 10.1016/j.resp.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boardman KC, Aryal AM, Miller WM, Waters CM. Actin re-distribution in response to hydrogen peroxide in airway epithelial cells. J Cell Physiol. 2004;199:57–66. doi: 10.1002/jcp.10451. [DOI] [PubMed] [Google Scholar]
- 7.Brealey D, Brand M, Hargreaves I Heales S, Land J, Smolenski R, Davies NA, Cooper CE, Singer M. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360:219–223. doi: 10.1016/S0140-6736(02)09459-X. [DOI] [PubMed] [Google Scholar]
- 8.Brown LA, Harris FL, Guidot DM. Chronic ethanol ingestion potentiates TNF-α-mediated oxidative stress and apoptosis in rat type II cells. Am J Physiol Lung Cell Mol Physiol. 2001;281:L377–L386. doi: 10.1152/ajplung.2001.281.2.L377. [DOI] [PubMed] [Google Scholar]
- 9.Burke-Gaffney A, Hellewell PG. Endogenous nitric oxide limits cytokine-induced damage of murine lung epithelial cells. Am J Physiol Lung Cell Mol Physiol. 1997;272:L707–L713. doi: 10.1152/ajplung.1997.272.4.L707. [DOI] [PubMed] [Google Scholar]
- 10.Carraway MS, Welty-Wolf KE, Kantrow SP, Huang YC, Simonson SG, Que LG, Kishimoto TK, Piantadosi CA. Antibody to E- and L-selectin does not prevent lung injury or mortality in septic baboons. Am J Respir Crit Care Med. 1998;157:938–949. doi: 10.1164/ajrccm.157.3.9707129. [DOI] [PubMed] [Google Scholar]
- 11.Chang JX, Chen S, Ma LP, Jiang LY, Chen JW, Chang RM, Wen LQ, Wu W, Jiang ZP, Huang ZT. Functional and morphological changes of the gut barrier during the restitution process after hemorrhagic shock. World J Gastroenterol. 2005;11:5485–5491. doi: 10.3748/wjg.v11.i35.5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coopersmith CM, Stromberg PE, Dunne WM, Davis CG, Amiot DM, 2nd, Buchman TG, Karl IE, Hotchkiss RS. Inhibition of intestinal epithelial apoptosis and survival in a murine model of pneumonia-induced sepsis. JAMA. 2002;287:1716–1721. doi: 10.1001/jama.287.13.1716. [DOI] [PubMed] [Google Scholar]
- 13.Coulter KR, Doseff A, Sweeney P, Wang Y, Marsh CB, Wewers MD, Knoell DL. Opposing effect by cytokines on Fas-mediated apoptosis in A549 lung epithelial cells. Am J Respir Cell Mol Biol. 2002;26:58–66. doi: 10.1165/ajrcmb.26.1.4285. [DOI] [PubMed] [Google Scholar]
- 14.Cowley RA, Mergner WJ, Fisher RS, Jones RT, Trump BF. The subcellular pathology of shock in trauma patients: studies using the immediate autopsy. Am Surg. 1979;45:255–269. [PubMed] [Google Scholar]
- 15.Crouser ED, Julian MW, Blaho DV, Pfeiffer DR. Endotoxin-induced mitochondrial damage correlates with impaired respiratory activity. Crit Care Med. 2002;30:276–284. doi: 10.1097/00003246-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Crouser ED, Julian MW, Joshi MS, Bauer JA, Wewers MD, Hart JM, Pfeiffer DR. Cyclosporin A ameliorates mitochondrial ultrastructural injury in the ileum during acute endotoxemia. Crit Care Med. 2002;30:2722–2728. doi: 10.1097/00003246-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Crouser ED, Julian MW, Dorinsky PM. Ileal VO2-DO2 alterations induced by endotoxin correlate with severity of mitochondrial injury. Am J Respir Crit Care Med. 1999;160:1347–1353. doi: 10.1164/ajrccm.160.4.9810116. [DOI] [PubMed] [Google Scholar]
- 18.Fein AM, Lippmann M, Holtzman H, Eliraz A, Goldberg SK. The risk factors, incidence and prognosis of ARDS following septicemia. Chest. 1983;83:40–42. doi: 10.1378/chest.83.1.40. [DOI] [PubMed] [Google Scholar]
- 19.Fink MP, Delude RL. Epithelial barrier dysfunction: a unifying theme to explain the pathogenesis of multiple organ dysfunction at the cellular level. Crit Care Clin. 2005;21:177–196. doi: 10.1016/j.ccc.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Frank JA, Pittet JF, Lee H, Godzich M, Matthay MA. High tidal volume ventilation induces NOS2 and impairs cAMP-dependent air space fluid clearance. Am J Physiol Lung Cell Mol Physiol. 2003;284:L791–L798. doi: 10.1152/ajplung.00331.2002. [DOI] [PubMed] [Google Scholar]
- 21.Fries W, Muja C, Crisafulli C, Cuzzocrea S, Mazzon E. Dynamics of enterocyte tight junctions: effects of experimental colitis and two different anti-TNF strategies. Am J Physiol Gastrointest Liver Physiol. 2008;294:G938–G947. doi: 10.1152/ajpgi.00469.2007. [DOI] [PubMed] [Google Scholar]
- 22.Han X, Fink MP, Uchiyama T, Yang R, Delude RL. Increased iNOS activity is essential for pulmonary epithelial tight junction dysfunction in endotoxemic mice. Am J Physiol Lung Cell Mol Physiol. 2004;286:L259–L267. doi: 10.1152/ajplung.00187.2003. [DOI] [PubMed] [Google Scholar]
- 23.Hersch M, Gnidec AA, Bersten AD, Troster M, Rutledge FS, Sibbald WJ. Histologic and ultrastructural changes in nonpulmonary organs during early hyperdynamic sepsis. Surgery. 1990;107:397–410. [PubMed] [Google Scholar]
- 24.Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Matuschak GM, Buchman TG, Karl IE. Apoptotic cell death in patients with sepsis, shock and multiple organ dysfunction. Crit Care Med. 1999;27:1230–1251. doi: 10.1097/00003246-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Huang M, Camara AK, Stowe DF, Qi F, Beard DA. Quantitative analysis of mitochondrial membrane potential measurements with JC-1. FASEB J. 2007;21:946. [Google Scholar]
- 26.Husain KD, Coopersmith CM. Role of intestinal epithelial apoptosis in survival. Curr Opin Crit Care. 2003;9:159–163. doi: 10.1097/00075198-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Johnston JD, Harvey CJ, Menzies IS, Treacher DF. Gastrointestinal permeability and absorptive capacity in sepsis. Crit Care Med. 1996;24:1144–1149. doi: 10.1097/00003246-199607000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Joshi MS, Julian MW, Huff JE, Bauer JA, Xia Y, Crouser ED. Calcineurin regulates myocardial function during acute endotoxemia. Am J Respir Crit Care Med. 2006;173:999–1007. doi: 10.1164/rccm.200411-1507OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knoell DL, Julian MW, Bao S, Besecker B, Macre JE, Leikauf GD, DiSilvestro RA, Crouser ED. Zinc-deficiency increases organ damage and mortality in a murine model of polymicrobial sepsis. Crit Care Med. 2009;37:1380–1388. doi: 10.1097/CCM.0b013e31819cefe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meunier V, Bourrie M, Berger Y, Fabre G. The human intestinal epithelial cell line Caco-2; pharmacological and pharmacokinetic applications. Cell Biol Toxicol. 1995;11:187–194. doi: 10.1007/BF00756522. [DOI] [PubMed] [Google Scholar]
- 31.Moss M, Bucher B, Moore FA, Moore EE, Parsons PE. The role of chronic alcohol abuse in the development of acute respiratory distress syndrome in adults. JAMA. 1996;275:50–54. [PubMed] [Google Scholar]
- 32.Overhaus M, Togel S, Pezzone MA, Bauer AJ. Mechanisms of polymicrobial sepsis-induced ileus. Am J Physiol Gastrointest Liver Physiol. 2004;287:G685–G694. doi: 10.1152/ajpgi.00359.2003. [DOI] [PubMed] [Google Scholar]
- 33.Pittet D, Harbarth S, Suter PM, Reinhart K, Leighton A, Barker C, Macdonald F, Abraham E. Impact of immunomodulating therapy on morbidity in patients with severe sepsis. Am J Respir Crit Care Med. 1999;160:852–857. doi: 10.1164/ajrccm.160.3.9809033. [DOI] [PubMed] [Google Scholar]
- 34.Reers M, Smith TW, Chen LB. J-aggregate formation of a carbocyanine as a quantitative fluorescent indicator of membrane potential. Biochemistry. 1991;30:4480–4486. doi: 10.1021/bi00232a015. [DOI] [PubMed] [Google Scholar]
- 35.Ritz M, Fraser R, Tam W, Dent J. Impacts and patterns of disturbed gastrointestinal function in critically ill patients. Am J Gastroenterology. 2000;95:3044–3052. doi: 10.1111/j.1572-0241.2000.03176.x. [DOI] [PubMed] [Google Scholar]
- 36.Robbins RA, Springall DR, Warren JB, Kwon OJ, Buttery LD, Wilson AJ, Adcock IM, Riveros-Moreno V, Moncada S, Polak J, Barnes PJ. Inducible nitric oxide synthase is increased in murine lung epithelial cells by cytokine stimulation. Biochem Biophys Res Commun. 1994;198:835–843. doi: 10.1006/bbrc.1994.1119. [DOI] [PubMed] [Google Scholar]
- 37.Sambuy Y, De Angelis I, Ranaldi G, Scarino ML, Stammati A, Zucco F. The Caco-2 cell line as a model of the intestinal barrier: influence of cell culture and culture-related factors on Caco-2 cell functional characteristics. Cell Biol Toxicol. 2005;21:1–26. doi: 10.1007/s10565-005-0085-6. [DOI] [PubMed] [Google Scholar]
- 38.Santa Cruz V, Dugas TR, Kanz MF. Mitochondrial dysfunction occurs before transport of tight junction deficits in biliary epithelial cells exposed to bile from methylenedianiline-treated rats. Toxicol Sci. 2005;84:129–138. doi: 10.1093/toxsci/kfi061. [DOI] [PubMed] [Google Scholar]
- 39.Schlag G, Redl H, van Vuuren CJ, Davies J. Hyperdynamic sepsis in baboons: II. Relation of organ damage to severity of sepsis evaluated by a newly developed morphological scoring system. Circ Shock. 1992;38:253–263. [PubMed] [Google Scholar]
- 40.Shah P, Jogani V, Bagchi T, Misra A. Role of Caco-2 cell monolayers in prediction of intestinal drug absorption. Biotechnol Prog. 2006;22:186–198. doi: 10.1021/bp050208u. [DOI] [PubMed] [Google Scholar]
- 41.Smith JJ, Travis SM, Greenberg EP, Welsh MJ. Cystic fibrosis airway epithelia fail to kill bacteria because of abnormal airway surface fluid. Cell. 1996;85:229–236. doi: 10.1016/s0092-8674(00)81099-5. [DOI] [PubMed] [Google Scholar]
- 42.Sugi K, Musch MW, Field M, Chang EB. Inhibition of Na+, K+-ATPase by interferon gamma down-regulates intestinal epithelial transport and barrier function. Gastroenterology. 2001;120:1393–1403. doi: 10.1053/gast.2001.24045. [DOI] [PubMed] [Google Scholar]
- 43.Swank GM, Deitch EA. Role of the gut in multiple organ failure: bacterial translocation and permeability changes. World J Surg. 1996;20:411–417. doi: 10.1007/s002689900065. [DOI] [PubMed] [Google Scholar]
- 44.Taylor FB. Baboon model of E. coli sepsis: role of phospholipids microparticles in DIC. Sepsis. 1999;3:125–133. [Google Scholar]
- 45.Tran DD, Groeneveld AB, van der Meulen J, Nauta JJ, Strack van Schijndel RJ, Thijs LG. Age, chronic disease, sepsis, organ failure, and mortality in a medical intensive care unit. Crit Care Med. 1990;18:474–479. doi: 10.1097/00003246-199005000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Unno N, Menconi MJ, Salzman AL, Smith M, Hagen S, Ge Y, Ezzell RM, Fink MP. Hyperpermeability and ATP depletion induced by chronic hypoxia or glycolytic inhibition in Caco-2BBe monolayers. Am J Physiol Gastrointest Liver Physiol. 1996;270:G1010–G1021. doi: 10.1152/ajpgi.1996.270.6.G1010. [DOI] [PubMed] [Google Scholar]
- 47.van Kaam AH, Lachmann RA, Herting E, De Jaegere A, van Iwaarden F, Noorduyn LA, Kok JH, Haitsma JJ, Lachmann B. Reducing atelectasis attenuates bacterial growth and translocation in experimental pneumonia. Am J Respir Crit Care Med. 2004;169:1046–1053. doi: 10.1164/rccm.200312-1779OC. [DOI] [PubMed] [Google Scholar]
- 48.Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–353. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 49.Vincent J, Zambon M. Why do patients who have acute lung injury/acute respiratory distress syndrome die from multiple organ dysfunction syndrome? Implications for management. Clin Chest Med. 2006;27:725–731. doi: 10.1016/j.ccm.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 50.Wang Q, Guo X, Wells-Byrum D, Noel G, Pritts TA, Ogle CK. Cytokine-induced epithelial permeability changes are regulated by the activation of the p38 mitogen-activated protein kinase pathway in cultured Caco-2 cells. Shock. 2008;29:531–537. doi: 10.1097/shk.0b013e318150737f. [DOI] [PubMed] [Google Scholar]
- 51.Ware LB. Modeling human lung disease in animals. Am J Physiol Lung Cell Mol Physiol. 2008;294:L149–L150. doi: 10.1152/ajplung.00472.2007. [DOI] [PubMed] [Google Scholar]
- 52.Watanabe E, Muenzer JT, Hawkins WG, Davis CG, Dixon DJ, McDunn JE, Brackett DJ, Lerner MR, Swanson PE, Hotchkiss RS. Sepsis induces extensive autophagic vacuolization in hepatocytes: a clinical and laboratory-based study. Lab Invest. 2009;89:549–561. doi: 10.1038/labinvest.2009.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Watts JA, Kline JA, Thornton LR, Grattan RM, Brar SS. Metabolic dysfunction and depletion of mitochondria in hearts of septic rats. J Mol Cell Cardiol. 2004;168:141–150. doi: 10.1016/j.yjmcc.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 54.Welty-Wolf KE, Carraway MS, Huang CT, Simonson SG, Kantrow SP, Piantadosi CA. Bacterial priming increases lung injury in gram-negative sepsis. Am J Respir Crit Care Med. 1998;158:610–619. doi: 10.1164/ajrccm.158.2.9704064. [DOI] [PubMed] [Google Scholar]
- 55.Yamaya M, Finkbeiner WE, Chun SY, Widdicombe JH. Differentiated structure and function of cultures from human tracheal epithelium. Am J Physiol. 1992;262:L713–L724. doi: 10.1152/ajplung.1992.262.6.L713. [DOI] [PubMed] [Google Scholar]
- 56.Zheng B, Cantley LC. Regulation of epithelial tight junction assembly and disassembly by AMP-activated protein kinase. Proc Natl Acad Sci USA. 2007;104:819–822. doi: 10.1073/pnas.0610157104. [DOI] [PMC free article] [PubMed] [Google Scholar]